Abstract
Introduction
It is unknown how the COVID-19 pandemic has affected the care of vulnerable chronic hemodialysis (HD) patients across regions, particularly in low and lower-middle income countries (LLMICs). We aimed to identify global inequities in HD care delivery during the COVID-19 pandemic.
Methods
The ISN and the Dialysis Outcomes and Practice Patterns Study (DOPPS) conducted a global online survey of HD units between March and November, 2020, to ascertain practice patterns and access to resources relevant to HD care during the COVID-19 pandemic. Responses were categorized according to World Bank income classification for comparisons.
Results
Surveys were returned from 412 facilities in 78 countries: 15 (4%) in low-income countries (LICs), 111 (27%) in lower-middle income countries (LMICs), 145 (35%) in upper-middle income countries (UMICs), and 141 (34%) in high-income countries (HICs). Respondents reported that diagnostic tests for SARS-CoV-2 were unavailable or of limited availability in LICs (72%) and LMICs (68%) as compared with UMICs (33%) and HICs (20%). The number of patients who missed HD treatments was reported to have increased during the COVID-19 pandemic in LICs (64%) and LMICs (67%) as compared with UMICs (31%) and HICs (6%). Limited access to HD, intensive care unit (ICU) care, and mechanical ventilation among hospitalized patients on chronic dialysis with COVID-19 were also reportedly higher in LICs and LMICs as compared with UMICs and HICs. Staff in LLMICs reported less routine testing for SARS-CoV-2 when asymptomatic as compared with UMICs and HICs—14% in LICs and 11% in LMICs, compared with 26% and 28% in UMICs and HICs, respectively. Severe shortages of personal protective equipment (PPE) were reported by the respondents from LICs and LMICs compared with UMICs and HICs, especially with respect to the use of the N95 particulate-air respirator masks.
Conclusion
Striking global inequities were identified in the care of chronic HD patients during the pandemic. Urgent action is required to address these inequities which disproportionately affect LLMIC settings thereby exacerbating pre-existing vulnerabilities that may contribute to poorer outcomes.
Keywords: advocacy, chronic hemodialysis, COVID-19, inequity, kidney failure, nephrology
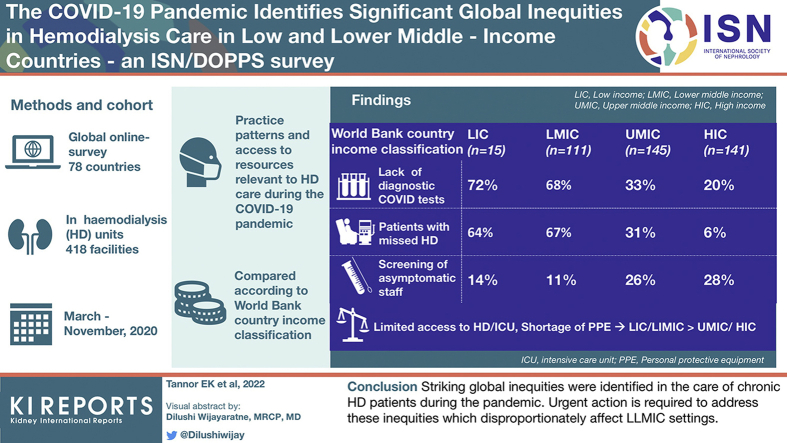
Graphical abstract
The COVID-19 pandemic has had a devastating global impact on health care delivery,1,2 disproportionally affecting LLMICs as a result of longstanding insufficient health care investment, relatively poor health care infrastructure, and low numbers of skilled health care workers.3, 4, 5 The delivery of kidney replacement therapy, and in particular HD, has been particularly challenging during this unprecedented period.6
The mortality related to SARS-CoV-2 infections in patients with kidney failure receiving kidney replacement therapies (dialysis and kidney transplantation) has been significantly higher than the mortality in the general population, ranging from 10% to 41%.7, 8, 9, 10, 11, 12, 13 The risk of COVID-19 infection is particularly high in the HD population, owing to the need for frequent visits to health care settings for treatments, inability to maintain social distancing during transportation, and dialysis sessions in some dialysis units.6,7,14,15
Intrinsically fragile health care systems, lack of diagnostic testing for SARS-CoV-2, low staff numbers with high rates of staff sickness during the pandemic, and shortage of PPE have challenged LLMICs since the beginning of the pandemic. In addition, increased costs needed for the implementation of protocols, transportation barriers caused by lockdowns and, health care professional burnout have potentiated the duration and magnitude of the effect of the pandemic on dialysis services.16,17
COVID-19 infection guidelines have been drawn up by various organizations including the Centers for Disease Control and Prevention, the European Renal Association—European Dialysis and Transplant Association, and the United Kingdom Renal Association to guide clinicians to optimize patient and staff safety, prevent SARS-CoV-2 infection, and manage patients with COVID-19 on HD.18, 19, 20, 21 In addition, the African Association of Nephrology published recommendations with a focus on LLMIC settings in Africa.20 Successful implementation of such guidelines has been dependent on availability of the required resources and infrastructure, including but not limited to SARS-CoV-2 testing facilities, adequate PPE for staff and patients, and isolation rooms within HD units for management of patients diagnosed with COVID-19. The provision of adequate resources to implement these guidelines set against chronically underfunded health care systems may be a significant challenge in many LLMICs.3
Inequities in health care delivery for patients with kidney failure on HD in LLMICs as compared with UMICs and HICs are likely to have been worsened by the COVID-19 pandemic. Data on such inequities will be important to advocate for directed improvements in HD care during and after the pandemic for better outcomes in the population living with kidney failure. To the best of our knowledge, no study has systematically collected information on the ground across all income groups globally to support these assumptions. As such, the ISN and the DOPPS undertook an online survey to better understand the global challenges and inequities in HD care delivery consequent to the COVID-19 pandemic. The main objective of the present work was to describe global inequities in care of chronic HD patients according to the income status based on World Bank classification as a tool for advocacy and change.
