Abstract
Background
Refugees, and other forcibly displaced people, face mental distress and may be disproportionately affected by risk factors for suicide. Little is known about suicidal behaviour in these highly mobile populations because collecting timely, relevant, and reliable data is challenging.
Methods and findings
A systematic review was performed to identify studies of any design reporting on suicide, suicide attempts, or suicidal ideation among populations of displaced people. A sensitive electronic database search was performed in August 2020, and all retrieved studies were screened for relevance by two authors. Studies were categorised by the population being evaluated: refugees granted asylum, refugees living in temporary camps, asylum seekers, or internally displaced people. We distinguished between whether the sampling procedure in the studies was likely to be representative, or the sample examined a specific non-representative subgroup of displaced people (such as those already diagnosed with mental illness). Data on the rates of suicide or the prevalence of suicide attempts or suicidal ideation were extracted by one reviewer and verified by a second reviewer from each study and converted to common metrics. After screening 4347 articles, 87 reports of 77 unique studies were included. Of these, 53 were studies in representative samples, and 24 were based on samples of specific target populations. Most studies were conducted in high-income countries, and the most studied population subgroup was refugees granted asylum. There was substantial heterogeneity across data sources and measurement instruments utilised. Sample sizes of displaced people ranged from 33 to 196,941 in studies using general samples. Suicide rates varied considerably, from 4 to 290 per 100,000 person-years across studies. Only 8 studies were identified that compared suicide rates with the host population. The prevalence of suicide attempts ranged from 0.14% to 15.1% across all studies and varied according to the prevalence period evaluated. Suicidal ideation prevalence varied from 0.17% to 70.6% across studies. Among refugees granted asylum, there was evidence of a lower risk of suicide compared with the host population in 4 of 5 studies. In contrast, in asylum seekers there was evidence of a higher suicide risk in 2 of 3 studies, and of a higher risk of suicidal ideation among refugees living in camps in 2 of 3 studies compared to host populations.
Conclusion
While multiple studies overall have been published in the literature on this topic, the evidence base is still sparse for refugees in camps, asylum seekers, and internally displaced people. Less than half of the included studies reported on suicide or suicide attempt outcomes, with most reporting on suicidal ideation. International research networks could usefully define criteria, definitions, and study designs to help standardise and facilitate more research in this important area.
Registration
PROSPERO CRD42019137242.
Introduction
Conflict remains a substantial threat to global population health. The number of people forcibly displaced is higher than ever with record levels of 82.4 million in 2020 (>1% of the world’s population), which is more than double compared to 10 years earlier [1]. Internally displaced people (IDP) make up the largest group of displaced people, at 48.0 million in 2020 [2]. The numbers of refugees and asylum seekers are estimated at 26.4 million and 4.1 million in 2020, respectively [2]. As conflicts become more protracted, the management of non-communicable disease and mental health have resulted in additional challenges [3, 4].
Suicide and suicide attempts have a profound impact on individuals, families, and communities. The World Health Organization (WHO) estimates that approximately 700,000 individuals died by suicide in 2019, with men dying at about twice the rates among women [5]. It is among the leading causes of death worldwide, with more deaths due to suicide than to malaria, breast cancer, war and homicide. The reduction of suicide mortality has been prioritized by the WHO as a global target and included as an indicator in the United Nations Sustainable Development Goals (SDGs) under target 3.4 [6, 7].
Refugees and other forcibly displaced people may be disproportionately affected by suicide risk [8, 9]. Mental health may be adversely impacted by displacement. Refugees face additional stressors during enforced departure from their homeland and on arrival in the host country such as discrimination, detention, language and cultural barriers [8]. ‘Losses’ identified include family and friends, homeland, status, community contact, language, financial assets, income, and financial security [10]. While most suicides are known to occur in low- and middle-income countries (79%) [11], the risks of suicide and suicidal behaviour among forcibly displaced people are unknown.
Previous reviews of suicide in refugee populations found a range of suicide proportions from 3.4% to 34% of recorded deaths [8]. Little is known about populations still in displacement because collecting timely, relevant, and reliable data is challenging in populations that are highly mobile. Suicide is also heavily stigmatized or even illegal in many countries, so suicidal behaviours may go under-reported and people at risk of suicide may be reluctant to seek help [12]. Regular monitoring of suicide across different risk groups is essential for effective national suicide prevention strategies [13]. This provides essential information for understanding the scope of the problem so that interventions can be tailored to meet the needs of specific populations.
This systematic review aims to synthesise what is known about the rates and prevalence of suicide and suicidal behaviour among displaced people from published literature.
Methods
The protocol for this systematic review was registered with PROSPERO (CRD42019137242). In the review protocol it was planned to include studies of people who have been displaced because of natural disasters, but due to the large number of studies, estimates from these populations will now be reported in a separate systematic review. Initially, studies on populations affected by conflict but who have not been displaced were also considered for inclusion. However, the difficulty in defining these populations and the variable level of exposure to conflict, led the author team to decide against including these studies. Studies were also excluded if they reported prevalence estimates for returned asylum seekers or displaced populations (i.e. people not currently displaced), or for economic migrants.
Inclusion criteria
Study designs
Studies of any design that could provide an estimate of the rate or prevalence of suicide or suicide attempts, or prevalence of suicidal ideation, in populations of displaced people were considered for inclusion. This included observational studies (longitudinal population-based cohort studies, case-control, and cross-sectional surveys) and baseline rates or prevalence in randomised controlled trials of interventions targeted at the populations of interest. Case reports, reviews, and case series were excluded. Publication status was not used to determine eligibility.
Populations
Studies were included if they reported on populations (of any age) of forcibly displaced people, which we defined as people who have had to leave their homes in the context of an emergency because of a deliberate event such as conflict or war. This includes those who identified as refugees or asylum seekers (i.e. displaced people who cross international borders) as well as internally displaced people (i.e. people who remain in their own country). A list of common definitions for terms used in this review are provided in Box 1.
Box 1. Definitions of subgroups of displaced people used in this review.
Outcomes
All studies reporting data on rate or prevalence of suicide, suicide attempts, and suicidal ideation among populations of displaced people were considered for inclusion. For this review we consider suicidal ideation to mean having thoughts or ideas about the possibility of ending one’s life, a suicide attempt to be an attempt to die by suicide that results in survival, and suicide to be intentionally causing one’s death. These outcomes were defined in each study by the authors of the primary studies. We considered suicide estimates measured by death registers, surveillance systems, autopsies (verbal and recorded), and medical records, and estimates of suicidal attempts and ideation measured using validated tools or survey questions.
As the design of the included studies varied, the source and type of data reported for these outcomes also varied. All relevant data for these outcomes was extracted and presented according to data source, host country, and prevalence period (i.e. lifetime prevalence, point prevalence). Where available, data were also extracted on comparative estimates between displaced people and host or general populations.
Search methods
A broad search strategy informed by experts in this area was developed to maximise sensitivity, combining medical subject headings and free text terms (see S1 Table) to identify relevant studies in the following databases:
MEDLINE (Pubmed)
Embase (OVID)
CINAHL (Cumulative Index to Nursing and Allied Health Literature, EBSCOHost)
PsycINFO (EBSCOHost)
Social Science Citation Index (SSCI, Web of Science)
Scopus (Elsevier)
Global Index Medicus at http://search.bvsalud.org/ghl/index.php
Suicide Information and Education Collection (SIEC) database
Searches were conducted in April 2019 and updated in August 2020. Searches were not limited by publication date, geographical location, or language. The reference lists of relevant articles and reviews were screened to identify additional studies.
Selection of studies
Two reviewers independently screened the abstracts of all studies identified by the search strategy. Following this stage, two reviewers also independently screened full texts of studies appearing to meet the inclusion criteria. Discrepancies were discussed among the reviewers, and where necessary a third reviewer assessed the study under discussion until a consensus was reached.
Data extraction and management
One reviewer extracted study characteristics and relevant outcome data from all included studies. A second reviewer cross-checked all extracted data and any discrepancies between the two reviewers were discussed. Relevant information extracted from each study included: population characteristics (such as ethnicity, age, religion, trauma exposure, and duration of resettlement), setting, study design, study dates, data collection method and source of data. For each of the three outcomes of interest, the number of participants analysed as well as summary statistics were extracted where available. Host countries/territories (where studies were conducted) were classified into the four World Bank income levels (i.e., low, lower middle, upper middle, high).
Methodological quality
The search strategy was designed to capture the breadth of the available literature in this population. As a result, a variety of study designs were considered for inclusion in this review. This prevented the use of a single checklist approach to assessing methodological quality and required a more pragmatic approach. The assessment in this review was based on the study design and the source from which data were obtained. Using this pragmatic approach, we judged studies drawing on vital events registration, specific demographic surveillance, and longitudinal population-based cohorts to be of higher quality while studies drawing on data from retrospective cohorts/analysis and cross-sectional surveys were considered low quality.
Data synthesis
The following common metrics were calculated using the extracted data for each study, when possible, to facilitate comparison across studies, population groups, and settings: suicide rate per 100,000 person-years, prevalence of suicide attempt in percentage, and prevalence of suicidal ideation in percentage with 95% confidence intervals (CIs). Where data were also available comparing the rates or prevalence of the three outcomes in displaced people with the general population of the host country, relative estimates (relative risks or hazard ratios) with 95% CIs were calculated and presented.
We chose not to pool rates of suicide across studies due to the heterogeneity of study designs and used narrative syntheses with tabulated and textual descriptions systematically reporting results for the three aspects of suicidal behaviour. Comparative results with host populations were synthesised using the vote counting based on the direction of effect method [14, 15].
The reporting of studies and results in this review are grouped into two main categories, based on their likely representativeness to the target population or to a target subgroup (for example, adolescents, pregnant women):
studies using representative or non-selected samples of the target group (that is, evaluating where possible the whole population or whole subgroup, as applicable), referred to below as “general samples”, and
studies using selected samples of the target group based on their inclusion criteria that may confound the outcomes (for example, known high risk groups within the populations of displaced people, such as those already diagnosed with mental illness), referred to below as “specific samples”.
Furthermore, within each category results are presented separately for the following five population subgroups:
refugees granted permanent asylum status,
refugees living in refugee camps or with only temporary protection,
asylum seekers,
mixed samples of refugees & asylum seekers, and
internally displaced people.
Due to possible overlap, if a study reports the population as asylum seekers living in camps, this was categorised under refugees living in camps.
Results
Included studies
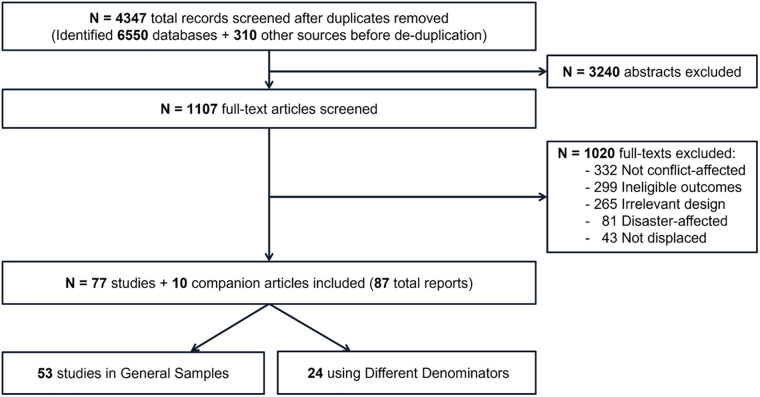
A total of 6899 records were identified by the electronic searches. Following removal of duplicates, 4347 abstracts were screened by two reviewers. Of these, 1107 full-text articles were considered potentially relevant. Finally, 87 articles reporting on 77 studies [16–92] plus 10 companion articles [93–102] were included in this review. Reasons for study exclusions are outlined in the PRISMA flow diagram (Fig 1). Five of the included articles were published in languages other than English. These were Danish, Dutch, two in German, and Spanish [50, 79, 83, 90, 99].
Fig 1. PRISMA flow diagram.
Of the 77 included studies, 53 were in general samples and 24 used specific samples. The types of data sources used for each outcome are presented below. Characteristics of the 53 included studies and their populations that used general samples are presented in Table 1, grouped by population subgroup. Additional characteristics are also reported in the corresponding outcome results tables. Study characteristics and results for the specific samples (n = 24 studies) are reported in S2 Table. The various samples evaluated by these studies included people diagnosed/referred for mental health conditions, intoxication-related emergency department admissions, forensic autopsies ordered by attorney’s office, and emergency department admissions that required a forensic exam.
