Abstract
Background: Very few papers covering the anticancer activity of azulenes have been reported, as compared with those of antibacterial and anti-inflammatory activity. This led us to investigate the antitumor potential of fifteen 4,6,8-trimethyl azulene amide derivatives against oral malignant cells. Methods: 4,6,8-Trimethyl azulene amide derivatives were newly synthesized. Anticancer activity was evaluated by tumor-specificity against four human oral squamous cell carcinoma (OSCC) cell lines over three normal oral cells. Neurotoxicity was evaluated by cytotoxicity against three neuronal cell lines over normal oral cells. Apoptosis induction was evaluated by Western blot and cell cycle analyses. Results: Among fifteen derivatives, compounds 7, 9, and 15 showed the highest anticancer activity, and relatively lower neurotoxicity than doxorubicin, 5-fluorouracil (5-FU), and melphalan. They induced the accumulation of a comparable amount of a subG1 population, but slightly lower extent of caspase activation, as compared with actinomycin D, used as an apoptosis inducer. The quantitative structure–activity relationship analysis suggests the significant correlation of tumor-specificity with a 3D shape of molecules, and possible involvement of inflammation and hormone receptor response pathways. Conclusions: Compounds 7 and 15 can be potential candidates of a lead compound for developing novel anticancer drugs.
Keywords: 4,6,8-trimethyl azulene amide; oral cancer; tumor-specificity; neurotoxicity; QASR; molecular shape; caspase 3; cell cycle; NFκB; hormone receptor
1. Introduction
Azulene is a 10 π-electron non-benzenoid aromatic hydrocarbon with a fused structure of five- and seven-membered rings, showing a deep blue coloration. The resonance structure of azulene contains ionic cyclopentadienide and tropylium substructures, resulting in electrophilic substitution reactions at the 1- and 3-positions and nucleophilic addition reactions at the 2-, 4-, 6-, and 8-positions, along with the 2-position at the five-membered ring in some cases [1,2,3].
Azulene derivatives, including guaiazulene (Figure S1A), are present in many plants and mushrooms, and applied as optoelectronic devices and ingredients used for hundreds of years in antiallergic, antibacterial, and anti-inflammatory therapies [4]. Several research studies have reported the applications of azulenes on oral diseases. For example, gargling with sodium azulene has been applied to maintain the compliance with afatinib treatment [5]. Azulene rinse has been applied to dry mouth and salivary gland dysfunction following radiotherapy, but with no convincing evidence [6]. Oral administration of marzulene (l-glutamine plus azulene) stimulates repair mechanisms of rat gastric mucosa after NaOH injury [7]. Guaizulene alleviated the paracetamol-induced glutathione (GSH) depletion and hepatic damage, possibly by its antioxidant activity [8]. Photodynamic activation of a lower concentration of guaiazulene suppressed inflammatory markers in peripheral blood mononuclear cells possibly by generating singlet oxygen [9]. On the other hand, very few reports of anticancer activity and quantitative structure–activity relationship (QSAR) analysis of azulenes have been reported [10,11,12].
In order to determine the tumor-specificity of azulene derivatives, we decided to use a set of four human oral squamous cell carcinoma cell lines and three human normal oral mesenchymal cells, rather than using human normal epithelial cells. This decision was based on our previous findings that (i) human normal epithelial cells (oral keratinocyte HOK, primary gingival epithelial cells HGEP) cannot be grown in regular culture medium (DMEM + 10%FBS) and, (ii) when HOK and HGEP were cultured in their specific growth factor-enriched medium, they began to rapidly grow like malignant cells, acquiring extremely higher sensitivity against anticancer drugs, resulting in the reduction of TS values below 1.0 [13].
We have previously investigated the anticancer activity of three groups of azulenes against human oral squamous cell carcinoma (OSCC) cell lines (Ca9-22, HSC-2, HSC-3, HSC-4) in comparison with three normal human oral mesenchymal cells (gingival fibroblast, HGF; periodontal ligament fibroblast, HPLF; pulp cell, HPC) (Figure S1B–D): Ten alkylaminoguaiazulene derivatives (Figure S1B) showed very weak tumor-specificity (TS = 1.1–2.3) [14]. Among ten guaiazulene amide derivatives (Figure S1C), only one compound showed higher tumor-specificity (TS > 28.9) [15]. The tumor-specificity of all twenty-one azulene amide derivatives (Figure S1D) were very weak (TS = 0.8~7.1) [16].
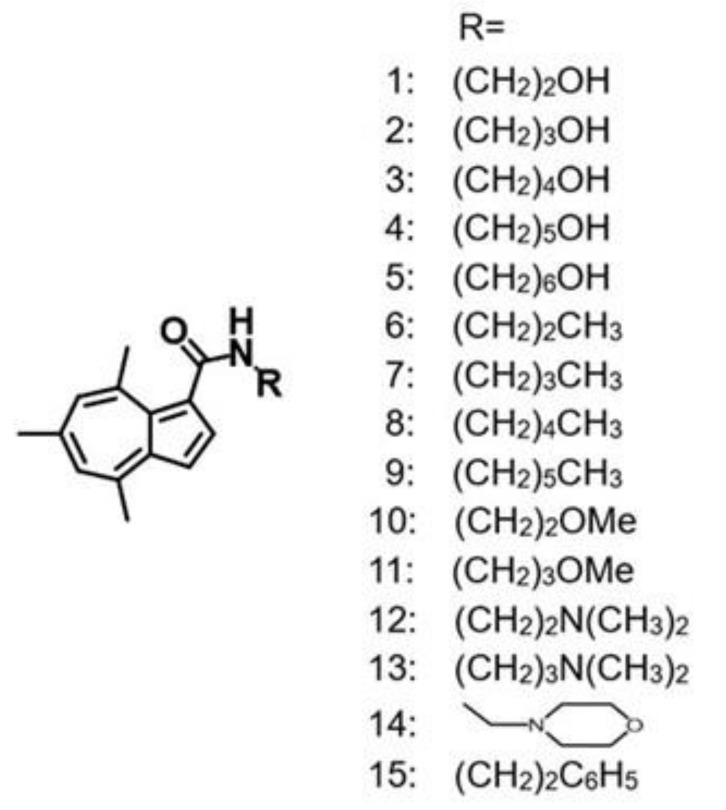
In continuation of finding more tumor-selective compounds, a total of fifteen 4,6,8-trimethyl azulene amide derivatives (Figure 1) were investigated for their cytotoxicity against four OSCC cell lines and three normal human oral mesenchymal cells. Since many cancer drugs have been reported to show severe neurotoxicity [17,18,19], neurotoxicity of fifteen 4,6,8-trimethyl azulene amide derivatives was also compared with those of popular anticancer drugs.
Figure 1.
Structures of 4,6,8-trimethyl azulene amide derivatives.