Methods
A survey to assess the impact of COVID-19 on dialysis services was developed by DOPPS and ISN investigators and administered in May to June 2020 to medical directors at sites participating in DOPPS phase 7 in May 2020 (including 41 returns from China facilities).22 The DOPPS and ISN agreed to extend the survey to countries not participating in DOPPS, including LLMICs. The ISN requested country-member societies and registries to provide a list of dialysis units in their country, including HD and peritoneal dialysis, private and public, university affiliated and nonaffiliated, and hospital- and satellite-based units. The adapted survey (Survey questionnaire) was subsequently disseminated to units in all countries in 2 stages, as follows:
Stage 1 (stratified random sample): For countries with fewer than 40 HD units, all units were invited to participate. For countries with >40 HD units, a stratified (by region/province and facility size) random sample of 20 units was selected. The survey was open for completion between November 18, 2020, and March 13, 2021. Responses were received from 43 of 113 invited countries, and a total of 209 surveys were returned.
Stage 2 (convenience sample): Responding to concerns that some adverse patient or staff experiences may be overlooked by a stratified random sampling approach, the survey was opened out to all HD or peritoneal dialysis centers between March 3, 2021, and March 13, 2021. A total of 162 surveys from 78 countries were returned.
Returned questionnaires from the initial China DOPPS survey (n = 41), stage 1 of the ISN survey (n = 209), and stage 2 of the ISN survey (n = 162) were combined for a total of 412 responses in 78 unique countries. Results were presented descriptively by country income category (according to the World Bank classifications) as low-, lower middle–, upper middle–, and high-income countries based on gross national income per capita in current US dollar (using the Atlas method exchange rates) of the previous year (i.e., 2020 in this case)23 (see Supplementary Table S1 for country breakdown of income and geography status). The Arbor Research Collaborative for Health Reference Ethical and Independent Review Services approved the study (IRB000007807) before its commencement. We ensured that digital personal identifiers were not requested, so no responses could be traced back to individuals or units completing the survey. The participants consented to deidentified responses being securely stored on ISN and Arbor servers.
Results
The study included 412 responses (Table 1) from 78 countries, with 15 (4%) responses from 7 LICs, 111 (27%) from 19 LMICs, 145 (35%) from 22 UMICs, and 141 (34%) from 30 HICs (see Supplementary Table S1 for list of responding countries). Overall, Africa had the highest number of responses (76 [18%] from 18 countries). Responses from LICs and LMICs were also mainly from Africa (11 [73%] and 53 [48%], respectively), whereas responses from UMICs were mainly from North and East Asia (45 [31%]), South East Asia and Oceania (27 [19%]), Eastern/Central Europe (22 [15%]), and Latin America (21 [15%]). HIC responses were mainly from Western Europe (59 [41%]). The HD units of the survey respondents were located in urban areas in country income groups as follows: LICs (100%), LMICs (79%), UMICs (88%), and HICs (67%). Of the HD units, 67% were in the public sector in LICs and 40% in LMICs. HD was the sole kidney replacement therapy available in 87% of LICs and 79% of LMICs. Both HD and peritoneal dialysis were available in 7% of LICs and 21% of LMICs as compared with 55% and 70% in UMICs and HICs, respectively.
Table 1.
Respondents’ dialysis unit characteristics, by country World Bank income status
| Survey participation | All | World Bank classification |
|||
|---|---|---|---|---|---|
| Low income | Lower-middle income | Upper-middle income | High income | ||
| n facilities | 412 | 15 | 111 | 145 | 141 |
| n countries | 78 | 7 | 19 | 22 | 30 |
| ISN region, % | |||||
| Africa | 18 | 73 | 48 | 8 | 1 |
| Europe (Eastern/Central) | 11 | 0 | 1 | 15 | 16 |
| Latin America | 8 | 0 | 10 | 15 | 1 |
| Middle East | 3 | 27 | 0 | 1 | 4 |
| Newly independent states and Russia, % | 5 | 0 | 2 | 12 | 0 |
| N. America/Caribbean | 7 | 0 | 0 | 0 | 20 |
| Asia (North and East) | 15 | 0 | 0 | 31 | 11 |
| Asia (South East and Oceania) | 13 | 0 | 17 | 19 | 6 |
| Asia (South) | 6 | 0 | 23 | 0 | 0 |
| Europe (Western) | 14 | 0 | 0 | 0 | 42 |
| Health care sector, % | |||||
| Public health care | 46 | 67 | 40 | 41 | 54 |
| Private health care | 27 | 20 | 37 | 30 | 17 |
| Academic/university hospital | 27 | 13 | 23 | 29 | 29 |
| Location, % | |||||
| Rural area | 10 | 0 | 8 | 4 | 17 |
| Urban area | 79 | 100 | 79 | 88 | 67 |
| Suburban area | 12 | 0 | 13 | 8 | 16 |
| Services offered, % | |||||
| Adults only | 70 | 47 | 49 | 68 | 90 |
| Children only | 2 | 7 | 2 | 1 | 2 |
| Both | 28 | 47 | 50 | 31 | 8 |
| Modalities available, % | |||||
| HD only | 50 | 87 | 79 | 44 | 28 |
| PD only | 1 | 7 | 0 | 1 | 2 |
| HD and PD | 48 | 7 | 21 | 55 | 70 |
HD, hemodialysis; PD, peritoneal dialysis.
