Abstract
Study Design:
Retrospective cross-sectional study.
Objectives:
It is generally believed that the apical vertebra has the largest axial rotation in adolescent idiopathic scoliosis. We investigated the relationship between apical axial vertebral rotation (apicalAVR) and maximal axial vertebral rotation (maxAVR) in both major and minor curves using biplanar stereo-imaging.
Methods:
EOS 2D/3D biplanar radiograph images were collected from 332 patients with adolescent idiopathic scoliosis (Cobb angle range 10°-122°, mean age 14.7 years). Based on the X-ray images, with the help of 3D full spine reconstructions Cobb angle, curvature level, apicalAVR and maxAVR were determined. These parameters were also determined for minor curves in Lenke 2, 3, 4, 6 type patients. Maximal thoracic rotation and maximal thoracolumbar/lumbar rotation were calculated. Statistical analysis was performed with descriptive statistics, Shapiro-Wilk test, and Wilcoxon signed-rank test.
Results:
The apical vertebrae were the most rotated vertebra in only 40.4% of the major curves, and 31.7% in minor curves. MaxAVR significantly exceeded apicalAVR values in the major curves (P < .001) as well as in minor curves (P < .001). The 2 parameters differed significantly in each severity group and Lenke type.
Conclusions:
The apical vertebrae were not the most rotated vertebra in more than half of cases investigated indicating that apicalAVR and maxAVR should be considered as 2 distinct parameters, of which maxAVR fully describes the axial dimension of scoliosis. Furthermore, the substitution of maxAVR for the apicalAVR should be especially avoided in double and triple curves, as the apical vertebra was even less commonly the most rotated in minor curves.
Keywords: adolescent idiopathic scoliosis, apical vertebral rotation, maximal vertebral rotation, biplanar imaging, EOS 2D/3D
Introduction
Adolescent idiopathic scoliosis is a 3-dimensional (3D) deformity. 1 In addition to the deformity in the frontal and sagittal planes, axial rotation of the vertebrae is also present and is increasingly being addressed during evaluation. 2
At the end of the 1980s, Stokes 3 found the highest axial rotation to lie “close to” the apex of the curve, that is, at the apical vertebrae or within 2 vertebral levels of it. Later computed tomography–based investigations, however, found the apical vertebrae to be consistently the most rotated, in contrast to Stokes’s results.4,5
Since then, determination of apical axial vertebral rotation (apicalAVR) has come to be regarded as one of the most important components for radiographic evaluation of the axial dimension of scoliosis and over time the apical vertebra has come to be regarded as the de facto vertebra with the highest rotation. 6 Indeed, in the majority of studies only the apicalAVR parameter is measured and conclusions are drawn from it with regard to the efficacy of vertebral rotations of surgical treatments.7,8 As a result of such studies, apical AVR has been shown to be correlated with cosmetic and satisfaction outcomes. 6
However, there are few reports describing the degree of rotation of the maximally rotated vertebra or “maximal axial vertebral rotation” (maxAVR). Kotwicki et al 9 found maxAVR was between 10° and 24° close to the T9 vertebra in Lenke 1 patients. Charles et al 10 found the maximal thoracic vertebral rotation between T6 and T10 vertebrae, with an average of 22.7° in standing position and the maximal lumbar vertebral rotation was measured at an average of 25.8° and was found at L1 and L3 vertebrae in Lenke 3 patients.
The introduction of EOS 2D/3D imaging technology to many clinics in recent years has allowed a greater ability to make well-reproducible measurements of vertebral rotation in a standing position. 11 Furthermore, full spine 3D reconstructions can be performed at ultra-low radiation doses, an important advantage in adolescent imaging. 12 The results of one recent EOS-based study of 158 patients are consistent with the early findings of Stokes 3 that while the apical vertebra is most commonly the maximally rotated vertebra, there can be a difference of 1 or 2 segments in 9.5% of cases. 13
The purpose of this study was to determine AVRs in the major and minor curves of adolescent idiopathic scoliosis using EOS 2D/3D imaging in a larger population, and to determine if the apical vertebra was the maximally rotated. According to our hypothesis, the apical vertebrae do not always have the largest axial rotation in adolescent idiopathic scoliosis.
