Abstract
gyrA point mutations in 335 clinical Pseudomonas aeruginosa isolates were examined mainly by nonisotopic single-strand conformation polymorphism analysis and direct sequencing. Seven types of missense gyrA mutations were observed in 70 of 335 strains (20.9%), and ciprofloxacin MICs were ≥3.13 μg/ml for 63 of 70 strains (90.0%). These included two double point mutations and three novel mutations (Ala-67→Ser plus Asp-87→Gly, Ala-84→Pro, and Gln-106→Leu). Thr-83→Ile mutants were predominantly observed (63 of 70 mutants) and showed high-level fluoroquinolone resistance (ciprofloxacin MIC at which 50% of isolates are inhibited, 25 μg/ml).
Fluoroquinolones have potent antimicrobacterial activity against gram-positive and -negative bacteria including Pseudomonas aeruginosa, a clinically important pathogen (10). Their targets are considered to be DNA gyrase and topoisomerase IV. Both are essential bacterial type II topoisomerases that catalyze the passage of DNA strands through one another by topological transformation and that are required for cell growth and division. DNA gyrase consists of two each of the A and B subunits, which are encoded by the gyrA and gyrB genes, respectively, and these constitute the active form of the enzyme, A2B2 (4, 21, 23, 28).
The emergence of fluoroquinolone resistance in P. aeruginosa since the introduction of fluoroquinolones into clinical use and the development of resistant mutants during drug therapy have been reported (for reviews, see references 9, 20, and 30). The resistance of this organism has become of clinical importance, because it is associated with therapeutic failures. In P. aeruginosa, several quinolone resistance mechanisms have been proposed. Genetic studies revealed that the gyrA mutation is responsible for quinolone resistance and that the GyrA alteration leads to the resistance of DNA gyrase to inhibition by quinolones (8, 11, 22). Some investigators have reported that the GyrA alteration played a major role in fluoroquinolone resistance in clinical isolates of P. aeruginosa (2, 34).
Single-strand conformation polymorphism (SSCP) analysis is based on the theory that denatured PCR fragments with different sequences migrate differently in a nondenaturing polyacrylamide gel because of their altered folded structures due to a sequence alteration(s) (6, 17). Several investigators have applied SSCP analysis to the detection of gyrA mutations in several bacterial species (3, 14, 19, 24, 25, 29).
In 1994 and 1995, 335 strains of P. aeruginosa were randomly collected from clinical specimens from individual patients at 30 hospitals in Japan. The MICs for the strains were determined by the agar dilution method (12) with approximately 5 × 103 CFU in Mueller-Hinton II agar (BBL, Cockeysville, Md.) after 20 h of incubation at 37°C.
A pair of primers, PaGA1 (5′-TGACGGCCTGAAGCCGGTGCAC) and PaGA4 (5′-TATCGCATGGCTGCGGCGTTG), was synthesized. Their sequences were reported by Kureishi et al. (13). We amplified the region that included codons 38 to 122 to encompass the region containing codons 67 through 106, which has been proved to be the quinolone resistance-determining region in Escherichia coli (33). PCR was carried out as described previously (24), with some modifications.
The SacII site (CCGCGG) is present between nucleotides 248 and 253 in the wild-type gyrA gene, whereas it is absent from the mutant gyrA gene. For restriction fragment length polymorphism (RFLP) analysis, the PCR products were treated with SacII (ToYoBo, Tokyo, Japan) at 37°C for 2 h, and the fragments were separated on a 3% low-melting-point agarose gel, followed by ethidium bromide staining.
For SSCP analysis, the PCR products (2 μl) were mixed with 10 μl of sample buffer (24). After heat denaturation at 94°C for 5 min, samples (11 μl) were separated on a polyacrylamide gel (10% T [total monomer concentration], 2% C [cross-linker concentration]; 12 cm by 13.7 cm by 0.75 mm) containing 5% glycerol in 25 mM Tris–192 mM glycine–2 mM EDTA (18) at 24 ± 0.2°C at a constant voltage of 200 for 9 h and 20 min. The gels were stained with SYBR Green II RNA Gel Stains (TaKaRa Biomedicals, Shiga, Japan) for 20 min to selectively detect single-stranded DNA.
