Abstract
We tested the hypothesis that exposure of extracellular Mycobacterium tuberculosis to low concentrations (<100 ppm) of nitric oxide (NO) for short periods (24 h or less) will result in microbial killing. We observed that NO had both dose- and time-dependent cidal effects that were very significant by two-way analysis of variance (F ratios of 13.4 [P < 0.001] and 98.1 [P < 0.0001], respectively). Conceivably, extracellular bacilli in patients with pulmonary tuberculosis might be vulnerable to exogenous NO.
In healthy humans, nitric oxide (NO) is synthesized from three types of NO synthases, an endothelial type (eNOS), a neuronal type, and an inducible type (iNOS) thought to be important in the intracellular killing of Mycobacterium tuberculosis in vivo (7–9, 12, 13, 17). The dominant mechanism(s) whereby iNOS-derived NO results in microbial killing is still unknown (17). Multiple molecular targets exist, including intracellular targets of peroxynitrite, the product of the reaction between NO and superoxide (19).
Whereas the vasodilatory action of eNOS-derived NO can be reproduced with exogenous (inhaled) NO (14, 16, 18), there has to date been no attempt to reproduce the mycobactericidal action of iNOS-derived NO with exogenous NO. If exogenous NO destroys mycobacteria plated on nutrient-rich growth medium, then it might also destroy extracellular bacilli within the airways of patients with pulmonary tuberculosis. This would accelerate disinfection of the airways, a particularly desirable goal in the era of disease caused by drug-resistant organisms, and reduce the likelihood of drug resistance emerging in susceptible strains during standard therapy (6).
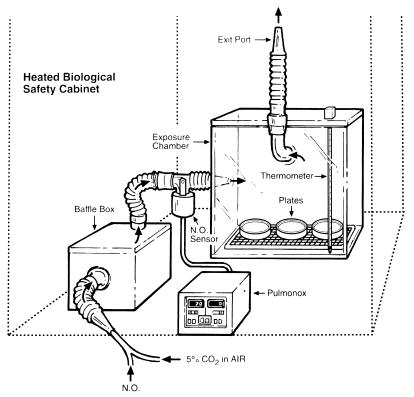
To test the hypothesis that in vitro exposure of M. tuberculosis to NO will result in microbial killing, we built an airtight exposure chamber that could be seated in a heated biological safety cabinet (Fig. 1). This chamber measured 31 by 31 by 21 cm and is made of Plexiglas. It has a lid which can be firmly sealed, a single entry port and a single exit port through which continuous, low-flow, sterile 5 to 10% CO2 in air can pass, and a thermometer. A Y connector in the inflow tubing allows delivery of NO, at predetermined concentrations, to the exposure chamber. Between the Y connector and the exposure chamber is a baffle box which mixes the gases. Finally, between the baffle box and the exposure chamber is placed an in-line NO analyzer (Pulmonox Sensor; Pulmonox Research and Development Corp., Tofield, Alberta, Canada). This analyzer continuously measures the NO concentration in the gas mixture entering the exposure chamber.
FIG. 1.
Exposure chamber and NO delivery system.
On the day before an experiment a precise quantity of actively growing virulent M. tuberculosis was plated on solid medium (Middlebrook 7H10 with oleic acid-albumin-dextrose-catalase enrichment) after careful dilution by McFarland nephelometry (a 1-in-10 dilution that was diluted further to an estimated 103 bacteria/ml; a 0.1-ml inoculum of this suspension was used) (10). Control and test plates were prepared for each experiment. Control plates were placed in a CO2 incubator (Forma Scientific, Marietta, Ohio) and were incubated in a standard fashion at 37°C in 5 to 10% CO2 in air. The test plates were placed in the exposure chamber for a predetermined period of time, after which they were removed and placed in the incubator along with the control plates. The temperature of the exposure chamber was maintained at 32 to 34°C. The colony counts on the control and test plates were measured at 2, 3, and 6 weeks from the day of plating. Reported counts are those measured at 3 weeks and are expressed as a percentage of the control counts.
Experiments were of two varieties: (i) those that involved exposure of the drug-susceptible laboratory strain H37RV to fixed concentrations of sterile NO, i.e., 0 (sham), 25, 50, 70, and 90 ppm, for periods of 3, 6, 12, and 24 h, and (ii) those that involved exposure of a multidrug (isoniazid and rifampin)-resistant wild strain of M. tuberculosis to fixed concentrations of sterile NO, i.e., 70 and 90 ppm, for periods of 3, 6, 12 and 24 h. One experiment with 90 ppm NO and in which both strains of M. tuberculosis were used was extended to allow a total exposure time of 48 h.
