Abstract
Objectives:
Masked hypertension (MH) -- a blood pressure (BP) phenotype characterized by a clinic BP in the normal range but elevated BP outside the office – is associated with early hypertension-mediated organ damage. This study examined early target organ manifestations of MH diagnosed by home (HBPM) and ambulatory (ABPM) BP monitoring.
Methods:
Left ventricular (LV) structure and diastolic function measured by echocardiography, urinary microalbumin, and coronary artery calcification were evaluated in 420 patients with high clinic BP (systolic BP 120 – 150 mmHg or diastolic BP 80 - 95 mmHg). Evidence of hypertension-mediated organ damage was compared in patients with sustained normotension, MH, and sustained hypertension based on measurements by HBPM, daytime ABPM, and 24-hour ABPM.
Results:
The 420 participants averaged 48 (12) [mean (SD)] years of age; the average clinic BP was 130 (13)/81 (8) mmHg. In subjects with MH diagnosed by HBPM, indexed LV mass, relative wall thickness, and e’ and E/e’ (indices of LV relaxation), were generally intermediate between values observed in normotensives and sustained hypertensives, and were significantly greater in MH than normotensives. Similar trends were observed when MH was diagnosed by ABPM, but a diagnosis of MH was not as reliably associated with LV remodeling or impaired LV relaxation in comparison to normotensives. There were trends towards greater likelihoods of detectable urinary microalbumin and coronary calcification in MH than in normotensives.
Conclusions:
These results support previous studies demonstrating early hypertension-mediated organ damage in patients with MH, and suggest that HBPM may be superior to ABPM in identifying patients with MH who have early LV remodeling and diastolic LV dysfunction.
Keywords: masked hypertension, ambulatory blood pressure monitoring, home blood pressure monitoring, left ventricular mass, diastolic function, albuminuria, coronary artery calcium
Introduction:
Masked hypertension (MH) is a distinct blood pressure (BP) phenotype characterized by a clinic BP in the normal range but elevated BP outside the office. Recent studies suggest that the prevalence of MH in adult patients is between 10 and 25% [1-5], and may be even greater in patients with borderline elevated office BP. [6]
There is evidence that individuals with MH are at higher risk of adverse events than those with sustained normotension (i.e., normal BP in and out of the office), and that the incidence of cardiovascular events approaches that observed in patients with sustained hypertension (i.e., high BP both in and out of the office). [1-4,7,8] This increased cardiovascular morbidity may be a manifestation of hypertension-mediated organ damage in patients with MH. Cross-sectional studies have demonstrated a greater left ventricular (LV) mass index in subjects with MH compared to those with sustained normotension. [9-12] Others have found that MH is characterized by impaired LV diastolic function [13], increased carotid intima-media thickness [12], and microalbuminuria. [11,14] Many of these studies have been performed in cohorts that included patients with treated hypertension. The methods for diagnosing MH have varied; in most studies out-of-office BP has been determined by either home BP monitoring (HBPM) or ambulatory BP monitoring (ABPM), but few have examined both.
In this analysis, we (1) compared measures of hypertension-mediated organ damage (LV structure, LV diastolic function, urinary microalbumin, and coronary artery calcification) in patients with normotension, MH, and sustained hypertension; and (2) examined whether MH was more reliably associated with hypertension-mediated organ damage when diagnosed by HBPM or ABPM.
Methods:
Subjects:
We recruited 420 adults from primary care clinics through a combination of passive and active recruitment strategies. To be eligible, potential subjects had to be > 30 years of age with no diagnosis of hypertension and on no BP-lowering drugs; and have a systolic BP of 120-150 mmHg or diastolic BP of 80-95 mmHg on their most recent clinic visit. Exclusion criteria included pregnancy, clinical cardiovascular disease, diabetes, persistent atrial fibrillation or other cardiac arrhythmia, dementia, and any condition that would preclude wearing an ambulatory BP monitor. Potential participants were also excluded if the average BP on the first visit to the research clinic was ≥160/100 mmHg or < 110/70 mmHg.
BP measurement:
All subjects underwent BP measurement in the research clinic, by HBPM, and by ABPM. Details of BP measurement techniques have been described previously. [6]
Research clinic BP measurements were performed on 4 visits to the clinical research center over the course of 10 days. On each visit, 3 seated measurements were acquired after 5 minutes of rest using a validated oscillometric device (Welch Allen “Vital Signs”, Skaneateles Falls, NY, USA). [15] The office BP was calculated as the average of the second and third measurements from the research clinic visits.
HBPM measurements were acquired using a validated oscillometric home monitor (Omron 705CP). [16] Participants were carefully instructed in HBPM techniques, and were asked to perform a series of measurements on 5 consecutive days. After a 5 minute rest, BP was measured 3 times in the morning and 3 times in the evening. For each home series, the first 2 days of measurements and the first measurement of each set of measurements was discarded. The remaining 12 measurements were averaged and defined as the home BP. [17]
Twenty-four hour ABPM was performed using an Oscar 2 oscillometric monitor (Suntech Medical, Morrisville, NC), a device that has been independently validated. [18,19] The monitors were programmed to measure BP at 30 minute intervals during the day and at 1 hour intervals at night. A minimum of 14 awake readings and 6 sleep measurements was required for an ABPM session to be considered adequate. [20] The mean values for awake and 24-hour BPs were calculated.