Site-directed mutations were introduced into a plasmid carrying the wild-type P. aeruginosa gyrA gene, pGL2B5 (13), by using the QuickChange Site Directed Mutagenesis Kit (Stratagene, La Jolla, Calif.) according to the manufacturer’s instructions. Two pairs of primers, 5′-CGTGCTACCACA(C/A)CATCTGGCGCTACAGCGGCACG (the desired mutations are underlined) and their respective complementary oligonucleotides were used to introduce the Thr-83→Ile plus Asp-87→His mutation and the Thr-83→Ile plus Asp-87→Asn mutation, respectively; these mutations have been reported previously (31) but were not observed in our 335 strains.
Direct sequencing of the PCR products was carried out as described previously (24), with minor modifications. Oligonucleotides PaGA1 and PaGA4 and oligonucleotide PaGA7 (5′-AACTACGATGGCACCGAG) were used as primers for DNA sequencing.
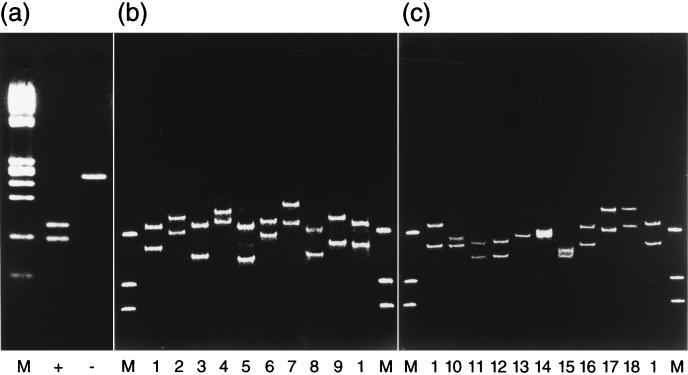
The 335 clinical isolates were examined under the optimized conditions, and PCR products of the expected size were obtained from all strains tested. By SSCP analysis, 18 band patterns could be differentiated, and each pattern corresponded to a distinct mutation. Figure 1 shows the SSCP patterns of the 18 types of sequences. The band patterns were reproducible and distinct from each other. Because RFLP-SSCP analysis is simple and rapid, it would be suitable for epidemiological surveillance.
FIG. 1.
Detection of gyrA mutations by PCR-RFLP analysis (a) and PCR-SSCP analysis of SacII site-positive (b) and -negative (c) DNA. Lanes M, molecular size standard (HaeIII-digested φX174); lane +, SacII site-positive DNA fragment; lane −, SacII site-negative DNA fragment; lanes 1, wild type; lane 2, mutant containing alteration of GCC→GCT at codon 67 (silent); lane 3, mutant containing alteration of CGT→CGA at codon 68 (silent); lane 4, mutant containing alteration of CCG→CCA at codon 79 (silent); lane 5, mutant containing alteration of CGC→CGT at codon 91 (silent); lane 6, mutant containing alteration of Asp-87→Asn; lane 7, mutant containing alterations of CCG→CCA at codon 79 (silent) plus Asp-87→Gly; lane 8, mutant containing alterations of Ala-67→Ser plus Asp-87→Gly; lane 9, mutant containing alteration of Gln-106→Leu; lane 10, mutant containing alteration of Thr-83→Ile; lane 11, mutant containing alterations of CGT→CGA at codon 68 (silent) plus Thr-83→Ile; lane 12, mutant containing alterations of Thr-83→Ile plus CGC→CGT at codon 91 (silent); lane 13, mutant containing alterations of Thr-83→Ile plus Asp-87→Gly; lane 14, mutant containing alterations of Thr-83→Ile plus Asp-87→Asn; lane 15, mutant containing alterations of Thr-83→Ile plus Asp-87→His; lane 16, mutant containing alteration of GCG→GCA at codon 84 (silent); lane 17, mutant containing alteration of Ala-84→Pro; lane 18, mutant containing alterations of GCG→GCA at codon 84 (silent) plus Asp-87→Tyr. Lanes 6 through 13, 17, and 18, quinolone-resistant clinical strains; lanes 14 and 15, mutated plasmids derived from pGL2B5; lanes 16 and 18, generous gifts from T. Schollaardt, namely, P4394 and Y4492, respectively.
