Abstract
To fight the COVID-19 pandemic, messenger RNA (mRNA) vaccines were the first to be adopted by vaccination programs worldwide. We sought to investigate the short-term effect of mRNA vaccine administration on endothelial function and arterial stiffness. Thirty-two participants (mean age 37 ± 8 years, 20 men) who received the BNT162b2 mRNA COVID-19 vaccine were studied in three sessions in a sequence-randomized, sham-controlled, assessor-blinded, crossover design. The primary outcome was endothelial function (assessed by brachial artery flow-mediated dilatation (FMD)), and the secondary outcomes were aortic stiffness (evaluated with carotid-femoral pulse wave velocity (PWV)) and inflammation (measured by high-sensitivity C-reactive protein (hsCRP) in blood samples). The outcomes were assessed prior to and at 8 h and 24 h after the 1st dose of vaccine and at 8 h, 24 h, and 48 h after the 2nd dose. There was an increase in hsCRP that was apparent at 24 h after both the 1st dose (−0.60 [95% confidence intervals [CI]: −1.60 to −0.20], p = 0.013) and the 2nd dose (maximum median difference at 48 h −6.60 [95% CI: −9.80 to −3.40], p < 0.001) compared to placebo. The vaccine did not change PWV. FMD remained unchanged during the 1st dose but decreased significantly by 1.5% (95% CI: 0.1% to 2.9%, p = 0.037) at 24 h after the 2nd dose. FMD values returned to baseline at 48 h. Our study shows that the mRNA vaccine causes a prominent increase in inflammatory markers, especially after the 2nd dose, and a transient deterioration of endothelial function at 24 h that returns to baseline at 48 h. These results confirm the short-term cardiovascular safety of the vaccine.
Keywords: SARS-CoV-2, COVID-19, Vaccine, Endothelial dysfunction, Arterial stiffness, Inflammation
Overview of study results describing the effect of the COVID-19 vaccine on endothelial function and arterial stiffness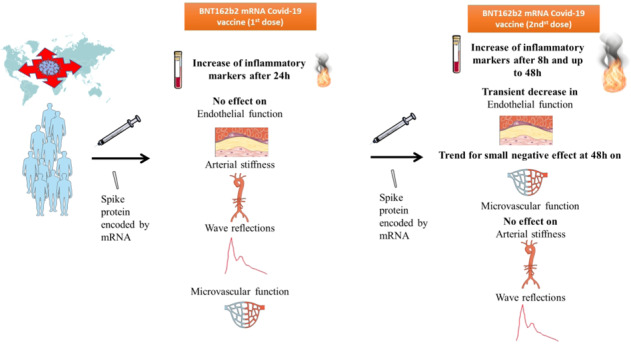
Introduction
The identification of the first severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections and deaths in China in late 2019 rapidly evolved into an unprecedented worldwide pandemic, with more than 380 million cases of coronavirus disease 2019 (COVID-19) and almost 6,000,000 deaths [1]. An enormous effort was undertaken throughout the world to develop medications and vaccines to tackle the increase in deaths and the pressure on health care systems by the pandemic. Currently, at least 140 leading vaccine candidates have been investigated or are under investigation, while more than 190 are in preclinical development [2]. The first vaccine to be approved was Comirnaty (BNT162b2), a messenger ribonucleic acid (mRNA)-based vaccine that produces a membrane-anchored full-length spike protein of the virus and is the first of its type to be used for widespread immunization [3]. mRNA vaccines represent a promising alternative to conventional vaccine approaches because of their capacity for rapid development, the potential for low-cost manufacture, safe administration, and high potency [4]. Currently, more than 10 billion vaccinations in total have been performed worldwide without the report of any substantial complications [5, 6].
SARS-CoV-2 uses angiotensin-converting enzyme 2 (ACE2), a membrane-bound aminopeptidase that is expressed in the lungs, endothelium, heart, and other tissues, as a receptor for its entrance into cells [7]. Accordingly, the hypothesis emerged that SARS-CoV-2 infection, by affecting the endothelium, could increase cardiovascular risk, especially in susceptible patients, either directly or through the activation of the inflammatory cascade [7]. Concerns were also augmented by indirect evidence that the detection of the spike protein in brain endothelial cells was associated with the formation of microthrombi, while pseudovirions (spike, envelope, and membrane proteins) without viral RNA are present in the endothelia of cerebral microvessels [8]. Therefore, it was hypothesized that the viral spike protein that is the target of the principal COVID-19 vaccines could also be one of the basic agents causing damage to distant organs, including the brain, heart, lung, and kidney [8]. Arterial function biomarkers are validated predictors of cardiovascular risk and, as we and others have shown, are able to detect even subtle short-term treatment-related cardiovascular effects, including the effects of vaccines [9–12].
While mRNA vaccines have been widely administered in the last 2 months, their effect on arterial function is not yet defined. In the present study, we investigated the short-term effect of the BNT162b2 mRNA COVID-19 vaccine on endothelial function, arterial stiffness, and inflammatory indices.
