Abstract
We aimed to assess whether high school students’ sleep quality, mental health and learning changed during the COVID-19 pandemic as adolescents transitioned from learning online back to studying in person. We conducted an anonymous online cross-sectional survey study at three competitive high schools in Vilnius, Lithuania, after they were reopened. Students provided subjective views on their study quality, their health as well as daily life while studying either virtually or in person and completed the Beck depression inventory (BDI), the Generalized anxiety scale-7 (GAD-7) and the Pittsburgh sleep quality index (PSQI). Among 628 (70.4% female) respondents, 268 (42.7%), 342 (54.5%) and 398 (63.4%) are suspected to have depression, an anxiety disorder or poor sleep, respectively. Students reported better study quality (Z = −12.435, p < 0.001) and physical health (Z = −9.176, p < 0.001), but worse sleep quality (Z = −19.489, p < 0.001), shorter sleep duration (Z = −19.509, p < 0.001) and worse self-reported mental health (Z = −2.220, p < 0.05) while learning in person. However, higher scores of in-person study quality and physical health were associated with lower depression and anxiety levels as well as better sleep. Our study suggests that the reopening of schools may exacerbate sleep and mental health-related issues among high school students but also be beneficial for their academic development and levels of physical activity.
Keywords: adolescents, anxiety, physical health, survey
1. Introduction
After the worldwide spread of SARS-CoV-2 was declared a pandemic in March 2020, many countries employed nationwide lockdowns to prevent the collapse of their medical systems [1]. One of the restrictive measures enforced during lockdowns was school closures. They were thought to limit the transmission of SARS-CoV-2 among children and adolescents and prevent them from infecting relatives at home [2]. It remains debatable whether this practice helps to effectively decrease the spread of SARS-CoV-2 and if school closures are acceptable at all, considering the benefits schools provide as both educational and societal institutions [3,4,5]. After transitioning to online learning, students faced a completely different daily routine that changed their learning experience, sleep patterns and social interactions [6,7,8]. While it has been argued that lockdowns may disrupt sleep, exacerbate mental health problems and reduce physical student activity, highschoolers could also benefit from later waking hours and flexible learning schedules [9,10,11,12,13,14,15,16]. However, there remains little data on how high school students perceive the return to live education after several months of online learning [17,18,19,20,21].
In recent years, the view of health being a state of “complete well-being” shifted towards a dynamic definition of health, which revolves around the capacity to “react to all kinds of environmental events having the desired emotional, cognitive, and behavioral responses and avoiding those undesirable ones” [22]. Similarly, recent conceptualizations of mental health emphasize that it is “a dynamic state of internal equilibrium which enables individuals to use their abilities in harmony with universal values of society” [23]. Self-rated single-item measures of overall mental health or the evaluation of scales used to detect selected clinical entities (e.g., anxiety, depression or poor quality of sleep) can help to quantify the benefits and disadvantages that the COVID-19 pandemic had for the health of the youngest generations of individuals in our societies [24,25,26]. Moreover, the pandemic, which was a major global environmental event, offers a unique opportunity to review in-person teaching from a public health perspective and raise the possibility of changing school schedules or using widely available online tools to improve the health and daily lives of adolescents.
We report data of a cross-sectional survey conducted at three competitive high schools in Vilnius, Lithuania. The aim of our study was to assess how high school students perceive their (1) sleep, (2) mental health, (3) physical health and (4) learning experience during COVID-19 lockdowns and after school reopening.
We intended to test the following hypotheses:
H1.
High school students perceive their sleep quality to be better and sleep duration to be longer during school closure.
H2.
High school students report worse mental and physical health during lockdowns.
H3.
Online learning is perceived to be of lower quality than learning in person.
H4.
After school reopening, the relationship between quality of sleep and the perceived quality of studies is mediated by symptoms of anxiety and depression.
2. Materials and Methods
2.1. Subjects and Procedure
An online anonymous questionnaire was distributed through closed communication groups among students of three high schools (9th to 12th grade) in Vilnius, the capital of Lithuania, from 20 October 2021 to 20 November 2021. High schools were selected based on their academic performance in the academic year 2020/2021—a non-random convenience sample was sought from the three best performing public schools in the city. The inclusion criteria were being enrolled in one of the three schools and having completed and submitted answers to each item of the questionnaire. Only responses to open-ended survey items judged to be intentionally misleading (e.g., 20 h of commute per day, 30,000 min of being outside daily, etc.) were excluded from the analysis.
