Abstract
Background
Despite surgical advances, acute type A aortic dissection remains a life-threatening disease with high mortality and morbidity. Tracheostomy is usually used for patients who need prolonged mechanical ventilation in the intensive care unit (ICU). However, data on the risk factors for requiring tracheostomy and the impact of tracheostomy on outcomes in patients after Stanford type A acute aortic dissection surgery (AADS) are limited.
Methods
A retrospective single-institutional study including consecutive patients who underwent AADS between January 2016 and December 2019 was conducted. Patients who died intraoperatively were excluded. Univariate analysis and multivariate logistic regression analysis were used to identify independent risk factors for postoperative tracheostomy (POT). A nomogram to predict the probability of POT was constructed based on independent predictors and their beta-coefficients. The area under the receiver operating characteristic curve (AUC) was performed to assess the discrimination of the model. Calibration plots and the Hosmer–Lemeshow test were used to evaluate calibration. Clinical usefulness of the nomogram was assessed by decision curve analysis. Propensity score matching analysis was used to analyze the correlation between requiring tracheostomy and clinical prognosis.
Results
There were 492 patients included in this study for analysis, including 55 patients (11.2%) requiring tracheostomy after AADS. Compared with patients without POT, patients with POT experienced longer ICU and hospital stay and higher mortality. Age, cerebrovascular disease history, preoperative white blood cell (WBC) count and renal insufficiency, intraoperative amount of red blood cell (RBC) transfusion and platelet transfusion were identified as independent risk factors for POT. Our constructed nomogram had good discrimination with an AUC = 0.793 (0.729–0.856). Good calibration and clinical utility were observed through the calibration and decision curves, respectively. For better clinical application, we defined four intervals that stratified patients from very low to high risk for occurrence of POT.
Conclusions
Our study identified preoperative and intraoperative risk factors for POT and found that requiring tracheostomy was related to the poor outcomes in patients undergoing AADS. The established prediction model was validated with well predictive performance and clinical utility, and it may be useful for individual risk assessment and early clinical decision-making to reduce the incidence of tracheostomy.
Keywords: Acute type A aortic dissection, Postoperative tracheostomy, Risk factors, Outcomes, Nomogram
Introduction
Respiratory failure needing prolonged ventilator support is a frequent and serious complication and is also a common cause of in-hospital deaths in patients undergoing Stanford type A acute aortic dissection surgery (AADS) [1]. About 28.9%-34.6% of patients with AADS had prolonged mechanical ventilation postoperatively, which was associated with an increased risk of morbidity and mortality [2, 3]. Tracheostomy is commonly used for patients requiring prolonged mechanical ventilation in the intensive care unit (ICU) to optimize the work of breathing or facilitate weaning [4]. Some studies reported the number of patients undergoing tracheostomy after AADS and the incidence was about 4.7% to 11.8% [2, 5, 6].
Patients who underwent tracheostomy had been found to have significantly longer mechanical ventilation time and hospital stay but a lower hospital mortality compared with those not receiving a tracheostomy among the patients requiring mechanical ventilation in the ICU setting [7]. In addition, the dramatically longer duration of hospitalization and worse survival were observed in patients requiring tracheostomy after some major surgeries, such as liver transplant and congenital heart surgery [8, 9]. However, the outcomes of patients receiving a tracheostomy after AADS have rarely been described before. Moreover, to our knowledge, no studies have been conducted to identify clinical risk factors of postoperative tracheostomy (POT) in patients after AADS.
The present study was undertaken to explore the relationship between POT and the outcomes in patients who underwent AADS, and also to identify independent predictors for POT among these patients and thus construct a prediction model to predict the occurrence of POT.
Methods
Study population
A retrospective study was performed at a single center. The consecutive patients who underwent AADS at our institution between January 2016 and December 2019 were studied. Patients who died during the surgery were excluded from this study.
This study was conducted in accordance with ethical statement of the Declaration of Helsinki and was approved by The Ethics Committee of Tongji Medical College of Huazhong University of Science and Technology (IORG No. IORG0003571). The requirement of written informed consent was waived by The Ethics Committee of Tongji Medical College of Huazhong University of Science and Technology (IORG No. IORG0003571) due to its observational, retrospective nature.
Baseline data
Baseline data including demographics, comorbidities, preoperative laboratory values and surgical procedure were documented. Specifically, the demographics contained age, sex, body mass index, history of smoking and drinking; comorbidities included diabetes mellitus, hypertension, cardiac surgery history, general surgery history, pulmonary artery hypertension, cerebrovascular disease, atrial fibrillation, pericardial effusion, chronic obstructive pulmonary disease, left ventricular ejection fraction, gastrointestinal tract disease, NYHA class III-IV, peripheral vascular disease, renal insufficiency, diameter of the left ventricle, diameter of the right ventricle, diameter of the right atrium, and diameter of the left atrium; preoperative laboratory data contained platelet count, serum albumin, serum globulin, serum creatinine, white blood cell (WBC) count, red blood cell (RBC) count, hemoglobin; surgical procedure included isolated AADS, AADS combined with coronary artery bypass grafting, AADS combined with coronary artery bypass grafting, AADS combined with other types of cardiac surgery, AADS combined with valve surgery, AADS combined with valve and coronary surgery, cardiopulmonary bypass time, deep hypothermic circulatory arrest, aortic cross clamp time, transfusion of red blood cells and platelet.
Endpoints
Performing a tracheostomy on the patients after AADS was the primary endpoint of this study. The clinicians performed the tracheostomies through the percutaneous route in the ICU. The indications for tracheostomy in this study included bypass of upper airway obstruction, prolonged mechanical ventilation, predicted difficult reintubation, repeated intubation, one or more failed trails of extubation, and the need for tracheal access to remove thick pulmonary secretions. The secondary endpoints included readmission to ICU, the length of ICU and hospital stays, and mortality.
