Abstract
The ability to comprehensively assess the diet of infants is essential for monitoring adequate growth; however, it is challenging to assess dietary intake with a high level of accuracy. Infants rely on surrogate reporting by caregivers. This study aimed to determine if surrogate reporters (e.g., caregivers) could use an image-based mobile food record adapted (baby mFR) to record infants’ eating occasions, and via caregiver feedback, could assess the usability and feasibility of the baby mFR in recording infants’ diets. This was a cross-sectional study in which surrogate reporters (e.g., caregivers) recorded all food and beverage intake (including human milk) of the infant over a 4-day period. Trained research staff evaluated all images submitted during data collection for different indicators of quality. All surrogate reporters were asked to complete a usability questionnaire at the end of the 4-day data collection period. Basic descriptive analyses were performed on the infants 3–12 months of age (n = 70). A total of 91% (n = 64) of surrogate reporters used the baby mFR to record their infants’ eating occasions. The mean number of images submitted daily per participant via the mFR was 4.2 (SD 0.2). A majority of submitted images contained the fiducial marker and the food and/or beverage was completely visible. The mFR was found to be easy to use; however, suggestions were provided to increase utility of the application such as the inclusion of a bottle button and reminders. An image-based dietary assessment method using a mobile app was found to be feasible for surrogate reporters to record an infant’s food and beverage intake throughout the day.
Keywords: infant diet, mobile food record technology, acceptability
1. Introduction
Adequate nutrition is important for achieving normal growth and development during infancy. Therefore, dietary assessment is an integral component of infant growth monitoring [1]. However, the accuracy of the assessment of complementary feeding and dietary intakes in infants is reliant on surrogate reporting by caregivers. Surrogate reporting is influenced by the amount of time spent with the infant and knowing the full details of any food prepared elsewhere (e.g., at daycare) during the assessment period. A systematic review concluded weighed food records provided the best estimates of energy as estimated by doubly labeled water for children 0.5–4 years of age [2]. This method, however, places a much higher burden on those undertaking the recording (aka infant surrogate reporters).
Mobile technology offers a wide range of feasible options for dietary assessment, which are easier to incorporate into daily routines due to its widespread adoption. Incorporating user images captured by mobile technology has improved the accuracy of conventional dietary assessment methods by adding eating occasion details such as time as well as reducing underreporting when compared with traditional assessment methods [3].
One image-based method, the Technology Assisted Dietary Assessment (TADA) system [4,5], uses an image-based dietary record application, the mobile food record (mFR) [6,7], to capture before and after eating images from the mobile device. Automated image analysis [8] or a trained analyst can identify the foods in the image and estimate portion size of foods consumed [9,10,11]. This method provides real-time data collection and eliminates reliance on the respondent’s memory, proxy reports, and ability to write and/or estimate portions [9]. The mFR has been identified as feasible for use in assessing the diets of children as young as 3 years [10] of age and through to adults [12,13,14]. Adults (18–49 y) are the highest adopters of mobile devices and represent the majority of parents with young children [15]. Therefore, determining the feasibility, or ease and convenience of use, by surrogates (aka caregivers) of the mFR for infant dietary assessment merits exploration. This study is the first time that an image-based dietary assessment approach has been used to capture the total diet of infants which may improve accuracy of dietary assessment in infants through reducing surrogate burden [3]. Addressing feasibility, which includes determining willingness, adherence and compliance, are all an important aspects to evaluate as they inform important parameters for further research such as validation studies [16]. The purpose of this study was to determine if surrogate reporters (e.g., caregivers) could successfully use the mFR adapted for infants, referred to as the baby mFR in this paper, to record their infants’ eating occasions over a 4-day period. In addition, this study gathered the perspective of the caregivers on usability of the baby mFR. This study addresses identified recommendations for using a mobile app specifically designed for capturing dietary assessment of infants [17].
2. Materials and Methods
This cross-sectional examination of the baby mFR was conducted with an ethnically diverse sample of infants between 3 and 12 months of age residing on O‘ahu, Hawai‘i between March 2018 and February 2019. This age range was selected in order to examine complementary food introduction and diet diversity, which was reported in a separate publication [18].