The NO analyzer was calibrated at least every third experiment with oxygen (0 ppm of NO) and NO at 83 ppm.
For each NO exposure time and NO concentration studied, at least two and, in most cases, three or four separate experiments were performed with three to six exposure plates per set. The colony counts determined for each exposure plate were expressed as a percentage of the mean colony count for the matched nonexposed control plates. The values from all experiments with each NO concentration and exposure time were then averaged. These data were analyzed by two-way analysis of variance (ANOVA) with the F statistic to test for independent effects of NO exposure time and NO concentration and for the effects of any interaction between them on the colony counts.
With two exceptions the incubation environment exactly simulated the usual incubation environment of M. tuberculosis in a diagnostic laboratory. First, the temperature of our exposure chamber was maintained at 32 to 34°C rather than the usual 37°C to avoid desiccation of the nutrient medium upon which the bacteria were plated, and second, the test plates were openly exposed. That a stable and comparable incubation environment was reproduced was verified in four sham experiments with the H37RV laboratory strain of M. tuberculosis. The colony counts on plates exposed to 5 to 10% CO2 in air (0 ppm NO) at 32 to 34°C in the exposure chamber were not significantly different from those on control plates placed in the laboratory CO2 incubator at 37°C (Table 1).
TABLE 1.
Colony counts after exposure of laboratory strain H37RV of M. tuberculosis to various concentrations of NO for periods of 3, 6, 12, and 24 h
| NO (concn) | Colony count (mean ± SE) at the following exposure times (h)a:
|
|||
|---|---|---|---|---|
| 3 | 6 | 12 | 24 | |
| 0 | 107 ± 5 (6) | 100 ± 5 (6) | 97 ± 9 (6) | 105 ± 5 (18) |
| 25 | 109 ± 6 (12) | 109 ± 4 (12) | 102 ± 3 (12) | 66 ± 4 (18) |
| 50 | 97 ± 5 (12) | 96 ± 2 (12) | 69 ± 3 (12) | 41 ± 5 (18) |
| 70 | 80 ± 10 (7) | 63 ± 12 (7) | 58 ± 12 (11) | 21 ± 6 (11) |
| 90 | 101 ± 15 (11) | 67 ± 7 (11) | 64 ± 7 (14) | 15 ± 3 (15) |
Colony counts are expressed as a percentage of the count for the control. Values in parentheses refer to the number of plates prepared for each NO concentration at each time interval.
Seventeen experiments of the first variety, in which plates were inoculated with a 0.1-ml suspension of 103 bacteria of the H37RV strain of M. tuberculosis per ml were exposed to a fixed concentration (0, 25, 50, 70, or 90 ppm) of NO for increasing periods of time (3, 6, 12, and 24 h), were performed. The results have been pooled and are outlined in Table 1. NO had both dose- and time-dependent cidal effects that were very significant by two-way ANOVA (F ratios, 13.4 [P < 0.001] and 98.1 [P < 0.0001], respectively), and NO also had a statistically significant interactive effect on microbial killing efficacy (F ratio, 2.03 [P < 0.048]). Although there was some variability in the percentage of organisms killed from experiment to experiment increasing the standard error of the pooled data, the dose and time effects were highly reproducible. Only one control plate and one test plate (12-h incubation time with 90-ppm NO) were contaminated. That the effect of NO was cidal and not inhibitory was confirmed by the absence of new colony formation beyond 3 weeks.
Dose-related microbial killing did not appear to increase with NO at a concentration greater than 70 ppm, since the colony counts on plates exposed to NO at 70 and 90 ppm were indistinguishable. At 24 h of NO exposure at both the 70- and 90-ppm levels, more than one-third of the exposed plates were sterile. One experiment with NO at 90 ppm was extended to allow for a total exposure time of 48 h; all of the plates in that experiment were sterile (Table 2).
TABLE 2.
Colony counts after exposure of a multidrug-resistant wild strain of M. tuberculosis to NO for periods of 3, 6, 12, 24, and 48 h
| NO (concn) | Colony count (mean ± SE) at the following exposure timesa:
|
||||
|---|---|---|---|---|---|
| 3 | 6 | 12 | 24 | 48 | |
| 70 | 113 ± 2 (4) | 75 ± 4 (4) | 85 ± 10 (4) | 66 ± 4 (4) | ND |
| 50 ± 25 (4) | 10 ± 5 (4) | ND | |||
| 90 | 97 ± 11 (2) | 91 ± 11 (2) | 71 ± 8 (2) | 36 ± 10 (2) | ND |
| 59 ± 4 (4) | 32 ± 3 (4) | 0 ± 0 (4) | |||
| 79 ± 5 (4)b | 20 ± 3 (4)b | 0 ± 0 (4)b | |||
Colony counts are expressed as a percentage of the count for the control. Each series represents an individual experiment; values in parentheses refer to the number of plates prepared for each experiment at each time interval. ND, not determined.
