Abstract
Background and Aim
Providing gender‐sensitive health services is emphasized by the World Health Organization. This study aimed to assess and prioritize the needs for the gender‐sensitive sexually transmitted infections/human immunodeficiency viruses (STIs/HIV) prevention services by a valid and reliable questionnaire.
Methods
This was an exploratory mixed methods sequential study in Shiraz Iran 2019. The first phase was a qualitative study on 37 providers and managers of the services who were recruited using the purposive and then snowball sampling method. In the second phase, following the content analysis of the qualitative data and a review of related literature, a questionnaire was developed and its psychometric properties were evaluated. Then, in the third phase, the questionnaire was used to assess and prioritize the needs through a quantitative descriptive cross‐sectional study on all 290 providers of STI/HIV prevention services affiliated with Shiraz University of Medical Sciences.
Results
The finding of the qualitative phase showed gender‐sensitive STI/HIV prevention services should provide gender‐sensitive care and education by the trained personnel and manages with appropriate facilities and equipment. Providing these services also requires supportive policies, intersectoral cooperation, and community capacitation. In the second phase, a questionnaire was developed with 63 items. Assessment of psychometric properties of the questionnaire demonstrated the scale content validity index and ratio (S‐CVI = 0.98 and S‐CVR = 0.87, respectively), as well as the reliability of the questionnaire (internal consistency = 0.972 and intracluster correlation coefficient = 0.910). Results of the third descriptive phase of the study demonstrated the highest priorities for gender‐sensitive education (92.01 ± 11.76%) and care services (92.11 ± 12.04%), respectively.
Conclusions
To improve the quality of the services, a gender‐based education and care process, as well as a gender‐sensitive structure, including gender‐sensitive personnel, facilities, and management are necessary. Recognizing and meeting the needs for gender‐sensitive services will improve the quality of the services.
Keywords: gender, health service assessment, reproductive health services, STIs/HIV prevention
1. INTRODUCTION
Gender norms and roles can influence individuals' mental, physical, social health, and well‐being. 1 Gender norms can impact women's and men's health through different health‐related behaviors and access to care. 2 There is a growing trend of documents showing that gender norms and behaviors are effective on the pattern of spreading sexually transmitted infections/human immunodeficiency virus (STIs/HIV) among men and women. 3 Studies show a higher frequency of STIs and HIV and more vulnerability of women comparing to men. 4 A review on 130 studies during 2009–2016 reports on the prevalence of STIs, including chlamydia, gonorrhea, trichomoniasis, and syphilis showed the prevalence of 3.8%, 0.9%, 5.3%, and 0.5% in women, respectively; and the prevalence of 2.7%, 0.7%, 0.6%, and 0.5% among men, correspondingly. 5
Restricted gender norms and the low social status of women make them vulnerable to STIs/HIV. This problem may arise due to their very low authority for decision‐making in sexual relationships. 6 Sometimes, women hide STIs as they concern to lose their partner, or they do not seek ways to protect themselves in the event of a partner's STIs infection. 7 Also, male gender roles may predispose them to STIs. Early initiation of sexual relationships and having multiple sex partners increase male risk of STIs. 8 , 9 Furthermore, men would not usually seek counseling and treatment services for STIs/HIV and acquired immunodeficiency syndrome (AIDS) because of a myth that “seeking care is a sign of weakness” and it is not masculine behavior in their gender norms. 5 , 10 Therefore, providing gender‐based counseling and care services seems to be necessary for STIs/HIV care services.
Gender is a fundamental factor that shapes health systems and outcomes. 11 Gender norms are among the most important effective factors on STIs/HIV incidence and care services. 12 Hence recognizing the behaviors arising from gender norms affecting STIs/HIV prevention behaviors and services seems to be necessary.
Nowadays, providing gender‐sensitive health services is emphasized by the World Health Organization. 13 , 14 Gender‐sensitive health services mean that health authorities have the knowledge and are able to perceive existing gender differences and to integrate these into their decision‐making and actions. 15 Therefore, gender‐based special needs in any community and culture should be known and considered in providing STIs/HIV prevention services. 16 The needs assessment requires a valid and reliable tool. Therefore, developing valid and reliable questionnaires to assess the real needs for providing gender‐sensitive services helps health care managers to improve the quality of the services. 17 To our knowledge either there are limited studies to assess needs for gender‐based reproductive health services 17 , 18 or no tool to assess needs for providing STIs/HIV prevention services.
There are very few studies on the gender‐based special needs for STI/HIV prevention services. Lichtenstein et al. 19 showed men's concern about stigmatization as the main barrier for seeking STI prevention and treatment services. Garcia et al. 20 stated that stigma causes many people to avoid seeking STI‐related services because of experiences, such as discrimination, indifference, and overt hostility in the health care setting. They mentioned to a world‐wide barrier to a full range of reproductive health services such as restricted access to STI testing, criminalization of sexual behaviors associated with STI transmission, for example, commercial sex work or same‐sex sexual relationships. A study in Nigeria demonstrated that a greater proportion of males than of females had sought treatment for their STIs (64% vs. 48%). Females had lower odds than males of having sought STI treatment (odds ratio: 0.6). 21 Rahmanian et al. 22 in Iran used a valid and reliable questionnaire to assess the needs of gender‐sensitive adolescents reproductive health services (ANQ‐GSARHS), indicating the priorities for providing gender‐sensitive services for adolescents, such as providing contraceptives for female adolescents, educating female adolescents about STIs, counseling male adolescents about confronting with peer pressure, employment of trained male providers for male adolescents' reproductive health services, and improving knowledge of providers about adolescents' reproductive health. However, to our knowledge, there is no study to understand the gender‐based needs of STIs/HIV prevention services. Besides, very few tools are available to assess gender sensitivity in STIa services, 23 male participation in perinatal care services, 24 and reproductive health services. 25 The most comprehensive questionnaire to assess gender sensitivity in reproductive health services is available at the level of staff and facilities. 26
Therefore, considering the daily incidence of more than 1 million (STIs) cases worldwide 27 ; 26.4 million cases of four curable STIs (Chlamydia trachomatis, Neisseria gonorrhoeae, syphilis, and Trichomonas vaginalis) in the Eastern Mediterranean region 28 ; and respecting to 59,531 estimated number of people with HIV in Iran in 2021 29 and also growing spread of STIs and HIV in Iran, 30 as well as the importance of gender‐specific needs assessment in STIs/HIV health services with a valid and reliable tool, this exploratory mixed sequential study aimed to assess and prioritize the needs of gender‐sensitive STIs/HIV prevention services, by a valid and reliable questionnaire.
2. METHODS
2.1. Design of the study
This was a mixed‐method exploratory sequential qualitative–quantitative study. The exploratory sequential study is used when the researcher is interested in following up qualitative findings with quantitative analysis. This two‐phase approach is particularly useful for a researcher interested in developing a new instrument or treatment protocol. 31 Therefore, the first phase of the present study was a qualitative study to produce codes and themes. These codes were used for the concept definition and item generation of the questionnaire. In the second phase, the questionnaire's psychometric properties were assessed. Thereafter, in the third phase, the questionnaire was used for a descriptive cross‐sectional study to assess and prioritize the needs for gender‐sensitive STIs/HIV prevention services. 31 Therefore, the method section is presented in these three abovementioned phases, (1) qualitative phase, (2) tool development phase, and (3) quantitative phase.