Table 1 presents the incidence of the wild-type strains and the 17 mutations, including three novel types (Ala-67→Ser plus Asp-87→Gly, Ala-84→Pro, and Gln-106→Leu), observed among all the strains and plasmids examined. The Thr-83→Ile mutation was the most frequent, while other mutations were rare. Twenty-six strains contained silent mutations, which do not lead to amino acid substitutions.
TABLE 1.
Types of point mutation(s) and respective incidence among the 335 clinical isolates
| SacII site | Type of mutation | Amino acid change | Nucleotide change | Incidence (no. [%] of strains) |
|---|---|---|---|---|
| Positive | Wild type | None | None | 243 (72.5) |
| Silent mutations | Ala-67→Ala (silent) | GCC→GCT | 2 (0.6) | |
| Arg-68→Arg (silent) | CGT→CGA | 9 (2.7) | ||
| Pro-79→Pro (silent) | CCG→CCA | 6 (1.8) | ||
| Arg-91→Arg (silent) | CGC→CGT | 5 (1.5) | ||
| Single missense mutations with or without silent mutation | Asp-87→Asn | GAC→AAC | 2 (0.6) | |
| Pro-79, Asp-87→Pro (silent), Gly | CCG, GAC→CCA, GGC | 1 (0.3) | ||
| Gln-106→Leu | CAG→CTG | 1 (0.3) | ||
| Double missense mutations | Ala-67, Asp-87→Ser, Gly | GCC, GAC→TCC, GGC | 1 (0.3) | |
| Negative | Silent mutation | Ala-84→Ala (silent) | GCG→GCA | 0a |
| Single missense mutations with or without silent mutation | Thr-83→Ile | ACC→ATC | 60 (17.9) | |
| Arg-68, Thr-83→Arg (silent), Ile | CGT, ACC→CGA, ATC | 2 (0.6) | ||
| Thr-83, Arg-91→Ile, Arg (silent) | ACC, CGC→ATC, CGT | 1 (0.3) | ||
| Ala-84→Pro | GCG→CCG | 1 (0.3) | ||
| Ala-84, Asp-87→Ala (silent), Tyr | GCG, GAC→GCA, TAC | 0b | ||
| Double missense mutations | Thr-83, Asp-87→Ile, Gly | ACC, GAC→ATC, GGC | 1 (0.3) | |
| Thr-83, Asp-87→Ile, Asn | ACC, GAC→ATC, AAC | 0c | ||
| Thr-83, Asp-87→Ile, His | ACC, GAC→ATC, CAC | 0c | ||
| Total | 335 (100) |
Table 2 shows the susceptibilities of the 335 clinical strains and strain Y4492 to 10 fluoroquinolones. Most of the strains containing wild-type GyrA were susceptible to all fluoroquinolones tested. Among the drugs tested, ciprofloxacin was the most potent against them (MIC at which 50% of isolates are inhibited [MIC50], 0.20 μg/ml), followed by tosufloxacin and then CS-940 and norfloxacin. When ciprofloxacin resistance was designated as an MIC of ≥3.13 μg/ml, the proportion of resistant strains was 9 of 265 (3.4%) among the strains containing wild-type GyrA. In contrast, this ratio increased to 63 of 70 (90.0%) for GyrA mutants, and this ratio was significantly higher than that for strains containing wild-type GyrA (by the χ2 test, P < 0.001).
TABLE 2.