Methods
Study population and design
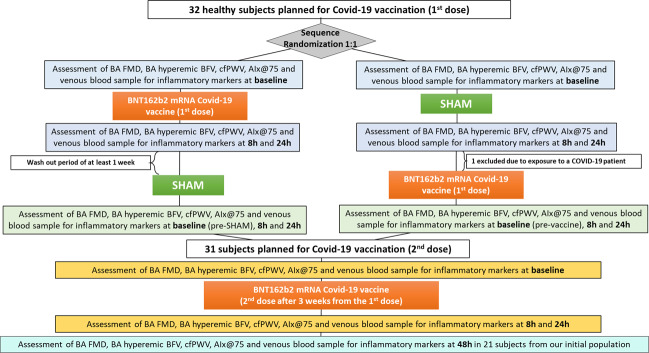
Thirty-two participants (mean age 37 ± 8 years, 20 men) without known cardiovascular disease, diabetes, or systemic inflammatory disease were enrolled to receive the BNT162b2 (Comirnaty®, BioNTech, Mainz, Germany; Pfizer, New York City, NY, USA) mRNA vaccine (2 doses, 30 μg per dose with a 3-week period between the 1st and the 2nd doses) in a sequence-randomized, sham-controlled, assessor-blinded, three-period (1st vaccine dose, 2nd vaccine dose, placebo), crossover design (Fig. 1). Sessions were sequence-randomized with a washout period of at least 7 days between sessions. The sham procedure group was injected with an equal volume of normal saline as placebo. The outcomes were biomarkers of arterial function and inflammation and were assessed prior to and at 8 h and 24 h after the 1st and 2nd vaccine doses. A subset of 21 subjects was also evaluated at 48 h after the 2nd vaccine dose. The additional endpoint at 48 h after the 2nd dose of vaccine was predefined and decided based on the results of an interim analysis of the first ten patients that was performed to ensure safety and no protocol violations. All patients were screened for sociodemographic data and cardiovascular risk factors. One patient was excluded from the final analysis because of exposure to a COVID-19 patient after the first study period and the requirement for self-isolation for the rest of the study. The trial was reported according to the CONSORT guidelines [13]. The study complied with the Declaration of Helsinki, the protocol was approved by our Institutional Research Ethics Committee, and all subjects gave written informed consent.
Fig. 1.
Study flow diagram
Primary and secondary outcomes
The primary outcome of the study was endothelial function as assessed by brachial artery flow-mediated dilatation (FMD) at 24 h after the 2nd dose compared to placebo. Secondary outcomes were aortic stiffness, which was evaluated with carotid-femoral pulse wave velocity (PWV); wave reflections, which were estimated with the aortic augmentation index corrected for a heart rate of 75 beats per minute (AIx@75); microvascular function, which was estimated with the hyperemic mean blood flow velocity (HMBFV) of the brachial artery; and inflammation, which was estimated through the measurement of high-sensitivity C-reactive protein (hsCRP) in blood samples at the rest of the time points.
Study design
Measurements of vascular biomarkers were conducted in a dedicated laboratory with good repeatability. All measurements were performed by the same two examiners (VG, ES) throughout the study who were blinded to the details of individual patients. On all three occasions, subjects fasted and abstained from smoking and caffeine, ethanol, and flavonoid-containing beverage intake for at least 6 hours before each session. All vascular studies were performed in a quiet, temperature-controlled room at 23 °C [8]. After a 10-min rest period, measurements for evaluation of aortic stiffness, wave reflections, and endothelial function of the brachial artery were taken in the supine position in this fixed order. At the completion of vascular studies, blood was drawn, and plasma or serum was separated by centrifugation and stored at −70 °C.
Evaluation of endothelial and microvascular function
FMD of the brachial artery is dependent on endothelial nitric oxide release and can be used as an estimate of endothelial function. FMD was determined by high-resolution vascular ultrasound (LOGIQ P3, GE Healthcare, Fairfield, CT) according to guidelines [14]. Briefly, endothelium-dependent FMD was determined by measuring the change in the diameter of the brachial artery for 2 min after reactive hyperemia for 5 min. FMD was calculated as the percentage change in brachial artery diameter from baseline: FMD (%) = [(postocclusion diameter − resting diameter)/resting diameter] × 100. Analyses were conducted offline by two different investigators blinded to subject treatment. The repeatability coefficient for FMD in our unit is 2%.
The baseline and hyperemic time-averaged velocity (cm/sec) values over each 3-s bin were calculated on the ultrasound system using the manufacturer’s on-screen software. The derived hyperemic mean brachial artery blood flow velocity was used as a marker of microvascular function.
Evaluation of aortic stiffness
Carotid-femoral PWV, an established index of aortic stiffness [11, 15], was calculated from measurements of the pulse transit time and the distance traveled between two recording sites (PWV equals distance in meters divided by transit time in seconds) with a validated noninvasive device (Complior®, Artech Medical, Pantin, France). Two different pulse waves were obtained simultaneously at two sites (at the base of the neck for the common carotid and over the right femoral artery) with two transducers. The distance was defined as the distance from the suprasternal notch to the femoral artery minus the distance from the carotid artery to the suprasternal notch.
Measurement of central pressures and wave reflection indices
Central (aortic) blood pressures (BPs) and AIx@75bpm, a composite index of wave reflections and arterial stiffness [11, 16], were calculated using a validated, commercially available system (SphygmoCor®, AtCor Medical, Sydney, Australia), which employs the principle of applanation tonometry. Waveforms of radial pressure were calibrated according to sphygmomanometric systolic BP and diastolic BP measured in the brachial artery. AIx@75, calculated as the augmented pressure divided by the pulse pressure, was expressed as a percentage and corrected for a heart rate of 75 beats per minute.