Patients and Methods
Patients
Following approval by institutional ethics committee, we reviewed 9872 EOS 2D/3D stereo images (EOS Imaging, Paris, France) made during the routine work of our department between 2007 and 2018 and cases were selected in which adolescent idiopathic scoliosis was the indicating diagnosis. Exclusion criteria were early onset, secondary scoliosis, prior spine surgery, or any associated musculoskeletal disease. All patients not in the required position during image capture (described below) were excluded, as this could influence rotation measurements, leaving 332 individuals.
The mean age of the population was 14.7 years (range 10-17 years) and there were 267 girls and 65 boys due to the gender-associated incidence of the disease. 14 Mean Cobb angle was 37.7° (range 10°-122°). Distribution of patients by age and scoliosis severity as per SOSORT Consensus is shown in Table 1. 15
Table 1.
Distribution of Studied Population by Age and Scoliosis Severity.
| Cobb angle | Age (years) | |||||||
|---|---|---|---|---|---|---|---|---|
| 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | |
| ≤20° | 5 | 5 | 8 | 5 | 16 | 15 | 12 | 10 |
| 21°-35° | 7 | 3 | 9 | 16 | 29 | 24 | 15 | 15 |
| 36°-40° | 0 | 0 | 2 | 3 | 3 | 3 | 6 | 2 |
| 41°-50° | 1 | 2 | 2 | 7 | 13 | 5 | 6 | 7 |
| 51°-55° | 0 | 0 | 1 | 3 | 4 | 1 | 1 | 0 |
| ≥56° | 0 | 5 | 7 | 13 | 17 | 11 | 7 | 6 |
| Sum | 13 | 15 | 29 | 47 | 82 | 59 | 47 | 40 |
Imaging Protocol and 3D Modeling
Image-pairs were captured using the EOS 2D/3D scanner, with patients in the special “knuckles on clavicles” position, which has been shown to allow more accurate 3D spine reconstructions. 16
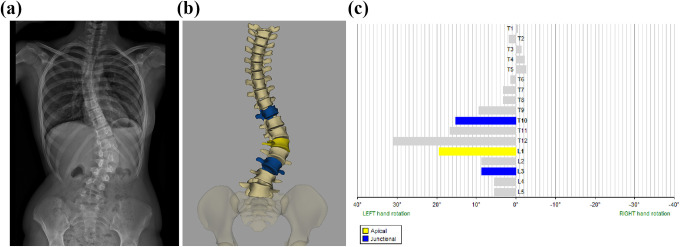
Full spine 3D reconstructions were made using sterEOS software V1.4.4.5297, which is aligned by the user to the contours of each thoracic and lumbar vertebra. 17 The software automatically calculates the Cobb angle, curvature level in addition to the serial AVR values for Th1-L5 vertebrae (Figure 1). AVR was calculated based on the axial displacement of the vertebrae relative to the pelvis, with left hand rotation defined as positive. The Cobb angle and AVR values were calculated by the software in both positive and negative ranges, so the absolute values of the parameters were used for following calculations. The apical vertebra is automatically identified by the sterEOS software in major curves and was manually determined in minor curves.
Figure 1.
(a) EOS full spine image of a patient with adolescent idiopathic scoliosis. (b) Three-dimensional (3D) reconstruction of the spine from Th1 to L5 vertebra. (c) diagrammatic representation of axial rotation of each vertebra from T1 to L5 (yellow: apical vertebra; blue: end vertebra). Images based on data from the same Lenke 5 patient.
The maxAVR and the distance from the apical vertebra were determined from the serial data on axial rotation of the vertebrae. These same parameters were also determined for minor curves in double and triple curves (Lenke 2, 3, 4, 6). Maximal thoracic rotation was determined in Lenke 1, 2, 3, and 4 patients and maximal thoracolumbar/lumbar rotation calculated in the Lenke 4, 5, and 6 groups.
