Abstract
Study Design:
Systematic review.
Objectives:
Osteoporosis is one of the most common diseases of the elderly, whereby vertebral body fractures are in many cases the first manifestation. Even today, the consequences for patients are underestimated. Therefore, early identification of therapy failures is essential. In this context, the aim of the present systematic review was to evaluate the current literature with respect to clinical and radiographic findings that might predict treatment failure.
Methods:
We conducted a comprehensive, systematic review of the literature according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) checklist and algorithm.
Results:
After the literature search, 724 potentially eligible investigations were identified. In total, 24 studies with 3044 participants and a mean follow-up of 11 months (range 6-27.5 months) were included. Patient-specific risk factors were age >73 years, bone mineral density with a t-score <−2.95, BMI >23 and a modified frailty index >2.5. The following radiological and fracture-specific risk factors could be identified: involvement of the posterior wall, initial height loss, midportion type fracture, development of an intravertebral cleft, fracture at the thoracolumbar junction, fracture involvement of both endplates, different morphological types of fractures, and specific MRI findings. Further, a correlation between sagittal spinal imbalance and treatment failure could be demonstrated.
Conclusion:
In conclusion, this systematic review identified various factors that predict treatment failure in conservatively treated osteoporotic fractures. In these cases, additional treatment options and surgical treatment strategies should be considered in addition to follow-up examinations.
Keywords: osteoporotic fracture, treatment failure, compression fracture, risk factor
Objectives
Osteoporosis is one of the most common diseases in the elderly population today. For a long time, its socio-economic importance was underestimated, but it has become more and more important in recent years.1,2 One of the major clinical consequences is the appearance of various bone fractures. Vertebral compression fractures are especially important, in particular compression fractures of both endplates. Even today, the consequences for patients suffering this fracture type are underestimated due to the fracture-related ventralization of the body’s center of gravity and, as a result, increased torque above the fracture might. This requires a significant increase in back muscle forces to maintain balance and an increased pressure load on the adjacent end plates, leading to a five-fold increased risk of fracture of the adjacent vertebral bodies as a result. The devastating consequences are reflected in the downward spiral described by Gold back in 1996. 3 He postulated that fracture-related changes lead to a decrease in the vital capacity of the lungs, the restriction of mobility and further bone loss with the consecutive occurrence of new fractures. Ultimately, this course results in increased mortality. 3 According to Johnell et al., the 5-year mortality rate after a vertebral fracture is 72%. In comparison, after hip fracture, the rate is “only” 59%. 4 Therefore, sufficient treatment is essential to maintain quality of life and to avoid a complicated course as described by Gold. In most cases, a conservative procedure including pain control, bracing, early rehabilitation and osteoporotic treatment is the treatment of choice. The results of this approach are promising with a high rate of fracture healing, minor residual deformity and satisfactory functional recovery. However, in some cases, prolonged pain and other serious complications, like non-union, vertebral collapse, neurological deficits and kyphotic deformity can be observed.
In order to avoid the above-mentioned hazards, early identification of therapy failures is essential. Numerous clinical and radiographic investigations have identified risk factors that might predict treatment failure with the conservative treatment of osteoporotic vertebral fracture. With this knowledge, fractures with a high risk of failure could be identified early and treated adequately.
In this context, the aim of the present systematic review was to evaluate the current literature with respect to clinical and radiographic findings that might predict treatment failure and high complication rates after conservative treatment of osteoporotic vertebral fracture.
Material and Methods
Study Design
We conducted a comprehensive, systematic review of the literature according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) checklist and algorithm. 5
Study Characteristics
Investigations between 2000 to 2020 were included. For analyses, prospective and retrospective observational investigations were considered.
Information Source
The authors performed an initial search of PubMed and Google databases for investigations for possible inclusion in the review.
Search
The keywords used in the research were “(osteoporotic vertebral fracture OR osteoporotic compression fracture OR osteoporotic spinal fracture) AND (pseudoarthrosis OR non-union OR conservative treatment failure OR vertebral collapse OR intravertebral cleft) AND (English OR German) NOT (cervical spine).”
Study Selection
The authors limited the research to observational studies, while systematic reviews, meta-analyses, case series and case reports were excluded. Titles and abstracts were independently reviewed by 2 authors (MJS, UJAS). Duplicates were removed and full texts were checked for suitability. In cases where a decision could not be taken based on information from the title and abstract, the full text was evaluated. The final decision was made based on the analysis of the full text.