2. Results
2.1. Tumor-Specificity
Four human oral squamous cell carcinoma cell line (Ca9-22 originated from gingiva; HSC-2, HSC-3, HSC-4 from tongue) and three human mesenchymal normal oral cells (gingival fibroblast HGF, periodontal ligament fibroblast (HPLF) and pulp cells (HPC) were incubated for 48 h with various concentrations of compounds 1–15 and three reference compounds (doxorubicin (DOX), 5-fluorouracil (5-FU), melphalan (l-phenylalanine mustard, L-PAM) in DMEM supplemented with 10% fetal bovine serum (FBS) and antibiotics. Viable cell number was then determined by an MTT method in triplicate. Cytotoxicity of dimethyl sulfoxide (DMSO), used for dissolving these compounds, was subtracted. The cytotoxicity experiments were performed three times, and 50% cytotoxic concentration (CC50) was determined from the dose–response curve done in triplicate (Figures S2–S4), and listed in Table 1. We have noticed that Ca9-22 (derived from gingiva) is more sensitive than other oral squamous cell lines (HSC-2, HSC-3, HSC-4) (derived from tongue) to most of the azulene compounds, and oral squamous cells are more sensitive than normal mesenchymal cells. Since such trends, however, are reproducible in three independent experiments (as shown in supplementary data Figures S2–S4), we presented the mean value.
Table 1.
Cytotoxicity of 4,6,8-trimethyl azulene amide derivatives and reference compounds against human oral squamous cell carcinoma cell lines and human normal oral cells.
| CC50 (μM) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Human Oral Squamous Cell Carcinoma Cells | Human Normal Oral Cells | ||||||||||||
| Ca9-22 | HSC-2 | HSC-3 | HSC-4 | Mean | HGF | HPLF | HPC | Mean | TS | PSE | |||
| (A) | (B) | (C) | (D) | (D/B) | (C/A) | 100D/B2 | 100C/A2 | ||||||
| 1 | 335.1 | 400.0 | 397.4 | 400.0 | 383.1 | 400.0 | 400.0 | 400.0 | 400.0 | 1.0 | 1.2 | 0.3 | 0.4 |
| 2 | 379.3 | 377.8 | 400.0 | 400.0 | 389.3 | 400.0 | 400.0 | 400.0 | 400.0 | 1.0 | 1.1 | 0.3 | 0.3 |
| 3 | 233.4 | 400.0 | 400.0 | 377.8 | 352.8 | 400.0 | 400.0 | 400.0 | 400.0 | 1.1 | 1.7 | 0.3 | 0.7 |
| 4 | 288.1 | 313.8 | 361.0 | 375.6 | 334.6 | 400.0 | 391.6 | 376.9 | 389.5 | 1.2 | 1.4 | 0.3 | 0.5 |
| 5 | 53.5 | 40.8 | 63.2 | 106.5 | 66.0 | 293.3 | 363.9 | 181.9 | 279.7 | 4.2 | 5.5 | 6.4 | 10.2 |
| 6 | 71.1 | 86.9 | 59.0 | 196.9 | 103.5 | 400.0 | 400.0 | 400.0 | 400.0 | 3.9 | 5.6 | 3.7 | 7.9 |
| 7 | 41.6 | 55.1 | 38.9 | 62.9 | 49.6 | 400.0 | 356.9 | 400.0 | 385.6 | 7.8 | 9.6 | 15.7 | 23.1 |
| 8 | 46.7 | 52.4 | 46.3 | 60.1 | 51.4 | 354.9 | 266.8 | 328.0 | 316.6 | 6.2 | 7.6 | 12.0 | 16.2 |
| 9 | 29.3 | 33.9 | 33.8 | 35.2 | 33.0 | 298.2 | 156.1 | 112.5 | 189.0 | 5.7 | 10.2 | 17.3 | 34.8 |
| 10 | 124.2 | 337.0 | 181.3 | 328.7 | 242.8 | 400.0 | 400.0 | 400.0 | 400.0 | 1.7 | 3.2 | 0.7 | 2.6 |
| 11 | 55.9 | 76.5 | 46.3 | 81.6 | 65.1 | 400.0 | 355.6 | 400.0 | 385.2 | 5.9 | 7.2 | 9.1 | 12.8 |
| 12 | 110.7 | 162.7 | 101.3 | 155.6 | 132.6 | 303.2 | 270.7 | 168.0 | 247.3 | 1.9 | 2.7 | 1.4 | 2.5 |
| 13 | 120.5 | 173.1 | 73.6 | 153.6 | 130.2 | 327.7 | 293.0 | 201.6 | 274.1 | 2.1 | 2.7 | 1.6 | 2.3 |
| 14 | 391.1 | 377.8 | 309.4 | 400.0 | 369.6 | 400.0 | 400.0 | 400.0 | 400.0 | 1.1 | 1.0 | 0.3 | 0.3 |
| 15 | 19.9 | 16.8 | 29.4 | 21.5 | 21.9 | 400.0 | 400.0 | 377.8 | 392.6 | 17.9 | 20.1 | 81.7 | 101.0 |
| DOX | 0.4 | 0.2 | 0.4 | 0.1 | 0.3 | 10.0 | 9.0 | 10.0 | 9.7 | 34.5 | 25.1 | 12,325.0 | 6270.0 |
| 5-FU | 191.2 | 703.0 | 673.5 | 33.1 | 400.2 | 1000.0 | 1000.0 | 1000.0 | 1000.0 | 2.5 | 5.2 | 0.6 | 2.7 |
| L-PAM | 34.7 | 11.9 | 20.1 | 6.9 | 18.4 | 200.0 | 200.0 | 173.4 | 191.1 | 10.4 | 5.8 | 56.5 | 16.6 |
Cells were incubated for 48 h with test compounds, and viable cell number was determined by MTT methods in triplicate. All dose–response curves of three independent experiments are shown in Figures S2–S4. The CC50 (determined from the dose–response curves), TS, and PSE values are listed in Table S1. DOX, doxorubicin; 5-FU, 5-fluorouracil; L-PAM, melphalan.
When four cancer cells and three normal oral cells were used, compound 15 showed the highest tumor-specificity (TS = 17.9), followed by compound 7 (TS = 7.8) and compound 9 (TS = 5.7), higher than that of 5-FU (TS = 2.5) (D/B in Table 1). When two gingival tissue-derived cells Ca9-22 and HGF were used, compound 15 again showed the highest tumor-specificity (TS = 20.1), followed by compound 9 (TS = 10.2) and compound 7 (TS = 9.6) (C/A in Table 1).
