Abstract
Diffuse uterine leiomyomatosis is a rare and benign condition which involves the development of innumerable poorly defined, confluent smooth muscle nodules that replace most of the uterine parenchyma. It results in a symmetrically enlarged uterus. The etiology of these benign tumors is not completely understood. Patients with leiomyomatosis usually present with menorrhagia or dysmenorrhea, abdominal pain and infertility and in most cases hormonal treatment fails to control the symptoms. In this manuscript, we present a case of a 36-year-old woman who underwent hysterectomy due to diffuse uterine leiomyomatosis with a review of the literature.
Keywords: Leiomyomatosis, MRI, Fibroids, Uterine mass
Introduction
Leiomyomas are the most common benign uterine neoplasm [1] and usually present as circumscribed masses with characteristic imaging features [1,2]. However, unusual patterns of leiomyomas growth are described in the literature, including diffuse leiomyomatosis [3]. In this rare entity, the myometrium is symmetrically expanded by innumerable small and confluent leiomyomas [1].
This case report illustrates the radiologic findings and histopathologic features of diffuse uterine leiomyomatosis.
Case report
A 36-year-old woman presented with a 1-year history of lower abdominal discomfort and dysmenorrhea. The patient's obstetrical history included 1 pregnancy 10 years before that resulted in the delivery of 1 healthy full- term infant. The patient had no significant gynecological, medical or family history. Physical examination showed an enlarged uterus extending above the umbilicus with no other abdominal or pelvic pathologic findings. The patient underwent abdominal and pelvic Magnetic Resonance Imaging (MRI) to further characterize these findings, which revealed a markedly enlarged uterus replaced by innumerable nodules that blend with one another. These nodules exhibit predominantly low to intermediate signal intensity on T2-weighted images relative to normal myometrium (Fig. 1). No apparent cystic changes were appreciated and the nodules demonstrated relatively homogeneous enhancement on the post-gadolinium sequences (Fig. 2). Both ovaries had normal appearance.
Fig. 1.
MRI T2-weighted findings. Sagittal (A) and coronal (B) T2-weighted image show an enlarged uterus with innumerable and poorly circumscribed nodules that replace the normal uterine parenchyma. The endometrium was significantly elongated but its canal appears preserved (*).
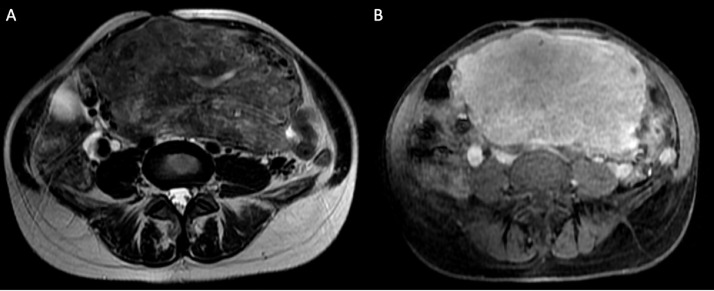
Fig. 2.
MRI axial plane of the uterus. T2-weighted image (A) demonstrates that myometrium is symmetrically expanded by confluent and indistinct leiomyomas. Post-gadolinium fat-suppressed T1-weighted image (B) shows homogeneous enhancement of the uterine nodules.
A total abdominal hysterectomy was performed without major complications. The hysterectomy specimen consisted of a 1945-gram uterus; the uterus and cervix measured together 16.5cm. The cervix and endometrium were normal. Microscopic analysis revealed various smooth-muscle nodules of different shape and size replacing the entire myometrium (Fig. 3). The nodules were confluent with low mitotic count. No atypia or tumor cell necrosis were seen.
Fig. 3.
Microscopic examination of the uterus. Uncountable leiomyomas were found scattered in the myometrium (A). In this view (HE, low power) 6 nodules are identified (*). B) The tumor nodules are composed of spindle cells growing in a fascicular pattern (HE, high power). The neoplastic cells have eosinophilic cytoplasm and cigar-shaped nuclei.
Discussion
Diffuse uterine leiomyomatosis is a quite rare entity characterized by multiple [1,2], poorly defined and usually small-sized leiomyomas (all having a diameter that frequently ranges from a few millimeters and 3 cm) involving all the myometrium leading to a symmetrically enlarged uterus [4]. It frequently affects women between the third and fourth decades of life with a typically clinical course characterized by menorrhagia and infertility [4,5]. There are no specific risk factors reported in the literature associated with this disease [5]. Microscopic examination shows that these uterine nodules are essentially constituted of benign cellular smooth muscle [2].
Regarding imaging techniques, ultrasonography is the first line imaging modality to assess pelvic cavity and uterine or ovarian disorders [6]. However, MRI, due to its multiplanar imaging capabilities and excellent soft-tissue contrast, is frequently the optimal imaging modality to assess female pelvis [7,8]. Furthermore, MRI has also an important role in complementary pre-treatment mapping, including the evaluation of its number, size and their location within the layers of the uterus and in differential diagnostic issues [8]. While typical leiomyomas are well circumscribed masses with an asymmetrical involvement of the uterus, most of those associated with diffuse leiomyomatosis have indistinct borders and coalesce together [1,7]. Leiomyomas usually demonstrate low to intermediate signal intensity on T2-weighted images relative to normal myometrium which can be difficult to appreciate in leiomyomatosis since majority of myometrium is substituted by the smooth-muscle nodules. Contrast-enhanced sequences show variable enhancement of the uterine masses [1,7,8].
