Abstract
Objective:
To assess whether clinical and/or laboratory-confirmed diagnosis of maternal influenza during pregnancy increases the risk of seizures in early childhood.
Design:
Analysis of prospectively collected registry data for children born between 2009 and 2013 in three high income countries. We used Cox regression to estimate country-level adjusted hazard ratios (aHRs); fixed effects meta-analyses were used to pool adjusted estimates.
Setting:
Population-based.
Participants:
1 360 629 children born between 1 January 2009 to 31 December 2013 in Norway, Australia (New South Wales) and Canada (Ontario).
Exposure:
Clinical and/or laboratory-confirmed diagnosis of maternal influenza infection during pregnancy.
Main outcome measures:
We extracted data on recorded seizure diagnosis in secondary/specialist health care between birth and up to seven years of age; additional analyses were performed for the specific seizure outcomes “epilepsy” and “febrile seizures”.
Results:
Among 1 360 629 children in the study population, 14 280 (1.0%) were exposed to maternal influenza in utero. Exposed children were at increased risk of seizures (aHR 1.17, 95% confidence interval (CI) 1.07 to 1.28), and also febrile seizures (aHR 1.20, 95% CI 1.07 to 1.34). There was no strong evidence of an increased risk of epilepsy (aHR 1.07, 95% CI 0.81 to 1.41). Risk estimates for seizures were higher after influenza infection during the second and third trimester than for first trimester.
Conclusions:
In this large international study, prenatal exposure to influenza infection was associated with increased risk of childhood seizures.
Introduction
Infections during pregnancy may be associated with increased risk of adverse neurodevelopmental outcomes in childhood, including seizures.(1–6) Febrile seizures, the most common seizure event in childhood, affect 2–5% of children under five years of age.(7) Simple febrile seizures are generally not associated with long-term consequences, while more serious or recurrent events have been associated with an increased risk of epilepsy and certain psychiatric disorders.(8–10) Pregnant women are at higher risk of influenza-associated complications,(11) and influenza infection during pregnancy is associated with adverse perinatal outcomes.(12) However, the specific role of prenatal exposure to maternal influenza infection in the risk of offspring seizure disorders is unclear.
With registry data from three high-income countries (Norway, Canada, Australia) we established a large, population-based cohort to explore whether children with prenatal exposure to maternal influenza had an increased risk of seizures in early childhood.
Methods
Data sources and study population
Birth records from 1 January, 2009 to 31 December, 2013 were obtained from the Medical Birth Registry of Norway,(13) the New South Wales (NSW) Perinatal Data Collection (Australia),(14) and the BORN Ontario Birth Registry (Canada),(15) and linked to routine health administrative data from medical consultations and hospitalizations in mothers and children (supplemental methods; supplemental table S1).
Maternal influenza infection
Maternal influenza infection was defined by an influenza diagnosis during country-specific yearly influenza seasons (supplemental table S2). In Norway, we identified influenza diagnoses from primary and secondary care databases and laboratory-confirmed influenza records from the national surveillance system for communicable diseases; in Ontario, we used diagnoses from primary and secondary care data; while in Australia, we identified influenza diagnoses from secondary care data and state-wide notification records for laboratory-confirmed influenza. In Norway, laboratory-confirmed influenza records were only available for the 2009–2010 pandemic influenza season (defined as April 2009 to April 2010). All maternal influenza cases diagnosed in seasons subsequent to the 2009–2010 pandemic season were defined as seasonal influenza.
Seizures
We included the following diagnoses from secondary/specialist health care settings: ICD-10 codes R56.0 “Febrile convulsions”, R56.8 “Other and unspecified convulsions,” G40 and G41 “Epilepsy” (supplemental table S3). Our primary outcome was the combined group “any seizure”, defined as any record of these four codes. We defined the subgroup “Febrile seizures” as any record of R56.0, between ages three months to five years.(16) “Epilepsy” was defined by at least two recorded diagnoses of G40 or G41.
Covariates
In multivariable models we adjusted for parity, maternal age, multiple birth, season and year of conception, socio-economic status, maternal epilepsy, and smoking during pregnancy. Socio-economic status was measured using country-standardized methods. Further details on covariates are provided in supplemental table S1.
Statistical analyses
Individual data sharing was not possible between countries due to privacy restrictions, therefore data were analysed separately within each country according to a standardized study protocol. We used Cox proportional hazards models, with days from birth as the underlying time metric, to estimate crude and adjusted hazard ratios (aHR) for any seizures in childhood after prenatal exposure to any maternal influenza infection (seasonal or pandemic), and further stratified by (a) seasonal influenza, and (b) pandemic influenza. Any influenza infection was further categorized by trimester at time of diagnosis. The comparison group comprised children of mothers without influenza diagnosis while pregnant. Additional analyses were performed for “febrile seizures” and “epilepsy”. Children were followed from birth until first seizure, death, emigration, or 31 December 2016. Follow-up time ranged from three years to seven years, except for NSW children who were censored on their 6th birthday. For febrile seizures, follow up was from three months of age until the 5th birthday. We created unadjusted cumulative incidence curves for seizures by exposure status using pooled aggregate data with monthly intervals. Robust standard errors accounted for dependency between siblings. Up to 3.9% with missing information were excluded. The proportional hazards assumption was evaluated through visual inspection, and found valid. Pooled estimates were generated using a fixed–effects meta-analysis with inverse variance weighting of individual-country results.(17) Heterogeneity was assessed using the I2 statistic, calculated as 100% × (Q–df)/Q, where Q is Cochrane’s heterogeneity statistic and df denotes degrees of freedom.(18)
We conducted sensitivity analysis with laboratory-confirmed influenza as exposure; and with multivariate logistic regression, a sensitivity analysis limited to the first three years of life. To address whether associations were explained by inherited susceptibility to infection, we repeated the primary model in Norway data with exclusion of children with a recorded diagnosis of influenza
Ethical approval
This study was approved by the Norwegian Regional Committee for Medicine and Health Research Ethics (ref. 2010/2583), the Children’s Hospital of Eastern Ontario Research Ethics Board (No. 17/04PE), the ICES Privacy Office (No. 2018–0901-137–000), the NSW Population & Health Services Research Ethics Committee, and the Curtin University Human Research Ethics Committee (HRE2017–0808). Each committee provided a waiver of consent for participants.