2.2. Measures
The questionnaire consisted of ten parts:
Demographic data (age, sex, grade);
Items rated on a scale from 0 to 10: (a) the quality of studies, (b) psychological health, (c) physical health, (d) sleep quality, (e) overall well-being (exhausted vs. well-rested) either at the time of the survey (i.e., while learning in person) or during studies online (i.e., retrospectively);
The average of (a) hours spent studying, (b) hours of sleep, (c) minutes spent outside and (d) minutes of physical activity (including fast-paced walking) per day either at the time of the survey or during studies online;
The average hours of commute while learning in person;
The perceived advantages and disadvantages of online learning (multi-choice);
COVID-19-related questions: being diagnosed with COVID-19 by polymerase chain reaction (PCR), being in isolation, using masks in the classroom, being vaccinated;
Causes of pandemic-associated anxiety (multi-choice);
The Beck depression inventory (BDI, scores from 0 to 63 with higher score indicating more expressed symptoms of depression). A cut-off score of ≥16 for the BDI has been proposed to differentiate between adolescents with and without relevant symptoms of depression (73.0% sensitivity, 80.3% specificity) [27,28]. The Cronbach α of the scale was 0.915;
The Generalized anxiety scale-7 (GAD-7, scores from 0 to 21, with a higher score indicating more expressed symptoms of anxiety). A cut-off score of ≥8 for the GAD-7 provides 77% sensitivity and 82% specificity for detecting any anxiety disorder [29,30]. The Cronbach α of the scale was 0.914;
The Pittsburgh sleep quality index (PSQI, scores from 0 to 21, with a higher score indicating worse sleep quality). A cut-off score of >5 for the PSQI provides 89.6% sensitivity and 86.5% specificity to detect poor sleep quality [31]. The Cronbach α of the scale was 0.708.
2.3. Statistical Analysis
A sample of at least 172 was needed to include up to 10 independent variables in a multiple linear regression model with α = 0.05, 1 − β = 0.95 and f2 = 0.15 (computed by entering respective input parameters in G*Power 3.1.9.7). Data analysis was carried out in IBM SPSS Statistics 26 (IBM, Chicago, IL, USA). The Kolmogorov–Smirnov test was used to assess the normality of the continuous variables. The Wilcoxon test was applied to compare two paired groups for variables measured at two time points: (1) at the time of the survey (i.e., while learning in person) and (2) during studies online (i.e., indicated retrospectively). The Kruskal–Wallis H and the Mann–Whitney U tests were employed for comparisons of independent subgroups. Variables associated with BDI, GAD-7 and PSQI were investigated through Spearman’s correlations and by performing a stepwise linear regression analysis with PSQI as the dependent variable. A path analysis was conducted in Amos Graphics 22 to define the mediating role of anxiety and depression in the relationship between the perceived quality of studies (while learning in person) and the quality of sleep.
3. Results
There were 643 responses, of which 628 (97.7%) comprised the final study sample (individuals who provided inappropriate and/or implausible answers were excluded). The main characteristics of the sample are presented in Table 1. There were 268 (42.7%) individuals who scored ≥16 on the BDI, 342 (54.5%) who scored ≥8 on the GAD-7 and 398 (63.4%) who scored >5 on the PSQI.
Table 1.
General characteristics of the participants in the study.
| Characteristic | n (%) or Mean (SD) | |
|---|---|---|
| Number of respondents | 628 | |
| Sex | Female | 442 (70.4) |
| Male | 186 (29.6) | |
| Age | 16.1 (1.2) | |
| Grade | 9th | 165 (26.3) |
| 10th | 198 (31.5) | |
| 11th | 151 (24.0) | |
| 12th | 114 (18.2) | |
| COVID-19 PCR+ | 69 (11.0) | |
| COVID-19 Hospitalization | 2 (0.3) | |
| Wears masks at school | 627 (99.8) | |
| Class had to isolate since September 2021 | 39 (6.2) | |
| Days in isolation | 0.6 (2.4) | |
| In isolation during survey | 6 (1.0) | |
| Had only classes in person during the past month | 563 (89.6) | |
| Vaccinated against COVID-19 | 530 (84.4) | |
| Parents agreed (or would agree) with COVID-19 vaccination | 569 (90.6) | |
| BDI | 15.4 (11.3) | |
| GAD-7 | 9.2 (5.9) | |
| PSQI | 6.9 (3.3) |
BDI—the Beck depression inventory; GAD-7—the Generalized anxiety scale-7; PCR+—a positive polymerase chain reaction test; PSQI—The Pittsburgh sleep quality index.
On average, students perceived the quality of their studies and their physical health to be better while studying in person (Table 2). Students of the 10th grade reported the worst study quality (Kruskal–Wallis H(3) = 15.24, p = 0.002) and psychological health (H(3) = 17.62, p = 0.001) while learning in person. Final-year students had worse physical health (H(3) = 15.00, p = 0.002), slept less (H(3) = 10.07, p = 0.018), spent less time outside (H(3) = 12.21, p = 0.007) or engaging in physical activities (H(3) = 22.99, p < 0.001) than younger adolescents.
