Abstract
BACKGROUND:
Devolution of healthcare services in Kenya resulted in a large number of newly recruited tuberculosis (TB) coordinators. We describe a unique collaboration between a national tuberculosis program (NTP), a local, and an international non-governmental organization to build human resource capacity in TB care and prevention.
METHODS:
From 2016 to 2021, the Kenya Division of National Tuberculosis, Leprosy and Lung Disease Program, Centre for Health Solutions-Kenya, and the International Union Against Tuberculosis and Lung Disease developed and conducted a series of 7-day training courses. A key focus of training was the introduction of TBData4Action, an approach involving the local use of routinely available data to strengthen decision-making and support supervision.
RESULTS:
Implementation outcomes included training 331 (96%) coordinators out of 344, representing all 47 counties, 37 national officers and 21 other stakeholders using the country-tailored curriculum, including hands-on group work by county teams and field practicals. Thirty-five national facilitators were identified and mentored as local faculty. Training costs were reduced by 75% compared with international alternatives.
CONCLUSION:
The collaboration resulted in the training of the majority of the coordinators in a standardized approach to TB care. A sustainable approach to capacity building in local data use was found feasible; the model could be adapted by other NTPs.
Keywords: local data use; sub-national, devolution; capacity building; Africa
Abstract
CONTEXTE :
La décentralisation des services de santé au Kenya a conduit au recrutement d’un grand nombre de nouveaux coordinateurs TB. Nous décrivons une collaboration unique entre un programme national de lutte contre la TB (NTP), une organisation non gouvernementale locale et une organisation non gouvernementale internationale visant à renforcer les capacités humaines en matière de prévention et de soins de la TB.
MÉTHODES :
De 2016 à 2021, la division kényane du programme national de lutte contre la tuberculose, la lèpre et les maladies respiratoires, le Centre for Health Solutions-Kenya et l’Union internationale contre la tuberculose et les maladies respiratoires ont développé et dispensé une série de formations en 7 jours. La formation mettait l’accent sur l’introduction de l’approche TBData4Action, qui promeut une utilisation locale des données disponibles en routine afin de renforcer la prise de décision et d’épauler les activités de supervision.
RÉSULTATS :
Les résultats de la mise en place de cette formation comprenaient la formation de 331 (96%) coordinateurs sur 344, représentant l’ensemble des 47 pays, 37 administrateurs nationaux et 21 autres acteurs formés à l’aide du programme adapté aux besoins du pays concerné (dont travail de groupe pratique par les équipes nationales et travaux pratiques sur le terrain). Trente-cinq facilitateurs nationaux ont été identifiés et formés comme enseignants locaux. Les coûts de la formation ont été réduits de 75% par rapport aux alternatives internationales.
CONCLUSION :
La collaboration a permis de former la majorité des coordinateurs à l’aide d’une approche standardisée de soins de la TB. Une approche durable de renforcement des capacités en matière d’utilisation des données locales s’est avérée réalisable. Ce modèle peut être adapté à d’autres NTP.
Kenya ranks among the highest burden countries globally for TB, HIV-associated TB and multi-drug-resistant TB.1 The Kenya Division of National Tuberculosis, Leprosy and Lung Disease Program (DNTLD-P) was established in 1980.2 Kenya experienced a peak in TB notifications in 2006 at 116,723, followed by a decline to about 76,000 in 2016.3 DNTLD-P addressed the peak through aggressive pro-grammatic management of TB-HIV co-infection and early adoption (2011) of rapid molecular testing, increasing both bacteriological confirmation and and detection of rifampicin-resistant TB.4–6 The 2016 national prevalence survey, however, demonstrated an unexpectedly high TB prevalence of 558/100,000 population with a TB treatment coverage of only 45%.7
In 2013, the devolution of the Kenyan healthcare services resulted in a change from a provincial TB management structure with 12 provincial TB coordinators to a county structure, with 47 county TB and leprosy coordinators (CTLCs), and decentralized TB planning, implementation and funding of TB control programs.8,9 Many of the new county and sub-county coordinators (SCTLCs) had varying levels of competence in TB care and prevention and in sub-national programming. The DNTLD-P in collaboration with the Centre for Health Solutions-Kenya (CHS; Nairobi, Kenya) through the USAID-supported TB Accelerated Response and Care (TB ARC) activity proposed to fill this training gap through a country-wide, standardized training program.