Eligible participants in this study were infants between 3 and 12 months of age that had already started complementary feeding, infants identified by their surrogate reporters as having Native Hawaiian, Pacific Islander, and/or Filipino ethnicity, and infants who had a surrogate reporter that was 18 years of age or older. Additional eligibility for surrogate reporters included access to an iOS mobile device with reliable access to the Internet. This sample of convenience was primarily recruited through community events (e.g., Baby Expo), community programs (e.g., Special Supplemental Nutrition Program for Women, Infants, and Children), and social networking (e.g., Facebook groups). This study was deemed Exempt by the University of Hawai‘i Institutional Review Board. Consent was obtained in writing from the surrogate reporters for both their participation and their infant’s participation prior to collecting any data. Surrogate reporters were compensated with a USD 40 gift card for their participation.
Surrogate reporting via caregivers using the baby mFR provided the dietary data to do the assessment. The baby mFR collected breastfeeding occasion via a timer feature and complementary feeding occasions via a camera feature capturing pre- and post-images of all foods and beverages consumed.
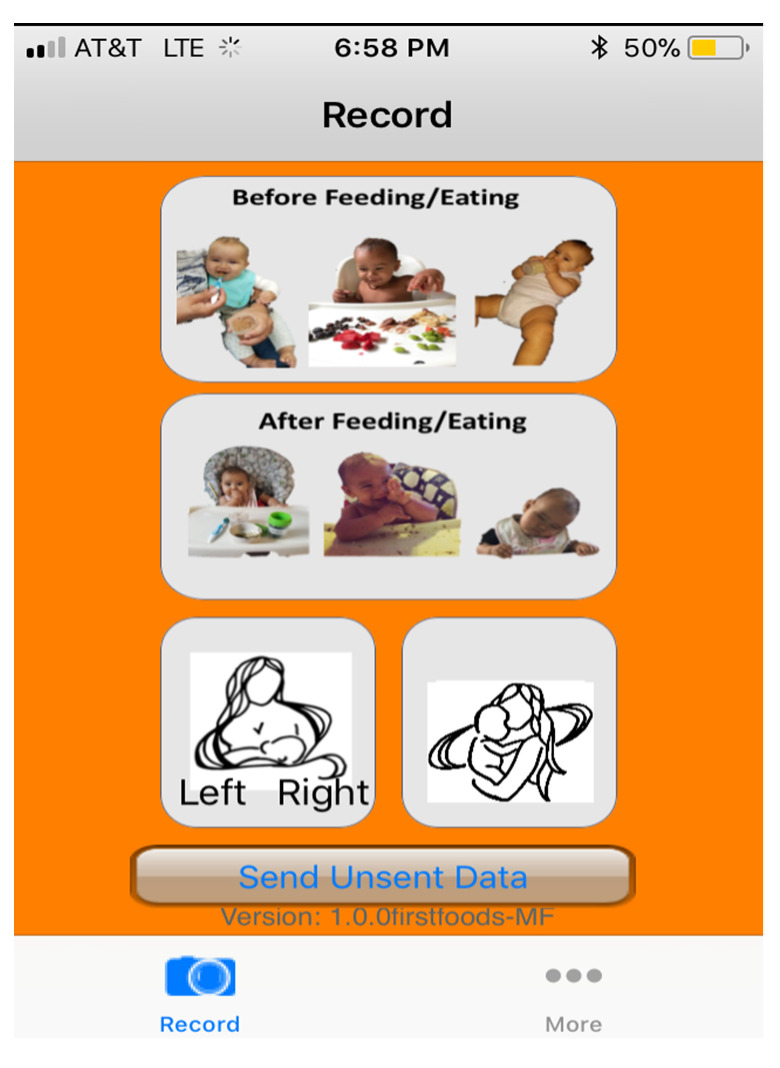
The baby mFR is a mobile application running on an iOS platform designed to use the camera on a smart device to capture food and beverage intake, which is then used to estimate energy and nutrient intakes. All captured images were automatically uploaded to the secure TADA website, when a wireless connection was available. Each surrogate was also provided with fiducial markers (FM) to include in all recorded images in the bottom left corner. The FM acts as a size and color reference which enhances the ability of the trained analyst to assess the content of the image or for automated analysis to occur as part of an image recognition system [19]. Prior to data collection, the baby mFR app was loaded on to the surrogate reporter’s mobile device and the surrogate reporter was trained on its use. The data collection period was informed by previous studies [10,20] as this was the first time this method was applied to infants. Surrogate reporters were instructed to complete a 4-day food record (Thursday–Sunday) using the baby mFR. Pre- and post-images of all foods and beverages consumed by the infant participant over the 4-day period were captured by the baby mFR. The baby mFR included interchangeable color borders (i.e., red or green) to guide the surrogate on when to take the image as published elsewhere [7,10]. At the conclusion of the 4-day collection period, researchers logged into the TADA website to view images [7]. As needed, images from the baby mFR were reviewed with the surrogate reporters by a member of the research team to verify content and to probe for any forgotten foods or beverages. A unique feature of the baby mFR was a timer to record the start and end of a breastfeeding event. See Figure 1 for a depiction of the baby mFR home screen.
