SUMMARY
Providing in-patient nursing care inevitably involves shift work and shift patterns have been identified as an important factor in determining well-being and satisfaction among nurses. Shifts of 12 h or longer have become increasingly common for nurses in hospitals in some European countries. Longer shifts offer a potential to benefit from a compressed working week, with fewer work days and more days off-work, lower commuting costs, and increased flexibility. Most people find shift work less desirable compared to standard working hours. A cross-sectional cohort study was conducted at the Mostar University Hospital in 2019. A total of 157 subjects participated in the study, 22 (14%) of which were male (medical technicians) and 135 (86%) female (nurses). The mean age of study subjects was 33.3 years (min=20, max=54, SD=8.033). Results of this study suggested that nurses working irregular rotating shifts, with more family members to look after and more than 18 years of professional experience were affected by sleep disturbances between shifts. The study showed that shift work nurses had significantly higher levels of cortisol and prolactin compared with first-shift nurses/medical technicians. The results of this study are expected to stimulate further studies of sleep disturbances among shift nurses.
Key words: Cortisol, Prolactin, Circadian rhythm, Nurses
Introduction
Providing in-patient nursing care inevitably involves shift work and shift patterns have been identified as an important factor in determining well-being and satisfaction among nurses (1-5). Shifts of 12 h or longer have become increasingly common for nurses in hospitals in some European countries (6). Longer shifts offer a potential to benefit from a compressed working week, with fewer work days and more days off-work, lower commuting costs, and increased flexibility (7). Most people find shift work less desirable compared with standard working hours. The main reason for this is when working at a non-standard time (e.g., night shift), which is not in concordance with the biological clock (circadian rhythm), individuals tend to develop a ‘social jet lag’, discrepancy between sleep timing on work days and free days (7-11). However, previous studies on shift length in Europe did not provide evidence for nurses working a compressed work week, so it is not clear if working 12-h shifts is associated with fewer days at work (6, 12, 13). Differences in work hour regulations among countries may limit the generalizability of the United States (US) research. The US has regulations governing nurses’ work hours that differ from the European Working Time Directive, in terms of limiting weekly hours, including overtime, and providing extra protection for between-shift rest hours and night work (14). Prolonged irregular shift work can affect the quality of sleep and social life, and may, in severe cases, cause health problems such as hypertension and gastrointestinal problems, breast cancer, particularly among women performing shift work during young adulthood (15-20). Cortisol, which is a hormone secreted by the adrenal gland, plays a crucial role in stress responses and helps the human body adapt to its environment (21). When sleep begins, the hypothalamic-pituitary-adrenal (HPA) axis becomes inert (22). Occasional sleep loss is associated with activation of the HPA axis, while waking up in the middle of the night is caused by sudden release of cortisol. The cortisol awakening response refers to a rapid increase in cortisol levels within 30-45 min of waking, which is closely related to HPA axis activity (23). Shift rotations stimulate HPA axis activity in the neuroendocrine system, which disrupts the negative regulation of corticosteroids (24). A negative correlation exists between the morning and pre-sleep cortisol levels of shift workers and sleep duration (25). Thus, shift type may also influence cortisol patterns in the body.
The aim of this study was to evaluate the cortisol and prolactin levels in nurses after a night shift (shift work) and at the beginning of the first shift (standard day working hours), and whether shift work affected their circadian rhythm.