For this analysis, a normal clinic BP was defined as < 140/90 mmHg, a normal home BP was defined as < 135/85 mmHg, a normal awake ambulatory BP was defined as < 135/85 mmHg, and a normal 24-hour ambulatory BP was defined as < 130/80 mmHg. Using HBPM, normotension was defined as normal office and normal home BPs; MH as normal office but elevated home BPs; and sustained hypertension as elevated office and home BPs. A similar classification scheme was employed using awake and 24-hour ambulatory BPs as the referent out-of-office measurement techniques.
Assessment of hypertension-mediated organ damage:
Cardiac ultrasound studies were performed in the University of North Carolina research echocardiography laboratory. Two-dimensional images of the LV, pulsed wave Doppler transmitral flow velocity profiles, and tissue Doppler profiles of the septal mitral annular motion were acquired and stored in DICOM format for subsequent quantification by a single blinded observer (AH) using an off-line analysis system. All measurements were performed on three cardiac cycles and averaged. LV end-diastolic diameter (LVEDD), posterior wall thickness (PWT), and interventricular septal thickness (IVST) were measured at end-diastole just distal to the mitral valve tips. LV mass was estimated using a cube function model with a correction factor, as described in the American Society of Echocardiography Recommendations on the Use of Echocardiography in Adult Hypertension. [21] To adjust for variations in heart size due to differences in body size, indexed LV mass was calculated as LV mass/height2.7. [22] Relative wall thickness, an index of concentric remodeling of the LV, was calculated as (PWT+IVST)/LVEDD. Measures of LV diastolic function included peak early diastolic mitral annulus velocity (e’) and the ratio of the early (E) transmitral Doppler flow velocity to e’ (E/e’ ratio). Lower values for e’ and greater values for E/e’ suggest impaired LV relaxation.
Coronary artery calcium was assessed by cardiac computed tomography (CT) in a subset of subjects (n = 322) that consented to this procedure. Studies are performed on a 64-slice dual source scanner (Somatom Definition, Siemens, Forchheim, Germany). When heart rate and scan time could be minimized the prospectively gated sequential scanning mode was utilized in order to reduce radiation exposure, otherwise spiral acquisitions were performed. All studies were read by a single cardiologist with training and expertise in cardiac CT (LK) who was blinded to clinical and BP data. All lesions with a detection threshold of > 130 HU were identified. Images were scored for the presence or absence of coronary calcium, and if present the coronary artery calcium load was computed using the method described by Agatston, et al. [23]
Urinary albumin (using an immunoturbidometric assay) and creatinine (by a kinetic assay) were measured on a single morning spot urine specimen. The lower limit of detection of albumin was 0.6 mg/dl. Values for albumin were categorized as detectable or not, and microalbuminuria was defined as > 30 mg albumin/g creatinine.
Demographic and anthropomorphic data:
Demographic data were collected by self-administered questionnaire. Height and weight were measured at the first clinic visit for calculation of body mass index (BMI).
Study approval:
This study was conducted with the understanding and the consent of each participant, and was approved by the Office of Human Research Ethics at the University of North Carolina at Chapel Hill.
Analyses:
Anthropomorphic and demographic characteristics of the study cohort were calculated as mean ± standard deviation or median (25th and 75th percentile), or number (%).
For each method of measuring out-of-office BP, mean (SD) or median (range) values of measures of target organ damage were calculated for patients with true normotension, masked hypertension, and sustained hypertension. Differences between values for masked hypertension and normotension, and sustained hypertension and normotension, were analyzed by two sample t-tests if the outcome was continuous and normally distributed, and by Mann-Whitney tests if the outcome was continuous but non-normally distributed. Chi-squared tests were used if the outcome was categorical. Differences between the subjects in the 3 blood pressure categories were examined by analysis of variance (ANOVA) adjusted for age, race, gender, and body mass index.
Results:
Characteristics of the study participants are shown in Table 1. The mean age was [mean (SD)] 48 (12) years; most were between 30 and 44 years of age (43%) or between 45 and 64 years of age (46%). Slightly over half were female, and 21% were black. Most subjects were overweight (34%) or obese (38%). The average clinic BP was 130 (13)/81 (8) mmHg. Home BP was slightly lower, and both daytime and 24-hour ambulatory BP’s were higher, than office BP.
Table 1.