Patient-Level Impact
Diagnostic Testing for SARS-CoV-2 Infection
At the peak of the first wave of the pandemic in April 2020/May 2020, diagnostic polymerase chain reaction testing was more frequently unavailable or of limited availability by the respondents in LICs (72%) and LMICs (68%) compared with UMICs (32%) and HICs (20%) (Table 2). These proportions had declined by the time of the survey in November 2020 to March 2021 in LMICs (21%), UMICs (9%), and HICs (5%), and to a lesser extent in LICs (62%). Routine diagnostic testing for asymptomatic patients was reportedly performed by 7% in LICs, 14% in LMICs, 19% in UMICs, and 23% in HICs. The turnaround time for results of diagnostic (polymerase chain reaction) testing was longer by the respondents from LLMICs as compared with UMICs and HICs (Table 2). Patients paid out-of-pocket for diagnostic test more frequently according to respondents in LMICs (40%) as compared with LICs (14%), UMICs (6%), and HICs (2%) (Table 2).
Table 2.
PCR and antibody testing of patients with kidney failure treated with chronic hemodialysis and staff, by World Bank classification
| Survey participation | All | World Bank classification |
|||
|---|---|---|---|---|---|
| Low income | Lower-middle income | Upper-middle income | High income | ||
| n facilities | 384 | 14 | 106 | 132 | 132 |
| Availability of PCR testing | |||||
| In April/May 2020, % | |||||
| Not available | 13 | 29 | 25 | 8 | 7 |
| Limited | 26 | 43 | 43 | 24 | 13 |
| Moderate | 33 | 29 | 24 | 34 | 42 |
| Widespread | 27 | 0 | 9 | 34 | 39 |
| Now,a % | |||||
| Not available | 5 | 8 | 9 | 4 | 3 |
| Limited | 8 | 54 | 13 | 5 | 2 |
| Moderate | 21 | 23 | 32 | 26 | 8 |
| Widespread | 66 | 15 | 46 | 65 | 88 |
| Anticipated in 3–6 mo, % | |||||
| Not available | 7 | 0 | 10 | 6 | 5 |
| Limited | 9 | 46 | 14 | 5 | 2 |
| Moderate | 19 | 54 | 25 | 27 | 6 |
| Widespread | 66 | 0 | 51 | 61 | 87 |
| Availability of antibody testing, % | |||||
| In April/May 2020 | |||||
| Not available | 58 | 64 | 74 | 43 | 57 |
| Limited | 33 | 29 | 24 | 38 | 35 |
| Universal testing | 10 | 7 | 2 | 19 | 8 |
| Now,a | |||||
| Not available | 31 | 57 | 40 | 31 | 21 |
| Limited | 42 | 36 | 42 | 35 | 47 |
| Universal testing | 27 | 7 | 18 | 34 | 32 |
| Anticipated in 3–6 mo | |||||
| Not available | 26 | 46 | 38 | 26 | 14 |
| Limited | 41 | 39 | 34 | 38 | 48 |
| Universal testing | 33 | 15 | 27 | 36 | 38 |
| Testing process/procedures,a % | |||||
| Time to receive antibody test results | |||||
| On the day of testing | 35 | 15 | 40 | 51 | 22 |
| 1–2 d | 25 | 8 | 16 | 25 | 33 |
| 3–7 d | 12 | 15 | 7 | 8 | 18 |
| More than 1 wk | 2 | 8 | 1 | 1 | 2 |
| Test not available | 27 | 54 | 36 | 16 | 26 |
| Time to receive PCR test results | |||||
| On the day of testing | 34 | 21 | 13 | 26 | 60 |
| 1–2 d | 45 | 29 | 54 | 49 | 37 |
| 3–7 d | 16 | 43 | 26 | 21 | 2 |
| More than 1 wk | 2 | 0 | 3 | 1 | 2 |
| Test not available | 3 | 7 | 5 | 3 | 1 |
| Routine asymptomatic PCR testing for | |||||
| Dialysis patients | 19 | 7 | 14 | 19 | 23 |
| Staff | 22 | 14 | 11 | 26 | 28 |
| Payer for majority of PCR tests | |||||
| Health care system | 73 | 71 | 50 | 81 | 84 |
| Patient insurance | 8 | — | 4 | 9 | 12 |
| Patient out-of-pocket | 15 | 14 | 40 | 6 | 2 |
| Test not available | 4 | 14 | 6 | 4 | 2 |
PCR, polymerase chain reaction.
As of survey completion date (November 2020–February 2021); April 2020/May 2020 data based on recall at time of survey completion.