Figure 1.
Home screen for the baby Mobile Food Record (mFR) application.
All surrogate reporters were asked to complete an online questionnaire administered through a research web application. Surrogates reported basic demographic information of the infant participant (e.g., age, race/ethnicity) and answered a semi-qualitative usability questionnaire modified from a previous study in children [10]. The questions included in the usability questionnaire are presented in Appendix A.
For this study a human analyst examined all images on the TADA website. Information about each image was entered into a Google Form specifically designed for this study. Such information included the date and timestamp of each image, presence of before or after images, visibility of all foods and beverages and/or the FM, and other non-food objects captured in the image. Breastfeeding timing data and surrogate reporter’s responses to the baby mFR usability questionnaire were also summarized. Open-ended responses were used to provide further context to Likert responses in the usability questionnaire (See Appendix A for examples). All quantitative data were analyzed descriptively (frequencies and means) using IBM SPSS statistics version 27 (IBM Corporation, Armonk, NY, USA).
3. Results
3.1. Participants
A total of 70 infants and their surrogate reporters participated in the study. As indicated in Table 1, a majority of the infants were between the ages of 6 and 12 months, and were identified by their caregiver as Native Hawaiian or Part Native Hawaiian ethnicity. The study was almost evenly distributed between boys and girls, and those who were given and not given human milk (Table 1).
Table 1.
Characteristics of infants, 3–12 months of age, that participated in the study (n = 70).
| Characteristics | n (%) a |
|---|---|
| Age group | |
| 3–5 months | 14 (20) |
| 6–12 months | 56 (80) |
| Sex | |
| Boy | 38 (54) |
| Girl | 32 (46) |
| Ethnicity b | |
| Part-Native Hawaiian or Native Hawaiian | 50 (71) |
| Pacific Islander only c | 4 (6) |
| Part-Filipino or Filipino | 35 (50) |
| Currently receiving human milk | 40 (57) |
a Percentages may not add up to 100 due to rounding, b More than one race/ethnicity may have been self-selected, therefore will not add to 100%, c Self-reported Pacific Islander ethnic groups included Chamorro, Samoan, Tongan, Maori, Tahitian, and Micronesian.
3.2. Mobile Food Record
The majority of participants (n = 64, 91%) recorded 4 out of 4 days of dietary intake. Three participants provided 3 days of dietary intake (4%), two participant completed 2 days of dietary intake (3%), and one participant did 1 day (1%). A total of 66 surrogate reporters (94%) used the baby mFR app to record their infant’s food and beverage intake. Four surrogate reporters (6%) used their mobile device to take images of their infant’s food and beverage intake and texted these images directly to the researchers. Twenty-three (33%) surrogate reporters used both the baby mFR app to upload images and texted food/beverage images or information to the researchers. The mean number of images submitted per day per participant via the mFR app was 4.2 (SD 0.2). As described in Table 2, over 50% of before and after images had a FM. The food was completely visible in almost 75% of the before (n = 414) and after images (n = 412).
Table 2.
Assessment of images captured using the baby mobile food record (mFR) or via mobile device among infants, 3–12 months of age (n = 66).
| Mode of Submission | ||||
|---|---|---|---|---|
| mFR | Text | |||
| Total Number of Images | 1114 | 66 | ||
| Before | After | Before | After | |
| Fiducial Marker | n (%) a | n (%) a | n (%) a | n (%) a |
| Absent | 165 (30) | 176 (32) | 42 (100) | 24 (100) |
| Partially Present | 65 (12) | 60 (11) | 0 (0) | 0 (0) |
| Present | 329 (59) | 319 (58) | 0 (0) | 0 (0) |
| Location of Fiducial Marker in Image | ||||
| Absent | 165 (30) | 176 (32) | 42 (100) | 24 (100) |
| Bottom-Left Corner | 198 (35) | 185 (33) | 0 (0) | 0 (0) |
| Bottom-Right Corner | 79 (14) | 70 (13) | 0 (0) | 0 (0) |
| Center Bottom | 97 (17) | 101 (18) | 0 (0) | 0 (0) |
| Center Top | 4 (1) | 6 (1) | 0 (0) | 0 (0) |
| Top-Left Corner | 9 (2) | 9 (2) | 0 (0) | 0 (0) |
| Top-Right Corner | 7 (1) | 8 (1) | 0 (0) | 0 (0) |
| Food and Beverage Visibility | ||||
| Forgot to Take an Image of Eating Occasion | 8 (1) | 36 (7) | 0 (0) | 0 (0) |
| Completely Visible | 414 (74) | 412 (74) | 36 (86) | 20 (83) |
| Partially Visible | 118 (21) | 99 (18) | 5 (12) | 4 (17) |
| Not Visible | 19 (3) | 8 (1) | 1 (2) | 0 (0) |
| Participant In Image | 30 (5) | 37 (7) | 5 (12) | 2 (8) |
a Disclaimer: may not add up to 100 due to rounding.