2.2. Phase 1: The qualitative phase of the study
2.2.1. Design
This phase of the study was a qualitative study with a content analysis approach. The codes extracted from the qualitative phase were used for item generation for the questionnaire. For developing the questionnaire, the steps described by Waltz et al. 32 were used. Respecting the first step for the questionnaire development, the qualitative phase was performed to explain needs for gender‐sensitive STIs/HIV prevention services and the extracted codes were used for the items generation.
2.2.2. Study settings
The research interviews were conducted in primary health care centers, voluntary counseling and testing services, and hospitals affiliated with Shiraz University of Medical Sciences (SUMS), as well as the relevant STIs/HIV prevention headquarters in Shiraz, and the Ministry of Health in Tehran in Iran. The participants were all interviewed in their workplace
2.2.3. Participants
Participants were STIs/HIV care providers and managers or policymakers.
2.2.4. Eligibility criteria
The inclusion criteria for participation were at least 2 years of working experience as a provider, manager, or policymaker of STIs/HIV prevention services.
2.2.5. Sampling method
The participants were selected using the purposive and snowball sampling method. Recruitment continued until data saturation was reached.
2.2.6. Outcome measures
Explaining the need for gender‐sensitive STII/HIV prevention services.
2.2.7. Tool for data collection
Data were collected using in‐depth interviews using a semi‐structured questionnaire. The guide questions for the interview were: “How do you perceive the concept of gender‐sensitive STIs/HIV prevention services”; “what is your perception about the gender roles that may affect sexual health”; and “what is necessary for a gender‐sensitive STIs/HIV services?” and “how these services could be provided?” A demographic questionnaire was also used for data collection.
2.2.8. Study procedure
Data were collected using a deep face‐to‐face individual interview by using the semi‐structured interviews and continued until data saturation; that is, when no new code of data was added to the study. The interviews were conducted by the second author Dr. Rahmanian, who is an assistant professor in the Department of Midwifery and Reproductive Health at SUMS. After being introduced to the interviewer, the participants were informed about the goals of the study and promised the confidentiality of their personal information. Also, field notes were made during and after the interview. The interviews were performed after two pilot interviews. The average duration of interviews was about 60–90 min. All interviews were audiotaped, transcribed verbatim, and analyzed consecutively.
2.2.9. Data rigor and trustworthiness
To assess the trustworthiness of data, four criteria of Lincoln and Guba's 33 were used, including credibility, dependability, confirmability, and transferability. To increase credibility, adequate time was allocated to data collection and frequent reviewing of the data. In addition, integration of data collection methods, that is, individual interviews and observations increased the credibility of the data. The participants (the service providers) were observed at the STIs/HIV prevention services and field notes were taken. Field notes are a qualitative approach, most often used in ethnography. Field notes are written observations recorded during or immediately following participant observations in the field and are considered critical to understanding phenomena encountered in the field. 34
Some codes extracted from interviews were reviewed by four participants, including two managers and also two service providers, who had not participated in the study to ensure that the results accurately depicted the participants' experiences and perceptions. To confirm the dependability of the data, code‐recode and external checking were used. To assess the confirmability of the data, the researchers abandoned all their assumptions and thoughts and carefully documented all the research steps, and allowed external auditors to investigate all the steps. To ensure transferability and comprehensiveness, a clear explanation of the methods of collecting and analyzing the data was presented along with examples of the statements made by the participants.
2.2.10. Data analysis
The data were analyzed by using MAXQUDA10 and a conventional content analysis based on the criteria proposed by Graneheim and Lundman. 35 After transcribing, the recorded interviews, the transcripts were carefully reviewed by the researcher two to three times to achieve an accurate understanding of the interview contents. The text was divided into meaning units, meaning units were condensed while preserving the meaning and labeled with codes. Similar codes were then categorized into subcategories, and the subcategories were classified into a category based on common properties. The latent content of the similar categories was eventually formulated as a theme.
2.2.11. Ethical considerations
Before conducting the interviews, the researcher briefed the participants on the objectives of the study and assured them that their responses will be confidential. Informed written and verbal consent was also obtained from the participants for participating in the study and recording the interviews.
2.3. Phase 2: The questionnaire development and assessment of the psychometric properties
The method of this phase of the study is described in two parts: (1) the questionnaire development and (2) the assessment of psychometric properties of the questionnaire.
2.3.1. The questionnaire development
2.3.1.1.
Design: To develop the questionnaire the deductive‐inductive approach was conducted. In other words, the items were generated from the extracted codes from the qualitative, and then were completed by the extracted items from the literature review. Also, Waltz et al.'s 32 four steps of a questionnaire development were used.
The qualitative phase was performed using the conventional content analysis method to explain the concept and dimensions of gender‐sensitive STI/HIV prevention services. The primary pool of items and subscales of the questionnaire were respectively generated from codes and categories extracted from the data analysis of the qualitative phase. A few items were also added to the pool after a literature review.
2.3.1.2.
The literature review: To ensure that the items and construct definition aligns with relevant prior research and to identify existing survey scales or items that might be used, an extensive literature review was conducted.
2.3.1.3.
Search strategy: The preferred reporting items for systematic reviews 36 was used to identify and articulate the needs for the STIs/HIV services. We used appropriate operators, such as AND and OR, and a combination of search strategies for each database. We conducted a comprehensive search using the keywords “STI,” “HIV,” “AIDS,” “prevention,” “Care,” “Service,” “Gender,” and “questionnaire” in Scopus, PubMed, Science Direct, Google Scholar, SID, World Health Organization, International Confederation of Planned Parenthood, United Nation Population fund websites, and Magiran databases.
2.3.1.4.
Eligibility criteria: The inclusion criteria were Persian or English sources, the articles published between 1990 and 2019 in the abovementioned databases.
Some appropriate items were recognized in the review and added to the primary pool of items. In this way, the initial questionnaire was prepared for evaluating the psychometric properties.
2.3.2. Psychometric properties of the questionnaire
The questionnaire was assessed regarding its validity and reliability as below:
2.3.2.1.
Validity of the questionnaire: Face validity and content validity as the theoretical and representational validity of the questionnaire was evaluated by qualitative and quantitative methods. The validity of a questionnaire can be established using a panel of experts that explore theoretical constructs. This form of validity exploits how well the idea of a theoretical construct is represented in an operational measure. This is called translational or representational validity. 37
2.3.2.2.
Face validity: For qualitative face validity assessment, 15 providers of STIs/HIV prevention services were asked about the items' difficulty, irrelevancy, and ambiguity. 32 Next, for quantitative face validity assessment, they were asked to specify the importance of the items on a 5‐point scale. Then the impact scores were calculated using the following formula: “impact score = importance × frequency.” Afterward, the impact score of each item was calculated and evaluated by the cut‐off point of >1.5. 38 , 39 So, the items with the impact score ≥1.5 was considered appropriate.
2.3.2.3.
Content validity: For qualitative content validity assessment, 10 experts in reproductive health, midwifery, and nursing were asked to provide feedback on the questionnaire regarding grammar, appropriate word use, and appropriate placement of phrases. Then, for quantitative content validity assessment, the content validity ratio (CVR) and content validity index (CVI) were measured. 40
2.3.2.4.