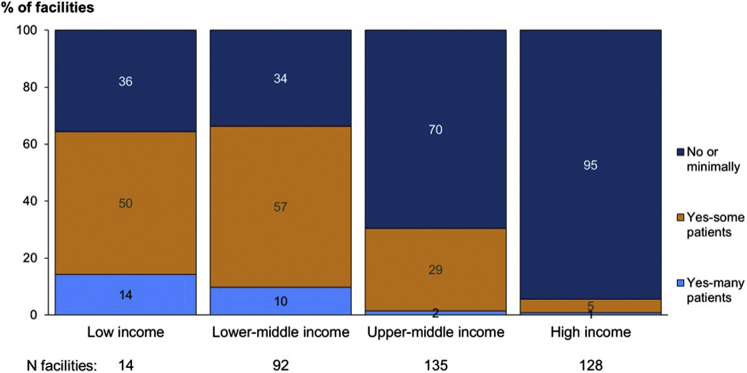
Interruption to HD Delivery
As compared with prepandemic, respondents from HD facilities in the LLMICs reported an increase in missed HD sessions for patients during the pandemic (Figure 1). Transportation to and from HD units during the pandemic was reported to be more challenging by 31% of the respondents from HD units in LICs and 38% in LMICs compared with 16% and 19% in UMICs and HICs, respectively. Duration of HD sessions was reported to be more frequently reduced for logistic reasons or to limit exposure to SARS-CoV-2 infection by the respondents from LICs (28%) and LMICs (27%) compared with UMICs (20%) and HICs (15%). Major supply disruptions of HD consumables, such as dialyzers, were frequently reported by the respondents from LICs (25%) and LMICs (24%). Major disruption to HD water processing was reported by 16% of the respondents from HD units in LICs and 8% in LMICs.
Figure 1.
Facilities reporting that the number of patients missing HD treatments has increased during the pandemic, by country World Bank country income. HD, hemodialysis.
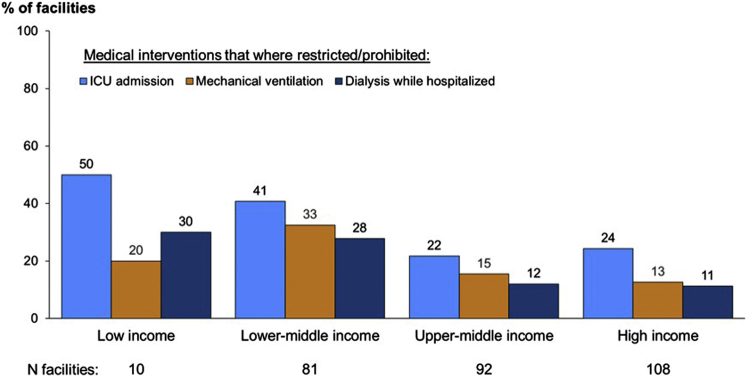
Access to ICU Care, Mechanical Ventilation, In-Hospital HD Became More Restricted During Versus Before the Pandemic for HD Patients Requiring Admission to Hospital Because of COVID-19 Infection
Access to HD and ICU-level care for admitted patients with SARS-CoV-2 infection who were on chronic HD (during vs. before the pandemic) was reportedly more limited in LICs and LMICs as compared with UMICs and HICs (Figure 2). The respondents reported that the admitted patients in LICs and LMICs were less likely to be offered mechanical ventilation when required during versus before the pandemic (Figure 2).
Figure 2.
Medical interventions became more restricted or prohibited for chronic dialysis patients admitted to the hospital with COVID-19 during versus before the pandemic, by World Bank country income. ICU, intensive care unit.
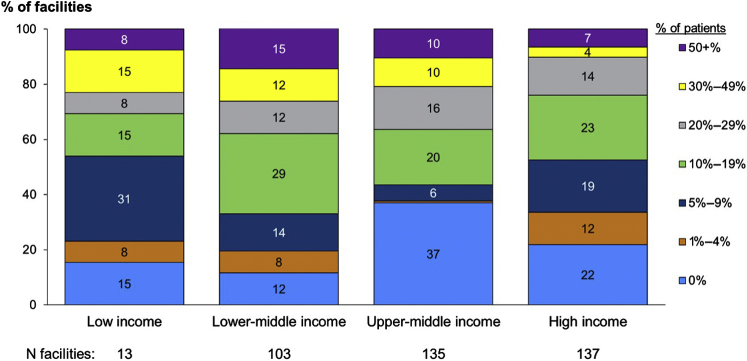
Incidence and Mortality in COVID-19 Infection and Outcomes for Patient Treated With Chronic HD
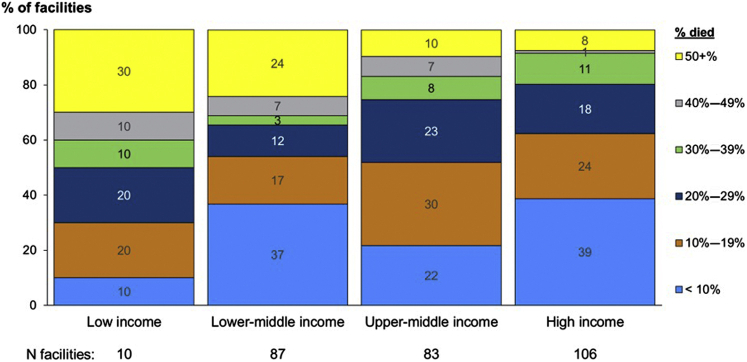
Respondents in 23% of LICs and 27% of LMICs reported confirmed or suspected COVID-19 cases in >30% of patients as compared with 20% in UMICs and 11% in HICs (Figure 3). Mortality was higher in LLMICs with 30% of the respondents from LIC setting reporting >50% mortality as compared with 8% of the respondents in HICs (Figure 4).