Results
There were 1 360 629 eligible children born in Norway, NSW and Ontario between January 1, 2009 and December 31, 2013 (supplemental figure S1). Of these, 14 280 (1.0%) had a mother diagnosed with influenza during pregnancy, of which 8762 (61.3%) had laboratory confirmed influenza. Characteristics of children and mothers are in table 1 (stratified by country in supplemental table S4). A total of 35 073 children (2.6%) had at least one record of a seizure, 22 624 children (1.7%) of a febrile seizure episode, 2993 children (0.2%) were defined with epilepsy, and the remainder had “other and unspecified convulsions”.
Table 1.
Maternal influenza status and characteristics of children born 2009 – 2013 in Norway, New South Wales (Australia), and Ontario (Canada) (pooled data)
| All countries |
||||
|---|---|---|---|---|
| No. of children | Maternal influenza in pregnancy† | |||
| Characteristic | N | (%)* | n | (%)‡ |
| All children § | 1 360 629 | 14 280 | (1.0) | |
| Maternal age at delivery | ||||
| <20 | 39 388 | (2.9) | 443 | (1.1) |
| 20–24 | 175 085 | (12.9) | 2033 | (1.2) |
| 25–29 | 384 788 | (28.3) | 4384 | (1.1) |
| 30–34 | 458 829 | (33.7) | 4707 | (1.0) |
| 35–39 | 247 825 | (18.2) | 2254 | (0.9) |
| ≥40 | 54 714 | (4.0) | 459 | (0.8) |
| Maternal smoking in pregnancy | ||||
| No | 1 174 081 | (86.3) | 11 565 | (1.0) |
| Yes | 145 023 | (10.7) | 1558 | (1.1) |
| Information declined¶ | 41 525 | (3.1) | 1157 | (2.8) |
| Maternal history of epilepsy | ||||
| Yes | 5296 | (0.4) | 101 | (1.9) |
| No | 1 355 333 | (99.6) | 14 179 | (1.0) |
| Parity | ||||
| 0 | 586 634 | (43.1) | 5169 | (0.9) |
| 1 | 477 322 | (35.1) | 5760 | (1.2) |
| ≥2 | 296 673 | (21.8) | 3351 | (1.1) |
| Gestational age at birth | ||||
| Preterm (<37 weeks) | 95 994 | (7.1) | 961 | (1.0) |
| Term (≥37 weeks) | 1 264 635 | (92.9) | 13 319 | (1.1) |
| Multiple birth | ||||
| Yes | 43 765 | (3.2) | 429 | (1.0) |
| No | 1 316 864 | (96.8) | 13 851 | (1.1) |
| Season of conception ǁ | ||||
| Winter | 339 763 | (25.0) | 2589 | (0.8) |
| Spring | 324 349 | (23.8) | 2785 | (0.9) |
| Summer | 340 333 | (25.0) | 4433 | (1.3) |
| Autumn | 356 184 | (26.2) | 4473 | (1.3) |
Column percentages
Maternal influenza diagnosis during pregnancy. Norway: any diagnosis in primary care using International Classification of Primary Care code R80, or in secondary or specialist health care using International Statistical Classification of Diseases revision 10 codes J09, J10 or J11, or laboratory-confirmed pandemic influenza. NSW: any laboratory-confirmed or hospital diagnosed influenza infection during pregnancy. Ontario: any diagnosis in primary care using modified ICD-9 code 487, or in urgent or in-patient health care using International Statistical Classification of Diseases revision 10 codes J09, J10 or J11. N.b. Influenza diagnoses only valid during country-specific yearly influenza seasons
Row percentages
Children born between January 1, 2009 and December 31, 2013
Category in use for Norway data only
Northern Hemisphere : Winter (Dec-Feb), Spring (Mar-May), Summer (Jun-Aug), Autumn (Sep-Nov); Southern Hemisphere: Winter (Jun-Aug), spring (Sep-Nov), Summer (Dec-Feb), Autumn (Mar-May).
The cumulative incidence of any seizures was higher in children exposed to prenatal exposure maternal influenza in pregnancy (3.42%; 95% confidence interval (CI) 3.13 to 3.74%) than in unexposed children (2.63%; 95% CI 2.60 to 2.66%) (figure 1A), with a pooled adjusted hazard ratio (aHR) of 1.17 (95% CI 1.07 to 1.28; figure 2; country-specific associations presented in supplemental table S5). Estimates were similar for seasonal influenza (aHR 1.16; 95% CI 1.03 to 1.31) and pandemic influenza (aHR 1.17; 95% CI 1.01 to 1.35) (figure 2 and supplemental figure S2). For febrile seizures, the cumulative incidence was higher in exposed (2.21%; 95% CI 1.98 to 2.47%) than in unexposed (1.69%; 95% CI 1.67 to 1.71%) (figure 1B), with adjusted HR for any influenza;1.20; 95% CI 1.07 to 1.34 (seasonal influenza: aHR 1.19; 95% CI 1.03 to 1.38; pandemic influenza: aHR 1.20; 95% CI 1.01 to 1.44; figure 3 and supplemental figure S3; country specific associations presented in supplemental table S6).