Table 2.
A comparison of health and daily-life-related factors during classes online and in-person.
| Characteristic | Classes Online | Classes in Person | Wilcoxon Test Statistic |
|---|---|---|---|
| Quality of studies a | 7 (0–10) | 8 (0–10) | −12.435 *** |
| Mental health a | 7 (0–10) | 6 (0–10) | −2.220 * |
| Physical health a | 7 (0–10) | 8 (0–10) | −9.176 *** |
| Sleep quality a | 9 (0–10) | 5 (0–10) | −19.489 *** |
| Well-being (exhausted vs. well-rested) a | 8 (0–10) | 4 (0–10) | −14.733 *** |
| Hours of studying per day b | 7.5 (2.7) | 9.2 (2.6) | −15.580 *** |
| Hours of sleep per day b | 8.1 (1.2) | 6.2 (1.2) | −19.509 *** |
| Hours of commute per day b | n/a | 1.7 (0.9) | n/a |
| Minutes outside per day b | 63.5 (62.0) | 82.4 (67.8) | −6.848 *** |
| Minutes of physical activity per day b | 53.3 (55.7) | 63.0 (62.7) | −4.344 *** |
a—value on a scale from 0 (worst) to 10 (best); median (range); b—mean (standard deviation); n/a—not applicable; *—p < 0.05; ***—p < 0.001.
Respondents of the 10th grade were more favorable towards the quality of studies online (H(3) = 25.98, p < 0.001), reported better psychological as well as physical health during lockdowns (H(3) = 9.13, p = 0.028 and H(3) = 10.79, p = 0.013, accordingly). They also had better sleep (H(3) = 14.24, p = 0.003), reported higher levels of energy (H(3) = 9.73, p = 0.021) and exercised more (H(3) = 8.30, p = 0.040) than 12th-year students while studying online.
Female students had less favorable views towards online (Z = −2.86, p = 0.004) but not in-person (Z = −0.68, p = 0.497) learning. They also regarded their physical and mental health as well as their sleep quality and well-being to be worse both while learning online and in-person (p < 0.05). Female respondents scored higher on the BDI (Mdn = 16 vs. Mdn = 9, Z = −8.08, p < 0.001), GAD-7 (Mdn = 10 vs. Mdn = 5, Z = −8.11, p < 0.001) and PSQI (Mdn = 7 vs. Mdn = 5.5, Z = −5.57, p < 0.001) as well. There was no difference in these measures between individuals who reported COVID-19 infections and the ones who did not.
Opinions about studying online and reported COVID-19-related problems are presented in Table 3.
Table 3.
The outlook of high school students towards online learning and the COVID-19 pandemic.
| Characteristic | n | % |
|---|---|---|
| Advantages of online learning | ||
| More time to sleep | 557 | 88.7% |
| Better teaching quality | 54 | 8.6% |
| It is safer during the pandemic | 469 | 74.7% |
| More free time | 422 | 67.2% |
| Easier to keep a good diet | 308 | 49.0% |
| No need to wear a mask | 464 | 73.9% |
| No need to commute | 454 | 72.3% |
| A more comfortable learning environment | 299 | 47.6% |
| Disadvantages of online learning | ||
| Impossible to meet friends | 411 | 65.4% |
| Impossible to attend extracurricular activities | 168 | 26.8% |
| Lack of help from teachers | 325 | 51.8% |
| Lack of interaction with teachers and school staff | 319 | 50.8% |
| Lack of physical activity | 273 | 43.5% |
| Worse teaching quality | 401 | 63.9% |
| A less comfortable learning environment | 160 | 25.5% |
| Causes for anxiety: the impact of the pandemic on.... | ||
| learning and gain of new knowledge | 385 | 61.3% |
| my family’s health | 277 | 44.1% |
| my health | 264 | 42.0% |
| future studies and career | 260 | 41.4% |
| my relationships with friends | 235 | 37.4% |
| my relationship with family members | 88 | 14.0% |
| the social and economic situation of my family | 170 | 27.1% |
| Reported causes for not vaccinating a | ||
| Previous COVID-19 infection | 37 | 37.8% |
| Because of possible side-effects | 32 | 32.7% |
| My parents/guardians do not agree with me being vaccinated | 31 | 31.6% |
| I do not believe the vaccine is effective to stop the spread of COVID-19 | 14 | 14.3% |
| I do not believe the vaccine is effective against COVID-19 | 13 | 13.3% |
| I cannot be vaccinated as confirmed by a physician | 4 | 4.1% |
| Student-reported effects of wearing face masks | ||
| Lack of air | 268 | 42.7% |
| Headache | 187 | 29.8% |
| Increased fatigue | 256 | 40.8% |
| Skin problems | 318 | 50.6% |
| No effects | 154 | 24.5% |
a—the percent of unvaccinated individuals is indicated.