One of the work pillars of the International Union Against Tuberculosis and Lung Disease (The Union; Paris, France) is training, particularly in TB and lung health. For decades, The Union held international courses in Ethiopia and Tanzania, attracting TB program staff from across Africa. In 2016, The Union revised its international course and launched ‘Principles in TB Care and Prevention: Translating Knowledge to Action’ in Zimbabwe.10 The revised curriculum includes field practicals emphasizing TBData4Action, an approach developed by The Union Zimbabwe office and the National TB Program in Zimbabwe.11,12 TBData4Action introduces a set of indicators that cover key components of TB diagnosis and treatment, and promotes active use of routinely available TB data by local staff from health facilities upwards to strengthen quality of TB services and programmatic management.
In 2016, a collaboration between the DNTLD-P, CHS and The Union was formed to bring The Union’s international course to Kenya for country-wide training of all coordinators, specifically targeting identified training gaps. The aim of this paper is to describe the implementation outcomes from the unique training effort between these three organizations to build human resource capacity in TB care and prevention.13
METHODS
Setting
The DNTLD-P staffed with 45 technical officers (2020) is responsible for developing the national TB strategy, policy formulation, dissemination, monitoring and evaluation. At county level, there are 48 CTLCs and 296 SCTLCs whose core mandate is the implementation of DNTLD-P policies through direct TB service delivery, coupled with monitoring and evaluation at sub-county and facility level. In 2020, Kenya (estimated population of 47.6 million) had over 10,000 health facilities; 4,398 provided TB treatment and of these, 2,178 provided TB diagnostic services of which 189 had GeneXpert® platforms (Cepheid, Sunnyvale, CA, USA).3,14 Two TB reference laboratories provided culture and drug susceptibility testing. One central medical store was responsible for the distribution of TB medicines and other commodities. Kenya had ongoing training initiatives that were didactic and classroom-based.
Training implementation period
Planning for the national training was initiated in November 2016. The inaugural training occurred in May 2017, and the last iteration was conducted in July 2021.
Training curriculum development
The overarching goal was to develop a high-quality, comprehensive, practical, and sustainable training program in TB care and prevention, including TBData4Action. The aim was to empower coordinators and healthcare workers at large to find more people with TB, while simultaneously improving the quality of services by strengthening not only the use of facility, sub-county and county TB data but also by supporting supervision by TB coordinators. One underpinning of TBData4Action is the use of catchment populations to calculate rates (per 100,000 population) at each facility, sub-county and county permitting comparisons, a process that is not possible when only absolute numbers are examined. These comparisons facilitate identification of ‘underperforming’ facilities, sub-counties and counties that require targeted investigations and support.
Before this training, most programmatic attention focused on the TB care cascade from the time of diagnosis, rather than from the time of detection of people with presumed TB, thereby missing gaps during the pretreatment phase. The use of TBData4Action is designed to equip coordinators and technical officers with skills to provide data-driven support supervision and technical assistance. Based on The Union‘s international course, we collaboratively developed a bespoke curriculum for Kenya guided by the 2016 national prevalence survey findings,7 the TB indicators reported in 2016 and subsequent years, and the recurrently identified programmatic gaps. These gaps included low utilization of rapid molecular diagnostic testing despite updated algorithms, absence of robust specimen sample referral systems, pretreatment loss to follow-up, and low pediatric TB notifications.15
Training
Training schedules supported attendance by county teams (CTLCs and their respective SCTLCs) as a group. Training venues were purposefully chosen based on counties where field practicals could easily be conducted. Availability of a hotel venue that could accommodate all the participants and faculty in a quiet environment with access to the field sites was considered. After identifying host counties, permission was sought from the county health director to conduct training and field visits within their authority via a letter from the DNTLD-P head. Once approval was obtained, the DNTLD-P issued participant invitations, while CHS managed training logistics (Figure 1 and Supplementary Table S1).
