Abstract
Most health care approaches to understanding social ills are rooted in strain or ecological models. Strain models assume that the impact of poor physical health operates through the individual, that it is the individual suffering from poor health who engages in social ills as a means of adapting, and that the impact of poor health is rather direct and immediate. Meanwhile, ecological approaches of health acknowledge how poor health may impact others and the collective, but poorly account for the case in which this is not so, leaving unexplained the many instances of people who are in poor health but remain actively engaged with their communities and preserve relationships that nurture trust, shared norms, and cooperation. To rectify this problem, we introduce the concept of “compulsive immobility”: the situation in which those in poor health are compelled to stay indoors and refrain from community socialization. We argue that compulsive immobility mediates the relationship between poor physical health and collective efficacy, suggesting that illness, specifically to a point of physical immobility (e.g., bedridden), enables poor health to detract from collective efficacy. This allows scholars to both acknowledge how poor health may impact the individual and community, while specifying the mechanism through which it operates. To support our claim, we draw on GSS data to examine the relationship among poor health, health-related immobility, and collective efficacy. Our results provide empirical support for our argument, revealing that general health conditions influenced the level of generalized trust directly and indirectly through compulsive immobility. We conclude with suggestions on how compulsive immobility might impact neighborhood crime and propose ways through which subsequent research may refine and further test compulsive immobility as a mediator between poor health and collective efficacy.
Highlights
-
•
Build upon health and social science research by examining the indirect relationship between health and collective efficacy.
-
•
Introduce the concept of “compulsive immobility” to elucidate the relationship between health and collective efficacy.
-
•
Draw on GSS data to examine this relationship.
-
•
Find support for compulsive immobility as a mediator in the relationship between health and collective efficacy.
-
•
Conclude with suggestions for future research and refinement of compulsive immobility.
1. Introduction
Health care practitioners and researchers have concerned themselves with a host of social ills. The relationship between social forces and health is well documented, with the field of health care sociology noting the relevance of social factors, such as social capital and networks, on health behaviors and outcomes (Barabasi, 2007). Social relationships have been found to influence mortality rates, unhealthy risk-behaviors, and disease morbidity (Smith & Christakis, 2008). For example, marriage is associated with lower mortality rates (Hu & Goldman, 1990), peer eating habits are associated with the formation of unhealthy weight-control behaviors in adolescent girls (Eisenberg, Neumark-Sztainer, Story, & Perry, 2005), and breast cancer in a peer is associated with an increased likelihood that her friend will get screened (Murabito et al., 2001). These approaches to health and social networks posit that social ties influence health through five possible mechanisms: 1) the provision of social support, 2) social influence through norms 3) social engagement, 4) person-to-person contacts, and 5) access to resources (Berkman et al., 2000). While insightful, these approaches assume that the relationship between health and social forces primarily operates unidirectionally—that social relations influence health. However, we argue that the opposite may also be true. If social capital and relationships influence health, how may health influence the accumulation [or maintenance] of social capital and trusting relationships with others? With this, we introduce the concept of “compulsive immobility” the forced, compulsory, involuntary immobility that arises due to poor physical health (e.g., bed ridden), and lay out a theoretical and empirical argument why compulsive immobility matters for social relations, capital and collective efficacy.
There is some precedent to explore this reasoning. For example, existing research found a short-term rise in mortality after the death of a spouse (Martikainen and Valkonenen, 1996), decreased health status of a child with ill parents (Weismann et al., 1987), and increased likelihood of becoming obese when in close contact with an obese friend (Christakis & Fowler, 2007). Yet, this is just the beginning, as current models do not adequately consider how one's poor health may also matter for the social well-being of others.
While previous research exemplifies how social ills—namely poverty and inadequate social capital and interpersonal ties—influence an individual's health, we believe these models fall short in their understanding of the relationship between health and social ills. It is not only the ill individual who adapts to their condition that matters for population health, but also the ill person's relationship with others. Their ability to interact, create social ties and trusting relationships, and act together also suffers. How one's health may matter for the social fabric of her community or group summarizes a key gap in existing literature—one that this paper seeks to remedy. Conventional thinking in the fields of public health and social medicine establishes that social relationships are determinants of health outcomes, but we propose and empirically test a theoretical model hypothesizing that health may also influence aspects of social integration. With this, we argue that an understanding of the relationship between poor physical health and social attitudes can benefit from greater engagement with ecological theories (Kawachi, Kennedy, & Wilkinson, 1999).
As one of the most established ecological frameworks, social disorganization theory identifies key mechanisms through which the social health of a community may be strengthened or weakened. Ultimately, the social organization of a community depends on its members forming positive social ties and trusting relationships, as these are core to social integration and the normative influence that follows. Neighborhoods are organized when its residents interact with each other, creating social cohesion and effectively communicating and establishing local norms. Socially disorganized neighborhoods suffer from a lack of residential interaction and communication, consequently struggling to develop shared, agreed upon norms, and social cohesion. This undermines residents’ ability to establish positive and productive collective attitudes and exert the informal social controls that encourage conformity. An important factor in this process is collective efficacy.
Collective efficacy—the extent to which a group of people can act together to recognize and solve shared problems and achieve shared goals—is vitally important for understanding several social ills. Child maltreatment, intimate partner violence, educational performance, youth activism, disaster recovery, and overall violence (Abdullah, Emery, & Jordan, 2020; Ortiz & Ostertag, 2014; Cohen, 2006; Hoy, Sweetland, & Smith, 2002; Jackson, 2016; Sampson, Raudenbush, & Earls, 1997; Velasquez & LaRose, 2015) are variously influenced by collective efficacy. Collective efficacy is dependent on people's ability to trust each other and cooperate around similar, shared norms and values, which develop out of people's frequent and regular interaction. When interaction is sporadic, limited, or infrequent, it hinders people's ability to create the trust, shared norms, and cooperation necessary for collective efficacy. What's more, collective efficacy is useless if people do not perceive it, that is, if people do not see themselves as willing and able to work collectively to tackle shared goals and satisfy shared norms. Further, while collective efficacy emphasizes group qualities, it has been convincingly applied to individuals as well, linking the individual to the collective (Clear, 2007).