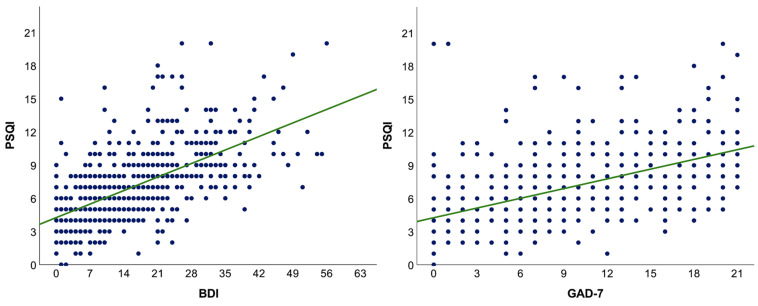
Measures of anxiety (rs = 0.57, p < 0.001) and depression (rs = 0.62, p < 0.001) were correlated with sleep quality (Figure 1) and associated with subjective estimates of health and daily-life-related aspects during studies in person (Table 4 and Table 5).
Figure 1.
The relationship between sleep quality and symptoms of depression or anxiety. A linear regression fit line is presented in green. BDI—the Beck depression inventory; GAD-7—the Generalized anxiety scale-7; PSQI—The Pittsburgh sleep quality index.
Table 4.
Spearman’s correlations between health and daily-life-related factors while studying in person and scores of sleep quality as well as anxiety scales.
| Characteristic (While Studying in Person) | PSQI | GAD-7 | BDI |
|---|---|---|---|
| Quality of studies | −0.36 *** | −0.30 *** | −0.35 *** |
| Mental health | −0.40 *** | −0.47 *** | −0.53 *** |
| Physical health | −0.36 *** | −0.31 *** | −0.41 *** |
| Sleep quality | −0.56 *** | −0.38 *** | −0.38 *** |
| Well-being (exhausted vs. well-rested) | −0.54 *** | −0.51 *** | −0.54 *** |
| Hours while studying per day | 0.24 *** | 0.27 *** | −0.22 *** |
| Hours of sleep per day | −0.58 *** | −0.32 *** | −0.33 *** |
| Hours of commute per day | 0.12 * | 0.06 | −0.07 |
| Minutes outside per day | −0.09 * | −0.07 | −0.09 * |
| Minutes of physical activity per day | −0.14 *** | −0.19 *** | −0.22 *** |
*—p < 0.05; ***—p < 0.001; BDI—the Beck depression inventory; GAD-7—the Generalized anxiety scale-7; PSQI—The Pittsburgh sleep quality index.
Table 5.
Results of a stepwise linear regression model with PSQI as the dependent variable (F(7,620) = 113.97, p < 0.001, R2adj = 0.558).
| Independent Variables | βstandardized | t | p |
|---|---|---|---|
| Constant | n/a | 17.733 | <0.001 |
| BDI | 0.331 | 8.309 | <0.001 |
| Hours of sleep per day | −0.282 | −8.575 | <0.001 |
| Quality of sleep a | −0.202 | −5.700 | <0.001 |
| Quality of studies a | −0.138 | −4.490 | <0.001 |
| GAD-7 | 0.133 | 3.488 | 0.001 |
| Mental health a | 0.095 | 2.709 | 0.007 |
| Minutes outside per day | −0.060 | −2.242 | 0.025 |
Excluded variables: grade, sex, COVID-19 (confirmed by PCR, yes/no), isolation during the survey (yes/no), physical health a, well-being (exhausted vs. well-rested), hours of studying per day, hours of commute per day, minutes of physical activity per day, subjective evaluation from 0 (worst possible) to 10 (best possible) while studying in person; BDI—the Beck depression inventory; GAD-7—the Generalized anxiety scale-7; PSQI—The Pittsburgh sleep quality index; n/a—not applicable.