FIGURE 1.
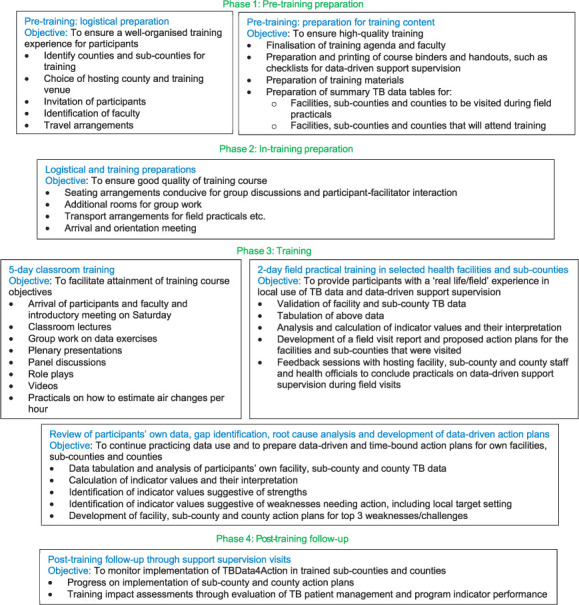
Flow chart of phases in training preparation and implementation, national training courses in TB care and prevention in Kenya, 2017–2021.
Participants pre-filled TB summary data tables for facilities in their sub-counties with assistance from the DNTLD-P and CHS; data tables of field practical facilities were constructed by CHS and DNTLD-P.
Training implementation
Training courses were conducted from Sunday morning through midday Saturday with two days of field practicals. Pre- and post-tests were administered to participants on Day 1 and 7. End-of-day reflections and an end-of-training evaluation were also conducted.
Adjustment of training content
The course facilitators reviewed the daily reflections at the end of each day and the evaluations at the end of each training. This informed constant course changes as well as the design of subsequent training courses. (Figure 1 and Supplementary Table S2).
Developing local faculty
A major training goal was the development of a local faculty to reduce dependency on international facilitators. Faculty members, drawn from all DNTLD-P levels and CHS, were identified among the course participants. At subsequent training courses, they were then mentored by pairing them with experienced faculty members to co-facilitate sessions. We also employed the teach-back methodology.16
Costing
We documented actual undiscounted costs and calculated the overall average cost of each training course and the average cost per participant. We compared the overall average cost per participant of an in-country training with the cost of attendance at an international alternative.
RESULTS
Adapted training curriculum and approach
The training course consisted of four phases (Figure 1). We applied participatory adult education pedagogy and included didactic sessions, group work, plenary presentations, panel discussions and role-plays into training sessions. A comprehensive list of indicators for using the TBData4Action approach was developed based on WHO indicators and country priorities (Supplementary Tables S3 and S4). Participants were asked to analyze two sets of TB data: 1) field practical sites, and 2) their own facilities, sub-counties and counties. Based on the latter, they developed time-bound action plans. Post-training action plan follow-up occurred during routine support supervision visits. In addition, a pilot of remote (online) mentorship was conducted in Mombasa County in late 2019.
High training coverage achieved
From May 2017 to July 2021, 11 training sessions were conducted reaching 96% (331/344) coordinators from all 47 counties (Figure 2). In June 2019, a special session for 37 national-level program officers was held. In total, 389 individuals were trained inclusive of implementing partners (Table 1).
FIGURE 2.
