Abstract
Background and Aims:
An enlarged gastrojejunal anastomosis (GJA) is associated with weight regain after Roux-en-Y (RYGB) and can be corrected with endoscopic (ENDO) or surgical (SURG) revision; however, there has been no direct comparison between techniques. This study aims to compare serious adverse event (SAE) rates and weight loss profiles between ENDO and SURG revisional techniques over a 5-year period.
Methods:
Retrospective matched cohort study of RYGB patients who underwent ENDO or SURG revision for weight regain with an enlarged GJA (>12 mm). ENDO patients were matched 1:1 to SURG patients based on completion of 5-year follow-up, age, sex, body mass index (BMI), initial weight loss, and weight regain. Demographics, GJA size, SAEs, and weight profiles were collected. The primary outcome was comparison of SAE rates between groups. Secondary outcomes included weight loss comparisons. A Fisher exact test was used to compare the SAE rate, and a Student t-test was used for weight comparisons.
Results:
Sixty-two RYGB patients with weight regain and an enlarged GJA (31 ENDO, 31 matched SURG) were included. Baseline characteristics were similar between groups. The adverse event rate in the ENDO group (6.5%) was lower than the SURG group (29.0%); p=0.043. There was a total of 0 (0%) and 6 (19.4%) serious (severe) adverse events in the ENDO and SURG groups, respectively (p=0.02). There was no significant difference in weight loss at 1, 3, and 5 years.
Conclusions:
Endoscopic revision of the gastrojejunal anastomosis is associated with significantly fewer total and severe adverse events and similar long-term weight loss when compared with surgical revision.
Keywords: Roux-en-Y gastric bypass, weight regain, recidivism, transoral outlet reduction (TORe), restorative obesity surgery endoluminal (ROSE), revisional bariatric surgery, limb lengthening
Introduction:
The Roux-en-Y gastric bypass (RYGB) is one of the most commonly performed bariatric surgeries worldwide 1 and is effective at reversing components of the metabolic syndrome, including waist circumference reduction, type 2 diabetes mellitus, hypertension, and hypertriglyceridemia 2. This primarily results from large weight loss after the procedure, with total weight loss between 25% to 30% and excess weight loss between 57% to 68.3% at 5 years 3–6. Despite successful weight loss after RYGB, weight regain in subsequent years is common 7, with an average of 20% to 30% of pre-bypass weight regained at 10 years after the initial operation. Nearly one-third of individuals regain almost their entire pre-bypass weight 8. There are often multifactorial etiologies to weight regain, including anatomic, medical, behavioral and psychosocial factors 9–11. One of the anatomic causes is dilation or incompetence of the gastrojejunal anastomosis (GJA), particularly when the diameter is greater than 15 mm to where as much as 8% of percent maximal weight loss is regained for every 10 mm increase in GJA diameter measured at 5 years post-RYGB 12, 13. When GJA incompetence or dilation occurs, repair with diameter reduction has been demonstrated through both endoscopic and surgical approaches 14, 15.
The transoral outlet reduction (TORe) is an endoscopic procedure performed with endoscopic suturing of the GJA tightened around a 6 to 10 mm balloon, which has been shown to be safe and technically feasible 15, 16. Although variable suture patterns are performed, the purse-string pattern has been associated with the greatest weight loss 17. Adverse event rates after TORe have been reported between 5% and 11.4% 18, 19 and total weight loss as high as 8.8% at 5 years 19. Contrarily, prior surgical GJA revision has been associated with successful weight loss, however major adverse event rates between 8% and 50% 20, 21. Despite its proven safety and efficacy, long-term comparison of TORe safety and weight loss success to surgical GJA revision remains unknown. The primary aim of this study was to compare the safety of the endoscopic Transoral Outlet Reduction (TORe) to surgical GJA revision for the indication of weight regain after prior Roux-en-Y gastric bypass (RYGB). The secondary aim was to evaluate the efficacy of inducing weight loss after TORe compared with surgical GJA revision.