Figure 1.
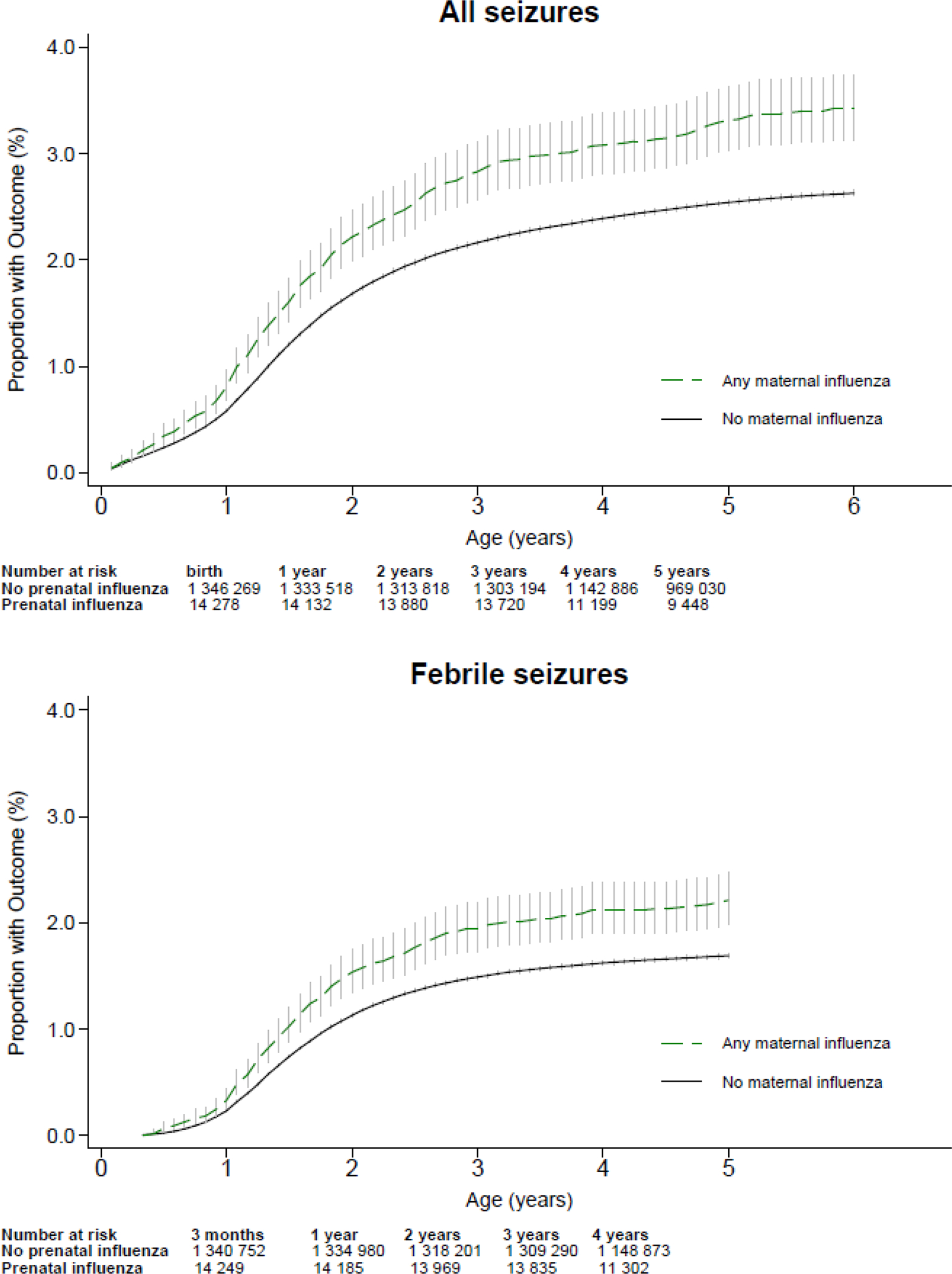
Cumulative incidence of (a) any seizures and (b) febrile seizures, according to exposure to maternal influenza during pregnancy: Pooled data for Norway, New South Wales (Australia) and Ontario (Canada), vertical lines show the 95% confidence intervals
Figure 2:
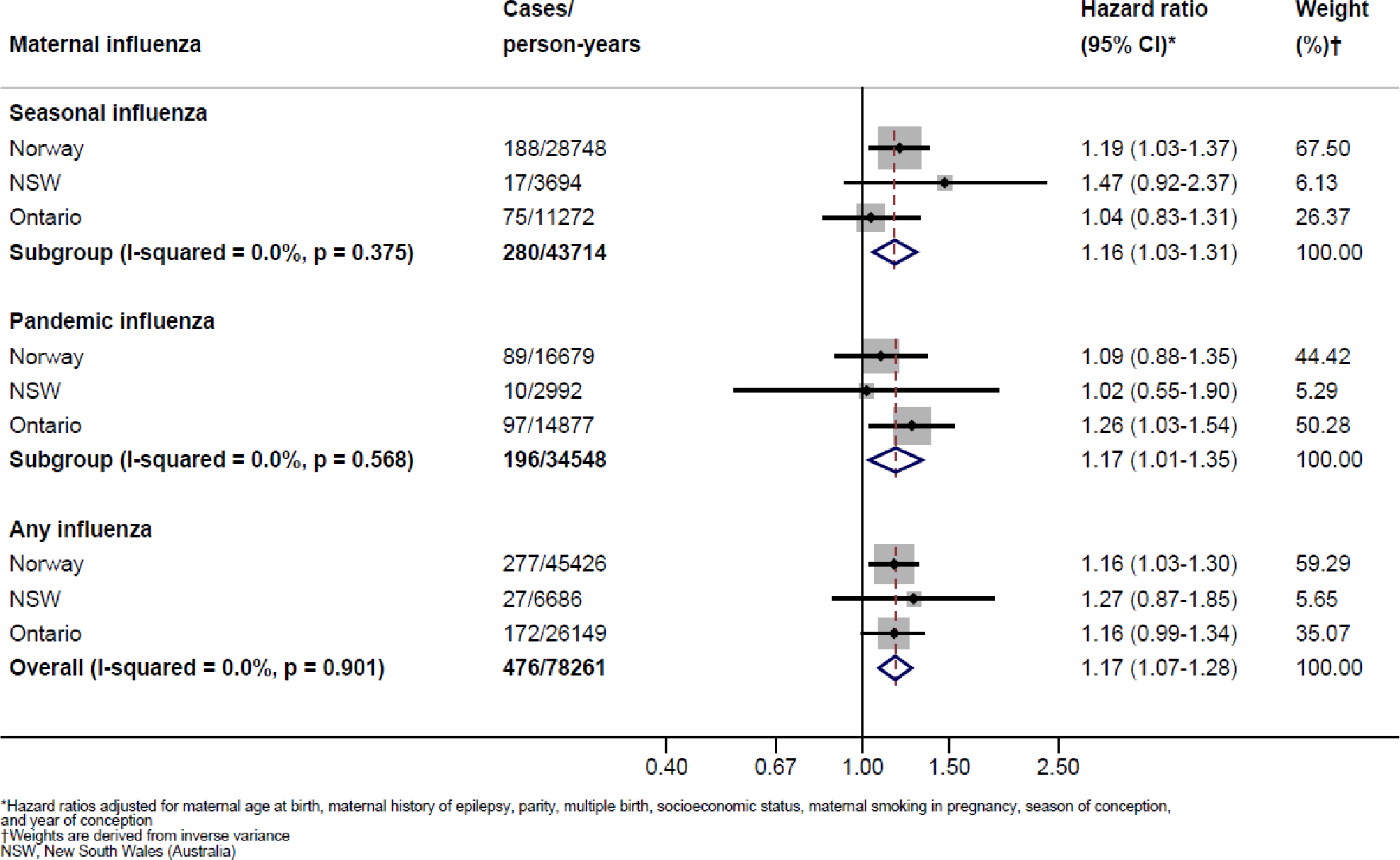
Meta analyses of the associations between prenatal influenza and any seizures in early childhood
Figure 3:
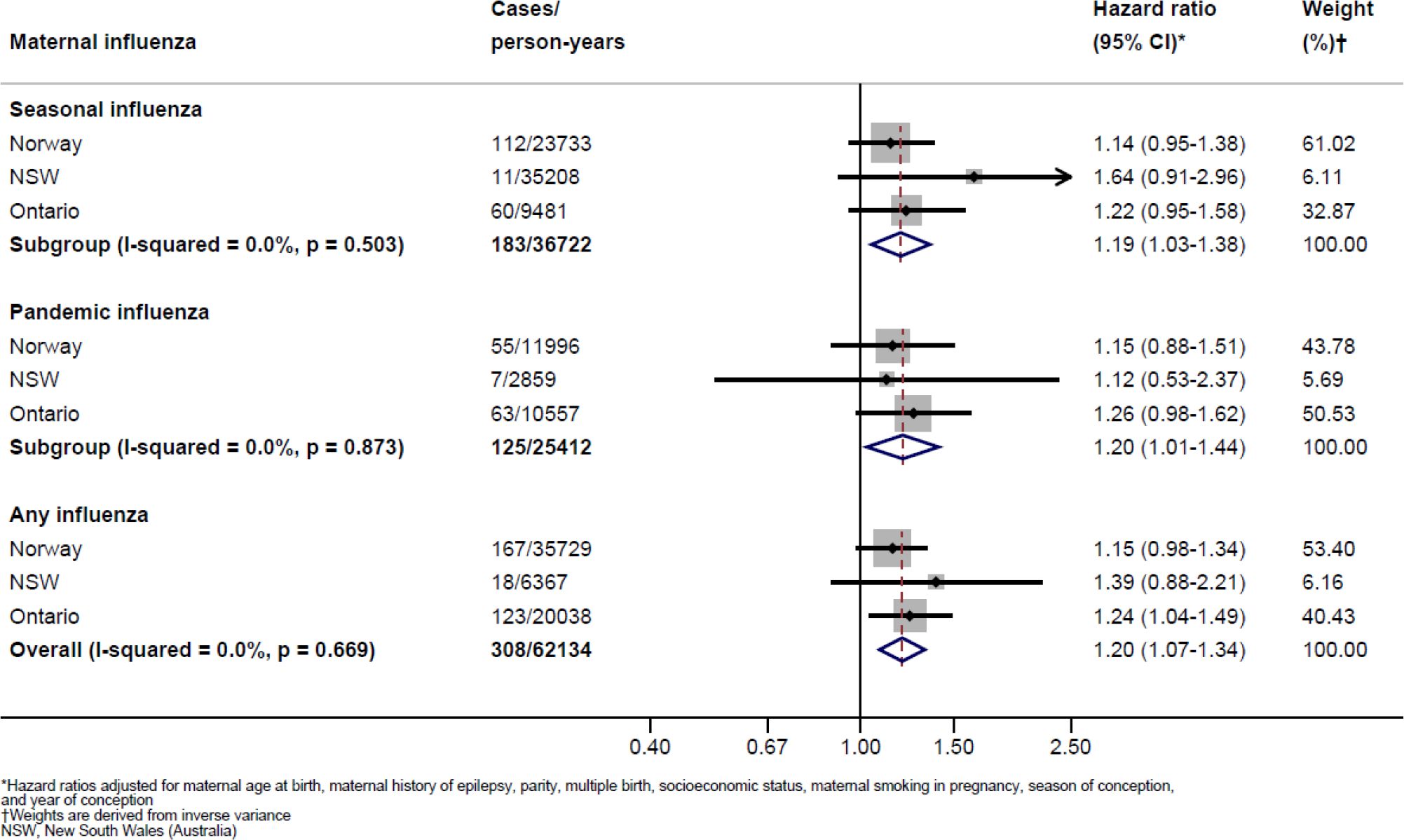
Meta analyses of the associations between prenatal influenza and febrile seizures in early childhood
Risk of seizures was elevated for influenza infection in 2nd and 3rd trimesters (2nd trimester aHR 1.24; 95% CI 1.08 to 1.41; 3rd trimester aHR 1.20; 95% CI 1.00 to 1.44), but not with first trimester infection (aHR 1.03; 95% CI 0.87 to 1.22;figure 4; country-specific associations presented in supplemental table S7).