Results for the H37RV laboratory strain.
Four experiments (two experiments each with NO at 70 and 90 ppm) of the second variety, in which plates were inoculated with a 0.1-ml suspension of 103 bacteria of a multidrug-resistant wild strain of M. tuberculosis per ml were exposed to a fixed concentration (either 70 or 90 ppm) of NO for increasing periods of time (3, 6, 12, and 24 h), were performed. Again, NO had significant dose- and time-dependent cidal effects (Table 2). Although the percent killing at 24 h was less than that observed with strain H37RV, when an inoculum of this strain was exposed to NO at 90 ppm for a period of 48 h, there was also 100% killing.
We have demonstrated that exogenous NO delivered at concentrations of less than 100 ppm exerts a powerful dose- and time-dependent mycobacteriocidal action. This action was observed for both the H37RV laboratory strain and a multidrug-resistant wild strain of M. tuberculosis, suggesting that the mechanism of action of NO is independent of the pharmacologic actions of isoniazid and rifampin.
The relative ease with which NO may be delivered exogenously and the theoretical ability of NO to rapidly destroy the extracellular population of bacilli in the patient with sputum smear-positive pulmonary tuberculosis, especially drug-resistant disease, make NO of great clinical appeal. Consideration of this application of NO, however, raises important caveats. First, would doses of NO of 100 ppm or less delivered over a period of 48 h be safe for humans? Clinical experience indicates that NO is very safe. Doses that are effective in vitro, for example, 80 ppm, are delivered for up to 2 weeks to neonates with hypoxic respiratory failure and persistent pulmonary hypertension without significant adverse effects (14, 16).
Second, would exogenous NO exert negative feedback inhibition of iNOS resulting in a decreased host response to intracellular mycobacteria? Such feedback inhibition has been demonstrated in vitro (1, 4, 5), but whether it occurs in vivo and, if it does, whether it is reversible are unknown.
Third, could population density, which is known to have a profound effect on the microbicidal activities of a variety of agents, be an important determinant of the effect of NO? In order to achieve countable colonies the population density tested in our in vitro system was relatively low, i.e., 103 bacteria or CFU/ml, in comparison to the numbers of bacteria that may be present in the sputum of patients with smear-positive pulmonary tuberculosis (105 to 106 CFU/ml) (20).
Fourth, although NO is known to be extremely soluble (3), would it diffuse into the bronchial mucus or liquid caseum that contains the extracellular bacilli in vivo?
Fifth, might strains of M. tuberculosis vary in their susceptibilities to NO, as has been suggested by others and which appeared to be the case in our study (15)?
Sixth, and finally, might airway injury, an invariable accompaniment of pulmonary tuberculosis (11), reduce ventilation to diseased areas of the lung and limit the access of NO to the very regions that harbor the largest concentrations of bacilli (2)?
Further studies that will examine these questions are being pursued in our laboratory.
Acknowledgments
We are especially grateful to the Mycobacteriology Laboratory staff, especially Sylvia Chomyc and Lisa Meyers at the University of Alberta and Joyce Wolfe at the University of Manitoba, to Krika Duke and John Minski for excellent technical assistance, to Irvin Mayers and Dick Jones for review, and to Susan Falconer for preparation of the manuscript.