Methods:
Study design
This was a retrospective matched cohort study of RYGB patients with weight regain, at least partially attributable to an incompetent or dilated GJA22, who underwent endoscopic TORe (ENDO) or surgical GJA revision (SURG) treatment at 2 tertiary referral centers. These 2 groups were followed over a 5-year duration from an index date of GJA revision. A patient search was systematically performed using a large Research Patient Data Registry (RPDR) to identify patients who previously underwent treatment for weight regain after RYGB due to an incompetent or dilated GJA. All patients were sequentially included within the original database, which was reported previously19. From this database, matching to surgical patients was performed as described below. Of note, patients included in the endoscopy cohort were previously included in a five-year follow-up study without comparison group 19. Institutional Review Board approval was obtained for retrospective review of data used in this study (approval number: 2003P-001597, renewed approval on 05/08/2020).
ENDO patients were matched 1:1 to SURG patients based on completion of 5-year follow-up, age within 7 years, sex, body mass index (BMI) within 5 kg/m2, initial percentage of total weight loss (%TWL) between RYGB and nadir weight within 10%, and weight regain within 5%. Weight regain was calculated as the percentage of weight that was regained from the initial postoperative total weight loss (between preoperative weight and postoperative nadir). Patient demographics, GJA size, adverse events, and weight parameters were obtained. The inclusion of trainee participation was recorded as all patient interventions were performed at 2 large academic teaching hospitals. Adult patients were included if they were >18 years of age, had received a diagnosis of weight regain or inadequate weight loss after RYGB at least partially attributable to an incompetent or dilated GJA, and had undergone either endoscopic or surgical GJA rvision. At our institution, patients are eligible for bypass revision if they have regained ≥15% of initial maximum weight loss (%TWL after the initial operation) and are at least 2 years postoperative. To date, there are no universal definitions; however, these parameters have been referenced previously 19. Patients were excluded if they underwent endoscopic or surgical revision for an alternative cause of weight regain, such as gastrogastric fistula or limb lengthening.
Outcome Measures
The primary outcome was comparison of adverse event rates between groups. Adverse events were delineated based on validated reporting standards. The American Society for Gastrointestinal Endoscopy (ASGE) lexicon for reporting endoscopic adverse events was referenced to delineate adverse events of interest 23. This lexicon was developed through consultation with members from the National Surgical Quality Improvement Program (NSQIP) 24, which has been embraced among surgical specialties as a platform for adverse event reporting 25. “Early” adverse events were characterized as those occurring within 30 days after revision, compared with “late” adverse events, which are those that occurred beyond 30 days. Secondary outcomes included comparisons of the amount of weight loss, reported using absolute weight loss (kg), body mass index (BMI; kg/m2), percentage of total weight loss (%TWL) and percentage of excess weight loss (%EWL) at 1, 3, and 5 years after gastric bypass revision. Weight at time of revision served as the index weight used for calculation of the follow-up weight parameters.
Statistical Analysis
Standard statistical analyses were used. Specifically, a Fisher exact test was used to compare rate of adverse events and Student t-test was used for weight comparisons. Statistical significance was noted when p-values were <0.05. Statistical analyses were performed using SAS software, version 9.4 (SAS Institute, NC, USA).