Participant characteristics (N = 420)
| Characteristic | Mean (SD) or Number [%] |
|---|---|
| Age (yr) | 48 (12) |
| Female sex | 237 [56] |
| Race | |
| Black | 90 [21] |
| White | 314 [75] |
| Other | 16 [4] |
| Hispanic ethnicity | 17 [4] |
| Body mass index (kg/m2) | 29 (6) |
| Nonsmoker | 389 [93] |
| Total cholesterol (mg/dl) | 200 (37) |
| LDL cholesterol (mg/dl) | 143 (38) |
| HDL cholesterol (mg/dl) | 57 (18) |
| BP averages | |
| Clinic BP (mmHg) | 130 (13) / 81 (8) |
| Home BP (mmHg) | 127 (11) / 79 (8) |
| Daytime BP (mmHg) | 142 (14) / 84 (9) |
| 24 hr ambulatory BP (mmHg) | 138 (14) / 81 (9) |
| Education level | |
| Some high school | 6 [2] |
| High school graduate | 25 [6] |
| Some college | 81 [19] |
| College graduate | 307 [73] |
BP = blood pressure; HDL = high density lipoprotein; LDL = low density lipoprotein
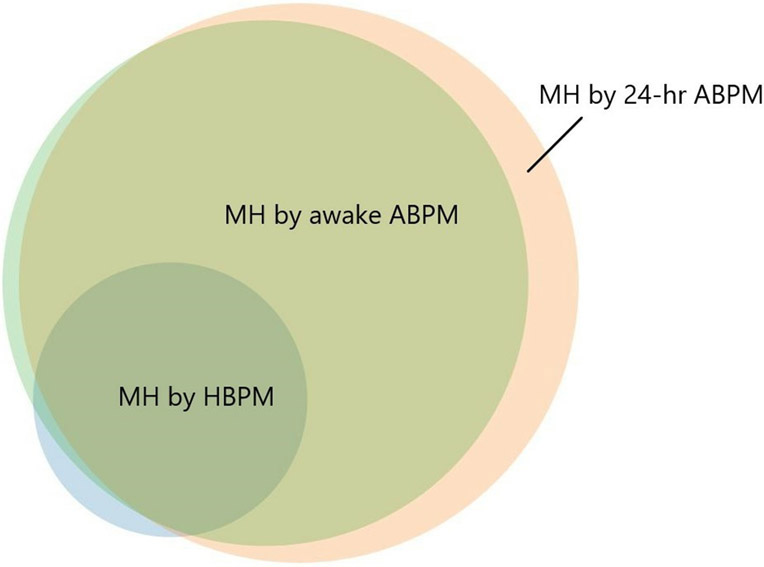
The percentages of subjects diagnosed with each BP phenotype by the 3 methods of out-of-clinic BP measurements are shown in Table 2. The numbers of subjects diagnosed with MH were greater using either measure of ABPM than by using HBPM. The relationships between the participants with MH diagnosed by the 3 methods are illustrated in the Figure. Those with MH by HBPM, for the most part, represented a subset of those diagnosed by ABPM; only 3 of those with MH by HBPM did not have this diagnosis confirmed by 24-hour ABPM, and only 2 did not have MH by awake ABPM. Most (175 of 180) subjects with MH by awake ABPM had this BP phenotype by 24-hour ABPM; an additional 28 subjects had MH by 24-hour ABPM but not awake ABPM.
Table 2.
Number of patients with each BP phenotype according to method of out-of-office BP measurement
| Method of out-of-office measurement |
Sustained normotension |
Masked hypertension | Sustained hypertension |
|---|---|---|---|
| Home BP | 191 | 49 | 60 |
| Daytime ambulatory BP | 114 | 180 | 108 |
| 24-hr ambulatory BP | 90 | 204 | 109 |
BP = blood pressure
Figure.
Venn diagram illustrating relationships of participants with masked hypertension diagnosed by home blood pressure monitoring (HBPM), awake ambulatory blood pressure monitoring (ABPM), and 24-hour ABPM.
Measures of hypertension-mediated organ disease for subjects with normotension, MH, and sustained hypertension as determined by HBPM are shown in Table 3. Indexed LV mass and relative wall thickness were greater in subjects with MH than in normotensives. Similarly, mean values for e’ and E/e’ suggested impaired LV relaxation in MH compared to normotensives. Values for these indices of LV structure and diastolic function were generally intermediate between values observed in patients with normotension and sustained hypertension. Analogous data for BP phenotypes diagnosed by awake and 24-hour ABPM are shown in Tables 4 and 5, respectively. As observed when MH was defined using HBPM, values for LV mass index, relative wall thickness, e’, and E/e’ were generally between values for normotensives and sustained hypertensives. However, a diagnosis of MH was not as reliably associated with ventricular remodeling or impaired LV relaxation in comparison to normotensives.
Table 3.