Content validity ratio: To ensure the selection of the most important items, CVR was calculated for each item. The experts signified their opinions by assigning each item scores of 1–3, which correspond to “not necessary,” “useful but not essential,” and “essential,” respectively. The scores were then calculated using the following formula: CVR = (Ne – N/2)/(N/2), where Ne is the number of experts indicating an item as “essential” and N is the total number of experts. The accepted value was determined based on Lawshe's table and the number of experts. 41 The opinions of the 10 experts were referred to in evaluating the CVR with 0.62 regarded as acceptable. 41
2.3.2.5.
Content validity index: This index was calculated based on Waltz and Bausell's 40 criteria to ensure that the items of the questionnaire are appropriately designed to measure content. The expert evaluation was focused on relevance, clarity, and simplicity and was expressed using a 4‐point Likert scale (scores 1–4, respectively).
The CVI score of each item was computed as the number of experts giving a rating of 3 or 4 to the relevancy, clarity, and simplicity of each item, divided by the total number of experts. Based on this index, an entire statement was initially measured in terms of relevance, after which its acceptability was determined according to the following criteria: CVI > 0.79, the item is relevant, between 0.70 and 0.79, the item needs revisions, and if the value is below 0.70 the item is eliminated. 42 Scale‐level content validity index (S‐CVI) and scale‐level content validity ratio (S‐CVR) were also computed by calculating the mean of CVI and CVR values. S‐CVI 0.9% were considered as the acceptable validity index of the questionnaire. 42
2.3.3.
Reliability of the questionnaire: To assess the reliability of the questionnaire, the internal consistency, as well as the stability of the questionnaire, was measured.
2.3.3.1.
Internal consistency: Cronbach's coefficient α was calculated to examine the internal consistency of the subscales and the entire instrument. Values above 0.79 are considered acceptable in a descriptive study. 43
2.3.3.2.
Stability: The stability was also assessed by the test–retest method and through the completion of the questionnaires by 15 care providers within a 2‐week interval. Intraclass correlation coefficient (ICC) was also calculated to assess the stability of the questionnaire. If the ICC is above 0.7, the stability was considered appropriate. 44
2.3.3.3.
Describing the questionnaire and the scoring system: The final version of the questionnaire was a valid and reliable questionnaire that was used to measure needs for gender‐sensitive STIs/HIV prevention services with three‐level scales from “not at all” to “completely” important, which were scored from 0 to 2. The total score and the scores for the subscales of the questionnaire were calculated and converted to 0–100. High scores show more important needs for the gender‐sensitive STIs/HIV prevention services.
2.3.4. Outcome measures
CVI, CVR, α Cronbach's, ICC of the questionnaire were the outcome measures in this phase of the study.
2.4. Phase 3: The quantitative phase of the study “needs assessment for a gender‐sensitive STIs/HIV prevention services”
2.4.1. Design of the study
This was a descriptive cross‐sectional study in Shiraz‐Iran 2019.
2.4.2. Subjects of the study
All 290 providers of STIs/HIV prevention service providers participated in the study.
2.4.3. Inclusion criteria
The eligibility criteria for participation were at least 2 years of work experience in reproductive health care services, including STIs/HIV prevention care and counseling.
2.4.4. The setting of the study
All 37 health centers affiliated with SUMS and nine hospitals in Shiraz‐Iran.
2.4.5. Sampling
All 290 STIs/HIV prevention care providers. So, the subjects of the study were recruited using the survey convenience method of sampling.
2.4.6. Tool for data collection
The tools for data collection were (1) a demographic information questionnaire and; (2) a valid and reliable questionnaire that was developed in the second phase of the study (gender‐sensitive STIs/HIV prevention services [GSPS]). The validity and reliability of the questionnaire are described in the second phase of the study.
2.4.7. Outcome measures
The outcome measure in this phase of the study was the score of the needs for gender‐sensitive STIs/HIV prevention services. The needs were assessed by GSPS. High scores show more important needs for the gender‐sensitive STIs/HIV prevention services.
2.4.8. Data analysis
Data were analyzed by SPSS V‐22. p < 0.05 was considered significant. Figure 1 shows the procedure of the study.
Figure 1.
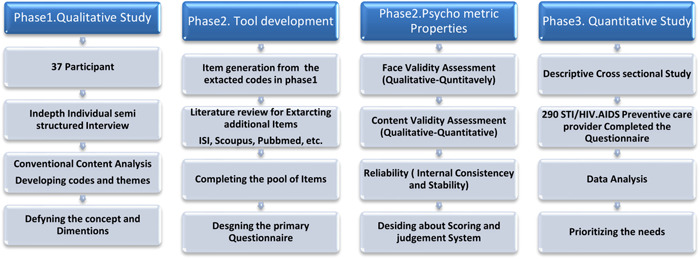
Procedure of the exploratory mixed sequential qualitative–quantitative study to assess needs for the gender‐sensitive STIs/HIV prevention services. AIDS, acquired immunodeficiency syndrome; STI/HIV, sexually transmitted infections/human immunodeficiency virus
2.5. Ethical considerations
Ethics were considered by describing the aims and procedure of the study for the participants. Written consent was obtained from all participants of the study. The confidentiality of information was guaranteed, as the name and personal information were not mentioned in tapes, transcripts, and the questionnaires. Permission was given by authorities in Shiraz and Tehran. The study was approved by the Ethical Committee of Shahid Beheshti University of Medical Sciences.
3. RESULTS
3.1. Phase 1: The qualitative phase of the study
In the qualitative phase, 37 participants (14 general practitioners, 13 midwives, 6 public health providers, 3 nurses, and a previous Minister of Health) were interviewed. They were also 13 men and 24 women. The average age of participants was 43.1 years, and the duration of work experience was 16.2 years. The results of the qualitative phase showed 63 codes categorized in 8 subthemes and 3 themes (Table 1). The extracted concept for gender‐sensitive STIs/HIV prevention services was: “the services with the appropriate structure, including gender‐sensitive personnel, facilities, and management as well as the appropriate process, including gender‐sensitive care and education. To achieve gender‐sensitive services, appropriate policies, the collaboration of different systems, and community empowerment are necessary for development and promotion of gender‐sensitive” (Figure 2).
Table 1.
The final version of the questionnaire to assess needs for gender‐sensitive STIs/HIV prevention services (GSPS)
| Not at all | Average | Completely | |
|---|---|---|---|
| How important are following supportive policies for the gender‐sensitive STIs/HIV care services | |||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
| How important are the following intersectional collaborations for the gender‐sensitive STIs/HIV care services | |||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
| How important are the following strategies for community capacitation in helping STIs/HIV prevention programs? | |||
|
|||
|
|||
|
|||
|
|||
| How important are the following characteristics for providers of STIs/HIV prevention services? | |||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
| How important are the following facilities for providing STIs/HIV prevention services? | |||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
| How important are the following management actions for providing STIs/HIV prevention services? | |||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
| How important are the following care services for providing STIs/HIV prevention services? | |||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
| How important are the following educations for providing STIs/HIV prevention services? | |||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
|
|||
Abbreviations: IUD, intrauterine device; STIs/HIV, sexually transmitted infections/human immunodeficiency virus.
Figure 2.