Results:
Baseline Characteristics
A total of 62 RYGB patients (31 ENDO, 31 matched SURG) were included for analysis. All participants in both groups completed 5-year follow-up. Baseline cohort characteristics are shown in Table 1. Mean (SD) age was 48.6 (9.5) years in the ENDO group compared with 48.1 (8.4) years in SURG (p=0.84). Both groups contained 26 (83.9%) females (p=1.0). The mean (SD) duration between RYGB and date of GJA revision was 9.1 (3.2) and 6.7 (4.1) years in the ENDO and SURG groups, respectively (p=0.01). Percent initial total weight loss (%TWL) after RYGB was 40.8 (8.7) and 37.1 (12.7) in the ENDO and SURG groups, respectively (p=0.2). Percent weight regain from initial lost weight after RYGB was similar between groups; 52.8% (34.1) in ENDO and 55.3% (29.5) in SURG (p=0.77). Weight and BMI before revision was 111.1 (29.3) kg and 40.5 (9.4) kg/m2 in the ENDO group and 114.6 (30.2) kg (p=0.65) and 41.5 (9.1) kg/m2 (p=0.68) in the SURG group. The mean GJA diameter in the ENDO group (n=31) was 24.4 (6.4) mm and GJA diameter within the SURG group (n=10) was 19.6 (1.2) mm (p=0.03). All endoscopic procedures had trainee involvement (n=31; 100%) compared with 29 (93.5%) in the surgical group.
Table 1:
Baseline characteristics of endoscopic and surgical cohorts
| Demographics at time of revision | Endoscopic (n=31) | Surgical (n=31) | P value |
|---|---|---|---|
| Age – years | 48.6 (9.5) | 48.1 (8.4) | 0.84 |
| Female – n (%) | 26 (83.9) | 26 (83.9) | 1.0 |
| Time since RYGB – years | 9.1 (3.2) | 6.7 (4.1) | 0.01 |
| Percent of total weight loss between RYGB and nadir – % | 40.8 (8.7) | 37.1 (12.7) | 0.2 |
| Percent weight regain from initial post-bypass loss – % | 52.8 (34.1) | 55.3 (29.5) | 0.77 |
| Weight prerevision – kg | 111.1 (29.3) | 114.6 (30.3) | 0.65 |
| BMI prerevision – kg/m2 | 40.5 (9.4) | 41.5 (9.1) | 0.68 |
Presented as mean (standard deviation). RYGB: Roux-en-Y gastric bypass. BMI: body mass index.
Procedural Techniques
All patients who underwent endoscopic revision received sedation with general anesthesia and CO2 insufflation was used throughout the procedure. Endoscopic examination was performed using a standard upper endoscope to confirm the presence of a dilated or incompetent gastrojejunal anastomosis, lack of contraindications such as active gastric or jejunal ulceration and administer simethicone 120mL approximately 90 cm distal to the GJA within the Roux limb. An overtube was then placed, followed by application of argon plasma coagulation (APC) in a circumferential pattern surrounding the GJA to reduce tissue compliance and enhance tissue strength for suturing. The endoscope was then exchanged for a dual-channel therapeutic endoscope with the Apollo Overstitch device (Apollo Endosurgery, Austin, Tex, USA). Either interrupted sutures or a circumferential purse-string pattern was deployed around the GJA and the suture tightened around a 6 to 10 mm dilator balloon before cinching. This was followed by placement of simple interrupted stitches (1–2) within the gastric pouch for reinforcement when feasible.
All patients who underwent surgical revision received sedation with general anesthesia. Patient positioning and decision between a laparoscopic and open approach were dependent on surgeon preference and patient anatomy. Multiple techniques were deployed; however, all patients underwent revision of the gastrojejunal anastomosis with either oversewing of present GJA (n=5) or resection and creation of a new GJA using hand sewing or stapler techniques (n=26). Among oversewn GJA cases, 3 were laparotomies and 2 were laparoscopies. Among new GJA cases, 11 were laparotomies and 15 were laparoscopies. Additionally, gastric pouch shortening was performed in 21 (60%) of new GJA cases and 5 (100%) of cases who received oversewing of the existing GJA.