For clinical application of candidate compounds, the database of their tumor-specificity and cytotoxicity against tumor cells provides useful information. Thus, PSE (Potency–Selectivity Expression (the ratio of the tumor-specificity to the CC50 against cancer cells) × 100) was calculated for all compounds. Compound 15 showed the highest value (PSE = 81.7; 101.0), followed by compound 9 (PSE = 17.3; 34.8) and compound 7 (PSE = 15.7; 23.1) (100D/B2; 100C/A2 in Table 1). PSE values of all derivatives were two-orders lower than that of doxorubicin (PSE = 12,325; 6270). However, PSE values of compounds 7, 9, and 15 were higher than that of 5-FU (PSE = 0.6; 2.7), and PSE value of compound 15 was higher than that of L-PAM (PSE = 56.5; 16.6). Based on these data, compounds 7, 9, and 15 were chosen for further analysis.
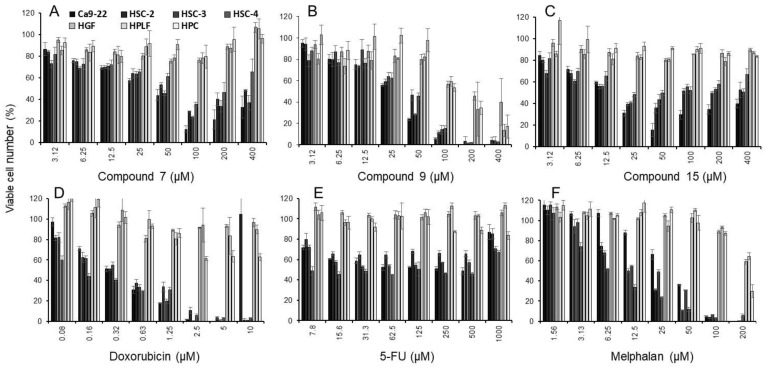
Dose–response curve of compounds 7, 9, and 15 and three reference compounds are shown in Figure 2. Compound 9 (B), doxorubicin (D) and melphalan (F) were cytotoxic, whereas compound 7 (A), compound 15 (C), and 5-FU (E) were cytostatic.
Figure 2.
Dose–response curves of cytotoxicity induction by compound 7 (A), compound 9 (B), compound 15 (C), doxorubicin (D), 5-FU (E), and melphalan (F). Cells were incubated for 48 h with the indicated concentrations of compounds. Each value represents mean ±S.D. from three independent experiments which were done in triplicate. All data of the dose–response of fifteen 4,6,8-trimethyl azulene amide derivatives and three reference compounds (doxorubicin, 5-FU, melphalan) are available in supplementary files (Figures S2–S4 and Table S1).
2.2. Apoptosis-Inducing Activity
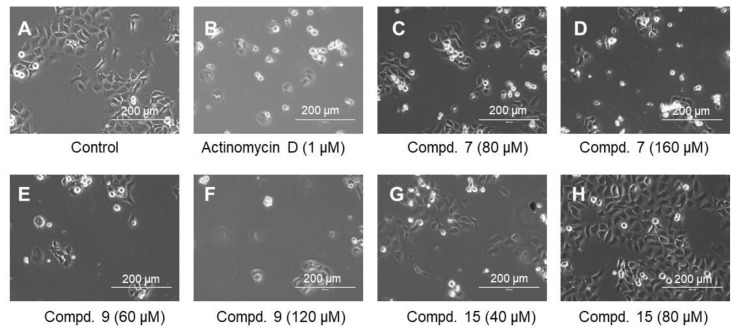
Microscopical observation revealed that actinomycin D (1 μM) (B), a higher concentration of compound 7 (160 μM) (D), and low and high concentrations of compound 9 (60 and 120 μM) (E, F) induced cell shrinkage. On the other hand, compound 15 did not induce such morphological changes at 40 and 80 μM (G, H) (Figure 3).
Figure 3.
Morphological change induced in Ca9-22 cells after 24 h incubation without (control) (A), or with the indicated concentrations of actinomycin D (B), compound 7 (C,D), compound 9 (E,F) or compound 15 (G,H).
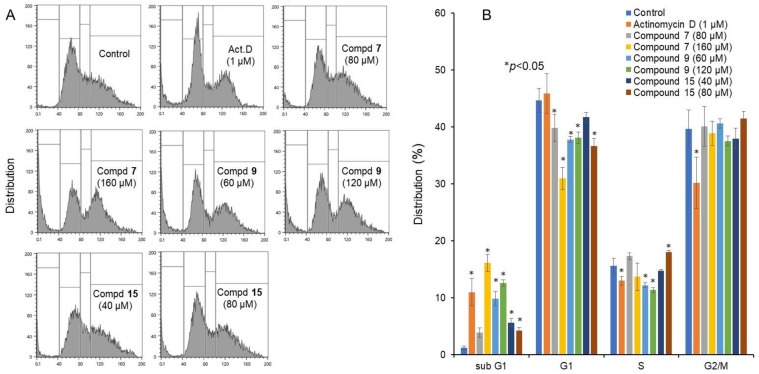
Similarly, actinomycin D (1 μM), and higher concentration of compound 7 (160 μM), low and high concentrations of compound 9 (60 and 120 μM) increased the relative proportion of subG1 population (that reflect DNA fragmentation) to a nearly comparable level attained by actinomycin D. On the other hand, compound 15 at higher concentration (80 μM) only slightly increased subG1 population (p < 0.05) (Figure 4).
Figure 4.
Cell cycle analysis of cytotoxicity induction by 4,6,8-trimethyl azulene amide derivatives. Ca9-22 cells were incubated for 24 h with the indicated concentrations of test samples and subjected to a cell sorter. (A) Representative cell cycle distribution pattern; (B) distribution into subG1, G1, S and G2/M phase. Each value represents the mean ±S.D. of triplicate determinations. * p < 0.05 between control and sample, examined by one-way ANOVA and Dunnett’s post-test.
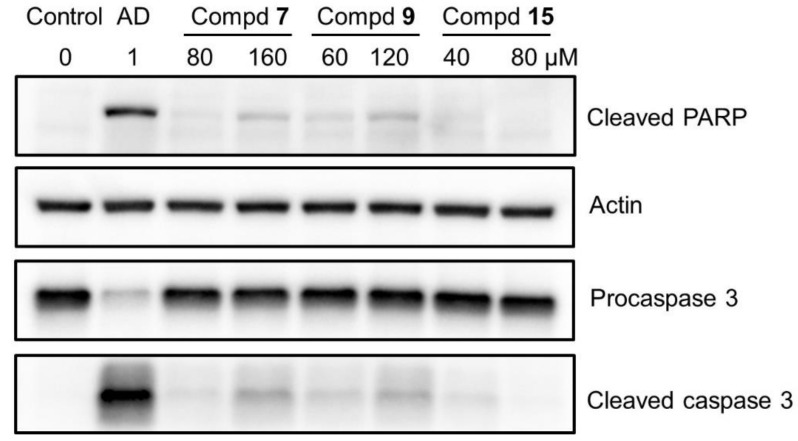
Western blot analysis demonstrated that compounds 7 and 9, but not compound 15, induced the cleavage of poly ADP-ribose polymerase (PARP) and procaspase 3, suggesting the induction of apoptosis (Figure 5). Since the extent of apoptosis induction was much lower than that induced by actinomycin D, the possibility of induction of other types of cell death such as necrosis has been suggested.