Figure 4:

Meta analyses of the associations between prenatal influenza and all seizures in early childhood, by trimester of infection
For epilepsy, the cumulative incidence of epilepsy was slightly higher in exposed children (supplemental figure S4). However, after adjustment the HR of epilepsy after prenatal exposure to maternal influenza was 1.07; 95% CI 0.81 to 1.41; supplemental figure S5; country-specific associations presented in supplemental table S8).
When restricting to seizures up to age three, the pooled adjusted odds ratio was 1.20 (95% CI 1.08 to 1.32; supplemental figure S6). Estimates for laboratory-confirmed influenza were similar to the main results, although the evidence for association was weaker (any seizure; aHR 1.17; 95% CI 0.80 to 1.73; supplemental figure S7). When excluding children with an influenza diagnosis in childhood, the aHR was 1.17; 95% CI 1.04 to 1.33, virtually identical to the estimate for the full sample (aHR 1.16; 95% CI 1.04 to 1.30; supplemental tables S5 and S9, Norway data only).
Discussion
With registry data from three high-income countries on more than 1.3 million children, we found that prenatal exposure to maternal influenza during pregnancy was associated with a 15–20% increased incidence of seizures in early childhood. Estimates were similar for “any seizure” and for the more specific “febrile seizure” outcome. There was no strong evidence of an increased risk of epilepsy.
The use of large population-based registries has several strengths, including negligible bias from selection of participants or loss to follow-up. Also, using multiple independent registries reduces potential bias from possible differences in reporting. Although ascertainment of outcomes was similar across the three countries, the majority of influenza diagnoses in Norway and Ontario were clinical, while 99.9% of NSW influenza diagnoses were laboratory-confirmed. However, potential exposure misclassification was most likely non-differential by seizure outcomes, which may have attenuated associations. Women with more severe symptoms are more likely to seek health care, thus our results may reflect more severe influenza illness. Still, results were consistent across countries and between clinical and laboratory-confirmed diagnoses, suggesting no strong bias of misclassification.
It is possible that the observed associations could be influenced by inherited susceptibility to infection. We did not have information on all infections during childhood. However, results were very similar when restricting to children with no recorded influenza diagnosis during childhood. There could also be an inherited risk of seizure disorders, and we adjusted for maternal history of epilepsy, but did not have complete data on other maternal conditions. However, genetically transmitted susceptibility to infection or seizures would be unlikely to differ by trimester, so our findings of higher estimates for exposure in second and third trimester suggests an independent effect of maternal infection.
Estimates were mostly unchanged after adjustment, indicating little confounding. Still, residual confounding cannot be ruled out. For example, registry data on influenza vaccination was incomplete and was not evaluated. Pregnant women were recommended influenza vaccination in all three countries during the study period, though uptake is low (Canada <20% in 2014,(19) Australia 27% in 2011(20)). Pediatric vaccination, either for influenza or other conditions, may be associated with transient febrile illness. However, it is unlikely to be associated with maternal influenza in pregnancy, and was therefore not considered a potential confounder. We did not adjust for gestational age, as this is a potential mediating variable, and adjustment could introduce bias.(21) Information on medication use was not available. Drugs commonly used to treat influenza symptoms not only influence severity of symptoms, but could hypothetically influence fetal neurodevelopment.(22)
As this study is based on large and complete populations, we could not validate the accuracy or completeness of the seizure diagnoses. However, seizure episodes in young children are a dramatic experience, and caregivers are likely to seek medical care for first seizure episodes in children. Furthermore, a diagnosis of epilepsy is likely to be established in secondary or specialist care and is therefore likely captured in the registries. Approximately 2.6% of children had at least one recorded seizure diagnosis during follow-up, and 1.7% had at least one recorded diagnosis of febrile seizure. Diagnostic coding practices may vary, adding to the uncertainty of outcome validity. In a study from Denmark, the predictive value of the ICD-10 code R56.0 for febrile seizures was high.(23) The most common type of seizure in the age groups in our study is febrile seizure,(24) and we assume that the majority of R56 records in secondary care are likely to represent febrile seizures. The broader outcome “any seizures” reflects a more heterogeneous mix of seizures: primarily febrile seizures, but also seizures due to other causes, such as acute symptomatic seizures connected to head trauma or infections, or the first epileptic seizure before a diagnosis of epilepsy is made, as well as epileptic seizures. Associations between prenatal exposure to maternal influenza and febrile seizures were of similar magnitude as the overall seizure outcome, indicating that influenza may have similar effects on several seizure subtypes, or that different seizures may overlap within the registered codes. To be categorised as having epilepsy, we required at least two registrations of epilepsy diagnoses during the study period, an approach which has been shown to have a positive predictive value of 88% when using Norwegian registry data.(25) At the end of our study period (children aged 3–7 years), the cumulative incidence of epilepsy was 0.22%. This is slightly lower than that observed in studies conducted in other high-income countries, in which the cumulative incidence of epilepsy by age 5 ranged from 0.4% to 0.7%.(25–27) The lower incidence of epilepsy in our study may be due to our strict definition. It is also possible that children who were diagnosed with epilepsy after our follow-up period ended were misclassified in our study as experiencing other (non-epileptic) types of seizure due to the tendency to for a first epileptic seizure to be diagnosed as a febrile or non-specified seizure.