Figure 3.
Reported facility percent of HD patients with confirmed/suspected COVID-19, by country World Bank country income. HD, hemodialysis.
Figure 4.
Reported facility percent of HD patients with confirmed/suspected COVID-19 who died, by country World Bank country income. HD, hemodialysis.
Staff-Level Impact
Staff Testing
Staff in HD units in LLMICs reported less routine testing for SARS-CoV-2 when asymptomatic as compared with UMICs and HICs—14% of staff in LICs and 11% in LMICs, compared with 26% and 28% in UMICs and HICs, respectively.
Use of PPE by Staff
There were differences in the availability and use of PPE by staff in HD units across income levels especially with plastic aprons, isolation gowns, and eye protection. PPE use was proportionally lower in LLMICs as compared with UMICs and HICs (Table 3).
Table 3.
Use of personal protective equipment, by income
| Survey participation | All | World Bank classification |
|||
|---|---|---|---|---|---|
| Low income | Lower-middle income | Upper-middle income | High income | ||
| n facilities | 382 | 14 | 102 | 136 | 130 |
| Particulate-air filter respirators (e.g., N95 masks), % | |||||
| For direct contact—with all patients | 36 | 39 | 40 | 35 | 32 |
| For direct contact—only for patients with suspected/confirmed cases | 51 | 46 | 47 | 57 | 48 |
| Not available in this dialysis unit | 10 | 15 | 11 | 8 | 9 |
| Available, but not used | 4 | 0 | 2 | 0 | 10 |
| Surgical mask, % | |||||
| For direct contact—with all patients | 89 | 79 | 92 | 92 | 84 |
| For direct contact—only for patients with suspected/confirmed cases | 6 | 14 | 1 | 5 | 9 |
| Not available in this dialysis unit | 1 | 0 | 1 | 2 | 1 |
| Available, but not used | 4 | 7 | 6 | 1 | 6 |
| Extended face mask use program for staffa | 75 | 93 | 71 | 74 | 76 |
| Use of face masks by staff beyond manufacturer shelf-lifeb | 31 | 50 | 40 | 29 | 25 |
| Gloves, % | |||||
| For direct contact—with all patients | 84 | 86 | 92 | 89 | 73 |
| For direct contact—only for patients with suspected/confirmed cases | 15 | 14 | 7 | 11 | 25 |
| Not available in this dialysis unit | 0 | 0 | 0 | 0 | 0 |
| Available, but not used | 1 | 0 | 1 | 0 | 2 |
| Eye protection, % | |||||
| For direct contact—with all patients | 63 | 31 | 60 | 70 | 63 |
| For direct contact—only for patients with suspected/confirmed cases | 30 | 39 | 24 | 28 | 35 |
| Not available in this dialysis unit | 4 | 23 | 9 | 2 | 0 |
| Available, but not used | 3 | 8 | 7 | 1 | 2 |
| Isolation gown, % | |||||
| For direct contact—with all patients | 47 | 42 | 43 | 58 | 40 |
| For direct contact—only for patients with suspected/confirmed cases | 46 | 42 | 44 | 39 | 56 |
| Not available in this dialysis unit | 4 | 17 | 8 | 2 | 2 |
| Available, but not used | 3 | 0 | 5 | 1 | 3 |
| Plastic apron, % | |||||
| For direct contact—with all patients | 45 | 29 | 39 | 57 | 42 |
| For direct contact—only for patients with suspected/confirmed cases | 31 | 29 | 33 | 28 | 33 |
| Not available in this dialysis unit | 16 | 43 | 21 | 12 | 12 |
| Available, but not used | 8 | 0 | 7 | 2 | 13 |
Use of the same mask for direct contact with different patients.
Implemented by dialysis clinic.
Shortages of PPE
Severe shortages of PPE were reported by the respondents from LICs and LMICs compared with UMICs and HICs, especially with respect to the use of the N95 particulate-air respirator masks (Table 4). Face masks were reportedly used beyond the manufacturers’ shelf-life in 50%, 40%, 29%, and 25% in LICs, LMICs, UMICs, and HICs, respectively. Staff reported paying directly out-of-pocket for PPE more frequently in LICs (58%) and LMICs (76%) compared with UMICs (53%) and HICs (21%).
Table 4.