REFERENCES
- 1.Assreuy J, Cunha F Q, Liew F Y, Moncada S. Feedback inhibition of nitric oxide synthase activity by nitric oxide. Br J Pharmacol. 1993;108:833–837. doi: 10.1111/j.1476-5381.1993.tb12886.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bass H, Henderson J A M, Heckscher T, Oriol A, Anthonisen N R. Regional structure and function in bronchiectasis. Am Rev Respir Dis. 1968;97:598–609. doi: 10.1164/arrd.1968.97.4.598. [DOI] [PubMed] [Google Scholar]
- 3.Borland C D R, Higgenbottam T W. A simultaneous single breath measurement of pulmonary diffusing capacity with nitric oxide and carbon monoxide. Eur Respir J. 1989;2:56–63. [PubMed] [Google Scholar]
- 4.Buga G M, Griscavage J M, Rogers N E, Ignarro L J. Negative feedback regulation of endothelial cell function by nitric oxide. Circ Res. 1993;73:808–812. doi: 10.1161/01.res.73.5.808. [DOI] [PubMed] [Google Scholar]
- 5.Bult H, De Meyer G R Y, Jordaens F H, Herman A G. Chronic exposure to exogenous nitric oxide may suppress its endogenous release and efficacy. J Cardiovasc Pharmacol. 1991;17:S79–S82. [Google Scholar]
- 6.Canetti G. Present aspects of bacterial resistance in tuberculosis. Am Rev Respir Dis. 1965;92:687–703. doi: 10.1164/arrd.1965.92.5.687. [DOI] [PubMed] [Google Scholar]
- 7.Chan J, Tanaka K, Carroll D, Flynn J, Bloom B R. Effects of nitric oxide synthase inhibitors on murine infection with Mycobacterium tuberculosis. Infect Immun. 1995;63:736–740. doi: 10.1128/iai.63.2.736-740.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan J, Xing R, Magliozzo R S, Bloom B R. Killing of virulent Mycobacterium tuberculosis by reactive nitrogen intermediates produced by activated murine macrophages. J Exp Med. 1992;175:1111–1122. doi: 10.1084/jem.175.4.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Denis M. Interferon-gamma-treated murine macrophages inhibit growth of tubercle bacilli via the generation of reactive nitrogen intermediates. Cell Immunol. 1991;132:150–157. doi: 10.1016/0008-8749(91)90014-3. [DOI] [PubMed] [Google Scholar]
- 10.Hendrickson D A, Krenz M M. Regents and stains. In: Balows A, Hausler W J Jr, Herrmann K L, Isenberg H D, Shadomy H J, editors. Manual of clinical microbiology. 5th ed. Washington, D.C: American Society for Microbiology; 1991. pp. 1289–1314. [Google Scholar]
- 11.Long R, Maycher B, Dhar A, Manfreda J, Hershfield E, Anthonisen N R. Pulmonary tuberculosis treated with directly observed therapy: serial changes in lung structure and function. Chest. 1998;113:933–943. doi: 10.1378/chest.113.4.933. [DOI] [PubMed] [Google Scholar]
- 12.Lowenstein C J, Dinerman J L, Snyder S H. Nitric oxide: a physiologic messenger. Ann Intern Med. 1994;120:227–237. doi: 10.7326/0003-4819-120-3-199402010-00009. [DOI] [PubMed] [Google Scholar]
- 13.Nozaki Y, Hasegawa Y, Ichiyama S, Nakashima I, Shimokata K. Mechanism of nitric oxide-dependent killing of Mycobacterium bovis BCG in human alveolar macrophages. Infect Immun. 1997;65:3644–3647. doi: 10.1128/iai.65.9.3644-3647.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The Neonatal Inhaled Nitric Oxide Study Group. Inhaled nitric oxide in full-term and nearly full-term infants with hypoxic respiratory failure. N Engl J Med. 1997;336:597–604. doi: 10.1056/NEJM199702273360901. [DOI] [PubMed] [Google Scholar]
- 15.O’Brien L, Carmichael J, Lowrie D B, Andrew P W. Strains of Mycobacterium tuberculosis differ in susceptibility to reactive nitrogen intermediates in vitro. Infect Immun. 1994;62:5187–5190. doi: 10.1128/iai.62.11.5187-5190.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roberts J D, Jr, Fineman J R, Morin F C, III, et al. for the Inhaled Nitric Oxide Study Group. Inhaled nitric oxide and persistent pulmonary hypertension of the newborn N Engl J Med 1997336605–610. [DOI] [PubMed] [Google Scholar]
- 17.Rook, G. A. W. 1997. Intractable mycobacterial infections associated with genetic defects in the receptor for interferon gamma: what does this tell us about immunity to mycobacteria? Thorax 52(Suppl. 3):S41–S46. [DOI] [PMC free article] [PubMed]
- 18.Rossaint R, Falke K J, Lopez F, Slama K, Pison U, Zapol W M. Inhaled nitric oxide for the adult respiratory distress syndrome. N Engl J Med. 1993;328:399–405. doi: 10.1056/NEJM199302113280605. [DOI] [PubMed] [Google Scholar]
- 19.Szabo C. The pathophysiological role of peroxynitrite in shock, inflammation and ischemia-reperfusion injury. Shock. 1996;6:79–88. doi: 10.1097/00024382-199608000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Yeager H, Jr, Lacy J, Smith L R, LeMaistre C A. Quantitative studies of mycobacterial populations in sputum and saliva. Am Rev Respir Dis. 1967;95:998–1004. doi: 10.1164/arrd.1967.95.6.998. [DOI] [PubMed] [Google Scholar]