A 47 white old man living in Calabria (southern Italy), was admitted to our hospital for a six-month history of weight loss and painful dysphagia. Eighteen months earlier he had an episode of high grade fever, and subsequently had been diagnosed in another Institution with Wilson disease because of hepatosplenomegaly, mild pancytopenia, slight increase of cupremia in one measurement, a report of an evanescent kayser-Fleischer ring, and no alternative diagnoses arising from viral serology and bone marrow and liver biopsies.
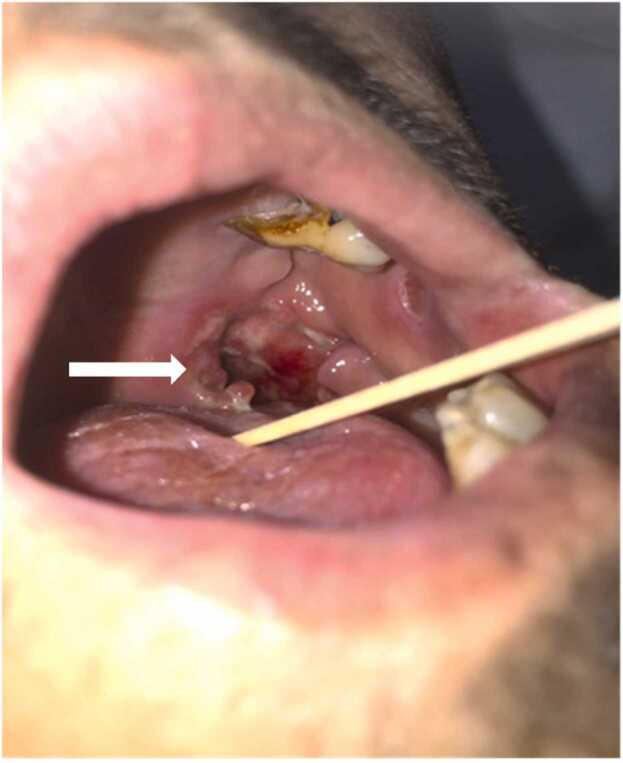
The physical examination of the patient showed liver and spleen enlargement and a large ulceration with irregular borders of the left tonsil and soft palate (Fig. 1).
Fig. 1.
Mucosal leishmaniasis: ulceration of the soft palate with detachment of the left anterior tonsil pillar (arrow).
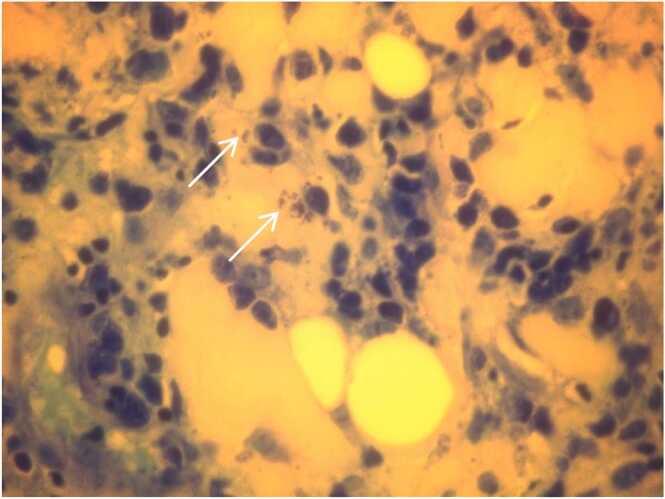
Neurological examination was normal. Laboratory data showed a severe pancytopenia (hemoglobin 7.1 g/dl, normal values 13–17; platelets 29.000/mm3, normal values 150.000–450.000; Leukocytes 1.100/mm3, normal values 4.000–11.000) and low levels of serum albumin (1.9 g/dl, normal values 3.5–5.5). Ceruloplasmin was normal (26 mg/dl, normal range 20–63) while cupremia was low (25 mcg/dl, normal range 81–156). No Kayser-Fleischer ring was detected on ocular examination. In the suspicion of a carcinoma, a biopsy of the oral ulceration was performed. Meanwhile, considering not proven the previous diagnosis of Wilson disease, we sought for alternative diagnoses. Serum antibodies anti-leishmania were positive, as well as leishmania DNA testing with the polymerase chain reaction in peripheral blood and in the bone marrow biopsy. The histological examination of the oral biopsy showed an inflammatory infiltrate with histiocytes containing intracytoplasmic bodies suggestive of Leishmania spp. Amastigotes (Fig. 2).