Data Items
The main prerequisite was that the included studies investigated conservatively treated osteoporotic vertebral fractures, confirmed by clinical and radiologic diagnostics. Studies were selected according the following inclusion criteria: (a) presence of an osteoporotic vertebral fracture, (b) conservative therapy regime and (c) investigation of one or more primary outcome parameters. Definition of treatment failure and therefore primary outcome parameters were non-union (pseudoarthrosis), intravertebral cleft, kyphotic deformity, neurological complications and vertebral collapse. Studies that handled other pathological fractures caused by metastatic disease, myeloma or spondylodiscitis were excluded, as well as those including patients with sequential fractures after vertebroplasty or kyphoplasty.
Synthesis of Results
We extracted data concerning study characteristics including authors’ names, title, year of publication, journal of publication, number of patients, time of follow-up and type of study. For the description of the study population number of patients, sex and age were collected. Outcome parameters were analyzed according inclusion criteria and were assigned to 4 groups: (i) patient specific risk factors, (ii) fracture specific risk factors, (iii) radiological risk factors and (iv) others. For all included studies we used the Oxford Centre for Evidence-Based Medicine 2011 for defining the level of evidence. 6
Results
Study Characteristics
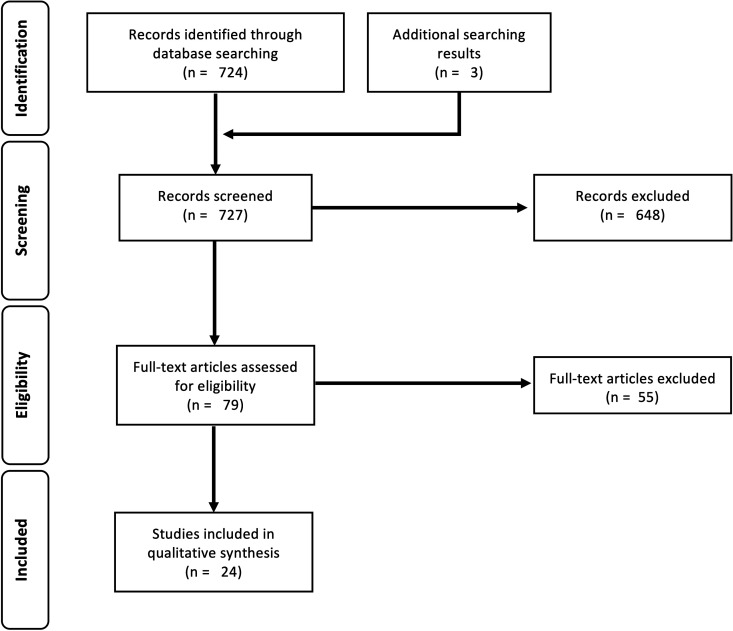
The initial research identified 724 potentially eligible scientific publications in both databases and 3 additional publications. Among these, 648 were excluded after screening of the titles and abstracts because they did not meet the inclusion criteria. After screening the full-text articles, a further 55 were excluded (Figure 1). Therefore, a total of 24 studies were finally included in the systematic review and were analyzed. Full-selection process is shown in PRISMA flow chart in Figure 1.
Figure 1.
PRISMA flow chart.
In summary, 3044 participants with a mean follow-up time of 11 months (range 6-27.5) were analyzed within this systematic review. All investigations were published in the English language and had a cohort design. Eleven were retrospective investigations, while 13 prospective studies. Table 1 shows the study characteristics of the included investigations.
Table 1.
Study Characteristics of the Included Investigations.