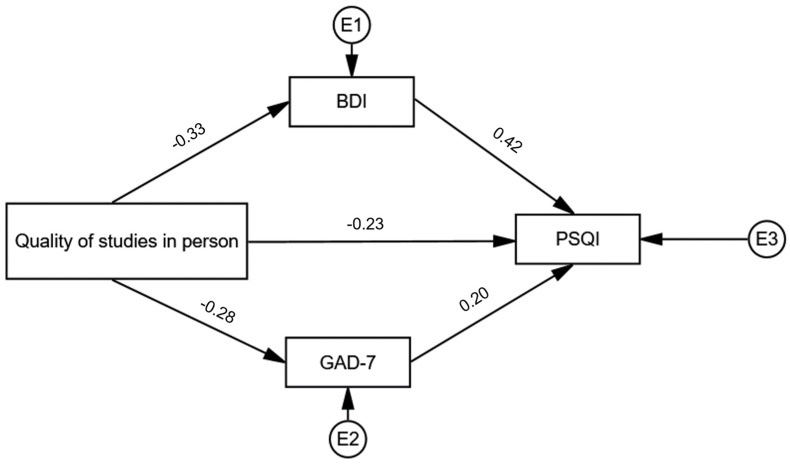
A mediation analysis revealed that the association between the perceived quality of studies and sleep quality (standardized direct effect −0.23, p < 0.001) is mediated by indirect effects of anxiety and depression (combined standardized indirect effect: −0.19, p < 0.001), Figure 2.
Figure 2.
A mediation analysis of the relationship between the reported quality of studies and the quality of sleep (PSQI) through symptoms of anxiety (GAD-7) and depression (BDI). Standardized effect estimates are presented. BDI—the Beck depression inventory; E—error term; GAD-7—the Generalized anxiety scale-7; PSQI—The Pittsburgh sleep quality index.
4. Discussion
4.1. General Findings
We report the results of an online cross-sectional survey involving 628 high school students in Lithuania. The study sample was predominantly female; however, it had an even distribution of respondents from the four grades (9th to 12th). Students also had relatively high vaccination rates, and the vast majority were able to keep studying in person one month before completing the survey. It is of note that vaccination for COVID-19 was widely available in the country and alternative measures of infection control (e.g., rapid antigen or pooled PCR testing) were installed in schools to complement mask use, disinfection, social distancing and ventilation. Overall, we were able to fully confirm three of our hypotheses: high school students reported better and longer sleep during lockdown (H1); they perceived online learning to be of inferior quality as compared to learning in person (H3); and the relationship between the quality of sleep and the perceived quality of studies was mediated by symptoms anxiety and depression after school reopening (H4). Moreover, while high school students reported worse physical health during lockdowns, their evaluation of mental health was higher during school closures, thus only partially confirming H2. In summary, the survey confirmed previous findings that school reopening leads to decreased sleep duration and increased physical activity (i.e., changes opposite to those observed after the initiation of lockdowns) but did not support the alleviation of mental health issues (measured as a self-rated mental health status) post-lockdown [18,20]. To the best of our knowledge, the study is also the first to address the relationship between the quality of learning, anxiety, depression and the quality of sleep after school reopening.
4.2. Differences in Health and Quality of Learning during Online and In-Person Studies
Before the time of our study, Lithuanian students had experienced two simultaneous COVID-19-associated lockdowns and school closures (March–June 2020 and November 2020–June 2021) and returned to learn in person in September 2021 [32]. After school reopening in September 2021, participants of our study reported improved quality of their studies as well as physical health and spent more time studying or being physically active. On the other hand, sleep quality, sleep hours, energy levels and mental health were subjectively evaluated to be worse. Such results suggest that a “trade-off” may exist between (a) good academic experience and physical activity (learning in person) and (b) optimal sleep quality and good mental health (learning online). However, our data does not indicate that the two groups of variables (a and b) are mutually exclusive. For instance, correlation analysis provided evidence that well-evaluated studies do not preclude good sleep quality and low levels of depression and anxiety: in fact, the more students appreciated their studies in person, the less they scored on the PSQI, BDI and GAD-7. A path analysis suggested that better study quality is also related to better sleep through a negative association with both the BDI and the GAD-7. Further, more hours of physical activity and better self-rated physical health were both associated with better sleep quality and lower levels of depression and anxiety. Therefore, bad sleep quality and persisting mental health issues after school reopening are most likely determined by other factors than improved study quality and increased physical activity. Among them could be changes in school schedules (e.g., the need to wake up earlier to attend classes) and daily commutes, which may decrease sleep hours and be detrimental for students whose endogenous circadian cycles trend towards later awakening [13,14,15,33]. Longer study hours and the continuous risk of COVID-19 may increase anxiety. It is noteworthy that anxiety, depression and bad sleep may also have a bidirectional interaction [34]. While the cross-sectional design of our study does not allow direct comparison of depression or anxiety levels and sleep quality during and after lockdown, two in five students could be suspected to have a significant depressive disorder, more than half to have an anxiety disorder, while almost two-thirds surpassed the PSQI threshold for poor sleep at the time of the survey (i.e., while learning in person). Further studies are required, however, to reveal adjustments (e.g., later school start times, student counseling) that could be beneficial in improving students’ sleep as well as mental health after returning to school.