Derivation and verification of predictive model
We used clinical data to develop a risk model to predict the probability of tracheostomy in patients after they received AADS. Univariate analysis was used to screen out variables that were possibly associated with POT in the cohort. The potential risk factors which were significant in the univariate analysis (P < 0.10) were entered into the multivariate logistic regression analysis. A nomogram was constructed based on the independent predictors and their beta-coefficients in the multivariate analysis. Internal validation of the prediction model was assessed by bootstrapping using 1000 replications. The calibration, discrimination and clinical utility were conducted to evaluate the predictive performance of the nomogram. The area under the receiver operating characteristic (ROC) curve (AUC) or Harrell’s concordance index (C-index) was performed to assess the discrimination of the prediction model. The calibration curve was used to analyze the agreement between nomogram-predicted and actually observed probability. Decision curve analysis was conducted to assess the clinical utility of the nomogram by quantifying the standardized net benefits at different risk threshold.
Statistical analysis
SPSS software (version 26.0) and R software (version 4.0.3) were used for statistical analysis. Descriptive statistical analyses were performed for categorical and continuous variables. Categorical variables were presented as n (%), and continuous variables were presented as mean ± standard deviation or median (interquartile range). We compared categorical variables using the Chi-square or Fisher exact test, non-normal variables with the Mann–Whitney U test, normally distributed variables with the Student's t test. Propensity score matching analysis was performed to reduce potential selection bias to analyze the correlation between requiring tracheostomy and clinical prognosis in this study. The nearest available matching (1:1) method was used for propensity score matching with the caliper of 0.03. P value < 0.05 was considered statistically significant.
Results
Baseline characteristics
A total of 496 patients underwent type A acute aortic dissection repair surgeries during the 4-year period in our institution. After excluding 4 patients who died intraoperatively, 492 patients were included in the analysis. Of these, 55 patients (11.2%) required tracheostomy after AADS. The flow chart of this study is presented in Fig. 1. The average age of the entire cohort was 49.6 years, males accounted for 75.6%, the average body mass index reached 25.3 kg/m2, and the proportion of smoking history was 43.9%. In addition, hypertension, isolated AADS, and deep hypothermic circulatory arrest application, these variables accounted for more than 50% of the population in our study.
Fig. 1.
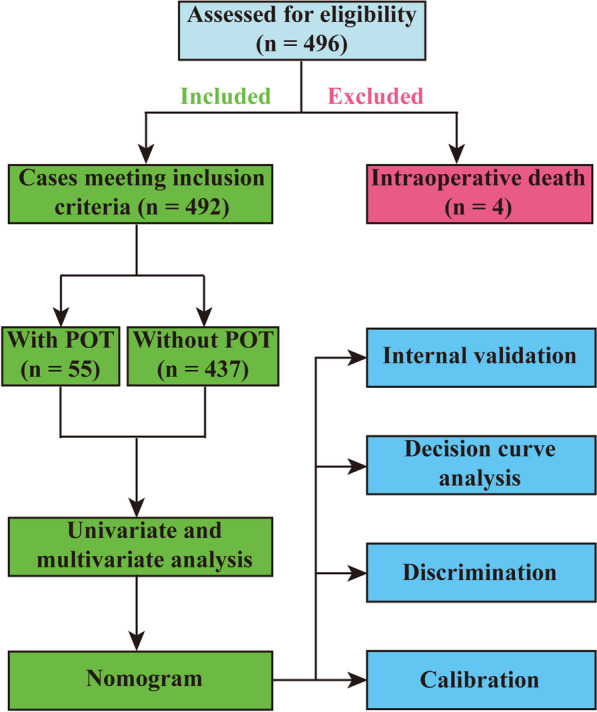
Flow chart of the study. AADS, Stanford type A acute aortic dissection surgery; POT, postoperative tracheostomy
Development and validation of risk predictive model
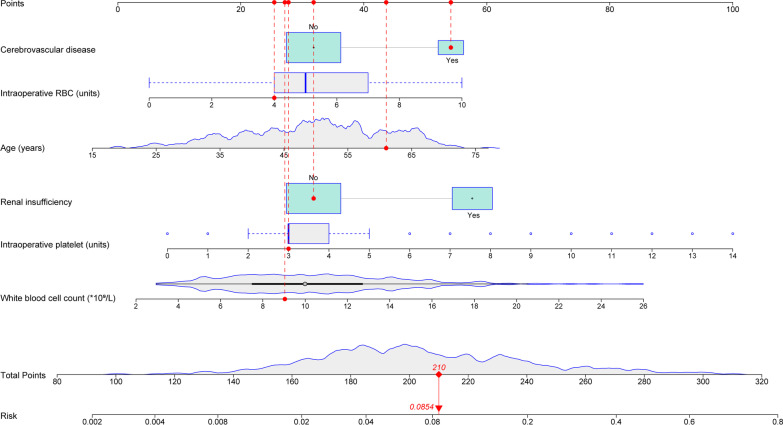
The univariate analysis was performed to screen out several potential risk factors for POT in patients undergoing AADS (Table 1). Before the establishment of a multivariate model, collinearity diagnostics were conducted. By stepwise forward selection, six risk factors were identified to independently predict the occurrence of POT, including age, cerebrovascular disease history, preoperative WBC count and renal insufficiency, intraoperative amount of RBC transfusion and platelet transfusion (Table 2). Then a nomogram was constructed based on previous multivariate model, and the regression coefficient of each predictor was scaled to points of 0–100, reflecting the relative importance of each predictor (Fig. 2). The probability of needing tracheostomy in a patients can be calculated by summing all the variables scores, and the risk of POT after AADS ranged from 0.002 to 0.8 on the nomogram.
Table 1.