| Study | Year | Study design | Sample size (n) | Follow up | Predictors of failure | Outcome parameter | Level of evidence |
|---|---|---|---|---|---|---|---|
| Lee et al. 7 | 2012 | Prospective | 259 | 1-year | Patient age >78.5 years | pain relief | 2 |
| t score <−2.95 | |||||||
| BMI >25.5 kg/m2 | |||||||
| Final height loss >28.5% | |||||||
| Zhang et al. 8 | 2019 | Retrospective | 173 | >6 months | Patient age >73.5 years | Pain relief | 3 |
| BMI >23.65 kg/m2 | Bed-rest related com-plications | ||||||
| BMD −3.45 | |||||||
| Modified frailty index 2.5 | |||||||
| Shah et al. 9 | 2016 | Prospective | 30 | 9 months | Patient age | Neurologic compromise | 2 |
| Higher kyphotic angle | Vertebral collapse | ||||||
| Pain relief | |||||||
| Goldstein et al. 10 | 2016 | Retrospective | 153 | 15 months | Patient age | 3 | |
| Final height loss | |||||||
| Kyphotic angle differences | |||||||
| Hoshino et al. 11 | 2013 | Prospective | 362 | 6 months | Middle column injury | 2 | |
| Female sex | |||||||
| Patient age | |||||||
| Previous use of steroids | |||||||
| Low mini-mental state | |||||||
| Park et al. 12 | 2018 | Retrospective | 60 | Initial kyphotic angle | Neurologic compromise | 3 | |
| Initial height loss | |||||||
| Intravertebral cleft | |||||||
| Posterior wall involvement | |||||||
| Midportion type (MRI) | |||||||
| Thoracolumbar level | |||||||
| Aortic calcification | |||||||
| Hayashi et al. 13 | 2016 | Prospective | 36 | Morphology of the injured posterior wall | Neurologic compromise | 2 | |
| Tsujio et al. 14 | 2011 | Prospective | 350 | 6 months | Thoracolumbar spine | Non-union | 2 |
| Middle-column injury | |||||||
| Confined high intensity in T2-weighted MRI | |||||||
| Diffuse low intensity in T2-weighted MRI | |||||||
| Ito et al. 15 | 2002 | Retrospective | 28 | Intravertebral cleft | Neurologic compromise | 3 | |
| Vertebral collapse | |||||||
| Sugita et al. 16 | 2005 | Retrospective | 73 | 23.4 months | Intravertebral cleft | Pain | 3 |
| Swelled-front type | Vertebral collapse | ||||||
| Bow-shaped type | |||||||
| Projecting type | |||||||
| Seao et al. 17 | 2017 | Retrospective | 97 | >12 months | Involvement of both endplates | Vertebral collapse | 3 |
| Diffuse signal change in T1-weighted MRI | Neurologic compromise | ||||||
| Patil et al. 18 | 2014 | Retrospective | 64 | 27.5 months | Involvement of superior endplate | Kyphotic deformity | 3 |
| Anterior cortical wall fracture | |||||||
| Adjacent fracture | |||||||
| Ha et al. 19 | 2013 | Prospective | 75 | 6 months | >15% increase in height loss | Vertebral collapse | 2 |
| >10° increase in kyphotic angle | Pain | ||||||
| Midportion type fracture | |||||||
| Involvement of posterior wall | |||||||
| Nakamae et al. 20 | 2017 | Prospective | 217 | Vertebral instability | Neurological deficit | 2 | |
| Pain | |||||||
| Wakao et al. 22 | 2018 | Prospective | 30 | >12 months | Changes of kyphotic angle | Need for surgery | 2 |
| Mobility of collapsed vertebrae | |||||||
| EuroQol questionnaires | |||||||
| Numerical rating scale | |||||||
| Cho et al. 21 | 2013 | Prospective | 62 | Prone cross-table lateral radiographs | IVC | 2 | |
| Smorgick et al. 22 | 2020 | Retrospective | 124 | 14 months | Spinopelvic configuration | Height loss | 3 |
| Iwata et al. 24 | 2016 | Prospective | 48 | 6 months | Global spinal malalignment | Non-union | 2 |
| Ohnishi et al. 25 | 2018 | Retrospective | 46 | Ventralization of C7 plumb line | Vertebral collapse | 3 | |
| Kanchiku et al. 27 | 2014 | Retrospective | 109 | 6 months | Total type fracture in T1-weighted MRI | Vertebral collapse | 3 |
| Wide type fracture in T2-weighted MRI | Non-union | ||||||
| Neurologic deficit | |||||||
| Omi et al. 32 | 2014 | Prospective | 63 | STIR sequence | Non-union | 2 | |
| Kyphosis | |||||||
| Back pain | |||||||
| Kataoka et al. 28 | 2017 | Prospective | 69 | 4 weeks | Early physical activity | Pain | 2 |
| Ha et al. 29 | 2016 | Prospective | 105 | 3 months | Use of bisphosphonate | Inter-vertebral cleft | 2 |
| Fujimoto et al. 30 | 2017 | Retrospective | 411 | Termination level of conus medullaris | Neurologic deficit | 3 |
Patient-Specific Risk Factors
Older age (>78.5 years), severe osteoporosis (t-score <−2.95), overweight (BMI >25.5 kg/m2) and larger collapse rates (>28.5%) were risk factors for failed conservative treatment reported by Lee et al. 7 Zhang et al. found comparable results with different limits. 8 Their logistic regression analysis revealed that age >73.5 years, bone mineral density <−3.45, BMI >23.65 kg/m2 and a modified Frailty Index (mFI) >2.5 (out of 11 variables) were high-risk factors for conservative treatment failure. 80% of the patients having an mFI >3 had bed rest-related complications. Other investigations confirmed that especially higher age is a significant risk factor for severe vertebral collapse and higher kyphotic angle.9,10
How far initial conservative treatment interventions influence patient outcomes was investigated by Hoshino et al. 11 In this report, 362 patients were enrolled in a prospective multicenter study. Female sex and advanced age were associated with an SF-36 physical component summary (PCS) ≤ 40. Low Mini-Mental State Examination scores at enrolment were associated with an SF-36 PCS ≤ 40 and reduced activities of daily living. The previous use of steroids was associated with an SF-36 mental component summary (MCS) ≤40, prolonged back pain, and vertebral collapse.