Table 1. Characteristics of included studies using general samples, grouped by population type.
| Author, Pub. Year | Population Summary | Setting | Ethnicity (Region of Origin) | Age* (y) | Gender | Religion | Trauma Exposure | Duration of Resettlement* (y) | Data Collection |
|---|---|---|---|---|---|---|---|---|---|
| Source or Measurement | |||||||||
| Refugees granted permanent asylum status: | |||||||||
| Alley 1982 [18] | Indochinese refugees who had entered Utah (USA) beginning in 1978 | Community | All Indochinese | NR | NR | NR | NR | NR | Survey |
| Amin 2021 [20] | 9-year cohort aged 16–64 years on Dec 31, 2004 | Community | Eritrean, Ethiopian, Somali, Afghani, Iranian, Iraqi, Syrian, Chilean, former Yugoslavian | range: 16–64 | M- 58% | NR | NR | NR | National Cause of Death and inpatient records registers |
| Ao 2016 [21] | Adults in 7 cities in Georgia, New York, Arizona, and Texas | Community | All Bhutanese | median 34 (range: 18–83) | Mixed | 72% Hindu, 10% Buddhist, 16% Christian | 36% had experienced 4–7 traumatic events pre-migration, and 34% had experienced ≥8 | median: 1.8 | Beck Scale for Suicidal Ideation |
| (Range: 0.2–5) | |||||||||
| Bhui 2003 [25] | Somali refugees in the London Borough of Greenwich (UK) | Community | All Somali | mean: 40.4; range: 20–88 | M- 51% | NR | Shortage of food and water, no shelter, poor health, torture, imprisonment, murder, separated from family and enforced isolation | Men: 7.9; Women: 8.2 | BDI Suicide items |
| Choi 2020 [30] | Youth in 7th-12th grade with either father/ mother born in North Korea | Classrooms in middle and high schools | All North Korean | NR | F- 41% | NR | NR | NR | Korean Youth’s Risk Behavior Survey |
| Hollander 2020 [42] | Cohort aged 16 and up who were born between 1975 and 1984 | Community | 19% former Yugoslavian, 18% Iraqi, 13% Central Asian, 11% Somali or Eritrean or Ethiopian or Djibouti, 11% Southeast Asian, 10% Iranian, 7% Baltics or Russian, 7% North Asian, 4% North African | 24.8 (7.0) | M- 59% | NR | NR | 1–6 | Causes of Death Register |
| (at cohort entry) | |||||||||
| Jankovic 2013 [47] | Refugees from former Yugoslavia who experienced war trauma residing in UK, Italy, Germany | NR | All from former Yugoslavia | 41.6 | M- 49% | NR | Mean war events: 6.8 | NR | MINI International Neuropsychiatric Interview |
| (10.8) | |||||||||
| Meyerhoff 2020 [55] | Adults living in the greater Burlington, Vermont region | a local community center and a community mental health clinic serving refugees | All Bhutanese | mean: 41 | M- 52% | 65% Hindu, 17% Buddhist, 13% Christian, 5% Kirat | NR | NR | Beck Scale for Suicidal Ideation |
| Nickerson 2019 [60] | Adults literate in Arabic, Farsi, Tamil or English | Community | 67% Iraqi, 20% Syrian, 6% Iranian, 3% Afghani | 39.0 (12.5) | M- 53% | NR | potentially traumatic events: mean 3.30 (SD 3.30) | 1.44 (1.37) | PHQ-9 (item 9) questionnaire and additional suicidal intent questions |
| Noh 2017 [61] | North Korean refugees living in Seoul (South Korea) | Hana Center (a representative welfare center supported by the Korean government to assist NKRs in South Korea) | All North Korean | ≥30 years | M- 23% | NR | NR | 68% been in South Korea for <5 | Health questionnaire |
| Norredam 2013 [62] | Refugees in Denmark from January 1993 to December 1999 and native Danes | Community | 57% former Yugoslavian, 16% North African, 11% Iraqi, 10% other Middle Eastern | >18 years | Males: Refugees 56%; Danish-born 56% | NR | NR | NR | Danish Register on Causes of Death |
| Park 2018 [64] | North Korean refugee youth living in South Korea | Schools | Born in North Korea or China | mean 19; range: 13 to 17 | M- 33% | NR | NR | NR | Questionnaire |
| Salama 2020† [71] | Migrants living in 6 big cities | Community | 59% Kurdish, 41% Somali | range: 18–64 | F- 52% | Somalis and the majority of Kurds (75%) were Muslim | NR | >1 | Hopkins Symptoms Checklist-25 (suicidal ideation item of HSCL-25) |
| Saunders 2017 [72] | Youth living in Ontario | Community | Mixed | range: 10–24 | M-~50% | NR | NR | Range: 0–10 | Ontario Registrar General Vital Statistics-Deaths registry |
| Saunders 2019 [73] | Adults living in Ontario for <10 years | Community | Mixed | NR | Mixed | NR | NR | <10 | National Ambulatory Care Reporting System and Ontario Registrar General Vital Statistics-Deaths registries |
| Sobhanian 2006 [76] | Former refugee detainees from the Woomera Detention Centre living Australia | Community | Iranian and Afghani | 31.8 (9.2); range: 18 to 70 | M- 69% | NR | NR | Time in the detention centre ranged from 2 to 21 months; 11.30 months (3.80); Time living in the community ranged from 1 to 20; mean 6.97 months | The Truncated Assessment of Self-Destructive |
| Thoughts (TASDT) | |||||||||
| Tousignant1999 [85] | Adolescents from refugee families living in Canada | Schools | 35 countries of origin were represented: El Salvador, Cambodia, Laos, Iran, Vietnam and the regions of Southeast Asia and Central America | mean: 15.7; range: 13 to 19 | M- 48% | NR | NR | NR | Diagnostic Interview Schedule for Children Version 2.25 (DISC-2.25) for DSM-III-R diagnoses |
| Um 2020 [86] | Adults living in Seoul, Gyeonggi Province, and Incheon | Household | All North Korean | mean: 40.6 | F- 67% | 68% Christian | NR | mean: 6.3 | 5-item suicidal ideation scale |
| Vigod 2019 [87] | Mothers within 1 year postpartum in Ontario | Community | Mixed | mean: 30 | F- 100% | NR | NR | NR | National Ambulatory Care Reporting System database |
| Westman 2006 [89] | National cohort aged 25–64 years | Community | Eastern European, Middle Eastern, other non-European countries‡ | range: 25–64 | Mixed (disaggregated below) | NR | NR | NR | National Cause of Death Register |
| Refugees in refugee camps or with temporary protection: | |||||||||
| Akinyemi 2012 [16] | Adults residing >1 year in Oru Refugee Camp | Refugee camp | 66% Liberian, 33% Sierra-Leonean, 1% Togolese | 34.8 (12.8) | M- 59% | 70% Christian, 30% Muslim | NR | 8.6 (4.8) | Mini-International Neuropsychiatric Interview (MINI) |
| Al-Modallal 2012 [17] | Refugee women attending healthcare centers in the cities of Amman, Zarqa, and Irbid (Jordan) | Health care centers in refugee camps | NR | Range: 16 to 62 | F- 100% | NR | NR | NR | Survey |
| Falb 2013 [32] | Refugee women living in 3 camps along the Thai-Burma Border | Refugee camps | Mostly Burmese (79% Karen, 21% other) | 32.1 (8.4) | F- 100% | Christian: 54%; other 46% | 80/848 reported conflict victimization | NR | Questionnaire |
| Fellmeth 2016 [33] | Migrant and refugee pregnant women in a refugee camp along the Thailand-Myanmar border | Refugee camp | Mostly Burmese | Women who died by suicide: 18 to 36 | F- 100% | NR | NR | NR | Clinic review of maternal deaths (MMR among live births) |
| Hermans 2017 [39] | Refugees in long-stay refugee camps at Lesbos (Greece) | Refugee camps | 36% Syrian, 28% Afghani, 20% Pakistani | Median: 23 (IQR 28–38); 23% children | NR | NR | NR | NR | Clinical assessment |
| Itani 2017a [45] | Middle school students in Gaza and West Bank | Occupied Palestinian Territory and UNRWA refugee camps’ schools | All Palestinian | most 13–15 | F- 53% | NR | NR | NR | Global School-based Student Health Survey |
| Itani 2017b [45] | Middle school students in Jordan | UNRWA refugee camp schools | All Palestinian | most 13–15 | M- 52% | NR | NR | NR | Global School-based Student Health Survey |
| Itani 2017c [45] | Middle school students in Lebanon | UNRWA refugee camp schools | All Palestinian | most 13–15 | F- 54% | NR | NR | NR | Global School-based Student Health Survey |
| Itani 2017d [45] | Middle school students in Syria | UNRWA refugee camp schools | All Palestinian | most 13–15 | M- 51% | NR | NR | NR | Global School-based Student Health Survey |
| Rahman 2003 [66] | Afghan mothers in refugee camps in Pakistan | Refugee camps | All Afghani | 28.2 (7.3) | F- 100% | NR | NR | 13 (3.4) months | Pushto version of the Self-Reporting Questionnaire (SRQ- 20) |
| Slodnjak 2002 [75] | Refugee students from Bosnia and Herzegovina and Slovenian students from same age and school grade | School | All Bosnian and Herzegovina | 14 to 15 | M—refugees: 47%; Slovenian-born: 49% | NR | 80% of the student refugees and 90% of their relatives had experienced war events | NR | Interviews |
| Ssenyonga 2012 [78] | Adults resident at Nakivale camp | Refugee camp | All Congolese (DRC) | ≥18 | Mixed | NR | Domestic violence exposure: mean 11.3 (SD 6.3) lifetime events, and 2.1 (SD 3.6) ongoing events | NR | Survey |
| Vijayakumar 2017 [88] | Residents of refugee camps in Tamil Nadu, South India | 2 refugee camps | All Sri Lankan | mean: 40 | F- 58% | 71% Hindu, 29% Christian, 1% Muslim | Trauma during war: a) 31% lost/got separated from significant family member/friend; b) 27% confirmed/presumed death of family member/friend; c) 16% lost/got separated from 1st-degree relative | mean: 18.3 | Beck’s Scale for Suicidal Ideation, and additional questions |
| Yu 2008 [91] | Refugees in protective facilities under the South Korean government protection in 2 Chinese cities | Protective facilities | All North Korean | range: 15–59 | F- 71% | NR | NR | range: from under 1 to over 5 | Personality Assessment Index (Suicide Ideation subscale of PAI; Morey 1991) |
| Mixed refugees populations: | |||||||||
| Stein 2010 [81] | Refugees sub-group among general populations surveyed in 21 low-, middle-, and high-income countries | NR | Nigeria, South Africa, Brazil, Colombia, Mexico, United States, India, Japan, New Zealand, China, Belgium, Bulgaria, France, Germany, Italy, the Netherlands, Romania, Spain, Ukraine, Israel, Lebanon | >18 | Mixed | NR | NR | NR | World Mental Health (WMH) version of the WHO Composite International Diagnostic Interview (CIDI) and Suicidality Module of the WMH-CIDI |
| Asylum seekers: | |||||||||
| Cheney 2017 [29] | Male-to-female transgender asylum seekers in California | An advocacy and immigration legal services organization | All Mexican | mean: 32 (range: 20–58) | 100% male-to-female transgender | NR | All had experienced physical and/or sexual assaults | NR | Review of declaration documents that were part of asylum application, including professional psychological evaluation |
| Cohen 2008 [31] | Asylum seekers in immigration removal centres and prisons | Immigration removal centres and prisons | Mixed | NR | Mixed | NR | NR | NR | Specific monitoring data (from medical records) |
| Fuhrer 2016 [35] | Asylum seekers in Halle (Germany) | NR | Mixed | >15 years | M- 85% | NR | NR | NR | Hopkins-Symptom-Checklist 25 (HSCL 25) and the Harvard Trauma Questionnaire |
| (Had to speak Arab, Farsi/Dari, French, Hindi or English) | |||||||||
| Goosen 2011 [37] | Asylum seekers living in reception centres | Residential asylum seeker reception centres | Afghani, Iraqi, Angolan, Congolese (DRC), Azerbaijani, former Yugoslavian, Somali, Sudanese | ≥15 | Mixed (disaggregated below) | NR | NR | NR | A national standard suicidal behaviour notification form |
| Grupp 2020 [38] | Adults fluent in English, German, French, Farsi, Arabic, Kurdish, or Tigrinya | in their accommodation, at meeting points for asylum seekers, or through language courses | 28% Iranian, 19% Eritrean, 17% Somali, 10% Afghani, 8% Cameroonian, 7% Syrian | 30.5 (8.1) | M- 66% | NR | NR | 15.1 months | PHQ-9 |
| (23.2) | |||||||||