Over 40% (n = 30) of all the infant participants in this study had breastfeeding timing data. The mean number of breastfeeding events each day were similar; however, the mean duration of a breastfeeding event in minutes was higher during the weekend days (Saturday and Sunday) versus the weekdays (Thursday and Friday). A majority of breastfeeding events were between 1 min and 120 min in duration (Table 3).
Table 3.
Descriptive data of breastfeeding events of infants, 3–12 months of age (n = 30), captured using the mobile food record (mFR) breastfeeding timer.
| mFR Recording Day | ||||
|---|---|---|---|---|
| Variable | Thursday | Friday | Saturday | Sunday |
| Sample size (n) | 25 | 30 | 27 | 25 |
| Mean (SD) | Mean SD |
Mean SD |
Mean SD |
|
| Number of breastfeeding events recorded | 4.9 (3.5) | 5 (3.6) | 5.6 (3.4) | 4.1 (3.1) |
| Duration of breastfeeding events in minutes | 7.0 (6.3) | 12.8 (11.8) | 17.5 (18.3) | 36.1 (48.4) |
| n (%) | n (%) | n (%) | n (%) | |
| Number of breastfeeding events <1 min | 20 (16) | 6 (4) | 18 (12) | 4 (4) |
| Number of breastfeeding events between 1 and 120 min | 102 (84) | 143 (95) | 132 (87) | 92 (89) |
| Number of breastfeeding events >120 min | 0 (0) | 1 (1) | 2 (1) | 7 (7) |
3.3. Surrogate Reporter Feedback
When surrogate reporters were asked how long they would be willing to record their baby’s intake using the baby mFR, 35% (n = 25) responded for seven days and 34% (n = 24) responded for four days. A majority of surrogate reporters (n = 64, 91%) indicated the baby mFR did not change the way they were feeding their baby. Eighty percent (n = 56) of surrogate reporters indicated they never or almost never had problems using the mFR. Of those that indicated they had problems the most common issues were related to the speed of uploading images, recognition of the FM, image clarity, and the breastfeeding timer.
As shown in Table 4, a majority of surrogate reporters found the mFR easy to use. Reasons provided by surrogate reporters on its ease were related to the convenience of the app being on their phone, minimalist design, and clearly labeled buttons. “It was easy to use and since I carry my phone with me wherever I go, it was much easier to use than writing everything down”, “Because the button selections were minimal, it made it very dummy proof and easy to use”, “The app was clearly labeled and I liked the marker used to determine the angle of each picture. It was user friendly and the ease of it made it easier for me to access and use it properly”, and “They [mFR icons] were relatable. I knew what they were indicating”. A majority of surrogate reporters also found taking before and after eating images, as well as including the FM in the images easy to do. One surrogate reporter commented “Kept one fiducial market in my purse for on the go and one in the kitchen”.
Table 4.
Likert responses from caregivers of infants 3–12 months of age (n = 70) to the baby mobile food record (mFR) usability questionnaire.