In all included investigations, gender, multivertebral fractures, combination with previous fractures and pre-treatment VAS scores were not risk factors for failure.
Fracture-Specific Risk Factors
A total of 11 studies dealt with fracture-specific risk factors for the conservative treatment of osteoporotic vertebral body fractures.
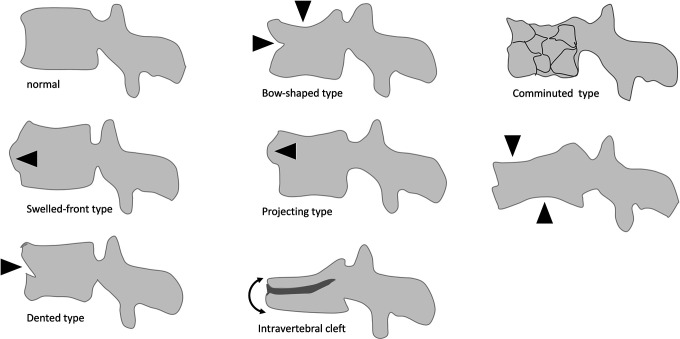
Four studies investigated risk factors for the occurrence of delayed neurologic deficits in patients.12-15 Two of these identified posterior wall involvement as a risk factor.13,14 Additionally, initial height loss, midportion type fractures, swelled front type as well as dented type fractures in accordance with Sugita et al. (Figure 2), complex fracture morphology, development of an intravertebral cleft, fracture instability, fractures at the thoracolumbar junction, and specific MRI changes that will be mentioned later in the text were listed12-16
Figure 2.
Another investigation looked at risk factors for vertebral collapse and spinal canal compromise resulting in neurologic symptoms. 17 They concluded that posterior vertebral body height loss, fracture involvement of both endplates and specific MRI changes conferred higher risk.
Two studies reported risk factors for poor clinical outcomes defined as moderate to severe pain or vertebral collapse.11,16 Risk factors were the following: bow-shaped type fractures, projecting type fractures and swelled front type fractures (Figure 2). Hoshino et al. defined poor outcomes either as low physical component scores (SF 36), a low level of independence or high pain levels. Risk factors were posterior wall fractures, particularly comminuted fracture types. 11
Three studies looked for risk factors for progressive vertebral collapse or progressive kyphosis. 10 Two investigations identified both the location at the thoracolumbar junction and midportion type fractures as risk factors.18,19 Development of an intravertebral cleft (IVC), A2 as well as A4 fracture type according to AO Spine, posterior wall fractures, involvement of the superior endplate, anterior wall fracture, and adjacent level fractures were further risk factors.101 819 One study looked at risk factors for the development of a symptomatic intravertebral cleft after conservative treatment. 20 The authors found posterior wall fracture and vertebral instability as risk factors.
Radiological Risk Factors
Conventional radiological imaging
A lateral conventional radiograph in the standing position is considered the primary tool to detect sintering and segmental kyphosis. However, its benefit in predicting the failure of conservative therapy remains unclear. Two retrospective and one prospective multicenter investigations were able to identify 2 risk factors.
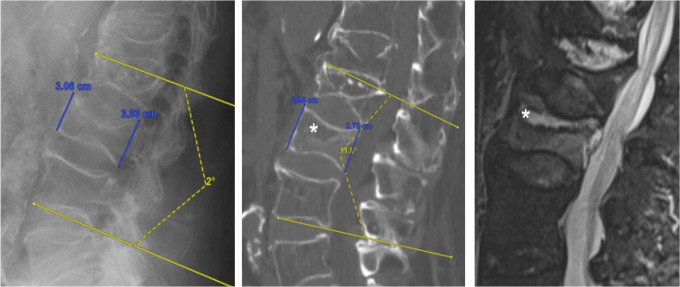
Firstly, the appearance of an intravertebral cleft (IVC) well-presented in additional functional images or in lateral radiographs in the prone position was associated with the occurrence of non-union (Figure 3). 21 Following the results of a multicenter study on 350 patients, the associated destruction of the central column was the main predictive factor for an unstable non-union. 17
Figure 3.
