Abstract
Background
Elderly patients represent a high-risk group with increased risk of death from COVID-19. Despite the number of published studies, several unmet needs in care for older adults exist.
Objectives
To discuss unmet needs of COVID-19 in this special population.
Sources
A literature review for studies on COVID-19 in elderly patients published between December 2019 and November 2021 was performed. Clinical questions were formulated to guide the literature search. The search was conducted in the MEDLINE database, combining specific search terms. Two reviewers independently conducted the search and selected the studies according to the prespecified clinical questions.
Content
Elderly patients with COVID-19 have peculiar characteristics. They may have atypical clinical presentation, with no fever and with delirium or neurological manifestations as the most common signs, with potential delayed diagnosis and increased risk of death. The reported fatality rates among elderly patients with COVID-19 are extremely high. Several factors, including comorbidities, atypical presentation, and exclusion from intensive care unit care, contribute to this excess of mortality. Age alone is frequently used as a key factor to exclude the elderly from intensive care, but there is evidence that frailty rather than age better predicts the risk of poor outcome in this category. Durability of vaccine efficacy in the elderly remains debated, and the need for a third booster dose is becoming increasingly evident. Finally, efforts to care for elderly patients who have survived after acute COVID-19 should be implemented, considering the high rates of long COVID sequelae and the risk of longitudinal functional and cognitive decline.
Implications
We highlight peculiar aspects of COVID-19 in elderly patients and factors contributing to high risk of poor outcome in this category. We also illuminated gaps in current evidence, suggesting future research directions and underlining the need for further studies on the optimal management of elderly patients with COVID-19.
Keywords: COVID-19, Elderly, Frailty, Geriatric, Long COVID, Older, SARS-CoV-2, Vaccines
Introduction and rationale for the review
Since the start of the COVID-19 pandemic, elderly patients have been identified as one of the most vulnerable categories [1]. Several studies investigating this population have been published, but the currently available evidence provides contrasting and heterogeneous data.
Elderly patients with COVID-19 are known to present with atypical clinical features, such as delirium or neurological signs in the absence of fever or productive cough [2]. Moreover, the elderly are usually underrepresented in clinical trials, limiting current knowledge about their response to treatments and vaccines. Finally, criteria for deciding to forgo intensive care unit (ICU) care are not clear, and frequently age itself (and not performance status) is considered a key factor in whether to admit a patient to the ICU.
This paper aims to underline the peculiarity of COVID-19 in elderly patients and to discuss some critical points that clinicians should know when caring for this special population. The current evidence and its limitations have been summarized and implications for the future have been highlighted to guide the clinical research in this field.
Methods and sources
We reviewed the medical literature for studies on COVID-19 in the specific population of elderly patients, published between December 2019 and November 2021. This review is structured around the following clinical questions:
-
1.
What is the epidemiology of COVID-19 in elderly patients?
-
2.
Do elderly patients with COVID-19 have a peculiar clinical presentation?
-
3.
Do elderly patients with COVID-19 have a higher risk of mortality compared to younger ones?
-
4.
Does frailty affect access to care and the outcome of elderly patients?
-
5.
What are the knowledge gaps on the efficacy and safety of drugs to treat COVID-19 in elderly patients?
-
6.
What is the efficacy of vaccines in the elderly?
-
7.
What is the impact of long COVID-19 in the elderly?
The search was conducted in the MEDLINE database combining the following search terms: (COVID-19 OR SARS-CoV-2) AND (elderly OR older OR nursing home). Considering the huge number of published articles, we also added the filter ‘age≥65 years’. English language restriction was applied. Systematic reviews, meta-analyses, randomized clinical trials, and observational studies were considered. Case series and clinical cases were not included. Two reviewers independently conducted the search (VP and GT) and reviewed the studies. Any discrepancies were resolved by a third reviewer (MF). The reviewers conducted an initial screening of titles and abstracts of published articles and reviewed full articles to assess each study's eligibility for inclusion. A study was included if it was considered likely to provide valid and useful information and met the clinical questions previously discussed.
Epidemiology
Since the end of 2019, SARS-CoV-2 has caused over 6 million deaths worldwide, especially in the older population [3]. Epidemiological data on COVID-19 in elderly patients are heterogeneous across countries. The organization and resilience of healthcare systems, variations in aged populations in different countries, criteria to establish COVID-19–attributable deaths, and sociocultural practices for elderly care lead to substantial variability in reported data. Data from Europe showed that during the first wave of the pandemic, COVID-19 was responsible for 41.6% of deaths for men over 80 years of age [4]. Despite a reduction in COVID-19 mortality during the second wave, poor outcomes still remained high in this category of patients.
COVID-19 represents a challenge in nursing home/long-term care facilities (LTCF), which registered a disproportionally high number of deaths during the pandemic [5]. A study conducted in South Carolina showed that LTCF residents with COVID-19 were more likely to be hospitalized and die compared to older adults living in the community (hospitalization rates: 1953/7366 (26.5%) vs 7007/47 148 (14.9%); mortality rates: 1760/7366 (23.9%) vs 2839/47 148 [6%]) [6].
Epidemiology of COVID-19 in the elderly continues to change, according to restriction measures adopted by governments and vaccine access, and data need to be continually updated according to the spread of variants of concern (VOCs) all over the world.