Susceptibilities of 336 clinical isolates of P. aeruginosa to 10 fluoroquinolones
| Drug | MIC (μg/ml) for strains with the following GyrA alterationsa (type of change):
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PAO1 | Wild type (n = 265)b
|
Thr-83→Ile (PU→NH) (n = 63)
|
Ala-84→Pro (NH→NH) (n = 1) | Asp-87→Gly (−1c→PU) (n = 1) | Asp-87→Asn (−1→PU) (n = 2) | Asp-87→Tyrd (−1→PU) (n = 1) | Gln-106→Leu (PU→NH) (n = 1) | Ala-67, Asp-87→Ser, Gly (NH, −1→PU, PU) (n = 1) | Thr-83, Asp-87→Ile, Gly (PU, −1→NH, PU) (n = 1) | |||||
| Range | 50% | 90% | Range | 50% | 90% | |||||||||
| Norfloxacin | 0.39 | 0.20–100 | 0.78 | 3.13 | 1.56–400 | 100 | 200 | 25 | 12.5 | 1.56, 12.5 | 12.5 | 25 | 12.5 | 200 |
| Ofloxacin | 0.78 | 0.39–100 | 1.56 | 6.25 | 3.13–800 | 50 | 200 | 25 | 12.5 | 3.13, 25 | 12.5 | 25 | 12.5 | 200 |
| Enoxacin | 0.78 | 0.20–200 | 1.56 | 6.25 | 3.13–>400 | 100 | >400 | 25 | 25 | 3.13, 25 | 50 | 25 | 25 | 200 |
| Ciprofloxacin | 0.10 | 0.025–50 | 0.20 | 0.78 | 0.39–400 | 25 | 50 | 6.25 | 3.13 | 0.78, 3.13 | 6.25 | 3.13 | 3.13 | 50 |
| Tosufloxacin | 0.20 | 0.05–>25 | 0.39 | 1.56 | 0.10–>25 | >25 | >25 | 6.25 | 6.25 | 0.78, 1.56 | 3.13 | 1.56 | 6.25 | >25 |
| Lomefloxacin | 0.78 | 0.39–200 | 1.56 | 6.25 | 0.78–800 | 200 | 400 | 50 | 25 | 6.25, 50 | 25 | 50 | 25 | 400 |
| Fleroxacin | 0.78 | 0.20–200 | 1.56 | 6.25 | 3.13–>1,600 | 100 | 400 | 25 | 12.5 | 3.13, 25 | 25 | 25 | 12.5 | 400 |
| Sparfloxacin | 0.78 | 0.20–200 | 1.56 | 3.13 | 1.56–>1,600 | 100 | 200 | 12.5 | 12.5 | 1.56, 12.5 | 12.5 | 25 | 6.25 | 200 |
| Gatifloxacin | 0.78 | 0.20–50 | 1.56 | 3.13 | 1.56–200 | 50 | 100 | 12.5 | 6.25 | 1.56, 6.25 | 6.25 | 12.5 | 6.25 | 50 |
| CS-940 | 0.39 | 0.10–50 | 0.78 | 3.13 | 1.56–800 | 50 | 100 | 6.25 | 3.13 | 0.78, 12.5 | 3.13 | 12.5 | 6.25 | 100 |
Silent mutation is neglected.
n indicates number of strains.
−1, negatively charged.
Strain Y4492.
Mutants with a Thr-83→Ile alteration showed high-level resistance to all 10 fluoroquinolones tested. The MIC50s for mutants with a Thr-83→Ile alteration were from 32-fold higher (ofloxacin and gatifloxacin [AM-1155]) to 128-fold higher (with norfloxacin, ciprofloxacin, tosufloxacin, and lomefloxacin) than the MIC50s for strains containing wild-type GyrA.
Although few strains contained point mutations other than the Thr-83→Ile mutation, the following tendencies were observed. Every type of GyrA mutant containing a missense mutation(s) showed cross-resistance to all fluoroquinolones tested. GyrA mutants containing a Thr-83→Ile alteration showed higher levels of resistance to fluoroquinolones than mutants containing a different single point mutation. Comparing the degree of rise in the MICs or MIC50s of the fluoroquinolones tested for the mutants with the different mutations, the level of deterioration of antibacterial activity was relatively small with gatifloxacin, CS-940, and sparfloxacin, whereas it was high with lomefloxacin, ciprofloxacin, and norfloxacin.