Laboratory measurements
Blood samples were collected at baseline and at all time points and periods with individuals in the supine position after an overnight fast, centrifuged at 4000 revolutions per minute for 12 min at 4 °C and stored at −70 °C. HsCRP levels were measured with an immunoturbidimetric assay (CRP vario; Abbott, Wiesbaden, Germany).
Statistical analysis
Statistical normality was checked using the Kolmogorov–Smirnov test. Normally distributed continuous variables are presented as the mean ± SD. Nonnormally distributed variables were log-transformed for analyses and are presented as the median (25–75th percentile). Categorical variables are reported as frequencies and percentages.
Characteristics and resting cardiovascular parameters were compared between the 1st dose vaccine sessions and sham placebo sessions using the paired t test. An analysis of variance (two-way ANOVA) was used to detect statistically significant changes in variables within each session separately (3 time points for the 1st dose and placebo and 4 time points for the 2nd dose). Between-group comparisons at each time point were performed using ANCOVA. The dependent variable was the variable at each predetermined time point. Fixed effects included the treatment and sequence. The baseline value of the variable at each session was used as a covariate. Both vaccine sessions (1st and 2nd) were compared to the sham session. For the nonnormally distributed hsCRP, an independent-sample Mann–Whitney U test was performed to compare hsCRP values at each time point between the vaccination and sham procedure arms. Multiple imputation was employed to adequately deal with missing values. The multiple imputation assumption (values missing total at random) was confirmed by comparing individuals with complete data with those with incomplete data.
Sample size calculations were based on previous data from our unit [9], where the standard deviation of the difference between two measurements of FMD in the same individual was 2.75%. Therefore, we estimated that 30 subjects would provide 80% power at a 5% level of significance to detect a treatment-induced difference of 1.5% in FMD in a crossover design. Taking into consideration a possible dropout rate of 5%, we recruited 32 subjects. A P-value of less than 0.05 was considered statistically significant. Data analysis was performed using the SPSS statistical package for Windows (version 24.0, SPSS Inc., Chicago, Illinois, USA).
Results
Baseline characteristics
There were no differences in any baseline characteristics between the 1st dose vaccine session and the sham session (Tables 1, 2). Conversely, significantly higher values of blood pressure were observed at baseline between the 2nd dose vaccine session and the sham session (Table 2).
Table 1.
Baseline characteristics of the study population (n = 31)
| Age (years) | 37.2 ± 8.3 |
| Sex (males) | 20 (65) |
| Height (m) | 174.5 ± 9.4 |
| Weight (kg) | 76.8 ± 15.9 |
| Body mass index (kg/m2) | 25.1 ± 3.8 |
| Waist (cm) | 91.1 ± 14.6 |
| Hip (cm) | 104.6 ± 7.6 |
| Hypertensives, n (%) | 3 (10) |
| Dyslipidemia, n (%) | 6 (19) |
| Current smokers, n (%) | 7 (23) |
Categorical variables are presented as absolute or relative frequencies, while continuous variables as mean value ± SD.
Table 2.
Baseline characteristics of the study sessions
| BNT162b2 mRNA COVID-19 vaccine (1st dose) | BNT162b2 mRNA COVID-19 vaccine (2nd dose) | Sham vaccine | p-value Vaccine (1st dose) vs. placebo and Vaccine (2nd dose) vs. placebo | |
|---|---|---|---|---|
| Brachial systolic pressure (mmHg) | 115.4 ± 11.6 | 120.3 ± 13.9 | 115.00 ± 16.2 | 0.88 and 0.02 |
| Brachial diastolic pressure (mmHg) | 71.8 ± 8.8 | 74.4 ± 9.3 | 69.7 ± 8.7 | 0.26 and 0.01 |
| Mean pressure (mmHg) | 86.7 ± 8.1 | 89.7 ± 10.0 | 84.6 ± 9.9 | 0.22 and 0.003 |
| Heart Rate (beats/min) | 73.8 ± 10.1 | 75.4 ± 11.4 | 71.4 ± 9.4 | 0.11 and 0.01 |
| Central systolic pressure (mmHg) | 102.1 ± 9.0 | 105.5 ± 11.1 | 101.0 ± 12.9 | 0.61 and 0.01 |
| Central diastolic pressure (mmHg) | 72.9 ± 8.7 | 75.9 ± 9.4 | 70.9 ± 8.8 | 0.27 and 0.007 |
| Augmentation index corrected for heart rate at 75 bpm (%) | 10.5 ± 12.7 | 9.9 ± 11.5 | 8.0 ± 12.2 | 0.11 and 0.25 |
| Carotid-femoral pulse wave velocity (m/s) | 7.0 ± 1.6 | 6.5 ± 1.0 | 6.8 ± 1.4 | 0.18 and 0.16 |
| Brachial artery flow-mediated dilatation (%) | 9.7 ± 3.9 | 9.8 ± 3.8 | 10.0 ± 3.4 | 0.76 and 0.81 |
| Brachial artery hyperemic mean blood flow velocity (cm/s) | 43.9 ± 21.7 | 50.0 ± 12.1 | 53.0 ± 20.1 | 0.08 and 0.48 |
| High-sensitivity C-reactive protein (mg/L) | 1.00 (0.55–2.30) | 0.80 (0.45–1.80) | 0.90 (0.45–1.80) | 0.12 and 0.76 |
Variables as mean value ± SD for normally distributed and median value (25th–75th percentile) for skewed variables. Vaccine (1st dose) vs. placebo and vaccine (2nd dose) vs. placebo baseline sessions were compared using the paired Student’s t test for normally distributed variables and with Wilcoxon Signed Rank test for skewed variables.