| Strongly Agree or Agree | Neither Agree or Disagree | Disagree or Strongly Disagree | |
|---|---|---|---|
| Questions | n (%) a | n (%) a | n (%) a |
| The mFR was easy to use | 66 (94) | 3 (4) | 1 (1) |
| The directions about how to use the mFR were easy to follow | 65 (93) | 3 (4) | 2 (3) |
| Knowing when to take an image of my child’s eating was easy | 65 (93) | 4 (6) | 1 (1) |
| Remembering to take an image before my child ate was easy | 50 (71) | 10 (14) | 10 (14) |
| Remembering to take an image after my child ate was easy | 45 (64) | 15 (21) | 10 (14) |
| Remembering to push the button before breastfeeding my child was easy b | 17 (25) | 10 (14) | 12 (17) |
| Remembering to push the button after breastfeeding my child was easy b | 11 (15) | 9 (13) | 19 (27) |
| I found it easy to include the fiducial marker in the picture of my child’s meals | 42 (60) | 13 (19) | 15 (22) |
| The mFR interfered with my daily activities | 2 (3) | 19 (27) | 49 (70) |
| Understanding the purpose of the mFR motivated me to use it c | 61 (87) | 7 (10) | 1 (1) |
| Overall, the mFR was a nuisance to use | 3 (4) | 19 (27) | 48 (69) |
| Overall, the mFR was enjoyable to use | 53 (76) | 16 (23) | 1 (1) |
| I would like to participate in another study using the mobile food record. | 58 (83) | 10 (14) | 2 (2) |
a Not all percentages will add up to 100 due to rounding. b This question was not applicable to all participants. c There was one missing response.
One area in which surrogate reporters found to be not easy to do was starting and stopping the breastfeeding timer (Table 4). Reasons shared by surrogate reporters included “The timer went off when I switched to another app” and “Because I breastfeed whenever, wherever, it was difficult for me to keep up with recording my feedings because I don’t always have my phone by me”.
Caregivers overwhelmingly agreed knowing the purpose of the study motivated their use (Table 4), commenting “I liked knowing I was helping research concerning my child” and “I liked taking pics of my daughter’s food and knowing I was helping you folks out”.
Other notable comments provided by surrogate reporters included the importance of other individuals having the mFR downloaded to their devices to record their baby’s intake. Comments from surrogate reporters included “Actually, my mom had to because I had to go to work 3 out of the 4 days of the study. So she downloaded it to her phone and took most of the lunch and dinner pictures for me” and “Boss helped take pics, she was ok, and boyfriend also used it”. In addition, surrogate reporters’ provided suggestions for improvements to the mFR. Improvements were related to the icons used such as, “A simple example of before and after pictures would have been better instead of three babies making it too busy icons”, as well as for other features “I would suggest having a bottle option on the menu to select the number of ounces instead of needing to take a picture of it”, “Would be nice to add texts and self-identify what it is”, and “more reminders”.
4. Discussion
This is the first study to evaluate the use of an image-based novel dietary assessment application, the baby mFR, to capture the diet of Native Hawaiian, Pacific Islander, and/or Filipino infants 3–12 months of age, a population underrepresented in research [21]. These results indicate that the mFR is a feasible method to conduct dietary assessment in infants. The baby mFR provides great utility to infant dietary assessment as it reduces the burden of other traditional methods of dietary assessment such as a dietary record and recall. The use of mobile technology, which is widely prevalent [15], provides data in real time without the burden of completing hand-written dietary records. As demonstrated in this study’s findings, a majority of surrogate reporters were willing to use the mFR in another study indicating a positive reception to the application.
An unexpected outcome of this study, which was only seen in one other study which used the mFR in young adults with Down Syndrome [14] but not seen in previous mFR studies with children or adults [9,10], was the submission of images directly from the surrogate reporters’ mobile device via text message versus through the baby mFR. As indicated in the feedback from surrogate reporters, providing dietary intake information on their infant was a communal affair where other family members, friends, babysitter, or other acquaintances would contribute images on the infants’ intake when the surrogate reporter was not present. Since the baby mFR was only installed on the primary surrogate reporter’s device, images taken from other devices were submitted via text messages to the research team. Future research is needed to explore the utility of uploading the baby mFR on multiple devices for conducting infant dietary assessment. This potentially would also ameliorate the number of eating occasions missing image(s) due to the infant being cared for by someone without access to the baby mFR.
The baby mFR was developed to assess at-the-breast feeding sessions through the use of a timer, which would be less burdensome and costly than other measures of assessment [22]. This feature allowed researchers to distinguish between human milk received directly from the breast versus expressed [23]. Distinguishing how human milk is received by infants may be important as a previous study has shown that health outcomes differ between the feeding modes [24]. Further work is needed to evaluate the breastfeeding timing data for outliers. In this paper, three different cut-offs were used, <1 min, between 1 and 120 min and >120 min. There are various ways in which timing data can be interpreted such as less than 5 [17] or 10 [25] minutes as snacks or lasting as long as 120 min [26]. However, duration of the at-the-breast sessions may have significant variability such as night feeds lasting longer than during the day feeds, and differences in the length of feeds for younger versus older infants. In addition, there seemed to be a higher number of short timing sessions, e.g., <1 min, in the first day of data collection than in later days. This may be a result of reporters getting familiar with the feature’s functionality. However, the frequency of breastfeeding events found in this study were similar to what has been documented elsewhere [27]. Another consideration to increase functionality of the mFR for infant dietary assessment, as suggested by participant caregivers, would be to include a bottle feature which would allow researchers to more easily assess expressed milk, formula, and other liquids provided to infants.