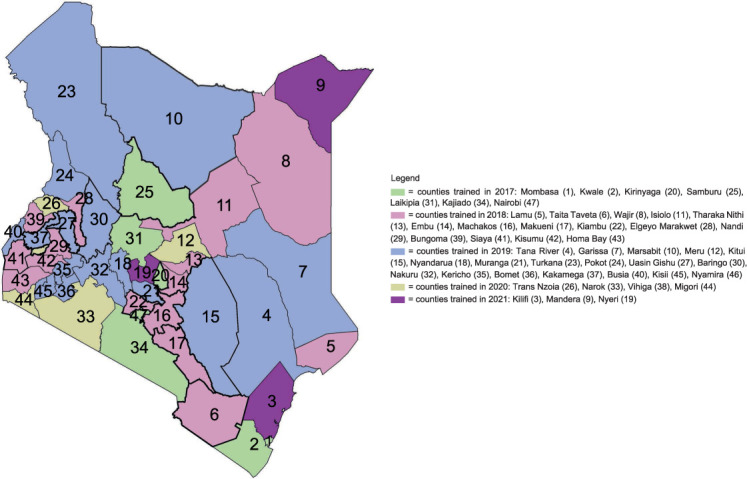
Map of Kenya showing counties trained by year of training with all 47 counties trained over a 5-year period.
TABLE 1.
Characteristics of participants of national training courses in TB care and prevention, Kenya, 2017–2021 (n = 389)
| Characteristic | n (%) |
|---|---|
| Sex | |
| Male | 228 (59) |
| Female | 161 (41) |
| Cadre | |
| Sub-county coordinator | 281 (72) |
| County coordinator | 50 (13) |
| National program officer | 37 (10) |
| Implementing partner organization staff | 21 (5) |
Local faculty capacity building for sustainability
Two local trainers (one female) attended the Union’s International Principles Course in Zimbabwe before the in-country training. During in-country courses, 36 additional local trainers, of whom 15 (42%) were female, were mentored. Sixteen (44%) were CTLCs, 15 (42%) partner organization staff, and 5 (14%) national-level officers. We progressively shifted facilitation from international to local faculty (22% in training #1 to 88% in training #11) (Figure 3).
FIGURE 3.
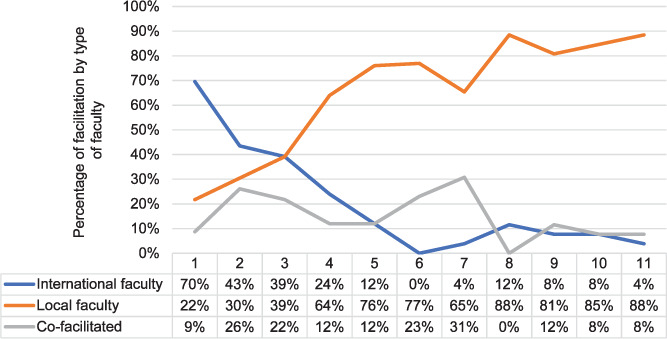
Changes in faculty composition in county training courses in TB care and prevention in Kenya, 2017–2021.
Development and follow-up of county TB action plans
All participants developed sub-county and county action plans based on challenges identified through tabulation, analysis and interpretation of their own TB data. All action plans were presented at the final day plenary for discussion and critique (Table 2). Following training, action plans were shared with the DNTLD-P, which then provided national technical assistance and follow-up.
TABLE 2.
Samples of action plans before and after national training in TB care and prevention, Kenya, 2017–2021
| A) Sample of pre-training Action Plan* | |||
|
| |||
| Gap | Action | Responsible person | Timeline |
|
| |||
| Low case notification rates of 83% | Active case-finding in all departments | CTLC and SCTLC | Immediately |
| Sub-county did not achieve child TB target: 8% achieved | Active case-finding through sensitisation of HCWs | CTLC and SCTLC | Immediately |
* While identified gaps are data driven, the identified actions are non-specific, not time-bound and not data-driven.