Subjects and Methods
A cross-sectional cohort study was conducted at the Mostar University Hospital between February 1 and July 14, 2019. A total of 157 subjects participated in the study, 22 (14%) of which were male (medical technicians) and 135 (86%) female (nurses), mean age 33.3 years (range 20-54 years, SD=8.033). Study subjects were divided into two groups, as follows: experimental group including 80 (51%) subjects working in shifts (12 working hours-24 hours off-work, 12 working night shift hours-48 hours off-work); and control group including 77 (49%) subjects working morning shifts, i.e. seven working hours (7:30 am to 2:30 pm). Inclusion criteria were nurses/medical technicians aged 20-55 years with working experience longer than 6 months in shifts and workplace with permanent employment (permanently employed nurses). Exclusion criteria were nurses/medical technicians younger than 20 and older than 55 years, subjects with less than 6 months of working experience, pregnancy, endocrine disorders and taking medications that can affect hormonal status, and a workplace with definite employment (nurses without permanent employment). The study was approved by the Ethics Committee of the Mostar University Hospital and was conducted in accordance with the Declaration of Helsinki principles. All subjects were previously informed on the purpose of the study, privacy and confidentiality of personal information, and they provided their written consent for participation in the study. In experimental group, blood for determination of metabolic (hormonal) status was sampled after night shift at 8:00 am. In control group, blood sampling was performed upon their arrival to work. Immediately before blood sampling, at 7:30 am, intravenous cannulas were set in all subjects, and at the abovementioned time (with a 30-min delay), a sample was taken into a biochemical tube. With the introduction of intravenous cannula, the effect of pain due to the possible increase of cortisol concentration was reduced. Blood was centrifuged at 3500 rpm, serum samples were separated into special tubes and stored at -20 °C until analysis. The subjects of both groups fulfilled six scales of the shortened version of the Standard Shiftwork Index (SSI), which was used to examine the influence of shift work on the circadian rhythm. The SSI scale consists of general information (age, sex, marital status, number of household members, work experience, number of weekly work hours, number of night shifts and day shifts, and their duration in a month) and five scales. The first scale refers to sleep and fatigue of nurses/medical technicians, and was used to test the quality of sleep, time for sleep compensation, restfulness after sleep, sleepiness during working hours, taking sleep pills, fatigue and energy during working hours. Total score on the scale is calculated as the sum of answers to all questions, where higher results indicate greater sleeping disorder. The second scale refers to the health and well-being of the subject, and was used to test symptoms of the most common diseases, diagnosed illnesses, consumption of alcohol, coffee, tea and cigarettes, and the feelings of usefulness, concentration and self-confidence. The third scale refers to the social and family situation, and was used to test satisfaction with the time provided by the working system for particular social activities (sports activities, partners, children, hobbies, going out, excursions, chores, religious activities, etc.). The fourth scale refers to problems in shift work, and was used to test the influence of work on the problems in the fields of sleep, social and family life, work effect, and organizational problems at the workplace. The fifth scale refers to the personality and was used to test subjective feelings of excitement, hastiness, mood and sociability. More detailed information on the need for sleeping in leisure time (getting up, going to sleep) is required, as well as data to determine the types of subjects in relation to general life satisfaction and daily habits and rhythm of life (morning type, evening type).
Statistical analysis
The data collected were filed and analyzed using IBM SPSS Statistics 20.0. Descriptive statistics presented the basic attributes of the samples, including frequency distribution, frequency percentage, mean and SD. The χ2-test was used to test differences between categorical variables, while the independent samples t-test was used for analysis of differences between continuous variables. The level of probability of p<0.05 was considered statistically significant. According to the Shapiro-Wilk normality test results, the distributions of results of major outcome measures were normal for some variables, while for other variables, they deviated significantly from the normal distribution. Specifically, the cortisol value scores, as well as the results on the energy scale were normally distributed in both groups.
