Abstract
Age-related hearing loss (presbycusis) is a prevalent condition attributed primarily to inner ear dysfunction. Little is known about age-related changes in the ossicular joints or their contribution to presbycusis. Herein, we performed a histopathologic analysis of the incudomalleolar joint (IMJ) in specimens from the National Temporal Bone Registry with audiometrically confirmed presbycusis but without histologically observed sensory, neural, strial or mixed features. Twenty-two ‘indeterminate’ presbycusis (IP) cases and thirteen young, normal hearing ears were examined. The age for the IP group was 76.3 ± 10.9 and 32.1 ± 9.5 for the young group (p < 0.05). The joint space between the two ossicles was 22% wider in the IP group (138 ± 58.0 μm) compared to young ears (113 ± 49.0 μm) (p < 0.05). We report that IP ears have a wider IMJ than young ears. Findings have implications for understanding a potential source of presbycusis in indeterminate cases.
Keywords: otopathology, presbycusis, indeterminate presbycusis, cochlear conductive presbycusis, incudomalleolar joint
INTRODUCTION
Age-related high frequency hearing loss (presbycusis) is a near universally experienced condition that affects around two thirds of individuals older than 70 in the United States and has been shown to increase the risk of social isolation and cognitive decline.1,2 Despite its prevalence, the precise etiology of presbycusis remains unclear. There are thought to be four causes of presbycusis (sensory, neural, strial, and indeterminate). While sensory, neural, and strial causes of presbycusis have audiometric and histopathologic correlates, indeterminate presbycusis (IP) lacks a distinct pathologic cause.3–7
Anecdotal as well as histopathologic evidence suggest that the effects of aging may localize to the ossicular chain and more specifically the incudomalleolar (IMJ) and incudostapedial (ISJ) joint spaces.8,9 Additionally, functional and audiometric evidence indicates that aging may increase compliance of the ossicular chain which can result in high-frequency conductive hearing losses.10,11 During life, high frequency conductive hearing loss may not be audiometrically identified due to limitations in bone conduction measures above 4kHz.
We hypothesize that ‘indeterminate’ presbycusis could be the result of an increased width of the IMJ. Herein, we conduct a quantitative histopathologic analysis of the IMJ in patients with previously labeled ‘indeterminate’ presbycusis and compare measures to young, normal hearing ears.
MATERIALS AND METHODS
All temporal bone specimens included in this study are a part of the National Temporal Bone Bank and were available for review at the Massachusetts Eye and Ear Infirmary. Methods for preparation and analysis have been described.12 The original sections were examined microscopically by otopathologists and the histologic and histopathologic features were recorded. Cases were included for analysis if there was audiometrically documented presbycusis without clear histopathological evidence of sensory, neural, strial, or mixed features. Cases were excluded if there was any history of otologic disease, ear surgery, head trauma, exposure to excessive noise or ototoxic medications (Figure 1A). Inclusion criteria for controls were age < 45 with air conduction ≤ 30 dB at 2kHz, 4kHz, 6kHz and 8 kHz. 12 previously described ‘indeterminate’ presbycutic patients (22 ears) were identified and compared with 9 young, normal hearing subjects (13 ears). The protocol was approved by the human subjects committee of the institutional review board at Mass Eye and Ear. Protocol # 2019P003272.
Figure 1.