| Huemer 2011 [44] | Unaccompanied minors aged 15–18 years | 8 residential accommodations for unaccompanied refugee minors | 34% Gambian, 27% Somali, 20% Nigerian, 5% Guinea-Bissau, 14% other African | 17.0 (0.8) | M- 85% | 66% Muslim, 22% Christian | NR | NR | Mini-International Neuropsychiatric Interview for children and adolescents (MINI Kid) |
| Keller 2003 [48] | Detained asylum seekers in New York, New Jersey, and Pennsylvania | Detention centers | 77% African, 10% Eastern European, 6% Asian, 4% South American, 3% Middle Eastern | 28 (7.3) | M- 80% | NR | 74% had been tortured before immigration, 59% reported murder of family member or friend, 26% reported sexual assault | NR | Self-report in physician interview |
| Koppenaal 2003 [50] | Asylum seekers accommodated in housing facilities of the Central Organ Asylum Seekers | Housing facilities for asylum seekers | Mixed | All ages included | Mixed | NR | NR | NR | Statistics Netherlands causes of death list |
| Mittendorfer-Rutz 2020 [57] | Unaccompanied minors/ youth | 4 state agencies and 2 NGOs | Mixed | range: 10–21 | Mixed | NR | NR | NR | NGOs data and reports to the Health and Social Care Inspectorate. Validated using the national forensic autopsies register database |
| Nickerson 2019 [60] | Adults literate in Arabic, Farsi, Tamil or English | Community | 48% Iranian, 22% Sri Lankan, 12% Iraqi, 4% Afghani | 35.4 (8.6) | M- 69% | NR | PTE: mean 7.21 (SD 4.83) | 3.65 (1.32) | PHQ-9 (item 9) questionnaire, and additional suicidal intent question |
| Staehr 2006 [79] | Asylum seekers aged 15 and up | Hospitals and Red Cross asylum centres | 20% Iraqi, 15% Bosnian-Hercegovina, 14% Afghani, 6% Kosovon, 4% Iranian, 41% Other | ≥15 | Mixed | NR | ~1/3 of those with suicidal behaviour experienced imprisonment and torture/war, 4 reported rape, and 4 forced marriage | mean: 12.3 months | Asylum centre reports and hospital records |
| Steel 2004 [80] | 10 families from one ethnic group held for a protracted period | A remote detention facility | NR (all same ethnic group; 14 parents + their 20 children) | Ranges: parents 28–44; children 3–19 | F-64% (parents) | 71% Muslim | All adults reported traumatic experiences in their country of origin, with it being common for one parent to have been imprisoned and tortured for political reasons. All families reported fleeing their country of origin out of fear for the life of one or all of the family members. All families described traumatic experiences in detention. | mean: 2.3 (range: 2.0–2.7) | Structured Clinical Interview for DSM-IV Axis I Disorders; and Schedule for Affective Disorders and Schizophrenia for School-Age Children |
| Sultan 2001 [82] | Detained refugees in Sydney | Detention centre | Afghani, Iraqi, Iranian, former Yugoslavian, etc. | NR | M- 85% | NR | 58% had been physically tortured, 27% experienced the murder or disappearance of immediate family member | mean: 2.1 (minimum 9 months) | Semi-structured interview |
| Winkler 2019 [90] | Asylum seekers in Berlin | 9 refugee shelters | 37% Syrian, 15% Afghani, 9% Iraqi, 8% Albanian, 6% Iranian, 5% Moldovan | 30.6 (10.0) | M- 75% | NR | NR | 128 days (177) | Questionnaire |
| Mixed samples of refugees & asylum seekers: | |||||||||
| Bhui 2006 [26] | Somali refugees in the London Boroughs of Tower Hamlets and Lambeth (UK) | Primary care and community | All Somali | ≥18 years | M- 49% | NR | NR | NR | MINI Neuropsychiatric Interview |
| Leiler 2019 [52] | Adults in asylum accommodations in Jämtland-Härjedalen county | 13 asylum accommodations | 38% Afghani, 27% Syrian, etc. | 71% were <35 years | M- 72% | NR | NR | NR | PHQ-9 (item 9) |
| Sohn 2019 [77] | Refugees in various stages of the refugee approval process residing in Seoul and Gyeonggi province | Community | 51% Sub-Saharan African (Nigerian, Ethiopian, Liberian), 34% Middle Eastern (Yemeni, Egyptian), 8% Asian, etc. | 34% <30; 39% 31–40; 21% 41–50; 6% >51 | M- 72% | NR | NR | 38% <1; 41% 1–5; 21% >5 | Korean National Health and Nutrition Examination Survey |
| Tay 2019 [84] | Rohingya from Myanmar or the offspring of at least one Rohingya parent | 49 villages | All Rohingya | 28.3 (9.0) | M- 78% | NR | 81% tortured, 80% witnessed rape or sexual violence, 69% no food or water, 64% witnessed murder of friends or family, 62% no shelter, 61% witnessed mass killings or atrocities, 56% forced to flee home | 47 months (44) | Suicidal ideation was assessed using an item on the depression screen: “how often have you thought about taking your own life in the last two weeks?” |
| Internally displaced people: | |||||||||
| Kim 2007 [49] | Internally displaced persons in Nyala, South Darfur | 6 IDP camps | Sudanese | 34 | Mixed | 99% Muslim Sunni, 1% Christian | NR | mean 6.1 months (SE 0.1) | PHQ-9; and yes/no interview questions |
| Marroquín Rivera 2020 [54] | Adolescents displaced by armed conflict | Community | Colombian | range: 12–17 | F- 64% | NR | NR | NR | National Mental Health Survey |
| Salah 2013 [70] | Internally displaced persons in Khartoum and Gezira IDP areas in Central Sudan | Settlements for IDP | Sudanese | median: 35; range: 18 to 85 | M- 44% | NR | Moved due to war/ problem Khartoum: 8.1%; Gezira: 17.5% | Khartoum 18.6 (10.1); Gezira: 18.9 (10.3) | MINI International Neuropsychiatric Interview |
| Tamayo Martinez 2016 [83] | Adults internally displaced due to conflict | Community | Colombian | mean: 41.2 (95% CI: 39.7, 42.7) | F- 51% | NR | 61% exposed to traumatic events themselves or a close person | NR | National Mental Health Survey |
*Presented as Mean (SD) unless otherwise noted.
†Data were extracted and pooled for the Somali and Kurdish groups as these were reported to be majority refugees in the publication.
‡Westman 2006 study’s main countries of birth were, by region, Eastern European: Czechoslovakia, Estonia, Hungary, Romania, Soviet Union; Middle Eastern: Lebanon, Iran, Iraq, Syria, Turkey; Other non-European: Chile, Ethiopia, India, Somalia, Thailand. These regions were extracted since they were reported as mainly refugee countries in the publication.
Abbreviations: BDI = Beck Depression Inventory; F = female; M = male; NR = not reported; PHQ = Patient Health Questionnaire; pub = publication; y = years.
Suicide
Among the studies using general samples, 11 reported on suicide rates [20, 33, 37, 42, 49, 57, 62, 72, 73, 79, 89]. Suicide results, including a visual bar chart display and some characteristics are presented in Table 2. Six of these studies were in refugees granted asylum, one was in refugees living in a refugee camp, three were in asylum seekers, and one was in internally displaced people. Nine studies were conducted in high income level host countries (HIC; as per 2021 World Bank classification), while the study in a refugee camp was in Thailand (an upper middle-income country, UMIC) and the one study on internally displaced people was in Sudan (a low income country, LIC). The sample size of displaced people in these studies ranged from 4164 to 196,941.
Table 2. Suicide rates per 100,000 person-years in general samples, grouped by population type (and then by data source and by host country).
| Author, Pub. Year | Population Type | Host Country | Data Source | Study Dates | Suicides, n out of N | Suicide Rate, per 100,000 person-years* |
|---|---|---|---|---|---|---|
| (Income level) | ||||||
| Saunders 2017 [72] | Refugees granted asylum | Canada | Vital events registration | 1996–2012 | n = 27 | 4.2 |
| (HIC) | (NR) | |||||
| Saunders 2019 [73] | Refugees granted asylum | Canada | Vital events registration | 2003–2014 | 23 out of 58,082 | 6.1† |
| (HIC) | ||||||
| Norredam 2013 [62] | Refugees granted asylum | Denmark | Vital events registration | 1994–2007 | 29 out of 29,139 | 8‡ |
| (HIC) | ||||||
| Amin 2021 [20] | Refugees granted asylum | Sweden | Vital events registration | 2005–2013§ | 226 out of 196,941 | 13.2 |
| (HIC) | ||||||
| Hollander 2020 [42] | Refugees granted asylum | Sweden | Vital events registration | 1991–2015 | 51 out of 38,123 | 10‡ |
| (HIC) | ||||||
| Westman 2006a¶ [89] | Refugees granted asylum | Sweden | Vital events registration | 1994–1999 | 35 out of 21,534 | 25.5# |
| (HIC) | ||||||
| Westman 2006b¶ [89] | Refugees granted asylum | Sweden | Vital events registration | 1994–1999 | 59 out of 54,643 | 20.2# |
| (HIC) | ||||||
| Westman 2006c¶ [89] | Refugees granted asylum | Sweden | Vital events registration | 1994–1999 | 43 out of 34,484 | 21.4# |
| (HIC) | ||||||
| Westman 2006d¶ [89] | Refugees granted asylum | Sweden | Vital events registration | 1994–1999 | 27 out of 21,801 | 20.2# |
| (HIC) | ||||||
| Westman 2006e¶ [89] | Refugees granted asylum | Sweden | Vital events registration | 1994–1999 | 10 out of 34,940 | 4.1# |
| (HIC) | ||||||
| Westman 2006f¶ [89] | Refugees granted asylum | Sweden | Vital events registration | 1994–1999 | 21 out of 35,541 | 9.4# |
| (HIC) | ||||||
| Fellmeth 2016 [33] | Refugees in camps | Thailand | Retrospective cohort | unclear** | 4 out of 24,323 | 16 |
| (UMIC) | ||||||
| Goosen 2011a [37] | Asylum seekers | Netherlands | Vital events registration | 2002–2007 | n = 32 (NR) | 25.6 |
| (Males) | (HIC) | |||||
| Goosen 2011b [37] | Asylum seekers | Netherlands | Vital events registration | 2002–2007 | n = 3 (NR) | 4.0 |
| (Females) | (HIC) | |||||
| Staehr 2006 [79] | Asylum seekers | Denmark | Specific monitoring | 2003 | 1 out of 4164 | 24.0†† |
| (HIC) | ||||||
| Mittendorfer-Rutz 2020 [57] | Asylum seekers | Sweden | Cross-sectional | 2017 | 12 out of 23,425 | 51.2 |
| (HIC) | ||||||
| Kim 2007 [49] | Internally displaced | Sudan | Cross-sectional | 2005 | 21 out of 7194‡‡ | 290 |
| (LIC) |
*Crude suicide rate, as the number per 100,000 persons per year, was reported unless otherwise marked.
†Saunders 2019 study: 95% CI 3.9, 9.2.
‡Rate estimated from estimated follow-up time (i.e., 12 years median in Norredam 2013, and 13 years in Hollander 2020 studies).
§The 9-year cohort was extracted for the Amin 2021 study.
¶Westman 2006 study’s adjusted results were disaggregated, for gender and birth region, as follows: (a) Eastern European males, (b) Middle Eastern males, (c) Other non-European males, (d) Eastern European females, (e) Middle Eastern females, (f) Other non-European females.
#Age-adjusted rate.
**Unclear whether it was 1998–2005 or 1998–2015.
††Staehr 2006 study data were extracted for the most recent year reported (i.e., 2003).
‡‡Denominator estimated using average reported study household size.
Abbreviations: HIC = high income country; LIC = low income country; NR = not reported; pub = publication; UMIC = upper middle income country.
All six studies in refugees granted asylum and one of the studies on asylum seekers used vital events registration as the data source. The other studies on asylum seekers used specific monitoring data as the data source or a cross-sectional study design. The study in a refugee camp was a retrospective cohort, and the one on internally displaced people used a cross-sectional study design.
Suicide rates ranged considerably from 4.0 to 290 per 100,000 person-years across the 11 studies in general samples (Table 2). In refugees granted asylum, suicide rates ranged from 4.1 to 25.5 per 100,000 person-years, while in asylum seekers suicide rates ranged from 4.0 to 51.2 per 100,000 person-years. The study in a refugee camp found a suicide rate of 16 per 100,000 person-years, while the study on internally displaced people (in Sudan, a LIC) had the highest suicide rate of 290 per 100,000 person-years.