Intravertebral cleft with consecutive spinal instability illustrated with a comparison of the supine position (CT and MRT) to the standing position.
Secondly, Nakamae et al. demonstrated in a retrospective investigation on 97 patients with osteoporotic vertebral fracture that the involvement of both endplates and the posterior wall on conventional radiographs have a higher tendency to collapse in the further course of conservative treatment. 20
Wakao et al. investigated patients with failed initial conservative treatment over a period of 3 months. 22 Risk factors for treatment failure were relevant fracture instability in extension and flexion radiographs.
Sagittal balance
Various investigations about osteoporotic vertebral fractures examined the relationships between spinopelvic parameters and fracture level, AO type or loss of height, respectively. Smorgick et al. evaluated 124 patients and found no significant correlation between pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), AO type or height loss of the fracture. 23
Looking at the rate of bony fusion, Iwata et al. evaluated 48 conservatively treated osteoporotic vertebral body fractures after 6 months. 24 They demonstrated that a PI minus LL (lumbar lordosis) over 30° and a distance of the C7 plumb line to the center of the fractured vertebral body (DSVA) over 5 cm were significant risk factors for lack of non-union. In a follow-up investigation by the same group, DSVA turned out to be a significant risk factor for vertebral collapse. 25
Finally, Kao et al. demonstrated that a PT over 27°, a sagittal vertebral axis (SVA) over 50 mm, a DSVA over 60 mm and a PI lower or higher than 40° to 60° were associated with increased pain, instability and failure of conservative therapy. 26
Magnetic resonance imaging
Fracture morphology
Tsujio et al. performed a prospective study and identified middle-column factures diagnosed by MRI as a prognostic risk factor for non-union. 14 Hoshiono et al. confirmed the diagnostic value of MRI and the prognostic significance of middle-column fractures. 11 Furthermore, other fracture morphology related aspects such as the intravertebral gap, vertebral split or endplate involvement are discussed elsewhere in this manuscript.
A further risk factor for failure of conservative treatment is the presence of multiple osteoporotic vertebral fractures by itself, regardless whether these were diagnosed at once or in combination with old fractures. 8 Therefore, the prognostic value of MRI to distinguish between fracture age in cases of multiple fractures is in this context rather low.
MRI sequences
The posterior vertebral height loss indicates failure of conservative therapy in patients with osteoporotic vertebral fractures. A diffuse low signal change in the sagittal plane of a T1-weighted MRI scan predicts posterior height loss and should be carefully evaluated in the initial imaging evaluation. 17 Furthermore, a prognostic classification for vertebral non-union has been established for T1-weighted MRI in combination with T2-weighted images. 27 The sole presence of confined high intensity or a diffuse low intensity area within the fractured vertebra in T2-weighted MRI images is an additional risk factor for non-union.
Other Risk Factors
Other potential risk factors that have been investigated include the timing of return to physical activity and medication with bisphosphonates.28-30 Kataoka et al. performed an observational investigation and found no association between early physical activity and progression of the fractured vertebral body’s collapse. 28 In a prospective study with 105 patients included, bisphosphonate use had no impact on pain and functional results during the conservative treatment of osteoporotic vertebral fractures. However, a history of bisphosphonate medication was associated with the occurrence of the intravertebral cleft sign. 29
Conclusion
From both socio-economic and individual points of view, osteoporosis is one of the major health burdens nowadays.1,2 Especially vertebral compression fractures, in particular compression fractures of both endplates, are frequent. However, the consequences for patients suffering this fracture type are still underestimated. Therefore, besides adequate osteoporotic treatment, early recognition of associated complications and treatment failure is the only solution to maintain quality of life, mobility and to avoid a complicated course.
According to our own experiences, the main reasons for therapy failure after conservative treatment were the wrong indication, missing follow-up controls as well as initially overlooked fractures. In those cases, multisegmental fractures or non-union with significant substance defects with consecutive instability (Figure 3), extensive vacuum phenomena in the affected vertebrae and severe post-traumatic kyphoses (> 25° in bisegmental base plate angle) could be observed.