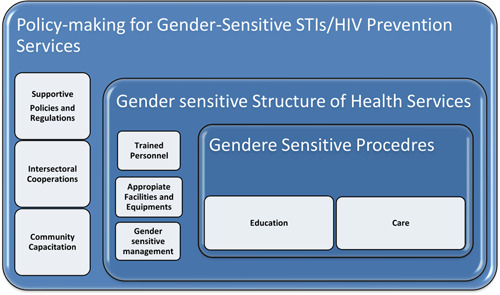
A schematic diagram of concept and dimensions of gender‐sensitive STIs/HIV prevention and care services. STIs/HIV, sexually transmitted infections/human immunodeficiency virus
3.2. Phase 2: The questionnaire development and psychometric properties assessment
3.2.1. The questionnaire development
The qualitative phase for the items generation: Sixty‐three extracted codes from the qualitative phase were categorized into eight subthemes and three themes. These codes and subthemes were used for the items generation and subscales of the questionnaire development.
3.2.2.
The literature review for completing the items: Three items were added to the item pool after the literature review, including: “Cooperating of sports organization for education and promotion of STIs/HIV prevention programs,” “Hotlines for response to the questions about STIs/HIV,” and “Providing self‐care education and the related booklets.” 45 , 46 , 47 Therefore, the primary GSPS questionnaire was developed with 66 items within eight subscales. Then, the psychometric properties of GSPS were assessed.
3.2.3. Psychometric properties of the questionnaire
The questionnaire was assessed regarding its validity and reliability as below:
3.2.4.
Validity of the questionnaire: Face and content validity as the theoretical and representational validity of the questionnaire was evaluated by qualitative and quantitative methods.
Face validity: Qualitative face validity resulted in corrections of five items and elimination of the Item “Develop long‐term health plans to increase the participation of men and adolescent boys in the prevention of sexually transmitted diseases” with an impact score of less than 1.5.
Content validity: Qualitative content validity assessment resulted in corrections of three items. Two further items including the items “Planning to deal with gender taboos such as premarital sex or homosexuality” and “Eliminate criminal offenses for exposing certain sexual behaviors” were omitted because of the CVI of less than 0.7. Content validity of GSPS was confirmed by S‐CVI and S‐CVR = 0.98 and S‐CVR = 0.87, respectively.
3.2.5.
Reliability of the questionnaire: To assess the reliability of the questionnaire, internal consistency and stability of the questionnaire were evaluated.
3.2.6.
Internal consistency: The internal consistency of GSPS was confirmed by α Cronbach = 0.972.
3.2.7.
Stability: Stability of the questionnaire was assessed and showed by test–retest method and calculating the intracluster correlation coefficient = 0.910.
After the procedure of face, content, reliability assessment, and the necessary corrections, the final valid and reliable questionnaire was developed with 63 items. Figure 3 shows the procedure of designing and validating the process of GSPS.
Figure 3.
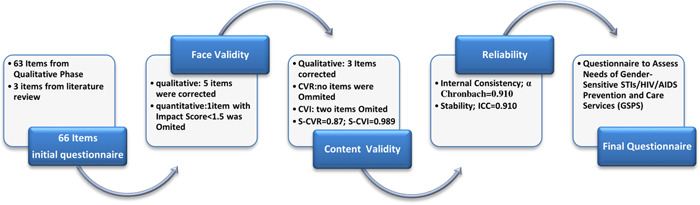
Results of validity and reliability assessment process of questionnaire to assess needs of gender‐sensitive STIs/HIV prevention and care services (GSPS‐63). AIDS, acquired immunodeficiency syndrome; ICC, intraclass correlation coefficient; S‐CVI, Scale‐level content validity index; S‐CVR, scale‐level content validity ratio; STIs/HIV, sexually transmitted infections/human immunodeficiency virus
3.2.8.
Describing the questionnaire and the scoring system: GSPS was a self‐completed questionnaire with 63 items. The items were scored on a three‐point scale of 0–2, for the importance of the item from “not at all” to “Completely.” The scores of items were summed up for calculation of total scores and then calculated scores were converted to 0–100. To convert the scores of the subscales and the entire questionnaire to a score of 0–100, the following conversion formula was used. Adjusted score = (the raw score obtained − minimum possible score/maximum possible − minimum possible score) × 100. High scores demonstrate the more important needs as the priorities for gender‐sensitive STIs/prevention services.
3.3. Phase 3: The quantitative phase of the study “assessment needs for gender‐sensitive STIs/HIV prevention services”
Two hundred ninety health providers participated in the study, with an average age of 33.48 ± 6.53 years (mean ± SD) and a working experience of 9.74 ± 5.65 years. The response rates of the participants were 100%. Table 2 demonstrated the participants' demographic characteristics.
Table 2.
Demographic characteristics of the STIs/HIV health care providers in Shiraz 2016 (n = 290)
| Characteristics | Category | Number | % |
|---|---|---|---|
| Gender | |||
| Female | 275 | 94.8 | |
| Male | 15 | 5.2 | |
| Age | |||
| 20–30 | 129 | 44.5 | |
| 31–40 | 121 | 41.7 | |
| >40 | 40 | 13.8 | |
| Education | |||
| Midwife (bachelor) | 229 | 79.0 | |
| Health educator (bachelor) | 23 | 10.8 | |
| Midwife (graduate diploma) | 30 | 7.9 | |
| Midwife (master) | 8 | 2.8 | |
| Job experience (years) | |||
| 2–10 | 179 | 61.7 | |
| 11–20 | 104 | 35.9 | |
| >20 | 7 | 2.3 | |
Abbreviation: STIs/HIV, sexually transmitted infections/human immunodeficiency virus.
Results of the quantitative descriptive phase demonstrated the highest priorities for the gender‐sensitive process (including care and educational dimensions) and then gender‐sensitive structure. The finding showed the highest priorities for the gender‐sensitive educational (92.01 ± 11.76%) and care services (92.11 ± 12.04%), respectively. Table 3 shows mean scores of all eight dimensions of the services and Table 4 demonstrates two priorities for the eight dimensions of the services.
Table 3.
Needs for gender‐sensitive STIs/HIV prevention services based on their priorities
| Sections | Dimensions | Mean ± SD (score 0–100) | Mean ± SD (score 0–100) |
|---|---|---|---|
| Process | Education | 92.01 ± 11.76 | 92.06 ± 12.04 |
| Care | 92.11 ± 12.04 | ||
| Structure of the Services | Human resources | 91.15 ± 13.31 | 90.52 ± 12.04 |
| Management | 90.53 ± 13.30 | ||
| Facilities | 89.35 ± 15.99 | ||
| Gender‐sensitive policies | Supportive policies | 86.22 ± 16.31 | 87.24 ± 14.05 |
| Intersectional cooperation | 86.80 ± 17.36 | ||
| Community empowerment | 91.07 ± 14.09 |
Abbreviation: STIs/HIV, sexually transmitted infections/human immunodeficiency virus.
Table 4.