Our findings suggest that prenatal exposure to influenza may impact susceptibility to seizures in childhood. It has previously been hypothesised that maternal infection in pregnancy could affect fetal neurodevelopment through various pathways. There could be a direct effect through infection of the fetal brain, or an indirect effect through maternal systemic immunological responses to infection, such as fever or elevated cytokine levels.(28, 29) Several studies address associations between infection in pregnancy and central nervous system disorders in offspring, particularly schizophrenia, for which some studies found an increased risk after prenatal exposure to maternal infection.(30) A recent study using Swedish registry data with follow-up into adulthood reported that any maternal infection during pregnancy requiring hospitalisation was associated with an increased risk of autism spectrum disorders (ASD) and depression in adulthood, but not with bipolar disease or psychosis.(31) Studies of prenatal exposure to influenza infection and childhood seizures have been lacking, and only a few studies have considered prenatal exposure to influenza and other neurodevelopmental outcomes in early childhood. A recent Norwegian cohort study reported modest associations between pandemic influenza in early pregnancy and psychomotor development at 6 months.(32) A large US cohort study did not find evidence of an association between influenza infection in pregnancy and risk of ASD in childhood.(33) In several studies, associations between prenatal exposure to non-influenza infections (such as genitourinary infections) and childhood seizures (including epilepsy) have been investigated,(1–6) with results generally supporting an association. We found indications that childhood seizures were associated with both pandemic and seasonal maternal influenza, suggesting that it may be symptoms related to infection(34, 35) or general responses to infection, rather than a specific influenza strain, which potentially impact the fetal brain.
Although the cumulative incidence of epilepsy was higher in children exposed to maternal influenza, in adjusted analysis this result had high uncertainty. It is possible that this finding indicates that any potential influence of prenatal influenza exposure on the fetal brain is confined to a lower threshold of febrile seizures only. However, despite using three large population-based data sources, the number of epilepsy cases among children exposed to prenatal maternal influenza was small, and study follow up ended at age seven.
Seizure episodes in childhood are common(7) and represent a substantial burden to caregivers and the health care system. There is strong evidence to support the safety and effectiveness of influenza vaccination during pregnancy,(36) and our findings suggest that preventing influenza during pregnancy may confer additional benefits for the child.
Conclusion
This large prospective cohort study across three high-income countries found that prenatal exposure to maternal influenza was associated with seizures in early childhood, although the evidence supporting an association with early childhood epilepsy was not strong. Associations between maternal influenza in pregnancy and childhood seizures were modest, and consistent across the three different countries. Seizures were linked to influenza infection during the second and third trimesters of pregnancy, while findings for first trimester infection were uncertain.
Supplementary Material
What is already known on this topic.
Maternal infections during pregnancy have been linked to childhood seizures.
Whether prenatal exposure to maternal influenza is linked to seizure disorders in the child is not known.
What this study adds.
We used population-based registry data from Norway, Canada and Australia to investigate the impact of prenatal exposure to maternal influenza on seizures in early childhood.
We found consistent evidence that maternal influenza in pregnancy was associated with a higher risk of seizures in early childhood.
Infections during pregnancy, including influenza, may influence susceptibility to seizures in childhood. Preventing influenza infection during pregnancy through vaccination may confer additional benefits on offspring.
Acknowledgements
The authors are grateful to Better Outcomes Registry & Network (BORN) Ontario, Ottawa, Canada and ICES for providing data access in Ontario, and the Centre for Health Record Linkage, New South Wales, Australia for performing linkage and providing the study dataset for Australia.
Funding
This work was funded by the Research Council of Norway through its Centres of Excellence funding scheme, project number 262700 and by the Norwegian Institute of Public Health. In Ontario, this research was supported by an Operating Grant from the Canadian Institutes of Health Research (AO1-151541), and supported by ICES, a non-profit research institute funded by an annual grant from the Ontario Ministry of Health (MOH) and Ontario Ministry of Long-Term Care (MLTC). In NSW, this research was supported by a National Health and Medical Research Council project grant (GNT 1099655). This research was supported in part by the Intramural Program of the National Institute of Environmental Health Sciences, NIH.
Footnotes
Competing interests
We declare no competing interests.
Disclaimer
The opinions, results, and conclusions reported in this article are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOH or Ontario MLTC is intended or should be inferred. This study is based in part on data provided by Better Outcomes Registry and Network (“BORN”), part of the Children’s Hospital of Eastern Ontario. The interpretation and conclusions contained herein do not necessarily represent those of BORN Ontario. Parts of this material are based on data and/or information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions and statements expressed in the material are those of the author(s), and not necessarily those of CIHI. (Ontario data).