Clinical presentation and risk of death
A growing number of studies have highlighted that elderly patients may have atypical clinical presentation [7], with fever occurring less frequently in older patients compared to younger ones [8]. Mounting evidence supports a high frequency of delirium and neuropsychiatric manifestations in this category of patients [9]. Confusion at hospital admission is significantly more common in COVID-19 patients ≥70 years old compared to younger ones (n = 30/152 (19.9%) vs n = 2/188 (1.1%); p < 0.001) [10], and in a recent meta-analysis conducted on 9031 patients with COVID-19 the prevalence of delirium was 28.2% (25/5490) in patients over 65 years old compared to 15.7% (12/3293) in younger adults [11]. The occurrence of delirium in elderly patients with COVID-19 has been associated with a mortality rate of 48.4% [11]. Other atypical presentations may include falls, generalized weakness, diminished food intake, changes in behaviour, malaise, and functional decline [12].
Accurate screening for typical and atypical symptoms of COVID-19 in elderly patients is crucial to avoid diagnostic errors both in the emergency department and in special contexts such as nursing homes or LTCFs [13]; the underreporting of symptoms in such structures contributes to a delayed diagnosis with consequent spread of the virus [13].
A meta-analysis including more than 600 000 individuals showed that mortality changes across age categories, ranging from 9.5% (8073/85 358) in patients 60 to 69 years old up to 29.6% (41 958/141 745) in those aged >80 years [1]. Table 1, Table 2 summarize mortality rates extrapolated from clinical studies conducted in elderly patients with COVID-19 and factors associated with poor outcome [[14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31]]. Among biomarkers of infection, an increase in procalcitonin values was associated with increased risk of hospital death in patients >75 years old, but not in younger ones [32]. Further studies are warranted to investigate patients' related factors and biomarkers independently associated with death in this population.
Table 1.
Reported mortality rates of elderly patients with COVID-19 from clinical studies
| Study | Design | Population | Period | No. | Mortality rates |
|---|---|---|---|---|---|
| Jung C [14] | Prospective | ICU pts ≥70 y old | March–December 2020 | 2625 | 30-d mortality: 42.6% first surge; 40.9% second surge 90-day mortality: 49.2% first surge; 59.7% second surge |
| Guillon A [15] | Cross-sectional | ICU pts ≥80 y old | March–May 2020 | 480 | ICU mortality: 62.5% 6-mo mortality: 72.1% |
| Aw D [16] | Retrospective | Pts ≥65 y old | March–April 2020 | 677 | 30-d mortality: 40.8% |
| Blomaard L [17] | Retrospective | Pts ≥70 y old | February–March 2020 | 1530 | In-hospital mortality: 38.4% |
| Singhal S [18] | Meta-analysis | Pts ≥60 y old | December 2019–May 2020 | 13 624 | Mortality: 11% (weighted pooled prevalence) |
| Covino M [19] | Prospective | Pts ≥80 y old | April 2020–March 2021 | 729 | In-hospital mortality: - 34.4% in pts 80–84 y old - 42% in pts 85–89 y old - 61.5% in pts 90–94 y old |
| Guo Y [20] | Retrospective | Pts >65 y old | December 2019–March 2020 | 14 238 | Case fatality ratio: 19.4% |
| Meis-Pinheiro U [21] | Retrospective | Residents in LTCF | March–April 2020 | 2092 | Mortality: 21.7% |
| Brill S [22] | Retrospective | Pts >80 y old (subgroup) | March–April 2020 | 150 | In-hospital mortality: 60% |
| Chinnadurai R [23] | Retrospective | Pts ≥65 y old (subgroup) | March–April 2020 | 150 | In-hospital mortality: - 65–75 y: 37% - 75–85 y: 53% - >85 y: 62% |
| Miles A [24] | Retrospective | Pts ≥70 y old | March–April 2020 | 217 | In-hospital mortality: 51.2% |
| Kundi H [25] | Nationwide cohort | Pts ≥65 y old | March–June 2020 | 18 234 | In-hospital mortality: 18.2% |
| Mendes A [26] | Retrospective | Pts ≥65 y old | March–April 2020 | 234 | In-hospital mortality: 32% |
| Owen R K [27] | Retrospective | Pts ≥65 y old | March–April 2020 | 285 | In-hospital mortality: 43% |
| Steinmeyer Z [28] | Retrospective | Older pts | March–May 2020 | 94 | In-hospital mortality: 18% |
| Blanc F [29] | Retrospective | Pts ≥65 y old | March–April 2020 | 89 | In-hospital mortality: 29.2% |
| Silva NJ [30] | Cross-sectional | Pts ≥60 y old (subgroup) | March–June 2020 | 12 925 | In-hospital mortality: 76.9% |
| Dres M [31] | Prospective | ICU pts >60 y old | February–May 2020 | 1199 | 28-d mortality 41% 60-d mortality 45% 90-d mortality 46% |
ICU, intensive care unit; pts, patients.
Table 2.
Potential reasons explaining the higher risk of poor outcomes in elderly patients with COVID-19
| Factors | Consequences |
|---|---|
| Comorbidities |
|
| Ageing |
|
| Atypical clinical presentation |
|
| Exclusion of elderly patients from ICU |
|
| Underrepresentation of elderly in RCTs |
|
ICU, intensive care unit; RCT, randomized clinical trial.