Univariate analysis of possible risk factors for POT after AADS
| Characteristic | Without POT n = 437 (%) | With POT n = 55 (%) | χ2/Z/t | P value |
|---|---|---|---|---|
| Demographics | ||||
| Male | 322 (73.7) | 50 (90.9) | 7.860 | 0.005 |
| Age (years) | 49.27 ± 11.33 | 52.58 ± 10.83 | 2.051 | 0.041 |
| Body mass index (kg/m2) | 25.26 ± 3.65 | 25.93 ± 4.04 | 1.226 | 0.206 |
| Smoking history | 186 (42.6) | 30 (54.5) | 2.848 | 0.091 |
| Drinking history | 151 (34.6) | 25 (45.5) | 2.527 | 0.112 |
| Underlying conditions | ||||
| Hypertension | 292 (66.8) | 43 (78.2) | 2.903 | 0.088 |
| Diabetes mellitus | 19 (4.3) | 2 (3.6) | 0.061 | 0.806 |
| Chronic obstructive pulmonary disease | 5 (1.1) | 0 (0) | 0.636 | 0.425 |
| Cerebrovascular disease | 71 (16.2) | 17 (30.9) | 7.150 | 0.007 |
| Peripheral vascular disease | 63 (14.4) | 4 (7.3) | 2.119 | 0.145 |
| Renal insufficiency | 138 (31.6) | 35 (63.6) | 22.021 | < 0.001 |
| Gastrointestinal tract disease | 37 (8.5) | 5 (9.1) | 0.024 | 0.876 |
| Atrial fibrillation | 2 (0.5) | 2 (3.6) | 6.121 | 0.013 |
| Cardiac surgery history | 29 (6.6) | 3 (5.5) | 0.112 | 0.738 |
| General surgery history | 90 (20.6) | 11 (20.0) | 0.011 | 0.918 |
| NYHA class III-IV | 38 (8.7) | 3 (5.5) | 0.672 | 0.412 |
| Pulmonary artery hypertension | 14 (3.2) | 0 (0) | 1.814 | 0.178 |
| Pericardial effusion | 121 (27.7) | 12 (21.8) | 0.854 | 0.356 |
| Diameter of the left atrium (cm) | 3.5 (3.1, 3.9) | 3.7 (3.3, 4.0) | 2.459 | 0.014 |
| Diameter of the left ventricle (cm) | 4.8 (4.5, 5.3) | 4.7 (4.4, 5.2) | 0.889 | 0.374 |
| Diameter of the right atrium (cm) | 3.7 (3.5, 4.0) | 3.7 (3.5, 4.0) | 0.108 | 0.914 |
| Diameter of the right ventricle (cm) | 3.6 (3.3, 3.9) | 3.6 (3.4, 3.9) | 0.672 | 0.502 |
| Left ventricular ejection fraction (%) | 62 (60, 65) | 62 (60, 65) | 0.340 | 0.733 |
| Laboratory values | ||||
| White blood cell count (× 109/L) | 9.8 (7.3, 12.5) | 12.1 (9.0, 14.7) | 3.350 | 0.001 |
| Red blood cell count (× 1012/L) | 4.2 (3.8, 4.6) | 4.3 (3.9, 4.7) | 1.404 | 0.160 |
| Hemoglobin (g/L) | 127 (113, 139) | 132 (122, 142) | 1.831 | 0.067 |
| Platelet count (× 109/L) | 160 (127, 208) | 149 (119, 181) | 1.901 | 0.057 |
| Serum creatinine (μmol/L) | 78.0 (65.2, 109.0) | 83.0 (69.0, 115.5) | 2.840 | 0.005 |
| Serum albumin (g/L) | 37.8 (35.0, 40.9) | 37.8 (33.6, 40.5) | 0.497 | 0.619 |
| Serum globulin (g/L) | 25.6 (22.9, 28.3) | 25.6 (22.0, 28.3) | 0.316 | 0.752 |
| Operative variables | ||||
| Surgical types | 0.080 | 0.999 | ||
| Isolated AADS | 286 (65.4) | 36 (65.5) | ||
| Combined valve surgery | 98 (22.4) | 12 (21.8) | ||
| Combined coronary artery bypass grafting | 23 (5.3) | 3 (5.5) | ||
| Combined valve and coronary surgery | 24 (5.5) | 3 (5.5) | ||
| Combined other types of cardiac surgery | 6 (1.2) | 1 (0.2) | ||
| Deep hypothermic circulatory arrest | 257 (58.8) | 33 (60.0) | 0.029 | 0.866 |
| Cardiopulmonary bypass time (minutes) | 209 (174, 256) | 229 (196, 264) | 2.025 | 0.043 |
| Aortic cross clamp time (minutes) | 120 (96, 147) | 121 (107, 148) | 1.487 | 0.137 |
| Transfusion of red blood cells (units) | 5 (4, 7) | 7 (5, 9) | 5.257 | < 0.001 |
| Transfusion of platelet (units) | 3 (2, 4) | 4 (3, 7) | 5.009 | < 0.001 |
AADS, Stanford type A acute aortic dissection surgery; POT, postoperative tracheostomy
Table 2.
Multivariate analysis of independent risk factors for POT after AADS
| Characteristic | Coefficient | Standard error | OR (95% CI) | P value |
|---|---|---|---|---|
| Age (years) | 0.035 | 0.015 | 1.035 (1.005–1.067) | 0.023 |
| Cerebrovascular disease | 0.719 | 0.364 | 2.053 (1.007–4.187) | 0.048 |
| White blood cell count (× 109/L) | 0.111 | 0.042 | 1.118 (1.030–1.213) | 0.007 |
| Renal insufficiency | 0.874 | 0.333 | 2.396 (1.247–4.604) | 0.009 |
| Transfusion of red blood cell (units) | 0.189 | 0.090 | 1.208 (1.012–1.442) | 0.036 |
| Transfusion of platelet (units) | 0.166 | 0.071 | 1.180 (1.028–1.356) | 0.019 |
| Intercept | -7.466 | 1.174 | 0.001 | < 0.001 |
AADS, Stanford type A acute aortic dissection surgery; CI, confidence interval; OR, odds ratio; POT, postoperative tracheostomy
Fig. 2.