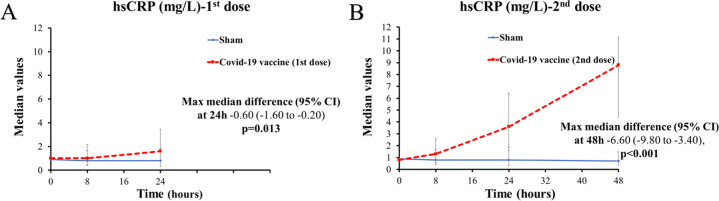
Effect on hsCRP
There was a significant increase in hsCRP that was apparent at 24 h after the 1st dose (max median difference at 24 h −0.60 [95% confidence interval [CI]: −1.60 to −0.20], p = 0.013, Fig. 2A). Similarly, the increase in hsCRP was significant compared to the sham session at 24 h, but there was a much steeper increase in hsCRP with time, and the difference reached its peak at 48 h (maximum median difference at 48 h −6.60 [95% CI: −9.80 to −3.40], p < 0.001, Fig. 2B) (Supplementary Tables 1–3).
Fig. 2.
High-sensitivity C-reactive protein (hsCRP, Panels A and B) in the BNT162b2 mRNA COVID-19 (1st and 2nd dose) and sham sessions during the study (median and interquartile range of measurement). CI Confidence intervals
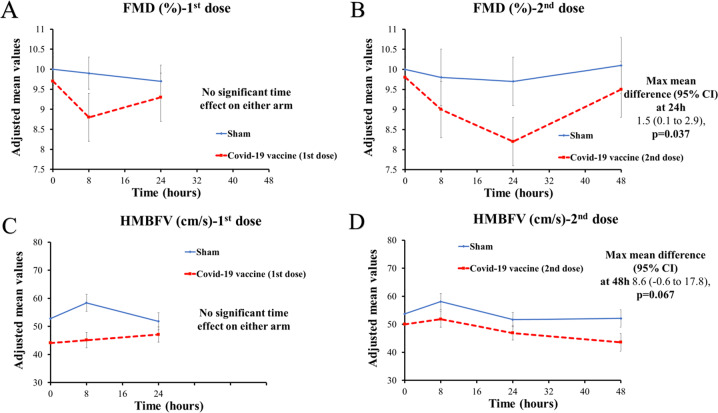
Effects on FMD and HMBFV
The 1st dose of the vaccine did not induce significant changes in FMD during the 1st study period compared to placebo (Fig. 3A). In contrast, FMD had a statistically significant change with time after the 2nd dose. Specifically, FMD decreased significantly by 1.5% (0.1% to 2.9%) at 24 h after the 2nd dose (Fig. 3B). FMD values returned to baseline values at 48 h (Supplementary Tables 1–3).
Fig. 3.
Endothelial (A, B) and microvascular function (C, D) as assessed by brachial flow-mediated dilatation (FMD) and hyperemic mean blow flow velocity (HMBFV) in the BNT162b2 mRNA COVID-19 (1st and 2nd dose) and sham sessions during the study (mean and standard error of measurement). Values, where no time interaction was observed, are adjusted means from ANCOVA (fixed effects included time and baseline value was the covariate), while when time interaction was observed, adjusted mean values from ANCOVA (fixed effects included treatment and sequence and baseline value was the covariate) per time point were used. The latter model was used for estimating the mean difference. CI Confidence interval
The 1st dose of the vaccine did not induce significant changes in HMBFV during the 1st study period compared to placebo (Fig. 3C). In contrast, there was a significant reduction in HMBFV with time after the 2nd dose. The lowest value was observed at 48 h, when HMBFV was numerically lower than with placebo, but the difference between the two sessions did not reach statistical significance (maximum mean difference at 48 h 8.6 [95% CI: −0.6 to 17.8], p = 0.067) (Fig. 3D).
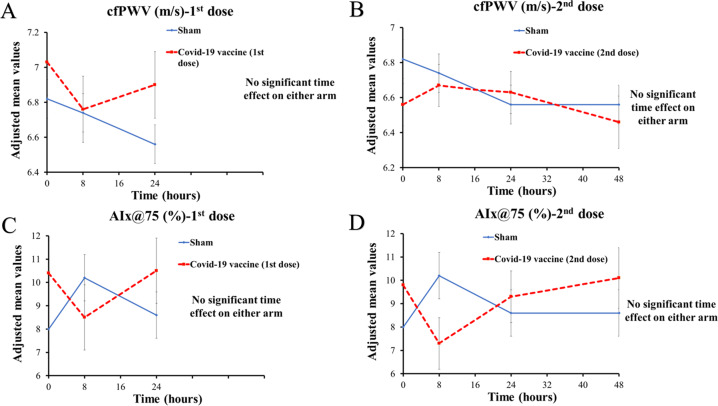
Effects on carotid-femoral PWV and wave reflection indices
The vaccine did not induce significant changes in PWV with time after either the 1st or the 2nd dose (Fig. 4A, B). Similarly, no significant changes in AΙx@75 were noted with time after either of the two vaccine sessions (Fig. 4C, D and Supplementary Tables 1–3).