Shortages of personal protective equipment at any point in the pandemic, by World Bank country income
| Survey participation | All | World Bank classification |
|||
|---|---|---|---|---|---|
| Low income | Lower-middle income | Upper-middle income | High income | ||
| n facilities | 342 | 14 | 101 | 97 | 130 |
| Particulate-air filter respirators (e.g., N95 masks), % | |||||
| No shortage | 39 | 21 | 19 | 53 | 47 |
| Moderate shortage | 38 | 29 | 43 | 38 | 36 |
| Severe shortage | 14 | 43 | 24 | 4 | 10 |
| Not available (before or during pandemic) | 9 | 7 | 15 | 5 | 7 |
| Surgical mask, % | |||||
| No shortage | 72 | 57 | 59 | 83 | 76 |
| Moderate shortage | 22 | 36 | 32 | 14 | 19 |
| Severe shortage | 5 | 7 | 7 | 2 | 5 |
| Not available (before or during pandemic) | 1 | 0 | 2 | 1 | 0 |
| Gloves, % | |||||
| No shortage | 80 | 79 | 69 | 85 | 84 |
| Moderate shortage | 17 | 21 | 23 | 14 | 14 |
| Severe shortage | 3 | 0 | 7 | 1 | 2 |
| Not available (before or during pandemic) | 0 | 0 | 1 | 0 | 0 |
| Eye protection, % | |||||
| No shortage | 63 | 36 | 41 | 71 | 78 |
| Moderate shortage | 25 | 29 | 34 | 23 | 19 |
| Severe shortage | 7 | 7 | 13 | 3 | 4 |
| Not available (before or during pandemic) | 6 | 29 | 12 | 3 | 0 |
| Isolation gown, % | |||||
| No shortage | 58 | 36 | 31 | 74 | 70 |
| Moderate shortage | 31 | 29 | 50 | 21 | 23 |
| Severe shortage | 7 | 14 | 10 | 4 | 6 |
| Not available (before or during pandemic) | 4 | 21 | 10 | 1 | 1 |
| Plastic apron, % | |||||
| No shortage | 57 | 36 | 41 | 71 | 61 |
| Moderate shortage | 22 | 14 | 29 | 17 | 21 |
| Severe shortage | 5 | 14 | 10 | 2 | 3 |
| Not available (before or during pandemic) | 16 | 36 | 20 | 10 | 14 |
COVID-19 Training and Guidance From Within Institutions
Institutional guidance or training for staff in infection control procedures and PPE use during care of patients with COVID-19 was less frequently provided in LICs as compared with LMICs. Provision of guidance on infection control was reported by 33% of the respondents from LICs as compared with 73% from LMICs. Guidance and training for staff in PPE use were reported by 25% of the respondents in LICs as compared with 74% in LMICs.
Psychological Support of Staff
Psychological support for staff during the COVID-19 pandemic was limited in all settings with support services reported to be available by 31% and 32% of the respondents in LICs and LMICs, respectively, as compared with 58% in UMIC and 52% in HIC. Staff working in HICs and UMICs were more likely to receive one-on-one private counseling in HICs (28%) and UMICs (27%), respectively, compared with LICs (23%) and LMICs (16%), respectively.
Discussion
The COVID-19 pandemic has global devastating consequences on health systems globally and has further highlighted and widened the gap of health care inequities between lower- and upper-income countries.17,24, 25, 26 This is the first report to study challenges in dialysis delivery during the COVID-19 pandemic across countries of different World Bank income status categories.23 Our report identifies that there are important global inequities in the availability of diagnostic testing, availability and use of PPE, and restricted-access dialysis sessions and ICU care in LLMICs as compared with non-LLMICs.
At the time of the survey, diagnostic testing for SARS-CoV-2 infection was not available or of limited availability for patients in LICs and LMICs as compared with UMICs and HICs. Many governments provide diagnostic testing for symptomatic patients but not for asymptomatic cases.27 Most LLMICs had very few testing centers leading to backlogs and delay in results during the peak of the pandemic.28 Restrictions in testing may have led to the spread of SARS-CoV-2 infection in these HD units. Delays in receiving COVID-19 diagnostics results may also delay HD care and delivery of interventions associated with HD, such as vascular access procedures, which may have critical consequences for some patients. Contributing to these delays and inequities, the respondents reported that patients in LLMICs were more likely to have to pay out-of-pocket for diagnostic testing and that test results took longer to process. The cost of in-patient diagnostic testing has been shown to range from as low as $10 to as high as $1390 depending on the setting.29 Reduced testing for COVID-19 infection among staff could lead to increased transmission in the HD unit among clinical staff and to already vulnerable patients with kidney failure.15
Adequate provision and use of PPE is an important measure to prevent the spread of SARS-CoV-2.18, 19, 20, 21,30,31 Staff in HD units in LLMICs not only reported that they were less frequently tested for SARS-CoV-2 infection when asymptomatic but also reported shortages in the availability of PPE. Moreover, the staff had to purchase the PPE themselves and were more likely to use disposable PPE beyond the manufacturers’ stated shelf-life as compared with the staff from UMICs and HICs.
Patients receiving HD in LLMICs reportedly missed their treatments more frequently than patients in UMICs and HICs. This was likely owing to greater transportation challenges occurring in LLMICs during the peak of the pandemic, lack of work/funds, and severe local lockdowns and curfews. Such barriers have been described by others and can lead to death independent of infection with COVID-19.32 In addition, it has been described that some private facilities in LLMICs refused to dialyze patients with symptoms suggestive of COVID-19, owing to the perceived stigma of COVID-19 infection and lack of capacity to isolate patients with COVID-19 on dialysis. Referral of these patients to oversubscribed and under-resourced public hospitals likely further increased transmission risks in these facilities.33,34
Access to in-patient care, ICU care, or mechanical ventilation was reportedly more restricted for patients receiving HD in LLMICs. Generally, patients with kidney failure have multiple comorbidities and are assumed to have poor prognosis with high in-hospital mortality, especially when on chronic HD.35, 36, 37 There are data suggesting that poor outcomes are not universal in patients with COVID-19 and kidney disease, once appropriate ICU care and mechanical ventilation are available.38 However, access to ICU care for HD patients with COVID-19 infection in LLMICs was restricted during the pandemic compared with access to ICU care for the same group of patients pre-pandemic. This suggests that dialysis dependence was likely used (officially or unofficially) as a triage criterion, as has been suggested/implemented elsewhere.39 Most LLMICs generally have limited availability of adequate ICU facilities and have fewer specialty-trained staff and less standardized processes of care.40 Delivery of ICU care may have been even more difficult as a result of the strain on the health system owing to the COVID-19 pandemic,26,41 leading to very strict triaging criteria for ICU admissions and mechanical ventilation. The necessity of triage practices under pandemic circumstances highlights the importance of accurate prognostication, transparency of the decision-making process, psychological support for the staff, and the importance of palliative and supportive care.39
Aligned with the current evidence, the study respondents reported higher mortality with COVID-19 infection for patients treated with chronic HD in LLMICs than non-LLMICs.3,6,24 Though mortality was subjectively reported by the survey respondents, limited testing for COVID-19 infection, lack of availability of suitable PPE, disruption of HD care, and restricted access to ICU care and mechanical ventilation may have in combination contributed the reported greater proportion of deaths among HD patients in LLMICs compared with UICs and HICs observed in our study.