Hypertension-mediated organ damage by BP phenotype defined by HBPM
| Normotension (n=191) |
Masked HTN (n=49) |
p-value (Masked HTN vs. normotension) |
Sustained HTN (n=60) |
p-value (Sustained HTN vs. normotension) |
p-value between 3 categories |
|
|---|---|---|---|---|---|---|
| Blood pressure | ||||||
| Home systolic BP (mmHg) | 121.5 (7.9) | 134.2 (8.5) | <0.001 | 139.4 (8.3) | <0.001 | <0.001 |
| LV structure | ||||||
| LV mass index | 32.5 (7.6) | 35.2 (6.9) | 0.025 | 36.0 (8.0) | 0.003 | 0.015 |
| LV relative wall thickness | 0.36 (0.06) | 0.39 (0.06) | 0.002 | 0.38 (0.06) | 0.005 | 0.010 |
| LV diastolic function | ||||||
| e’ (cm/s) | 8.8 (2.4) | 7.8 (2.0) | 0.009 | 7.5 (1.6) | <0.001 | <0.001 |
| E/e’ | 8.9 (2.4) | 9.6 (2.2) | 0.070 | 10.1 (2.5) | 0.002 | 0.026 |
| Albuminuria | ||||||
| Albumin/creatinine ratio | 0 (0-727) | 0 (0-141) | 0.159 | 0 (0-5985) | <0.001 | 0.910 |
| Detectable albumin (%) | 19 | 31 | 0.092 | 43 | <0.001 | 0.007 |
| Coronary calcium | ||||||
| Agatston score | 0 (0-5985) | 0 (0-2688) | 0.249 | 0 (0-867) | 0.742 | 0.950 |
| Presence of calcium (%) | 23 | 36 | 0.121 | 25 | 0.775 | 0.122 |
adjusted by race, age, gender, and body mass index
BP = blood pressure; HTN = hypertension; HBPM = home blood pressure monitoring; LV = left ventricular
Table 4.
Hypertension-mediated organ damage by BP phenotype defined by awake ABPM
| Normotension (n=114) |
Masked HTN (n=180) |
p-value (Masked HTN vs. normotension) |
Sustained HTN (n=108) |
p-value (Sustained HTN vs. normotension) |
p-value between 3 categories |
|
|---|---|---|---|---|---|---|
| Blood pressure | ||||||
| Awake ambulatory systolic BP (mmHg) | 127.3 (5.5) | 145.8 (10.8) | <0.001 | 151.1 (13.1) | <0.001 | <0.001 |
| LV structure | ||||||
| LV mass index | 32.2 (7.9) | 34.4 (7.3) | 0.018 | 34.5 (8.0) | 0.027 | 0.005 |
| LV relative wall thickness | 0.37 (0.06) | 0.36 (0.06) | 0.435 | 0.37 (0.06) | 0.190 | 0.451 |
| LV diastolic function | ||||||
| e’ (cm/s) | 8.9 (2.6) | 8.5 (2.1) | 0.165 | 7.6 (1.7) | <0.001 | <0.001 |
| E/e’ | 9.1 (2.5) | 9.1 (2.2) | 0.990 | 9.9 (2.4) | 0.017 | 0.011 |
| Albuminuria | ||||||
| Albumin/creatinine ratio | 0 (0-727) | 0 (0-141) | 0.115 | 0 (0-925) | 0.003 | 0.379 |
| Detectable albumin (%) | 17 | 26 | 0.076 | 35 | 0.002 | 0.006 |
| Coronary calcium | ||||||
| Agatston score | 0 (0-5985) | 0 (0-2688) | 0.387 | 0 (0-867) | 0.121 | 0.543 |
| Presence of calcium (%) | 22 | 26 | 0.527 | 31 | 0.169 | 0.795 |
adjusted by race, age, gender, and body mass index
ABPM = ambulatory blood pressure monitoring; BP = blood pressure; LV = left ventricular
Table 5.
Hypertension-mediated organ damage by BP phenotype defined by 24-hr ABPM
| Normotension (n=90) |
Masked HTN (n=204) |
p-value (Masked HTN vs. normotension) |
Sustained HTN (n=109) |
p-value (Sustained HTN vs. normotension) |
p-value between 3 categories |
|
|---|---|---|---|---|---|---|
| Blood pressure | ||||||
| 24 hr ambulatory systolic BP (mmHg) | 122.6 (5.1) | 140.6 (10.9) | <0.001 | 146.8 (12.8) | <0.001 | <0.001 |
| LV structure | ||||||
| LV mass index | 32.7 (8.3) | 33.9 (7.3) | 0.219 | 34.7 (7.3) | 0.084 | 0.058 |
| LV relative wall thickness | 0.36 (0.06) | 0.36 (0.06) | 0.846 | 0.37 (0.06) | 0.329 | 0.693 |
| LV diastolic function | ||||||
| e’ (cm/s) | 8.8 (2.6) | 8.5 (2.2) | 0.488 | 7.6 (1.7) | <0.001 | <0.001 |
| E/e’ | 9.1 (2.6) | 9.1 (2.2) | 0.986 | 9.9 (2.4) | 0.026 | 0.010 |
| Albuminuria | ||||||
| Albumin/creatinine ratio | 0 (0-204) | 0 (0-727) | 0.078 | 0 (0-925) | 0.005 | 0.442 |
| Detectable albumin (%) | 16 | 26 | 0.055 | 34 | 0.004 | 0.010 |
| Coronary calcium | ||||||
| Agatston score | 0 (0-631) | 0 (0-5985) | 0.353 | 0 (0-867) | 0.09 | 0.621 |
| Presence of calcium (%) | 22 | 26 | 0.617 | 32 | 0.206 | 0.841 |
adjusted by race, age, gender, and body mass index
ABPM = ambulatory blood pressure monitoring; BP = blood pressure; LV = left ventricular
As shown in Tables 3-5, few subjects had microalbuminuria (i.e., albumin/creatinine ratio > 30 mg/g). However, approximately 25-30% of those with MH had detectable albuminuria, greater than the 15-20% of those with sustained normotension and less than the 35-45% of those with sustained hypertension. Regardless of the method for diagnosing MH, the difference between MH and normotensives did not achieve statistical significance. Similarly, coronary calcium was observed in a minority of the subset of subjects who underwent CT scanning, and there was a nonsignificant trend toward a higher prevalence in MH than in normotensives.