In addition to the early detection of a progress, it is even more important to identify appropriate fractures that pose a high risk of treatment failure. It has to be emphasized that the presence of one or more of those factors is not a contraindication for conservative treatment. However, the affected patient as well as the treating physician should be aware of the potential risks and check-ups should be done more regularly.
In this context, previous investigations identified older age, severe osteoporosis and overweight as potential patient specific risk factors.7,8 The different defined cut-off values between the cited studies could be explained by different study populations with consecutive differences in life expectancy and culture (Republic of Korea versus China). In conclusion, age >73 years, bone mineral density t <−2.95 and BMI >23 have to be mentioned. Additionally, the previous use of steroids was associated with SF-36 MCS ≤40, prolonged back pain and vertebral collapse. 11
Accordingly, the occurrence of neurologic deficits, involvement of the posterior wall, initial height loss, midportion type fractures, complex fracture morphology, development of an intravertebral cleft, fracture instability, and fractures at the thoracolumbar junction were independent risk factors.12-15 Furthermore, the change of the anatomical relation between the vertebral column and the spinal cord due to fracture-related deformity is an underestimated factor. 30 Especially, changes in the context of fractures can cause variations in the termination level of the medullary cone, which may pose a risk factor for delayed neurological deterioration. 30
With a focus on vertebral collapse and kyphosis, posterior vertebral body height loss, fracture involvement of both endplates, location at the thoracolumbar junction, AO Spine type A4 fracture as well as adjacent level fractures were negative prognostic factors.101 720 Furthermore, Sugita defined different types of fractures, whereby bow-shaped type fractures, projecting type fractures and swelled front type fractures were associated with higher rates of vertebral collapse. 16
In terms of sagittal balance, the DSVA turned out to be a significant risk factor for vertebral collapse development. 25 As a result of the associated spinal imbalance, there is increased strain on the muscles with subsequent fatigue and functional restrictions. 31 A diffuse low signal change in the sagittal plane of a T1-weighted MRI scan predicts posterior height loss and should be carefully evaluated in the initial imaging evaluation. 17 Furthermore, a stronger signal in the STIR sequence can predict the appearance of kyphosis pain. 32
Risk factors for poor outcomes are low physical component scores (SF-36), a low level of independence and high pain levels, as well as posterior wall fractures, particularly comminuted fracture types as well as a PT over 27°, an SVA over 50 mm, a DSVA over 60 mm and a PI lower or higher than 40°-60°.11,26
With regard to the development of non-union, the appearance of an IVC as well as the destruction of the central column seem to be the main predictive factors.81 114 Iwata et al. analyzed a possible correlation with sagittal parameters and demonstrated that a PI-LL over 30° and a DSVA over 5 cm were further predictive factors for non-union. 24
Interestingly, the fracture age of additional vertebral fracture seems to be irrelevant. Regardless of whether these were diagnosed at once or in combination with older fractures, both situations represent a risk factor for the failure of conservative treatment. 8
The use of bisphosphonates had no impact on pain and functional results during conservative treatment for osteoporotic vertebral fractures, but was associated with the occurrence of intravertebral cleft signs. 29 Based on these findings, the authors suggested the suspension of bisphosphonate medication during the fracture healing period for acute fractures. This suggestion has been challenged by a recent systematic review on the effect of osteoporosis medication on fracture healing. 33
This systematic review has some limitations. First, the definition of treatment failure was not consistent in most investigations. Second, study designs, study population and follow-up vary between the included investigations. Both circumstances make comparison of the results as well as further statistical evaluation in the form of a correlation analysis difficult. Third, we have not considered the influence of osteoporotic treatment. In this context, a positive effect on fracture healing was mentioned by some investigations.