Fig. 2.
Histology of oral biopsy. Inflammatory infiltrate of histiocytes with Leishmania bodies (arrows). May Grunwald Giemsa stain, × 400.
Treatment with intravenous liposomal amphotericin b was started, and the conditions of the patient progressively improved.
Leishmaniasis is a vector-borne systemic disease that can occur as cutaneous, mucosal or visceral form [1]. Visceral leishmaniasis is fatal if left untreated [2]. Its zoonotic form, caused by Leishmania infantum, occurs in the Mediterranean basin, China, the Middle East and South America, and has dogs as the main reservoir. Typical manifestations include chronic fever, weight loss, hepatosplenomegaly, and pancytopenia on blood examination [2]. Very rarely visceral and mucosal leishmaniasis coexist [1].
The rarity of visceral and mucosal leishmaniasis in Europe makes their diagnosis difficult and frequently delayed, and their presentation often mistaken for another disease [1], [3]. In our patient the diagnosis was postponed in particular because no parasites were seen on the first bone marrow biopsy. However, sensitivity of this exam is time dependent, ranging from 55% to 90% [4].
Ethical approval
This case report has obtained approval from the head of the Internal Medicine unit at the Department of Internal Medicine of the Azienda Ospedaliera di Cosenza (Italy).
Ethics approval and informed consent
This case report has obtained approval from the head of the Internal Medicine unit at the Department of Internal Medicine of the Azienda Ospedaliera di Cosenza (Italy).
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Funding
This case report has been undertaken by the authors without any form of sponsorship or support from any individual or institution.
CRediT authorship contribution statement
Carlo Bova, Andrea de Vuono, Martina Ruvio, Francesca Serena Pignataro and Elio Fiaschi: Conception and design of the study. Carlo Bova: draft of the manuscript. Andrea de Vuono, Martina Ruvio, Francesca Serena Pignataro and Elio Fiaschi: Review of the manuscript for important intellectual content.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Conflict of Interest
Each author declares that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article.
Contributor Information
Carlo Bova, Email: carbova@libero.it.
Andrea de Vuono, Email: a.devuono@aocs.it.
Martina Ruvio, Email: m.ruvio@aocs.it.
Francesca Serena Pignataro, Email: f.pignataro@aocs.it.
Elio Fiaschi, Email: e.fiaschi@aocs.it.
References
- 1.Darcis G., Van der Auwera G., Giot J.B., Hayette M.P., Tassin F., Arrese Estrada J., et al. Recurrence of visceral and muco-cutaneous leishmaniasis in a patient under immunosuppressive therapy. BMC Infect Dis. 2017;17(1):478. doi: 10.1186/s12879-017-2571-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van Griensven J., Diro E. Visceral leishmaniasis: recent advances in diagnostics and treatment regimens. Infect Dis Clin N Am. 2019;33(1):79–99. doi: 10.1016/j.idc.2018.10.005. [DOI] [PubMed] [Google Scholar]
- 3.Chong G.M., Ong D.S.Y., de Mendonça Melo M., van Hellemond J.J. Painful and swollen tongue: mucosal leishmaniasis due to Leishmania infantum. Int J Infect Dis. 2021;113:109–112. doi: 10.1016/j.ijid.2021.09.071. Epub 2021 Sep 29. [DOI] [PubMed] [Google Scholar]
- 4.Dhariwal A., Jawad S., Bicanic T. Case report: visceral leishmaniasis falsely diagnosed as Q fever. Am J Trop Med Hyg. 2020;103(5):1927–1929. doi: 10.4269/ajtmh.19-0731. [DOI] [PMC free article] [PubMed] [Google Scholar]