Discussion:
In this cohort, compared to participants with sustained normotension, those with MH had evidence of greater hypertension-mediated organ manifestations, including increased LV mass and relative wall thickness and impaired LV relaxation, and a nonsignificant trend toward a greater prevalence of detectable urinary albumin and coronary artery calcium. The extent of target organ damage was less than that seen in those with sustained hypertension. MH was more reliably associated with early cardiac manifestations of high BP when diagnosed by HBPM than by ABPM.
A number of studies have demonstrated increased left ventricular mass in patients with MH compared to those with normal BP’s outside the clinic. [9-12] Most of these prior analyses have utilized ABPM to define BP phenotypes. In a systematic review and meta-analysis of 12 studies, Cuspidi, et al, reported that left ventricular mass index showed a progressive increase from normotensive to MH to sustained hypertension subjects. [9] There is a paucity of data, however, describing the cardiac consequences of MH defined by HBPM. Hanninen, et al, examined end-organ manifestations of MH as defined by HBPM and ABPM in 261 men and women representative of the general population of Turku, Finland, some of whom were prescribed anti-hypertensive medications. As in our study, individuals with normal office BP but elevated home BP tended to have greater indexed LV mass than those with normal BPs in both settings (p = 0.06), while mean LV mass index values were similar in sustained normotensives and those with MH defined only by ABPM. [11] Our data are also consistent with findings from the Improving Detection of Hypertension study. In a cohort of 408 men and women not on treatment with BP-lowering medications, ambulatory systolic BP was higher than either home or office BP. LV mass index by echocardiography was more closely correlated with home systolic BP than with systolic BP measured either by ABPM or in the office. [24] Among participants with clinic BP < 140/90 mmHg, LV mass index was greater in those with MH by both home and ambulatory monitoring than in those with MH diagnosed by only one method or in those with sustained normotension. [25]
Impaired LV relaxation and elevated left atrial pressure are common findings in patients with hypertension and may ultimately lead to the syndrome of heart failure. [26] Evidence of early diastolic LV dysfunction can be detected in patients with high BP even before the development of LV hypertrophy [27], and MH may predict the future development of diastolic LV dysfunction. [28] We assessed characteristics of LV filling by pulsed wave and tissue Doppler echocardiography. The mitral annulus early diastolic velocity derived by tissue Doppler imaging (e’) and the ratio of early LV filling velocity E to e’ (E/e’) are reproducible indices of LV relaxation. As previously described by Oe, et al, [13] in the Masked Hypertension study, there was a progressive decrease in e’ and increase in E/e’, suggesting worsening left ventricular diastolic function, from normotension to MH to sustained hypertension. In our cohort, HBPM was more effective than ABPM in identifying MH associated with impaired LV relaxation.
Microalbuminuria, defined as urinary albumin > 30 mg/g creatinine, is an important risk factor for cardiovascular disease in patients with or without diabetes or hypertension. [29-31] Even lower levels of albumin excretion within the normal range may be associated with cardiovascular risk. [32-34] The prevalence of microalbuminuria was low in our cohort. Detectable levels of albumin, however, tended to be more common in subjects with MH than in normotensives, and less common than in sustained hypertensives. Similarly, although the majority of our young, relatively healthy subjects who underwent CT scanning had no detectable coronary calcification, there was a trend toward a greater prevalence of coronary calcium in those with MH than in normotensives. Data from a large cohort of asymptomatic patients without known coronary heart disease demonstrate that hypertension is associated with coronary calcification, and that calcification is associated with a higher risk of cardiovascular events in individuals with high blood pressure. [35] We are not aware of other studies that have examined the relationship between MH and coronary calcium.
In our study cohort, average values for awake and 24-hour ABPM were higher than for clinic BP. Clinic BP was measured with meticulous technique, with values acquired after 5 minutes of rest and averaged over multiple visits, and many of our subjects who had modestly elevated BP’s in primary care offices had normal research clinic pressures. Since ambulatory BP was, on average, higher than clinic BP, the prevalence of MH as defined by ABPM was high. Home BP’s tended to be lower than clinic BP’s, however, and thus more subjects were classified as having sustained normotension – and fewer had MH – when the BP phenotype was determined by home monitoring. Similar findings have been described in other cohorts. [24,36] Ambulatory BP tends to exceed clinic BP in young and middle-aged individuals, as enrolled in this study. [37,38] In contrast, home BP is usually less than clinic BP across age ranges. [37] The difference between the prevalences of MH by ambulatory and home monitoring was greater in our cohort than in some previous studies, perhaps due to differences in subject characteristics, monitoring protocols, and BP measurement devices.