Adverse Events
The overall adverse event rate was significantly lower in the ENDO group than the SURG group (6.5% vs 29.0%; p=0.04) (Table 2). When comparing adverse event rates across hospitals where surgical revisions were performed, there was no difference between sites (p=0.78). SAEs within the ENDO group included GJA stenosis requiring balloon dilation (1) and gastrointestinal bleeding (1). SAEs within the SURG group included leak (3), GJA stenosis requiring balloon dilation (2), ulcer (1), gastrointestinal bleeding (1), incarcerated incisional hernia (1), and high-grade small-bowel obstruction (1). Regarding severity, there were a total of 0 (0%) and 6 (19.4%) serious (severe) adverse events in the ENDO and SURG groups, respectively (p=0.02). These included postoperative leak (3), incarcerated incisional hernia (1), deep abdominal wall abscess (1), and high-grade SBO (1) in the SURG group. A total of 1 (2.9%) adverse event was considered early in the ENDO group, whereas 7 (22.3%) were early in the SURG group (p=0.53).
Table 2:
Adverse event rate comparison
| Outcome | ENDO (n=31) |
SURG (n=31) |
P value |
|---|---|---|---|
|
| |||
| AE – n (%) | 2 (6.5) | 9 (29) | 0.043 |
| Gastrointestinal leak/perforation | 0 | 3 (9.7) | |
| Ulcer | 0 | 1 (3.2) | |
| GJA stenosis | 1 (3.2) | 2 (6.5) | |
| Gastrointestinal bleeding | 1 (3.2) | 1 (3.2) | |
| Small-bowel obstruction | 0 | 1 (3.2) | |
| Incarcerated incisional hernia | 0 | 1 (3.2) | |
|
| |||
| Serious adverse events – n (%) | 0 | 6 (19.4) | 0.024 |
|
| |||
| Early adverse events – n (%) | 1 (3.2) | 7 (22.3) | 0.53 |
Adverse event rate comparison between endoscopic and surgical GJA revision. AE: Adverse Event. GJA: Gastrojejunal anastomosis. Serious adverse events determined in reference to the American Society for Gastrointestinal Endoscopy (ASGE) lexicon for reporting endoscopic adverse events 23 and the National Surgical Quality Improvement Program (NSQIP) 25. Early events defined as those which occurred within 30 days of revision.
Weight Loss
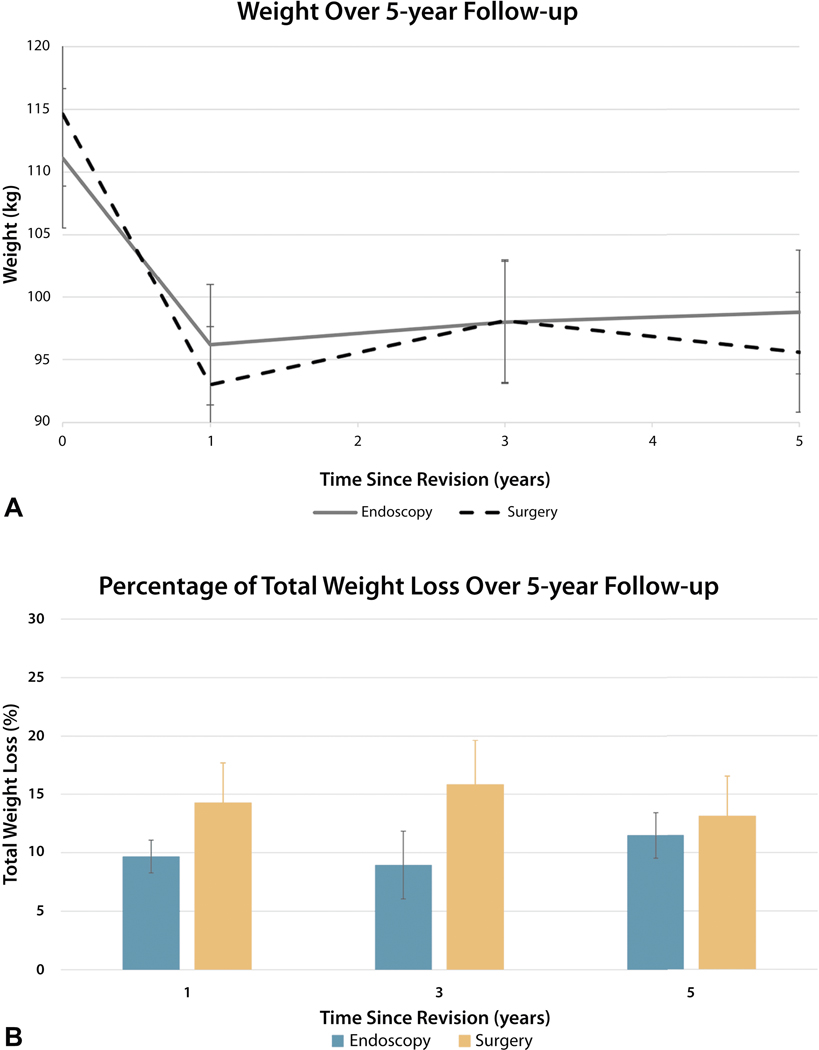