Results
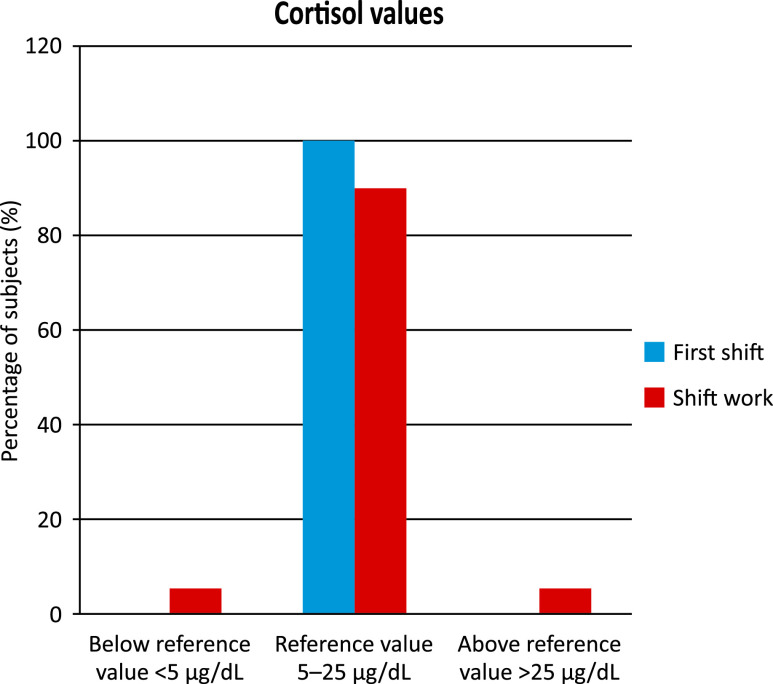
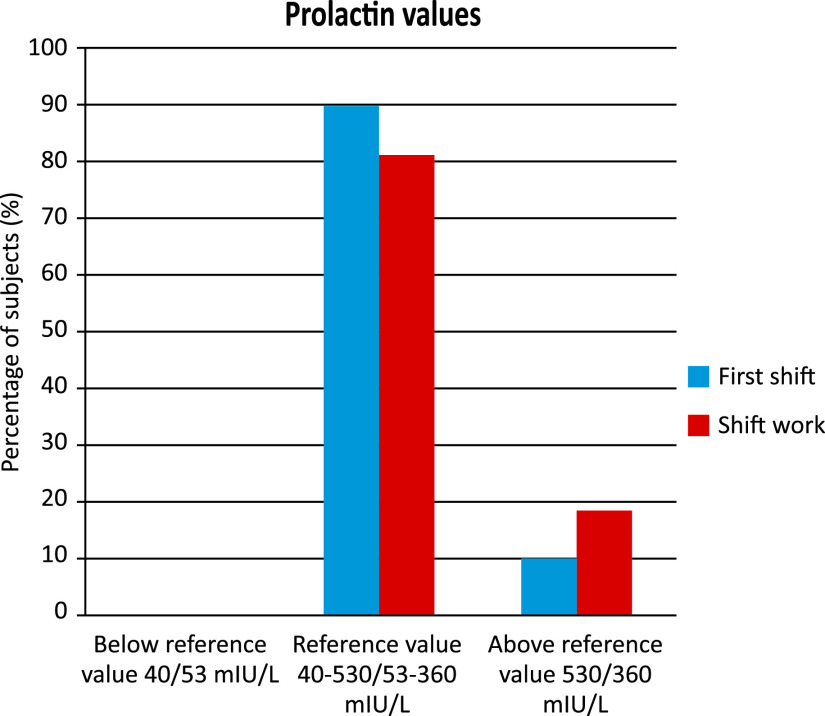
The results on the morning-evening scale and total fatigue were normally distributed only in the shift work group. Distribution of prolactin value scores significantly deviated from normal distribution in both groups, and was positively asymmetric, as was the distribution of scores on the workload scale. These asymmetric results were not irregular when it comes to measuring prolactin values or to the application of clinical instruments on a healthy population, and they do not represent an obstacle for using parametric tests, but merely speak of the nature of the phenomenon examined (26). Statistically significant differences were determined in the levels of cortisol and prolactin between the nurses/medical technicians working in first shift and nurses/medical technicians working in shifts, with significantly higher levels of cortisol and prolactin recorded in the latter (Table 1). All study nurses/medical technicians working in first shift had their cortisol levels within the reference values, whereas 5% of those working in shifts had cortisol levels lower than the reference values, and the same number had cortisol levels higher than the reference values (Fig. 1). Although the number of nurses/medical technicians with prolactin values exceeding the reference values was greater in the experimental group working in shifts than in the control group working first shift, the difference was not statistically significant (χ2=2.193, p=0.139) (Fig. 2). Significant differences between the two groups were determined in the evaluation of fatigue during working hours, which showed the subjects working first shift to exhibit higher restfulness as compared with restfulness felt by the subjects working in shifts after a night shift, but also when compared with restfulness in the subjects working in shifts after a daily shift. The subjects working in shifts showed significantly higher levels of sleep difficulties than the subjects working first shift. There were no significant differences in chronic fatigue (lack of energy) between the two study groups (Table 2). Significant differences were determined in the level of workload in certain parts of the day between the two groups, with the subjects working in shifts reporting higher workload estimates in all parts of the day than those working first shift (Table 3). The length of work experience was significantly negatively related to the workload evaluation in the afternoon and evening hours. The more work experience the subjects had, the lower was their evaluation of workload in the afternoon and evening hours. The mentioned relationships were low to moderate. The results depicted in Table 4 show that subjects with greater work experience had less daily need for sleep, reported poor sleep and more frequent use of sleeping pills. Subjects with greater work experience reported lower levels of fatigue after work as well. No significant correlations were found between work experience and results on the post-sleep fatigue scale, or in the overall results on the sleep problem scale. On average, the subjects working in shifts more frequently considered that the system of working in shifts interfered with the activities they would like to do in their leisure time and with their family responsibilities, as compared with the subjects working first shift (Table 5). Furthermore, the subjects working in shifts showed more sleep problems than those working first shift. There were no significant differences between the two groups of subjects according to the morningness/eveningness type.