Data from the Norwegian Patient Registry have been used in this publication. The interpretation and reporting of these data are the sole responsibility of the authors, and no endorsement by the Norwegian Patient Registry is intended nor should be inferred.
Data availability statement
The Ontario dataset from this study were linked using unique encoded identifiers and analysed at ICES, where they are held securely in coded form. While data sharing agreements prohibit ICES from making the dataset publicly available, access may be granted to those who meet pre-specified criteria for confidential access, available at www.ices.on.ca/DAS. The full dataset creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are, therefore, either inaccessible or may require modification. The NSW dataset is stored securely at the Curtin University School of Public Health and access is restricted to named investigators in Australia. The Norwegian data set contains personal data and cannot be made public due to confidentiality requirements according to Norwegian legislations. However, researchers who are interested in analysing data from the registries used in this study may apply to the appropriate registry owners after having obtained all necessary approvals according to Norwegian legislations.
References
- 1.Sun Y, Vestergaard M, Christensen J, Nahmias AJ, Olsen J. Prenatal Exposure to Maternal Infections and Epilepsy in Childhood: A Population-Based Cohort Study. Pediatrics. 2008;121:e1100–e7 Online. [DOI] [PubMed] [Google Scholar]
- 2.Miller JE, Pedersen LH, Sun Y, Olsen J. Maternal Use of Cystitis Medication and Childhood Epilepsy in a Danish Population-based Cohort. Paediatr Perinat Epidemiol. 2012;26:589–95 doi: 10.1111/j.1365-3016.2012.01317.x [published Online. [DOI] [PubMed] [Google Scholar]
- 3.Nørgaard M, Ehrenstein V, Nielsen RB, Bakketeig LS, Sørensen HT. Maternal Use of Antibiotics, Hospitalisation for Infection during Pregnancy, and Risk of Childhood Epilepsy: A Population-Based Cohort Study. PLoS ONE. 2012;7:e30850 doi: 10.1371/journal.pone.0030850 [published Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu CS, Pedersen LH, Miller JE, et al. Risk of Cerebral Palsy and Childhood Epilepsy Related to Infections before or during Pregnancy. PLoS ONE. 2013;8:e57552 doi: 10.1371/journal.pone.0057552 [published Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller JE, Pedersen LH, Vestergaard M, Olsen J. Maternal Use of Antibiotics and the Risk of Childhood Febrile Seizures: A Danish Population-Based Cohort. PLoS ONE. 2013;8:e61148 doi: 10.1371/journal.pone.0061148 [published Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whitehead E, Dodds L, Joseph KS, et al. Relation of Pregnancy and Neonatal Factors to Subsequent Development of Childhood Epilepsy: A Population-Based Cohort Study. Pediatrics. 2006;117:1298–306 doi: 10.1542/peds.2005-1660 [published Online. [DOI] [PubMed] [Google Scholar]
- 7.Subcommittee on Febrile Seizures. Febrile Seizures: Guideline for the Neurodiagnostic Evaluation of the Child With a Simple Febrile Seizure. Pediatrics. 2011;127:389–94 doi: 10.1542/peds.2010-3318 [published Online. [DOI] [PubMed] [Google Scholar]
- 8.Vestergaard M, Pedersen CB, Sidenius P, Olsen J, Christensen J. The Long-Term Risk of Epilepsy after Febrile Seizures in Susceptible Subgroups. Am J Epidemiol. 2007;165:911–8 doi: 10.1093/aje/kwk086 [published Online. [DOI] [PubMed] [Google Scholar]
- 9.Bertelsen EN, Larsen JT, Petersen L, Christensen J, Dalsgaard S. Childhood Epilepsy, Febrile Seizures, and Subsequent Risk of ADHD. Pediatrics. 2016;138:e20154654 doi: 10.1542/peds.2015-4654 %J Pediatrics [published Online. [DOI] [PubMed] [Google Scholar]
- 10.Dreier JW, Li J, Sun Y, Christensen J. Evaluation of Long-term Risk of Epilepsy, Psychiatric Disorders, and Mortality Among Children With Recurrent Febrile Seizures: A National Cohort Study in Denmark. JAMA Pediatrics. 2019;173:1164–70 doi: 10.1001/jamapediatrics.2019.3343 %J JAMA Pediatrics [published Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fell DB, Bhutta ZA, Hutcheon JA, et al. Report of the WHO technical consultation on the effect of maternal influenza and influenza vaccination on the developing fetus: Montreal, Canada, September 30-October 1, 2015. Vaccine. 2017;35:2279–87 doi: 10.1016/j.vaccine.2017.03.056 [published Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fell DB, Savitz DA, Kramer MS, et al. Maternal influenza and birth outcomes: systematic review of comparative studies. BJOG. 2017;124:48–59 doi: 10.1111/1471-0528.14143 [published Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Norwegian Institute of Public Health. Medical Birth Registry of Norway. [Google Scholar]
- 14.NSW Department of Health. NSW Perinatal Data Collection [Google Scholar]
- 15.Better Outcomes Registry & Network (BORN) Ontario. About BORN. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Academy of Pediatrics. Febrile Seizures: Long-Term Management of Children with Fever-Associated Seizures. Pediatrics. 1980;66:1009–12 Online. [PubMed] [Google Scholar]
- 17.Deeks Jonathan J, Altman Douglas G, Bradburn. MJ Statistical Methods for Examining Heterogeneity and Combining Results from Several Studies in Meta-Analysis. Systematic Reviews in Health Care 2001:285–312. [Google Scholar]