Nomogram for predicting postoperative tracheostomy. Each red dot represents each variable value of the patient. The total point is 210, corresponding to a probability of 8.5% to develop postoperative hyperlactatemia. RBC, red blood cell
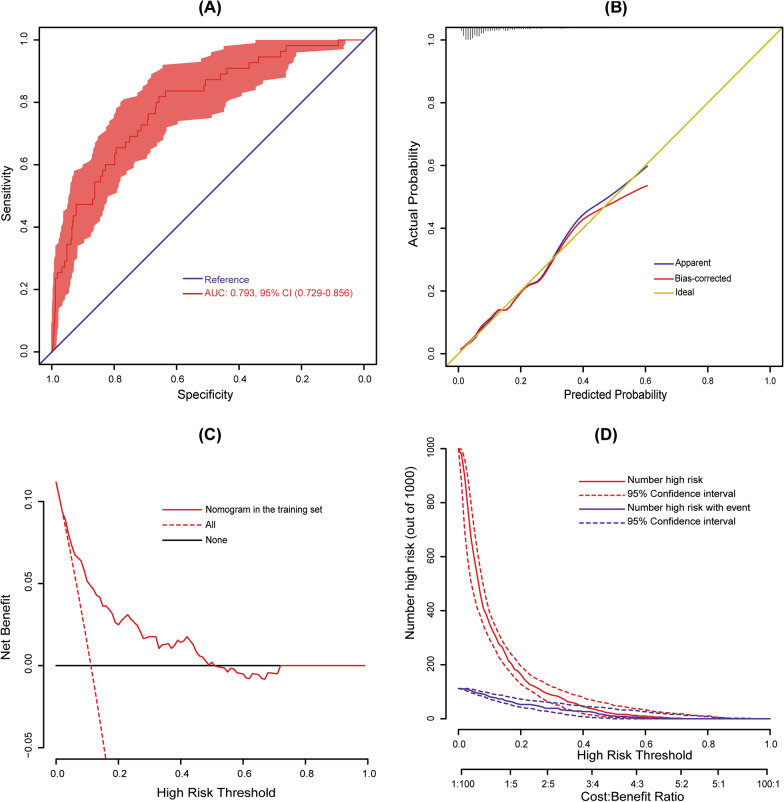
The constructed model was validated internally, and the internal validation was conducted using a bootstrap method with 1,000 resamples in our cohort. The AUC was 0.793 (95% CI 0.729–0.856), indicating good discrimination of our nomogram (Fig. 3a). The calibration plot was used to test goodness-of-fit of the model, which was well calibrated through visual inspection (Fig. 3b). The decision curve demonstrated that compared with “intervention for all” or “no intervention” strategies, our predictive model could gain more clinical net benefits when the risk threshold was set between 0.04 and 0.50 (Fig. 3c). The clinical impact curve also showed that the model had good predictive ability and clinical utility (Fig. 3d).
Fig. 3.
Assessment and validation of the nomogram. a ROC curve for the nomogram; b calibration plot of the nomogram. Ideal line represents perfect prediction that nomogram-predicted probability matches actually observed probability. c decision curves of the nomogram. Net benefit is plotted against various probability threshold; and d clinical impact curves of the nomogram. The total number of high-risk patients and the number of those with positive event are drawn against various risk threshold. ROC, receiver operating characteristic; AUC, area under the receiver operating characteristic curve; CI, confidence interval
Risk stratification
Four intervals were identified as high risk, medium, low, very low risk intervals for POT based on the total calculated scores, corresponding to estimated probabilities of 0.05, 0.1, and 0.3 (Table 3). About 8.7% patients were grouped into high risk interval with a score > 207 points. Meanwhile, 197 patients (40%) were grouped into very low risk interval with a score < 156 points. On one hand, there was no significance between the observed probability and the estimated probability in each interval, showing good consistency (Fig. 4). On the other hand, the significant differences existed between the observed probabilities or the estimated probabilities in different intervals, indicating reasonable grouping.
Table 3.
Risk intervals of POT based on the nomogram
| Risk intervals | Very low risk (< 156 points) | Low risk (156–174 points) | Medium risk (175–207 points) | High risk (> 207 points) |
|---|---|---|---|---|
| Estimated probability (%) | < 5 | 5–10 | 10–30 | > 30 |
| Observed probability, % (95% CI) | 3.0 (0.6–5.5) | 7.4 (2.7–12.1) | 16.2 (9.7–22.6) | 44.2 (28.7–59.7) |
| No. of patients (%) | 197 (40.0) | 122 (24.8) | 130 (26.5) | 43 (8.7) |
CI, confidence interval; POH, postoperative tracheostomy
Fig. 4.
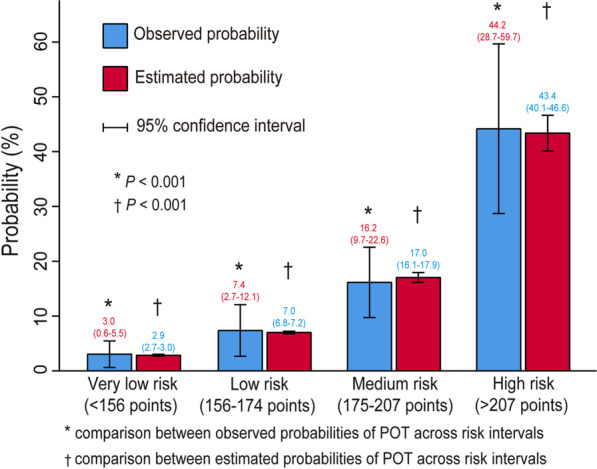
Bar chart showing the agreement between observed and estimated probabilities
Outcomes
Among the whole patients, 55 patients had a tracheostomy after AADS. Compared with that of patients without POT, the proportion of patients with POT who experienced readmission to the ICU or in-hospital death after surgery was significantly larger (P < 0.001, Table 4). Significant prolongation in ICU and hospital stays were also observed in patients receiving a tracheostomy (P < 0.05). Further propensity matching analysis was performed, and 50 patients were extracted from each group (Table 5). Except for readmission to ICU, tracheostomy was still significantly related to other adverse results.