As this study was limited to only iOS users, future studies should explore the mFR use on other mobile device operating systems. Additional studies are needed to validate the mFR such as with biomarkers or a controlled feeding trial to assess reporting accuracy, especially in regard to estimating the volume of human milk consumed during breastfeeding events which are difficult to obtain precisely [28]. Further validation of the mFR to perform automated image analysis including food identification, portion size and contextual processing within the infant population would also be warranted similarly to what has been done among adults and adolescents [11,29,30,31]. Accurate infant dietary assessment data are especially important to inform future iterations of the recently added U.S. Dietary Guidelines for children 0–24 months [32,33].
5. Conclusions
An active image-based dietary assessment method using a mobile device was found to be feasible, convenient, and easy to use for caregivers’ to record their infant’s food and beverage intake throughout the day. The significance of this study is that it is the first to evaluate the surrogate use of the mFR among infants younger than 12 months and warrants further research validating its accuracy.
Acknowledgments
The authors would like to thank the study participants and community partners.
Appendix A
Table A1.
Usability questionnaire to assess the feasibility of a mobile food record to assess eating occasions of infants 3–12 months of age.
| Questions |
|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
a Likert response scale: Strongly agree, agree, neither agree or disagree, disagree, strongly disagree, b Likert response scale: Strongly agree, agree, neither agree or disagree, disagree, strongly disagree, not applicable, c Response options: 1–7 days/week, 1–4 weeks/month, d Likert response scale: Never, almost never, sometimes, fairly often, very often, e Likert response scale: Extremely comfortable, mostly comfortable, somewhat comfortable, not too comfortable, not comfortable at all, f Response options: Yes, no.
Author Contributions
Conceptualization, M.K.F., J.N.-O., F.Z. and C.J.B.; methodology, M.K.F., J.N.-O. and C.J.B.; software, Z.S. and F.Z.; formal analysis, M.K.F., J.K., C.Y. and G.L.; writing—original draft preparation, M.K.F.; writing—reviewing and editing M.K.F., J.K., J.N.-O., C.Y., G.L., Z.S., F.Z., D.A.K. and C.J.B.; funding acquisition, M.K.F. and J.N.-O. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by award number U54MD007601 by the National Institute on Minority Health and Health Disparities of the National Institutes of Health, the HMSA Foundation Community Fund grant #CF-021803, and the University of Hawai‘i at Mānoa Native Hawaiian Student Services ‘Ōiwi Undergraduate Research Fellowship Program.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of the University of Hawaiʻi at Mānoa (protocol code 2017-00845 and 7 March 2018).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to ethical restrictions.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mascarenhas M.R., Zemel B., Stallings V.A. Nutritional assessment in pediatrics. Nutrition. 1998;14:105–115. doi: 10.1016/S0899-9007(97)00226-8. [DOI] [PubMed] [Google Scholar]
- 2.Burrows T., Goldman S., Rollo M. A systematic review of the validity of dietary assessment methods in children when compared with the method of doubly labelled water. Eur. J. Clin. Nutr. 2020;74:669–681. doi: 10.1038/s41430-019-0480-3. [DOI] [PubMed] [Google Scholar]
- 3.Boushey C.J., Spoden M., Zhu F.M., Delp E.J., Kerr D.A. New mobile methods for dietary assessment: Review of image-assisted and image-based dietary assessment methods. Proc. Nutr. Soc. 2017;76:283–294. doi: 10.1017/S0029665116002913. [DOI] [PubMed] [Google Scholar]