Figure 5.
Western blot analysis of compounds 7, 9, and 15. Ca9-22 cells were incubated for 24 h without (control) or with the indicated concentrations of test samples, and cell lysates were prepared as described in Materials and Methods. Protein (15 µg) was loaded to each lane for Western blot analysis, and the reacted bands were presented after contrast adjustment. Raw data of images after short, middle, and long exposures (without contrast adjustment) were shown in Supplementary Figure S5.
2.3. Neurotoxicity
Rat adrenal pheochromocytoma cell line (PC12), differentiated PC12 cells (Day 6) expressing characteristic neurites (dPC12), human neuroblastoma cell line (SH-SY5Y), and rat Schwann cell line (LY-PPB6) were treated for 48 h with various concentrations of test samples, and viable cell number was determined by MTT methods. Dose–response curve and CC50 values of three independent experiments are shown in supplementary Figure S6. The data were summarized in Table 2. Compounds 7 and 9 showed much lower neurotoxicity (NT = 1.4, 1.3, 1.0; 1.4, 1.0, 1.0) as compared with doxorubicin (NT = 70.6, 25.0, 44.9), 5-FU (NT = 11.0, 23.3, 3.4), and L-PAM (NT = 19.8, 7.2).
Table 2.
Neurotoxicity of 4,6,8-trimethyl azulene amide derivatives and reference compounds.
| CC50 (μM) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exp. 1 | Exp. 2 | Exp. 3 | |||||||||||
| PC12 | SH-SY5Y | LYPPB6 | Mean | PC12 | SH-SY5Y | LYPPB6 | Mean | dPC12 | Normal Cells | NT 1 | |||
| (E) | (F) | (G) | (D) | (D/E) | (D/F) | (D/G) | |||||||
| 7 | 59 | 400 | 400 | 286 | 68 | 400 | 400 | 289 | 400 | 386 | 1.4 | 1.3 | 1.0 |
| 9 | 35 | 73 | 56 | 55 | 36 | 63 | 74 | 58 | 19 | 189 | 3.5 | 3.3 | 10.2 |
| 15 | 378 | 42 | 400 | 273 | 400 | 400 | 400 | 400 | 400 | 393 | 1.4 | 1.0 | 1.0 |
| DOX | 0.07 | 0.02 | 0.32 | 0.14 | 0.26 | 0.12 | 0.78 | 0.39 | 0.22 | 10 | 70.6 | 25.0 | 44.9 |
| 5-FU | 14 | 5.85 | 250 | 89.95 | 2 | 1 | 125 | 43 | 297 | 1000 | 11.0 | 23.3 | 3.4 |
| L-PAM | N.D. | N.D. | N.D. | N.D. | 2 | 2 | 25 | 10 | 26 | 191 | N.D. | 19.8 | 7.2 |
1 Neurotoxicity (NT) was determined by dividing the mean values of CC50 against normal human oral cells (D) by the mean of CC50 against PC12, SH-SY5Y and LYPPB6 (E in Exp. 1 and F in Exp. 2) or the CC50 against differentiated PC12 cells (G). Dose–response curve from which the CC50 values were delineated in Figure S5. N.D., not determined.
2.4. Computational Analysis
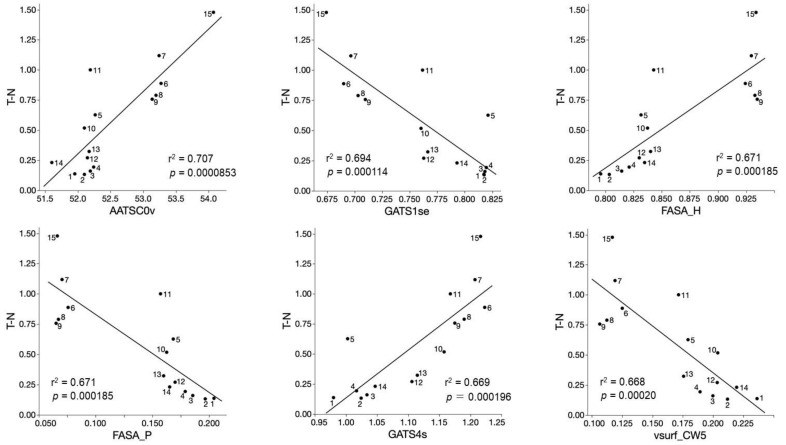
QSAR analysis of tumor-specificity of fifteen 4,6,8-trimethyl azulene amide derivatives (compounds 1–15) were performed next. Significant correlation (p < 0.05) was found between the cytotoxicity against human oral squamous (OSCC) cell lines and 220 chemical descriptors (supplemental data Table S2). Six chemical descriptors that showed the highest correlation with the cytotoxicity against OSCC cells are shown in Figure 6. The cytotoxicity of 4,6,8-trimethyl azulene amide derivatives against human OSCC cell lines was correlated (r2 = 0.668~0.707, p = 0.0000853~0.00020) positively with AATSC0v (Topological Structure) (A), FASA_H (water accessible surface area) (C), GATS4s (Topological Structure) (E), and negatively with GATS1se (Topological Structure), FASA_P (water accessible surface area of all polar atoms) and vsurf_CW5 (Capacity factor) (Figure 6). These data suggest that the tumor-specificity of 4,6,8-trimethyl azulene amide derivatives are related to chemical descriptors that reflect 3D structure (AATSC0v, FASA_H, GATS4s, GATS1se, FASA_P vsurf_CW5) (Table 3).
Figure 6.
Top six chemical descriptors that showed higher correlation (r2 = 0.668~0.707) with tumor specificity of fifteen 4,6,8-trimethyl azulene amide derivatives. The mean negative log TS values (T-N) were plotted.
Table 3.