Fig. 4.
Carotid-femoral pulse wave velocity (cfPWV, Panels A and B) and aortic augmentation index (C, D) corrected for heart rate (AIX@75) in the BNT162b2 mRNA COVID-19 (1st and 2nd dose) and sham sessions during the study (mean and standard error of measurement). Values, where no time interaction was observed, are adjusted means from ANCOVA (fixed effects included time and baseline value was the covariate), while when time interaction was observed, adjusted mean values from ANCOVA (fixed effects included treatment and sequence and baseline value was the covariate) per time point were used. The latter model was used for estimating the mean difference. CI Confidence interval
Effect of sex on the responses to COVID-19 vaccination
The responses of hsCRP, PWV, AIx@75, and HMBFV were not different between males and females or after the 1st or the 2nd dose. In contrast, the response of FMD was more potent after vaccination after both the 1st and 2nd doses for females than for males (Supplementary Fig. 1A, B).
Safety
Participants who received the vaccine reported both local and systemic reactions that are usually reported following the receipt of the BNT162b2 mRNA COVID-19 vaccine. Specifically, 28 out of 31 (90%) reported pain at the injection site after the first dose, but none reported systematic reactions (fever, fatigue, chills, muscle/joint pain). After the 2nd dose, 24 participants reported local reactions (77%), and 12 (39%) out of the 31 participants reported systemic reactions (7 fever and 12 muscle/joint pain and fatigue). No major adverse events were observed.
Discussion
This is the first study to demonstrate the effect of the BNT162b2 mRNA COVID-19 vaccine on endothelial function, arterial stiffness, wave reflection indices and inflammatory biomarkers (Fig. 5). This study shows, for the first time, that the BNT162b2 mRNA COVID-19 vaccine causes a prominent increase in inflammatory markers, especially after the 2nd dose, which is also associated with a moderate transient deterioration of endothelial function at 24 h. No significant time effect was observed for aortic stiffness or wave reflection indices. These results confirm the short-term cardiovascular safety of the vaccine despite its potent inflammatory response.
COVID-19, vaccines and cardiovascular risk
A large number of infectious agents have been linked with an increased cardiovascular risk. Pathogens can exert proatherogenic and proarteriosclerotic effects either directly, by infecting the vascular wall, or indirectly, through systemic inflammatory mechanisms [17]. It has been shown that there is a 5-fold increase in acute myocardial infarction risk and a 3-fold increase in stroke risk following an acute respiratory infection [18]. This risk might be even higher when the infectious agent causes direct endothelial and myocardial injury [19, 20]. The overactivation of the inflammatory cascade is one of the main mechanisms by which SARS-CoV-2 infection harms the cardiovascular system. Furthermore, SARS-CoV-2 is able to directly infect endothelial cells, inducing endothelial injury and endotheliitis (with infiltration of inflammatory cells into vessel walls) [21]. SARS-CoV-2, which enters endothelial cells through ACE2, downregulates ACE2 expression and reduces its activity; both have been shown to be associated with vascular dysfunction [7]. Subjects recovering from a recent (in the last month) SARS-CoV-2 infection have pronounced endothelial dysfunction and increased arterial stiffness compared to controls, supporting a deleterious effect of the infection on both small and large arteries [22]. The S protein alone can damage the endothelium, as manifested by endothelial nitric oxide synthase activity and impaired mitochondrial function. It seems that the S protein increases redox stress in endothelial cells and ultimately leads to ACE2 destabilization. A dysregulated renin-angiotensin system due to ACE2 reduction may exacerbate endothelial dysfunction, possibly leading to endotheliitis. Unlike an infection, the spike protein resulting from COVID-19 vaccination does not assemble into new viral particles. Instead, it attaches to the cell surface as it would to the viral surface. Finally, the spike protein is genetically modified to enhance the immune response and prevent its binding to ACE2 receptors. For these reasons, exogenous antibodies against the S protein and/or vaccination-generated antibodies not only protect against SARS-CoV-2 infection in the host but also prevent S protein-imposed endothelial injury during infection. One could argue that the short transient endothelial dysfunction noted after vaccination is a very small, transient price to pay compared to the abovementioned beneficial effects. The ongoing, large, international, multicenter COVID-19 Effects on Arterial Stiffness and Vascular Aging (CARTESIAN) study is expected to provide more robust data on the exact effect of the infection and COVID-19 vaccination on vascular health and aging in the long term [23]. However, even from early reports, there is convincing evidence that vascular parameters are predictive of cardiovascular events in COVID-19 patients [24, 25].
Although mRNA COVID-19 vaccines are considered safe, and the benefits from vaccination outweigh any known risk, data on the possible effects of these vaccines on the cardiovascular system are scarce. Some concern has been raised by the possible side effects of the produced spike on macro- and microcirculation. The detection of the spike protein in brain endothelial cells has been associated with the formation of microthrombi, while the detection of pseudovirions (spike, envelope, and membrane proteins) without viral RNA in the endothelia of cerebral microvessels may theoretically cause microvascular injury irrespective of the immune response [26, 27]. Furthermore, experimental data show the entrance of the spike protein in cardiac pericytes and pulmonary vascular cells, which promotes cell signaling leading to vascular cell dysfunction and cell growth/hypertrophy [28, 29]. It seems extremely interesting to be able to detect spike protein levels in plasma [30, 31], but to the best of our knowledge, no practical, clinical use has been implemented thus far while these techniques are not widely available for use to investigate whether there is an association between the observed changes in endothelial function and the spike levels in plasma [32].