When comparing weight loss parameters, ENDO patients experienced similar weight loss to SURG patients at 1, 3 and 5 years (Figure 1). At 1-year, the weight parameters for ENDO and SURG groups were weight (94.1 vs 96.9 kg; p=0.71), BMI (34.6 vs 35.1 kg/m2; p=0.82) absolute weight loss (10.8 vs 17.6 kg; p=0.16), %TWL (9.7% vs 14.3%; p=0.20) and %EWL (13.2 vs 18.6%; p=0.25). At 3-years, the weight parameters for ENDO and SURG groups were weight (101.1 vs 97.2 kg p=0.62), BMI (36.9 vs 35.2 kg/m2; p=0.47) absolute weight loss (11.2 vs 16.5 kg; p=0.32), %TWL (8.6% vs 15.8%; p=0.09) and %EWL (11.9% vs 19.5%; p=0.14). At 5-year follow-up, the weight parameters for ENDO and SURG groups were weight (97.2 vs 99.7 kg; p=0.71), BMI (35.4 vs 35.9 kg/m2; p=0.83), absolute weight loss (13.9 vs 14.3 kg; p=0.93), %TWL (11.5% vs 13.1%; p=0.67), and %EWL (15.4% vs 15.8%; p=0.92).
Figure 1:
Weight loss during 5-year follow-up. A, Mean (95% confidence interval) weights (kg) in ENDO and SURG groups during 5-year follow-up. B, Mean (standard error) percentage of total weight loss (%) in ENDO and SURG groups over 5-year follow-up.
Discussion:
Gastrojejunal anastomosis incompetence or dilation is a common cause for weight regain after Roux-en-Y Gastric bypass and can be treated through either endoscopic or surgical techniques. The present study demonstrates that endoscopy is associated with significantly fewer overall and severe adverse events than the surgical approach. Furthermore, there were no observed severe (serious) adverse events within the endoscopy group, highlighting endoscopic TORe as a reproducible and safe procedure. Although this is likely multifactorial, a major benefit to the endoscopic approach is access to the treatment area (ie, GJA) with less impediment from anatomical barriers such as adhesions, which commonly occur around surgical sites such as the GJA. The adverse events associated with endoscopic revision tend to occur earlier and respond well to targeted therapies 19, whereas surgical adverse events, such as tissue ischemia, marginal ulceration or incisional hernia, tend to have a more protracted course 21, 26.
Additionally, weight loss between the 2 modalities appears to be similar at 1, 3, and 5 years. In considering these results, endoscopic revision may serve as a more favorable approach with safer risk profile as compared with surgical revision of the GJA. Nevertheless, surgical limb distalization would be a reasonable consideration in patients who fail to lose adequate weight after endoscopic revision, or when the GJA is not thought to be a major contributor to weight regain27.