In this study we found that most of the fluoroquinolone-resistant strains of P. aeruginosa possessed a point mutation of the Thr-83→Ile type; this was in accordance with previous reports (15, 32). This mutation was therefore considered to be selected more frequently, such as the Ser-83→Leu mutation in an E. coli mutant selected in a single step (7), and to survive under clinical, selective pressure. Point mutations were localized at codons 67, 83, 84, 87, and 106 and were closely related to fluoroquinolone resistance. In E. coli, gyrA mutations have been reported at codons 67, 81, 82, 83, 84, 87, and 106 (1, 5, 7, 16, 26, 27, 33). The sites of the point mutations in the gyrA gene of P. aeruginosa were nearly identical to those in E. coli. The results indicate that this restricted region probably plays a significant role in the quinolone-gyrase-DNA interaction, although contributions of mutations in other regions of the gyrA gene cannot be completely excluded.
Because the amino acid sequences of the quinolone resistance-determining region of P. aeruginosa is identical to that of E. coli except for that at position 83, the functional role of each residue is also likely to be identical. A Thr-83→Ile mutation in P. aeruginosa and the corresponding Ser-83→Leu, Trp, and Ala mutations reported in E. coli are all polar, uncharged (PU)-to-nonpolar, hydrophobic (NH) amino acid substitutions. Asp-87→Gly, Asn, and Tyr mutations, which are negatively charged-to-PU substitutions, were found in both P. aeruginosa and E. coli. However, Asp-87→His, a negatively charged-to-positively charged substitution, was also observed in P. aeruginosa, and Asp-87→Val, a negatively charged-to-NH substitution, was observed in E. coli. It is likely that a negatively charged amino acid at this position does not express the quinolone resistance phenotype (31). Ala-67→Ser, an NH-to-PU substitution, and Ala-84→Pro, an NH-to-NH substitution, found in this study were the same as those reported for E. coli, although the single mutation at position 67 was not found in our study. Exceptionally, at position 106, Gln→Leu, a PU-to-NH substitution, was observed in this study, while Gln→His and Arg, PU-to-positively charged substitutions, were reported in E. coli; the significance of this difference remains unknown.
Because clinical isolates have various genetic backgrounds, the MIC of a given fluoroquinolone sometimes varied more than 1,024-fold for strains with the same GyrA protein. To elucidate the definite relationship between types of GyrA mutations and the magnitude of resistance, a genetic investigation is under way.
Acknowledgments
We are grateful to T. Schollaardt, the University of Calgary, for generously providing plasmid pGL2B5 and clinical isolates P4394 and Y4492. We also thank K. Fujiwara and M. Ohtsuki, Sankyo Co., Ltd., for meaningful suggestions on DNA manipulations.
REFERENCES
- 1.Cambau E, Bordon F, Collatz E, Gutmann L. Novel gyrA point mutation in a strain of Escherichia coli resistant to fluoroquinolones but not to nalidixic acid. Antimicrob Agents Chemother. 1993;37:1247–1252. doi: 10.1128/aac.37.6.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cambau E, Perani E, Dib C, Petinon C, Trias J, Jarlier V. Role of mutations in DNA gyrase genes in ciprofloxacin resistance of Pseudomonas aeruginosa susceptible or resistant to imipenem. Antimicrob Agents Chemother. 1995;39:2248–2252. doi: 10.1128/aac.39.10.2248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Charvalos E, Peteinaki E, Spyridaki I, Manetas S, Tselentis Y. Detection of ciprofloxacin resistance mutations in Campylobacter jejuni gyrA by nonradioisotopic single-strand conformation polymorphism and direct DNA sequencing. J Clin Lab Anal. 1996;10:129–133. doi: 10.1002/(SICI)1098-2825(1996)10:3<129::AID-JCLA3>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 4.Drlica K, Zhao X. DNA gyrase, topoisomerase IV, and the 4-quinolones. Microbiol Mol Biol Rev. 1997;61:377–392. doi: 10.1128/mmbr.61.3.377-392.