MH is associated with a risk of CVD events and all-cause mortality that is twice that seen in normotensive individuals, and similar to the risk observed in sustained hypertensives. [39,40] This observation led to the recommendation in recent guideline statements that patients with elevated BP be screened for MH, and that treatment with antihypertensive medications be considered if MH is documented. [41,42] ABPM has been favored as the optimal method for measuring BP outside the clinic -- and therefore for diagnosing MH -- because of the abundance of data supporting its value in predicting adverse outcomes, independent of office BP. [43] Unfortunately, however, ABPM is not widely available and is associated with some expense. HBPM is an attractive alternative because it, like ABPM, provides incremental value to office measurements in predicting CVD events [43], and because many patients already have home monitoring devices and can acquire out of office data at minimal cost. [44] Effective utilization of this method requires the use of accurate, well-validated monitors; education and counselling of patients so that measurements are made with appropriate technique; accurate recording of values; and reliable transmission of data to health care providers. Our data suggest that HBPM may be the preferred method for diagnosing MH, more reliably identifying patients with early left ventricular remodeling and impaired left ventricular relaxation.
Our study has important strengths. It examined a cohort of patients -- untreated individuals with clinic systolic BPs within 20 mmHg of the partition values generally accepted for initiating medical therapy -- in whom out-of-office BP is important in refining clinical decision-making and in whom MH is relatively common. Although previous studies have examined the relationship of hypertension-mediated organ damage to MH defined on the basis of either home or ambulatory monitoring, few have compared results using these two forms of out-of-office BP measurements. Several limitations also merit acknowledgement. Our ABPM measurement protocol was designed to provide adequate data while minimizing subject burden; the measurement frequency of 30-minute intervals during the day and 60-minute intervals at night is in the range endorsed by some international guidelines [41,45], although more frequent measurement is recommended by others. [46] We measured urinary albumin on a single visit, rather than averaging 3 values. Since our study cohort consisted primarily of untreated middle-aged patients, the findings may not be generalizable to other groups. Our study cohort was relatively small, limiting the statistical power to fully examine some relationships.
In summary, in a cohort of untreated patients with high normal or modestly elevated BP’s, MH was diagnosed more often using ABPM than by using HBPM. In patients with MH, measures of hypertension-mediated organ damage tended to be intermediate between those who are normotensive and those with sustained hypertension. However, MH was more reliably associated with left ventricular remodeling and impaired LV relaxation when diagnosed by HBPM. These results suggest that HBPM may be superior to ABPM in identifying MH patients who have early evidence of target organ damage and who may warrant more aggressive BP lowering therapy.
Conflicts of interests and sources of funding
This study was funded by grant R01 HL098604 from the National Heart, Lung, and Blood Institute, with additional support provided through grant UL1 RR025747 from the National Institutes of Health.
Dr. Viera serves on the Medical Advisory Board of Suntech Medical, manufacturer of the Oscar 2 ambulatory BP monitor. For the remaining authors none were declared.
References
- 1.Björklund K, Lind L, Zethelius B, Andrén B, Lithell H. Isolated ambulatory hypertension predicts cardiovascular morbidity in elderly men. Circulation 2003; 107:1297–1302. [DOI] [PubMed] [Google Scholar]
- 2.Hansen TW, Jeppesen J, Rasmussen S, Ibsen H, Torp-Pedersen C. Ambulatory blood pressure monitoring and risk of cardiovascular disease: a population based study. Am J Hypertens 2006; 19:243–50. [DOI] [PubMed] [Google Scholar]
- 3.Ohkubo T, Kikuya M, Metoki H, Asayama K, Obara T, Hashimoto J, et al. Prognosis of “masked” hypertension and “white-coat” hypertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J Am Coll Cardiol 2005; 46:508–15. [DOI] [PubMed] [Google Scholar]