- 4.Zhu F., Mariappan A., Boushey C.J., Kerr D., Lutes K.D., Ebert D.S., Delp E.J. Technology-assisted dietary assessment. Proc. SPIE Int. Soc. Opt. Eng. 2008;6814:681411. doi: 10.1117/12.778616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu F., Bosch M., Woo I., Kim S., Boushey C.J., Ebert D.S., Delp E.J. The use of mobile devices in aiding dietary assessment and evaluation. IEEE J. Sel. Top. Signal. Process. 2010;4:756–766. doi: 10.1109/JSTSP.2010.2051471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Six B.L., Schap T.E., Zhu F.M., Mariappan A., Bosch M., Delp E.J., Ebert D.S., Kerr D.A., Boushey C.J. Evidence-based development of a mobile telephone food record. J. Am. Diet. Assoc. 2010;110:74–79. doi: 10.1016/j.jada.2009.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmad Z., Bosch M., Khanna N., Kerr D.A., Boushey C.J., Zhu F., Delp E.J. A mobile food record for integrated dietary assessment; Proceedings of the 2nd International Workshop on Multimedia Assisted Dietary Management; Amsterdam, The Netherlands. 16 October 2016; pp. 53–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.He J., Shao Z., Wright J., Kerr D., Boushey C., Zhu F. Multi-task image-based dietary assessment for food recognition and portion size estimation; Proceedings of the IEEE Conference on Multimedia Information Processing and Retrieval; Shenzhen, China. 6–8 August 2020; pp. 49–54. [DOI] [Google Scholar]
- 9.Daugherty B.L., Schap T.E., Ettienne-Gittens R., Zhu F.M., Bosch M., Delp E.J., Ebert D.S., Kerr D.A., Boushey C.J. Novel technologies for assessing dietary intake: Evaluating the usability of a mobile telephone food record among adults and adolescents. J. Med. Internet Res. 2012;14:e58. doi: 10.2196/jmir.1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aflague T.F., Boushey C.J., Guerrero R.T., Ahmad Z., Kerr D.A., Delp E.J. Feasibility and use of the mobile food record for capturing eating occasions among children ages 3–10 years in Guam. Nutrients. 2015;7:4403–4415. doi: 10.3390/nu7064403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhu F., Bosch M., Khanna N., Boushey C.J., Delp E.J. Multiple hypotheses image segmentation and classification with application to dietary assessment. IEEE J. Biomed. Health Inform. 2015;19:377–388. doi: 10.1109/JBHI.2014.2304925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boushey C.J., Spoden M., Delp E.J., Zhu F., Bosch M., Ahmad Z., Shvetsov Y.B., DeLany J.P., Kerr D.A. Reported energy intake accuracy compared to doubly labeled water and usability of the mobile food record among community dwelling adults. Nutrients. 2017;9:312. doi: 10.3390/nu9030312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kerr D.A., Harray A.J., Pollard C.M., Dhaliwal S.S., Delp E.J., Howat P.A., Pickering M.R., Ahmad Z., Meng X., Pratt I.S., et al. The connecting health and technology study: A 6-month randomized controlled trial to improve nutrition behaviours using a mobile food record and text messaging support in young adults. Int. J. Behav. Nutr. Phys. Act. 2016;13:52. doi: 10.1186/s12966-016-0376-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bathgate K.E., Sherriff J.L., Leonard H., Dhaliwal S.S., Delp E.J., Boushey C.J., Kerr D.A. Feasibility of assessing diet with a mobile food record for adolescents and young adults with down syndrome. Nutrients. 2017;9:273. doi: 10.3390/nu9030273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pew Research Center Mobile Fact Sheet. [(accessed on 27 October 2021)]. Available online: http://www.pewinternet.org/fact-sheet/mobile/
- 16.Arain M., Campbell M.J., Cooper C.L., Lancaster G.A. What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Med. Res. Methodol. 2010;10:67. doi: 10.1186/1471-2288-10-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johansson U., Venables M., Ohlund I., Lind T. Active image-assisted food records in comparison to regular food records: A validation study against doubly labeled water in 12-month-old infants. Nutrients. 2018;10:1904. doi: 10.3390/nu10121904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fialkowski M.K., Ng-Osorio J., Kai J., Swafford K., Langfelder G., Young C.G., Chen J.J., Zhu F.M., Boushey C.J. Type, timing, and diversity of complementary foods among native Hawaiian, Pacific Islander, and Filipino infants. Hawaii J. Health Soc. Welf. 2020;79:127–134. [PMC free article] [PubMed] [Google Scholar]