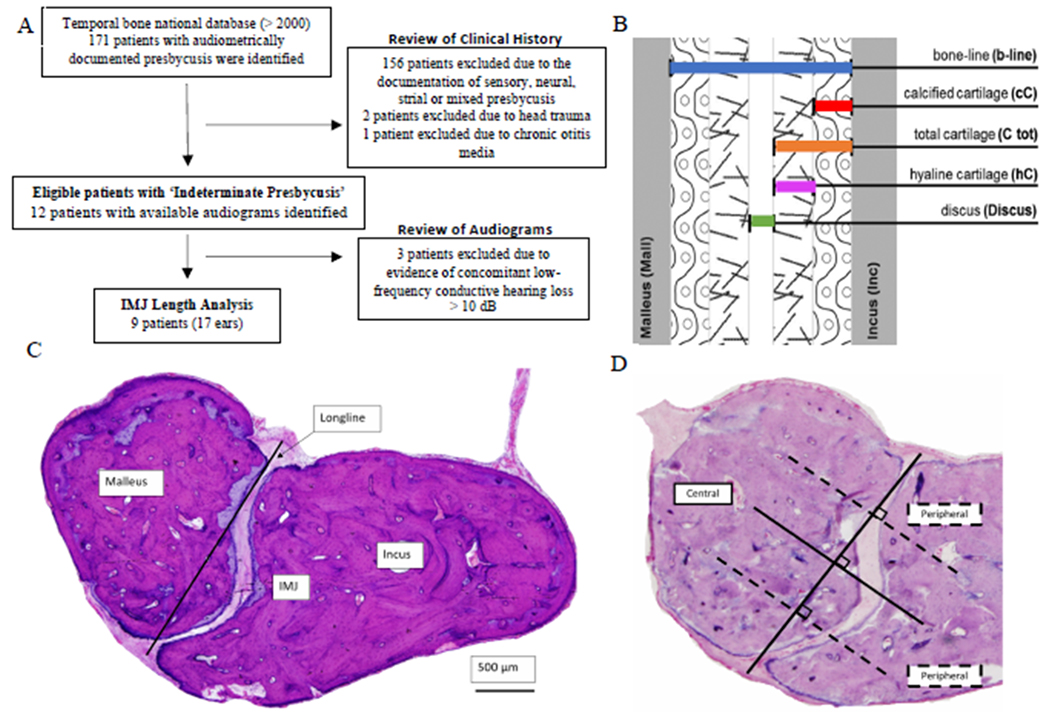
(A) Temporal Bone Selection Algorithm. (B) IMJ Length Analysis (Adopted from Fausch 2015). (C) Control IMJ section with labelled ossicles and longline. (D) Control IMJ section with central and peripheral positions labelled. IMJ = Incudomalleolar joint.
All images were obtained at 5x magnification and measurements were made in ImageJ (http://rsbweb.nih.gov/ij/). We adopted a method developed by Fausch and Röösli to capture 24 unique parameters (Figure 1B) on a single temporal bone section. 13 The section with the longest distance between the synovial membranes resting on the lateral ligaments of the joint capsule (Longline) was selected (Figure 1C). The IMJ was subsequently quartered to visualize three equidistant positions (one central, two peripheral) at which eight measurements of the IMJ could be made (Figure 1D).
All statistical analysis was performed using GraphPad Prism 8.0 (San Diego, California).
RESULTS
Patient demographics for both groups are shown in Table 1. Twenty-four width measurements were performed, analyzed, and statistically compared between the 2 groups. Example IMJ sections are shown for ‘indeterminate’ presbycutic patients (Figure 2A) and young ears (Figure 2B). The distance between the cartilaginous surfaces (discus) of each ossicle was found to be wider (Δ25.0 ± 10.6 μm [SEM]) in the ‘indeterminate’ presbycutic patients (138 ± 58.0 μm) when compared to young ears (113 ± 49.0 μm) (p <0.05) (Figure 2C). When this distance was compared according to its relative location along the IMJ, ‘indeterminate’ presbycutic ears were on average 34μm or 21% wider at the center (p=0.007) and 20μm or 22% wider at the periphery (p=0.052), when compared to young ears (Figure 2D). There were no differences in any of the other parameters, including the total distance between the osseous surfaces (B-line) or the cartilage levels along the length of the IMJ.
Table 1:
Patient Demographics
| General Characteristics | IP (n = 9 patients) (%) | Control (n = 9 patients) (%) |
|---|---|---|
| Age (mean ± standard deviation) | 73.2 ± 9.51 | 32.1 ± 9.47 |
| Males | 6 (66) | 3 (33) |
| Pure Tone Audiometry Results by Ear+ | ||
| Number of Ears | n = 17 (%) | n = 13 (%) |
| Normal Thresholds (< 20dB) | - | 13 (100) |
| Downsloping [≥2kHz] moderate to severe or profound pattern | 17 (100) | - |
All patients and controls had documented audiometry during life
Figure 2.