Statistical Analysis
Normality of the data was ensured with Shapiro-Wilk test and the Wilcoxon signed-rank test used to assess the relationship between apicalAVR and maxAVR. Results were considered significant at P < .05. Statistical analysis was performed using SPSS v.23 (IBM Corp) software.
Results
In 198 of 332 (59.6%) cases, the maximally rotated vertebra was not the apical vertebra in the major curves, and in 56 of 82 (68.3%) minor curves. The difference between apicalAVR and maxAVR values is detailed in Table 2.
Table 2.
Differences in Degrees Between apicalAVR and maxAVR in Major and Minor Curves.
| maxAVR-apicalAVR difference | Overlap | 0°-3° | 3°-5° | 5°-10° | >10° | Total |
|---|---|---|---|---|---|---|
| Major curve | 134 | 124 | 39 | 30 | 5 | 332 |
| Minor curve | 34 | 43 | 16 | 8 | 1 | 102 |
Abbreviation: AVR, axial vertebral rotation.
Major Curves: The Relationship of Apical Vertebral Rotation to Maximal Rotation in Major Curves
The mean apicalAVR value in major curves was 12.53° ± 9.15° versus mean maxAVR of 14.33° ± 9.68° (P < .001). Vertebral level differed up to 2 levels between the apical vertebra and maximally rotating vertebra (see Table 3). Maximal thoracic rotation (in the case of Lenke 1, 2, 3, and 4 curves) was located between the Th4 and Th11 vertebrae with an average rotation of 14.75° ± 11.12°. The maximal thoracolumbar/lumbar rotation (in Lenke 4, 5, and 6 curves) was found between the Th12 and L4 vertebrae with a mean value of 13.72° ± 7.16°.
Table 3.
Major Curves: Distance Between Maximally Rotated Vertebra and Apical Vertebrae in Major Curves (Mean ± SD).
| Distance from apical vertebrae | No. of cases | apicalAVR | maxAVR | P a |
|---|---|---|---|---|
| Overlap | 134 | 14.94° ± 10.17° | 14.94° ± 10.17° | — |
| 1 | 182 | 10.89° ± 8.16° | 13.91° ± 9.59° | <.001* |
| 2 | 16 | 10.87° ± 6.24° | 14.23° ± 6.16° | <.001* |
| Total | 332 | 12.53° ± 9.15° | 14.33° ± 9.68° | <.001* |
Abbreviation: AVR, axial vertebral rotation.
a P value is the result of Wilcoxon signed-rank test, P < .05 (*) was accepted as significant.
Data on apicalAVR and maxAVR in patient groups of varying severity is shown in Table 4. The relationship between the 2 examined parameters based on Lenke classification is detailed in Table 5.
Table 4.
Relationship Between apicalAVR and maxAVR in Different Severity Groups (Mean ± SD).
| Cobb angle | No. of cases | apicalAVR | maxAVR | P a |
|---|---|---|---|---|
| ≤20° | 76 | 6.70 ± 4.55° | 8.27 ± 4.46° | <.001* |
| 21°-35° | 118 | 9.34 ± 5.14° | 10.81 ± 4.90° | <.001* |
| 36°-40° | 19 | 16.36 ± 7.30° | 17.80 ± 6.95° | .008* |
| 41°-50° | 43 | 15.67 ± 5.07° | 17.27 ± 5.07° | <.001* |
| 51°-55° | 10 | 15.84 ± 5.77° | 19.10 ± 6.63° | .018* |
| ≥56° | 66 | 21.27 ± 13.05° | 23.97 ± 14.07° | <.001* |
| Total | 332 | 12.53 ± 9.15° | 14.33 ± 9.68° | <.001* |
Abbreviation: AVR, axial vertebral rotation.
a P value is the result of Wilcoxon signed-rank test, P < .05 (*) was accepted as significant.