Table 4.
Outcomes in patients with and without POT after AADS
| Variables | All patients n = 492 (%) | Without POTn = 437 (%) | With POTn = 55 (%) | χ2/Z | P value |
|---|---|---|---|---|---|
| Readmission to ICU | 44 (8.9) | 30 (6.9) | 14 (25.5) | 20.731 | < 0.001 |
| ICU stay (days) | 7 (5, 11) | 6 (5, 9) | 21 (17, 27) | 11.445 | < 0.001 |
| Hospital stay (days) | 21 (17, 27) | 21 (16, 26) | 30 (24, 42) | 6.521 | 0.049 |
| Mortality | 49 (10.1) | 29 (6.6) | 20 (36.4) | 48.142 | < 0.001 |
AADS, Stanford type A acute aortic dissection surgery; ICU, intensive care unit; POT, postoperative tracheostomy
Table 5.
Outcomes in patients with and without POT in patients undergoing AADS after propensity score matching
| Variables | Included patients n = 100 (%) | Without POT n = 50 (%) | With POT n = 50 (%) | χ2/Z | P value |
|---|---|---|---|---|---|
| Readmission to ICU | 19 (19) | 8 (16) | 11 (22) | 0.585 | 0.444 |
| ICU stay (days) | 15 (8, 21) | 8 (5, 11) | 20 (17, 26) | 7.535 | < 0.001 |
| Hospital stay (days) | 27 (19, 36) | 22 (18, 34) | 29 (23, 38) | 2.828 | 0.049 |
| Mortality | 30 (30) | 10 (20) | 20 (40) | 4.762 | 0.029 |
AADS, Stanford type A acute aortic dissection surgery; ICU, intensive care unit; POT, postoperative tracheostomy
Discussion
This study identified a rate of POT (11.2%) in patients undergoing AADS, which was similar to previously reported data [5, 10]. In addition, it may not be surprising that we found patients with a tracheostomy had increased resource utilization or in-hospital mortality following AADS compared to those without a tracheostomy. In-hospital mortality among patients treated with tracheostomies after AADS was 36.4%, which was comparable with previous results of cardiac surgical patients [11]. These findings in our study provide insight on the outcomes of the patients requiring tracheostomy after AADS, and emphasize the urgent need for early identification of these high-risk populations requiring tracheostomy.
Our study is the first to investigate the predictors of POT in patients with AADS and to build a nomogram model to predict POT. Based on the clinical data of 492 patients who underwent AADS at one institution, preoperative factors including age, cerebrovascular disease, WBC, renal insufficiency, as well as intraoperative factors including RBC and platelet transfusion, were identified to be independently associated with POT after AADS. Our predictive model was established relying on these risk factors and was validated with well predictive performance and good clinical utility. In order to better apply the model to the clinic, we further defined four levels of risk intervals to facilitate the risk stratification of patients.
The preoperative cerebrovascular disease was the risk factor (OR > 2) that contributed more to the development of requiring POT in our study. Mukerji et al. found that prior cerebrovascular disease was significantly related to increased intubation duration and lower successful extubation rate [12]. Stroke patients were at high risk of respiratory and swallowing dysfunction, and about a quarter of them required ventilatory support [13]. However, iatrogenic laryngotracheal stenosis which was commonly caused by endotracheal and/or tracheostomy tubes injury presented with a higher risk of tracheostomy dependence [14]. Our analysis also revealed the pre-existing renal insufficiency as another associated risk factor. Songdechakraiwut et al. reported that chronic renal insufficiency had 2.85-fold increased odds of POT after aortic aneurysm repair [15]. In addition, preoperative renal insufficiency has been indicated to be an important predictor of respiratory complications by Etz et al. [16]. The observed impairment of respiratory muscle strength and endurance in patients with chronic renal failure might predispose them to respiratory muscle fatigue, which may partly explain the potential association between renal insufficiency and the need for tracheostomy [17].
It was shown that the older age was correlated with increased risk of POT among our target study population, but the results of whether the probability of tracheostomy increases with age in several studies were inconsistent [8, 18, 19], and we think that this difference may be partly due to the different disease populations studied. Suzuki et al. suggested that age was negatively correlated with elevated WBC count before AADS [20]. Interestingly, our study showed that the higher the preoperative WBC count, the greater the possibility of necessitating tracheostomy after AADS. Ge et al. have identified elevated WBC count as independent risk factor for prolonged mechanical ventilation in patients undergoing AADS [21]. In addition, WBC elevation is a well-known acute-phase systemic inflammatory response in patients with aortic dissection, and it was also found to be an independent predictor of in-hospital death [20, 22]. Although the mechanism of the link between elevated WBC count and requiring POT is unclear, we speculate that it may be in relation to inflammatory damage involving the lungs induced by the acute aortic dissection. The strategy of leukocyte depletion during CPB which attenuates the CPB-induced inflammatory response by reducing endothelial activation and neutrophil transmigration can lead to improved oxygenation, earlier extubation, and shorter hospital stays [23, 24].