4.3. The Possible Influence of Demographic Factors on Unfavourable Views of Online Learning
In our study, students of the 10th grade had a more positive outlook towards online learning. They represent individuals who were in lower secondary education (i.e., the 8th grade) at the start of the pandemic and competed to enter high schools during the lockdown in 2020. Because of the public health crisis, students that year were selected based on previous merit rather than results of entrance exams. During our study, adolescents of the 10th grade were in the last year of a general curriculum and had not yet chosen study streams for final-exam-oriented studies of the 11th and 12th years of school. Noticeably, male students were also more satisfied with online learning and had better sleep and fewer symptoms of anxiety and depression after school reopening. While the reasons underlying a better experience of learning online among 10th grade or male students remain unclear, our data indicate that high school students should not be regarded as a homogenous group, as some may benefit from online learning more than others. On average, however, students were aware that the quality of their studies worsened during national lockdowns. It is noteworthy that our survey was based in some of the best high schools in the country and the pandemic’s impact on learning and gain of new knowledge was the most frequent cause for respondents’ anxiety. Therefore, the critical evaluation of online teaching may be explained by both high students’ expectations and the professors’ unpreparedness to rapidly transfer and adapt the curriculum for virtual teaching. It can be argued that the online form of teaching itself does not compromise the quality of education as long as students’ technological needs are met and studying is made a social and engaging process [35]. However, more than half of all students missed interactions with their peers or tutors and reported insufficient assistance from the teachers during virtual studies. It is thus important to remember that schools are also valuable social environments and should welcome students back as soon as adequate safety measures are available [6,7,36].
4.4. Practical Applications
Practical implications of our study concern the applicability of online learning in high schools as well as possible modifications to the current framework of studying in person. The results of our survey support the argument that lockdowns, which mostly simulated a situation of later school start times, were beneficial for the sleep of high school students [16]. It should also be noted that novel school policies (e.g., later school start times, the introduction of online courses) implemented specifically for students to sleep longer could have positive consequences for their mental and physical well-being [37]. However, high school students in our study were also aware of the substandard quality of their studies during lockdowns. As our findings indicate, the reduction in the quality of studies may itself be associated with symptoms of anxiety and depression or poor sleep. Thus, the complex relationship between mental health, physical well-being and learning should be acknowledged before implementing any new policies that could risk undermining high academic standards.
4.5. Limitations and Future Directions
Limitations of the current study are largely determined by its cross-sectional design: longitudinal data are needed to better define factors associated with poor sleep and mental health issues among high school students throughout the pandemic. Further, our survey was based in highly ranked schools of secondary education in a high-income country in Europe; thus, the results presented cannot be generalized to student populations of dissimilar social and economic backgrounds. Participation bias may have influenced results as students with no interest in their health or study quality were possibly less likely to participate. Finally, the current study relied only on subjective self-reported information and objective methods of data collection, such as actigraphy to determine sleep-related variables and structured interviews to investigate mental health problems, are needed to confirm our findings.
Future controlled trials are also required to better define the psychological and physical outcomes among students learning online (or in a hybrid way) compared to those attending live classes. In our study, only estimates of self-rated mental and physical health were compared while studying online during lockdowns versus learning in person after school reopening. Single-item self-reported measures are increasingly appreciated as tools that reflect future morbidity; however, they do not address the presence of distinct treatable conditions (e.g., depression) [25,26]. It is therefore important that the quality of sleep and symptoms of anxiety and depression are investigated in the setting of teaching online (or in a hybrid way) after the COVID-19 pandemic. Such studies could help determine, what are the positive and negative health effects of online learning in high schools in the absence of a global pandemic.
5. Conclusions
The results of the current study suggest that the reopening of high schools during the COVID-19 pandemic was beneficial for the quality of teaching and students’ physical health but had negative effects on their sleep and mental health. Around half of the high school students reported significant levels of anxiety, while almost two-thirds reported having poor sleep. Online learning was perceived to be of worse quality than studying in person, and problems gaining new knowledge were the primary cause for anxiety. Poor study quality after school reopening was related to worse quality of sleep both directly and through symptoms of anxiety and depression. In summary, our findings indicate that high school students could potentially benefit from new school policies aimed to improve student sleep while respecting high educational standards. Future studies should investigate options to improve sleep and mental health among high school students while ensuring study quality and students’ safety.
Acknowledgments
We thank representatives from the schools’ self-governments as well as high school students for their time and contribution to this study.