Table 5.
ApicalAVR and maxAVR Values Based on Lenke Classification (Mean ± SD).
| Lenke type | No. of cases | apicalAVR | maxAVR | P |
|---|---|---|---|---|
| 1 | 112 | 11.29° ± 8.89° | 13.39° ± 10.11° | <.001* |
| 2 | 27 | 16.75° ± 4.49° | 17.94° ± 3.58° | <.001* |
| 3 | 54 | 16.01° ± 13.6° | 17.5° ± 13.55° | <.001* |
| 4 | 3 | 20.33° ± 6.16° | 22.98° ± 5.32° | .109 |
| 5 | 120 | 11.02° ± 6.4° | 12.63° ± 6.43° | <.001* |
| 6 | 16 | 18.32° ± 5.9° | 20.93° ± 7.55° | .005* |
| Total | 332 | 12.53° ± 9.15° | 14.33° ± 9.68° | <.001* |
Abbreviation: AVR, axial vertebral rotation.
a P value is the result of Wilcoxon signed-rank test, P < .05 (*) was accepted as significant.
Minor Curves: The Relationship of Apical Vertebral Rotation to Maximal Rotation in Minor Curves
For structural minor curves, apicalAVR was 9.29° ± 6.95°, while maxAVR was found to be 11.21° ± 7.44° (P < .001). The relationship between the identified apical vertebrae to maximal rotation in minor curves is shown in Table 6.
Table 6.
Minor Curves: Distance between maximally rotated vertebra and apical vertebrae in minor curves (mean ± standard deviation). P-value is the result of Wilcoxon signed-rank test, p<0.05 was accepted as significant.
| Distance from apical vertebrae | No. of cases | apicalAVR | maxAVR | P |
|---|---|---|---|---|
| 0 | 34 | 8.92° ± 5.59° | 8.92° ± 5.59° | — |
| 1 | 59 | 10.06° ± 7.80° | 12.35° ± 8.07° | <.001* |
| 2 | 9 | 5.87° ± 4.46° | 11.76° ± 7.87° | <.001* |
| Total | 102 | 9.29° ± 6.95° | 11.21° ± 7.44° | <.001* |
Abbreviation: AVR, axial vertebral rotation.
a P value is the result of Wilcoxon signed-rank test, P < .05 (*) was accepted as significant.
The maximal thoracic rotation was 6.93° ± 7.62° in the minor curves of Lenke 2, 4, and 6 patients. Thoracolumbar/lumbar maximal rotation was found to be 13.18° ± 6.51° in the case of Lenke 3 and 4 minor curves.
Discussion
Rotational parameters can be a useful feature in monitoring scoliosis progression and assessing treatment outcomes.18,19 Several authors have developed scoliosis classifications that incorporate vertebral rotation in an attempt to describe all 3 dimensions of the curves; however, the apicalAVR parameter is commonly the only feature used to describe the axial dimension of the scoliosis.20,21
In this study, we found that the apical vertebra was not the most rotated in the majority of cases (59.6% of cases, 134 of 332 cases, see Table 1). Almost 54% of individuals (182 of 332) had maximal rotation in the vertebra adjacent to the apical vertebrum, and at a distance of 2 levels vertebra in 4.8% (16 of 332) of main curves and 8.8% (9/102) of minor curves. A similar range was reported by Stokes 3 in 1989 and more recently by Labaki et al. 13
Furthermore, significant differences in the magnitude of rotation between the apicalAVR and the maxAVR values were seen in both major and minor curves. This, alongside a similar finding by Labaki et al, 13 suggests that in a significant number of cases the apical vertebra should not considered to be the most rotated, in contrast to the general belief since the early 1990s.4,5
A significant difference between apicalAVR and maxAVR was seen across all severity groups and most Lenke classification groups. While a minor difference between the rotational parameters may not be of clinical significance, a difference of more than 5° could be detected in 10.5% (35 of 332) of curves. Although data describing a threshold for clinical importance is not available in the literature, Pankowski et al 22 recommended the use of direct vertebral rotation over the single concave rod rotation method due to an average 3.1° improvement in rotation, considerably less than the 5° margin for clinical effect theorized in our analysis. 22
The AVR of the minor curvature is not commonly measured in practice; however, with the sterEOS software it can easily be estimated. Minor curves exhibited an even larger qualitative difference than major curves with a maximally rotated apical vertebra in 30.0% (34 of 102) of cases, and a similar rate of 8.8% of minor curves exhibiting a >5° difference (9 cases). However, the definition of the apical vertebra as the vertebra most laterally displaced from the central sacral vertical line appears not to be a useful one as it is much less commonly the maximally rotated segment, as it does not have the same influence as the major curve. This was seen in our data, with the high number of cases in which the level of the maximal and apical vertebrae differed. As a result, apicalAVR appears to be even less suitable for describing rotation in minor curves.