Psychological support for HD staff was low in all settings but proportionally lower in LLMICs compared with UIC and HIC. Factors that have been shown to significantly increase psychological stress in health care staff are working in isolation wards, concern about acquiring COVID-19 infection in the workplace, shortages of PPE, and staff working in direct contact with patients with COVID-19.42 Respondents reported that during the pandemic, staff in LLMICs had less guidance and training than elsewhere. Evidence suggests that increasing staff knowledge of infection prevention, development of protocols, and educational activities can improve the morale among health care staff.43 Adding to the already significant workplace-based stress, health care staff have been victims of stigma in some countries as they were assumed to have COVID-19 infection and were prevented from using public facilities and public transportation.16,44,45 In the face of these psychological stressors with reduced support for the same in LLMIC, burnout and reduction in HD clinical staff should be expected as the pandemic continues.
The significant global reach of the ISN combined with the existing DOPPS networks and previous experience in capturing the reality of dialysis services across the globe is a major strength of this study. Our findings are likely to be both generalizable and informative for policymakers as the pandemic progresses, and also in future health care crises. Our study however had some limitations. The respondents completed the survey during varying times of the pandemic, and the pandemic peaks (up to survey date) varied by region, such that recall bias may have been differential. Responses from LICs were relatively few compared with LMICs, HICs, and UMICs potentially because LLMICs may have had reduced access to internet services and access to social media or may not have been aware of the web-based survey. Mortality of HD patients from COVID-19 was subjectively reported but is in line with published literature.7, 8, 9, 10, 11, 12, 13
In summary, although many global imbalances in dialysis care predate the pandemic, striking and unacceptable inequities related to the care of HD patients were identified comparing countries with different income categories. Different restrictions to COVID-19 diagnostic testing, availability of PPE for staff, access to ICU care and mechanical ventilation, and poor psychological support for staff during the pandemic clearly exemplify the fragility in HD service delivery across income categories. Additional challenges not captured in this survey, such as the unacceptably slow delivery of vaccines to LLMICs, have added another layer of inequity.46 Given this fact, HD units in LLMICs are still relying mainly on basic public health practices, such as hand washing, use of hand sanitizers, the wearing of facemasks, as well as social distancing in an attempt to prevent COVID-19 infection, whereas the rest of the world increases their vaccine coverage and eases restrictions.47
We conclude that urgent action is required to address these inequities that disproportionately affect LLMIC settings thereby exacerbating pre-existing vulnerabilities which may contribute to poorer outcomes. In the modern era of medical practice and globalization, the existence and widening of such health inequities are unacceptable. In solidarity with patients living on HD and those who care for them, the nephrology community must urgently add its voice to the calls for global equity in access to all resources needed to detect and treat COVID-19 as well as to life-saving vaccinations.
Disclosure
RPF reports receiving research grants from Fresenius Medical Care; receiving consulting fees from AstraZeneca, Bayer, Novo Nordisk, Boehringer-Lilly, and Retrophin; and conducting voluntary work for the ISN and KDIGO. VJ reports receiving grants from Baxter Healthcare, GlaxoSmithKline, NephroPlus, and Biocon; receiving honoraria from AstraZeneca and Baxter Healthcare; participating in Zydus and GlaxoSmithKline data safety monitoring boards; and is the past president of the ISN. AL is a member of ISN ExCom, a member of OSEA Regional Board, and Chair of the ISN Disaster Preparedness Working Group. BR reports receiving consultancy fees or travel reimbursement since 2019 from AstraZeneca, GlaxoSmithKline, and Kyowa Kirin Co. All the other authors declared no competing interests.
Acknowledgments
The authors thank the national society and registry countries and ISN regional board leaders who provided the lists of dialysis centers that we were then able to contact. We are grateful to Charu Malik and Paul Laffin at ISN for their support and Silvia Salaro at ISN who assisted with contacting the country leaders and deploying the survey. We are grateful to staff at Arbor Research Collaborative for Health for supporting survey development and deployment. This research has previously been reported at Kidney Week 2021 (American Society of Nephrology).
Author Contributions
BR, RPF, MG, and RP (Dialysis Outcomes and Practice Patterns Study) developed the study idea and initial questionnaire. FC, RA, EKT, GD, AL, VL, DS, CP, RE, and VJ adapted the survey. RA and FC disseminated the survey to ISN members (with the support of ISN). BB performed the analysis. EKT wrote the first draft of the manuscript, with edits by GD, RPF, VL, and BR. All authors reviewed the manuscript and approved its final draft.
Footnotes
Survey questionna ire.
Table S1. Survey returns by country and World Bank country income.