Historically, the standard treatment of choice for diffuse leiomyomatosis has been hysterectomy as hormonal treatment frequently fails to control the symptoms. However, as the majority of patients with this disease are of reproductive age, hysterectomy represents a difficult choice unlikely to be easily accepted by young women who wish to have a future pregnancy. Other treatment options have to be evaluated with the aim of preserving fertility and the uterus [9]. Literature reports successful pregnancies in woman who were treated with gonadotropin-releasing hormone agonists or minimally invasive hysteroscopic myomectomy with removing of submucosal leiomyomas [9,10]. Another conservative treatment option with reported promising results is uterine artery embolization (UAE). In fact, symptomatic fibroids are currently treated with increasing frequency with UAE and this technique is gaining acceptance worldwide as an effective alternative to hysterectomy or myomectomy. Therefore, it should be considered as a treatment option for women of reproductive age with diffuse leiomyomatosis [10].
In conclusion, MRI can establish with a high degree of confidence the definitive diagnosis of diffuse leiomyomatosis which might allow the patient management by a multidisciplinary team for therapeutic decision-making process depending on patient desire for fertility. Therefore, it is important that radiologists are aware of this benign disease and its imaging appearances.
Footnotes
Competing Interest: The authors have declared that no competing interests exist.
Patient Consent: The corresponding author confirm that written, informed consent was obtained from the patient.
References
- 1.Kido A, Togashi K, Koyama T, Yamaoka T, Fujiwara T, Fujii S. Diffusely enlarged uterus: evaluation with MR imaging. Radiographics. 2003;23(6):1423–1439. doi: 10.1148/rg.236035033. [DOI] [PubMed] [Google Scholar]
- 2.Ueda H, Togashi K, Konishi I, Kataoka ML, Koyama T, Fujiwara T, et al. Unusual appearances of uterine leiomyomas: MR imaging findings and their histopathologic backgrounds. Radiographics. 1999;19 doi: 10.1148/radiographics.19.suppl_1.g99oc04s131. Spec No:S131-45. [DOI] [PubMed] [Google Scholar]
- 3.Coskun A, Ozdemir O, Vardar MA, Kiran G, Arikan D, Ersoz C. A case with diffuse uterine leiomyomatosis and review of the literature. Clin Exp Obstet Gynecol. 2008;35(3):227–230. [PubMed] [Google Scholar]
- 4.Otsubo Y, Nishida M, Arai Y, Ichikawa R, Sakanaka M. Diffuse uterine leiomyomatosis in patient with successful pregnancy following new surgical management. Arch Gynecol Obstet. 2014;290(4):815–818. doi: 10.1007/s00404-014-3309-2. [DOI] [PubMed] [Google Scholar]
- 5.Baschinsky DY, Isa A, Niemann TH, Prior TW, Lucas JG, Frankel WL. Diffuse leiomyomatosis of the uterus: a case report with clonality analysis. Hum Pathol. Nov 2000;31(11):1429–1432. [PubMed] [Google Scholar]
- 6.Pai D, Coletti MC, Elkins M, Ladino-Torres M, Caoili E. Diffuse uterine leiomyomatosis in a child. Pediatr Radiol. 2012;42(1):124–128. doi: 10.1007/s00247-011-2114-3. Epub 2011 Jun 28. [DOI] [PubMed] [Google Scholar]
- 7.Kubik-Huch RA, Weston M, Nougaret S, Leonhardt H, Thomassin-Naggara I, Horta M, et al. European society of urogenital radiology (ESUR) guidelines: MR imaging of leiomyomas. Eur Radiol. 2018;28(8):3125–3137. doi: 10.1007/s00330-017-5157-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nougaret S, Cunha TM, Benadla N, Neron M, Robbins JB. Benign uterine disease: the added role of imaging. Obstet Gynecol Clin North Am. 2021;48(1):193–214. doi: 10.1016/j.ogc.2020.12.002. [DOI] [PubMed] [Google Scholar]
- 9.Kido A, Monma C, Togashi K, Ueda H, Itoh K, Fujii S, Konishi J. Uterine arterial embolization for the treatment of diffuse leiomyomatosis. J Vasc Interv Radiol. 2003;14(5):643–647. doi: 10.1097/01.rvi.0000071095.76348.e0. [DOI] [PubMed] [Google Scholar]
- 10.Koh J, Kim MD, Jung DC, Lee M, Lee MS, Won JY, et al. Uterine artery embolization (UAE) for diffuse leiomyomatosis of the uterus: clinical and imaging results. Eur J Radiol. 2012;81(10):2726–2729. doi: 10.1016/j.ejrad.2011.11.010. [DOI] [PubMed] [Google Scholar]