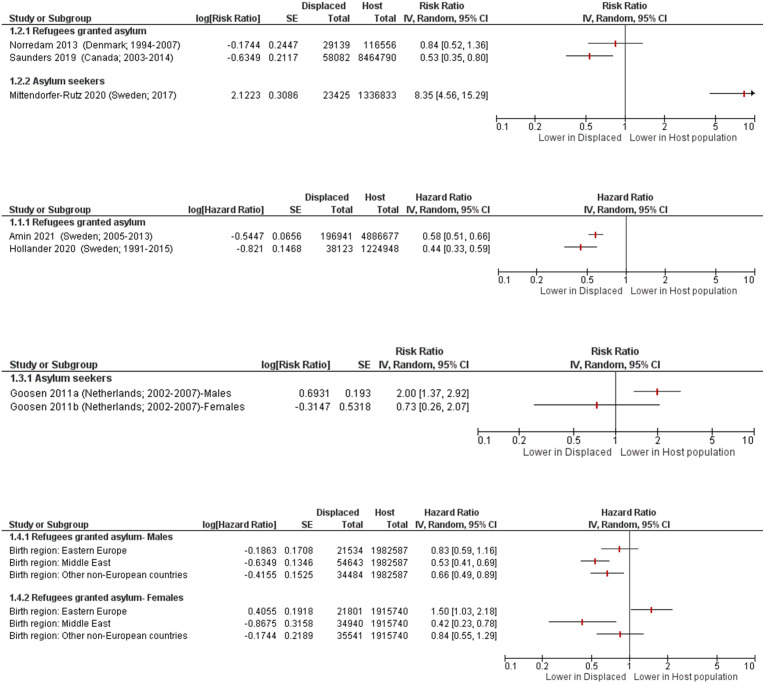
Only eight studies with general samples also compared suicide rates in displaced people to the host population, including five studies in refugees granted asylum and three conducted in asylum seekers. Seven studies [20, 37, 42, 57, 62, 72, 89] reported data in formats that could be presented visually in forest plots, which were grouped by outcome measure and then sub-grouped by population type (Fig 2).
Fig 2. Suicide in displaced people compared to host country population.
Norredam 2013 [62] adjusted for age and income; Amin 2021 [20] adjusted for socio-demographic, labour market marginalisation and morbidity factors (i.e. sex, age, educational level, family situation and type of residential area, days with full-time unemployment, net days with sickness absence, granted disability pension, history of suicide attempt; history of inpatient or specialised outpatient healthcare); Hollander 2020 [42] adjusted for attained age, gender, and disposable income; Goosen 2011 [37] standardised for age; Westman 2006 [89] adjusted for age, marital status, socioeconomic status, and hospitalization for psychiatric disorders or substance abuse; Saunders 2019 [73] and Mittendorfer-Rutz 2020 [57] were unadjusted.
Among the studies in refugees granted asylum, there was evidence of a lower risk of suicide compared with the host population in four studies [20, 42, 62, 72]. The final study on refugees granted asylum [89] reported lower, higher, and inconclusive risk compared with the host population depending on gender of the refugees and their birth region. In contrast, among the studies in asylum seekers there was evidence of a higher suicide risk compared with the host population in two studies [50, 57], including one study that reported age-standardised mortality ratios (SMR) of 2.8 [95% CI 1.5, 4.1] in males, and 1.5 [95% CI 0.0, 3.6] in females [50]. The third asylum seekers study was inconclusive about whether the risk was higher or lower, as it varied based on gender [37].
An additional study [31] on asylum seekers in detention in the UK estimated 211 suicides per 100,000, however, a rate estimate could not be calculated as total person-year was not reported.
Only two studies using specific samples were identified that reported on suicide rates; one study described forensic autopsies of deceased refugees [36], and the other study only reported on the proportion of suicides amongst causes of death in refugees [41] (S3 Table).
Suicide attempt
Among the studies using general samples, 15 [17, 18, 20, 30, 39, 47–49, 54, 55, 77, 79, 83, 85, 88] reported on the prevalence of suicide attempts (Table 3). The results are ordered by timeframe for the prevalence estimates and then sub-grouped by population type. Six of these studies were in refugees granted asylum, three were in refugees living in refugee camps, one was in mixed refugees & asylum seekers, two were in asylum seekers, and three were in internally displaced people. Ten studies were from high income countries, and the other five were conducted in India (a lower middle-income country, LMIC), Jordan (UMIC), Sudan (LIC), and two in Colombia (UMIC). The sample sizes of displaced people ranged from 53 to 196,941.
Table 3. Suicide attempt prevalence percentage in general samples, ordered by timeframe (and then by population type).
| Author, Pub. Year | Population Type | Host Country | Data Source | Study Dates | Suicide Attempts, n out of N | Time-frame* | Prevalence†, % |
|---|---|---|---|---|---|---|---|
| (Income level) | (95% CI)‡ | ||||||
| Amin 2021 [20] | Refugees granted asylum | Sweden | Prospective cohort | 2005–2013§ | 1607 out of 196,941 | 9 years | 0.82¶ |
| (HIC) | (0.78 to 0.86) | ||||||
| Vijayakumar 2017 [88] | Refugees in camps | India | Cross-sectional | NR | 11 out of 1755 | 15 months | 0.63# |
| (LMIC) | (0.31 to 1.1) | ||||||
| Tousignant 1999 [85] | Refugees granted asylum | Canada | Cross-sectional | NR | 7 out of 203 | 1 year | 3.5** |
| (HIC) | (1.4 to 7.0) | ||||||
| Choi 2020 [30]*** | Refugees granted asylum | South Korea | Cross-sectional | 2011–2018 | 13 out of 86 | 1 year | 15.1†† |
| (8.3 to 24.5) | |||||||
| Staehr 2006 [79] | Asylum seekers | Denmark | Specific monitoring | 2003 | 43 out of 4164 | 1 year | 1.0‡‡ |
| (HIC) | (0.75 to 1.4) | ||||||
| Sohn 2019 [77]*** | Mixed populations | South Korea | Cross-sectional | NR | 1 out of 129 | 1 year | 0.78§§ |
| (0.02 to 4.2) | |||||||
| Kim 2007 [49] | Internally displaced | Sudan | Cross-sectional | 2005 | 28 out of 1260 | 1 year | 2.2 |
| (LIC) | (1.5 to 3.2) | ||||||
| Keller 2003 [48] | Asylum seekers | USA | Cross-sectional | 2001–2002 | 2 out of 70 | 5 months¶¶ | 2.9 |
| (HIC) | (0.35 to 9.9) | ||||||
| Hermans 2017 [39] | Refugees in camps | Greece | Prospective cohort | 2016 | 4 out of 2291 | 6 weeks | 0.18## |
| (HIC) | (0.05 to 0.45) | ||||||
| Jankovic 2013 [47]*** | Refugees granted asylum | UK, Italy, Germany | Cross-sectional | 2005–2006 | 6 out of 854 | 1 month | 0.70 |
| (0.26 to 1.5) | |||||||
| Meyerhoff 2020 [55] | Refugees granted asylum | USA | Cross-sectional | NR | 4 out of 53 | 1 week | 7.6 |
| (HIC) | (2.1 to 18.2) | ||||||
| Alley 1982 [18] | Refugees granted asylum | USA | Cross-sectional | 1980 | 6 out of 4192 | NR | 0.14 |
| (HIC) | (0.05 to 0.31) | ||||||
| Al-Modallal 2012 [17] | Refugees in camps | Jordan | Cross-sectional | NR | 21 out of 287 | NR | 7.3 |
| (UMIC) | (4.6 to 11.0) | ||||||
| Tamayo Martinez 2016 [83] | Internally displaced | Colombia | National statistics | 2015 | N = 943 surveyed††† | NR | 5.5 |
| (UMIC) | (3.1 to 9.6) | ||||||
| Marroquín Rivera 2020 [54] | Internally displaced | Colombia | Cross-sectional | 2015 | 9 out of 99 | NR | 9.1 |
| (UMIC) | (4.2 to 16.6) |
*Timeframe refers to either how far back participants were asked about the occurrence of a suicide attempt (for example, in the past year), or the follow-up time.
†Prevalence rate per 100,000 person-years (i.e., the number per 100,000 persons per year) is also presented when it was either reported or it could be estimated from study follow-up time.
‡Confidence intervals (of prevalence percentages) were calculated using Stata 12.
§The 9-year cohort was extracted for the Amin 2021 study.
¶Amin 2021 study’s reported rate is 94.2 per 100,000 person-years.
#Vijayakumar 2017 study’s estimated rate is 500 per 100,000 person-years.
**Tousignant 1999 study’s estimated rate is 3450 per 100,000 person-years.
††Choi 2020 study’s estimated rate is 15,100 per 100,000 person-years.
‡‡Staehr 2006 study’s reported rate is 1032 per 100,000 person-years (for the most recent year reported, i.e., 2003).
§§Sohn 2019 study’s estimated rate is 775 per 100,000 person-years.
¶¶Median 5 months (range 1–54).
##Hermans 2017 study’s reported rate is 1400 per 100,000 person-years (95% CI, 30 to 2800).
***High income countries (HIC).
†††Absolute number of suicide attempts was not reported.
Abbreviations: A.S. = asylum seekers; HIC = high income country; LIC = low income country; LMIC = lower middle income country; NR = not reported; pub = publication; Ref. = refugees; UMIC = upper middle income country.
Two of the 15 studies had a prospective cohort design, one used specific monitoring data as the data source, one used national statistics, while 11 studies had a cross-sectional design. The prevalence timeframe of the studies (i.e. either how far back participants were asked about the occurrence of a suicide attempt or the follow-up time) ranged from 1 week to 9 years.
The prevalence of suicide attempts ranged from 0.14% to 15.1% across the studies in general samples (Table 3). In refugees granted asylum, the prevalence of suicide attempt ranged from 0.14% to 15.1%, and in the refugees living in camps it ranged from 0.18% to 7.3%. In the studies on asylum seekers the prevalence was 1.0% and 2.9%, and in internally displaced people it ranged from 2.2% to 9.1%. The study in mixed refugees & asylum seekers found a suicide attempt prevalence of 0.78%. The one study in a LIC (Sudan) did not find a higher prevalence than average.
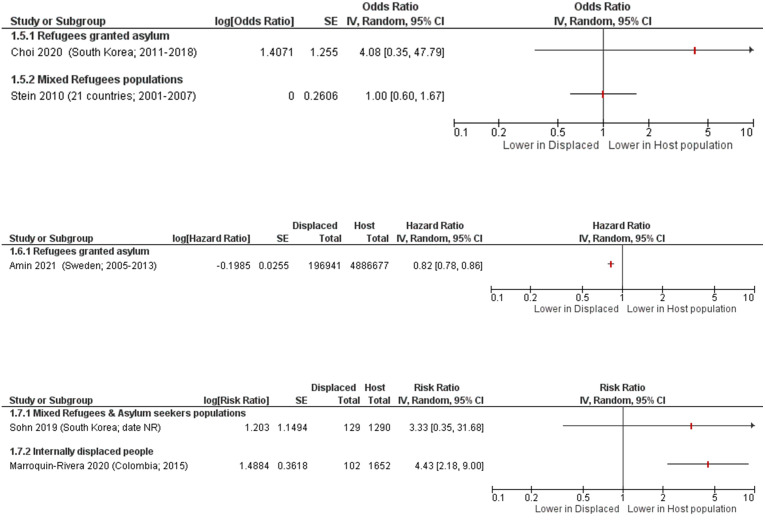
Six studies in general samples compared the prevalence of suicide attempts in displaced people to the host population. Only five of these studies [20, 30, 54, 77, 81] reported data in formats that could be presented visually in forest plots (Fig 3). Two of these studies were in refugees granted asylum, one was in mixed refugees & asylum seekers, one was in internally displaced people, and one was a pooled report of mixed refugee populations across 21 countries [81].
Fig 3. Suicide attempts in displaced people compared to host population forest plots, grouped by outcome measure and then sub-grouped by population type.
Choi 2020 [30] adjusted for interview year; Stein 2010 [81] adjusted for person-year, country, demographic factors (age, sex, time-varying education, time-varying marriage), interactions between life course and demographic variables, parent psychopathology, and childhood adversities; Amin 2021 [20] adjusted for socio-demographic, labour market marginalisation and morbidity factors (i.e. sex, age, educational level, family situation and type of residential area, days with full-time unemployment, net days with sickness absence, granted disability pension, history of suicide attempt; history of inpatient or specialised outpatient healthcare); Sohn 2019 [77] age- and gender-matched; Marroquin-Rivera 2020 [54] unadjusted.
In the two studies on refugees granted asylum, one reported a lower risk of suicide attempt than in the host population [20] while the other reported a higher risk [30]. The study of mixed refugee types [81] reported an odds ratio of 1.00 [95% CI 0.60, 1.67] indicating little to no difference between the refugees and the host populations. In one study [77] on mixed refugees & asylum seekers, they found a higher risk of suicide attempts. One study [54] on internally displaced people found a 4-fold greater risk of suicide attempt compared to the host population, RR 4.43 [95% CI 2.18, 9.00]. In addition, one study [79] found asylum seekers had a 3.4 times higher rate of suicide attempts compared to the host population (unadjusted).
One study [87] reported a composite outcome of self-harm or suicide. Refugees granted asylum were evaluated over a one-year timeframe and prevalence was reported as 0.10%, the rate was 101.2 per 100,000 person-years, and the comparative result was RR 0.80 [95% CI 0.58, 1.08] (unadjusted) for self-harm or suicide compared to the host population.