Table 1. Cortisol and prolactin concentrations in nurses and medical technicians working night shift and morning shift.
| Variable | M | SD | t | df | p value | |
|---|---|---|---|---|---|---|
| Cortisol | First shift (n=77) | 14.29 ug/dL | 3.879 | -2.345 | 144 | 0.020* |
| Shift work (n=80) | 16.04 ug/dL | 5.338 | ||||
| Prolactin | First shift (n=77) | 284.84 mlU/L | 150.06 | -2.366 | 136 | 0.019* |
| Shift work (n=80) | 358.52 mlU/L | 232.77 |
*p<0.05
Fig. 1.
Cortisol values in subjects working first shift and those working in shifts with regard to reference values.
Fig. 2.
Prolactin values in subjects working first shift and those working in shifts with regard to reference values.
Table 2. Significance of differences in pooled results on the scale of sleep and fatigue, energy and workload.
| Group | M | SD | t | df | p value | |
|---|---|---|---|---|---|---|
| Fatigue | First shift | 3.01 | .993 | -5.607 | 155 | <0.001* |
| Night shift | 3.88 | .933 | ||||
| Fatigue | First shift | 3.01 | .993 | -3.953 | 155 | <0.001* |
| Daily shift | 3.68 | 1.099 | ||||
| Sleep difficulties and fatigue | First shift | 17.40 | 2.751 | -4.167 | 155 | <0.001* |
| Shift work | 19.20 | 2.673 | ||||
| Lack of energy | First shift | 2.49 | 0.853 | -1.265 | 155 | 0.208 |
| Shift work | 2.66 | 0.821 | ||||
| Workload in the morning | First shift | 11.95 | 3.688 | -5.866 | 155 | <0.001* |
| Shift work | 15.26 | 3.389 | ||||
| Workload in the afternoon | First shift | 8.06 | 4.840 | -10.196 | 129 | <0.001* |
| Shift work | 14.66 | 3.114 | ||||
| Workload at night | First shift | 6.01 | 4.093 | -15.490 | 155 | <0.001* |
| Shift work | 15.36 | 3.454 |
*p<0.05
Table 3. Significance of the relationship of work experience with workload in different parts of the day.
| Workload-morning | Workload-afternoon | Workload-night | Lack of energy | |
|---|---|---|---|---|
| Work experience | -0.151 | -0.175* | -0.316** | -0.090 |
*p<0.05; **p<0.001
Table 4. Significance of the connection between work experience and sleep problems.
| Daily need for sleep | Bad sleep | Fatigue after sleep | Sleeping pills | Fatigue daily shift | Fatigue night shift | Total sleep problems | |
|---|---|---|---|---|---|---|---|
| Work experience | -0.201* | 0.188* | -0.077 | 0.200* | -0.225* | -0.187* | -0.135 |
*p<0.05
Table 5. Evaluation of interference with leisure time and family responsibilities in the system of shift work, sleep problems and type of morningness/eveningness caused by this system.