In this paper, we present a framework for understanding how poor physical health influences the members of a community, their social capital and relationships, and ultimately, a community's ability to achieve collective efficacy. While collective efficacy is important for a variety of social ills, and the mechanisms that cultivate collective efficacy appear clear, they are not all equally significant. Indeed, given the particular social phenomenon under investigation, the causal factors that cultivate perceptions of collective efficacy may differ and/or have differing effects. For example, in identifying several components of collective efficacy affected by residential mobility through incarceration, or “coercive mobility” (Clear, 2007), Clear highlights human capital, social capital, and social networks as being the most important. Under the phenomenon of coercive mobility, residential mobility via cycles of incarceration and reentry destabilizes collective efficacy by creating anonymity through the reduction of human capital and social capital, which hinders the formation of strong network ties and trusting relationships among a community.
We wish to focus attention on the role of health on perceptions of collective efficacy. Here, the general line of thinking goes as follows: poor health challenges people's ability to develop collective efficacy, or perceptions of, by impeding interaction and communication among neighbors, friends, and relatives. Because people are in poor health, they cannot interact with their neighbors and acquaintances. When concentrated in a community or neighborhood, the assumed consequences hinder the development or maintenance of collective efficacy. While this makes sense, upon closer inspection it leaves unexplained the many instances of people who are in poor health but nonetheless remain actively engaged with their neighbors and interact in ways that nurture or maintain trust, shared norms, and cooperation. For example, the obese, chronic smokers, and those with high blood pressure, high cholesterol, and diabetes may be considered in poor health, but also active and engaged with their neighbors and enjoy considerable social capital. That is, these health conditions do not always nor automatically stop the mechanisms that foster collective efficacy.
We believe there is an additional approach on this theoretical component of collective efficacy, as the theoretical link between poor health and collective efficacy is not as direct as dominant models of health care assume, nor do they sufficiently account for the many people who are in poor health but continue to communicate and interact with their neighbors. There is an important mediating factor that has gone unexamined in existing research—one that helps rectify this problem. It is not poor health per se, that hinders, weakens, or challenges collective efficacy. Rather, it is when health become so severe that one becomes immobile, that poor health matters for collective efficacy. Specifically, poor health does not necessarily lead to collective efficacy (though it may), but to immobility, and from here, to weak collective efficacy. It is this immobility that matters for collective efficacy, as it renders one's social capital largely mute and hinders one's social interaction with local others. With this, collective efficacy, or perceptions of, diminish and the monitorial, informal social controls that come with it become ineffective. From here, we may theorize any variety of social ills that might result. We call this phenomenon “compulsive immobility”, as it stresses the forced and unwanted lack of mobility that may arise due to poor health. The need to remain indoors, perhaps in a wheelchair or bed ridden, because one's poor health becomes so severe that they are compelled to be immobile characterizes this phenomenon. Before this point, one may be in poor health, but nonetheless still somewhat active and mobile, greeting neighbors, picking up litter around their homes, keeping an eye on their surroundings, and recognizing suspicious activities. To address this gap in theory, we argue that the mediating factor of compulsive immobility links poor health to diminished collective efficacy, as it recognizes the many cases of people in poor health who continue to interact and communicate with their neighbors and passersby, effectively monitoring their neighborhoods and contributing to its solidarity.
1.1. Collective efficacy and residential mobility
Issues of residential mobility are particularly important for collective efficacy, and the host of social problems that might follow. Understood as the frequency of moves for an individual or percentage of people in and out of neighborhoods, residential mobility poses considerable challenges to residents' ability to interact and create the social ties and the perceptions so important to collective efficacy. Applied to explain both individual-level phenomena of personal well-being and the primacy of personal self (Oishi, 2010) as well as community level factors such as gentrification, changes in local economies and job structures, housing values and fluctuating costs of rental properties, aggressive eviction practices (Desmond, 2017) and mass incarceration (Clear, 2007; Clear, Rose, & Ryder, 2001; Rose & Clear, 1998), residential mobility creates anonymity and impedes social cohesion (Cructhfield et al., 1982; Cructhfield, 1989; Desmond, 2017), which weakens collective efficacy (Bellair, 2000; Stretesky, Schuck, & Hogan, 2004; Warner and Peirce, 1993). These factors either give people little reason to leave their homes (e.g., lack of community organizations) or pressures them to stay indoors (large unsupervised groups of teens). Of particular interest is Clear and colleagues' concept of coercive mobility, which provides a phenomenon-specific model of residential mobility and its influence on collective efficacy. Coercive mobility proposes that the concentrated and constant removal of community members and subsequent reentry produces community disorganizing effects. When applied to incarceration, the argument is that mass incarceration, because it's so concentrated and constant, further disorganizes already disorganized communities and exacerbates challenges to establishing positive social relationships and collective action. Indeed, the macrosocial factor of mass incarceration contextualizes and specifies the broader mechanism of residential mobility. Aside from the implied negative consequences of high residential mobility on collective efficacy, imprisonment further disorganizes communities because family members of incarcerated individuals are also likely to relocate. Many families move to different neighborhoods seeking outside parental care for children with an incarcerated parent, and families also move upon a family member's reentry into society to distance themselves from the neighborhood influences that might have contributed to the initial imprisonment. Furthermore, incarceration drastically disrupts social networks. Clear posits that incarceration destabilizes social networks not only by removing individuals from their families and friends, but also by adding strain on family members who are likely to withdrawal from the community to cope with emotional distress, financial issues, or stigma. Moreover, social networks are further disrupted when an individual returns from prison, as families struggle to reabsorb a family member, and neighbors may socially withdrawal out of fear. Our notion of compulsive immobility similarly aims to provide a phenomenon-specific framework for the relationship between residential mobility and collective efficacy, but with regards to physical health. Given that concerns with social anonymity naturally arise when considering the impact of residential mobility on collective efficacy, we wish to specify the role of poor physical health as a facilitator of social anonymity and hindrance to collective efficacy. In order to do so, the conventional assumptions of the relationship between residential mobility and collective efficacy must be clarified in terms of physical health.