In conclusion, this systematic review identified various factors that predict treatment failure in conservatively treated osteoporotic fractures. In these cases, additional treatment options as well as non-conservative treatment should be considered. For example, accompanying therapy including daily teriparatide administration and rehabilitation over a period of 3 months seems to improve the clinical result significantly. 22 However, the presence of one or more risk factors should also tempt the attending physician toward other strategies like kyphoplasty, or in cases with already existing hyperkyphosis, neurological impairment and persistent pain to more invasive surgical treatment options. In the future, machine learning-based approaches will provide us with a new perspective on risk factor analysis. Instead of looking at separate risk factors, machine learning can incorporate a multitude of them and allow for a much better prediction. As an example, a recent investigation demonstrated that bone texture analysis combined with machine learning could identify patients at risk for vertebral body insufficiency fractures on standard CT scans with high accuracy. 34
Footnotes
Authors’ Note: Max J. Scheyerer and Ulrich J. A. Spiegl contributed equally to this study. In the original publication of the article, we have to mention an error in labeling Figure 2 and in legend Figure 3. In addition to the others mentioned risk factors the intervertebral cleft is not a risk factor, but rather the intravertebral one as shown in the figures. We apologize for any inconvenience.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Max J. Scheyerer, PD Dr.  https://orcid.org/0000-0003-1392-3990
https://orcid.org/0000-0003-1392-3990
Georg Osterhoff, PD Dr.  https://orcid.org/0000-0001-5051-0998
https://orcid.org/0000-0001-5051-0998
Gregor Schmeiser, PD Dr.  https://orcid.org/0000-0002-2432-8276
https://orcid.org/0000-0002-2432-8276
References
- 1.Holroyd C, Cooper C, Dennison E. Epidemiology of osteoporosis. Best Pract Res Clin Endocrinol Metab. 2008;22(5):671–685. [DOI] [PubMed] [Google Scholar]
- 2.Cooper C, Cole ZA, Holroyd CR, et al. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos Int. 2011;22(5):1277–1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gold DT. The clinical impact of vertebral fractures: quality of life in women with osteoporosis. Bone. 1996;18(3 Suppl):185S–9S. [DOI] [PubMed] [Google Scholar]
- 4.Johnell O, Kanis JA, Oden A, et al. Mortality after osteoporotic fractures. Osteoporos Int. 2004;15(1):38–42. [DOI] [PubMed] [Google Scholar]
- 5.Moher D, Liberati A, Tetzlaff J, Altman DG; for the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.OloEW G. The Oxford Levels of Evidence 2. Oxford Centre for Evidence-Based Medicine; 2011. [Google Scholar]
- 7.Lee HM, Park SY, Lee SH, Suh SW, Hong JY. Comparative analysis of clinical outcomes in patients with osteoporotic vertebral compression fractures (OVCFs): conservative treatment versus balloon kyphoplasty. Spine J. 2012;12(11):998–1005. [DOI] [PubMed] [Google Scholar]
- 8.Zhang J, He X, Fan Y, Du J, Hao D. Risk factors for conservative treatment failure in acute osteoporotic vertebral compression fractures (OVCFs). Arch Osteoporos. 2019;14(1):24. [DOI] [PubMed] [Google Scholar]
- 9.Shah S, Goregaonkar AB. Conservative management of osteoporotic vertebral fractures: a prospective study of thirty patients. Cureus. 2016;8(3):e542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goldstein S, Smorgick Y, Mirovsky Y, Anekstein Y, Blecher R, Tal S. Clinical and radiological factors affecting progressive collapse of acute osteoporotic compression spinal fractures. J Clin Neurosci. 2016;31:122–126. [DOI] [PubMed] [Google Scholar]
- 11.Hoshino M, Tsujio T, Terai H, et al. Impact of initial conservative treatment interventions on the outcomes of patients with osteoporotic vertebral fractures. Spine (Phila Pa 1976). 2013;38(11):E641–648. [DOI] [PubMed] [Google Scholar]
- 12.Park HY, Ahn JH, Ha KY, et al. Clinical and radiologic features of osteoporotic spine fracture with delayed neurologic compromises. World Neurosurg. 2018;120:e1295–e300. [DOI] [PubMed] [Google Scholar]
- 13.Hayashi T, Maeda T, Masuda M, Ueta T, Shiba K. Morphology of the injured posterior wall causing spinal canal encroachment in osteoporotic vertebral fractures. Spine J. 2016;16(8):946–950. [DOI] [PubMed] [Google Scholar]
- 14.Tsujio T, Nakamura H, Terai H, et al. Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion: a prospective multicenter study. Spine (Phila Pa 1976). 2011;36(15):1229–1235. [DOI] [PubMed] [Google Scholar]