The highest mortality rates (40%–80%) are reported in elderly patients admitted to the ICU [14,15,31]. Because of this finding, some intensivists were initially discouraged from admitting elderly patients to the ICU and used age as an exclusion criterion for ICU care [33]. This choice was justified by ethical consideration to prioritize younger patients in a time of reduced ICU capacity. However, an interesting study by the COVIP group unexpectedly showed that elderly patients admitted to the ICU during the second wave had higher short- and long-term mortality compared to the first wave [14]. Among the other potential explanations, the worse outcome might have been caused by the increased length of time spent in other departments before ICU admission, a hypothesis supported by decreased PaO2/FiO2 ratio at ICU admission in the second period [14]. Specific parameters to take into consideration for deciding whether an elderly patient should be admitted to ICU are discussed in the following.
Impact of frailty on access to intensive care and outcome
The mortality rate associated with COVID-19 is directly related to the classes of age of patients [19]. However, age alone is not a good predictor of survival when other factors such as frailty, comorbidity, gender, and disease severity are considered [19]. Several studies have showed that in elderly patients, outcomes are better predicted by frailty, using a clinical frailty scale (CFS), than by age itself [[34], [35], [36]]. The UK National Institute for Health and Care Excellence has advocated the use of CFS in clinical decisions in patients aged ≥65 years with COVID-19 [37]. In the context of COVID-19, a score of 1 to 3 is considered a lower risk of mortality, a score of 4 to 5 moderate risk, and a score of 6 to 9 high risk [38]. A recent meta-analysis showed that each one-point increase in CFS is associated with a 12% increase in mortality [39]. Therefore, it should be considered that mildly frail older adults may still have enough intrinsic capacity to withstand the stressors of hospitalization and make a good recovery; in patients at intermediate risk, an individualized evaluation is necessary.
Unfortunately, an internet-based survey showed that the main reason to exclude patients from ICU care was an individual decision by an intensivist, whilst comorbidity scores, such as CFS, were not used by the majority of clinicians [40]. The allocation of patients based only on age may generate ethical concerns, and age should not be the only determining factor in ICU triage decisions.
Efficacy of therapy specifically directed against SARS-COV-2
Some therapeutic strategies may have peculiar effects and are usually associated with increased risk of side effects in elderly patients. A recent study including patients with a median age of 69 years suggests that remdesivir is efficacious in preventing the progression of disease if administered within 5 days from the onset of symptoms [41]. Remdesivir demonstrated good safety in patients >80 years old [42], but some conditions, such as renal kidney disease, may represent common contraindications to use of this antiviral in elderly patients [43]. Although studies on the convalescent plasma against SARS-CoV-2 in adult patients are not fully conclusive [44], an RCT demonstrated that early administration of high-titre convalescent plasma in mildly ill older adults reduced the progression of COVID-19 [45]. Monoclonal antibodies (mAbs) showed efficacy in reducing the risk of disease progression and death and are now recommended in both outpatients and hospitalized patients with negative serology [46]. Although mAbs represent a promising therapeutic option, no data in elderly patients are available. Of note, some are not efficient against new variants (i.e. casirivimab/imdevimab is effective against Delta but loses its effectiveness against Omicron, unlike sotrovimab) [47].
Dexamethasone has been established as the standard of care in patients with severe COVID-19, but data in the elderly are controversial. The RECOVERY trial showed no effect of dexamethasone in the subgroup of patients >70 years of age [48]. Moreover, a secondary analysis of the COVIP study conducted in critically ill elderly patients with COVID-19 found an independent association of steroid use with increased mortality [49]. Conversely, corticosteroids were associated with a significant increase in overall survival at day 14 in patients aged >80 years hospitalized for severe COVID-19 in a recent study conducted in 36 hospitals in France and Luxembourg [50]. Hyperglycaemia is a potentially dangerous effect of steroid therapy and may be associated with poor outcome [51]. The available data suggest using steroids according to disease severity and comorbidities, with strict monitoring of potential adverse effects in the elderly.
Anticytokine antibodies such as tocilizumab were demonstrated to be an effective and safe therapeutic option in elderly patients with severe COVID-19, also in combination with steroids [52]. However, elderly patients treated with these drugs should be carefully monitored during the postdischarge phase because of a higher vulnerability to superinfections [53]. The dosage of low-molecular-weight heparin should be balanced according to the individual risk of bleeding in these patients [54]. Finally, antibiotic therapy should not be systematically prescribed on admission as initial bacterial pulmonary coinfections are rare. A study in elderly patients with COVID-19 pneumonia showed that early antibiotic treatment was not associated with decreased in-hospital mortality [55].
The lack of knowledge about the efficacy and safety of these treatments in elderly patients is also a consequence of their underrepresentation in clinical trials [56]. Major barriers for their inclusion in clinical trials are the comorbidities and cognitive disorders highly prevalent in these patients.
Efficacy of vaccines
There is general consensus that the elderly represent a high-risk group that should be offered vaccination with priority. However, compared to younger individuals, antibody response after vaccination is generally lower because of a gradual deterioration of the immune system with age, and neutralizing antibody immune response after vaccination declines more precipitously in elderly individuals [57]. Thus, the following knowledge gaps exist in vaccination in elderly individuals:
-
1.
The efficacy of vaccines in elderly compared to younger adults, especially against VOCs;
-
2.
The durability of immune response after a booster dose of vaccine; and
-
3.
The need for further booster doses.