| B) Sample of post-training Action Plan (on case-finding)† | |||
|
| |||
| Gap | Action | Responsible person | Timeline |
|
| |||
| In 4 sub-counties with low case notification (below the county average 203/100,000), use of presumptive TB register is at 60% of facilities | Implement use of presumptive TB register in 100% of facilities in these 4 sub-counties | CTLC and SCTLC | By end of next quarter |
| Low case notification rate of 250 vs. 426/100,000 | Increase the number of persons with presumptive TB by sending 2 people per day presenting to the health facility with respiratory symptoms to laboratory for sputum collection | CTLC and SCTLC to perform sensitization Facility staff to do referral |
By end of thequarter |
| TB notifications in children are 5% lower than the national average of 9% (expected 10–15%) | Perform contact investigation for 85% of all bacteriologically confirmed adults, screening 90% of exposed children <5 years of age | CTLC and SCTLC | By end of next quarter |
† Data-driven gaps were identified (e.g., “sub-county case detection of 218/100,000 vs. county detection rate of 325 and the national estimates of 450/100,000”) and specific, data-driven actions that are measurable and time bound (e.g., “register 2 persons per day visiting the health centre with respiratory symptoms into the presumptive register”).
| C) Sample of post-training action plan on childhood TB* | ||||
|
| ||||
| Gap | Root causes: the why?† | Action point | Responsible | Timeline |
|
| ||||
| Over 60% of the facilities in the county reported no childhood TB cases | ||||
| Inadequate capacity by SCTLCs on monitoring childhood TB activities in sub-counties | Provide technical assistance and support supervision on childhood TB to all SCTLCs and visit two priority sub-counties at least once per quarter | CTLC | End of quarter | |
| Low index of suspicion for childhood TB among health care workers | Conduct at least 2 childhood TB sensitisation sessions in every facility in sub-county within quarter | SCTLC | By end of the quarter | |
| TB screening is not taking place in childhood service delivery points, for e.g., maternal, neonatal and child health services, nutrition units, inpatient wards, etc. | Conduct on-job-mentorship in all service delivery points on TB screening within childhood service delivery points | CTLC, SCTLC, MNCH I/C, facility paediatricians, nutritionist etc. | By end of the quarter | |
| Inadequate contact tracing taking place among household contacts of adults with bacteriologically confirmed TB | Sensitise and conduct on-job training on documentation of contact registers | SCTLC, TB clinicians and nurses | By end of the quarter | |
*Low county childhood TB notification of 3% compared to national average of 9%.
† Root causes that inform the data-driven action gaps identified, e.g., because ‘there is a low index of suspicion for childhood TB among HCWs’, the action identified is to ‘conduct at least two childhood TB sensitisations in every facility in the sub-county within quarter’.
CTLC = county TB and leprosy coordinator; SCTLC = sub-county TB and leprosy coordinator; MNCH = maternal new-born and child health
Cost comparison of training alternatives
The average cost of the in-country training was USD1,906 (range USD1,256–2,604) per participant, with main cost drivers being participant accommodation, subsistence and travel payments, and facilitation fees. The cost of attendance at an international course was calculated at USD7,691 per participant.
Acceptability of the training demonstrated through participant feedback
Through the end-of-course evaluations, participants reported improvement in both their knowledge about TB care and prevention and their capacity to analyze and use TB data for decision-making. They predicted these skills would improve their supervisory skills, including the use of sub-national data to inform the focus of supervision and provide constructive and balanced feedback:
“I will analyze my sub-county data and make more data driven decisions” (sub-county coordinator).
“I will provide balanced feedback to facility staff” (sub-county coordinator).
The participants recognized the value of using catchment populations to calculate presumptive TB and TB notification rates:
“I will use the catchment populations to come up with estimated targets for 2018” (sub-county coordinator).
On the overall training experience, the participants acknowledged the change in approach:
“No more business as usual” (county coordinator).
Other training outcomes
Several positive unforeseen developments occurred as a result of the training courses. First, CHS developed a facility TB performance-monitoring chart (Figure 4), subsequently adopted by the DNTLD-P. By the end of 2020, this was used by all TB facilities in Kenya. The purpose of the chart is to track the monthly progress of selected key TBData4Action indicators at facility level. Second, nine regional desks (multidisciplinary teams consisting of officers from the DNTLD-P, CTLCs and implementing partner organizations) were set up to monitor regional performance and avail data-driven technical support to groups of counties with similar challenges in TB care and prevention. Finally, the fact that TBData4Action includes indicators to monitor management of people with presumptive TB, coupled with the shift to data-driven supervision, accelerated the national roll-out of the presumptive TB register and assisted its incorporation into the national electronic reporting system.