| Group | M | SD | t | df | p value | |
|---|---|---|---|---|---|---|
| Interference with leisure time | First shift | 2.06 | 1.080 | -7.370 | 155 | <0.001* |
| Shift work | 3.35 | 1.104 | ||||
| Interference with family responsibilities | First shift | 2.12 | 1.038 | -7.112 | 155 | <0.001* |
| Shift work | 3.33 | 1.088 | ||||
| Sleep problems | First shift | 2.71 | 1.441 | -7.701 | 136 | <0.001* |
| Shift work | 4.25 | 1.013 | ||||
| Eveningness | First shift | 12.19 | 2.920 | -1.855 | 155 | 0.066 |
| Shift work | 13.06 | 2.940 |
*p<0.05
Discussion
Shift working can result in desynchronization of the endogenous cycle, leading to disruption of normal sleep-wake rhythm of shift workers. Shift workers suffer from insufficient restorative sleep, which can lead to inability to tolerate morning shifts. In our study, a strong correlation was found in the rate of sleep disturbances between morning shift workers and those participants working a rotating shift system. Shift working nurses find it stressful to deal with the combination of family-home environment, their responsibilities in caring for children, and night shifts (27). Night shift after full day work at home does not allow sufficient time for rest and sleep, and our study found that shift work nurses more frequently used sleeping pills, which is consistent with the results of other studies (24-26). The ability to achieve sleep that is uninterrupted and of sufficient length, even under optimal conditions, is diminished with age. This explains the findings of this study where shift workers with more years of professional experience reported having more sleep disturbance problems (28, 29). Furthermore, there is a natural tendency for older people to become morning people rather than night owls, which makes night work difficult and may contribute to their resignation from night shifts. Age should be taken in consideration when scheduling shifts (30). Female nurses suffer more sleep problems in all shifts than males, and a possible explanation could be that female shift workers have more responsibilities of looking after their home and children, and the majority of housework, which may aggravate sleep problems and tiredness (31-33). Finally, shift nurses who preferred morning activities appeared to have less sleep problems between morning shifts, and this finding is consistent with other studies. No differences were observed according to family status, professional training, or circadian characteristics (languidness and flexibility).
Conclusion
Our results suggest that female nurses working in irregular rotating shifts, who have more family members to look after and more than 18 years of professional experience, suffer from sleep disturbance between shifts. Statistically significant differences were found in cortisol and prolactin levels in shift working nurses/medical technicians. This study found that shift working nurses had significantly higher levels of cortisol and prolactin in comparison to first shift nurses/medical technicians. The results of this study could stimulate further study of sleep disturbances in nurses working rotating shifts.
Acknowledgments
The authors would like to thank Vele Lab Mostar and Ante Ćurlin for assistance in this study. The study was supported by the Federal Ministry of Education and Science of Bosnia and Herzegovina.
References
- 1.Kilańska K, Gaworska-Krzemińska A, Karolczak A, Szynkiewicz P, Greber M. Work patterns and a tendency among Polish nurses to leave their job. Med Pr. 2019;70(2):145–53. 10.13075/mp.5893.00727 [DOI] [PubMed] [Google Scholar]
- 2.Simon M, Müller BH, Hasselhorn HM. Leaving the organization or the profession – a multilevel analysis of nurses’ intentions. J Adv Nurs. 2010;66(3):616–26. 10.1111/j.1365-2648.2009.05204.x [DOI] [PubMed] [Google Scholar]