There are a few limitations to consider. First, this is a retrospective comparison with risk for inherent limitations associated with this study design. A specific concern is that patient selection may be at least partially subject to confounding by indication as the presence of few or many comorbidities may dictate whether an individual received an endoscopic or surgical intervention. However, given a propensity for sicker patients to undergo less-invasive alternatives to surgery, confounding would be expected to bias the adverse event rate difference toward the null as opposed to favor endoscopy, as demonstrated in this study. Furthermore, this approach likely reflects broad clinical practice patterns as collaborative decision-making often occurs between medical and surgical specialties. Second, both endoscopic and surgical GJA revision techniques require experienced proceduralists in specialty centers, which therefore may affect generalizability of these results. Finally, a minority of the surgical cohort had GJA diameter size measurements, limiting our ability to match based on that parameter. Despite these limitations, this study has primary strengths including a direct comparison between endoscopic and surgical techniques and contains a large number of patients followed for 5 years compared with relatively smaller prior studies, particularly within the surgical literature.
In conclusion, endoscopic revision of the gastrojejunal anastomosis has an improved safety profile, with fewer total and serious adverse events, compared with surgical revision yet provides similar long-term weight loss.
ACRONYMS
- (AE)
Adverse Event
- (APC)
Argon plasma coagulation
- (ASGE)
American Society for Gastrointestinal Endoscopy
- (BMI)
Body Mass Index
- (ENDO)
Endoscopic
- (GJA)
Gastrojejunal Anastomosis
- (NSQIP)
National Surgical Quality Improvement Program
- (ROSE)
Restorative Obesity Surgery Endoluminal
- (RYGB)
Roux-en-Y Gastric Bypass
- (SAE)
Serious adverse event
- (SURG)
Surgical
- (TORe)
Transoral Outlet Reduction
- (%TWL)
Percentage of total weight loss
- (%EWL)
Percentage of excess weight loss
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.English WJ, DeMaria EJ, Brethauer SA, Mattar SG, Rosenthal RJ, Morton JM. American Society for Metabolic and Bariatric Surgery estimation of metabolic and bariatric procedures performed in the United States in 2016. Surg Obes Relat Dis 2018;14:259–263. [DOI] [PubMed] [Google Scholar]
- 2.Junges VM, Cavalheiro JM, Fam EF, Closs VE, Moraes JF, Gottlieb MG. Impact of Roux-en-Y gastric bypass surgery (RYGB) on metabolic syndrome components and on the use of associated drugs in obese patients. Arq Gastroenterol 2017;54:139–144. [DOI] [PubMed] [Google Scholar]
- 3.Arterburn D, Wellman R, Emiliano A, et al. Comparative Effectiveness and Safety of Bariatric Procedures for Weight Loss: A PCORnet Cohort Study. Ann Intern Med 2018;169):741–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maciejewski ML, Arterburn DE, Van Scoyoc L, et al. Bariatric Surgery and Long-term Durability of Weight Loss. JAMA Surg 2016;151:1046–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peterli R, Wölnerhanssen BK, Peters T, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: the SM-BOSS randomized clinical trial. Jama 2018;319:255–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salminen P, Helmiö M, Ovaska J, et al. Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss at 5 years among patients with morbid obesity: the SLEEVEPASS randomized clinical trial. Jama 2018;319:241–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adams TD, Davidson LE, Litwin SE, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med 2017;377:1143–1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 2007;357:741–52. [DOI] [PubMed] [Google Scholar]