Most of these concerns with collective efficacy assume that residents must physically move from their residence. That is, it is the movement of people out of their neighborhood that matters for collective efficacy. Yet, Sampson and Wilson. (1995) hinted that this need not be the case, as lack of community organizations and presence of unsupervised teens give people little reason or motive to leave their homes. We wish to explore this line of thinking more seriously. We argue that the same consequences for collective efficacy may arise from residents who remain in their neighborhood but confined indoors due to poor physical health. These individuals are those who suffer from what we term “compulsive immobility”: the need to remain indoors due to poor physical health. We build upon this line of theorizing centered on the importance of residential mobility on collective efficacy, as it is here where failures in interaction and communication occur, and where hurdles to developing social capital, trust with others, and cooperative actions arise. With our notion of compulsive immobility, we wish to draw attention to the role of poor health in collective efficacy.
1.2. Compulsive immobility
Our notion of compulsive immobility helps clarify a potential problem with how researchers approach questions of residential mobility and its consequences (e.g., collective efficacy, social disorganization, personal well-being). In some cities or regions of the US, especially in the south, neighborhood residents might own their homes with generations of family members living there for decades. In such cases, where collective efficacy may nonetheless remain weak and crime is high, the notion of residential mobility as it is commonly understood seems inconsistent. Yet, if residents are compelled into staying indoors due to ongoing physical illnesses (such as those associated with heart disease, diabetes, high blood pressure, obesity, etc.), they are hindered from interacting with their neighbors. This, we argue, has the same consequence for collective efficacy, as Sampson noted regarding lack of community organizations and presence of unsupervised teens, but with residents compelled to stay indoors due to physical health problems.
There is some precedent to examine the relationship between health, residential [im]mobility, and collective efficacy and therefore develop the line of reasoning we propose in this paper. For example, Morris, Manley, and Sabel (2018) highlight growing evidence that residential mobility may have a negative impact on a wide range of health outcomes, calling for future research to elucidate mobility's complex relationship with health outcomes and noting a necessity to “consider the geographical clustering of individual health phenomena, and to obtain accurate effects at both the individual and contextual level” (124). Furthermore, Heilman (2017) found evidence that neighborhood rates of Hepatitis-C have a positive association with place-level indicators of social disorganization, with another study revealing that higher levels of neighborhood social disorganization are associated with higher diabetes morbidity (Kowitt, Donahue, Fisher, Mitchell, & Young, 2018). Jacobson et al. (2020) offer insight closer to our conceptualization of the problem. With findings indicating residential mobility to not be associated with increased rates of certain chronic diseases, they suggest that immobility may be due to the “healthy mover effect”: those who engage in residential mobility are likely in better health than those who do not. These studies provide some groundwork upon which we base our discussion of compulsive immobility, which follows that poor health results in high rates of community members confined to the indoors, preventing social interaction and impeding community organization and collective efficacy. Combining these with work on social disorganization and collective efficacy, we may argue that due to poor health, people remain in their homes, unable to participate in the interaction, socialization and normative informal controls that constitute organized neighborhoods. Bedridden, ill adults are unable to socialize and interact with their neighbors, which forms the basis of the informal social controls that help organize a neighborhood by contributing to its collective efficacy.
1.3. Theoretical framework
What are the mechanisms that explain the linkages between poor health, compulsive immobility, and collective efficacy? In developing his theory of coercive mobility, Todd Clear (2007) provides some insight that we draw from in framing our argument and supporting evidence. While applying these to his theory of coercive mobility, they may similarly be applied to our concept of compulsive immobility. First is human capital, which is defined as the personal resources an individual brings to the social and economic marketplace (Clear, 2007). Individuals lose a significant amount of human capital when immobile due to an inability to build on or expand their personal resources. Indeed, higher levels of sickness are found to be positively associated with inactivity, downward social mobility, and unemployment (Billingsley, 2020). Second is social capital, which is the capacity of a person to call upon social ties to advance some personal interest. The building of social capital involves the mutual exchange of human capital among individuals within a group. Simply, “social capital relies upon (and in turn promotes) human capital” (Clear, 2007, p. 81), thus because compulsively immobile people lack human capital, they are therefore unlikely able to build social capital. Research in this area demonstrates that social capital “serves as a productive input in health status” (Folland and Nauenberg, 2018: 2). Moreover, Shultz et al. (2009) notably find positive associations between the health of disadvantaged young parents and social interactions, with the health of the child being insignificant. This evidence suggests that health influences social capital, contrary to past research mainly indicating social capital's influence on health. Therefore, along with hindering the advancement of human capital, compulsive immobility is likely to diminish social capital, as those immobilized due to poor health lack the ability to establish positive relationships.
Social capital and human capital are intricately related to the third factor, social networks, the array of relationships in which a person lives, works, and engages in recreation. Through its effects on human and social capital, compulsive immobility also diminishes an individual's ties to other individuals and groups within a community. The disruption of social networks is a predictable consequence of compulsive immobility, as sick individuals often withdraw from community engagement and their family members. These three factors are all in service to the fourth, which is the focus of this paper, collective efficacy. Collective efficacy, a normative concept, assumes a group understanding of collective problems and approaches to solve them. Importantly, Clear posits that collective efficacy is dependent on human capital, social capital, and social networks, asserting, “[collective efficacy] relies upon the community's sense of shared interest in each other's prospects” (Clear, 2007, p. 82), which are only realized upon accumulation of the aforementioned factors. Thus, challenges posed to developing and maintaining human capital, social capital and trusting social networks all threaten collective efficacy. People suffering from compulsive immobility struggle with maintaining the capital and networks they may have created years earlier. They may no longer be able to develop the interpersonal relationships that promote collective efficacy. Lastly is social control. While we do not extend our argument directly to explain social control, nor do we provide the data to do so, work on collective efficacy speaks to social control, as the influence of non-intimate relationships to get people to conform to the expectations of voluntary social groups, employers, and religious institutions, among others, are key outcomes of collective efficacy. We argue that poor health informs collective efficacy through the mediating variable of compulsive immobility. It is not only the sick, but those who are so ill or in poor physical health that they are compelled to remain indoors, that leads to diminishing human capital, social capital, and social networks for both the physically ill and their families.