An additional three studies reported only a composite outcome of self-harm or suicide attempt. One [72] was conducted in refugees granted asylum, and the study timeframe ranged from 5–14 years. Prevalence was 0.68%, and the rate was 8.09 per 100,000 person-years [95% CI 7.31, 8.93]. The comparative result was found to be RR 0.85 [95% CI 0.77, 0.94] (unadjusted) for this composite outcome. In contrast, one of two studies [37] was conducted in asylum seekers, and the study timeframe was not reported. The rate was 119.2 per 100,000 person-years in males, and 188.2 per 100,000 person-years in females. Compared to the host population for self-harm or suicide attempt, asylum seekers had age-standardised RR 1.42 [95% CI 1.20, 1.66] in males, and RR 1.00 [95% CI 0.84, 1.18] in females. The other study [80] in asylum seekers assessed 10 detained families and found the prevalence of self-harm or suicide attempt was 29.4%.
Nine studies using specific samples of the target populations reported on suicide attempts (S4 Table).
Suicidal ideation
Among the studies with general samples, 37 [16–18, 21, 25, 30, 32, 35, 44, 45, 47–49, 52, 54, 55, 60, 61, 64, 66, 70, 71, 75, 77–80, 82–84, 86, 88, 90] reported on the prevalence of suicidal ideation (Table 4). The findings were ordered by prevalence timeframe and sub-grouped by population type. 11 studies were in refugees granted asylum, 11 were in refugees living in refugee camps, eight were in asylum seekers, three were in mixed refugees & asylum seekers, and four were in internally displaced people. 22 studies were from high income countries, and 15 were conducted in: India (LMIC), Lebanon (UMIC), Malaysia (UMIC), Nigeria (LMIC), Occupied Palestinian Territory (LMIC), Pakistan (LMIC), Syria (LIC), Thailand (UMIC), Uganda (LIC), and two each in Colombia (UMIC), Jordan (UMIC), and Sudan (LIC).
Table 4. Suicidal ideation prevalence percentage in general samples, ordered by timeframe (and then by population type).
| Author, Pub. Year | Population Type | Host Country * | Data Source | Study Dates | Suicidal Ideation, n out of N | Time-frame † | Prevalence ‡ , % |
| (Income level) | (95% CI) § | ||||||
| Park 2018 [64] | Refugees granted asylum | South Korea | Specific monitoring | 2017–2018 | 29 out of 174 | 1 year | 16.7¶ |
| (HIC) | (11.5 to 23.1) | ||||||
| Choi 2020 [30] | Refugees granted asylum | South Korea | Cross-sectional | 2011–2018 | 24 out of 86 | 1 year | 27.9# |
| (HIC) | (18.8 to 38.6) | ||||||
| Noh 2017 [61] | Refugees granted asylum | South Korea | Cross-sectional | 2008–2014 | 153 out of 656 | 1 year | 23.3** |
| (HIC) | (20.1 to 26.8) | ||||||
| Um 2020 [86] | Refugees granted asylum | South Korea | Cross-sectional | 2014 | 127 out of 405 | 1 year | 31.4†† |
| (HIC) | (26.9 to 36.1) | ||||||
| Ao 2016 [21] | Refugees granted asylum | USA | Cross-sectional | 2008–2011 | 9 out of 423 | 1 year | 2.1‡‡ |
| (HIC) | (1.0 to 4.0) | ||||||
| Itani 2017a [45]¶¶¶ | Refugees in camps | Occupied Palestinian T. | National statistics | 2010 | 2257 out of 8526 | 1 year | 26.5§§ |
| (25.5 to 27.4) | |||||||
| Itani 2017b [45] | Refugees in camps | Jordan | Cross-sectional | 2010 | 404 out of 1495 | 1 year | 27.0§§ |
| (UMIC) | (24.8 to 29.4) | ||||||
| Itani 2017c [45] | Refugees in camps | Lebanon | Cross-sectional | 2010 | 431 out of 2168 | 1 year | 19.9§§ |
| (UMIC) | (18.2 to 21.6) | ||||||
| Itani 2017d [45] | Refugees in camps | Syria | Cross-sectional | 2010 | 567 out of 2114 | 1 year | 26.8§§ |
| (LIC) | (24.9 to 28.8) | ||||||
| Staehr 2006 [79] | Asylum seekers | Denmark | Specific monitoring | 2003 | 7 out of 4164 | 1 year | 0.17¶¶ |
| (HIC) | (0.07 to 0.35) | ||||||
| Sohn 2019 [77] | Mixed Ref. & A.S. populations | South Korea | Cross-sectional | NR | 4 out of 129 | 1 year | 3.1## |
| (HIC) | (0.85 to 7.8) | ||||||
| Kim 2007 [49] | Internally displaced | Sudan | Cross-sectional | 2005 | 66 out of 1257 | 1 year | 5.3*** |
| (LIC) | (4.1 to 6.6) | ||||||
| Keller 2003 [48] | Asylum seekers | USA | Cross-sectional | 2001–2002 | 18 out of 70 | 5 months††† | 25.7 |
| (HIC) | (16.0 to 37.6) | ||||||
| Jankovic 2013 [47] | Refugees granted asylum | UK, Italy, Germany (HIC) | Cross-sectional | 2005–2006 | 81 out of 854 | 1 month | 9.5 |
| (7.6 to 11.7) | |||||||
| Akinyemi 2012 [16] | Refugees in camps | Nigeria | Cross-sectional | 2010 | 49 out of 444 | 1 month | 11.0 |
| (LMIC) | (8.3 to 14.3) | ||||||
| Rahman 2003 [66] | Refugees in camps | Pakistan | Cross-sectional | 2002 | 96 out of 297 | 1 month | 32.3 |
| (LMIC) | (27.0 to 38.0) | ||||||
| Falb 2013 [32] | Refugees in camps | Thailand | Cross-sectional | 2008 | 63 out of 848 | 1 month | 7.4 |
| (UMIC) | (5.8 to 9.4) | ||||||
| Nickerson 2019a [60] | Refugees granted asylum | Australia | Cross-sectional | 2015–2018 | 12 out of 826 | 2 weeks | 1.5 |
| (HIC) | (0.75 to 2.5) | ||||||
| Vijayakumar 2017 [88] | Refugees in camps | India | Cross-sectional | NR | 16 out of 1303 | 2 weeks | 1.2 |
| (LMIC) | (0.70 to 2.0) | ||||||
| Nickerson 2019b [60] | Asylum seekers | Australia | Cross-sectional | 2015–2018 | 21 out of 259 | 2 weeks | 8.1 |
| (HIC) | (5.1 to 12.1) | ||||||
| Leiler 2019 [52] | Mixed Ref. & A.S. populations | Sweden | Cross-sectional | 2016–2017 | 173 out of 510 | 2 weeks | 33.9 |
| (HIC) | (29.8 to 38.2) | ||||||
| Salama 2020 [71] | Refugees granted asylum | Finland | Cross-sectional | 2010–2012 | 80 out of 850 | 1 week | 9.4 |
| (HIC) | (7.5 to 11.6) | ||||||
| Meyerhoff 2020 [55] | Refugees granted asylum | USA | Cross-sectional | NR | 4 out of 60 | 1 week | 6.7 |
| (HIC) | (1.9 to 16.2) | ||||||
| Fuhrer 2016 [35] | Asylum seekers | Germany | Cross-sectional | 2015 | 12 out of 214 | 1 week | 5.6 |
| (HIC) | (2.9 to 9.6) | ||||||
| Huemer 2011 [44] | Asylum seekers | Austria | Cross-sectional | NR | 4 out of 41 | current state | 9.8 |
| (HIC) | (2.7 to 23.1) | ||||||
| Steel 2004 [80] | Asylum seekers | Australia | Cross-sectional | 2002–2003 | 24 out of 34 | current state | 70.6 |
| (HIC) | (52.5 to 84.9) | ||||||
| Sultan 2001 [82] | Asylum seekers | Australia | Cross-sectional | 2001 | 23 out of 33 | current state | 69.7 |
| (HIC) | (51.3 to 84.4) | ||||||
| Bhui 2003 [25] | Refugees granted asylum | UK | Cross-sectional | NR | 62 out of 177 | NR | 35.0 |
| (HIC) | (28.0 to 42.5) | ||||||
| Alley 1982 [18] | Refugees granted asylum | USA | Cross-sectional | 1980 | 10 out of 4192 | NR | 0.24 |
| (HIC) | (0.12 to 0.44) | ||||||
| Al-Modallal 2012 [17] | Refugees in camps | Jordan | Cross-sectional | NR | 39 out of 287 | NR | 13.6 |
| (UMIC) | (9.9 to 18.1) | ||||||
| Slodnjak 2002 [75] | Refugees in camps | Slovenia | Cross-sectional | 1994 | 64 out of 265 | NR | 24.1 |
| (HIC) | (19.1 to 29.8) | ||||||
| Author, Pub. Year | Population Type | Host Country * | Data Source | Study Dates | Suicidal Ideation, n/N | Time-frame * | Prevalence † , % |
| (Income level) | (95% CI) ‡ | ||||||
| Ssenyonga 2012 [78] | Refugees in camps | Uganda | Cross-sectional | NR | 89 out of 426 | NR | 20.9 |
| (LIC) | (17.1 to 25.1) | ||||||
| Winkler 2018 [90] | Asylum seekers | Germany | Cross-sectional | 2015–2016 | 87 out of 496 | NR | 17.5 |
| (HIC) | (14.3 to 21.2) | ||||||
| Tay 2019 [84] | Mixed Ref. & A.S. populations | Malaysia | Cross-sectional | NR | 228 out of 959 | NR | 23.8 |
| (UMIC) | (21.1 to 26.6) | ||||||
| Tamayo Martinez 2016 [83] | Internally displaced | Colombia | National statistics | 2015 | N = 943 surveyed§§§ | NR | 12.5 |
| (UMIC) | (9.0 to 17.1) | ||||||
| Marroquín Rivera 2020 [54] | Internally displaced | Colombia | Cross-sectional | 2015 | 20 out of 101 | NR | 19.8 |
| (UMIC) | (12.5 to 28.9) | ||||||
| Salah 2013 [70] | Internally displaced | Sudan | Cross-sectional | 2008 | 9 out of 1876 | NR | 0.48 |
| (LIC) | (0.22 to 0.91) |
*Refers to Country or Territory as applicable.
†Timeframe refers to either how far back participants were asked about the occurrence of suicidal ideation (for example, in the past year), or the follow-up time.
‡Prevalence rate per 100,000 person-years (i.e., the number per 100,000 persons per year) is also presented when it was either reported or it could be estimated from study follow-up time.
§Confidence intervals (of prevalence percentages) were calculated using Stata 12.
¶Park 2018 study’s estimated rate is 16,700 per 100,000 person-years.
#Choi 2020 study’s estimated rate is 27,900 per 100,000 person-years.
**Noh 2017 study’s estimated rate is 23,300 per 100,000 person-years.
††Um 2020 study’s estimated rate is 31,400 per 100,000 person-years.
‡‡Ao 2016 study’s estimated rate is 2100 per 100,000 person-years.
§§Itani 2017a, 2017b, 2017c, and 2017d studies’ estimated rates are, per 100,000 person-years: 26,500, 27,000, 19,900, and 26,800 (respectively).
¶¶Staehr 2006 study’s reported rate is 168 per 100,000 person-years (for the most recent year reported, i.e., 2003).
##Sohn 2019 study’s estimated rate is 3100 per 100,000 person-years.
***Kim 2007 study’s estimated rate is 5300 per 100,000 person-years.
†††Median was 5, range 1–54 months.
§§§Absolute number having suicidal ideation was not reported.
¶¶¶Lower middle income (as per World Bank classification, 2021).
Abbreviations: A.S. = asylum seekers; HIC = high income country; LIC = low income country; LMIC = lower middle income country; NR = not reported; pub = publication; Ref. = refugees; T. = Territory; UMIC = upper middle income country.
Two of the 37 studies used specific monitoring data as the data source, two used national statistics, and 33 had a cross-sectional design. The timeframe of the evaluation ranged from the ‘current state’ to 1 year. Sample sizes of displaced people ranged from 33 to 8526.
Prevalence of suicidal ideation ranged from 0.17% to 70.6% across the studies in general samples (Table 4). In refugees granted asylum, the prevalence of suicidal ideation ranged from 0.24% to 35.0%, and in refugees living in camps it ranged from 1.2% to 32.3%. In asylum seekers the prevalence ranged from 0.17% to 70.6%, and in internally displaced people from 0.48% to 19.8%. The mixed refugees & asylum seekers studies reported prevalences of 3.1%, 23.8% and 33.9%. There was not a pattern of generally higher prevalence in low income countries across the 4 LIC studies.