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hallett P, Maxwell A. Novel quinolone resistance mutations of Escherichia coli DNA gyrase A protein: enzymatic analysis of the mutant proteins. Antimicrob Agents Chemother. 1991;35:335–340. doi: 10.1128/aac.35.2.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hayashi K. PCR-SSCP: a simple and sensitive method for detection of mutations in the genomic DNA. PCR Methods Appl. 1991;1:34–38. doi: 10.1101/gr.1.1.34. [DOI] [PubMed] [Google Scholar]
- 7.Heisig P, Tschorny R. Characterization of fluoroquinolone-resistant mutants of Escherichia coli selected in vitro. Antimicrob Agents Chemother. 1994;38:1284–1291. doi: 10.1128/aac.38.6.1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hirai K, Suzue S, Irikura T, Iyobe S, Mitsuhashi S. Mutations producing resistance to norfloxacin in Pseudomonas aeruginosa. Antimicrob Agents Chemother. 1987;31:582–586. doi: 10.1128/aac.31.4.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hooper, D. C., and J. S. Wolfson. 1989. Bacterial resistance to the quinolone antimicrobial agents. Am. J. Med. 87(Suppl. 6C):17S–23S. [PubMed]
- 10.Hooper D C, Wolfson J S. Fluoroquinolone antimicrobial agents. N Engl J Med. 1991;324:384–394. doi: 10.1056/NEJM199102073240606. [DOI] [PubMed] [Google Scholar]
- 11.Inoue Y, Sato K, Fujii T, Hirai K, Inoue M, Iyobe S, Mitsuhashi S. Some properties of subunits of DNA gyrase from Pseudomonas aeruginosa PAO1 and its nalidixic acid-resistant mutant. J Bacteriol. 1987;169:2322–2325. doi: 10.1128/jb.169.5.2322-2325.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Japanese Society of Chemotherapy. Revision of methods for determining minimum inhibitory concentrations. Chemotherapy (Tokyo) 1981;29:76–79. . (In Japanese.) [Google Scholar]
- 13.Kureishi A, Diver J M, Beckthold B, Schollaardt T, Bryan L E. Cloning and nucleotide sequence of Pseudomonas aeruginosa DNA gyrase gyrA gene from strain PAO1 and quinolone-resistant clinical isolates. Antimicrob Agents Chemother. 1994;38:1944–1952. doi: 10.1128/aac.38.9.1944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Munakata N, Morohoshi F, Saitou M, Yamazaki N, Hayashi K. Molecular characterization of thirteen gyrA mutations conferring nalidixic acid resistance in Bacillus subtilis. Mol Gen Genet. 1994;244:97–103. doi: 10.1007/BF00280192. [DOI] [PubMed] [Google Scholar]
- 15.Nakano M, Deguchi T, Kawamura T, Yasuda M, Kimura M, Okano Y, Kawada Y. Mutations in the gyrA and parC genes in fluoroquinolone-resistant clinical isolates of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 1997;41:2289–2291. doi: 10.1128/aac.41.10.2289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Oram M, Fisher L M. 4-Quinolone resistance mutations in the DNA gyrase of Escherichia coli clinical isolates identified by using the polymerase chain reaction. Antimicrob Agents Chemother. 1991;35:387–389. doi: 10.1128/aac.35.2.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Orita M, Suzuki Y, Sekiya T, Hayashi K. Rapid and sensitive detection of point mutations and DNA polymorphisms using the polymerase chain reaction. Genomics. 1989;5:874–879. doi: 10.1016/0888-7543(89)90129-8. [DOI] [PubMed] [Google Scholar]
- 18.Oto M, Miyake S, Yuasa Y. Optimization of nonradioisotopic single strand conformation polymorphism analysis with a conventional minislab gel electrophoresis apparatus. Anal Biochem. 1993;213:19–22. doi: 10.1006/abio.1993.1379. [DOI] [PubMed] [Google Scholar]