Group mean values for maximal thoracic, thoracolumbar and lumbar rotation were lower than those found in the literature9,10; however, this may be due to the fact that scoliosis patients not reaching the indication for surgery were also included. A wider range for maximal rotation was seen than that described in previous studies, with Th4-Th5, Th11-12, and L4 vertebrae also observed.9,10 This would indicate to us that a maximally rotated vertebra can occur anywhere from Th4 to L4 in adolescent idiopathic scoliosis.
The retrospective nature of the study is a limitation, but we believe that as the radiological examinations was performed in a standardised position, similar results would be produced in prospective study. The possibility of measurement error may also exist, which we aimed to reduce by examining a high number of patients. It was felt that the sterEOS software could be improved further, as at present the apical point is always defined as a vertebra, although an intervertebral disc may often lie in the apical position. While it is still routine to always refer to a vertebra as the most rotated structure, we feel this is a point that could be refined in future updates of the software. Our values in the less common Lenke 4 group were not statistically evaluable due to the low number of elements.
Our results aim to provide a basis for a more accurate understanding of the axial dimension of adolescent scoliosis and emphasise that the maxAVR parameter may characterise axial deformation more accurately than the apicalAVR. We believe that due to a statistically significant difference and possible clinical difference reported here and in one other recent study, 13 this justifies the consideration of maxAVR in 3D scoliosis classifications in place of apicalAVR, especially in the case of minor curves. Moreover, our results also indicate the need for a discussion and possible reevaluation of the many studies where only apicalAVR was used to describe the rotation component.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the ÚNKP-19-3 New National Excellence Program of the Ministry for Innovation and Technology.
ORCID iD: Kristóf József, MD  https://orcid.org/0000-0002-0369-703X
https://orcid.org/0000-0002-0369-703X
References
- 1.Mehta MH. Radiographic estimation of vertebral rotation in scoliosis. J Bone Joint Surg Br. 1973;55:513–520. [PubMed] [Google Scholar]
- 2.Perdriolle R, Vidal J. Morphology of scoliosis: three-dimensional evolution. Orthopedics. 1987;10:909–915. [DOI] [PubMed] [Google Scholar]
- 3.Stokes IA. Axial rotation component of thoracic scoliosis. J Orthop Res. 1989;7:702–708. [DOI] [PubMed] [Google Scholar]
- 4.Marchesi DG, Transfeldt EE, Bradford DS, Heithoff KB. Changes in vertebral rotation after Harrington and Luque instrumentation for idiopathic scoliosis. Spine (Phila Pa 1976). 1992;17:775–780. [DOI] [PubMed] [Google Scholar]
- 5.Willers U, Transfeldt EE, Hedlund R. The segmental effect of Cotrel-Dubousset instrumentation on vertebral rotation, rib hump and the thoracic cage in idiopathic scoliosis. Eur Spine J. 1996;5:387–393. [DOI] [PubMed] [Google Scholar]
- 6.Jankowski PP, Yaszay B, Cidambi KR, Bartley CE, Bastrom TP, Newton PO. The relationship between apical vertebral rotation and truncal rotation in adolescent idiopathic scoliosis using 3D reconstructions. Spine Deform. 2018;6:213–219. [DOI] [PubMed] [Google Scholar]