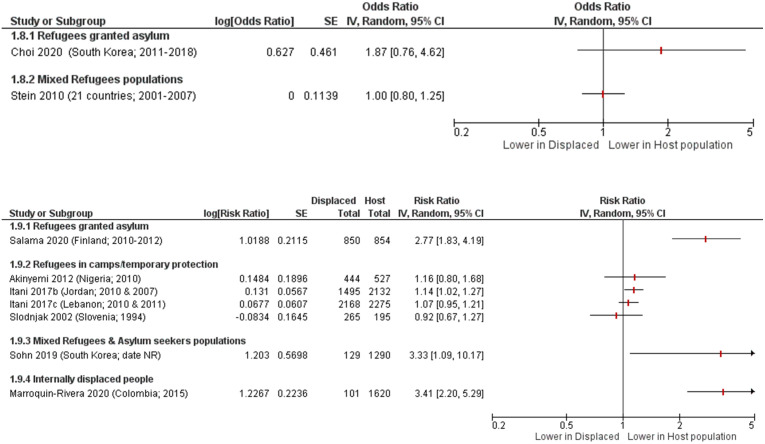
Only nine studies [16, 30, 45, 54, 71, 75, 77, 81] in general samples compared suicidal ideation in displaced people to the host population as displayed in Fig 4. Two of these studies were in refugees granted asylum, four were in refugees living in refugee camps with only temporary protection, one was in mixed refugees & asylum seekers, one was in internally displaced people, and one was a pooled report of mixed refugees across 21 countries [81].
Fig 4. Suicidal ideation in displaced people compared to host population forest plots, grouped by outcome measure and then by population type.
Choi 2020 [30] adjusted for interview year; Stein 2010 [81] adjusted for person-year, country, demographic factors (age, sex, time-varying education, time-varying marriage), interactions between life course and demographic variables, parent psychopathology, and childhood adversities; Sohn 2019 [77] age- and gender-matched; Akinyemi 2012 [16], Itani 2017 [45], Slodnjak 2002 [75], Marroquin-Rivera 2020 [54], and Salama 2020 [71] were unadjusted.
Among refugees living in refugee camps, there was evidence of a higher risk of suicidal ideation compared with the host population from three studies [16, 45], while one study reported a lower risk [75]. There was evidence of a higher risk of suicidal ideation among refugees granted asylum in two studies [30, 71]. Individual studies reported higher risk of suicidal ideation in mixed refugee and asylum seeker populations [77], and internally displaced people [54]. The report [81] of mixed refugees across 21 countries reported little to no difference in risk of suicidal ideation compared with the host population (OR 1.00 [95% CI 0.80, 1.25]).
An additional two studies in general samples reported a composite outcome of suicidal ideation or suicide attempt. One study [26] evaluated mixed refugees & asylum seekers, and the study timeframe was 1 month. Prevalence was 9.1% [95% CI 4.9, 15] for suicidal ideation or suicide attempt. The other [29] was conducted in asylum seekers, and the prevalence was 55.6% for this composite outcome. This study’s timeframe was not reported.
Three studies only reported continuous outcome data on suicidal ideation. One [76] was conducted in refugees granted asylum but the study’s timeframe was not reported. Mean score using the Suicidal Ideation Scale was 20.34 (SD 7.39). A study [91] in refugees with only temporary protection reported mean scores using the Personality Assessment Index’s Suicide Ideation subscale were 49.5 (SD 10.9) in males and 53.8 (SD 17.0) in females (timeframe was not reported). The other [38] assessed asylum seekers, and the timeframe was 2 weeks. Mean score using the PHQ-9 symptom severity Item 9 for suicidal ideation was 0.98 (SD 1.11).
Sixteen studies using specific samples reported on suicidal ideation (S5 Table).
Discussion
This systematic review identified 77 studies that reported on suicide, suicide attempts, or suicidal ideation in displaced people. Estimates of suicide rates from the studies which are more representative of refugee and asylum seeker populations (i.e. general samples) ranged widely and appeared to differ based on the source of the data and the population subgroup being assessed. Estimates of the prevalence of suicide attempts or suicidal ideation also ranged widely and were inconsistently reported across studies, making comparisons across groups challenging.
While numerous studies have been published on this topic, the evidence base is still sparse for the differing contexts of refugees in refugee camps, asylum seekers, and internally displaced people. Additionally, fewer than half of the studies reported on suicides or suicide attempts and almost one third of the studies were not representative samples of the target population. This systematic review has provided an overview of the populations, contexts, and study designs that have been used for research on suicide and suicidal behaviours in these populations, but further research is warranted to fill the gaps in knowledge around these specific populations.
The heterogeneity in study populations, designs, analytical approaches, and results mean that it is not possible to draw firm conclusions on the comparative rate of suicide in refugees and host populations. The results from different studies are inconclusive, with several studies suggesting that rates of suicide may be lower in refugees granted asylum than in the host populations [20, 42, 72, 89]. These results should be interpreted with caution because the variability of the available data may be due to effect estimates being mediated by a range of mechanisms. These factors might include the local context (such as rates or prevalence of suicidal behaviour in the host population, as well as possible confounders such as poverty and deprivation), as well as possible mechanisms of action, such as the extent of physical injury, loss of housing, financial distress, and the level of social support that is provided. The length of stay in a host country has also been suggested as a potential mediator, with refugees having a lower risk once they have lived in a host country for longer than 10 years [42].
The strengths of this systematic review included developing a sensitive search strategy and screening all results in duplicate, as well as careful evaluation and reporting of the data according to study design and population. However, there are some limitations to this review, particularly around the sparse international evidence base which prevents us from drawing firm conclusions. The wide variety of study designs and approaches to reporting risks prevented meta-analysis of the results. This variety in study designs also means that we were only able to do a relatively high-level assessment of methodological quality based on the source of data for the studies included in this review. Further data on mediators or risk factors for suicidal behaviour in these populations could add to the evidence base and strengthen the development of prevention or management interventions. In addition, there is potential for overlap in the five population subgroups used in this review. It is often difficult to distinguish which of these subgroups a study population belongs to without access to further population characteristics from the primary studies.
Despite the sparsity of studies, there is evidence of a high risk of suicide and suicidal behaviour among refugees in camps and asylum seekers, which suggests that these groups require additional support and monitoring. Strengthening the evidence base around the risk of suicidal behaviour in these vulnerable groups is needed to further develop understanding of the factors that influence them. Many factors have been suggested to influence the risk of suicide and suicidal ideation in these populations, including a combination of socioeconomic disadvantage [93], exposure to potentially traumatic events [103], increased depression and anxiety [104], or a lack of appropriate and accessible care [39, 105]. Improvements in understanding the suicide risk in these populations can be made by better routine data collection to enable consistent surveillance across countries. Countries hosting people affected by conflict, including refugees and asylum seekers, should ensure that these groups are identifiable in routine data [12, 104]. Agreed methods for analysing and presenting data would support comparisons between exposed populations in different countries and settings and would aid in quantitative synthesis of the risk of suicidal behaviours.
Finally, a better understanding of mediating factors may also help to inform policy responses and potential interventions for refugees or displaced people. A recent review found only a limited number of suicide prevention or response programs were implemented for refugee or displaced populations [4]. The review recommended programs that were multi-tiered, focussing on multiple levels of suicide prevention. A comprehensive approach to suicide prevention should include adequate surveillance, identify risk and protective factors, and ensure evaluation of programs following implementation. Studies on prevalence are well placed to identify risk and protective factors that might explain some of the variability across populations and contexts. For example, studies should consider including measures of local context as well as potential mediators such as experience of physical injury, loss of housing, financial hardship, levels of social support, legal context, and access to mental health services [106, 107].
Given the high risk of suicide in refugees in camps and asylum seekers, host countries should increase efforts to prevent suicide in asylum seekers, with actions that may span from speeding up asylum processes and improving social conditions of asylum seekers to offering better mental health prevention and management interventions. Given that prevalence of mental disorders is high in displaced people and that that these conditions appear associated with suicide attempts, there is a need to invest in prevention and care of mental disorders in this vulnerable group.
Supporting information
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Acknowledgments
The authors would like to acknowledge Alexandra Fleischmann, Mark van Ommeren and the WHO advisory group (Corrado Barbui, Fiona Charlson, Pim Cuijpers, David Gunnell, GJ Melendez-Torres, Wietse Tol, and Pieter Ventevogel) for advice on the protocol and review of the WHO-commissioned background paper.
The authors would also like to acknowledge additional members of the Cochrane Response team, Hanna Bergman, Jennifer Petkovic, Katrin Probyn, and Yanina Sguassero, for their assistance in extracting and checking data.
Data Availability
All relevant data are within the manuscript and its Supporting information files.
Funding Statement
The initial scoping study that led to this review was supported by a WHO Agreement for Performance of Work from the WHO Global Service Centre (WHO Registration 2019/891502-0, PO 202208554). This publication was funded by the Research, Evidence and Development Initiative (READ-It). READ-It (project number 300342-104) through UK aid from the UK government; however, the views expressed do not necessarily reflect the UK government’s official policies. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.United Nations Office for the Coordination of Humanitarian Affairs (OCHA). Global Humanitarian Overview 2022. New York: OCHA; 2021. https://gho.unocha.org/trends/forced-displacement-record-levels-covid-19-hampers-durable-solutions
- 2.United Nations High Commissioner for Refugees (UNHCR). Global Trends Forced Displacement in 2020. UNHCR; 2021. https://www.unhcr.org/60b638e37/unhcr-global-trends-2020
- 3.Spiegel PB, Checchi F, Colombo S, Paik E. Health-care needs of people affected by conflict: future trends and changing frameworks. The Lancet. 2010;375(9711):341–5. doi: 10.1016/S0140-6736(09)61873-0 [DOI] [PubMed] [Google Scholar]
- 4.Haroz EE, Decker, E., Lee, C. Evidence for suicide prevention and response programs with refugees: a systematic review and recommendations. Geneva: United Nations High Commissioner for Refugees (UNHCR); 2018. https://www.unhcr.org/5e15d3d84.pdf
- 5.World Health Organization. World health statistics 2021: monitoring health for the SDGs, sustainable development goals. Geneva: World Health Organization; 2021. [Google Scholar]
- 6.World Health Organization. Suicide in the world: Global health estimates. Geneva: World Health Organization; 2019. [Google Scholar]
- 7.United Nations General Assembly. Transforming our world: the 2030 Agenda for Sustainable Development: UN General Assembly; 2015. https://www.refworld.org/docid/57b6e3e44.html
- 8.Vijayakumar L, Jotheeswaran A. Suicide in refugees and asylum seekers. Mental health of refugees and asylum seekers. 2010:195–210. [Google Scholar]
- 9.Charlson F, van Ommeren M, Flaxman A, Cornett J, Whiteford H, Saxena S. New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. The Lancet. 2019. doi: 10.1016/S0140-6736(19)30934-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carta MG, Bernal M, Hardoy MC, Haro-Abad JM, Report on the Mental Health in Europe Working G. Migration and mental health in Europe (the state of the mental health in Europe working group: appendix 1). Clin Pract Epidemiol Ment Health. 2005;1:13. doi: 10.1186/1745-0179-1-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. Suicide in the world: Global health estimates. Geneva; 2019. [Google Scholar]
- 12.Vijayakumar L. Suicide Among Refugees—A Mockery of Humanity. Crisis. 2016;37(1):1–4. doi: 10.1027/0227-5910/a000385 [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization. Preventing Suicide: a global imperative. Geneva: World Health Organization; 2014. [Google Scholar]