Descriptors that significantly correlated with tumor-specificity (T–N) of fifteen 4,6,8-trimethyl azulene amide derivatives.
| Important Descriptors |
Significance of Correlation with T-N |
Meanings |
|---|---|---|
| AATSC0v | r2 = 0.707; p = 0.0000853 | Autocorrelation of Topological Structure of lag 0 atoms weighted by van der Waals volume |
| GATS1s | r2 = 0.694; p = 0.000114 | Autocorrelation of Topological Structure of lag 1 atoms weighted by Sanderson EN |
| FASA_H | r2 = 0.671; p = 0.000185 | Descriptor related to water accessible surface area of all hydrophobic atoms |
| FASA_P | r2 = 0.671; p = 0.000185 | Descriptor related to water accessible surface area of all polar atoms |
| GATS4s | r2 = 0.669; p = 0.000196 | Autocorrelation of Topological Structure of lag 4 atoms weighted by intrinsic state |
| vsurf_CW5 | r2 = 0.668; p = 0.00020 | Capacity factor |
2.5. Possible Nuclear Receptor/Stress Response Pathways
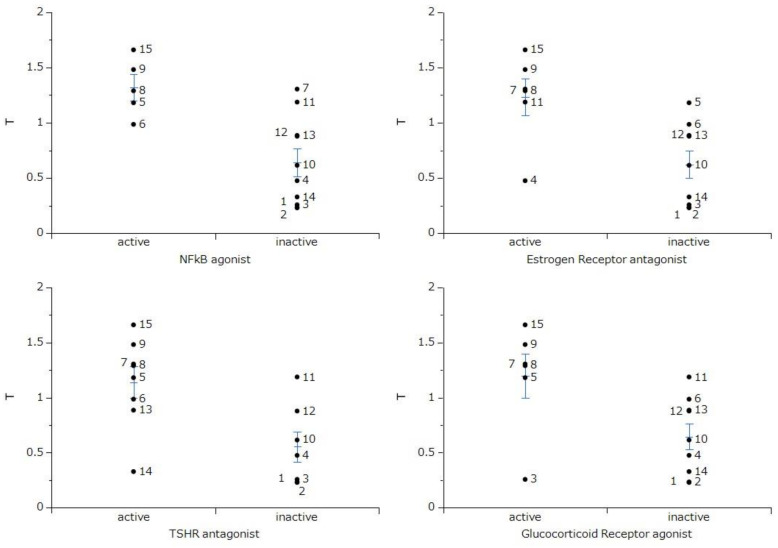
Nuclear receptors and stress response pathways that are possibly involved in the inhibition of OSCC growth by 4,6,8-trimethyl azulene amide derivatives were predicted. The specific cytotoxicity against OSCC cells were correlated with nuclear factor-kappa B (NFκB) agonist, estrogen receptor alpha with stimulator antagonist, thyroid stimulating hormone receptor (TSHR) antagonist, and glucocorticoid receptor agonist (Figure 7). These data suggest that the tumor-specificity of 4,6,8-trimethyl azulene amide derivatives might be coupled to the signaling pathway of NFκB and estrogen, thyroid stimulating hormone and glucocorticoid receptors.
Figure 7.
Nuclear receptor and stress response pathway involved in the selective toxicity against human oral squamous cell carcinoma cell lines. t-Test was performed on tumor cytotoxicity (T) between azulene derivatives predicted as active and inactive in each biochemical pathway. NFκB and TSHR indicate nuclear factor-kappa B and thyroid stimulating receptor, respectively.
3. Discussion
The present study demonstrated that tumor-specificity of fifteen 4,6,8-trimethyl azulene amide derivatives (mean TS value = 4.1) was generally lower than that of doxorubicin (TS = 35) (Table 1), confirming our previous papers (mean TS = 1.5) [13], 5.1 [14] and 2.0 [15]. Compounds 6–11 with alkyl groups showed a higher TS value (mean TS = 5.2) than compounds 1–5 with hydroxyalkyl groups (TS = 1.7) (Table 1). The size of side chain also may be the determinant of TS value: compounds 7, 9, and 15 having C4, C4, and C7 chain length showed the highest TS value (7.8, 5.7 and 17.9) (Table 1). This was supported by the QSAR analysis (Figure 6) that suggests the close association of TS value with chemical descriptors that reflect the 3D structure (AATSC0v, FASA_H, GATS4s, GATS1se, FASA_P vsurf_CW5) (Figure 6).
Dose–response curve demonstrated that compound 15 with the highest TS value inhibited the growth of Ca9-22 cells without complete killing of the cells (Figure 2C). Compound 15 induced trace amounts of a subG1 population (that reflects DNA fragmentation) (p = 0.029) (Figure 4) and caspase-3 activation (assessed by cleavage of PARP and procaspase 3) (Figure 5).
On the other hand, both compounds 7 and 9 were rather cytotoxic, inducing cell shrinkage (Figure 3C–F) and the accumulation of a subG1 population above 80 and 60 μM, respectively (p < 0.027) (Figure 2B), to a similar extent that was attained by actinomycin D (Figure 4). However, their caspase 3 activating activity was much lower than that of actinomycin D (Figure 5). This suggests the possibility that compounds 7 and 9 may induce different types of cell death from apoptosis.
Finally, a possible signaling pathway of 4,6,8-trimethyl azulene amide derivatives was estimated by Toxicity Predicators. Their tumor-specificity was matched at a higher probability with the onset of a signaling pathway of NFκB, and receptors for estrogen, thyroid stimulating hormone, and glucocorticoid (Figure 7). This is consistent with the reported anti-inflammatory activity of guaiazulene [4,9,20,21,22]. On the other hand, the involvement of other signaling pathways such as caspase and androgen receptor (Figure S7), transforming growth factor β (TGFβ), peroxisome proliferator activated receptor δ (PPARδ), endoplasmic reticulum stress (ER stress) response, and retinoid X receptor-α(RXR) (Figure S8) seems to be low. This further supports the non-apoptotic cell death induced by compounds 7, 9, and 15. It remains to identify the type of cell death induced by these compounds.
4. Materials and Methods
4.1. Materials
The following chemicals were obtained from the indicated companies: Dulbecco’s modified Eagle’s medium (DMEM) from Thermo Fisher Scientific (Waltham, MA, USA); FBS, 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT), doxorubicin-HCl (DOX), melphalan (L-PAM) from Sigma-Aldrich (St. Louis, MO, USA); dimethyl sulfoxide (DMSO), actinomycin D from Fujifilm Wako Pure Chemical (Osaka, Japan); 5-FU from Kyowa (Tokyo, Japan); culture plastic dishes and 96-well plates from Techno Plastic Products (Trasadingen, Switzerland). Protease and phosphatase inhibitors were purchased from Roche Diagnostics (Basel, Switzerland).
4.2. Synthesis of Alkylamidoazulene Groups
N-(2-hydroxyethyl)-4,6,8-trimethylazulene-1-carboxamide (compound 1), N-(3-hydroxypropyl)-4,6,8-trimethylazulene-1-carboxamide (compound 2), N-(4-hydroxybutyl)-4,6,8-trimethylazulene-1-carboxamide (compound 3), N-(5-hydroxypentyl)-4,6,8-trimethylazulene-1-carboxamide (compound 4), N-(6-hydroxyhexyl)-4,6,8-trimethylazulene-1-carboxamide (compound 5), N-propyl-4,6,8-trimethylazulene-1-carboxamide (compound 6), N-butyl-4,6,8-trimethylazulene-1-carboxamide (compound 7), N-pentyl-4,6,8-trimethylazulene-1-carboxamide (compound 8), N-hexyl-4,6,8-trimethylazulene-1-carboxamide (compound 9), N-(2-methoxyethyl)-4,6,8-trimethylazulene-1-carboxamide (compound 10), N-(3-methoxypropyl)-4,6,8-trimethylazulene-1-carboxamide (compound 11), N-(2-N′,N′-dimethylaminoethyl)-4,6,8-trimethylazulene-1-carboxamide (compound 12), N-(3-N′,N′-dimethylaminopropyl)-4,6,8-trimethylazulene-1-carboxamide (compound 13), N-(2-morpholinoethyl)-4,6,8-trimethylazulene-1-carboxamide (compound 14) and N-(2-phenylethyl)-4,6,8-trimethylazulene-1-carboxamide (compound 15) were synthesized by the reaction of trichloroacetyl derivatives and each amine at high yields, according to a previously published method [23,24,25].