- 4.Diaz KM, Veerabhadrappa P, Brown MD, Whited MC, Dubbert PM, Hickson DA. Prevalence, Determinants, and Clinical Significance of Masked Hypertension in a Population-Based Sample of African Americans: The Jackson Heart Study. Am J Hypertens 2015; 28:900–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang YC, Shimbo D, Muntner P, Moran AE, Krakoff LR, Schwartz JE. Prevalence of Masked Hypertension among US Adults with Nonelevated Clinic Blood Pressure. Am J Epidemiol 2017; 185:194–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Viera AJ, Lin F-C, Tuttle LA, Olsson E, Stankevitz K, Girdler SS, et al. Reproducibility of masked hypertension among adults 30 years or older. Blood Press Monit 2014; 19:208–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mancia G, Facchetti R, Bombelli M, Grassi G, Sega R. Long-term risk of mortality associated with selective and combined elevation in office, home, and ambulatory blood pressure. Hypertens (Dallas, Tex 1979) 2006; 47:846–53. [DOI] [PubMed] [Google Scholar]
- 8.Fagard RH, Van Den Broeke C, De Cort P. Prognostic significance of blood pressure measured in the office, at home and during ambulatory monitoring in older patients in general practice. J Hum Hypertens 2005; 19:801–7. [DOI] [PubMed] [Google Scholar]
- 9.Cuspidi C, Sala C, Tadic M, Rescaldani M, Grassi G, Mancia G. Untreated masked hypertension and subclinical cardiac damage: A systematic review and meta-analysis. Am J Hypertens 2015; 28:806–813. [DOI] [PubMed] [Google Scholar]
- 10.Redmond N, Booth JN, Tanner RM, Diaz KM, Abdalla M, Sims M, et al. Prevalence of masked hypertension and its association with subclinical cardiovascular disease in African Americans: Results from the Jackson heart study. J Am Heart Assoc 2015; 5:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hänninen M-RA, Niiranen TJ, Puukka PJ, Jula AM. Comparison of home and ambulatory blood pressure measurement in the diagnosis of masked hypertension. J Hypertens 2010; 28:709–714. [DOI] [PubMed] [Google Scholar]
- 12.Wojciechowska W, Stolarz-Skrzypek K, Olszanecka A, Klima Ł, Gąsowski J, Grodzicki T, et al. Subclinical arterial and cardiac damage in white-coat and masked hypertension. Blood Press 2016; 25:249–256. [DOI] [PubMed] [Google Scholar]
- 13.Oe Y, Shimbo D, Ishikawa J, Okajima K, Hasegawa T, Diaz KM, et al. Alterations in diastolic function in masked hypertension: Findings from the masked hypertension study. Am J Hypertens 2013; 26:808–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agarwal R. Albuminuria and masked uncontrolled hypertension in chronic kidney disease. Nephrol Dial Transplant 2017; 32:2058–2065. [DOI] [PubMed] [Google Scholar]
- 15.Jones CR, Taylor K, Poston L, Shennan AH. Validation of the Welch Allyn “Vital Signs” oscillometric blood pressure monitor. J Hum Hypertens 2001; 15:191–195. [DOI] [PubMed] [Google Scholar]
- 16.O’Brien E, Mee F, Atkins N, Thomas M. Evaluation of three devices for self-measurement of blood pressure according to the revised British Hypertension Society Protocol: the Omron HEM-705CP, Philips HP5332, and Nissei DS-175. Blood Press Monit 1996; 1:55–61. [PubMed] [Google Scholar]
- 17.Verberk WJ, Kroon AA, Kessels AGH, Lenders JWM, Thien T, van Montfrans GA, et al. The optimal scheme of self blood pressure measurement as determined from ambulatory blood pressure recordings. J Hypertens 2006; 24:1541–1548. [DOI] [PubMed] [Google Scholar]
- 18.Jones SC, Bilous M, Winship S, Finn P, Goodwin J. Validation of the OSCAR 2 oscillometric 24-hour ambulatory blood pressure monitor according to the International Protocol for the validation of blood pressure measuring devices. Blood Press Monit 2004; 9:219–223. [DOI] [PubMed] [Google Scholar]
- 19.Goodwin J, Bilous M, Winship S, Finn P, Jones SC. Validation of the Oscar 2 oscillometric 24-h ambulatory blood pressure monitor according to the British Hypertension Society protocol. Blood Press Monit 2007; 12:113–117. [DOI] [PubMed] [Google Scholar]
- 20.Thijs L, Hansen TW, Kikuya M, Björklund-Bodegård K, Li Y, Dolan E, et al. The International Database of Ambulatory Blood Pressure in relation to Cardiovascular Outcome (IDACO): protocol and research perspectives. Blood Press Monit 2007; 12:255–262. [DOI] [PubMed] [Google Scholar]
- 21.Sharman JE, Hare JL, Thomas S, Davies JE, Leano R, Jenkins C, et al. Association of masked hypertension and left ventricular remodeling with the hypertensive response to exercise. Am J Hypertens 2011; 24:898–903. [DOI] [PubMed] [Google Scholar]
- 22.de Simone G, Daniels SR, Devereux RB, Meyer RA, Roman MJ, de Divitiis O, et al. Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and impact of overweight. J Am Coll Cardiol 1992; 20:1251–1260. [DOI] [PubMed] [Google Scholar]
- 23.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte MJ, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990; 15:827–832. [DOI] [PubMed] [Google Scholar]
- 24.Schwartz JE, Muntner P, Kronish IM, Burg MM, Pickering TG, Bigger JT, et al. Reliability of Office, Home, and Ambulatory Blood Pressure Measurements and Correlation With Left Ventricular Mass. J Am Coll Cardiol 2020; 76:2911–2922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Anstey DE, Muntner P, Bello NA, Pugliese DN, Yano Y, Kronish IM, et al. Diagnosing Masked Hypertension Using Ambulatory Blood Pressure Monitoring, Home Blood Pressure Monitoring, or Both? Hypertension 2018; 72:1200–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115mmHg, 1990–2015. JAMA 2017; 317:165–182. [DOI] [PubMed] [Google Scholar]