Previous study has suggested that a lower preoperative platelet count was a risk factor for prolonged mechanical ventilation or postoperative pneumonia [2, 25]. But the preoperative platelets of the patients who underwent POT in our study were not significantly lower. Zindovic et al. confirmed that aortic dissection caused significant activation of the coagulation system including platelet activation, while surgery caused further derangement of the hemostatic system [26], and AADS is often complicated by excessive bleeding and allogeneic blood products transfusion [27]. In our analysis, platelet transfusion was identified as an intraoperative predictor for POT, consistent with previous studies [15], they reported that more intraoperative transfusion of platelet was independently associated with increased risk of POT with an odds ratio of 1.04. Prophylactic or emergency platelets transfusion is usually used in cases of a reduction in platelet count or dysregulation in platelet function which is related to bleeding risks and hemorrhagic complications [28]. However, patients receiving platelet transfusion during surgery experienced prolonged ventilation and intensive care after cardiac surgery [29]. Kornblith et al. also indicated that platelet transfusion was a significant independent risk factor for acute respiratory distress syndrome [30]. The potential explanations for these connections may come from conclusions of some published studies, that is, platelets play an important role in the pathogenesis of acute lung injury, and the platelet transfusion-related acute lung injury was the main determinant of increased mortality [31, 32]. Nonetheless, some measures may inhibit the release of proinflammatory cytokines, reduce reperfusion lung injury and preserve lung function, such as ulinastatin administration, a urinary trypsin inhibitor during CPB [33].
Transfusions of RBC and platelets have been related to systemic inflammatory response syndrome, transfusion related acute lung injury, and mortality, leading to increased hospitalization and healthcare costs [34]. In this study, intraoperative RBC transfusion was correlated with a dose-dependent increase in the risk of POT after AADS, although RBC transfusions are used to treat hemorrhage and to improve oxygen delivery to tissues [35]. A restrictive strategy of RBC transfusion has been found to be safe in patients undergoing some surgeries of high-risk large blood loss [36–38]. The use of intraoperative autologous platelet rich plasma in patients undergoing AADS was also related to a reduction in intraoperative RBC transfusions, as well as reduced ventilation time [39]. In addition, the application of moderate hypothermic circulatory arrest and unilateral selective antegrade cerebral perfusion (MHCA/uSACP) during the AADS was shown to represent a protective factor for POT [5].
The benefits of POT may be improved by the optimal timing of it for cardiac surgical patients, whereas this optimal time point is still unclear and controversial [4, 40]. Nonetheless, our study found that the relationship between needing POT and poor outcomes was still significant after limiting any influence of selection bias and the heterogeneity in preoperative variables and surgical extent. Consideration should be given to reducing unnecessary tracheostomy for the low-risk patients needing tracheostomy after AADS. Of course, our model may help early management of high-risk patients in order to reduce the occurrence of POT, including increasing awareness of implementing more careful postoperative airway care.
Some limitations are important to acknowledge. Inasmuch as this is a single-center study with a small sample size, our predictive model may not necessarily be applicable to other centers. Meanwhile, due to the retrospective nature of the study and lacking external validation, caution must be exercised before applying our model prospectively. Additionally, the implementation of the tracheostomy was determined by the cardiac intensivists at that time, which may induce bias as well. Moreover, our model involves blood transfusion variables, but we failed to collect data such as the amount of blood lost, hemoglobin, platelet count, etc. during the operation.
Conclusion
The incidence of requiring tracheostomy among the population with AADS was 11.2% in this study. Requirement for a tracheostomy in patients after AADS was associated with significant prolonged ICU and hospital stays and increased mortality. Our study identified six significant risk factors for POT and established a new model for predicting requiring POT in patients undergoing AADS. The constructed model may enable guidance of proper prevention at the early stage and better estimation of need to perform a tracheostomy in the follow-up treatment after AADS.
Acknowledgements
Not applicable.
Abbreviations
- AADS
Stanford type A acute aortic dissection surgery
- AUC
Area under the receiver operating characteristic curve
- CI
Confidence interval
- CPB
Cardiopulmonary bypass
- ICU
Intensive care unit
- MHCA/uSACP
Moderate hypothermic circulatory arrest and unilateral selective antegrade cerebral perfusion
- OR
Odds ratio
- POT
Postoperative tracheostomy
- ROC
Receiver operating characteristic
- RBC
Red blood cell
- WBC
White blood cell
Authors' contributions
(I) Conception and design: DW, SW, and YS; (II) Administrative support: AZ, XH, PY, LW, and XD; (III) Provision of study materials or patients: LW, XH, and XD; (IV) Collection and assembly of data: DW, HW, and AZ; (V) Data analysis and interpretation: DW, SW, and YS; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. All authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (Grant Nos. 81800413, 81801586, 81974048, and 82060092), Natural Science Foundation of Hubei Province (No. 2020CFB791), and Natural Science Foundation of Xinjiang Uygur Autonomous Region of China (No. 2020D01C181).
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available because it is part of a large comprehensive study but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with ethical statement of the Declaration of Helsinki and was approved by The Ethics Committee of Tongji Medical College of Huazhong University of Science and Technology (IORG No. IORG0003571). The requirement of written informed consent was waived by The Ethics Committee of Tongji Medical College of Huazhong University of Science and Technology (IORG No. IORG0003571) due to its observational, retrospective nature.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Dashuai Wang, Su Wang and Yu Song have contributed equally to this work.
Contributor Information
Xiaofan Huang, Email: dr_xfhuang@hust.edu.cn.
Ping Ye, Email: blue314@163.com.
Xinling Du, Email: xinlingdu@hust.edu.cn.