4.3. Cell Culture
Human normal oral cells (HGF, HPLF, HPC) were established according to the guideline of intramural Ethic Committee (No. A0808) at 12–20 population doubling level (PDL) [26] and OSCC cell lines (Ca9-22, HSC-2, HSC-3, HSC-4), rat adrenal pheochromocytoma cell line (PC12), a human neuroblastoma cell line (SH-SY5Y), and rat Schwann cell line (LY-PPB6) (Riken Cell Bank, Tsukuba, Japan) were cultured at 37 °C in DMEM supplemented with 10% heat (56 °C, 30 min)-inactivated FBS, 100 U/mL, penicillin G and 100 µg/mL streptomycin sulfate under a humidified 5% CO2 atmosphere, as described previously [16].
Differentiated PC12 cells were prepared by the “overlay method”, as described previously. In short, PC12 cells were cultured in the serum-free DMEM supplemented with 50 ng/mL NGF, and at Day 3 overlayed with fresh NGF solution. The Day 6 cells with ex-tended neurites were used for the experiment.
4.4. Synthesis Assay for Cytotoxic Activity
Cells were inoculated at 2 × 103 cells/0.1 mL in a 96-microwell plate. After 48 h, the medium was replaced with 0.1 mL of fresh medium containing different concentrations of test compounds. Control cells were treated with the same amounts of DMSO present in each diluent solution. Cells were incubated for 48 h and the relative viable cell number was then determined by the MTT method, as described previously [15]. We have prepared the controls that contain DMSO (1, 0.5, 0.25, 0.125, 0.063, 0.031, 0.016, 0.008%). Cytotoxicity induced by DMSO alone was subtracted from each well of a 96-microwell plate. The CC50 was determined from the dose–response curve of triplicate samples.
4.5. Calculation of Tumor-Selectivity Index (TS)
TS was calculated by dividing the mean CC50 (HGF + HPLF + HPC) by the mean CC50 (Ca9-22 + HSC-2 + HSC-3 + HSC-4), using seven cell lines ((D/B) in Table 1) [15], or dividing the CC50 (HGF) by the CC50 (Ca9-22) [(C/A) in Table 1], using two cell lines derived from the gingival tissue [27]. Normal keratinocytes, which are highly sensitive to many anticancer drugs [13,28], were not used in this study.
4.6. Calculation of Potency-Selectivity Expression (PSE)
PSE was calculated by dividing the TS value by the CC50 against tumor cells [15,29] [(D/B2) × 100 and (C/A2) × 100] (Table 1).
4.7. Western Blot Analysis
The cells were washed, lysed, and their protein extracts subjected to Western blot (WB) analysis, as described previously [30]. All protein samples of cell lysates (15 μg) were separated by SDS-PAGE using a Mini-Protean 3 Cell system (Bio-Rad Laboratories, Hercules, CA, USA). After electrophoresis, the separated proteins were transferred onto a PVDF filter using a Trans-Blot Turbo System (Bio-Rad Laboratories). The blots were blocked at room temperature for 50 min in skim milk (Morinaga-Nyugyo, Tokyo, Japan) and then probed for 120 min with a primary antibody cocktail (1:250) from Apoptosis Western Blot Cocktail kit (Abcam, Cambridge, UK). The blots were washed three times with Tris-buffered saline (pH 7.6) containing 0.05% Tween 20 and then probed for 90 min with a horseradish peroxidase-conjugated secondary antibody cocktail (1:100) from the kit. Immunoreactivities were detected using Amersham ECL Select (Cytiva, Tokyo, Japan). Images were acquired using ChemiDoc MP System (Bio-Rad Laboratories) and Image Lab 4.1 software (Bio-Rad Laboratories) [30].
4.8. Cell Cycle Analysis
Cells (approximately 106 cells) were fixed with paraformaldehyde (Fujifilm Wako Pure Chemical) in PBS(−) and treated with ribonuclease (RNase) A (Sigma-Aldrich). After staining with propidium iodide (PI, Fujifilm Wako Pure Chemical) in the presence of 0.01% Nonidet-40 (Nacalai Tesque, Kyoto, Japan) to prevent cell aggregation, the cells were filtered through Falcon® cell strainers (Corning Inc., Corning, NY, USA) and then subjected to cell sorting (SH800 Series, SONY, Tokyo, Japan), as described previously [16]. Cell cycle analysis was performed with Cell Sorter Software version 2.1.2. (SONY) [16].
4.9. Calculation of Chemical Descriptors
pCC50 (i.e., the −log CC50) was used for the comparison of the cytotoxicity between the compounds, since the CC50 values had a distribution pattern close to a logarithmic normal distribution. The mean pCC50 values for normal cells and tumor cell lines were defined as N and T, respectively [31]. Thus, T represents -log (mean CC50 against OSCC), N represents −log (mean CC50 against normal oral cells, T-N represents −log (mean CC50 for normal cells/mean CC50 for OSCC). The chemical structures were cleaned and standardized (removing salts and adjusting the protonation state (neutralize)). Then, the 3D-structure of each compound was generated by CORINA Classic (Molecular Networks GmbH, Nürnberg, Germany) and determined optimal 3D-structure with force field calculations (amber-10: EHT) in Molecular Operating Environment (MOE) version 2020.09 (Chemical Computing Group, Quebec, Canada). Chemical 2D and 3D descriptors were calculated with MOE version 2020.9 and Mordred version 1.2.0 (Python library) [32] based on optimal 3D structures. Descriptors that were duplicated and contained missing values and outliers were excluded from this analysis. Note that we regarded results outside 1st quartile −3 × interquartile (IQR) to 3rd quartile +3 × IQR range as outliers. Then, the multicollinearity of descriptors was analyzed. A threshold of 1 of the absolute value of the correlation coefficient was adopted as multicollinearity. When multicollinearity was detected, only descriptors that showed the highest correlation with objective variables among multicollinear descriptors was adopted. Finally, 1520 descriptors were used for this analysis.
4.10. Calculation of Chemical Descriptors
The activities against 59 signaling pathways [33], agonist and antagonist activities of the nuclear receptor, and stress response pathway were calculated by the chemical structures. In other words, all azulene derivatives were classified as positive or negative based on the calculated probabilities in Tox21 activity scores of 1 or higher for each signaling pathway using the Toxicity Predictor [33].