Items with the highest priorities in each dimension of STIs/HIV prevention services
| Dimensions | Priorities | Score | Frequency (%) | |||
|---|---|---|---|---|---|---|
| Mean(0–2) | SD | Not at all: 0 | Roughly: 1 | Completely: 2 | ||
| Care | Recommending condom use to clients with high‐risk sexual behavior | 1.88 | 0.31 | 0 | 11.0 | 89.0 |
| Assessment of penis abnormalities as the barrier for condom use | 1.88 | 0.31 | 0 | 11.4 | 88.6 | |
| Education | Educating women about self‐protection | 1.87 | 0.33 | 0 | 12.8 | 87.2 |
| Sexual health education based on the men's and women's special needs | 1.86 | 0.35 | 0.3 | 12.8 | 86.9 | |
| Education of negotiation skills | 1.86 | 0.34 | 0 | 13.8 | 86.2 | |
| Personnel | Trained providers about reproductive rights of women and men | 1.86 | 0.34 | 0 | 13.8 | 86.2 |
| Trained male personnel about counseling, diagnosis, and treatment of men's STIs | 1.85 | 0.35 | 0.3 | 13.4 | 86.3 | |
| Management | Providing continuing education for STIs/HIV care providers | 1.84 | 0.35 | 0 | 15.2 | 84.8 |
| Personnel protection in the case of support for women's reproductive health | 1.82 | 0.42 | 1.7 | 13.8 | 84.5 | |
| Facilities | Providing a secure and private environment for STIs risk assessment | 1.84 | 0.38 | 0.7 | 14.5 | 84.8 |
| Introducing facilities for diagnosis, treatment, and follow‐up of men with STIs | 1.83 | 0.39 | 0.7 | 16.6 | 82.7 | |
| Supportive policies | Making spouses aware of STIs for improving family health | 1.80 | 0.4 | 0.7 | 18.6 | 80.7 |
| Planning for abstinence promotion and the risk reduction policy (condom use and lowering partners) | 1.79 | 0.47 | 3.1 | 14.1 | 82.8 | |
| Intersectional cooperation | Academic research about sexual behavior in different communities | 1.75 | 0.46 | 1.7 | 20.7 | 77.6 |
| Determining common sexual medications in the private sector, effective in preventing or spreading STIs | 1.75 | 0.48 | 2.4 | 19.7 | 77.9 | |
| Community capacitation | Parents education for improving adolescents' sexual health | 1.83 | 0.37 | 0 | 16.9 | 83.1 |
| Promoting culturally appropriate programs for preventing sexual high‐risk behavior | 1.82 | 0.31 | 1.0 | 15.9 | 83.1 | |
Abbreviation: STIs/HIV, sexually transmitted infections/human immunodeficiency virus.
4. DISCUSSION
This is the first mixed exploratory study to explain the concept and dimensions of gender‐sensitive STIs/HIV/AIDS prevention services and then the needs and priorities for providing these services.
Gender‐sensitive STI/HIV prevention services were defined as: “the services with the appropriate structure, including gender‐sensitive personnel, facilities, and management, as well as the appropriate process, including gender‐sensitive care and education. To achieve gender‐sensitive services, appropriate policies, the collaboration of different systems, and community empowerment are necessary for development and promotion of gender‐sensitive.” According to the Donabdian model for evaluating the quality of health care, 48 information about the quality of care can be drawn from three dimensions of services, including “structure,” “process,” and “outcomes.” Assessment of the gender sensitivity of the services mentioned the importance of gender sensitivity of process and structure of STIs/HIV services. Consistent with other studies, the present study emphasizes the importance of cultural factors that define gender roles in any community on the quality of the services. 49
Subsequently, results of the quantitative phase showed that procedures of the services, (both care and educational process) are the most important priorities in providing these services. The most important care was stated to be “Recommending condom use to clients with high‐risk sexual behavior” and then “assessment of penis abnormalities as a barrier for condom use.” Otherwise, the results emphasized overcoming gender‐based barriers to men's sexual health and promoting condom use. Diminishing taboos and providing appropriate counseling for risk reduction and condom use as well as assessment of male reproductive system are also emphasized in previous studies. 50
Results showed three priorities for educational procedures, including “women's education about self‐protection” and “Sexual health education based on the men's and women's special needs” and “education on negotiation skills about condom use.” Women's education about these areas helps to improve couples' relationships, couples' sexual health, preventing high‐risk behavior of spouses, such as spouses' out of marriage partnership and multiple sexual partnerships and preventing sexual abuse, and finally, empower women's sexual reproductive health. It is documented that knowledge about condom and condom accessibility is not enough, rather overcoming the barriers of condom use are necessary, such as the overwhelming unequal status of women and men in a community and masculinity and myth about the male role in decision‐making. Furthermore, women's education on negotiation skills can be effective on the promotion of condom use. 7
The gender‐sensitive structure of the services showed the need for gender‐sensitive providers, facilities, and management. In the quantitative assessment, two priorities were demonstrated including “Trained Providers about reproductive rights of women and men” and “Trained male personnel about counseling, diagnosis, and treatment of men's STIs.” Female providers in many health care systems are the barriers for attending men in giving any care services, especially for STIs prevention and treatment services. Besides male care providers of some health care services lack the necessary information, which is also another barrier for attending men for the care and treatment of STIs. 51
Results revealed two priorities for gender‐sensitive management of the services, consisting of needs for “Providing continuing education for STIs/HIV care providers” and “Personnel protection in the case of support for women's reproductive health". World Health Organization 52 emphasized on development of health providers' education about reproductive health as a top priority in the management of health systems and also mentioned to be important for combating STIs dissemination. Besides, the need for “protecting personnel in the case of support of women's reproductive health right” is also demonstrated in previous studies. In these studies, health providers emphasized the necessity for personnel's education about appropriate interactions as well as the need for developing the legal supportive systems for this personnel in health and public organizations. 53 , 54
The results showed two top priorities for reforming facilities of the services, including “Providing a secure and private environment for STIs risk assessment” and “Introducing facilities for diagnosis, treatment, and follow‐up of men with STIs.” It is demonstrated that men need private counseling and care services at an appropriate time, preferably in the evening or weekend. 24 , 55 Furthermore, the services should be comprehensive and contain STIs/HIV preventive as well as curative care and follow‐up facilities. 47
The results demonstrated “supportive policies” as the priority of the services. Two items showed the highest scores, including “Making spouses aware about STIs, for improving family health” and “Planning for abstinence promotion and the risk reduction policy.” It is demonstrated that spouses' awareness about STIs prevention, their treatment, and preventing from recurrent infections is important. 56 In many countries spouses' counseling is compulsory in health services and counseling is performed in STI cases. 57 It seems a comprehensive sexual health education including a risk reduction program should be considered as a supportive policy for our community. Planning of skill‐based educational interventions that enhance behavioral and preventive beliefs and promote abstinence would reduce the risk of STIs. 58