FIGURE 4.
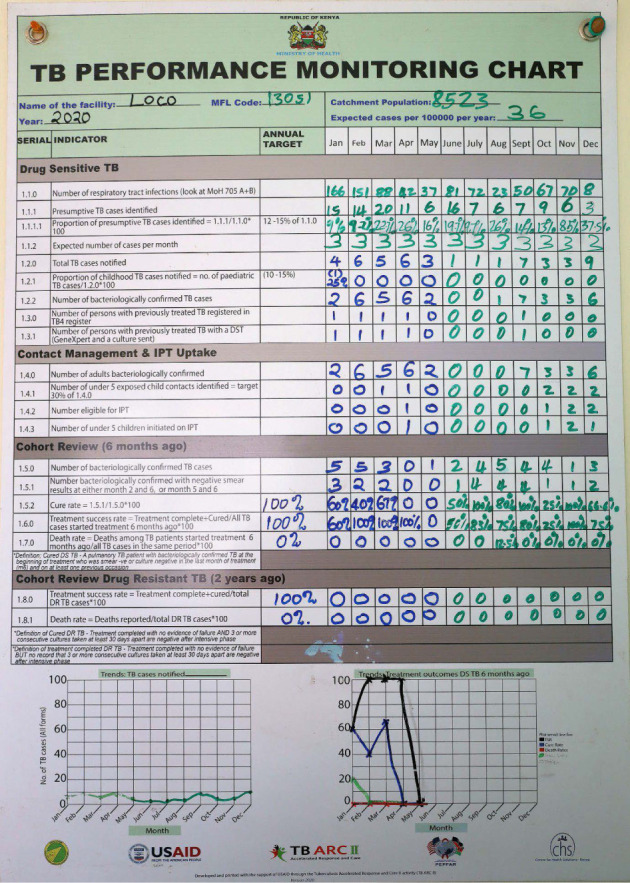
TB Performance Monitoring Chart used to track the monthly progress of selected key TBData4Action indicators at the facility.
DISCUSSION
In 5 years, we conducted 12 courses strongly focused on TBData4Action, reaching 96% of 344 TB coordinators in Kenya. Fifty-five DNTLD-P and partners involved in TB-HIV implementation were also trained. We mentored 36 local facilitators in addition to two individuals who attended The Union’s course in Zimbabwe.
We developed the curriculum based on understanding of specific training needs in Kenya and used participant feedback and faculty observations for continuous refinement. We applied principles of participatory adult education and problem-based learning, a departure from a purely didactic approach: the change was appreciated by participants, as indicated in their evaluations. The teach-back method further enhanced facilitation skills of local faculty. For the first time in TB training in Kenya, the course emphasized field practicals incorporating real-life scenarios and hands-on work with TB data to supplement class-room sessions.17 In addition to field practicum TB data, participants used their own TB data to develop action plans that “brought the training to their own door” and generated interest in immediate adoption through insights into day-to-day work. By training the entire county teams consisting of CTLC and SCTLCs as one group, we ensured the creation of a critical mass of trained coordinators sharing standardized information and building teams.
To maintain momentum in translating training into practice, courses were promptly followed by support supervision visits,18 during which sub-county and county action plans were followed up and lessons learned in TBData4Action reinforced through practice. CTLCs and SCTLSs reported that local staff improved the quality of TB data when they witnessed how data entered in their TB registers helped their work. Coordinators also reported transitioning from being “data clerks” who entered data into the national electronic TB information system to program support supervisors who used TB data for planning and design of interventions.