4.11. Statistical Analysis
Each experimental value was expressed as the mean ± standard deviation (SD) of triplicate or quadruplicate measurements. One-way ANOVA and Dunnett’s post-test were performed using IBM SPSS 27.0 statistics (IBM Co., Armonk, NY, USA). The correlation between chemical descriptors and cytotoxicity or tumor specificity was investigated using simple regression analyses by scikit-learn and SciPy with Python 3.8.5. Student’s t-test was performed using JMP Pro 6 (SAS Institute, Cary, NC, USA). The significance level was set at p < 0.05.
5. Conclusions
The present study demonstrated that three compounds from fifteen 4,6,8-trimethyl azulene amide derivatives selectively inhibited the growth of human oral squamous cell carcinoma cell lines. Their actions are either cytotoxic or cytostatic, accumulating subG1. The 3D-structure may be the determinant of tumor-selectivity. There was possible involvement of inflammation and hormone receptor pathway rather than caspase pathway in the selective cytotoxicity against OSCC cells. At present, TS values of compounds 7, 9, and 15 are not so high compared with anticancer drugs (Table 1). Since compound 9 was cytotoxic, further chemical modification of this compound that enhances the TS value should be done. On the other hand, compound 7, compound 15, and 5-FU showed cytostatic growth inhibition, and their action may be potentiated through combination with other types of anticancer drugs [34].
Acknowledgments
The authors thank Meikai and Universities for providing us with a comfortable research atmosphere (equipment).
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijms23052601/s1.
Author Contributions
Conceptualization, H.S., Y.U. and H.W.; software, K.K. and Y.U.; formal analysis, K.B.; investigation, K.N., Y.O., H.S., T.M., K.S., S.A. and Y.I.; writing—original draft preparation, H.S.; writing—review and editing, H.S., Y.U., M.H. and H.W.; funding acquisition, Y.U. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded in part by KAKENHI from the Japan Society for the Promotion of Science (JSPS) (No. 20K09885) (H.S.); Meikai University Miyata Research Fund B (H.S.); Josai University Research Fund (H.W.).
Institutional Review Board Statement
Ethical review and approval were waived for this study since we used only cultured cells that had been purchased from the RIKEN Cell Bank and the human normal oral cells established in our laboratory 11 years ago according to the guidelines of the intramural Ethics Committee (No. A0808).
Informed Consent Statement
Not applicable since we used only cultured cells.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Shoji T., Ito S., Yasunami M. Synthesis of Azulene Derivatives from 2H-Cyclohepta[b]furan-2-ones as Starting Materials: Their Reactivity and Properties. Int. J. Mol. Sci. 2021;22:10686. doi: 10.3390/ijms221910686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shoji T., Okujima T., Ito S. Development of Heterocycle-Substituted and Fused Azulenes in the Last Decade (2010–2020) Int. J. Mol. Sci. 2020;21:7087. doi: 10.3390/ijms21197087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murfin L.C., Lewis S.E. Azulene-A Bright Core for Sensing and Imaging. Molecules. 2021;26:353. doi: 10.3390/molecules26020353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bakun P., Czarczynska-Goslinska B., Goslinski T., Lijewski S. In vitro and in vivo biological activities of azulene derivatives with potential applications in medicine. Med. Chem. Res. 2021;30:834–846. doi: 10.1007/s00044-021-02701-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Okajima M., Miura S., Watanabe S., Tanaka H., Ito K., Ishida T., Makino M., Iwashima A., Matsumoto N., Sato K., et al. A prospective phase II study of multimodal prophylactic treatment for afatinib-induced adverse events in advanced non-small cell lung cancer (Niigata Lung Cancer Treatment Group 1401) Transl. Lung Cancer Res. 2021;10:252–260. doi: 10.21037/tlcr-20-649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Riley P., Glenny A.M., Hua F., Worthington H.V. Pharmacological interventions for preventing dry mouth and salivary gland dysfunction following radiotherapy. Cochrane Database Syst. Rev. 2017;7:Cd012744. doi: 10.1002/14651858.CD012744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hirasawa R., Tatsuta M., Iishi H., Baba M. Effect of marzulene on the restitution of rat gastric mucosa after NaOH-induced injury. Hepatogastroenterology. 1998;45:293–296. [PubMed] [Google Scholar]
- 8.Kourounakis A.P., Rekka E.A., Kourounakis P.N. Antioxidant activity of guaiazulene and protection against paracetamol hepatotoxicity in rats. J. Pharm. Pharmacol. 1997;49:938–942. doi: 10.1111/j.2042-7158.1997.tb06140.x. [DOI] [PubMed] [Google Scholar]
- 9.Phutim-Mangkhalthon A., Teerakapong A., Tippayawat P., Morales N.P., Morkmued S., Puasiri S., Priprem A., Damrongrungruang T. Anti-inflammatory effect of photodynamic therapy using guaiazulene and red lasers on peripheral blood mononuclear cells. Photodiag. Photodyn. Ther. 2020;31:101747. doi: 10.1016/j.pdpdt.2020.101747. [DOI] [PubMed] [Google Scholar]
- 10.Ayaz F., Yuzer A., Ince T., Ince M. Anti-Cancer and Anti-Inflammatory Activities of Bromo- and Cyano-Substituted Azulene Derivatives. Inflammation. 2020;43:1009–1018. doi: 10.1007/s10753-020-01186-0. [DOI] [PubMed] [Google Scholar]
- 11.Sibanda T., Selvarajan R., Tekere M., Nyoni H., Meddows-Taylor S. Potential biotechnological capabilities of cultivable mycobiota from carwash effluents. Microbiologyopen. 2017;6:e00498. doi: 10.1002/mbo3.498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li H., Hu Y., Wang X., He G., Xu Y., Zhu Q. Novel tricyclic poly (ADP-ribose) polymerase-1/2 inhibitors with potent anticancer chemopotentiating activity: Design, synthesis and biological evaluation. Bioorg. Med. Chem. 2016;24:4731–4740. doi: 10.1016/j.bmc.2016.08.016. [DOI] [PubMed] [Google Scholar]