On the other hand, the triggering of the inflammatory cascade itself might adversely affect vascular function. We and others have shown the acute harmful effect of inflammation on endothelial function and arterial stiffness [9, 10, 33, 34], which are reliable, validated predictors of cardiovascular risk [15, 16]. Furthermore, we and others have shown the effect of various vaccines on these parameters [35]. CRP levels are considered a pharmacodynamic marker for the mode of action of RNA vaccines that activates both innate and adaptive immune responses [36]. Innate immunity sensors are triggered by the intrinsic adjuvant activity of vaccines [37]. The lipid nanoparticle (LNP) carrier protects the mRNA to be delivered to lymphatics and promotes protein translation in lymph nodes. In lymph nodes, the LNP is engulfed by dendritic cells, which produce and present the antigen to T cells for the activation of the adaptive immune response [37].
Overall, the present study aimed to investigate both direct (by impacting host vascular cells) and indirect (by secretion of proinflammatory molecules and production of proapoptotic factors) effects of COVID-19 vaccination. For this purpose, we employed a wide array of validated vascular indices that target both macrovascular and microvascular function. While there were no changes after the 1st dose, there was a transient deterioration of endothelial function after the 2nd dose that was reversed at 48 h. This reversal attests to nonsignificant harm by the vaccine. The theoretical effect of spike proteins on microvascular function is not supported based on the fact that there was not a statistically significant reduction in HMBFV up to 48 hours after the 2nd dose when the spike proteins were at their highest levels. Furthermore, PWV did not change with time in our study. It is well established that PWV has pressure-dependent and pressure-independent determinants. The pressure-dependent component is not affected since there is no increase in BP, as we have shown. The endothelium affects the BP-independent component, but it is not the sole factor that does so. It appears that the magnitude of the endothelial effect after COVID-19 vaccination is not large enough to affect PWV by itself, providing further confirmation about vaccine safety. Therefore, the notion of the safety of the COVID-19 vaccination is further corroborated by the absence of any effect on arterial stiffness and wave reflections.
There are similarities and differences with other types of vaccines. While we confirmed the prominent activation of the inflammation pathway with vaccination, a novelty of our study is the assessment of a 2-dose vaccine on inflammation and vascular function. The type/technology of the vaccine seems to play a role. Indeed, as we have shown [10, 33], the Salmonella typhi vaccine (that contains purified Vi capsular polysaccharide of S. typhi that is a T cell-independent antigen of the bacterium and thus mediates protection through antibody-dependent mechanisms) had a potent deleterious effect both on FMD and arterial stiffness, whereas the single-dose H1N1 influenza vaccine that contains a monovalent, split inactivated form of the virus with a water‐in‐oil adjuvant (MF59, which leads to faster responses and dose sparing to achieve greater coverage) caused solely endothelial dysfunction up to 48 h [9]. In contrast, the current mRNA vaccine did not have any significant time effect on vascular biomarkers after the first dose, when the effect on inflammation was weaker; only after the 2nd dose was there a transient effect on FMD (peaking at 24 h) when the inflammation was more potent.
There was a dissociation of the timing of peak hsCRP and nadir FMD. However, this does not cast doubt on the etiologic link of the effect of inflammation on endothelial function. In one of our previous studies, we showed that an increase in CRP lags the peak of arterial dysfunction [10]. In contrast, the course of other inflammatory markers/mediators, such as IL-6, coincides temporally with arterial function changes. Finally, an additional, interesting finding is that the magnitude of hsCRP increase in this 2-dose regimen is much higher than what was observed from other single-dose vaccines thus far.
Sex differences in both the innate and adaptive immune systems have been previously reported and may account for the female advantage in COVID-19. Within the adaptive immune system, females have increased B cell production of immunoglobulin, more robust CD8 + T cell cytotoxic activity and higher numbers of CD4 + T cells than males. Women produce higher antibody titers in response to the trivalent inactivated seasonal influenza vaccination (TIV), as well as to most other pathogen vaccines, and report more severe local and systemic side effects. More specifically, females achieve equivalent protective antibody titers to males at half the dose of TIV, with serum testosterone levels inversely correlating with TIV antibody titers. These findings imply that females have an increased capacity to mount humoral immune responses compared to males. This could explain the larger effect on endothelial dysfunction in females than males.
Limitations
The population of the study is modest. However, this was based on an a priori estimation of the sample size, and as this is a hypothesis-generating study, we consider it adequate to derive reliable results for the primary outcome.
A 2nd sham procedure session was not performed. This decision was dictated by the very short, mandatory period (21 days) between the two doses that did not allow for an adequate washout period between sessions.
Values from the predefined inclusion of an additional time point at 48 h after the 2nd dose of vaccine were compared with values from the 24 h time point of the sham procedure. However, based on the minimal effect of time on all our endpoints, we believe that any error by this assumption would not affect our results in a clinically meaningful way.