Findings also showed two priorities for the intersectional cooperation for supporting the gender‐sensitive services, including “Academic research about sexual behavior in different communities” and “Determining common sexual medications in the private sector, effective on preventing or spreading of STIs.” Extensive research was demonstrated as an essential base for an evidence‐based intervention for promoting sexual health. 59 Since there are some limitations in public sectors for providing services to high‐risk individuals, information about taking these medications is low. It is revealed that a minority of youth are involved in premarital relationships. 60 Homosexuality is also forbidden and there is no information about the frequency of AIDS among these high‐risk groups. 61 Therefore, there is the global problem that information about high‐risk groups and social outcast groups such as sex workers are limited and it is the reason for limited success in STIs/HIV programs and so academic researchers are necessary. 62
Priorities for community capacitation, as another gender‐sensitive policy, were “Parents education for improving adolescents' sexual health” and “Promoting of culturally appropriate programs for preventing sexual high‐risk behavior.” Several studies documented that a close relationship between parents and children can reduce high‐risk behaviors 63 , 64 , 65 and prevent STIs/HIV among adolescents. 66 , 67 Studies demonstrated a majority of parents are unwilling to encourage their sons about condom use, as they presume youth are not sexually active. Thus developing educational programs for parents are necessary. 68 , 69 Besides, the educational level of parents was positively associated with talking of parents and adolescents about sexual health. 70 Also, in many Moslem countries, the success of high‐risk prevention programs is imitated because of the stigmatization of high‐risk sexual behaviors, while homosexuality or out of marriage sexual relationships and sex working is common in these countries and needs more care and risk reduction counseling services. 71 Many studies are also emphasized women's empowerment in sexual reproductive health behaviors as an essential policy for preventing STI/HIV. 72 , 73 Community empowerment is also necessary for moderating the effects of gender on STI risk‐related sexual behavior by mass media cooperation. 74
In this mix sequential exploratory study, we tried to assess the need for promoting gender‐based STI/HIV/AIDS prevention services in Iran, with a valid and reliable tool. Since gender stereotypes in Iranian culture are somewhat similar to other Middle‐East countries, the needs shown in this study can be similar for the countries of this region. Besides, the methodology of this study can be applied not only in the region but also in all countries to identify the specific needs of men and women for providing the appropriate gender‐based services and so to improve the quality of the services. According to The United Nations Population Fund's research report on the effects of culture and religion on reproductive health that was performed in 169 countries around the world, gender stereotypes were mentioned as the main barrier for reproductive health promotion. Then further research was recommended to identify needs in other countries with different cultures, to provide evidence‐based strategies to promote reproductive health by removing cultural barriers. 75
Therefore, we emphasize that gender‐restrictive norms undermine the health and wellbeing of all people. It is essential to address gender bias in the health system for achieving Sustainable Development Goals. Also, the World Health Organization's Global Health Sector Strategy on STIs 2016–2021 highlights the importance of gender equality in STI prevention and control programs. 76 Given the global recommendations and recent momentum in incorporating gender equality in policies and programs, the finding of the present study certainly has positive implications for the delivery of gender‐sensitive STIs/HIV preventive services. Also, this innovative design can be replicated in other settings. To our knowledge, this is the first study for assessing the needs for gender‐sensitive services, with an innovative design in the region where gender stereotypes are usually highlighted. We recommend conducting similar studies in other areas of reproductive health and other countries of the region and the world, especially in countries with deeper gender equality gaps.
4.1. Limitation
The taboo of talking about sexual issues was a limitation that was controlled by an explanation about the confidentiality of the information by providing a nameless questionnaire. Also, we did not mention the needs of individuals with gender dysphoria, as we believe they have vast special needs. Besides, since homosexuality in Iran is against the law and sharia, researching this area requires a different research design. We recommend further research focusing on sexual orientation/behavior and the needs for providing the services based on the specific needs of individuals with opposite sexual orientation and behavior. It should be noted that people with dysphonia have permission for surgery and gender reassignment. 77
Since the aim of the present study was to explain and determine the needs of the system to provide gender‐sensitive STI/HIV prevention services, we develop and use GSPS questionnaire with theoretical validity (content and face validity). We suggest factor analysis for empirical construct and criterion validity as well as theoretical validity assessment in future studies that aim at tool development.
5. CONCLUSION
This was the first mixed exploratory study to assess needs for gender‐sensitive STIs/HIV prevention services. With a theoretical valid and reliable tool (GSPS with S‐CVI = 0.98; S‐CVR = 0.87; α Cronbach = 0.91 stability; ICC = 0.910). It was demonstrated that providing STIs/HIV prevention services requires reforms to achieve a gender‐appropriate educational and care process, as well as a gender‐sensitive structure, including gender‐sensitive personnel, facilities, and management. These dimensions need advocacy by supportive policies and intersectional cooperation, as well as equipping the community for promoting gender‐sensitive STIs/HIV prevention services. Certainly, providing these comprehensive and efficient services improves the quality of the STIs/HIV prevention services. In this article, the need and priorities for making the gender‐sensitive STIs/HIV prevention services were explained. A valid and reliable questionnaire to assess these needs was developed and introduced. The paper made evidence‐based suggestions for managers and policymakers to improve the quality of the services by providing gender‐sensitive services.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
AUTHOR CONTRIBUTIONS
Conceptualization: Masoumeh Simbar, Fatemeh Rahmanian, Soheila Nazarpour, Ali Ramezankhani. Data curation: Masoumeh Simbar, Fatemeh Rahmanian, Farid Zayeri. Formal analysis: Fatemeh Rahmanian, Farid Zayeri: Not applicable. Investigation: Masoumeh Simbar, Fatemeh Rahmanian, Soheila Nazarpour, Ali Ramezankhani, Farid Zayeri. Methodology: Masoumeh Simbar, Fatemeh Rahmanian, Ali Ramezankhani. Project Administration: Masoumeh Simbar, Ali Ramezankhani. Resources: Masoumeh Simbar, Fatemeh Rahmanian, Soheila Nazarpour. Software: Not applicable. Supervision: Masoumeh Simbar, Soheila Nazarpour, Ali Ramezankhani, Farid Zayeri. Validation: Masoumeh Simbar, Fatemeh Rahmanian, Farid Zayeri. Visualization: Not applicable. Writing—original draft preparation: Masoumeh Simbar, Soheila Nazarpour. Writing—review and editing: Masoumeh Simbar, Soheila Nazarpour. All authors have read and approved the final version of the manuscript.
Simbar M, Rahmanian F, Nazarpour S, Ramezankhani A, Zayeri F. Priorities for a gender‐sensitive sexually transmitted infections and human immunodeficiency virus (STIs/HIV) services: an exploratory mixed methods study. Health Sci Rep. 2022;5:e553. 10.1002/hsr2.553
Contributor Information
Soheila Nazarpour, Email: soheilanazarpour@iauc.ac.ir.
Farid Zayeri, Email: fzayeri@yahoo.com.
DATA AVAILABILITY STATEMENT
The corresponding author Soheila Nazarpour confirms that he had full access to all of the data in the study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.