With regard to the efficacy of vaccination in elderly patients, contrasting data emerged from the literature (Table 3 ) [[58], [59], [60], [61], [62], [63]]. Phase II and III studies are limited by small sample sizes, exclusion of older people with frailty, and a relatively short follow-up. Real-world data from LTCF residents confirmed that mRNA vaccines had an estimated effectiveness of 71%, 88%, and 97% against SARS-CoV-2 infection, COVID-19 hospitalization, and death, respectively [64]. More specifically, the proportion of vaccinated patients with SARS-CoV-2 infection from the total number of infected patients was 292 of 8379 (3.5%), the proportion of vaccinated patients who were hospitalized from the total number of patients with COVID-19 who were hospitalized was 49 of 2509 (2%), and the proportion of vaccinated patients with COVID-19 who died compared with the total number of patients with COVID-19 who died was 16 of 1602 (1%).
Table 3.
Data from phase I–II and III studies on COVID-19 vaccines in the elderly
| Vaccine (type) | Phase I and II studies in the elderly | Phase III inclusion criteria | Phase III exclusion criteria | Proportion of elderly in phase III | Limitations |
|---|---|---|---|---|---|
| Pfizer/BioNTech BNT162b2 (mRNA) [58,61] |
Phase I clinical study showed that the GMT after the second dose was 149 in patients 65–85 y old | Adults ≥16 y old Healthy or with stable medical conditions |
Immunosuppressive therapy, or immunocompromising condition | 42% ≥ 55 y old | Low sample size of phase I and II studies Underrepresentation of elderly and patients with frailty Relatively short follow-up No data about VOCs |
| Moderna mRNA-1273 (mRNA) [60,62] | Phase II clinical study in patients >55 yold showed that antibody response of elderly was similar to that observed in younger people | Adults ≥18 y old Increased risk of SARS-CoV-2 infection |
Immunosuppressive therapy, or immunocompromising condition | 24.8% ≥ 65 y old | |
| AstraZeneca AZD-1222 (adenovirus vector) [59,63] | Analysis of a phase II study showed that neutralizing antibody titres were similar across all age groups | Adults ≥18 y old Increased risk of SARS-CoV-2 infection Healthy or stable medical condition |
Immunosuppressive or immunodeficient state Significant disease |
22.4% ≥ 65 y old |
However, a recent study showed a nonlinear relationship between age and immune response after the BNT162b2 vaccine, with a marked drop around the age of 80 years [57]. After the first dose, the geometric mean neutralization titre was lower in participants aged ≥80 years than in younger individuals (48.2 vs 104.1; p = 0.004). When individuals aged 80 years or more were tested between 3 and 12 weeks after their first dose, around half showed no evidence of neutralization [57]. Moreover, compared to the latter, patients ≥80 years old had a lower neutralizing activity to P.1 and B.1.1.7 variants [57].
In a study from Israel involving participants ≥60 years old, the rates of confirmed COVID-19 and severe illness were substantially lower (by a factor of 11.3% and 19.5%, respectively) among those who received a third booster dose of the BNT162b2 vaccine compared to the nonbooster group [65]. Current data suggest efficacy of mRNA-based COVID-19 vaccine boosters against the B.1.1.529 variant (Omicron) [66], but data on elderly are limited.
Long covid
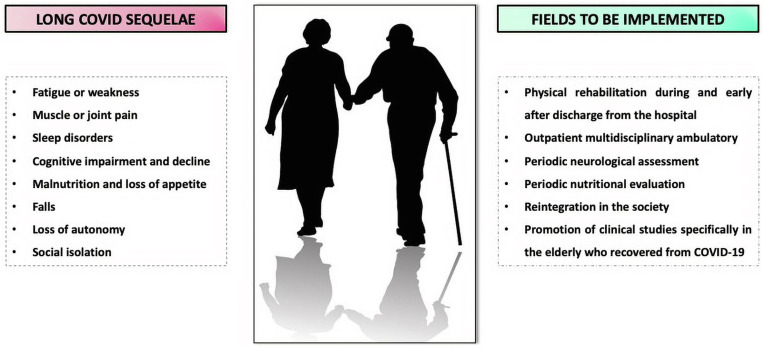
Several studies confirmed the presence of persistent symptoms after acute COVID-19, a condition known as long COVID, post-COVID, or long-haul COVID [67]. Long COVID in the elderly may include a huge spectrum of manifestations, ranging from cognitive decline to altered nutritional status (Fig. 1 ). In a large observational study, 76% (1265/1655) of patients reported long COVID symptoms [67]. In another study, 1095 of 2433 (45%) reported at least one symptom at 1-year follow-up, and older age was one of the strongest risk factors for reporting at least three symptoms [68]. Of note, 83% (137/165) of recovered elderly patients reported at least one persistent symptom, with fatigue as the most prevalent [69]. An increased risk of long-term cognitive decline after COVID-19 has been described in elderly individuals, particularly in patients recovered from severe COVID-19, among whom 59% (141/238) reported cognitive decline [70].
Fig. 1.
Long COVID sequelae frequently reported in the elderly and actions to be implemented.
Some aspects of COVID-19 sequelae in elderly patients remain unknown, with ongoing studies evaluating the decline of respiratory function 1 year or more after COVID-19 pneumonia and changes in the functional status of elderly patients with COVID-19 after discharge from the ICU.