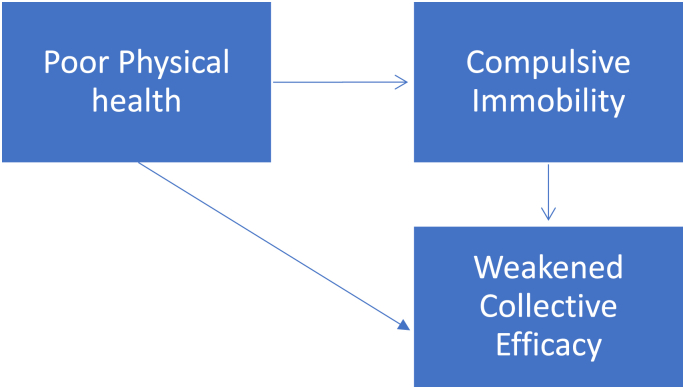
With this we offer our theoretical model (Model 1) and 4 hypotheses.
Model 1.
Theoretical flow chart.
Based on the theoretical model, we hypothesize that:
-
1)
Poor physical health status is positively associated with compulsive immobility;
-
2)
Poor physical health status is negatively associated with respondent's perception of collective efficacy, measured by generalized trust and social networking with neighbors, friends, and relatives;
-
3)
Physical immobility is negatively associated with respondent's perception of collective efficacy;
-
4)
The association between poor physical health status and perceived collective efficacy is mediated by compulsive immobility.
With these hypotheses, we argue that poor physical health status leads many residents to stay inside their homes (due to disabilities, incapacitations, chronic illnesses, etc.), hindering social interaction and therefore the establishment of collective efficacy and informal social controls. Our concept of compulsive immobility identifies an important place for public health researchers and practitioners to engage in discussions of collective efficacy and related social phenomena (e.g., crime).
2. Methods
2.1. Data and participants
We use General Social Survey (GSS) data from the University of Chicago's National Opinion Research Center (NORC) to examine and test some preliminary evidence of our argument. The GSS is a nationally representative sample of all non-institutionalized U.S. adults. To ensure statistical relevance, we extracted data only from years 2010–2018, which include five biannual waves of data collection. Our variables of interest include those pertaining to physical health, compulsive immobility, and collective efficacy. Given that survey questions in these categories are not necessarily posed to the same participants during each wave of data collection, we isolated a group of cases who had data for every one of our variables. This brought our sample size to 1547 participants with corresponding data for each variable. All data analyses were conducted using program Mplus 8.0 (Muthén and Muthén, 1998–2017).
2.2. Measures
We use two variables—health problems and general health—to measure our key independent variable physical health. The variable health problems was created by combining 5 different indicators pertaining to specific health issues. These health issues include arthritis, arm pain, back pain, diabetes, and hypertension/high blood pressure. Respondents answered “yes” or “no” to whether a doctor, nurse, or other health professional has ever told them that they had any of the above health problems. We recoded these variables and assigned a value of 1 to “yes,” and a value of 0 to “no.” These variables were then summed to create our index of physical health problems, with a higher score indicating worse health.
The general health variable captures responses to the question ‘Would you say that in general your health is Excellent, Very Good, Good, Fair, or Poor,’ with values 1–5 corresponding to each response category, respectively. A higher score on “General Health” corresponds to a respondent having relatively worse health.
To measure compulsive immobility, we created a measure called physical limitation from three related GSS variables. These variables include: 1) “Days of physical activity limitation”, measured by the question ‘During the past 30 days, for about how many days did your poor physical or mental health keep you from doing your usual activities, such as self-care, work, or recreation?‘; 2) “Days of poor physical health”, captured by the question ‘Now thinking about your physical health, which includes physical illness and injury, for how many days during the past 30 days was your physical health not good?‘; and 3) “Days of missed work for health”, corresponding to the question ‘During the past 30 days, about how many days did you miss work due to your mental or physical health?‘. These items are measured on a scale of 1–30 days, and we combined them into our “physical limitation” measure by taking the mean of the three.
We use two variables—generalized trust and social networks—to measure collective efficacy. Trust is a crucial factor of social disorganization and positively associated with social capital and collective efficacy (Galea, Karpati, & Kennedy, 2002; Sampson et al., 1997). Lack of trust creates communal anonymity (Wu, 2020), which can explain why some places see more violence than others (Sampson et al., 1997; Galea et al., 2002; Rosenfeld, Baumer, & Messner, 2007; Kawachi et al., 1999). Following the model of generalized trust, (Rosenfeld et al., 2007; Wu, 2020), we create an index of generalized trust using three GSS survey questions: 1) Generally speaking, would you say that most people can be trusted or that you can't be too careful in life? 2) Would you say that most of the time people try to be helpful, or that they are mostly just looking out for themselves? 3) Do you think most people would try to take advantage of you if they got a chance, or would they try to be fair? These variables each had a positive and negative response category, as well as a “depends” category. The positive and negative categories were coded to values of 1 and 3, respectively, and “depends” was assigned a value of 2. The index of generalized trust was computed by taking the mean of the three variables, where a higher score corresponds to lower trust.
Furthermore, social networks are an important indicator of collective efficacy. At the communal level, how often and with whom residents choose to spend their time are important considerations. To examine this, we created a variable called “social networks” from three related GSS variables. Participants were asked how often they spend a social evening with a) neighbors; b) relatives; and c) friends who live outside the neighborhood. Possible responses were (1: almost daily; 2: several times a week; 3: several times a month; 4: once a month; 5: several times a year; 6: Once a year; 7: never). Our “social networks” measure was calculated from the mean of these three variables, where a higher score corresponds to a lower level of social networks.