REFERENCES
- 1. Kaufman MR, Pulerwitz J. When sex is power gender roles in sex and their consequences. In: Agnew CR, Harman JJ, eds. Power in Close Relationships. Cambridge University Press; 2019:173‐191. [Google Scholar]
- 2. Heise L, Greene ME, Opper N, et al. Gender inequality and restrictive gender norms: framing the challenges to health. Lancet. 2019;393(10189):2440‐2454. [DOI] [PubMed] [Google Scholar]
- 3. Barker G, Nascimento M, Pulerwitz J, Ricardo C, Segundo M, Verma R. Engaging young men in violence prevention: reflections from Latin America and India. In: Leach F, Mitchell C, eds. Combating Gender Violence in and Around Schools. Cromwell Press; 2006. [Google Scholar]
- 4. Panchanadeswaran S, Johnson SC, Mayer KH, et al. Gender differences in the prevalence of sexually transmitted infections and genital symptoms in an urban setting in southern India. Sex Transm Infect. 2006;82(6):491‐495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rowley J, Vander Hoorn S, Korenromp E, et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull World Health Organ. 2019;97(8):548‐562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pourmohsen M, Simbar M, Nahidi F, Fakor F, Alavi Majd H. Women's experiences of infection with human papillomavirus in the face of disease symptoms: a qualitative study. Int J Womens Health Reprod Sci. 2020;8(1):37‐45. [Google Scholar]
- 7. Deming ME, Bhochhibhoya A, Ingram L, Stafford C, Li X. HIV/STI interventions targeting women who experience forced sex: a systematic review of global literature. Health Care Women Int. 2018;39(8):919‐935. [DOI] [PubMed] [Google Scholar]
- 8. Diamant‐Wilson R, Leathers SJ. Safer sex strategies and the role of gender among African American youth transitioning from foster care. Child Youth Serv Rev. 2020;111:104798. [Google Scholar]
- 9. Weber AM, Cislaghi B, Meausoone V, et al. Gender norms and health: insights from global survey data. Lancet. 2019;393(10189):2455‐2468. [DOI] [PubMed] [Google Scholar]
- 10. Pourmohsen M, Simbar M, Nahidi F, Fakor F, Majd HA. HPV risk factors and prevention behaviours: a review. J Clin Diagn Res. 2018;12(12):LE01‐LE05. [Google Scholar]
- 11. Hay K, McDougal L, Percival V, et al. Disrupting gender norms in health systems: making the case for change. Lancet. 2019;393(10190):2535‐2549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Haberland NA. The case for addressing gender and power in sexuality and HIV education: a comprehensive review of evaluation studies. Int Perspect Sex Reprod Health. 2015;41(1):31‐42. [DOI] [PubMed] [Google Scholar]
- 13. World Health Organization . Gender and Road Traffic Injuries. Geneva, Switzerland: Department of Gender and Women's Health; 2002.
- 14. Williams CT, Kim S, Meyer J, et al. Gender differences in baseline health, needs at release, and predictors of care engagement among HIV‐positive clients leaving jail. AIDS Behav. 2013;17(2):195‐202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Celik H, Lagro‐Janssen TA, Widdershoven GG, Abma TA. Bringing gender sensitivity into healthcare practice: a systematic review. Patient Educ Couns. 2011;84(2):143‐149. [DOI] [PubMed] [Google Scholar]
- 16. WCHM . Submission to Patient‐ and Consumer‐Centred Care Discussion Paper. Women's Centre for Health Matters; 2009.
- 17. Simbar M, Rahmanian F, Nazarpour S, Ramezankhani A, Eskandari N, Zayeri F. Design and psychometric properties of a questionnaire to assess gender sensitivity of perinatal care services: a sequential exploratory study. BMC Public Health. 2020;20(1):1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Simbar M, Rahmanian F, Nazarpour S, Ramezankhani A, Zayeri F. Needs for a gender‐based perimarital couples' counselling services in Iran. Nurs Open 2021;8(2):850‐857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lichtenstein B. Stigma as a barrier to treatment of sexually transmitted infection in the American deep south: issues of race, gender and poverty. Soc Sci Med. 2003;57(12):2435‐2445. [DOI] [PubMed] [Google Scholar]
- 20. Garcia PJ, Miranda AE, Gupta S, Garland SM, Escobar ME, Fortenberry JD. The role of sexually transmitted infections (STI) prevention and control programs in reducing gender, sexual and STI‐related stigma. eClinicalMedicine. 2021;33:100764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mmari KN, Oseni O, Fatusi AO. STI treatment‐seeking behaviors among youth in Nigeria: are there gender differences? Int Perspect Sex Reprod Health. 2010;36(2):72‐79. [DOI] [PubMed] [Google Scholar]
- 22. Rahmanian F, Nazarpour S, Simbar M, Ramezankhani A, Zayeri F. Needs assessment for gender sensitive reproductive health services for adolescents. Int J Adolesc Med Health. 2020;32(5). 10.1515/ijamh-2017-0201 [DOI] [PubMed] [Google Scholar]
- 23. Joint United Nations Programme on HIV/AIDS . UNAIDS report: sexual health education does lead to safer sexual behaviour. Press Release; 1997, p. 22.
- 24. Simbar M, Nahidi F, Ramezani‐Tehrani F, Akbarzadeh A. Educational needs assessment for men's participation in perinatal care. East Mediterr Health J. 2011;17(9):689‐696. [PubMed] [Google Scholar]
- 25. Orji E, Adegbenro C, Moses O, Amos O, Olanrenwaju O. Men's involvement in safe motherhood. J Turk Ger Gynecol Assoc. 2007;8(3):240‐246. [Google Scholar]
- 26. Newman C. Gender sensitivity assessment. Tools for RH Service Providers and Managers. IntraHeatlh International; 2003. [Google Scholar]
- 27. WHO . Report on global sexually transmitted infection surveillance. Geneva: WHO; 2018.
- 28. World Health Organization . Global incidence and prevalence of selected curable sexually transmitted infections‐2008. Geneva: World Health Organization; 2012. Accessed January 20, 2021. https://apps.who.int/iris/bitstream/10665/75181/1/9789241503839_eng.pdf?ua=1
- 29. HIVHUB . HIV/STI Surveillance Research Center, and WHO Collaborating Center for HIV Surveillance. 2021. Accessed January 20, 2021. https://hivhub.ir/
- 30. Ministry of Health and Medical Education (MOHME) . National AIDS Committee Secretariat, Islamic Republic of Iran AIDS progress report. 2012.
- 31. Creswell JW, Clark VLP. Designing and Conducting Mixed Methods Research. Sage Publications; 2017. [Google Scholar]
- 32. Waltz CF, Strickland OL, Lenz ER. Measurement in Nursing and Health Research. Springer Publishing; 2010. [Google Scholar]
- 33. Lincoln YS, Guba EG. Naturalistic Inquiry. Sage; 1985. [Google Scholar]
- 34. Allen M. The SAGE Encyclopedia of Communication Research Methods. Sage Publications; 2017. [Google Scholar]
- 35. Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105‐112. [DOI] [PubMed] [Google Scholar]
- 36. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA‐ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467‐473. [DOI] [PubMed] [Google Scholar]
- 37. Marca SC, Paatz P, Györkös C, et al. Validation of questionnaires and rating scales used in medicine: protocol for a systematic review of burnout self‐reported measures. medRxiv. 2020. 10.1101/2020.06.24.20138115 [DOI] [Google Scholar]
- 38. Khoshrang H, Dadgaran I, Shaigan H. Designing a questionnaire to measure threats and opportunities of e‐learning and determining its psychometric properties. Interdiscip J Virtual Learn Med Sci. 2014;5(3):1‐10. [Google Scholar]
- 39. Hajizadeh E, Asghari M. Statistical Methods and Analyses in Health and Biosciences a Research Methodological Approach. Jahade Daneshgahi Publications; 2011. [Google Scholar]
- 40. Waltz C, Bausell RB. Nursing Research: Design, Statistics, and Computer Analysis. F. A. Davis; 1983. [Google Scholar]
- 41. Lawshe CH. A quantitative approach to content validity. Pers Psychol. 1975;28(4):563‐575. [Google Scholar]
- 42. Polit DF, Beck CT. Essentials of Nursing Research: Appraising Evidence for Nursing Practice. 7th ed. Wolters Kluwer Health/Lippincott Williams & Wilkins; 2010. [Google Scholar]
- 43. Tavakol M, Dennick R. Making sense of Cronbach's alpha. Int J Med Educ. 2011;2:53‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Yarmohammadi Vasel M, Narenjiha H, Rafiey H. Developing and validation of life skills inventory for substance abusers. Soc Welf Q. 2011;10(39):151‐156. [Google Scholar]
- 45. WHO . Considerations for formulating Reproductive health laws. Geneva: World Health Organization; 2000.