- 7.Ilharreborde B, Sebag G, Skalli W, Mazda K. Adolescent idiopathic scoliosis treated with posteromedial translation: radiologic evaluation with a 3D low-dose system. Eur Spine J. 2013;22:2382–2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kato S, Debaud C, Zeller RD. Three-dimensional EOS analysis of apical vertebral rotation in adolescent idiopathic scoliosis. J Pediatr Orthop. 2017;37:e543–e547. [DOI] [PubMed] [Google Scholar]
- 9.Kotwicki T. Sagittal and transversal plane deformity in thoracic scoliosis. Stud Health Technol Inform. 2002;91:251–256. [PubMed] [Google Scholar]
- 10.Charles YP, Bouchaïb J, Walter A, Schuller S, Sauleau EA, Steib JP. Sagittal balance correction of idiopathic scoliosis using the in situ contouring technique. Eur Spine J. 2012;21:1950–1956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Aubaidi Z, Lebel D, Oudjhane K, Zeller R. Three-dimensional imaging of the spine using the EOS system: is it reliable? A comparative study using computed tomography imaging. J Pediatr Orthop B. 2013;22:409–412. [DOI] [PubMed] [Google Scholar]
- 12.Illés T, Somoskeöy S. The EOS™ imaging system and its uses in daily orthopaedic practice. Int Orthop. 2012;36:1325–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Labaki C, Otayek J, Massaad A, et al. Is the apical vertebra the most rotated vertebra in the scoliotic curve? J Neurosurg Spine. Published online August 23, 2019. doi:10.3171/2019.6.SPINE19203 [DOI] [PubMed] [Google Scholar]
- 14.Konieczny MR, Senyurt H, Krauspe R. Epidemiology of adolescent idiopathic scoliosis. J Children’s Orthop. 2012;7:3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Negrini S, Donzelli S, Aulisa AG, et al. 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018;13:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pasha S, Capraro A, Cahill PJ, Dormans JP, Flynn JM. Bi-planar spinal stereoradiography of adolescent idiopathic scoliosis: considerations in 3D alignment and functional balance. Eur Spine J. 2016;25:3234–3241. [DOI] [PubMed] [Google Scholar]
- 17.Rehm J, Germann T, Akbar M, et al. 3D-modeling of the spine using EOS imaging system: Inter-reader reproducibility and reliability. PLoS One. 2017;12:e0171258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nault ML, Mac-Thiong JM, Roy-Beaudry M, Turgeon I. Three-dimensional spinal morphology can differentiate between progressive and nonprogressive patients with adolescent idiopathic scoliosis at the initial presentation: a prospective study. Spine (Phila Pa 1976). 2014;39:E601–E606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cobetto N, Aubin CÉ, Parent S, Barchi S, Turgeon I, Labelle H. 3D correction of AIS in braces designed using CAD/CAM and FEM: a randomized controlled trial. Scoliosis Spinal Disord. 2017;12:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sangole AP, Aubin CE, Labelle H, et al. Three-dimensional classification of thoracic scoliotic curves. Spine (Phila Pa 1976). 2009;34:91–99. [DOI] [PubMed] [Google Scholar]
- 21.Kadoury S, Labelle H. Classification of three-dimensional thoracic deformities in adolescent idiopathic scoliosis from a multivariate analysis. Eur Spine J. 2012;21:40–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pankowski R, Roclawski M, Ceynowa M, Mikulicz M, Mazurek T, Kloc W. Direct vertebral rotation versus single concave rod rotation: low-dose intraoperative computed tomography evaluation of spine derotation in adolescent idiopathic scoliosis surgery. Spine (Phila Pa 1976). 2016;41:864–871. [DOI] [PubMed] [Google Scholar]