To obtain unbiased associations between collective efficacy and measures of physical health and physical limitation, we control five variables in our multivariate regression models. We control for respondents’ sex and race by using dummy variables, where 0=Female and 1=Male, and 1=White and 0=Other race. Because the distribution of the variable income was quite skewed, we recoded the variable by using the logarithm transformation. Additionally, we control for education level, and age via utilization of the corresponding GSS variables. The descriptive data (mean, standard deviation, and range) are presented in Appendix Table 1.
Table 1.
Descriptive statistics.
| Variable | Minimum | Maximum | Mean | Standard Deviation |
|---|---|---|---|---|
| Health Problems (Physical Health Problems [5]) | 0.00 | 5.00 | 0.90 | 1.09 |
| General Health | 1.00 | 5.00 | 2.40 | 1.03 |
| Physical Limitation | 0.00 | 30.00 | 1.77 | 4.06 |
| SexDUMMY (Respondent's Sex) | 0.00 | 1.00 | 0.45 | 0.50 |
| RaceDUMMY (Respondent's Race) | 0.00 | 1.00 | 0.74 | 0.44 |
| EducR | 0.00 | 20.00 | 13.64 | 3.05 |
| ageR | 18.00 | 89.00 | 48.72 | 17.71 |
| IncomeR | 5.86 | 12.69 | 9.95 | 1.19 |
| Generalized Trust | 1.00 | 3.00 | 2.06 | 0.73 |
| Social Networks | 1.00 | 7.00 | 4.01 | 1.21 |
3. Results
We conducted a multivariate regression model to test our first hypothesis, that is, whether poor physical health status is significantly associated with physical immobility—our measure of compulsive immobility (Table 2). As shown in Table 2, physical health problems (b = 0.80, p < 0.01) and poor general health (b = 0.69, p < 0.01) were both significantly and positively associated with limited physical mobility, providing empirical support for the first hypothesis. In terms of control variables, income was the only significant predictor, with higher income associated with lower levels of compulsive immobility. A decent 16% of the variation of compulsive immobility was explained by this model.
Table 2.
Ordinary least squares regression model predicting physical immobility.
| b | s.e | |
|---|---|---|
| Intercept | 0.65 | 0.69 |
| Physical problems | 0.80** | 0.06 |
| General health | 0.69** | 0.07 |
| Malea | −0.19 | 0.14 |
| Whitea | 0.23 | 0.15 |
| Education | 0.03 | 0.03 |
| Age | −0.01 | 0.01 |
| Income (log) | −0.17** | 0.07 |
| R2 | 0.16 | |
Note: N = 1547 *p<.05 **p<.01.
Male and white as the reference category.
We used stepwise regression models to test the second and the third hypothesis. Regarding respondent's social networking with friends, neighbors and relatives, our regression model (Model 1, Table 3) reveals that general health was significantly and positively associated with social networking, with every unit increase of general health leading to 0.10 unit increase of networking with friends, neighbors, and relatives (b = 0.11, p < 0.05). The measure of physical health problems, however, was not statistically significant. In model 2, the measure of physical limitations was included. This variable, however, was not statistically significant and had little effect on the magnitude of the regression coefficients of the other two health measures. Among control variables, race, education, and age were all statistically significant predictors in the posited directions. Generally speaking, white, older people, and those with lower education were less likely to spend a social evening with their neighbors, friends, and relatives.
Table 3.
Ordinary least squares regression models predicting networking with friends, neighbors, and relatives.
| Model 1 |
Model 2 |
|||
|---|---|---|---|---|
| b | s.e | b | s.e | |
| Intercept | 3.30** | 0.29 | 3.30** | 0.29 |
| Physical problems | 0.00 | 0.03 | 0.01 | 0.03 |
| General health | 0.11** | 0.03 | 0.12** | 0.03 |
| Physical immobility | −0.01 | 0.01 | ||
| Malea | 0.10 | 0.06 | 0.10 | 0.06 |
| Whitea | 0.16* | 0.06 | 0.16* | 0.06 |
| Education | −0.02* | 0.01 | −0.02* | 0.01 |
| Age | 0.01* | 0.00 | 0.01** | 0.00 |
| Income (log) | 0.02 | 0.03 | 0.02 | 0.03 |
| R2 | 0.04 | 0.04 | ||
Note: N = 1547 *p<.05 **p<.01.
Male and white as the reference category.
Table 4 explores the associations between physical health, physical immobility, and generalized trust. Model 1 shows that the two indicators of physical health—physical health problems and general health—were significantly associated with generalized trust. The higher the number of physical health problems, the lower the level of trust in others (b = 0.11, p <0.01). Similarly, poorer the general health was associated with a lower level of trust (b = 0.09, p < 0.01). In Model 2, the measure of physical limitation was introduced into the model, showing a significant and positive association with generalized trust. In other words, the higher the level of compulsive immobility, the lower the degree of trust in others (b = 0.02, p < 0.01). Among control variables, race, education and age were all statistically significant predictors. Overall, white, older people, and those lowly educated had lower levels of trust toward the society.
Table 4.
Ordinary least squares regression models predicting generalized trust.
| Model 1 |
Model 2 |
|||
|---|---|---|---|---|
| b | s.e | b | s.e | |
| Intercept | 4.90** | 0.24 | 3.58** | 0.18 |
| Physical problems | 0.11** | 0.02 | 0.07** | 0.02 |
| General health | 0.09** | 0.03 | 0.05** | 0.02 |
| Physical immobility | 0.02** | 0.01 | ||
| Malea | −0.05 | 0.05 | −0.03 | 0.04 |
| Whitea | −0.26** | 0.05 | −0.19** | 0.04 |
| Education | −0.08** | 0.01 | −0.06** | 0.01 |
| Age | −0.02** | 0.00 | −0.01** | 0.00 |
| Income (log) | −0.04 | 0.02 | −0.02 | 0.02 |
| R2 | 0.18 | 0.18 | ||
Note: N = 1547 *p<.05 **p<.01.