Implication for patient management and future research
Management of elderly patients with COVID-19 is becoming increasingly diverse and complex, in relation to the spread of VOC, reduced vaccine response, and availability of early immunotherapy and new antivirals. Available data are sparse and not sufficient to delineate a tailored management of elderly patients with COVID-19. Importantly, there are few and contrasting data on the efficacy and safety of treatments currently used against COVID-19 in this special population. Although our understanding is still evolving, some treatments currently used against COVID-19, such as steroids, have a high risk of side effects in elderly patients; alternative strategies, including early immunotherapy (e.g. mAbs) and anticytokine antibodies (e.g. tocilizumab), should be preferred in mild-to-moderate and severe COVID-19, respectively. Occurrence of adverse events should be carefully monitored in these patients.
Because this is not a systematic review, some limitations should be acknowledged. The determination of which studies to include and the conclusions may be subjective; no assessment of the quality of evidences has been performed; and selection bias and subjective weighting of the included studies may have occurred.
Future research should focus on specific therapeutic approaches and factors associated with survival to better allocate patients, maximizing their opportunity of clinical success. A more effective regulatory framework to ensure equitable inclusion of elderly patients in research is clearly needed. For high-quality trials, some authors have brought to light the need for creating a national network of skilled facilities engaged in interventional clinical trials. Logistic challenges may be overcome, implementing dedicated skilled staff and facilitating the consent procedures and methods for obtaining biospecimen and clinical data.
Transparency declaration
The authors have nothing to disclose. There was no funding.
Author contributions
VP and GT revised the literature and wrote the manuscript; MF revised the final manuscript and supervised the activities.
Editor: Sally J. Cutler
References
- 1.Bonanad C., García-Blas S., Tarazona-Santabalbina F., Sanchis J., Bertomeu-González V., Fácila L., et al. The effect of age on mortality in patients with Covid-19: a meta-analysis with 611,583 subjects. J Am Med Dir Assoc. 2020;21:915–918. doi: 10.1016/j.jamda.2020.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kennedy M., Helfand B.K.I., Gou R.Y., Gartaganis S.L., Webb M., Moccia J.M., et al. Delirium in older patients with COVID-19 presenting to the Emergency Department. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.29540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO Weekly epidemiological update on COVID-19. 2021. https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---22-march-2022 Available at:
- 4.Olabi B., Bagaria J., Bhopal S.S., Curry G.D., Villarroel N., Bhopal R. Population perspective comparing COVID-19 to all and common causes of death during the first wave of the pandemic in seven European countries. Public Health Pract (Oxf) 2021;2:100077. doi: 10.1016/j.puhip.2021.100077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Knock E.S., Whittles L.K., Lees J.A., Perez-Guzman P.N., Verity R., FitzJohn R.G., et al. Key epidemiological drivers and impact of interventions in the 2020 SARS-CoV-2 epidemic in England. Sci Transl Med. 2021;13 doi: 10.1126/scitranslmed.abg4262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Resciniti N.V., Fuller M., Sellner J., Lohman M.C. COVID-19 incidence and mortality among long-term care facility residents and staff in South Carolina. J Am Med Dir Assoc. 2021;22:2026–2031.e1. doi: 10.1016/j.jamda.2021.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lian J., Jin X., Hao S., Cai H., Zhang S., Zheng L., et al. Analysis of epidemiological and clinical features in older patients with Coronavirus Disease 2019 (COVID-19) outside Wuhan. Clin Infect Dis. 2020;71:740–747. doi: 10.1093/cid/ciaa242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pepe M., Maroun-Eid C., Romero R., Arroyo-Espliguero R., Arroyo-Espliguero R., Fernàndez-Rozas I., et al. Clinical presentation, therapeutic approach, and outcome of young patients admitted for COVID-19, with respect to the elderly counterpart. Clin Exp Med. 2021;21:249–268. doi: 10.1007/s10238-021-00684-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zazzara M.B., Penfold R.S., Roberts A.L., Lee K.A., Dooley H., Sudre C.H., et al. Probable delirium is a presenting symptom of COVID-19 in frail, older adults: a cohort study of 322 hospitalised and 535 community-based older adults. Age Ageing. 2021;50:40–48. doi: 10.1093/ageing/afaa223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gómez-Belda A.B., Fernández-Garcés M., Mateo-Sanchis E., Madrazo M., Carmona M., Piles-Roger L., et al. COVID-19 in older adults: what are the differences with younger patients? Geriatr Gerontol Int. 2021;21:60–65. doi: 10.1111/ggi.14102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shao S.C., Lai C.C., Chen Y.H., Chen Y.C., Hung M.J., Liao S.C. Prevalence, incidence and mortality of delirium in patients with COVID-19: a systematic review and meta-analysis. Age Ageing. 2021;50:1445–1453. doi: 10.1093/ageing/afab103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ohuabunwa U., Turner J., Johnson T. Atypical presentations among older adults with COVID-19 disease: a need for broadening the differential diagnosis. Gerontol Geriatr Med. 2021;7 doi: 10.1177/2333721421999313. 