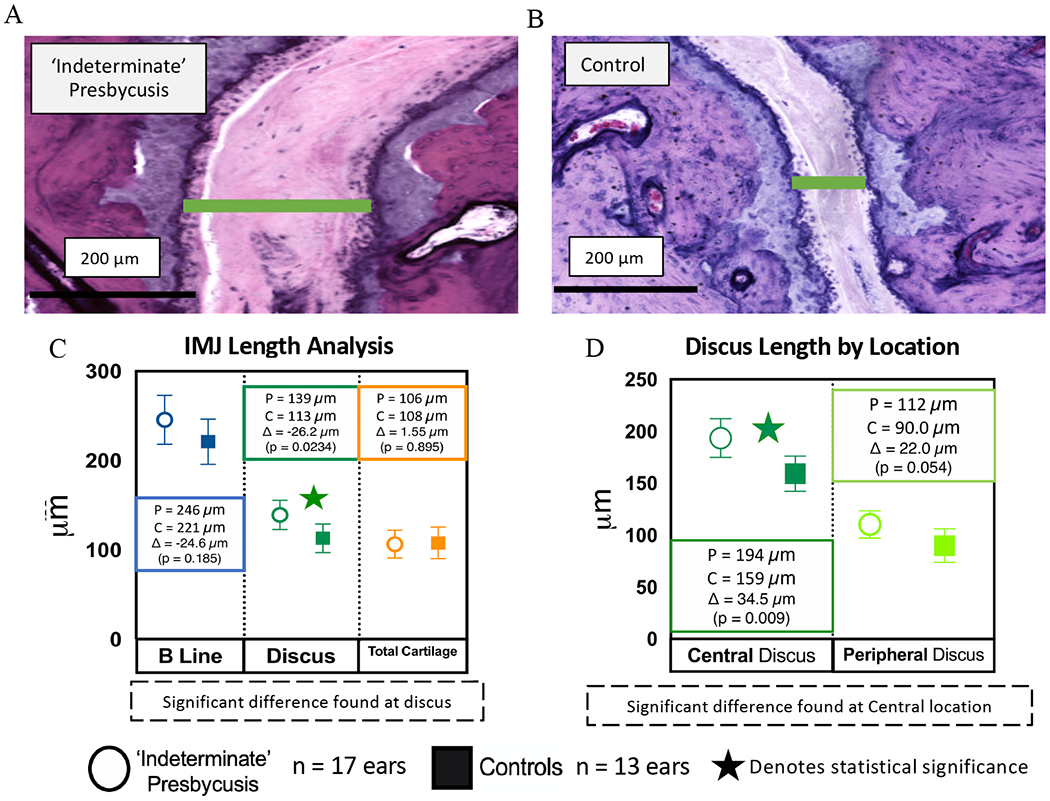
(A) Annotated Indeterminate Presbycusis Section at Central Location showing widened discus (compared to 2B). (B) Annotated Control Section at Central Location. (C) IMJ Length Analysis. Total Cartilage = Total Car Malleus + Total Car Incus. (D) Discus Length by Location (Central vs Peripheral).
DISCUSSION
This study demonstrates that compared to young ears, the IMJ is wider in a population of presbycutic ears without histopathologic evidence of sensory, neural, strial, or mixed features. We hypothesize that a widened IMJ may lead to alteration in joint compliance. Prior work in middle ear mechanics has demonstrated that increases in ossicular compliance may lead to increased absorption and decreased transfer of high-frequency sound.10,14,15 Our findings lend support to the hypothesis that the IMJ in patients with ‘indeterminate’ presbycusis may be more compliant, and therefore, provide a potential source of high frequency hearing loss. This finding augments our understanding of age-related hearing loss as a purely sensorineural pathology and bears clinical relevance for future research in middle ear reconstructive strategies as well as targeted treatment plans for presbycusis.
While our results support the role of the IMJ as a potential conductive lesion in presbycusis, further histopathologic work is necessary to evaluate the IMJ in all forms of presbycusis. This will allow us to determine if a widened joint space is unique to ‘indeterminate’ presbycusis or if it may also occur in other types of age-related hearing loss. Additional histopathologic work should be performed to identify changes at other locations in the conductive pathway including the ISJ and middle ear ligaments for patients with ‘indeterminate’ presbycusis.8,16,17 Further biomechanical work is necessary to explore how histologically observed differences in the ossicular chain affect middle ear immittance and conductive hearing.
CONCLUSION
The IMJ in patients with ‘indeterminate’ presbycusis was wider than in younger individuals without presbycusis. Further histopathologic and biomechanics research is necessary to understand the prevalence and functional effects of observed differences.
Acknowledgements:
The authors would like to thank MengYu Zhu for her help with obtaining - Temporal Bone Specimens for analysis. We would also like to acknowledge Dr. John Rosowski for his insightful feedback on the manuscript.