- 27.Aeschbacher BC, Hutter D, Fuhrer J, Weidmann P, Delacrétaz E, Allemann Y. Diastolic dysfunction precedes myocardial hypertrophy in the development of hypertension. Am J Hypertens 2001; 14:106–113. [DOI] [PubMed] [Google Scholar]
- 28.Wei F-F, Yang W-Y, Thijs L, Zhang Z-Y, Cauwenberghs N, Van Keer J, et al. Conventional and Ambulatory Blood Pressure as Predictors of Diastolic Left Ventricular Function in a Flemish Population. J Am Heart Assoc 2018; 7. doi: 10.1161/JAHA.117.007868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bigazzi R, Bianchi S, Baldari D, Campese VM. Microalbuminuria predicts cardiovascular events and renal insufficiency in patients with essential hypertension. J Hypertens 1998; 16:1325–1333. [DOI] [PubMed] [Google Scholar]
- 30.Jensen JS, Feldt-Rasmussen B, Strandgaard S, Schroll M, Borch-Johnsen K. Arterial hypertension, microalbuminuria, and risk of ischemic heart disease. Hypertens (Dallas, Tex 1979) 2000; 35:898–903. [DOI] [PubMed] [Google Scholar]
- 31.Dinneen SF, Gerstein HC. The association of microalbuminuria and mortality in non-insulin-dependent diabetes mellitus. A systematic overview of the literature. Arch Intern Med 1997; 157:1413–1418. [PubMed] [Google Scholar]
- 32.Ärnlöv J, Evans JC, Meigs JB, Wang TJ, Fox CS, Levy D, et al. Low-grade albuminuria and incidence of cardiovascular disease events in nonhypertensive and nondiabetic individuals: The framingham heart study. Circulation 2005; 112:969–975. [DOI] [PubMed] [Google Scholar]
- 33.Klausen K, Borch-Johnsen K, Feldt-Rasmussen B, Jensen G, Clausen P, Scharling H, et al. Very low levels of microalbuminuria are associated with increased risk of coronary heart disease and death independently of renal function, hypertension, and diabetes. Circulation 2004; 110:32–35. [DOI] [PubMed] [Google Scholar]
- 34.Gerstein HC, Mann JF, Yi Q, Zinman B, Dinneen SF, Hoogwerf B, et al. Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA 2001; 286:421–426. [DOI] [PubMed] [Google Scholar]
- 35.Graham G, Blaha MJ, Budoff MJ, Rivera JJ, Agatston A, Raggi P, et al. Impact of coronary artery calcification on all-cause mortality in individuals with and without hypertension. Atherosclerosis 2012; 225:432–437. [DOI] [PubMed] [Google Scholar]
- 36.Schwartz JE, Burg MM, Shimbo D, Broderick JE, Stone AA, Ishikawa J, et al. Clinic Blood Pressure Underestimates Ambulatory Blood Pressure in an Untreated Employer-Based US Population. Circulation 2016; 134:1794–1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ishikawa J, Ishikawa Y, Edmondson D, Pickering TG, Schwartz JE. Age and the difference between awake ambulatory blood pressure and office blood pressure: a meta-analysis. Blood Press Monit 2011; 16:159–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Conen D, Aeschbacher S, Thijs L, Li Y, Boggia J, Asayama K, et al. Age-specific differences between conventional and ambulatory daytime blood pressure values. Hypertension 2014; 64:1073–1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stergiou GS, Asayama K, Thijs L, Kollias A, Niiranen TJ, Hozawa A, et al. Prognosis of white-coat and masked hypertension: International Database of HOme blood pressure in relation to Cardiovascular Outcome. Hypertens (Dallas, Tex 1979) 2014; 63:675–682. [DOI] [PubMed] [Google Scholar]
- 40.Pierdomenico SD, Cuccurullo F. Prognostic value of white-coat and masked hypertension diagnosed by ambulatory monitoring in initially untreated subjects: an updated meta analysis. Am J Hypertens 2011; 24:52–58. [DOI] [PubMed] [Google Scholar]
- 41.Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertens (Dallas, Tex 1979) 2017; :HYP.0000000000000065. [Google Scholar]
- 42.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 2018; 39:3021–3104. [DOI] [PubMed] [Google Scholar]
- 43.Siu AL, U.S. Preventive Services Task Force. Screening for high blood pressure in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med 2015; 163:778–86. [DOI] [PubMed] [Google Scholar]
- 44.Viera AJ, Cohen LW, Mitchell CM, Sloane PD. How and why do patients use home blood pressure monitors? Blood Press Monit 2008; 13:133–137. [DOI] [PubMed] [Google Scholar]
- 45.Krause T, Lovibond K, Caulfield M, McCormack T, Williams B, Guideline Development Group. Management of hypertension: summary of NICE guidance. BMJ 2011; 343:d4891. [DOI] [PubMed] [Google Scholar]
- 46.Stergiou GS, Palatini P, Parati G, O’Brien E, Januszewicz A, Lurbe E, et al. 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens 2021; 39:1293–1302. [DOI] [PubMed] [Google Scholar]