The courses introduced the use of catchment populations. Catchment populations have been used widely in calculating uptake of immunization and skilled maternal deliveries in Kenya.19 The computation and use of presumptive TB and TB notification rates in TB care and prevention provides coordinators with an objective metric against which to analyse performance and initiate focused improvement measures.
We identified the following key elements for the success of the training collaboration. First, the DNTLD-P adopted and supported courses fully, with senior officers facilitating sessions and ensuring vital immediate follow-up of submitted TB action plans. Second, we developed a set of indicators to be tracked via TBData4Action that represent DNTLD-P priorities, including case-finding using presumptive TB registrations, identification of care cascade gaps, and pediatric TB. Third, the courses were repeatedly held in two counties, Kirinyaga and Laikipia, allowing the participants to see results of the locally adapted TBData4Action in place over time, and thus spur them on to push development in their own counties (e.g., appearance of data charts in clinics that tracked indicators over time). Fourth, by providing in-country training, the unit training cost ranged from one-fifth to one-third of the cost of an international course, while allowing most TB coordinators to be trained as a cohesive unit, as opposed to few individuals attending an international course with expected, but often inadequate, diffusion of knowledge throughout the system.20
The courses faced some challenges. The development of the data sets for the field practicals was labor-intensive and time consuming because this type of data compilation down to facility level had not been performed previously. This was one reason why we returned the courses to the same counties; once the data set was constructed, updating it in the same county was less time-consuming. Participants consistently described the week as an intense immersion with “lots of math.” Action plan follow-up by the DNTLD-P showed that some county and sub-county teams were slower to adopt TBData4Action.
We acknowledge that the best method of evaluating the impact of the courses is to evaluate its effect on relevant service delivery.17 This paper focused on implementation outcomes through collaborative development of an in-country training program. We found the training to be acceptable, appropriate, and feasible based on observations and feedback from participants. Building capacity of local faculty is a pathway to sustainability. Plans are ongoing to evaluate the impact of this national training on TB program quality indicators.
CONCLUSION
We report the development and outputs of a unique training collaboration to conduct country-wide capacity building in TB care and prevention, incorporating TBData4Action, with the goals to find more ‘missing’ people with TB in Kenya and to provide them with standardized, high-quality care.
ACKNOWLEDGMENTS
The authors want to thank the Kenya TB program for embracing this training wholeheartedly and the heads of program who have ensured the running of the courses over the years: K Kimenye (2017–2019), E Onyango (2019–2021) and the current head W Ejersa; and county health management teams and facility staff of Kirinyaga, Kisii, Laikipia, Meru, Mombasa, and Nakuru counties for providing access to facilities for field practicals and supporting the participants during the training: S Chebore (CHS), P Lodi (Bungoma County), T Malika (Kisumu County), C Migwambo (Homabay County), E Mueni (Nairobi County), S Macharia (DNTLD), J Mungai (CHS), D Mureithi (Laikipia County), C Mwamburi (Mombasa County), F Mwenda (Kirinyaga County), E Ng’ang’a (CHS), T Njoroge (CHS), M Wambura (Siaya County) and W Ikua (CHS), in-country faculty members who offered their time and expertise to deliver the courses; M Githiomi, T Kandie and R Kiplimo for ensuring that the pre-planning preparations of the county and facility data tables were done in a timely manner and for the delivery of some of the modules during training; and finally, as training is only as good as its planning, M Gaye-Ayrault (The Union), G Moemi (CHS), O Liesbeth (The Union) and E Kithinji (CHS). This implementation was made possible by the support of the American People through the United States Agency for International Development (USAID) through Tuberculosis Accelerated Response and Care activity (TB ARC and TB ARC II). The contents of this manuscript are the sole responsibility of Centre for Health Solutions – Kenya and collaborators, and do not necessarily reflect the views of USAID or the United States Government.
Footnotes
Conflicts of interest: none declared.