Male and white as the reference category.
Importantly, the introduction of physical limitations in Model 2 substantially decreased the magnitude of regression coefficients of the other two health measures. The coefficient of physical health problems, for example, decreased from 0.11 (Model 1) to 0.07 (Model 2), a 36% deduction. Similarly, the coefficient of general health decreased from 0.09 (Model 1) to 0.05 (Model 2), a 44% decrease. Such substantial decreases in regression coefficients suggest that compulsive immobility at least partially mediates the association between physical health problems and generalized trust, as well as the association between general health and generalized trust (Baron & Kenny, 1986). Moreover, we used the bias-corrected bootstrapping method with 5000 resampling (Hayes, 2017) to formally test whether these mediating effects were significant or not. Specifically, we utilized physical immobility as a mediator, general health and physical health problems as independent variables, and generalized trust as the dependent variable. The same demographic and socioeconomic status variables were controlled in the mediation analysis (Hayes, 2017). The indirect effect analyses indicated that the indirect effect of physical problems on generalized trust through physical immobility was statistically significant (b = 0.013, 95% confidence interval: 0.005, 0.021), as was the indirect effect of general health on generalized trust (b = 0.011, 95% confidence interval: 0.004, 0.019; results not shown but available upon request). Combined, these results provide partial support for our hypothesis 4. Whereas compulsive immobility did not mediate the effect of physical health on social network measures, it did mediate the effect of physical health indicators on generalized trust.
4. Conclusion
The aim of this article is to provide a more complete understanding into the role of health on collective efficacy. Most existing research tends to assume a strain theoretical framework, stressing the relationship between the ill individual and that individual's adaptation, and emphasizes the direction of influence flowing from social relationships to health outcomes. However, we propose considering the problem of health from an ecological perspective, where poor health outcomes influence social relationships, rather than [or in addition to] social relationships influencing poor health. With this, we underscore the importance of individual health on factors such as social capital and social mobility, and direct attention to the effects of poor health on collective efficacy. While this is not necessarily new, we note how current thinking fails to grasp the many instances in which those in poor health nonetheless maintain social capital and mobility, indicating a need to refine our thinking. Building on the importance of residential mobility for social integration (e.g., social disorganization theory) we examined the relationship between poor health and collective efficacy, as mediated by what we call compulsive immobility.
Despite the documented relationship between poor health and factors of collective efficacy, we suggest that this theoretical link may not be as direct as health care models assume. Current research fails to account for hindered communication and interaction between the ill individual and his/her neighborhood, and we aimed to address this gap through our novel concept of compulsive immobility. With this, we argued that poor health itself does not necessarily detract from a community's ability to achieve collective efficacy, but rather that poor health to the point of physical immobility can impede collective efficacy by weakening perceptions of shared social ties and capital with local others. Thus, we proposed that poor physical health can hinder collective efficacy, but crucially, through a mediating effect from physical immobility, or compulsive immobility. Extending our argument to the neighborhood level, we would claim that concentrated populations of the physically immobile can lead to concentrated perceptions of weak collective efficacy, which may identify the genesis of many communal social ills.
Using data from the General Social Survey, we empirically tested our theoretical framework by examining how poor physical health, mediated by compulsive immobility, negatively influences individual perceptions of collective efficacy. We found support for our first hypothesis with the multivariate regression model finding a significant relationship between poor physical health status and compulsive immobility. Notably, both measures of physical health status—our index of 5 physical health problems and poor general health—predicted significant positive increases in compulsive immobility. To test our second and third hypotheses, that is, whether poor physical health and physical immobility decrease perceptions of collective efficacy, we measured perceptions of collective efficacy by generalized trust and social networking with neighbors, relatives, and friends. Using stepwise regression models, we found that general health was significantly and positively associated with social networking, but our index physical health problems was not. Further, the introduction of physical immobility was not statistically significant, and it had little effect on the magnitude of 2 measures of physical health status. Thus, we did not find evidence that poor physical health status, mediated by compulsive immobility, influences social networking. Nevertheless, consistent with current research, general health was significantly and positively associated with social networking (Shultz et al., 2009).
Importantly, we found evidence that physical health and physical immobility are significantly associated with generalized trust. As shown in the analyses, respondents with a higher number of physical health problems and poorer health similarly tended to have significantly lower levels of trust in others. Of particular importance was our introduction of physical immobility into the regression model. Higher levels of health-related physical immobility significantly predicted lower levels of generalized trust, providing support for our second and third hypothesis. Moreover, because the introduction of physical limitation had a drastic and significant influence on the effects of our two measures of physical health status, we find support for our fourth hypothesis. Physical limitation had a significant mediating effect on the relationship between physical health and generalized trust. Thus, the evidence suggests that compulsive immobility is a phenomenon that amplifies the way in which poor health detracts from perceptions collective efficacy. Consistent with literature indicating that health influences social capital (Shultz et al., 2009), we contribute to growing evidence of diminished collective and social attitudes as a general consequence of poor health, not solely a contributor to poor health status. Furthermore, consistent with our hypotheses, these findings suggest that poor health may not directly influence collective efficacy, but rather requires additional factors to do so. Compulsive immobility was evidenced to be one of these factors, illuminating a crucial consideration in the investigation between health, social standing, and collective attitudes.