- 14.McKenzie JE, Brennan SE. Synthesizing and presenting findings using other methods. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al., editors. Cochrane handbook for systematic reviews of interventions. Version 62 (updated February 2021). London, UK: Cochrane; 2021. pp. 321–47. [Google Scholar]
- 15.Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368. doi: 10.1136/bmj.l6890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akinyemi OO, Owoaje ET, Ige OK, Popoola OA. Comparative study of mental health and quality of life in long term refugees and host populations in Oru-Ijebu, Southwest Nigeria. BMC research notes. 2012;5(1):1–9. doi: 10.1186/1756-0500-5-394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al-Modallal H. Patterns of coping with partner violence: Experiences of refugee women in Jordan. Public Health Nursing. 2012;29(5):403–11. doi: 10.1111/j.1525-1446.2012.01018.x [DOI] [PubMed] [Google Scholar]
- 18.Alley JC. Life-threatening indicators among the Indochinese refugees. Suicide & life-threatening behavior. 1982;12(1):46–51. doi: 10.1111/j.1943-278x.1982.tb01092.x [DOI] [PubMed] [Google Scholar]
- 19.Allodi F, Cowgill G. Ethical and psychiatric aspects of torture: A Canadian study. The Canadian Journal of Psychiatry / La Revue canadienne de psychiatrie. 1982;27(2):98–102. doi: 10.1177/070674378202700203 [DOI] [PubMed] [Google Scholar]
- 20.Amin R, Helgesson M, Runeson B, Tinghög P, Mehlum L, Qin P, et al. Suicide attempt and suicide in refugees in Sweden–a nationwide population-based cohort study. Psychological medicine. 2021;51(2):254–63. doi: 10.1017/S0033291719003167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ao T, Shetty S, Sivilli T, Blanton C, Ellis H, Geltman PL, et al. Suicidal ideation and mental health of Bhutanese refugees in the United States. Journal of immigrant and minority health. 2016;18(4):828–35. doi: 10.1007/s10903-015-0325-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aronsson B, Wiberg C, Sandstedt P, Hjern A. Asylum-seeking children with severe loss of activities of daily living: clinical signs and course during rehabilitation. Acta paediatrica (Oslo, Norway: 1992). 2009;98(12):1977–81. doi: 10.1111/j.1651-2227.2009.01499.x [DOI] [PubMed] [Google Scholar]
- 23.Belz M, Belz M, Özkan I, Graef-Calliess IT. Posttraumatic stress disorder and comorbid depression among refugees: assessment of a sample from a German refugee reception center. Transcultural Psychiatry. 2017;54(5–6):595–610. doi: 10.1177/1363461517745473 [DOI] [PubMed] [Google Scholar]
- 24.Betancourt TS, Newnham EA, Birman D, Lee R, Ellis BH, Layne CM. Comparing trauma exposure, mental health needs, and service utilization across clinical samples of refugee, immigrant, and US-origin children. Journal of traumatic stress. 2017;30(3):209–18. doi: 10.1002/jts.22186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bhui K, Abdi A, Abdi M, Pereira S, Dualeh M, Robertson D, et al. Traumatic events, migration characteristics and psychiatric symptoms among Somali refugees—preliminary communication. Social psychiatry and psychiatric epidemiology. 2003;38(1):35–43. doi: 10.1007/s00127-003-0596-5 [DOI] [PubMed] [Google Scholar]
- 26.Bhui K, Craig T, Mohamud S, Warfa N, Stansfeld SA, Thornicroft G, et al. Mental disorders among Somali refugees: developing culturally appropriate measures and assessing socio-cultural risk factors. Social psychiatry and psychiatric epidemiology. 2006;41(5):400–8. doi: 10.1007/s00127-006-0043-5 [DOI] [PubMed] [Google Scholar]
- 27.Bolton P, Lee C, Haroz EE, Murray L, Dorsey S, Robinson C, et al. A Transdiagnostic Community-Based Mental Health Treatment for Comorbid Disorders: Development and Outcomes of a Randomized Controlled Trial among Burmese Refugees in Thailand. PLoS Medicine. 2014;11(11). doi: 10.1371/journal.pmed.1001757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brown AD, Müller M, Hirschi T, Henssler JF, Rönz K, Exadaktylos AK, et al. Acute and mixed alcohol intoxications in asylum seekers presenting to an urban emergency department in Switzerland. BMC public health. 2019;19(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cheney MK, Gowin MJ, Taylor EL, Frey M, Dunnington J, Alshuwaiyer G, et al. Living outside the gender box in Mexico: testimony of transgender Mexican asylum seekers. American journal of public health. 2017;107(10):1646–52. doi: 10.2105/AJPH.2017.303961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Choi S, Kim K. We Don’t Belong Here: Adolescents of North Korean Refugee Families and Their Suicidal Behaviors. International Migration. 2020;58(6):232–46. [Google Scholar]
- 31.Cohen J. Safe in our hands?: a study of suicide and self-harm in asylum seekers. Journal of forensic and legal medicine. 2008;15(4):235–44. doi: 10.1016/j.jflm.2007.11.001 [DOI] [PubMed] [Google Scholar]
- 32.Falb KL, McCormick MC, Hemenway D, Anfinson K, Silverman JG. Suicide ideation and victimization among refugee women along the Thai-Burma border. Journal of traumatic stress. 2013;26(5):631–5. doi: 10.1002/jts.21846 [DOI] [PubMed] [Google Scholar]
- 33.Fellmeth G, Paw MK, Wiladphaingern J, Charunwatthana P, Nosten FH, McGready R. Maternal suicide risk among refugees and migrants. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics. 2016;134(2):223–4. doi: 10.1016/j.ijgo.2016.02.011 [DOI] [PubMed] [Google Scholar]
- 34.Ferrada-Noli M, Sundbom E. Cultural bias in suicidal behaviour among refugees with post-traumatic stress disorder. Nordic Journal of Psychiatry. 1996;50(3):185–91. [Google Scholar]
- 35.Fuhrer A, Eichner F, Stang A. Morbidity of asylum seekers in a medium-sized German city. European journal of epidemiology. 2016;31(7):703–6. doi: 10.1007/s10654-016-0148-4 [DOI] [PubMed] [Google Scholar]
- 36.Gleich S, Domingo O, Ackermann N, Schwerer M, Graw M, Schöpfer J. A post-mortem study of the cause of death and concomitant diseases of refugees in Munich (2014–2015). Rechtsmedizin. 2018;28(1):25–32. [Google Scholar]
- 37.Goosen S, Kunst AE, Stronks K, van Oostrum IE, Uitenbroek DG, Kerkhof AJ. Suicide death and hospital-treated suicidal behaviour in asylum seekers in the Netherlands: a national registry-based study. BMC public health. 2011;11:484. doi: 10.1186/1471-2458-11-484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grupp F, Piskernik B, Mewes R. Is depression comparable between asylum seekers and native Germans? An investigation of measurement invariance of the PHQ-9. J Affect Disord. 2020;262:451–8. doi: 10.1016/j.jad.2019.11.055 [DOI] [PubMed] [Google Scholar]
- 39.Hermans MPJ, Kooistra J, Cannegieter SC, Rosendaal FR, Mook-Kanamori DO, Nemeth B. Healthcare and disease burden among refugees in long-stay refugee camps at Lesbos, Greece. European journal of epidemiology. 2017;32(9):851–4. doi: 10.1007/s10654-017-0269-4 [DOI] [PubMed] [Google Scholar]
- 40.Hocking D, Sundram S. Demoralisation syndrome does not explain the psychological profile of community-based asylum-seekers. Comprehensive Psychiatry. 2015;63:55–64. doi: 10.1016/j.comppsych.2015.08.008 [DOI] [PubMed] [Google Scholar]
- 41.Hollander A-C. Social inequalities in mental health and mortality among refugees and other immigrants to Sweden–epidemiological studies of register data. Global health action. 2013;6(1):21059. doi: 10.3402/gha.v6i0.21059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hollander A-C, Pitman A, Sjöqvist H, Lewis G, Magnusson C, Kirkbride JB, et al. Suicide risk among refugees compared with non-refugee migrants and the Swedish-born majority population. The British Journal of Psychiatry. 2020;217(6):686–92. doi: 10.1192/bjp.2019.220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hougen HP. Physical and psychological sequelae to torture. A controlled clinical study of exiled asylum applicants. Forensic science international. 1988;39(1):5–11. doi: 10.1016/0379-0738(88)90113-2 [DOI] [PubMed] [Google Scholar]
- 44.Huemer J, Karnik N, Voelkl-Kernstock S, Granditsch E, Plattner B, Friedrich M, et al. Psychopathology in African unaccompanied refugee minors in Austria. Child Psychiatry & Human Development. 2011;42(3):307–19. [DOI] [PubMed] [Google Scholar]
- 45.Itani T, Jacobsen KH, Kraemer A. Suicidal ideation and planning among Palestinian middle school students living in Gaza Strip, West Bank, and United Nations Relief and Works Agency (UNRWA) camps. International journal of pediatrics & adolescent medicine. 2017;4(2):54–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jahangir F, ur Rehman H, Jan T. Degree of religiosity and vulnerability to suicidal attempt/plans in depressive patients among Afghan refugees. The International Journal for the Psychology of Religion. 1998;8(4):265–9. [Google Scholar]
- 47.Jankovic J, Bremner S, Bogic M, Lecic-Tosevski D, Ajdukovic D, Franciskovic T, et al. Trauma and suicidality in war affected communities. European psychiatry: the journal of the Association of European Psychiatrists. 2013;28(8):514–20. doi: 10.1016/j.eurpsy.2012.06.001 [DOI] [PubMed] [Google Scholar]
- 48.Keller AS, Rosenfeld B, Trinh-Shevrin C, Meserve C, Sachs E, Leviss JA, et al. Mental health of detained asylum seekers. The Lancet. 2003;362(9397):1721–3. doi: 10.1016/S0140-6736(03)14846-5 [DOI] [PubMed] [Google Scholar]
- 49.Kim G, Torbay R, Lawry L. Basic health, women’s health, and mental health among internally displaced persons in Nyala Province, South Darfur, Sudan. American journal of public health. 2007;97(2):353–61. doi: 10.2105/AJPH.2005.073635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Koppenaal H, Bos CA, Broer J. [High mortality due to infectious diseases and unnatural causes of death among asylum seekers in the Netherlands, 1998–1999]. Nederlands tijdschrift voor geneeskunde. 2003;147(9):391–5. Dutch. [PubMed] [Google Scholar]
- 51.Lama S, Francois K, Marwan Z, Sami R. Impact of the Syrian Crisis on the Hospitalization of Syrians in a Psychiatric Setting. Community mental health journal. 2016;52(1):84–93. doi: 10.1007/s10597-015-9891-3 [DOI] [PubMed] [Google Scholar]
- 52.Leiler A, Hollifield M, Wasteson E, Bjärtå A. Suicidal ideation and severity of distress among refugees residing in asylum accommodations in Sweden. International journal of environmental research and public health. 2019;16(15):2751. doi: 10.3390/ijerph16152751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lerner E, Bonanno GA, Keatley E, Joscelyne A, Keller AS. Predictors of suicidal ideation in treatment-seeking survivors of torture. Psychological trauma: theory, research, practice and policy. 2016;8(1):17–24. doi: 10.1037/tra0000040 [DOI] [PubMed] [Google Scholar]
- 54.Marroquín Rivera A, Rincón Rodríguez CJ, Padilla-Muñoz A, Gómez-Restrepo C. Mental health in adolescents displaced by the armed conflict: findings from the Colombian national mental health survey. Child and adolescent psychiatry and mental health. 2020;14:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Meyerhoff J, Rohan KJ. The desire to be dead among Bhutanese refugees resettled in the United States: Assessing risk. American journal of orthopsychiatry. 2020;90(2):236. doi: 10.1037/ort0000429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mezey AG. Psychiatric Illness in Hungarian Refugees. Journal of Mental Science. 1960;106(443):628–37. [Google Scholar]
- 57.Mittendorfer-Rutz EH, A; Hollander A. High suicide rates among unaccompanied minors/youth seeking asylum in Sweden. Crisis. 2020;41(4):314–7. doi: 10.1027/0227-5910/a000636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Neuner F, Kurreck S, Ruf M, Odenwald M, Elbert T, Schauer M. Can asylum-seekers with posttraumatic stress disorder be successfully treated? A randomized controlled pilot study. Cognitive behaviour therapy. 2010;39(2):81–91. doi: 10.1080/16506070903121042 [DOI] [PubMed] [Google Scholar]
- 59.Nguyen SD. Mental health services for refugees and immigrants. Psychiatric Journal of the University of Ottawa. 1984;9(2):85–91. [PubMed] [Google Scholar]
- 60.Nickerson A, Byrow Y, O’Donnell M, Mau V, McMahon T, Pajak R, et al. The association between visa insecurity and mental health, disability and social engagement in refugees living in Australia. European journal of psychotraumatology. 2019;10(1):1688129. doi: 10.1080/20008198.2019.1688129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Noh JW, Park H, Kwon YD, Kim IH, Lee YH, Kim YJ, et al. Gender Differences in Suicidal Ideation and Related Factors among North Korean Refugees in South Korea. Psychiatry investigation. 2017;14(6):762–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Norredam M, Olsbjerg M, Petersen JH, Laursen B, Krasnik A. Are there differences in injury mortality among refugees and immigrants compared with native-born? Injury prevention: journal of the International Society for Child and Adolescent Injury Prevention. 2013;19(2):100–5. doi: 10.1136/injuryprev-2012-040336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Olema DK, Catani C, Ertl V, Saile R, Neuner F. The hidden effects of child maltreatment in a war region: correlates of psychopathology in two generations living in Northern Uganda. Journal of traumatic stress. 2014;27(1):35–41. doi: 10.1002/jts.21892 [DOI] [PubMed] [Google Scholar]