- 13.Sakagami H., Okudaira N., Masuda Y., Amano O., Yokose S., Kanda Y., Suguro M., Natori T., Oizumi H., Oizumi T. Induction of Apoptosis in Human Oral Keratinocyte by Doxorubicin. Anticancer Res. 2017;37:1023–1029. doi: 10.21873/anticanres.11412. [DOI] [PubMed] [Google Scholar]
- 14.Uehara M., Minemura H., Ohno T., Hashimoto M., Wakabayashi H., Okudaira N., Sakagami H. In Vitro Antitumor Activity of Alkylaminoguaiazulenes. In Vivo. 2018;32:541–547. doi: 10.21873/invivo.11273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wada T., Maruyama R., Irie Y., Hashimoto M., Wakabayashi H., Okudaira N., Uesawa Y., Kagaya H., Sakagami H. In Vitro Anti-tumor Activity of Azulene Amide Derivatives. In Vivo. 2018;32:479–486. doi: 10.21873/invivo.11264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Imanari K., Hashimoto M., Wakabayashi H., Okudaira N., Bandow K., Nagai J., Tomomura M., Tomomura A., Uesawa Y., Sakagami H. Quantitative Structure-Cytotoxicity Relationship of Azulene Amide Derivatives. Anticancer Res. 2019;39:3507–3518. doi: 10.21873/anticanres.13497. [DOI] [PubMed] [Google Scholar]
- 17.Fumagalli G., Monza L., Cavaletti G., Rigolio R., Meregalli C. Neuroinflammatory Process Involved in Different Preclinical Models of Chemotherapy-Induced Peripheral Neuropathy. Front. Immunol. 2020;11:626687. doi: 10.3389/fimmu.2020.626687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sałat K. Chemotherapy-induced peripheral neuropathy-part 2: Focus on the prevention of oxaliplatin-induced neurotoxicity. Pharmacol. Rep. 2020;72:508–527. doi: 10.1007/s43440-020-00106-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Iijima Y., Bandow K., Amano S., Sano M., Hino S., Kaneko T., Horie N., Sakagami H. Protection of Bortezomib-induced Neurotoxicity by Antioxidants. Anticancer Res. 2020;40:3685–3696. doi: 10.21873/anticanres.14357. [DOI] [PubMed] [Google Scholar]
- 20.Magori N., Fujita T., Kumamoto E. Hinokitiol inhibits compound action potentials in the frog sciatic nerve. Eur. J. Pharmacol. 2018;819:254–260. doi: 10.1016/j.ejphar.2017.12.014. [DOI] [PubMed] [Google Scholar]
- 21.Cao T., Li Y., Yang Z., Yuan M., Li Y., Yang H., Feng Y., Yin S. Synthesis and Biological Evaluation of 3, 8-dimethyl-5-isopropylazulene Derivatives as Anti-gastric Ulcer Agent. Chem. Biol. Drug Des. 2016;88:264–271. doi: 10.1111/cbdd.12753. [DOI] [PubMed] [Google Scholar]
- 22.Ortiz M.I., Fernández-Martínez E., Soria-Jasso L.E., Lucas-Gómez I., Villagómez-Ibarra R., González-García M.P., Castañeda-Hernández G., Salinas-Caballero M. Isolation, identification and molecular docking as cyclooxygenase (COX) inhibitors of the main constituents of Matricaria chamomilla L. extract and its synergistic interaction with diclofenac on nociception and gastric damage in rats. Biomed. Pharmacother. 2016;78:248–256. doi: 10.1016/j.biopha.2016.01.029. [DOI] [PubMed] [Google Scholar]
- 23.Anderson A.G., Anderson R.G., Fujita T.S. Displacement reactions on 1-azulylmethyltrimethylammonium iodide. J. Org. Chem. 1962;27:4535–4539. doi: 10.1021/jo01059a100. [DOI] [Google Scholar]
- 24.Mathias L.J., Overberger C.G. Simple syntheses of 1,3-bis(perfluoroacethyl)azulene and 1,3-azulenedicarboxylic acid. J. Org. Chem. 1980;45:1701–1703. doi: 10.1021/jo01297a041. [DOI] [Google Scholar]
- 25.Toyama Y., Miyazawa S., Yokota M. Azulenes, their preparation, and antibacterial agents containing them. Jpn. Kokai Tokkyo Koho. 2014:JP 2004217602 A 2020040805. [Google Scholar]
- 26.Kantoh K., Ono M., Nakamura Y., Nakamura Y., Hashimoto K., Sakagami H., Wakabayashi H. Hormetic and anti-radiation effects of tropolone-related compounds. In Vivo. 2010;24:843–851. [PubMed] [Google Scholar]
- 27.Horikoshi M., Kimura Y., Nagura H., Ono T., Ito H. A new human cell line derived from human carcinoma of the gingiva. I. Its establishment and morphological studies. Nihon Koku Geka Gakkai Zasshi. 1974;20:100–106. doi: 10.5794/jjoms.20.100. [DOI] [PubMed] [Google Scholar]
- 28.Sugita Y., Takao K., Uesawa Y., Nagai J., Iijima Y., Sano M., Sakagami H. Development of Newly Synthesized Chromone Derivatives with High Tumor Specificity against Human Oral Squamous Cell Carcinoma. Medicines. 2020;7:50. doi: 10.3390/medicines7090050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sakagami H., Furukawa T., Satoh K., Amano S., Iijima Y., Koshikawa T., Asai D., Fukuchi K., Takemura H., Kanamoto T., et al. Re-Evaluation of Chemotherapeutic Potential of Pyoktanin Blue. Medicines. 2021;8:33. doi: 10.3390/medicines8070033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yamali C., Sakagami H., Uesawa Y., Kurosaki K., Satoh K., Masuda Y., Yokose S., Ece A., Bua S., Angeli A., et al. Comprehensive study on potent and selective carbonic anhydrase inhibitors: Synthesis, bioactivities and molecular modelling studies of 4-(3-(2-arylidenehydrazine-1-carbonyl)-5-(thiophen-2-yl)-1H-pyrazole-1-yl) benzenesulfonamides. Eur. J. Med. Chem. 2021;217:113351. doi: 10.1016/j.ejmech.2021.113351. [DOI] [PubMed] [Google Scholar]
- 31.Nagai J., Shi H., Kubota Y., Bandow K., Okudaira N., Uesawa Y., Sakagami H., Tomomura M., Tomomura A., Takao K., et al. Quantitative Structure-Cytotoxicity Relationship of Pyrano[4,3-b]chromones. Anticancer Res. 2018;38:4449–4457. doi: 10.21873/anticanres.12747. [DOI] [PubMed] [Google Scholar]
- 32.Moriwaki H., Tian Y.S., Kawashita N., Takagi T. Mordred: A molecular descriptor calculator. J. Cheminform. 2018;10:4. doi: 10.1186/s13321-018-0258-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kurosaki K., Wu R., Uesawa Y. A Toxicity Prediction Tool for Potential Agonist/Antagonist Activities in Molecular Initiating Events Based on Chemical Structures. Int. J. Mol. Sci. 2020;21:7853. doi: 10.3390/ijms21217853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang B., Zhou F., Hong J., Ng D.M., Yang T., Zhou X., Jin J., Zhou F., Chen P., Xu Y. The role of FOLFIRINOX in metastatic pancreatic cancer: A meta-analysis. World J. Surg. Oncol. 2021;19:182. doi: 10.1186/s12957-021-02291-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.