Author Contributions
Conceptualization, R.M., A.M. and K.P.; methodology, R.M., A.M. and K.P.; software, A.M., K.P. and R.M.; validation, R.M., A.M. and K.P.; formal analysis, A.M. and K.P.; investigation, A.M.; resources, A.M.; data curation, R.M., A.M. and K.P.; writing—original draft preparation, K.P.; writing—review and editing, R.M., A.M. and K.P.; visualization, A.M. and K.P.; supervision, R.M.; project administration, R.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval is not mandatory for anonymous surveys.
Informed Consent Statement
Respondents expressed their consent by voluntarily and anonymously entering the survey form and completing and submitting their answers online.
Data Availability Statement
Data supporting the findings may be provided from the corresponding author upon request.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Petersen E., Wasserman S., Lee S.-S., Go U., Holmes A.H., Al-Abri S., McLellan S., Blumberg L., Tambyah P. COVID-19–We urgently need to start developing an exit strategy. Int. J. Infect. Dis. 2020;96:233–239. doi: 10.1016/j.ijid.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nenna R., Zeric H., Petrarca L., Mancino E., Midulla F. Weighing policymaking: A narrative review of school closures as COVID-19 pandemic-mitigation strategies. Pediatr. Pulmonol. 2021;2021:1–8. doi: 10.1002/ppul.25787. [DOI] [PubMed] [Google Scholar]
- 3.Van Lancker W., Parolin Z. COVID-19, school closures, and child poverty: A social crisis in the making. Lancet Public Health. 2020;5:e243–e244. doi: 10.1016/S2468-2667(20)30084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brooks S.K., Smith L.E., Webster R.K., Weston D., Woodland L., Hall I., Rubin G.J. The impact of unplanned school closure on children’s social contact: Rapid evidence review. Eurosurveillance. 2020;25:2000188. doi: 10.2807/1560-7917.ES.2020.25.13.2000188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang G., Zhang Y., Zhao J., Zhang J., Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395:945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.It’s time to send children back to school. Nat. Med. 2021;27:1655. doi: 10.1038/s41591-021-01543-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spitzer M. Open schools! Weighing the effects of viruses and lockdowns on children. Trends Neurosci. Educ. 2021;22:100151. doi: 10.1016/j.tine.2021.100151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meherali S., Punjani N., Louie-Poon S., Rahim K.A., Das J., Salam R., Lassi Z. Mental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic Review. Int. J. Environ. Res. Public Health. 2021;18:3432. doi: 10.3390/ijerph18073432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gruber R., Saha S., Somerville G., Boursier J., Wise M.S. The impact of COVID-19 related school shutdown on sleep in adolescents: A natural experiment. Sleep Med. 2020;76:33–35. doi: 10.1016/j.sleep.2020.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou C., Li R., Yang M., Duan S., Yang C. Psychological Status of High School Students 1 Year After the COVID-19 Emergency. Front. Psychiatry. 2021;12:729930. doi: 10.3389/fpsyt.2021.729930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharma M., Aggarwal S., Madaan P., Saini L., Bhutani M. Impact of COVID-19 pandemic on sleep in children and adolescents: A systematic review and meta-analysis. Sleep Med. 2021;84:259–267. doi: 10.1016/j.sleep.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lian Q., Zuo X., Zhong X., Tu X., Zhang J., Shu C., Yu C., Lou C. The effect of COVID-19 school closures on adolescent sleep duration: An uncontrolled before-after study. BMC Public Health. 2021;21:1528. doi: 10.1186/s12889-021-11589-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Socarras L.R., Potvin J., Forest G. COVID-19 and sleep patterns in adolescents and young adults. Sleep Med. 2021;83:26–33. doi: 10.1016/j.sleep.2021.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weingart R., Bryan C., Olson D., Gazmararian J., Rosati B., Hale L., Van Gilder M. Adolescent sleep duration and timing during early COVID-19 school closures. Sleep Health. 2021;7:543–547. doi: 10.1016/j.sleh.2021.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Becker S.P., Dvorsky M.R., Breaux R., Cusick C.N., Taylor K.P., Langberg J.M. Prospective examination of adolescent sleep patterns and behaviors before and during COVID-19. Sleep. 2021;44:zsab054. doi: 10.1093/sleep/zsab054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saxvig I.W., Pallesen S., Sivertsen B., Hysing M., Evanger L.N., Bjorvatn B. Sleep during COVID-19-related school lockdown, a longitudinal study among high school students. J. Sleep Res. 2021:e13499. doi: 10.1111/jsr.13499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang J., Wang Y., Lin H., Chen X., Wang H., Liang H., Guo X., Fu C. Mental health problems among school-aged children after school reopening: A cross-sectional study during the COVID-19 post-pandemic in east China. Front. Psychol. 