- 9.van Hout GC, Verschure SK, van Heck GL. Psychosocial predictors of success following bariatric surgery. Obes Surg 2005;15:552–60. [DOI] [PubMed] [Google Scholar]
- 10.Perugini RA, Mason R, Czerniach DR, et al. Predictors of complication and suboptimal weight loss after laparoscopic Roux-en-Y gastric bypass: a series of 188 patients. Arch Surg 2003;138:541–5; discussion 545–6. [DOI] [PubMed] [Google Scholar]
- 11.Odom J, Zalesin KC, Washington TL, et al. Behavioral predictors of weight regain after bariatric surgery. Obes Surg 2010;20:349–56. [DOI] [PubMed] [Google Scholar]
- 12.Kumar N, Thompson CC. Transoral outlet reduction for weight regain after gastric bypass: long-term follow-up. Gastrointest Endosc 2016;83:776–9. [DOI] [PubMed] [Google Scholar]
- 13.Abu Dayyeh BK, Lautz DB, Thompson CC. Gastrojejunal stoma diameter predicts weight regain after Roux-en-Y gastric bypass. Clin Gastroenterol Hepatol 2011;9:228–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.León F, Maiz C, Daroch D, et al. Laparoscopic hand-sewn revisional gastrojejunal plication for weight loss failure after Roux-en-Y gastric bypass. Obes Surg 2015;25:744–9. [DOI] [PubMed] [Google Scholar]
- 15.Jirapinyo P, Kröner PT, Thompson CC. Purse-string transoral outlet reduction (TORe) is effective at inducing weight loss and improvement in metabolic comorbidities after Roux-en-Y gastric bypass. Endoscopy 2018;50:371–377. [DOI] [PubMed] [Google Scholar]
- 16.Thompson CC, Chand B, Chen YK, et al. Endoscopic suturing for transoral outlet reduction increases weight loss after Roux-en-Y gastric bypass surgery. Gastroenterology 2013;145:129–137.e3. [DOI] [PubMed] [Google Scholar]
- 17.Schulman AR, Kumar N, Thompson CC. Transoral outlet reduction: a comparison of purse-string with interrupted stitch technique. Gastrointest Endosc 2018;87:1222–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dhindsa BS, Saghir SM, Naga Y, et al. Efficacy of transoral outlet reduction in Roux-en-Y gastric bypass patients to promote weight loss: a systematic review and meta-analysis. Endosc Int Open 2020;8:E1332-e1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jirapinyo P, Kumar N, AlSamman MA, Thompson CC. Five-year outcomes of transoral outlet reduction for the treatment of weight regain after Roux-en-Y gastric bypass. Gastrointest Endosc 2020;91:1067–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hamdi A, Julien C, Brown P, et al. Midterm outcomes of revisional surgery for gastric pouch and gastrojejunal anastomotic enlargement in patients with weight regain after gastric bypass for morbid obesity. Obes Surg 2014;24:1386–90. [DOI] [PubMed] [Google Scholar]
- 21.Schwartz RW, Strodel WE, Simpson WS, Griffen WO Jr., Gastric bypass revision: lessons learned from 920 cases. Surgery 1988;104:806–12. [PubMed] [Google Scholar]
- 22.Thompson CC, Jacobsen GR, Schroder GL, Horgan S. Stoma size critical to 12-month outcomes in endoscopic suturing for gastric bypass repair. Surg Obes Relat Dis 2012;8:282–7. [DOI] [PubMed] [Google Scholar]
- 23.Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 2010;71:446–54. [DOI] [PubMed] [Google Scholar]
- 24.American College of Surgeons National Surgical Quality Improvement Program. December 11, 2020. www.acsnsqip.org.
- 25.Ko CY, Hall BL, Hart AJ, Cohen ME, Hoyt DB. The American College of Surgeons National Surgical Quality Improvement Program: achieving better and safer surgery. Jt Comm J Qual Patient Saf 2015;41:199–204. [DOI] [PubMed] [Google Scholar]
- 26.Tran DD, Nwokeabia ID, Purnell S, et al. Revision of Roux-En-Y Gastric Bypass for Weight Regain: a Systematic Review of Techniques and Outcomes. Obes Surg 2016;26:1627–34. [DOI] [PubMed] [Google Scholar]
- 27.Shin RD, Goldberg MB, Shafran AS, Shikora SA, Majumdar MC. Revision of Roux-en-Y Gastric Bypass with Limb Distalization for Inadequate Weight Loss or Weight Regain. Obes Surg 2019;29:811–818. [DOI] [PubMed] [Google Scholar]