- 46. WHO . Sexual and reproductive health core competencies in primary care: World Health Organization; 2011.
- 47. IPPF . From evidence to action: Advocating for comprehensive sexuality education. UK: The International Planned Parenthood Federation; 2009.
- 48. Donabedian A. An Introduction to Quality Assurance in Health Care. Oxford University Press; 2003. [Google Scholar]
- 49. Alilyyani B, Wong CA, Cummings G. Antecedents, mediators, and outcomes of authentic leadership in healthcare: a systematic review. Int J Nurs Stud. 2018;83:34‐64. [DOI] [PubMed] [Google Scholar]
- 50. Yu J, Tanaka Y, Yamaguchi Y, Matsuo H. The current status of knowledge and behavior related to STI prevention among high school students in Korea. Univers J Public Health. 2018;6(5):274‐283. [Google Scholar]
- 51. Simbar M, Nahidi F, Tehrani FR, Ramezankhani A. Fathers' educational needs for perinatal care in urban Iran: a qualitative approach. J Biosoc Sci. 2010;42(5):633‐641. [DOI] [PubMed] [Google Scholar]
- 52. WHO . Regional Office for Europe. Checklist for assessing the gender responsiveness of sexual and reproductive health policies. Geneva World Health Organization; 2010.
- 53. Cann K, Withnell S, Shakespeare J, Doll H, Thomas J. Domestic violence: a comparative survey of levels of detection, knowledge, and attitudes in healthcare workers. Public Health. 2001;115(2):89‐95. [DOI] [PubMed] [Google Scholar]
- 54. Sugg NK, Inui T. Primary care physicians' response to domestic violence. Opening Pandora's box. JAMA. 1992;267(23):3157‐3160. [PubMed] [Google Scholar]
- 55. Sendrowitz J, Solter C, Hainsworth G. Clinic assessment of youth friendly services: technical services Unit Pathfinder International; 2002.
- 56. Khalesi ZB, Simbar M, Azin SA. A qualitative study of sexual health education among Iranian engaged couples. Afr Health Sci. 2017;17(2):382‐390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. ECDC . Public health benefits of partner notification for sexually transmitted infections and HIV. Stockholm: European Centre for Disease Prevention and Control; 2013.
- 58. Wong ML, Ng JYS, Chan RKW, Chio MTW, Lim RBT, Koh D. Randomized controlled trial of abstinence and safer sex intervention for adolescents in Singapore: 6‐month follow‐up. Health Educ Res. 2017;32(3):233‐243. [DOI] [PubMed] [Google Scholar]
- 59. Khalesi ZB, Simbar M, Azin SA, Zayeri F. Public sexual health promotion interventions and strategies: a qualitative study. Electron Physician. 2016;8(6):2489‐2496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Bahrami N, Simbar M, Vedadhir A, Bukowski WM, Panarello B. Male Iranian adolescent's reasons for having an other‐gender friend. Int J Adolesc Med Health. 2016;29(3). 10.1515/ijamh-2015-0086 [DOI] [PubMed] [Google Scholar]
- 61. Feizzadeh A, Nedjat S, Asghari S, et al. Evidence‐based approach to HIV/AIDS policy and research prioritization in the Islamic Republic of Iran. East Mediterr Health J. 2010;16(3):259‐265. [PubMed] [Google Scholar]
- 62. Talbott JR. Size matters: the number of prostitutes and the global HIV/AIDS pandemic. PLOS One. 2007;2(6):e543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Shahhosseini Z, Simbar M, Ramezankhani A, Alavi Majd H. Supportive family relationships and adolescent health in the socio‐cultural context of Iran: a qualitative Study. Ment Health Fam Med. 2012;9(4):251‐256. [PMC free article] [PubMed] [Google Scholar]
- 64. Zare E, Simbar M, Shahhoseini Z, Alavi Majd H. The priorities of iranian male adolescents health needs. Am J Mens Health. 2017;11:1255‐1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Salehin S, Simbar M, Keshavarz Z, Nasiri M. Empowerment of mothers concerning female adolescent's reproductive health in Iran: a qualitative study. Crescent J Med Biol Sci. 2019;6(3):309‐317. [Google Scholar]
- 66. Phetla G, Busza J, Hargreaves JR, et al. “They have opened our mouths”: increasing women's skills and motivation for sexual communication with young people in rural South Africa. AIDS Educ Prev. 2008;20(6):504‐518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Adu‐Mireku S. Family communication about HIV/AIDS and sexual behaviour among senior secondary school students in Accra, Ghana. Afr Health Sci. 2003;3(1):7‐14. [PMC free article] [PubMed] [Google Scholar]
- 68. Tipwareerom W, Weglicki L. Parents' knowledge, attitudes, behaviors, and barriers to promoting condom use among their adolescent sons. Nurs Health Sci. 2017;19(2):212‐219. [DOI] [PubMed] [Google Scholar]
- 69. Salehin S, Simbar M, Keshavarz Z, Nasiri M. Parents' perspectives on challenges of sexual and reproductive health education to adolescents in Iran and the world: systematic review. J Isfahan Med Sch 2019;36(508):1540‐1553. [Google Scholar]
- 70. Taffa N, Haimanot R, Desalegn S, Tesfaye A, Mohammed K. Do parents and young people communicate on sexual matters. Ethiop J Health Dev. 2017;13(3):205‐210. [Google Scholar]
- 71. Hasnain M. Cultural approach to HIV/AIDS harm reduction in Muslim countries. Harm Reduct J. 2005;2:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Alimoradi Z, Kariman N, Simbar M, Ahmadi F. Empowerment of adolescent girls for sexual and reproductive health care: a qualitative study. Afr J Reprod Health. 2017;21(4):80‐92. [DOI] [PubMed] [Google Scholar]
- 73. Rashidi FR, Simbar M, Naz MSG, Fakari FR. Factors related to empowering Iranian women's fertility behaviors: a systematic review. J Obstet Gynecol Cancer Res. 2018;3(3):115‐122. [Google Scholar]
- 74. Carmack C, Rodriguez L. Social media usage as a correlate of STI risk‐related sexual behavior on the college campus: moderating effects of gender. Curr Psychol. 2018:39(5):1696‐1704. [Google Scholar]
- 75. UNFPA . Culture in the context of UNFPA Programming [Internet]; 2005. Accessed January 20, 2021. https://www.unfpa.org/publications/culture-context-unfpa-programming
- 76. World Health Organization . Global health sector strategy on HIV‐2021. Towards ending AIDS. Geneva: World Health Organization; 2016.
- 77. Simbar M, Nazarpour S, Mirzababaie M, et al. Quality of life and body image of individuals with gender dysphoria. J Sex Marital Ther. 2018;44(6):523‐532. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The corresponding author Soheila Nazarpour confirms that he had full access to all of the data in the study and takes complete responsibility for the integrity of the data and the accuracy of the data analysis.