2333721421999313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van den Besselaar J.H., Sikkema R.S., Koene F.M.H.P.A., van Buul L.W., Oude Munnink B.B., Frénay I., et al. Are presymptomatic SARS-CoV-2 infections in nursing home residents unrecognised symptomatic infections? Sequence and metadata from weekly testing in an extensive nursing home outbreak. Age Ageing. 2021;50:1454–1463. doi: 10.1093/ageing/afab081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jung C., Fjølner J., Bruno R.R., Wernly B., Artigas A., Bollen Pinto B., et al. Differences in mortality in critically ill elderly patients during the second COVID-19 surge in Europe. Crit Care. 2021;25:344. doi: 10.1186/s13054-021-03739-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guillon A., Laurent E., Godillon L., Kimmoun A., Grammatico-Guillon L. Long-term mortality of elderly patients after intensive care unit admission for COVID-19. Intensive Care Med. 2021;47:710–712. doi: 10.1007/s00134-021-06399-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aw D., Woodrow L., Ogliari G., Harwood R. Association of frailty with mortality in older inpatients with Covid-19: a cohort study. Age Ageing. 2020;49:915–922. doi: 10.1093/ageing/afaa184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blomaard L.C., van der Linden C.M.J., van der Bol J.M., Jansen S.W.M., Polinder-Bos H.A., Willems H.C., et al. Frailty is associated with in-hospital mortality in older hospitalised COVID-19 patients in The Netherlands: the COVID-OLD study. Age Ageing. 2021;50:631–640. doi: 10.1093/ageing/afab018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singhal S., Kumar P., Singh S., Saha S., Dey A.B. Clinical features and outcomes of COVID-19 in older adults: a systematic review and meta-analysis. BMC Geriatr. 2021;21:321. doi: 10.1186/s12877-021-02261-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Covino M., Russo A., Salini S., De Matteis G., Simeoni B., Della Polla D., et al. Frailty assessment in the emergency department for risk stratification of COVID-19 patients aged ≥80 years. J Am Med Dir Assoc. 2021;22:1845–18452.e1. doi: 10.1016/j.jamda.2021.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guo Y., Liu X., Deng M., Liu P., Li F., Xie N., et al. Epidemiology of COVID-19 in older persons, Wuhan, China. Age Ageing. 2020;49:706–712. doi: 10.1093/ageing/afaa145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meis-Pinheiro U., Lopez-Segui F., Walsh S., Ussi A., Santaeugenia S., Garcia-Navarro J.A., et al. Clinical characteristics of COVID-19 in older adults. A retrospective study in long-term nursing homes in Catalonia. PLoS One. 2021;16 doi: 10.1371/journal.pone.0255141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brill S.E., Jarvis H.C., Ozcan E., Burns T.L.P., Warraich R.A., Amani L.J., et al. COVID-19: a retrospective cohort study with focus on the over-80s and hospital-onset disease. BMC Med. 2020;18:194. doi: 10.1186/s12916-020-01665-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chinnadurai R., Ogedengbe O., Agarwal P., Money-Coomes S., Abdurrahman A.Z., Mohammed S., et al. Older age and frailty are the chief predictors of mortality in COVID-19 patients admitted to an acute medical unit in a secondary care setting- a cohort study. BMC Geriatr. 2020;20:409. doi: 10.1186/s12877-020-01803-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miles A., Webb T.E., Mcloughlin B.C., Mannan I., Rather A., Knopp P., et al. Outcomes from COVID-19 across the range of frailty: excess mortality in fitter older people. Eur Geriatr Med. 2020;11:851–855. doi: 10.1007/s41999-020-00354-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kundi H., Çetin E.H.Ö., Canpolat U., Aras S., Celik O., Ata N., et al. The role of frailty on adverse outcomes among older patients with COVID-19. J Infect. 2020;81:944–951. doi: 10.1016/j.jinf.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mendes A., Serratrice C., Herrmann F.R., Genton L., Périvier S., Scheffler M., et al. Predictors of in-hospital mortality in older patients with COVID-19: the COVID age study. J Am Med Dir Assoc. 2020;21:1546–1554.e3. doi: 10.1016/j.jamda.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Owen R.K., Conroy S.P., Taub N., Jones W., Bryden D., Pareek M., et al. Comparing associations between frailty and mortality in hospitalised older adults with or without COVID-19 infection: a retrospective observational study using electronic health records. Age Ageing. 2021;50:307–316. doi: 10.1093/ageing/afaa167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Steinmeyer Z., Vienne-Noyes S., Bernard M., Steinmeyer A., Balardy L., Piau A., et al. Acute care of older patients with COVID-19: clinical characteristics and outcomes. Geriatrics (Basel) 2020;5:65. doi: 10.3390/geriatrics5040065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blanc F., Waechter C., Vogel T., Schorr B., Demuynck C., Hunyadi C.M., et al. Therapeutic prevention of COVID-19 in elderly: a case-control study. Geroscience. 2021;43:2333–2343. doi: 10.1007/s11357-021-00397-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Silva N.J., Ribeiro-Silva R.C., Ferreira A.J.F., Teixeira C.S.S., Rocha A.S., Alves F.J.O., et al. Combined association of obesity and other cardiometabolic diseases with severe COVID-19 outcomes: a nationwide cross-sectional study of 21 773 Brazilian adult and elderly inpatients. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2021-050739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dres M., Hajage D., Lebbah S., Kimmoun A., Pham T., Béduneau G., et al. Characteristics, management, and prognosis of elderly patients with COVID-19 admitted in the ICU during the first wave: insights from the COVID-ICU study: prognosis of COVID-19 elderly critically ill patients in the ICU. Ann Intensive Care. 2021;11:77. doi: 10.1186/s13613-021-00861-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ticinesi A., Nouvenne A., Prati B., Guida L., Parise A., Cerundolo N., et al. The clinical significance of procalcitonin elevation in patients over 75 years old admitted for COVID-19 pneumonia. Mediators Inflamm. 2021;2021:5593806. doi: 10.1155/2021/5593806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Haas L.E.M., de Lange D.W., van Dijk D., van Delden J.J.M. Should we deny ICU admission to the elderly? Ethical considerations in times of COVID-19. Crit Care. 2020;24:321. doi: 10.1186/s13054-020-03050-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hewitt J., Carter B., Vilches-Moraga A., Quinn T.J., Braude P., Verduri A., et al. The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study. Lancet Public Health. 2020;5:e444–e451. doi: 10.1016/S2468-2667(20)30146-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sprung C.L., Joynt G.M., Christian M.D., Truog R.D., Rello J., Nates J.L. Adult ICU triage during the coronavirus disease 2019 pandemic: who will live and who will die? Recommendations to improve survival. Crit Care Med. 2020;48:1196–1202. doi: 10.1097/CCM.0000000000004410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jung C., Flaatten H., Fjølner J., Bruno R.R., Wernly B., Artigas A., et al. The impact of frailty on survival in elderly intensive care patients with COVID-19: the COVIP study. Crit Care. 2021;25:149. doi: 10.1186/s13054-021-03551-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.National Institute for Health and Care Excellence COVID-19 rapid guideline: managing COVID-19. https://www.nice.org.uk/guidance/ng191 [PubMed]
- 38.Kastora S., Kounidas G., Perrott S., Carter B., Hewitt J., Myint P.K. Clinical frailty scale as a point of care prognostic indicator of mortality in COVID-19: a systematic review and meta-analysis. EClinicalMedicine. 2021;36:100896. doi: 10.1016/j.eclinm.2021.100896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pranata R., Henrina J., Lim M.A., Lawrensia S., Yonas E., Vania R., et al. Clinical frailty scale and mortality in COVID-19: a systematic review and dose-response meta-analysis. Arch Gerontol Geriatr. 2021;93:104324. doi: 10.1016/j.archger.2020.104324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tiseo G., Yahav D., Paul M., Tinelli M., Gavazzi G., Mussini C., et al. What have we learned from the first to the second wave of COVID-19 pandemic? An international survey from the ESCMID Study Group for Infection in the Elderly (ESGIE) group. Eur J Clin Microbiol Infect Dis. 2022;41:281–288. doi: 10.1007/s10096-021-04377-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Falcone M., Suardi L.R., Tiseo G., Barbieri C., Giusti L., Galfo V., et al. Early use of remdesivir and risk of disease progression in hospitalized patients with mild to moderate COVID-19. Clin Ther. 2022 doi: 10.1016/j.clinthera.2022.01.007. S0149-2918(22)00012-1. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kanai O., Fujita K., Nanba K., Esaka N., Hata H., Seta K., et al. Safety of remdesivir for patients 80 years of age or older with Coronavirus Disease 2019 (COVID-19) Drugs Aging. 2021;38:1067–1074. doi: 10.1007/s40266-021-00908-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Remdesivir (Veklury®) prescribing information. Gilead Sciences, Inc.; Foster City, CA: 2022. https://www.gilead.com/-/media/files/pdfs/medicines/covid-19/veklury/veklury_pi.pdf Updated January. [Google Scholar]
- 44.Menichetti F., Popoli P., Puopolo M., Spila Alegiani S., Tiseo G., Bartoloni A., et al. Effect of high-titer convalescent plasma on progression to severe respiratory failure or death in hospitalized patients with COVID-19 pneumonia: a randomized clinical trial. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.36246. Erratum in: JAMA Netw Open 2021;4:e2144236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Libster R., Pérez Marc G., Wappner D., Coviello S., Bianchi A., Braem V., et al. Early high-titer plasma therapy to prevent severe Covid-19 in older adults. N Engl J Med. 2021;384:610–618. doi: 10.1056/NEJMoa2033700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Falcone M., Tiseo G., Valoriani B., Barbieri C., Occhineri S., Mazzetti P., et al. Efficacy of bamlanivimab/etesevimab and casirivimab/imdevimab in preventing progression to severe COVID-19 and role of variants of concern. Infect Dis Ther. 2021;10:2479–2488. doi: 10.1007/s40121-021-00525-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hoffmann M., Krüger N., Schulz S., Cossmann A., Rocha C., Kempf A., et al. The Omicron variant is highly resistant against antibody-mediated neutralization: implications for control of the COVID-19 pandemic. Cell. 2022;185:447–456. doi: 10.1016/j.cell.2021.12.032. e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.RECOVERY Collaborative Group. Horby P., Lim W.S., Emberson J.R., Mafham M., Bell J.L., Linsell L., et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jung C., Wernly B., Fjølner J., Bruno R.R., Dudzinski D., Artigas A., et al. Steroid use in elderly critically ill COVID-19 patients. Eur Respir J. 2021;58:2100979. doi: 10.1183/13993003.00979-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gallay L., Tran V.T., Perrodeau E., Vignier N., Mahevas M., Bisio F., et al. Fourteen-day survival among older adults with severe infection with severe acute respiratory syndrome Coronavirus 2 treated with corticosteroid: a cohort study. Clin Microbiol Infect. 2021;27:1145–1150. doi: 10.1016/j.cmi.2021.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Coppelli A., Giannarelli R., Aragona M., Penno G., Falcone M., Tiseo G., et al. Hyperglycemia at hospital admission is associated with severity of the prognosis in patients hospitalized for COVID-19: the Pisa COVID-19 study. Diabetes Care. 2020;43:2345–2348. doi: 10.2337/dc20-1380. [DOI] [PubMed] [Google Scholar]