- 18.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (Clinical research ed). 2003;327:557–60 doi: 10.1136/bmj.327.7414.557 [published Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Legge A, Dodds L, MacDonald NE, Scott J, McNeil SJC. Rates and determinants of seasonal influenza vaccination in pregnancy and association with neonatal outcomes. CMAJ. 2014;186:E157–E64 Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wiley KE, Massey PD, Cooper SC, et al. Uptake of influenza vaccine by pregnant women: a cross-sectional survey. Med J Aust. 2013;198:373–5 Online. [DOI] [PubMed] [Google Scholar]
- 21.Wilcox AJ, Weinberg CR, Basso O. On the Pitfalls of Adjusting for Gestational Age at Birth. Am J Epidemiol. 2011;174:1062–8 doi: 10.1093/aje/kwr230 [published Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bauer AZ, Kriebel D, Herbert MR, Bornehag C-G, Swan SH. Prenatal paracetamol exposure and child neurodevelopment: A review. Horm Behav. 2018;101:125–47 doi: 10.1016/j.yhbeh.2018.01.003 [published Online. [DOI] [PubMed] [Google Scholar]
- 23.Vestergaard M, Obel C, Henriksen TB, et al. The Danish National Hospital Register is a valuable study base for epidemiologic research in febrile seizures. J Clin Epidemiol. 2006;59:61–6 doi: 10.1016/j.jclinepi.2005.05.008 [published Online. [DOI] [PubMed] [Google Scholar]
- 24.Allen HW. The Prevalence and Incidence of Convulsive Disorders in Children. Epilepsia. 1994;35:S1–S6 doi: doi: 10.1111/j.1528-1157.1994.tb05932.x [published Online. [DOI] [PubMed] [Google Scholar]
- 25.Aaberg KM, Gunnes N, Bakken IJ, et al. Incidence and Prevalence of Childhood Epilepsy: A Nationwide Cohort Study. Pediatrics. 2017;139:e20163908 doi: 10.1542/peds.2016-3908 [published Online. [DOI] [PubMed] [Google Scholar]
- 26.Meeraus WH, Petersen I, Chin RF, Knott F, Gilbert R. Childhood epilepsy recorded in primary care in the UK. Arch Dis Child. 2013;98:195–202 doi: 10.1136/archdischild-2012-302237 [published Online. [DOI] [PubMed] [Google Scholar]
- 27.Kim H, Thurman DJ, Durgin T, Faught E, Helmers S. Estimating epilepsy incidence and prevalence in the US pediatric population using nationwide health insurance claims data. J Child Neurol. 2016;31:743–9 Online. [DOI] [PubMed] [Google Scholar]
- 28.Boulanger-Bertolus J, Pancaro C, Mashour GA. Increasing Role of Maternal Immune Activation in Neurodevelopmental Disorders. Front Behav Neurosci. 2018;12 doi: 10.3389/fnbeh.2018.00230 [published Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cordeiro CN, Tsimis M, Burd I. Infections and Brain Development. Obstet Gynecol Surv. 2015;70:644–55 doi: 10.1097/OGX.0000000000000236 [published Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brown AS, Derkits EJ. Prenatal Infection and Schizophrenia: A Review of Epidemiologic and Translational Studies. Am J Psychiatry. 2010;167:261–80 doi: 10.1176/appi.ajp.2009.09030361 [published Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.al-Haddad BJS, Jacobsson B, Chabra S, et al. Long-term Risk of Neuropsychiatric Disease After Exposure to Infection In Utero. JAMA Psychiatry. 2019;76:594–602 doi: 10.1001/jamapsychiatry.2019.0029 [published Online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Borren I, Tambs K, Gustavson K, et al. Early prenatal exposure to pandemic influenza A (H1N1) infection and child psychomotor development at 6 months–A population-based cohort study. Early Hum Dev. 2018;122:1–7 Online. [DOI] [PubMed] [Google Scholar]
- 33.Zerbo O, Qian Y, Yoshida C, Fireman BH, Klein NP, Croen LA. Association Between Influenza Infection and Vaccination During Pregnancy and Risk of Autism Spectrum Disorder. JAMA Pediatr. 2017;171:e163609–e doi: 10.1001/jamapediatrics.2016.3609 [published Online. [DOI] [PubMed] [Google Scholar]
- 34.Dreier JW, Andersen A-MN, Berg-Beckhoff G. Systematic Review and Meta-analyses: Fever in Pregnancy and Health Impacts in the Offspring. Pediatrics. 2014;133:e674–e88 Online. [DOI] [PubMed] [Google Scholar]
- 35.Flinkkilä E, Keski-Rahkonen A, Marttunen M, Raevuori A. Prenatal Inflammation, Infections and Mental Disorders. Psychopathology. 2016;49:317–33 Online. [DOI] [PubMed] [Google Scholar]
- 36.Fell DB, Tapia MD, Nunes MC. Chapter 7 - Influenza. In: Leuridan EE, Nunes MC, Jones CE, eds. Maternal Immunization: Academic Press; 2020:131–67. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The Ontario dataset from this study were linked using unique encoded identifiers and analysed at ICES, where they are held securely in coded form. While data sharing agreements prohibit ICES from making the dataset publicly available, access may be granted to those who meet pre-specified criteria for confidential access, available at www.ices.on.ca/DAS. The full dataset creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are, therefore, either inaccessible or may require modification. The NSW dataset is stored securely at the Curtin University School of Public Health and access is restricted to named investigators in Australia. The Norwegian data set contains personal data and cannot be made public due to confidentiality requirements according to Norwegian legislations. However, researchers who are interested in analysing data from the registries used in this study may apply to the appropriate registry owners after having obtained all necessary approvals according to Norwegian legislations.