- 3.Ball J, Day T, Murrell S, Dall’Ora C, Rafferty AM, Griffiths P, et al. Cross-sectional examination of the association between shift length and hospital nurses’ job satisfaction and nurse reported quality measures. BMC Nurs. 2017;16(26): 10.1186/s12912-017-0221-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galatsch M, Li J, Derycke H, Müller BH, Hasselhorn HM. Effects of requested, forced and denied shift schedule change on work ability and health of nurses in Europe – results from the European NEXT Study. BMC Public Health. 2013;13:1137. 10.1186/1471-2458-13-1137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benceković Ž, Benko I, Režek B, Grgas-Bile C. The role and promotion of nursing. Acta Clin Croat. 2016;55(2):271–8. Available from https://hrcak.srce.hr/index.php?show=clanak&id_clanak_jezik=243091 [Internet] 10.20471/acc.2016.55.02.14 [DOI] [PubMed] [Google Scholar]
- 6.Griffiths P, Dall’Ora C, Simon M, Ball J, Lindqvist R, Rafferty A-M, et al. Nurses’ shift length and overtime working in 12 European countries. Med Care. 2014;52(11):975–81. 10.1097/MLR.0000000000000233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Estryn-Béhar M, van der Heijden BIJM, NEXT Study Group . Effects of extended work shifts on employee fatigue, health, satisfaction, work/family balance, and patient safety. Work. 2012;41 Suppl 1:4283–90. 10.3233/WOR-2012-0724-4283 [DOI] [PubMed] [Google Scholar]
- 8.Bajraktarov S, Novotni A, Manusheva N, Nikovska DG, Miceva-Velickovska E, Zdraveska N, et al. Main effects of sleep disorders related to shift work – opportunities for preventive programs. EPMA J. 2011;2(4):365–70. 10.1007/s13167-011-0128-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parsons MJ, Moffitt TE, Gregory AM, Goldman-Mellor S, Nolan PM, Poulton R, et al. Social jetlag, obesity and metabolic disorder: investigation in a cohort study. Int J Obes (Lond). 2015;39(5):842–8. 10.1038/ijo.2014.201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Behrens T, Rabstein S, Wichert K, Erbel R, Eisele L, Arendt M, et al. Shift work and the incidence of prostate cancer: a 10-year follow-up of a German population-based cohort study. Scand J Work Environ Health. 2017;43(6):560–8. 10.5271/sjweh.3666 [DOI] [PubMed] [Google Scholar]
- 11.Vetter C, Dashti HS, Lane JM, Anderson SG, Schernhammer ES, Rutter MK, et al. Night shift work, genetic risk, and type 2 diabetes in the UK Biobank. Diabetes Care. 2018;41(4):762–9. 10.2337/dc17-1933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Juda M, Vetter C, Roenneberg T. Chronotype modulates sleep duration, sleep quality, and social jet lag in shift-workers. J Biol Rhythms. 2013;28(2):141–51. 10.1177/0748730412475042 [DOI] [PubMed] [Google Scholar]
- 13.Dall’Ora C, Griffiths P, Ball J, Simon M, Aiken LH. Association of 12 h shifts and nurses’ job satisfaction, burnout and intention to leave: findings from a cross-sectional study of 12 European countries. BMJ Open. 2015;5(9):e008331. 10.1136/bmjopen-2015-008331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sonati J, de Martino M, Vilarta R, Maciel É, Moreira E, Sanchez F, et al. Quality of life, health, and sleep of air traffic controllers with different shift systems. Aerosp Med Hum Perform. 2015;86(10):895–900. 10.3357/AMHP.4325.2015 [DOI] [PubMed] [Google Scholar]
- 15.Touitou Y, Reinberg A, Touitou D. Association between light at night, melatonin secretion, sleep deprivation, and the internal clock: health impacts and mechanisms of circadian disruption. Life Sci. 2017;173:94–106. 10.1016/j.lfs.2017.02.008 [DOI] [PubMed] [Google Scholar]
- 16.Costa G. Shift work and health: current problems and preventive actions. Saf Health Work. 2010;1(2):112–23. 10.5491/SHAW.2010.1.2.112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.van Bogaert P, Peremans L, van Heusden D, Verspuy M, Kureckova V, van de Cruys Z, et al. Predictors of burnout, work engagement and nurse reported job outcomes and quality of care: a mixed method study. BMC Nurs. 2017;16(5): 10.1186/s12912-016-0200-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Papantoniou K, Devore EE, Massa J, Strohmaier S, Vetter C, Yang L, et al. Rotating night shift work and colorectal cancer risk in the nurses’ health studies. Int J Cancer. 2018;143(11):2709–17. 10.1002/ijc.31655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tadinac M, Sekulić A, Hromatko I, Mazul-Sunko B, Ivančić R. Age and individual sleep characteristics affect cognitive performance in anesthesiology residents after a 24-hour shift. Acta Clin Croat [Internet]. 2014;53.(1.):22-30. Available from: https://hrcak.srce.hr/126143 [PubMed]