4.1. Limitations
While our analyses suggest compelling evidence that poor physical health and compulsive immobility negatively influence perceptions of collective efficacy, and that compulsive immobility has a significant mediating effect on the relationship between health and perceptions of collective efficacy, a few limitations to this study should be considered. First, because we use openly accessible data from the GSS, our variables do not measure group-level health directly. Instead, they provide generalizable insights into individuals' health statuses and degrees of physical limitation, outlining how these factors affect individual perceptions of collective efficacy. Second, also due to a limited data set, we did not measure community-levels of collective efficacy. Nevertheless, previous research has provided strong evidence that the perception of collective efficacy at the individual level has excellent predictive validity and is associated with multiple social outcomes (e.g., health and crime) at individual and neighborhood levels (Barnhart, Gearhart, & Maguire-Jack, 2018; Taylor, 2002). Finally, numerous studies find that neighborhood conditions (e.g., collective efficacy and crime) are salient predictors of residents’ physical health status (e.g., Barnhart et al., 2018; Kowitt et al., 2018), the direction of this causal association, however, is yet to be determined. Our analyses—which were based on GSS data collected from yearly cross-sectional samples—suffer the same problem. Our theoretical model, particularly the concept compulsive immobility, however, provides a compelling argument that physical health status may be more likely to drive social integration and collective efficacy, and our data provide some preliminary empirical support. Nevertheless, future research needs to use longitudinal data and more rigorous statistical techniques to assess the potentially bidirectional causality between these two factors.
4.2. Suggestions for future research
Given the preliminary evidence provided in this study and the aforementioned limitations, we suggest future research testing compulsive immobility utilize more direct measures of this phenomenon. Specifically, researchers should design specific measures of relationship between communal-level health outcomes, immobility, and indicators of collective efficacy. With the development of more direct measures of compulsive immobility, a broader scope of factors may be investigated. Access to quality health care exerts influence general health status, and given our findings, is likely to play a role in collective efficacy. An array of economic and policy implications related to compulsive immobility identify an important direction for future research not possible within the scope of this study's data. It is likely that health-related physical immobility also arises from factors pertaining to health care access, and therefore health care policy, suggesting a degree of coercion plays a role in this phenomenon. Moreover, with substantial evidence linking weak collective efficacy to neighborhood crime, we ask future researchers to design data sets inclusive of neighborhood health and direct measures of neighborhood crime. Doing so will illuminate another reason why health matters for community well-being and safety.
Funding
No funding was provided for this research.
Data
Anonymized, General Social Survey Data.
Author statement
Blake W. Powell: Conceptualization, Methodology, Investigation, Formal Analysis, Data Curation, Writing – Original Draft, Writing – Review and Editing. Stephen F. Ostertag: Conceptualization, Writing – Review and Editing, Supervision. Xiaojin Chen: Validation, Methodology, Software, Investigation, Formal Analysis.
Declaration of competing interest
None.
Contributor Information
Blake W. Powell, Email: bpowell4@tulane.edu.
Stephen F. Ostertag, Email: sosterta@tulane.edu.
Xiaojin Chen, Email: xchen1@tulane.edu.
References
- Abdullah A., Emery C.R., Jordan L.P. Neighborhood collective efficacy and protective effects on child maltreatment: A systematic literature review. Health and Social Care in the Community. 2020;28(6):1863–1883. doi: 10.1111/hsc.13047. [DOI] [PubMed] [Google Scholar]
- Barabási A.L. Network medicine—from obesity to the “diseasome”. New England Journal of Medicine. 2007;357(4):404–407. doi: 10.1056/NEJMe078114. [DOI] [PubMed] [Google Scholar]
- Barnhart S., Gearhart M.C., Maguire-Jack K. Perceptions of collective efficacy among single mothers: Insights for conceptualization and measurement. Journal of Family Issues. 2018;39(17):4019–4040. [Google Scholar]
- Baron R.M., Kenny D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bellair P.E. Informal surveillance and street crime: A complex relationship. Criminology. 2000;38(1):137–170. doi: 10.1111/j.1745-9125.2000.tb00886.x. [DOI] [Google Scholar]
- Berkman L.F., Glass T., Brissette I., Seeman T.E. From social integration to health: Durkheim in the new millennium. Social Science & Medicine. 2000;51(6):843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Billingsley S. Sick leave absence and the relationship between intra-generational social mobility and mortality: Health selection in Sweden. BMC Public Health. 2020;20(1):8. doi: 10.1186/s12889-019-8103-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christakis N.A., Fowler J.H. The spread of obesity in a large social network over 32 years. New England Journal of Medicine. 2007;357(4):370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- Clear T.R. Oxford University Press; 2007. Imprisoning communities. [Google Scholar]
- Clear T.R., Rose D.R., Ryder J.A. Incarceration and the community: The problem of removing and returning offenders. Crime & Delinquency. 2001;47(3):335–351. doi: 10.1177/0011128701047003003. [DOI] [Google Scholar]
- Cohen D.A. Brain K. Finch, Aimee Bower, and Narayan Sastry Collective efficacy and obesity: The potential influence of social factors on health. Social Science & Medicine. 2006;62(3):769–778. doi: 10.1016/j.socscimed.2005.06.033. [DOI] [PubMed] [Google Scholar]
- Crutchfield R.D. Labor stratification and violent crime. Social Forces. 1989;68(2):489–512. doi: 10.1093/sf/68.2.489. [DOI] [Google Scholar]
- Crutchfield R.D., Geerken M.R., Gove W.R. Crime rate and social integration the impact of metropolitan mobility. Criminology. 1982;20(3–4):467–478. doi: 10.1111/j.1745-9125.1982.tb00472.x. [DOI] [Google Scholar]