References
- 1.World Health Organization Global tuberculosis report, 2020. Geneva, Switzerland: WHO; 2020. [Google Scholar]
- 2.World Health Organization A brief history of tuberculosis control in Kenya. Geneva, Switzerland: WHO; 2009. [Google Scholar]
- 3.National Tuberculosis, Leprosy, and Lung Disease Program, Ministry of Health Kenya Annual report, 2019. Nairobi, Kenya: Ministry of Health Kenya; 2019. [Google Scholar]
- 4.Ministry of Health Kenya Division of National Tuberculosis, Leprosy and Lung Health. Annual report, 2012. Nairobi, Kenya: Ministry of Health Kenya; 2012. [Google Scholar]
- 5.Oliwa JN, et al. Variability in distribution and use of tuberculosis diagnostic tests in Kenya: a cross-sectional survey. BMC Infect Dis. 2018;18(1):328. doi: 10.1186/s12879-018-3237-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ardizzoni E, et al. Implementing the Xpert® MTB/RIF diagnostic test for tuberculosis and rifampicin resistance: outcomes and lessons learned in 18 countries. PLoS One. 2015;10(12):e0144656. doi: 10.1371/journal.pone.0144656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Masini E, et al. Kenya tuberculosis prevalence survey 2016: challenges and opportunities of ending TB in Kenya. PLoS One. 2018;14(1):e0211593. doi: 10.1371/journal.pone.0211593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Government of Kenya Nairobi, Kenya: Government of Kenya; 2010. The Constitution of Kenya, 2010. Kenya Law Reports; p. 31. [Google Scholar]
- 9.Tsofa B, et al. Devolution and its effects on health workforce and commodities management - early implementation experiences in Kilifi County, Kenya. Int J Equity Health. 2017;16(1):169. doi: 10.1186/s12939-017-0663-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.International Union Against Tuberculosis and Lung Disease Principles of tuberculosis care and prevention: translating knowledge to action. Paris, France: International Union Against Tuberculosis and Lung Disease; 2021. [Google Scholar]
- 11.Heldal E, et al. Local staff making sense of their tuberculosis data: Key to quality care and ending tuberculosis. Int J Tuberc Lung Dis. 2019;23(5):612–618. doi: 10.5588/ijtld.18.0549. [DOI] [PubMed] [Google Scholar]
- 12.Ministry of Health and Child Care Zimbabwe Harare, Zimbabwe: Ministry of Health and Child Care Zimbabwe, 2015. Making sense of TB data: guide for collection, analysis and use of TB data for health workers in Zimbabwe; pp. 1–119. [Google Scholar]
- 13.Proctor E, et al. Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38(2):65–76. doi: 10.1007/s10488-010-0319-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ministry of Health Nairobi, Kenya: Ministry of Kenya; 2020. Kenya Community Health Policy, 2020–2030; pp. 1–44. [Google Scholar]
- 15.Tollefson D, et al. Under-reporting of sputum smear-positive tuberculosis in Kenya. Int J Tuberc Lung Dis. 2016;20(10):1334–1341. doi: 10.5588/ijtld.16.0156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tryon C, et al. Teachback methodology: building global training capacity with a unique training-of-trainers course. Public Health Action. 2015;5(1):79–82. doi: 10.5588/pha.14.0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arnadottir T. Tuberculosis and public health: policy and principles in tuberculosis control. Paris, France: International Union Against Tuberculosis and Lung Disease; 2009. [Google Scholar]
- 18.Arnadottir T, Rieder HL, Enarson DA. Tuberculosis Programs Review Planning Technical Support: a manual of methods and procedures. Paris, France: International Union Against Tuberculosis and Lung Disease; 1998. [Google Scholar]
- 19.Ministry of Health Kenya Health Sector Strategic and Investment Plan (KHSSP) July 2013–June 2017. Nairobi, Kenya: Ministry of Health; 2013. [Google Scholar]
- 20.Barker PM, Reid A, Schall MW. A framework for scaling up health interventions: Lessons from large-scale improvement initiatives in Africa. Implement Sci. 2016;11(1):1–11. doi: 10.1186/s13012-016-0374-x. [DOI] [PMC free article] [PubMed] [Google Scholar]