- 19.Ouabdesselam S, Hooper D C, Tankovic J, Soussy C J. Detection of gyrA and gyrB mutations in quinolone-resistant clinical isolates of Escherichia coli by single-strand conformational polymorphism analysis and determination of levels of resistance conferred by two different single gyrA mutations. Antimicrob Agents Chemother. 1995;39:1667–1670. doi: 10.1128/aac.39.8.1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peterson L R. Quinolone resistance in clinical practice: occurrence and importance. In: Hooper D C, Wolfson J S, editors. Quinolone antimicrobial agents. 2nd ed. Washington, D.C: American Society for Microbiology; 1993. [Google Scholar]
- 21.Reece R J, Maxwell A. DNA gyrase: structure and function. Crit Rev Biochem Mol Biol. 1991;26:335–375. doi: 10.3109/10409239109114072. [DOI] [PubMed] [Google Scholar]
- 22.Robillard N J, Scarpa A L. Genetic and physiological characterization of ciprofloxacin resistance in Pseudomonas aeruginosa PAO. Antimicrob Agents Chemother. 1988;32:535–539. doi: 10.1128/aac.32.4.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roca J. The mechanisms of DNA topoisomerases. Trends Biochem Sci. 1995;20:156–160. doi: 10.1016/s0968-0004(00)88993-8. [DOI] [PubMed] [Google Scholar]
- 24.Takenouchi T, Ishii C, Sugawara M, Tokue Y, Ohya S. Incidence of various gyrA mutants in 451 Staphylococcus aureus strains isolated in Japan and their susceptibilities to 10 fluoroquinolones. Antimicrob Agents Chemother. 1995;39:1414–1418. doi: 10.1128/aac.39.7.1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tokue Y, Sugano K, Saito D, Noda T, Ohkura H, Shimosato Y, Sekiya T. Detection of novel mutations in the gyrA gene of Staphylococcus aureus by nonradioisotopic single-strand conformation polymorphism analysis and direct DNA sequencing. Antimicrob Agents Chemother. 1994;38:428–431. doi: 10.1128/aac.38.3.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Truong Q C, Van J-C N, Shlaes D, Gutmann L, Moreau N J. A novel, double mutation in DNA gyrase A of Escherichia coli conferring resistance to quinolone antibiotics. Antimicrob Agents Chemother. 1997;41:85–90. doi: 10.1128/aac.41.1.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vila J, Ruiz J, Marco F, Barcelo A, Goni P, Giralt E, Jimenez de Anta T. Association between double mutation in gyrA gene of ciprofloxacin-resistant clinical isolates of Escherichia coli and MICs. Antimicrob Agents Chemother. 1994;38:2477–2479. doi: 10.1128/aac.38.10.2477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang J C. DNA topoisomerases. Annu Rev Biochem. 1996;65:635–692. doi: 10.1146/annurev.bi.65.070196.003223. [DOI] [PubMed] [Google Scholar]
- 29.Wang T, Tanaka M, Sato K. Detection of grlA and gyrA mutations in 344 Staphylococcus aureus strains. Antimicrob Agents Chemother. 1998;42:236–240. doi: 10.1128/aac.42.2.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wolfson, J. S., and D. C. Hooper. 1989. Bacterial resistance to quinolones: mechanisms and clinical importance. Rev. Infect. Dis. 11(Suppl. 5):S960–S968. [DOI] [PubMed]
- 31.Yonezawa M, Takahata M, Banawa N, Matsubara N, Watanabe Y, Narita H. Analysis of the NH2-terminal 87th amino acid of Escherichia coli GyrA in quinolone-resistance. Microbiol Immunol. 1995;39:517–520. doi: 10.1111/j.1348-0421.1995.tb02236.x. [DOI] [PubMed] [Google Scholar]
- 32.Yonezawa M, Takahata M, Matsubara N, Watanabe Y, Narita H. DNA gyrase gyrA mutations in quinolone-resistant clinical isolates of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 1995;39:1970–1972. doi: 10.1128/aac.39.9.1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yoshida H, Bogaki M, Nakamura M, Nakamura S. Quinolone resistance-determining region in the DNA gyrase gyrA gene of Escherichia coli. Antimicrob Agents Chemother. 1990;34:1271–1272. doi: 10.1128/aac.34.6.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yoshida H, Nakamura M, Bogaki M, Nakamura S. Proportion of DNA gyrase mutants among quinolone-resistant strains of Pseudomonas aeruginosa. Antimicrob Agents Chemother. 1990;34:1273–1275. doi: 10.1128/aac.34.6.1273. [DOI] [PMC free article] [PubMed] [Google Scholar]