We chose to use the BNT162b2 (Comirnaty®) mRNA vaccine, as this was the first to be used and the one with the largest number of vaccines worldwide. Therefore, any assumptions made for this vaccine cannot be extrapolated to other COVID-19 vaccines, especially those that do not use mRNA technology. We hope that our study will serve as an impetus for studies with other vaccines.
Conclusion
The BNT162b2 mRNA vaccine for COVID-19 induces a moderate and transient short-term dysfunction of the endothelium that is almost entirely reversed in 48 h. The effect is explicable on the basis of either the direct or inflammatory-mediated effects of the vaccine. These findings expand our understanding of the overall cardiovascular profile and safety of the BNT162b2 mRNA COVID-19 vaccine and may have implications for the cardiovascular safety of the entire group of mRNA vaccines.
Supplementary information
Compliance with ethical standards
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41440-022-00876-6.
References
- 1.World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/?gclid=CjwKCAiAsaOBBhA4EiwAo0_AnPoKZSzbiK7p4rGVggeX8BwZkkKOksOTzIDYbYExXTksUQC5aIC8lRoCxXgQAvD_BwE. Accessed February, 2022.
- 2.World Health Organization. Draft landscape and tracker of COVID-19 candidate vaccines. https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines. Accessed February, 2022.
- 3.Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N. Engl J Med. 2020;383:2603–15. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin CJ, Mecham RP, Mann DL. RNA vaccines for COVID-19: 5 things every cardiologist should know. JACC Basic Transl Sci. 2020;5:1240–3. doi: 10.1016/j.jacbts.2020.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Our World In Data. Coronavirus (COVID-19) Vaccinations. 2021; https://ourworldindata.org/covid-vaccinations. Accessed February, 2022.
- 6.Shimabukuro T, Nair N. Allergic Reactions Including Anaphylaxis After Receipt of the First Dose of Pfizer-BioNTech COVID-19 Vaccine. JAMA. 2021;325:780–1. doi: 10.1001/jama.2021.0600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Libby P, Luscher T. COVID-19 is, in the end, an endothelial disease. Eur Heart J. 2020;41:3038–44. doi: 10.1093/eurheartj/ehaa623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Food and Drug Administration. Comment from J. Patrick Whelan MD PhD. 2020; https://www.regulations.gov/document/FDA-2020-N-1898-0246. Accessed February, 2021.
- 9.Vlachopoulos C, Xaplanteris P, Sambatakou H, Mariolis E, Bratsas A, Christoforatou E, et al. Acute systemic inflammation induced by influenza A (H1N1) vaccination causes a deterioration in endothelial function in HIV-infected patients. HIV Med. 2011;12:594–601. doi: 10.1111/j.1468-1293.2011.00935.x. [DOI] [PubMed] [Google Scholar]
- 10.Vlachopoulos C, Dima I, Aznaouridis K, Vasiliadou C, Ioakeimidis N, Aggeli C, et al. Acute systemic inflammation increases arterial stiffness and decreases wave reflections in healthy individuals. Circulation. 2005;112:2193–2200. doi: 10.1161/CIRCULATIONAHA.105.535435. [DOI] [PubMed] [Google Scholar]
- 11.Vlachopoulos C, Xaplanteris P, Aboyans V, Brodmann M, Cífková R, Cosentino F, et al. The role of vascular biomarkers for primary and secondary prevention. A position paper from the European Society of Cardiology Working Group on peripheral circulation: Endorsed by the Association for Research into Arterial Structure and Physiology (ARTERY) Society. Atherosclerosis. 2015;241:507–32. doi: 10.1016/j.atherosclerosis.2015.05.007. [DOI] [PubMed] [Google Scholar]
- 12.Tang DC, Nguyen HH. The Yin-Yang arms of vaccines: disease-fighting power versus tissue-destructive inflammation. Expert Rev Vaccines. 2014;13:417–27. doi: 10.1586/14760584.2014.882775. [DOI] [PubMed] [Google Scholar]
- 13.Dwan K, Li T, Altman DG, Elbourne D. CONSORT 2010 statement: extension to randomised crossover trials. BMJ. 2019;366:l4378. doi: 10.1136/bmj.l4378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thijssen DHJ, Bruno RM, van Mil A, Holder SM, Faita F, Greyling A, et al. Expert consensus and evidence-based recommendations for the assessment of flow-mediated dilation in humans. Eur Heart J. 2019;40:2534–47. doi: 10.1093/eurheartj/ehz350. [DOI] [PubMed] [Google Scholar]
- 15.Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;55:1318–27. doi: 10.1016/j.jacc.2009.10.061. [DOI] [PubMed] [Google Scholar]
- 16.Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar ME, Baou K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with central haemodynamics: a systematic review and meta-analysis. Eur Heart J. 2010;31:1865–71. doi: 10.1093/eurheartj/ehq024. [DOI] [PubMed] [Google Scholar]
- 17.Libby P, Loscalzo J, Ridker PM, Farkouh ME, Hsue PY, Fuster V, et al. Inflammation, Immunity, and Infection in Atherothrombosis: JACC Review Topic of the Week. J Am Coll Cardiol. 2018;72:2071–81. doi: 10.1016/j.jacc.2018.08.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Corrales-Medina VF, Musher DM, Shachkina S, Chirinos JA. Acute pneumonia and the cardiovascular system. Lancet. 2013;381:496–505. doi: 10.1016/S0140-6736(12)61266-5. [DOI] [PubMed] [Google Scholar]