- 15.Ito Y, Hasegawa Y, Toda K, Nakahara S. Pathogenesis and diagnosis of delayed vertebral collapse resulting from osteoporotic spinal fracture. Spine J. 2002;2(2):101–106. [DOI] [PubMed] [Google Scholar]
- 16.Sugita M, Watanabe N, Mikami Y, Hase H, Kubo T. Classification of vertebral compression fractures in the osteoporotic spine. J Spinal Disord Tech. 2005;18(4):376–381. [DOI] [PubMed] [Google Scholar]
- 17.Seo JY, Kwon YS, Kim KJ, Shin JY, Kim YH, Ha KY. Clinical importance of posterior vertebral height loss on plain radiography when conservatively treating osteoporotic vertebral fractures. Injury. 2017;48(7):1503–1509. [DOI] [PubMed] [Google Scholar]
- 18.Patil S, Nene AM. Predictors of kyphotic deformity in osteoporotic vertebral compression fractures: a radiological study. Eur Spine J. 2014;23(12):2737–2742. [DOI] [PubMed] [Google Scholar]
- 19.Ha KY, Kim YH. Risk factors affecting progressive collapse of acute osteoporotic spinal fractures. Osteoporos Int. 2013;24(4):1207–1213. [DOI] [PubMed] [Google Scholar]
- 20.Nakamae T, Fujimoto Y, Yamada K, et al. Relationship between clinical symptoms of osteoporotic vertebral fracture with intravertebral cleft and radiographic findings. J Orthop Sci. 2017;22(2):201–206. [DOI] [PubMed] [Google Scholar]
- 21.Cho JH, Shin SI, Lee JH, Yeom JS, Chang BS, Lee CK. Usefulness of prone cross-table lateral radiographs in vertebral compression fractures. Clin Orthop Surg. 2013;5(3):195–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wakao N, Takeuchi M, Riew DK, et al. Effect of an intensive conservative therapy with daily teriparatide administration and rehabilitation for osteoporotic delayed vertebral collapse and paralysis. Medicine (Baltimore). 2018;97(23):e10906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smorgick Y, Geftler A, Goldstein S, Mirovsky Y, Blecher R, Anekstein Y.Determination of any correlation between sagittal spinopelvic configuration and progressive collapse of acute osteoporotic compression spine fractures: a retrospective radiological analysis [published online January 8, 2020]. Asian Spine J. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iwata A, Kanayama M, Oha F, Hashimoto T, Iwasaki N. Does spinopelvic alignment affect the union status in thoracolumbar osteoporotic vertebral compression fracture? Eur J Orthop Surg Traumatol. 2017;27(1):87–92. [DOI] [PubMed] [Google Scholar]
- 25.Ohnishi T, Iwata A, Kanayama M, Oha F, Hashimoto T, Iwasaki N. Impact of spino-pelvic and global spinal alignment on the risk of osteoporotic vertebral collapse. Spine Surg Relat Res. 2018;2(1):72–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kao FC, Huang YJ, Chiu PY, Hsieh MK, Tsai TT. Factors predicting the surgical risk of osteoporotic vertebral compression fractures. J Clin Med. 2019;8(4):501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kanchiku T, Imajo Y, Suzuki H, Yoshida Y, Taguchi T. Usefulness of an early MRI-based classification system for predicting vertebral collapse and pseudoarthrosis after osteoporotic vertebral fractures. J Spinal Disord Tech. 2014;27(2):E61–65. [DOI] [PubMed] [Google Scholar]
- 28.Kataoka H, Ikemoto T, Yoshimura A, et al. Association of early physical activity time with pain, activities of daily living, and progression of vertebral body collapse in patients with vertebral compression fractures. Eur J Phys Rehabil Med. 2017;53(3):366–376. [DOI] [PubMed] [Google Scholar]
- 29.Ha KY, Park KS, Kim SI, Kim YH. Does bisphosphonate-based anti-osteoporosis medication affect osteoporotic spinal fracture healing? Osteoporos Int. 2016;27(2):483–488. [DOI] [PubMed] [Google Scholar]
- 30.Fujimoto K, Kanchiku T, Imajo Y, et al. Reduction of vertebral height with fragility vertebral fractures can induce variety of neurological deterioration. J Orthop Surg Res. 2017;12(1):145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 2010;35(25):2224–2231. [DOI] [PubMed] [Google Scholar]
- 32.Omi H, Yokoyama T, Ono A, Numasawa T, Wada K, Fujisawa Y. Can MRI predict subsequent pseudarthrosis resulting from osteoporotic thoracolumbar vertebral fractures? Eur Spine J. 2014;23(12):2705–2710. [DOI] [PubMed] [Google Scholar]
- 33.Shin YH, Shin WC, Kim JW. Effect of osteoporosis medication on fracture healing: an evidence based review. J Bone Metab. 2020;27(1):15–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Muehlematter UJ, Mannil M, Becker AS, et al. Vertebral body insufficiency fractures: detection of vertebrae at risk on standard CT images using texture analysis and machine learning. Eur Radiol. 2019;29(5):2207–2217. [DOI] [PubMed] [Google Scholar]