- Desmond M. Penguin Books; London: 2017. Evicted. [Google Scholar]
- Eisenberg M.E., Neumark-Sztainer D., Story M., Perry C. The role of social norms and friends' influences on unhealthy weight-control behaviors among adolescent girls. Social Science & Medicine. 2005;60(6):1165–1173. doi: 10.1016/j.socscimed.2004.06.055. [DOI] [PubMed] [Google Scholar]
- Folland S., Nauenberg E., editors. Elgar companion to social capital and health. Edward Elgar Publishing; 2018. https://EconPapers.repec.org/RePEc:elg:eebook:16697 Retrieved from. [Google Scholar]
- Galea S., Karpati A., Kennedy B. Social capital and violence in the United States, 1974–1993. Social Science & Medicine. 2002;55(8):1373–1383. doi: 10.1016/S0277-9536(01)00274-X. [DOI] [PubMed] [Google Scholar]
- Hayes A.F. Guilford Publications; 2017. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Heilman D. 2017. Social disorganization theory and hepatitis C incidence.http://d-scholarship.pitt.edu/33084/ Unpublished manuscript. [Google Scholar]
- Hoy W.K., Sweetland S.R., Smith P.A. Toward an organizational model of achievement in high schools : The significance of collective efficacy. Educational Administration Quarterly. 2002;38(1):77–93. [Google Scholar]
- Hu Y., Goldman N. Mortality differentials by marital status: An international comparison. Demography. 1990;27(2):233–250. [PubMed] [Google Scholar]
- Jackson A.L. The combined effect of women's neighborhood resources and collective efficacy on IPV. Journal of Marriage and Family. 2016;78(4):890–907. doi: 10.1111/jomf.12294. [DOI] [Google Scholar]
- Jacobson M., Crossa A., Liu S.Y., Locke S., Poirot E., Stein C., et al. Residential mobility and chronic disease among world trade center health registry enrollees, 2004–2016. Health & Place. 2020;61:102270. doi: 10.1016/j.healthplace.2019.102270. [DOI] [PubMed] [Google Scholar]
- Kawachi I., Kennedy B.P., Wilkinson R.G. Crime: Social disorganization and relative deprivation. Social Science & Medicine. 1999;48(6):719–731. doi: 10.1016/S0277-9536(98)00400-6. [DOI] [PubMed] [Google Scholar]
- Kowitt S.D., Donahue K.E., Fisher E.B., Mitchell M., Young L.A. How is neighborhood social disorganization associated with diabetes outcomes? A multilevel investigation of glycemic control and self-reported use of acute or emergency health care services. Clinical Diabetes and Endocrinology. 2018;4:19. doi: 10.1186/s40842-018-0069-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martikainen P., Valkonen T. Mortality after the death of a spouse: Rates and causes of death in a large Finnish cohort. American Journal of Public Health. 1996;86(8_Pt_1):1087–1093. doi: 10.2105/ajph.86.8_pt_1.1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris T., Manley D., Sabel C.E. Residential mobility: Towards progress in mobility health research. Progress in Human Geography. 2018;42(1):112–133. doi: 10.1177/0309132516649454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murabito J.M., Evans J.C., Larson M.G., Kreger B.E., Splansky G.L., Freund K.M.…Wilson P.W. Family breast cancer history and mammography: Framingham Offspring Study. American Journal of Epidemiology. 2001;154(10):916–923. doi: 10.1093/aje/154.10.916. [DOI] [PubMed] [Google Scholar]
- Muthén L.K., Muthén B.O. 8th ed. Muthén & Muthén; Los Angeles, CA: 1998-2017. Mplus user's guide. [Google Scholar]
- Oishi S. The psychology of residential mobility: Implications for the self. Social Relationships, and well-being. Perspectives on Psychological Science. 2010;5(1):5–21. doi: 10.1177/1745691609356781. [DOI] [PubMed] [Google Scholar]
- Ortiz D.G., Ostertag S.F. Katrina Bloggers and the Development of Collective Civic Action: The Web as a Virtual Mobilization Structure. The Sociological Perspective. 2014;57(1):52–78. doi: 10.1177/0731121413517558. [DOI] [Google Scholar]
- Rose D.R., Clear T.R. Incarceration, social capital, and crime: Implications for social disorganization theory. Criminology. 1998;36(3):441–480. doi: 10.1111/j.1745-9125.1998.tb01255.x. [DOI] [Google Scholar]
- Rosenfeld R., Baumer E., Messner S.F. Social trust, firearm prevalence, and homicide. Annals of Epidemiology. 2007;17(2):119–125. doi: 10.1016/j.annepidem.2006.07.016. [DOI] [PubMed] [Google Scholar]
- Sampson R.J., Raudenbush S.W., Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277(5328):918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Sampson R.J., Wilson W.J. In: Crime and inequality. Hagan J., Peterson R.D., editors. Stanford University Press; Stanford University Press; Stanford, CA: 1995. Toward a theory of race, crime, and urban inequality; pp. 37–56. [Google Scholar]
- Schultz J., Corman H., Noonan K., Reichman N.E. Effects of child health on parents' social capital. Social Science & Medicine. 2009;69(1):76–84. doi: 10.1016/j.socscimed.2009.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith K.P., Christakis N.A. Social networks and health. Annual Review of Sociology. 2008;34(1):405–429. doi: 10.1146/annurev.soc.34.040507.134601. [DOI] [Google Scholar]
- Stretesky P.B., Schuck A.M., Hogan M.J. Space matters: An analysis of poverty, poverty clustering, and violent crime. Null. 2004;21(4):817–841. doi: 10.1080/07418820400096001. [DOI] [Google Scholar]
- Taylor R.B. 2002. Fear of crime, social ties, and collective efficacy: Maybe masquerading measurement, maybe déjà vu all over again. [Google Scholar]
- Velasquez A., LaRose R. Youth collective activism through social media: The role of collective efficacy. New Media & Society. 2015;17(6):899–918. [Google Scholar]
- Warner B.D., Pierce G.L. Reexamining social disorganization theory using calls to the police as a measure of crime. Criminology. 1993;31(4):493–517. doi: 10.1111/j.1745-9125.1993.tb01139.x. [DOI] [Google Scholar]
- Weissman M.M., Gammon G.D., John K., Merikangas K.R., Warner V., Prusoff B.A., et al. Children of depressed parents: Increased psychopathology and early onset of major depression. Archives of General Psychiatry. 1987;44(10):847–853. doi: 10.1001/archpsyc.1987.01800220009002. [DOI] [PubMed] [Google Scholar]
- Wu C. How does gun violence affect americans' trust in each other? Social Science Research. 2020;91:102449. doi: 10.1016/j.ssresearch.2020.102449. [DOI] [PubMed] [Google Scholar]