- 19.Giustino G, Croft LB, Stefanini GG, Bragato R, Silbiger JJ, Vicenzi M, et al. Characterization of myocardial injury in patients with COVID-19. J Am Coll Cardiol. 2020;76:2043–55. doi: 10.1016/j.jacc.2020.08.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kotecha T, Knight DS, Razvi Y, Kumar K, Vimalesvaran K, Thornton G, et al. Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance. Eur Heart J. 2021;42:1866–78. [DOI] [PMC free article] [PubMed]
- 21.Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–8. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ratchford SM, Stickford JL, Province VM, Stute N, Augenreich MA, Koontz LK, et al. Vascular alterations among young adults with SARS-CoV-2. Am J Physiol Heart Circ Physiol. 2021;320:H404–10. [DOI] [PMC free article] [PubMed]
- 23.Rosa Maria B, Bart S, Bernhard H, Hughes A, Lacolley P, Mayer CC, et al. Covid-19 effects on ARTErial stIffness and vascular AgeiNg: CARTESIAN study rationale and protocol. Artery Res. 2020;27:59–68. doi: 10.2991/artres.k.201124.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rodilla E, Lopez-Carmona MD, Cortes X, Cobos-Palacios L, Canales S, Sáez MC, et al. Impact of arterial stiffness on all-cause mortality in patients hospitalized with COVID-19 in Spain. Hypertension. 2021;77:856–67. doi: 10.1161/HYPERTENSIONAHA.120.16563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schnaubelt S, Oppenauer J, Tihanyi D, Mueller M, Maldonado-Gonzalez E, Zejnilovic S, et al. Arterial stiffness in acute COVID-19 and potential associations with clinical outcome. J Intern Med. 2021;290:437–43. doi: 10.1111/joim.13275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buzhdygan TP, DeOre BJ, Baldwin-Leclair A, Bullock TA, McGary HM, Khan JA, et al. The SARS-CoV-2 spike protein alters barrier function in 2D static and 3D microfluidic in-vitro models of the human blood-brain barrier. Neurobiol Dis. 2020;146:105131. doi: 10.1016/j.nbd.2020.105131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Basta G. Direct or indirect endothelial damage? An unresolved question. EBioMedicine. 2021;64:103215. doi: 10.1016/j.ebiom.2021.103215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Suzuki YJ, Nikolaienko SI, Dibrova VA, Dibrova YV, Vasylyk VM, Noviko MY, et al. SARS-CoV-2 spike protein-mediated cell signaling in lung vascular cells. Vascul Pharmacol. 2021;137:106823. doi: 10.1016/j.vph.2020.106823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Avolio E, Gamez M, Gupta K, Williamson MK, Beltrami AP, Gupta K, et al. The SARS-CoV-2 spike protein disrupts the cooperative function of human cardiac pericytes-endothelial cells through CD147 receptor-mediated signalling: a potential non-infective mechanism of COVID-19 microvascular disease. Clin Sci (Lond) 2021;135:2667–89. doi: 10.1042/CS20210735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ogata AF, Cheng CA, Desjardins M, Senussi Y, Sherman AC, Powell M, et al. Circulating SARS-CoV-2 Vaccine Antigen Detected in the Plasma of mRNA-1273 Vaccine Recipients. Clin Infect Dis. 2022;74:715–8. doi: 10.1093/cid/ciab465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cognetti JS, Miller BL. Monitoring serum spike protein with disposable photonic biosensors following SARS-CoV-2 vaccination. Sensors. 2021;21:5857. doi: 10.3390/s21175857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Theoharides TC, Conti P. Be aware of SARS-CoV-2 spike protein: There is more than meets the eye. J Biol Regul Homeost Agents. 2021;35:833–8. doi: 10.23812/THEO_EDIT_3_21. [DOI] [PubMed] [Google Scholar]
- 33.Vlachopoulos C, Aznaouridis K, Dagre A, Vasiliadou C, Masoura C, Stefanadi E, et al. Protective effect of atorvastatin on acute systemic inflammation-induced endothelial dysfunction in hypercholesterolaemic subjects. Eur Heart J. 2007;28:2102–9. doi: 10.1093/eurheartj/ehm247. [DOI] [PubMed] [Google Scholar]
- 34.Jain S, Khera R, Corrales-Medina VF, Townsend RR, Chirinos JA. Inflammation and arterial stiffness in humans. Atherosclerosis. 2014;237:381–90. doi: 10.1016/j.atherosclerosis.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 35.Kharbanda RK, Walton B, Allen M, Klein N, Hingorani AD, MacAllister RJ, et al. Prevention of inflammation-induced endothelial dysfunction: a novel vasculo-protective action of aspirin. Circulation. 2002;105:2600–4. doi: 10.1161/01.CIR.0000017863.52347.6C. [DOI] [PubMed] [Google Scholar]
- 36.Sahin U, Muik A, Derhovanessian E, Vogler I, Kranz LM, Vormehr M, et al. COVID-19 vaccine BNT162b1 elicits human antibody and TH1 T cell responses. Nature. 2020;586:594–9. doi: 10.1038/s41586-020-2814-7. [DOI] [PubMed] [Google Scholar]
- 37.Teijaro JR, Farber DL. COVID-19 vaccines: modes of immune activation and future challenges. Nat Rev Immunol. 2021;21:195–7. doi: 10.1038/s41577-021-00526-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.