Grant Support:
NIH NIDCD K08DC018575
Footnotes
Level of Evidence: Retrospective Study
Financial Disclosures: None
Conflicts of Interest: None
REFERENCES
- 1.Livingston G, Sommerlad A, Orgeta V, et al. Dementia prevention, intervention, and care. Lancet Lond Engl. 2017;390(10113):2673–2734. doi: 10.1016/S0140-6736(17)31363-6 [DOI] [PubMed] [Google Scholar]
- 2.Tu NC, Friedman RA. Age-related hearing loss: Unraveling the pieces. Laryngoscope Investig Otolaryngol. 2018;3(2):68–72. doi: 10.1002/lio2.134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schuknecht HF. Further Observations On the Pathology of Presbycusis. Arch Otolaryngol. 1964;80(4):369–382. doi: 10.1001/archotol.1964.00750040381003 [DOI] [PubMed] [Google Scholar]
- 4.Schuknecht HF, Gacek MR. Cochlear pathology in presbycusis. Ann Otol Rhinol Laryngol. 1993;102(1 Pt 2):1–16. doi: 10.1177/00034894931020S101 [DOI] [PubMed] [Google Scholar]
- 5.Spicer SS, Schulte BA. Pathologic changes of presbycusis begin in secondary processes and spread to primary processes of strial marginal cells. Hear Res. 2005;205(1–2):225–240. doi: 10.1016/j.heares.2005.03.022 [DOI] [PubMed] [Google Scholar]
- 6.Chen MA, Webster P, Yang E, Linthicum FH. Presbycusic Neuritic Degeneration Within the Osseous Spiral Lamina: Otol Neurotol. 2006;27(3):316–322. doi: 10.1097/00129492-200604000-00005 [DOI] [PubMed] [Google Scholar]
- 7.Ramadan HH, Schuknecht HF. Is There a Conductive Type of Presbycusis? Otolaryngol Neck Surg. 1989;100(1):30–34. doi: 10.1177/019459988910000105 [DOI] [PubMed] [Google Scholar]
- 8.Goodhill V Bilateral Malleal Fixation and Conductive Presbycusis. Arch Otolaryngol - Head Neck Surg. 1969;90(6):759–764. doi: 10.1001/archotol.1969.00770030761019 [DOI] [PubMed] [Google Scholar]
- 9.Etholm B, Belal A. Senile changes in the middle ear joints. Ann Otol Rhinol Laryngol. 1974;83(1):49–54. doi: 10.1177/000348947408300109 [DOI] [PubMed] [Google Scholar]
- 10.Feeney MP, Sanford CA. Age effects in the human middle ear: Wideband acoustical measures. J Acoust Soc Am. 2004;116(6):3546–3558. doi: 10.1121/1.1808221 [DOI] [PubMed] [Google Scholar]
- 11.Whittemore KR, Merchant SN, Poon BB, Rosowski JJ. A normative study of tympanic membrane motion in humans using a laser Doppler vibrometer (LDV). Hear Res. 2004;187(1–2):85–104. doi: 10.1016/s0378-5955(03)00332-0 [DOI] [PubMed] [Google Scholar]
- 12.Schuknecht HF. Methods of Removal, Preparation and Study. In: Pathology of the Ear. 2nd ed. Lea & Febiger; 1993. [Google Scholar]
- 13.Fausch C, Röösli C. The incudomalleolar articulation in Down syndrome (trisomy 21): a temporal bone study. Otol Neurotol Off Publ Am Otol Soc Am Neurotol Soc Eur Acad Otol Neurotol. 2015;36(2):348–353. doi: 10.1097/MAO.0000000000000456 [DOI] [PubMed] [Google Scholar]
- 14.Nakajima HH, Ravicz ME, Merchant SN, Peake WT, Rosowski JJ. Experimental ossicular fixations and the middle ear’s response to sound: evidence for a flexible ossicular chain. Hear Res. 2005;204(1–2):60–77. doi: 10.1016/j.heares.2005.01.002 [DOI] [PubMed] [Google Scholar]
- 15.Rosowski JJ, Nakajima HH, Merchant SN. Clinical utility of laser-Doppler vibrometer measurements in live normal and pathologic human ears. Ear Hear. 2008;29(1):3–19. doi: 10.1097/AUD.0b013e31815d63a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moon CN, Hahn MJ. Primary malleus fixation: diagnosis and treatment. The Laryngoscope. 1981;91(8):1298–1307. doi: 10.1288/00005537-198108000-00012 [DOI] [PubMed] [Google Scholar]
- 17.Dai C, Cheng T, Wood MW, Gan RZ. Fixation and detachment of superior and anterior malleolar ligaments in human middle ear: Experiment and modeling. Hear Res. 2007;230(1–2):24–33. doi: 10.1016/j.heares.2007.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]