- 64.Park S, Rim SJ, Jun JY. Related Factors of Suicidal Ideation among North Korean Refugee Youth in South Korea. International journal of environmental research and public health. 2018;15(8). doi: 10.3390/ijerph15081694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Premand N, Baeriswyl-Cottin R, Gex-Fabry M, Hiller N, Framorando D, Eytan A, et al. Determinants of Suicidality and of Treatment Modalities in a Community Psychiatry Sample of Asylum Seekers. The Journal of nervous and mental disease. 2018;206(1):27–32. doi: 10.1097/NMD.0000000000000639 [DOI] [PubMed] [Google Scholar]
- 66.Rahman A, Hafeez A. Suicidal feelings run high among mothers in refugee camps: a cross-sectional survey. Acta psychiatrica Scandinavica. 2003;108(5):392–3. doi: 10.1034/j.1600-0447.2003.00220.x [DOI] [PubMed] [Google Scholar]
- 67.Ramel B, Taljemark J, Lindgren A, Johansson BA. Overrepresentation of unaccompanied refugee minors in inpatient psychiatric care. SpringerPlus. 2015;4:131. doi: 10.1186/s40064-015-0902-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Reko A, Bech P, Wohlert C, Noerregaard C, Csillag C. Usage of psychiatric emergency services by asylum seekers: Clinical implications based on a descriptive study in Denmark. Nord J Psychiatry. 2015;69(8):587–93. doi: 10.3109/08039488.2015.1019923 [DOI] [PubMed] [Google Scholar]
- 69.Richter K, Peter L, Lehfeld H, Zäske H, Brar-Reissinger S, Niklewski G. Prevalence of psychiatric diagnoses in asylum seekers with follow-up. BMC Psychiatry. 2018;18(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Salah TT, Abdelrahman A, Lien L, Eide AH, Martinez P, Hauff E. The mental health of internally displaced persons: an epidemiological study of adults in two settlements in Central Sudan. The International journal of social psychiatry. 2013;59(8):782–8. doi: 10.1177/0020764012456810 [DOI] [PubMed] [Google Scholar]
- 71.Salama E, Castaneda AE, Suvisaari J, Rask S, Laatikainen T, Niemelä S. Substance use, affective symptoms, and suicidal ideation among Russian, Somali, and Kurdish migrants in Finland. Transcultural psychiatry. 2020:1363461520906028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Saunders NR, Lebenbaum M, Stukel TA, Lu H, Urquia ML, Kurdyak P, et al. Suicide and self-harm trends in recent immigrant youth in Ontario, 1996–2012: a population-based longitudinal cohort study. BMJ open. 2017;7(9):e014863. doi: 10.1136/bmjopen-2016-014863 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Saunders NR, Chiu M, Lebenbaum M, Chen S, Kurdyak P, Guttmann A, et al. Suicide and self-harm in recent immigrants in Ontario, Canada: a population-based study. The Canadian Journal of Psychiatry. 2019;64(11):777–88. doi: 10.1177/0706743719856851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schoretsanitis G, Eisenhardt S, Ricklin ME, Srivastava DS, Walther S, Exadaktylos A. Psychiatric emergencies of asylum seekers; descriptive analysis and comparison with immigrants of warranted residence. International journal of environmental research and public health. 2018;15(7):1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Slodnjak V, Kos A, Yule W. Depression and parasuicide in refugee and Slovenian adolescents. Crisis. 2002;23(3):127–32. doi: 10.1027//0227-5910.23.3.127 [DOI] [PubMed] [Google Scholar]
- 76.Sobhanian F, Boyle GJ, Bahr M, Fallo T. Psychological status of former refugee detainees from the Woomera Detention Centre now living in the Australian community. Psychiatry, Psychology and Law. 2006;13(2):151–9. [Google Scholar]
- 77.Sohn JH, Lim J, Lee JS, Kim K, Lim S, Byeon N, et al. Prevalence of possible depression and post-traumatic stress disorder among community dwelling adult refugees and refugee applicants in South Korea. Journal of Korean medical science. 2019;34(11). doi: 10.3346/jkms.2019.34.e97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ssenyonga J, Kani D, Owens V. Posttraumatic stress disorder, suicide, domestic violence and social support among refugees. Int J Psychol. 2012;47:777-. [Google Scholar]
- 79.Staehr MA, Munk-Andersen E. [Suicide and suicidal behavior among asylum seekers in Denmark during the period 2001–2003. A retrospective study]. Ugeskrift for laeger. 2006;168(17):1650–3. Danish. [PubMed] [Google Scholar]
- 80.Steel Z, Momartin S, Bateman C, Hafshejani A, Silove DM, Everson N, et al. Psychiatric status of asylum seeker families held for a protracted period in a remote detention centre in Australia. Australian and New Zealand journal of public health. 2004;28(6):527–36. doi: 10.1111/j.1467-842x.2004.tb00042.x [DOI] [PubMed] [Google Scholar]
- 81.Stein DJ, Chiu WT, Hwang I, Kessler RC, Sampson N, Alonso J, et al. Cross-national analysis of the associations between traumatic events and suicidal behavior: Findings from the who world mental health surveys. PLoS ONE. 2010;5 (5) (no pagination)(e10574). doi: 10.1371/journal.pone.0010574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Sultan A, O’sullivan K. Psychological disturbances in asylum seekers held in long term detention: A participant–observer account. Medical Journal of Australia. 2001;175(11–12):593–6. doi: 10.5694/j.1326-5377.2001.tb143740.x [DOI] [PubMed] [Google Scholar]
- 83.Tamayo Martinez N, Rincon Rodriguez CJ, de Santacruz C, Bautista Bautista N, Collazos J, Gomez-Restrepo C. [Mental Problems, Mood and Anxiety Disorders in The Population Displaced by Violence in Colombia; Results of The National Mental Health Survey 2015]. Revista colombiana de psiquiatria. 2016;45 Suppl 1:113–8. Spanish. [DOI] [PubMed] [Google Scholar]
- 84.Tay AK, Rees S, Miah MAA, Khan S, Badrudduza M, Morgan K, et al. Functional impairment as a proxy measure indicating high rates of trauma exposure, post-migration living difficulties, common mental disorders, and poor health amongst Rohingya refugees in Malaysia. Translational psychiatry. 2019;9(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tousignant M, Habimana E, Biron C, Malo C, Sidoli-LeBlanc E, Bendris N. The Quebec Adolescent Refugee Project: psychopathology and family variables in a sample from 35 nations. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(11):1426–32. doi: 10.1097/00004583-199911000-00018 [DOI] [PubMed] [Google Scholar]
- 86.Um MY, Rice E, Lee JO, Kim HJ, Palinkas LA. Suicidal ideation among North Korean refugees in South Korea: Exploring the influence of social network characteristics by gender. Transcultural psychiatry. 2020:1363461520935314. doi: 10.1177/1363461520935314 [DOI] [PubMed] [Google Scholar]
- 87.Vigod SN, Arora S, Urquia ML, Dennis CL, Fung K, Grigoriadis S, et al. Postpartum self-inflicted injury, suicide, assault and homicide in relation to immigrant status in Ontario: a retrospective population-based cohort study. CMAJ open. 2019;7(2):E227–e35. doi: 10.9778/cmajo.20180178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Vijayakumar L, Mohanraj R, Kumar S, Jeyaseelan V, Sriram S, Shanmugam M. CASP—An intervention by community volunteers to reduce suicidal behaviour among refugees. The International journal of social psychiatry. 2017;63(7):589–97. doi: 10.1177/0020764017723940 [DOI] [PubMed] [Google Scholar]
- 89.Westman J, Sundquist J, Johansson LM, Johansson S-E, Sundquist K. Country of birth and suicide: a follow-up study of a national cohort in Sweden. Archives of Suicide Research. 2006;10(3):239–48. doi: 10.1080/13811110600582471 [DOI] [PubMed] [Google Scholar]
- 90.Winkler JG, Brandl EJ, Bretz HJ, Heinz A, Schouler-Ocak M. Psychische Symptombelastung bei Asylsuchenden in Abhängigkeit vom Aufenthaltsstatus. Psychiatrische Praxis. 2019;46(04):191–9. German. [DOI] [PubMed] [Google Scholar]
- 91.Yu SE, Jeon WT. Mental health of north korean refugees in protective facilities in china. Psychiatry investigation. 2008;5(2):70–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yüzbaşıoğlu Y, Işık GÇ. Retrospective analysis of forensic cases in refugees admitted to emergency department. The American journal of emergency medicine. 2019;37(9):1691–3. doi: 10.1016/j.ajem.2018.12.010 [DOI] [PubMed] [Google Scholar]
- 93.Akinyemi OO, Atilola O, Soyannwo T. Suicidal ideation: Are refugees more at risk compared to host population? Findings from a preliminary assessment in a refugee community in Nigeria. Asian journal of psychiatry. 2015;18:81–5. doi: 10.1016/j.ajp.2015.09.001 [DOI] [PubMed] [Google Scholar]
- 94.Betancourt TS, Newnham EA, Layne CM, Kim S, Steinberg AM, Ellis H, et al. Trauma history and psychopathology in war-affected refugee children referred for trauma-related mental health services in the United States. Journal of traumatic stress. 2012;25(6):682–90. doi: 10.1002/jts.21749 [DOI] [PubMed] [Google Scholar]
- 95.Björkenstam E, Helgesson M, Amin R, Lange T, Mittendorfer-Rutz E. Mental disorders and suicidal behavior in refugees and Swedish-born individuals: is the association affected by work disability? Social psychiatry and psychiatric epidemiology. 2020;55(8):1061–71. doi: 10.1007/s00127-019-01824-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Björkenstam E, Helgesson M, Amin R, Mittendorfer-Rutz E. Mental disorders, suicide attempt and suicide: differences in the association in refugees compared with Swedish-born individuals. The British Journal of Psychiatry. 2020;217(6):679–85. doi: 10.1192/bjp.2019.215 [DOI] [PubMed] [Google Scholar]
- 97.Cochran J, Geltman PL, Ellis H, Brown C, Anderton S, Montour J, et al. Suicide and suicidal ideation among Bhutanese refugees—United States, 2009–2012. MMWR Morbidity and mortality weekly report. 2013;62(26):533. [PMC free article] [PubMed] [Google Scholar]
- 98.Ellis BH, Lankau EW, Ao T, Benson MA, Miller AB, Shetty S, et al. Understanding Bhutanese refugee suicide through the interpersonal-psychological theory of suicidal behavior. The American journal of orthopsychiatry. 2015;85(1):43–55. doi: 10.1037/ort0000028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Richter K, Lehfeld H, Niklewski G. [Waiting for Asylum: Psychiatric Diagnosis in Bavarian Admission Center]. Gesundheitswesen (Bundesverband der Arzte des Offentlichen Gesundheitsdienstes (Germany)). 2015;77(11):834–8. German. doi: 10.1055/s-0035-1564075 [DOI] [PubMed] [Google Scholar]
- 100.Um MY, Rice E, Palinkas LA, Kim HJ. Migration-Related Stressors and Suicidal Ideation in North Korean Refugee Women: The Moderating Effects of Network Composition. Journal of traumatic stress. 2020;33(6):939–49. doi: 10.1002/jts.22549 [DOI] [PubMed] [Google Scholar]
- 101.Van Oostrum IE, Goosen S, Uitenbroek DG, Koppenaal H, Stronks K. Mortality and causes of death among asylum seekers in the Netherlands, 2002–2005. Journal of Epidemiology & Community Health. 2011;65(4):376–83. doi: 10.1136/jech.2009.087064 [DOI] [PubMed] [Google Scholar]
- 102.Vonnahme LA, Lankau EW, Ao T, Shetty S, Cardozo BL. Factors Associated with Symptoms of Depression Among Bhutanese Refugees in the United States. Journal of immigrant and minority health. 2015;17(6):1705–14. doi: 10.1007/s10903-014-0120-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Steel Z, Chey T, Silove D, Marnane C, Bryant RA, Van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. Jama. 2009;302(5):537–49. doi: 10.1001/jama.2009.1132 [DOI] [PubMed] [Google Scholar]
- 104.Lindert J, von Ehrenstein OS, Priebe S, Mielck A, Brähler E. Depression and anxiety in labor migrants and refugees–a systematic review and meta-analysis. Social science & medicine. 2009;69(2):246–57. [DOI] [PubMed] [Google Scholar]
- 105.Wong EC, Marshall GN, Schell TL, Elliott MN, Hambarsoomians K, Chun C-A, et al. Barriers to mental health care utilization for US Cambodian refugees. Journal of consulting and clinical psychology. 2006;74(6):1116. doi: 10.1037/0022-006X.74.6.1116 [DOI] [PubMed] [Google Scholar]
- 106.Ventevogel P, Ryan G, Kahi V, Kane J. Capturing the essential: Revising the mental health categories in UNHCR’s Refugee Health Information System. Intervention-Journal of Mental Health and Psychosocial Support in Conflict Affected Areas. 2019;17(1):13-. [Google Scholar]
- 107.Procter NG, Kenny MA, Eaton H, Grech C. Lethal hopelessness: Understanding and responding to asylum seeker distress and mental deterioration. International Journal of Mental Health Nursing. 2018;27(1):448–54. doi: 10.1111/inm.12325 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability Statement
All relevant data are within the manuscript and its Supporting information files.