- 19.Xu C., Zhu F., Khanna N., Boushey C.J., Delp E.J. Image enhancement and quality measures for dietary assessment using mobile devices. Proc. SPIE Int. Soc. Opt. Eng. 2012;8296:153–162. doi: 10.1117/12.909949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shoneye C.L., Dhaliwal S.S., Pollard C.M., Boushey C.J., Delp E.J., Harray A.J., Howat P.A., Hutchesson M.J., Rollo M.E., Zhu F., et al. Image-based dietary assessment and tailored feedback using mobile technology: Mediating behavior change in young adults. Nutrients. 2019;11:435. doi: 10.3390/nu11020435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bailey R.L., Stang J.S., Davis T.A., Naimi T.S., Schneeman B.O., Dewey K.G., Donovan S.M., Novotny R., Kleinman R.E., Taveras E.M., et al. Dietary and complementary feeding practices of US infants, 6 to 12 months: A narrative review of the federal nutrition monitoring data. J. Acad. Nutr. Diet. 2021. in press . [DOI] [PMC free article] [PubMed]
- 22.Scanlon K.S., Alexander M.P., Serdula M.K., Davis M.K., Bowman B.A. Assessment of infant feeding: The validity of measuring milk intake. Nutr. Rev. 2002;60:235–251. doi: 10.1301/002966402320289368. [DOI] [PubMed] [Google Scholar]
- 23.Rasmussen K.M., Felice J.P., O’Sullivan E.J., Garner C.D., Geraghty S.R. The meaning of “Breastfeeding” is changing and so must our language about it. Breastfeed. Med. 2017;12:510–514. doi: 10.1089/bfm.2017.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Azad M.B., Vehling L., Chan D., Klopp A., Nickel N.C., McGavock J.M., Becker A.B., Mandhane P.J., Turvey S.E., Moraes T.J., et al. Infant feeding and weight gain: Separating breast milk from breastfeeding and formula from food. Pediatrics. 2018;142:e20181092. doi: 10.1542/peds.2018-1092. [DOI] [PubMed] [Google Scholar]
- 25.Lanigan J.A., Wells J.C., Lawson M.S., Lucas A. Validation of food diary method for assessment of dietary energy and macronutrient intake in infants and children aged 6–24 months. Eur. J. Clin. Nutr. 2001;55:124–129. doi: 10.1038/sj.ejcn.1601128. [DOI] [PubMed] [Google Scholar]
- 26.The American College of Obstetricians and Gynecologists FAQ: Breastfeeding Your Baby. [(accessed on 17 December 2020)]. Available online: https://www.acog.org/womens-health/faqs/breastfeeding-your-baby?utm_source=redirect&utm_medium=web&utm_campaign=otn#baby.
- 27.Ghosh R., Mascie-Taylor C.G., Rosetta L. Longitudinal study of the frequency and duration of breastfeeding in rural Bangladeshi women. Am. J. Hum. Biol. 2006;18:630–638. doi: 10.1002/ajhb.20533. [DOI] [PubMed] [Google Scholar]
- 28.da Costa T.H., Haisma H., Wells J.C., Mander A.P., Whitehead R.G., Bluck L.J. How much human milk do infants consume? Data from 12 countries using a standardized stable isotope methodology. J. Nutr. 2010;140:2227–2232. doi: 10.3945/jn.110.123489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mao R., He J., Shao Z., Yarlagadda S.K., Zhu F. International Conference on Pattern Recognition. Springer; Berlin/Heidelberg, Germany: 2021. Visual aware hierarchy based food recognition; pp. 571–598. [Google Scholar]
- 30.Fang S., Shao Z., Kerr D.A., Boushey C.J., Zhu F. An end-to-end image-based automatic food energy estimation technique based on learned energy distribution images: Protocol and methodology. Nutrients. 2019;11:877. doi: 10.3390/nu11040877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang Y., He Y., Boushey C.J., Zhu F., Delp E.J. Context based image analysis with application in dietary assessment and evaluation. Multimed. Tools Appl. 2018;77:19769–19794. doi: 10.1007/s11042-017-5346-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.USDA Food and Nutrition Service Pregnancy and Birth to 24 Months. [(accessed on 24 May 2021)]; Available online: https://www.fns.usda.gov/resource/pregnancy-and-birth-24-months.
- 33.Raiten D.J., Raghavan R., Porter A., Obbagy J.E., Spahn J.M. Executive summary: Evaluating the evidence base to support the inclusion of infants and children from birth to 24 mo of age in the Dietary Guidelines for Americans—“the B-24 Project”. Am. J. Clin. Nutr. 2014;99:663S–691S. doi: 10.3945/ajcn.113.072140. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to ethical restrictions.