2021;12:5168. doi: 10.3389/fpsyg.2021.773134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Massar S.A.A., Ng A.S.C., Soon C.S., Ong J.L., Chua X.Y., Chee N.I.Y.N., Lee T.S., Chee M.W.L. Reopening after lockdown: The influence of working-from-home and digital device use on sleep, physical activity, and wellbeing following COVID-19 lockdown and reopening. Sleep. 2021;45:zsab250. doi: 10.1093/sleep/zsab250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jeffs E., Lucas N., Walls T. COVID-19: Parent and caregiver concerns about reopening New Zealand schools. J. Paediatr. Child Health. 2021;57:403–408. doi: 10.1111/jpc.15234. [DOI] [PubMed] [Google Scholar]
- 20.Ren Z., Xin Y., Ge J., Zhao Z., Liu D., Ho R.C.M., Ho C.S.H. Psychological impact of COVID-19 on college students after school reopening: A cross-sectional study based on machine learning. Front. Psychol. 2021;12:641806. doi: 10.3389/fpsyg.2021.641806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lourenço A., Martins F., Pereira B., Mendes R. Children are back to school, but is play still in lockdown? Play experiences, social interactions, and children’s quality of life in primary education in the COVID-19 pandemic in 2020. Int. J. Environ. Res. Public Health. 2021;18:12454. doi: 10.3390/ijerph182312454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leonardi F. The Definition of health: Towards new perspectives. Int. J. Health Serv. 2018;48:735–748. doi: 10.1177/0020731418782653. [DOI] [PubMed] [Google Scholar]
- 23.Galderisi S., Heinz A., Kastrup M., Beezhold J., Sartorius N. Toward a new definition of mental health. World Psychiatry. 2015;14:231–233. doi: 10.1002/wps.20231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ma L., Mazidi M., Li K., Li Y., Chen S., Kirwan R., Zhou H., Yan N., Rahman A., Wang W., et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021;293:78–89. doi: 10.1016/j.jad.2021.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Casu G., Gremigni P. Is a single-item measure of self-rated mental health useful from a clinimetric perspective? Psychother. Psychosom. 2019;88:177–178. doi: 10.1159/000497373. [DOI] [PubMed] [Google Scholar]
- 26.Ahmad F., Jhajj A.K., E Stewart D., Burghardt M., Bierman A.S. Single item measures of self-rated mental health: A scoping review. BMC Health Serv. Res. 2014;14:398. doi: 10.1186/1472-6963-14-398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee A., Park J. Diagnostic test accuracy of the beck depression inventory for detecting major depression in adolescents: A systematic review and meta-analysis. Clin. Nurs. Res. 2021:10547738211065105. doi: 10.1177/10547738211065105. [DOI] [PubMed] [Google Scholar]
- 28.Beck A.T., Steer R.A., Carbin M.G. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin. Psychol. Rev. 1988;8:77–100. doi: 10.1016/0272-7358(88)90050-5. [DOI] [Google Scholar]
- 29.Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 30.Kroenke K., Spitzer R.L., Williams J.B., Monahan P.O., Löwe B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007;146:317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 31.Buysse D.J., Reynolds C.F., III, Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 32.The Official Source of Information by the Government of the Republic of Lithuania on the Pandemic Situation in Lithuania. [(accessed on 16 April 2021)]. Available online: http://koronastop.lrv.lt/en/#information.
- 33.Meltzer L.J., Saletin J.M., Honaker S.M., Owens J.A., Seixas A., Wahlstrom K.L., Wolfson A.R., Wong P., A Carskadon M. COVID-19 instructional approaches (in-person, online, hybrid), school start times, and sleep in over 5000 U.S. adolescents. Sleep. 2021;44:zsab180. doi: 10.1093/sleep/zsab180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jansson M., Linton S.J. The role of anxiety and depression in the development of insomnia: Cross-sectional and prospective analyses. Psychol. Health. 2006;21:383–397. doi: 10.1080/14768320500129015. [DOI] [Google Scholar]
- 35.Costa S.A., Kavouras I., Cohen N., Huang T.T.K. Moving education online during the COVID-19 pandemic: Thinking back and looking ahead. Front. Public Health. 2021;9:1621. doi: 10.3389/fpubh.2021.751685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Willyard C. The science behind school reopenings. Nature. 2021;595:164–167. doi: 10.1038/d41586-021-01826-x. [DOI] [PubMed] [Google Scholar]
- 37.Owens J., Au R., Carskadon M., Millman R., Wolfson A., Braverman P.K., Adelman W.P., Breuner C.C., Levine D.A., Marcell A.V., et al. Insufficient sleep in adolescents and young adults: An update on causes and consequences. Pediatrics. 2014;134:e921–e932. doi: 10.1542/peds.2014-1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data supporting the findings may be provided from the corresponding author upon request.