References
- 1.De Santo LS, Romano G, Amarelli C, Onorati F, Torella M, Renzulli A, et al. Surgical repair of acute type A aortic dissection: continuous pulmonary perfusion during retrograde cerebral perfusion prevents lung injury in a pilot study. J Thorac Cardiovasc Surg. 2003;126(3):826–831. doi: 10.1016/s0022-5223(03)00583-x. [DOI] [PubMed] [Google Scholar]
- 2.Jin M, Ma WG, Liu S, Zhu J, Sun L, Lu J, et al. Predictors of prolonged mechanical ventilation in adults after acute Type-A aortic dissection repair. J Cardiothorac Vasc Anesth. 2017;31(5):1580–1587. doi: 10.1053/j.jvca.2017.03.036. [DOI] [PubMed] [Google Scholar]
- 3.Kimura N, Tanaka M, Kawahito K, Sanui M, Yamaguchi A, Ino T, et al. Risk factors for prolonged mechanical ventilation following surgery for acute type a aortic dissection. Circ J. 2008;72(11):1751–1757. doi: 10.1253/circj.cj-08-0306. [DOI] [PubMed] [Google Scholar]
- 4.Litton E, Law T, Stamp N. Tracheostomy in patients requiring prolonged mechanical ventilation after cardiac surgery. J Cardiothorac Vasc Anesth. 2019;33(1):91–92. doi: 10.1053/j.jvca.2018.07.014. [DOI] [PubMed] [Google Scholar]
- 5.Comas GM, Leshnower BG, Halkos ME, Thourani VH, Puskas JD, Guyton RA, et al. Acute type a dissection: impact of antegrade cerebral perfusion under moderate hypothermia. Ann Thorac Surg. 2013;96(6):2135–2141. doi: 10.1016/j.athoracsur.2013.06.085. [DOI] [PubMed] [Google Scholar]
- 6.Lau C, Robinson NB, Farrington WJ, Rahouma M, Gambardella I, Gaudino M, et al. A tailored strategy for repair of acute type A aortic dissection. J Thorac Cardiovasc Surg. 2021 doi: 10.1016/j.jtcvs.2020.12.113. [DOI] [PubMed] [Google Scholar]
- 7.Kollef MH, Ahrens TS, Shannon W. Clinical predictors and outcomes for patients requiring tracheostomy in the intensive care unit. Crit Care Med. 1999;27(9):1714–1720. doi: 10.1097/00003246-199909000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Graham RC, Bush WJ, Mella JS, Fridell JA, Ekser B, Mihaylov P, et al. Tracheostomy post liver transplant: predictors, complications, and outcomes. Ann Transplant. 2020;25:e920630. doi: 10.12659/aot.920630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mastropietro CW, Benneyworth BD, Turrentine M, Wallace AS, Hornik CP, Jacobs JP, et al. Tracheostomy after operations for congenital heart disease: an analysis of the society of thoracic surgeons congenital heart surgery database. Ann Thorac Surg. 2016;101(6):2285–2292. doi: 10.1016/j.athoracsur.2016.01.046. [DOI] [PubMed] [Google Scholar]
- 10.Hu Z, Wang Z, Chang J, Zhang M, Hu X, Ren Z, et al. Application of prosthesis eversion method for ascending aorta replacement guarantees better clinical outcomes of type A acute aortic dissection surgery. J Thorac Dis. 2021;13(2):533–540. doi: 10.21037/jtd-20-2578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walts PA, Murthy SC, Arroliga AC, Yared JP, Rajeswaran J, Rice TW, et al. Tracheostomy after cardiovascular surgery: an assessment of long-term outcome. J Thorac Cardiovasc Surg. 2006;131(4):830–837. doi: 10.1016/j.jtcvs.2005.09.038. [DOI] [PubMed] [Google Scholar]
- 12.Mukerji SS, Das S, Alabsi H, Brenner LN, Jain A, Magdamo C, et al. Prolonged intubation in patients with prior cerebrovascular disease and COVID-19. Front Neurol. 2021;12:642912. doi: 10.3389/fneur.2021.642912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schneider H, Hertel F, Kuhn M, Ragaller M, Gottschlich B, Trabitzsch A, et al. Decannulation and functional outcome after tracheostomy in patients with severe stroke (DECAST): a prospective observational study. Neurocrit Care. 2017;27(1):26–34. doi: 10.1007/s12028-017-0390-y. [DOI] [PubMed] [Google Scholar]
- 14.Gadkaree SK, Pandian V, Best S, Motz KM, Allen C, Kim Y, et al. Laryngotracheal stenosis: risk factors for tracheostomy dependence and dilation interval. Otolaryngol Head Neck Surg. 2017;156(2):321–328. doi: 10.1177/0194599816675323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Songdechakraiwut T, Aftab M, Chatterjee S, Green SY, Price MD, Preventza O, et al. Tracheostomy after thoracoabdominal aortic aneurysm repair: risk factors and outcomes. Ann Thorac Surg. 2019;108(3):778–784. doi: 10.1016/j.athoracsur.2019.02.063. [DOI] [PubMed] [Google Scholar]
- 16.Etz CD, Di Luozzo G, Bello R, Luehr M, Khan MZ, Bodian CA, et al. Pulmonary complications after descending thoracic and thoracoabdominal aortic aneurysm repair: predictors, prevention, and treatment. Ann Thorac Surg. 2007;83(2):S870–6. doi: 10.1016/j.athoracsur.2006.10.099. [DOI] [PubMed] [Google Scholar]
- 17.Bark H, Heimer D, Chaimovitz C, Mostoslovski M. Effect of chronic renal failure on respiratory muscle strength. Respiration. 1988;54(3):153–161. doi: 10.1159/000195516. [DOI] [PubMed] [Google Scholar]
- 18.Mu Z, Zhang Z. Risk factors for tracheostomy after traumatic cervical spinal cord injury. J Orthop Surg (Hong Kong) 2019;27(3):2309499019861809. doi: 10.1177/2309499019861809. [DOI] [PubMed] [Google Scholar]