- 20.Trošt Bobić T, Šečić A, Zavoreo I, Matijević V, Filipović B, Kolak Ž, et al. The impact of sleep deprivation on the brain. Acta Clin Croat. 2016;55(3):469–73. Available from https://hrcak.srce.hr/index.php?show=clanak&id_clanak_jezik=254705 [Internet] 10.20471/acc.2016.55.03.17 [DOI] [PubMed] [Google Scholar]
- 21.Engert V, Efanov SI, Duchesne A, Vogel S, Corbo V, Pruessner JC. Differentiating anticipatory from reactive cortisol responses to psychosocial stress. Psychoneuroendocrinology. 2013;38(8):1328–37. 10.1016/j.psyneuen.2012.11.018 [DOI] [PubMed] [Google Scholar]
- 22.Marković VM, Čupić Ž, Vukojević V, Kolar-Anić L. Predictive modeling of the hypothalamic-pituitary-adrenal (HPA) axis response to acute and chronic stress. Endocr J. 2011;58(10):889–904. 10.1507/endocrj.EJ11-0037 [DOI] [PubMed] [Google Scholar]
- 23.Powell DJ, Schlotz W. Daily life stress and the cortisol awakening response: testing the anticipation hypothesis. PLoS One. 2012;7(12):e52067. 10.1371/journal.pone.0052067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bostock S, Steptoe A. Influences of early shift work on the diurnal cortisol rhythm, mood and sleep: within-subject variation in male airline pilots. Psychoneuroendocrinology. 2013;38(4):533–41. 10.1016/j.psyneuen.2012.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kantermann T, Wehrens SMT, Ulhôa MA, Moreno C, Skene DJ. Noisy and individual, but doable: shift-work research in humans. Prog Brain Res. 2012;199:399–411. 10.1016/B978-0-444-59427-3.00022-8 [DOI] [PubMed] [Google Scholar]
- 26.Gamst G, Meyers LS, Guarino AJ. Analysis of variance designs: a conceptual and computational approach with SPSS and SAS. 1st edition. Cambridge, New York: Cambridge University Press, 2008; p. 594. [Google Scholar]
- 27.Matijaca H, Gaćina P, Rinčić G, Matijaca A, Josipović J, Stojsavljević S. Effects of occupational stress on the activation of hemostatic and inflammatory system. Acta Clin Croat. 2019;58(2):281–7. Available from https://hrcak.srce.hr/index.php?show=clanak&id_clanak_jezik=327303 [Internet] 10.20471/acc.2019.58.02.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schmidt RE, Cullati S, Mostofsky E, Haller G, Agoritsas T, Mittleman MA, et al. Healthcare-related regret among nurses and physicians is associated with self-rated insomnia severity: a cross-sectional study. PLoS One. 2015;10(10): available from https://www.ncbi.nlm.nih.gov/pmc/articles/pmc4598038/ [Internet] 10.1371/journal.pone.0139770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jehan S, Zizi F, Pandi-Perumal SR, Myers AK, Auguste E, Jean-Louis G, et al. Shift work and sleep: medical implications and management. Sleep Med Disord. 2017;1(2): Available from https://www.ncbi.nlm.nih.gov/pmc/articles/pmc5836745/ [Internet] [PMC free article] [PubMed] [Google Scholar]
- 30.Burgess PA. Optimal shift duration and sequence: recommended approach for short-term emergency response activations for public health and emergency management. Am J Public Health. 2007. April;97 Suppl 1:S88–92. Available from http://ajph.aphapublications.org/doi/10.2105/ajph.2005.078782 [Internet] 10.2105/AJPH.2005.078782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vitale SA, Varrone-Ganesh J, Vu M. Nurses working the night shift: impact on home, family and social life. J Nurs Educ Pract. 2015;5(10):70–8. 10.5430/jnep.v5n10p70 [DOI] [Google Scholar]
- 32.Zamanian Z, Nikeghbal K, Khajehnasiri F. Influence of sleep on quality of life among hospital nurses. Electron Physician. 2016;8(1):1811–6. 10.19082/1811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dong H, Zhang Q, Sun Z, Sang F, Xu Y. Sleep disturbances among Chinese clinical nurses in general hospitals and its influencing factors. BMC Psychiatry. 2017;17(1): Available from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5496307/ [Internet] 10.1186/s12888-017-1402-3 [DOI] [PMC free article] [PubMed] [Google Scholar]