- 52.Duarte-Millán M.A., Mesa-Plaza N., Guerrero-Santillán M., Morales-Ortega A., Bernal-Bello D., Farfán-Sedano A.I., et al. Prognostic factors and combined use of tocilizumab and corticosteroids in a Spanish cohort of elderly COVID-19 patients. J Med Virol. 2022;94:1540–1549. doi: 10.1002/jmv.27488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Falcone M., Tiseo G., Giordano C., Leonildi A., Menichini M., Vecchione A., et al. Predictors of hospital-acquired bacterial and fungal superinfections in COVID-19: a prospective observational study. J Antimicrob Chemother. 2021;76:1078–1084. doi: 10.1093/jac/dkaa530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Falcone M., Tiseo G., Barbieri G., Galfo V., Russo A., Virdis A., et al. Role of low-molecular-weight heparin in hospitalized patients with Severe Acute Respiratory Syndrome Coronavirus 2 pneumonia: a prospective observational study. Open Forum Infect Dis. 2020;7:ofaa563. doi: 10.1093/ofid/ofaa563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Putot A., Bouiller K., Laborde C., Gilis M., Févre A., Hacquin A., et al. Association between early antibiotic therapy and in-hospital mortality among older patients with SARS-CoV-2 pneumonia. J Gerontol A Biol Sci Med Sci. 2021:glab209. doi: 10.1093/gerona/glab209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Prendki V., Tau N., Avni T., Falcone M., Huttner A., Kaiser L., et al. A systematic review assessing the under-representation of elderly adults in COVID-19 trials. BMC Geriatr. 2020;20:538. doi: 10.1186/s12877-020-01954-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Collier D.A., Ferreira I.A.T.M., Kotagiri P., Datir R.P., Lim E.Y., Touizer E., et al. Age-related immune response heterogeneity to SARS-CoV-2 vaccine BNT162b2. Nature. 2021;596:417–422. doi: 10.1038/s41586-021-03739-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Polack F.P., Thomas S.J., Kitchin N., Absalon J., Gurtman A., Lockhart S., et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Falsey A.R., Sobieszczyk M.E., Hirsch I., Sproule S., Robb M.L., Corey L., et al. Phase 3 safety and efficacy of AZD1222 (ChAdOx1 nCoV-19) covid-19 vaccine. N Engl J Med. 2021;385:2348–2360. doi: 10.1056/NEJMoa2105290. NEJMoa2105290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Baden L.R., El Sahly H.M., Essink B., Kotloff K., Frey S., Novak R., et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384:403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Walsh E.E., Frenck R.W., Jr., Falsey A.R., Kitchin N., Absalon J., Gurtman A., et al. Safety and immunogenicity of two RNA-based Covid-19 vaccine candidates. N Engl J Med. 2020;383:2439–2450. doi: 10.1056/NEJMoa2027906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Anderson E.J., Rouphael N.G., Widge A.T., Jackson L.A., Roberts P.C., Makhene M., et al. Safety and immunogenicity of SARS-CoV-2 mRNA-1273 vaccine in older adults. N Engl J Med. 2020;383:2427–2438. doi: 10.1056/NEJMoa2028436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ramasamy M.N., Minassian A.M., Ewer K.J., Flaxman A.L., Folegatti P.M., Owens D.R., et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, phase 2/3 trial. Lancet. 2021;396:1979–1993. doi: 10.1016/S0140-6736(20)32466-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mazagatos C., Monge S., Olmedo C., Vega L., Gallego P., Martín-Merino E., et al. Effectiveness of mRNA COVID-19 vaccines in preventing SARS-CoV-2 infections and COVID-19 hospitalisations and deaths in elderly long-term care facility residents, Spain, weeks 53 2020 to 13 2021. Euro Surveill. 2021;26:2100452. doi: 10.2807/1560-7917.ES.2021.26.24.2100452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bar-On Y.M., Goldberg Y., Mandel M., Bodenheimer O., Freedman L., Kalkstein N., et al. Protection of BNT162b2 vaccine booster against Covid-19 in Israel. N Engl J Med. 2021;385:1393–1400. doi: 10.1056/NEJMoa2114255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Garcia-Beltran W.F., St Denis K.J., Hoelzemer A., Lam E.C., Nitido A.D., Sheehan M.L., et al. mRNA-based COVID-19 vaccine boosters induce neutralizing immunity against SARS-CoV-2 Omicron variant. Cell. 2022;185:457–466. doi: 10.1016/j.cell.2021.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Huang C., Huang L., Wang Y., Li X., Ren L., Gu X., et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397:220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhang X., Wang F., Shen Y., Zhang X., Cen Y., Wang B., et al. Symptoms and health outcomes among survivors of COVID-19 infection 1 year after discharge from hospitals in Wuhan, China. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.27403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tosato M., Carfì A., Martis I., Pais C., Ciciarello F., Rota E., et al. Prevalence and predictors of persistence of COVID-19 symptoms in older adults: a single-center study. J Am Med Dir Assoc. 2021;22:1840–1844. doi: 10.1016/j.jamda.2021.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Liu Y.H., Wang Y.R., Wang Q.H., Chen Y., Chen X., Li Y., et al. Post-infection cognitive impairments in a cohort of elderly patients with COVID-19. Mol Neurodegener. 2021;16:48. doi: 10.1186/s13024-021-00469-w. [DOI] [PMC free article] [PubMed] [Google Scholar]