- 19.Humble SS, Wilson LD, McKenna JW, Leath TC, Song Y, Davidson MA, et al. Tracheostomy risk factors and outcomes after severe traumatic brain injury. Brain Inj. 2016;30(13–14):1642–1647. doi: 10.1080/02699052.2016.1199915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suzuki K, Kimura N, Mieno M, Hori D, Sezai A, Yamaguchi A, et al. Factors related to white blood cell elevation in acute type A aortic dissection. PLoS ONE. 2020;15(2):e0228954. doi: 10.1371/journal.pone.0228954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ge M, Wang Z, Chen T, Cheng Y, Ye J, Lu L, et al. Risk factors for and outcomes of prolonged mechanical ventilation in patients received DeBakey type I aortic dissection repairment. J Thorac Dis. 2021;13(2):735–742. doi: 10.21037/jtd-20-2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang R, Chen S, Zhang H, Wang W, Xing J, Wang Y, et al. Biomarkers investigation for in-hospital death in patients with stanford Type A acute aortic dissection. Int Heart J. 2016;57(5):622–626. doi: 10.1536/ihj.15-484. [DOI] [PubMed] [Google Scholar]
- 23.Chen YF, Tsai WC, Lin CC, Tsai LY, Lee CS, Huang CH, et al. Effect of leukocyte depletion on endothelial cell activation and transendothelial migration of leukocytes during cardiopulmonary bypass. Ann Thorac Surg. 2004;78(2):634–42. doi: 10.1016/j.athoracsur.2004.02.091. [DOI] [PubMed] [Google Scholar]
- 24.Patel AN, Sutton SW, Livingston S, Patel A, Hunley EK, Hebeler RF, et al. Clinical benefits of leukocyte filtration during valve surgery. Am J Surg. 2003;186(6):636–9. doi: 10.1016/j.amjsurg.2003.09.001. [DOI] [PubMed] [Google Scholar]
- 25.Yao R, Liu X, He Y, Mei C, Shen Y, Zhan Q, et al. Low platelet count is a risk factor of postoperative pneumonia in patients with type A acute aortic dissection. J Thorac Dis. 2020;12(5):2333–2342. doi: 10.21037/jtd.2020.03.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zindovic I, Sjögren J, Bjursten H, Ingemansson R, Ingimarsson J, Larsson M, et al. The coagulopathy of acute Type A aortic dissection: a prospective. Observ Study J Cardiothorac Vasc Anesth. 2019;33(10):2746–2754. doi: 10.1053/j.jvca.2019.02.013. [DOI] [PubMed] [Google Scholar]
- 27.Guan XL, Wang XL, Liu YY, Lan F, Gong M, Li HY, et al. Changes in the hemostatic system of patients with acute aortic dissection undergoing aortic arch surgery. Ann Thorac Surg. 2016;101(3):945–951. doi: 10.1016/j.athoracsur.2015.08.047. [DOI] [PubMed] [Google Scholar]
- 28.Luc NF, Rohner N, Girish A, Didar Singh Sekhon U, Neal MD, SenGupta A. Bioinspired artificial platelets: past, present and future. Platelets. 2021: doi: 10.1080/09537104.2021.1967916. [DOI] [PMC free article] [PubMed]
- 29.van Hout FM, Hogervorst EK, Rosseel PM, van der Bom JG, Bentala M, van Dorp EL, et al. Does a platelet transfusion independently affect bleeding and adverse outcomes in cardiac surgery? Anesthesiology. 2017;126(3):441–449. doi: 10.1097/aln.0000000000001518. [DOI] [PubMed] [Google Scholar]
- 30.Kornblith LZ, Robles AJ, Conroy AS, Redick BJ, Howard BM, Hendrickson CM, et al. Predictors of postinjury acute respiratory distress syndrome: lung injury persists in the era of hemostatic resuscitation. J Trauma Acute Care Surg. 2019;87(2):371–378. doi: 10.1097/ta.0000000000002331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zarbock A, Ley K. The role of platelets in acute lung injury (ALI) Front Biosci (Landmark Ed) 2009;14:150–158. doi: 10.2741/3236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pereboom IT, de Boer MT, Haagsma EB, Hendriks HG, Lisman T, Porte RJ. Platelet transfusion during liver transplantation is associated with increased postoperative mortality due to acute lung injury. Anesth Analg. 2009;108(4):1083–1091. doi: 10.1213/ane.0b013e3181948a59. [DOI] [PubMed] [Google Scholar]
- 33.Bingyang J, Jinping L, Mingzheng L, Guyan W, Zhengyi F. Effects of urinary protease inhibitor on inflammatory response during on-pump coronary revascularization. Effect of ulinastatin on inflammatory response. J Cardiovasc Surg (Torino). 2007;48(4):497–503. [PubMed] [Google Scholar]
- 34.Valeri CR, Ragno G. An approach to prevent the severe adverse events associated with transfusion of FDA-approved blood products. Transfus Apher Sci. 2010;42(3):223–233. doi: 10.1016/j.transci.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 35.Sharma S, Sharma P, Tyler LN. Transfusion of blood and blood products: indications and complications. Am Fam Physician. 2011;83(6):719–724. [PubMed] [Google Scholar]
- 36.Naeem SS, Sodha NR, Sellke FW, Ehsan A. Impact of packed red blood cell and platelet transfusions in patients undergoing dissection repair. J Surg Res. 2018;232:338–345. doi: 10.1016/j.jss.2018.06.048. [DOI] [PubMed] [Google Scholar]
- 37.Mazer CD, Whitlock RP, Fergusson DA, Hall J, Belley-Cote E, Connolly K, et al. Restrictive or liberal red-cell transfusion for cardiac surgery. N Engl J Med. 2017;377(22):2133–2144. doi: 10.1056/NEJMoa1711818. [DOI] [PubMed] [Google Scholar]
- 38.Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman BR, Rhoads GG, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365(26):2453–2462. doi: 10.1056/NEJMoa1012452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sandhu HK, Tanaka A, Dahotre S, Charlton-Ouw KM, Miller CC, 3rd, Estrera AL, et al. Propensity and impact of autologous platelet rich plasma use in acute type A dissection. J Thorac Cardiovasc Surg. 2020;159(6):2288–97. doi: 10.1016/j.jtcvs.2019.04.111. [DOI] [PubMed] [Google Scholar]
- 40.Devarajan J, Vydyanathan A, Xu M, Murthy SM, McCurry KR, Sessler DI, et al. Early tracheostomy is associated with improved outcomes in patients who require prolonged mechanical ventilation after cardiac surgery. J Am Coll Surg. 2012;214(6):1008–16.e4. doi: 10.1016/j.jamcollsurg.2012.03.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available because it is part of a large comprehensive study but are available from the corresponding author on reasonable request.