STROBE Checklist.
Supplementary Material
Survey questionnaire.
Table S1. Survey returns by country and World Bank country income.
STROBE Checklist.
References
- 1.Sohrabi C., Alsafi Z., O’Neill N., et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) [published correction appears in Int J Surg. 2020;77:217] Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou F., Yu T., Du R., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study [published correction appears in Lancet. 2020;395:1038] Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hopman J., Allegranzi B., Mehtar S. Managing COVID-19 in low- and middle-income countries. JAMA. 2020;323:1549–1550. doi: 10.1001/jama.2020.4169. [DOI] [PubMed] [Google Scholar]
- 4.Diaz J.V., Riviello E.D., Papali A., Adhikari N.K., Ferreira J.C. Global critical care: moving forward in resource-limited settings. Ann Glob Health. 2019;85:3. doi: 10.5334/aogh.2413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mills A. Health care systems in low- and middle-income countries. N Engl J Med. 2014;370:552–557. doi: 10.1056/NEJMra1110897. [DOI] [PubMed] [Google Scholar]
- 6.Adapa S., Aeddula N.R., Konala V.M., et al. COVID-19 and renal failure: challenges in the delivery of renal replacement therapy. J Clin Med Res. 2020;12:276–285. doi: 10.14740/jocmr4160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hilbrands L.B., Duivenvoorden R., Vart P., et al. COVID-19-related mortality in kidney transplant and dialysis patients: results of the ERACODA collaboration [published correction appears in Nephrol Dial Transplant. 2021;36:1962] Nephrol Dial Transplant. 2020;35:1973–1983. doi: 10.1093/ndt/gfaa261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jager K.J., Kramer A., Chesnaye N.C., et al. Results from the ERA-EDTA Registry indicate a high mortality due to COVID-19 in dialysis patients and kidney transplant recipients across Europe. Kidney Int. 2020;98:1540–1548. doi: 10.1016/j.kint.2020.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Scarpioni R., Manini A., Valsania T., et al. Covid-19 and its impact on nephropathic patients: the experience at Ospedale “Guglielmo da Saliceto” in Piacenza. G Ital Nefrol. 2020;37:1–5. [PubMed] [Google Scholar]
- 10.Alberici F., Delbarba E., Manenti C., et al. A report from the Brescia Renal COVID Task Force on the clinical characteristics and short-term outcome of hemodialysis patients with SARS-CoV-2 infection. Kidney Int. 2020;98:20–26. doi: 10.1016/j.kint.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Valeri A.M., Robbins-Juarez S.Y., Stevens J.S., et al. Presentation and outcomes of patients with ESKD and COVID-19. J Am Soc Nephrol. 2020;31:1409–1415. doi: 10.1681/ASN.2020040470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Meester J., De Bacquer D., Naesens M., et al. Incidence, characteristics, and outcome of COVID-19 in adults on kidney replacement therapy: a regionwide registry study. J Am Soc Nephrol. 2021;32:385–396. doi: 10.1681/ASN.2020060875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Robinson B.M., Guedes M., Alghonaim M., et al. Worldwide early impact of COVID-19 on dialysis patients and staff and lessons learned: a DOPPS roundtable discussion. Kidney Med. 2021;3:619–634. doi: 10.1016/j.xkme.2021.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weinhandl E.D., Wetmore J.B., Peng Y., et al. Initial effects of COVID-19 on patients with ESKD. J Am Soc Nephrol. 2021;32:1444–1453. doi: 10.1681/ASN.2021010009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Combe C., Kirsch A.H., Alfano G., et al. At least 156 reasons to prioritize COVID-19 vaccination in patients receiving in-centre haemodialysis. Nephrol Dial Transplant. 2021;36:571–574. doi: 10.1093/ndt/gfab007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bagcchi S. Stigma during the COVID-19 pandemic. Lancet Infect Dis. 2020;20:782. doi: 10.1016/S1473-3099(20)30498-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tangcharoensathien V., Bassett M.T., Meng Q., Mills A. Are overwhelmed health systems an inevitable consequence of covid-19? Experiences from China, Thailand, and New York State. BMJ. 2021;372:n83. doi: 10.1136/bmj.n83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Basile C., Combe C., Pizzarelli F., et al. Recommendations for the prevention, mitigation and containment of the emerging SARS-CoV-2 (COVID-19) pandemic in haemodialysis centres. Nephrol Dial Transplant. 2020;35:737–741. doi: 10.1093/ndt/gfaa069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Control for Disease Control and Prevention Interim additional guidance for infection prevention and control for patients with suspected or confirmed COVID-19 in outpatient haemodialysis facilities. Control for Disease Control and Prevention. https://stacks.cdc.gov/view/cdc/85730 Published March 10, 2020.
- 20.Elsayed H.M., Wadee S., Zaki M.S., et al. Guidelines for the prevention, detection and management of the renal complications of COVID-19 in Africa. Afr J Nephrol. 2020;23:109–126. doi: 10.21804/23-1-4177. [DOI] [Google Scholar]
- 21.NICE, National Institute for Health and Care Excellence (UK) NICE, National Institute for Health and Care Excellence (UK). COVID-19 rapid guideline: dialysis service delivery. NICE Guidelines. https://www.nice.org.uk/guidance/ng160 Published 2020. [PubMed]
- 22.Aylward R., Bieber B., Guedes M., et al. The global impact of the COVID-19 pandemic on in-center hemodialysis services: an ISN-dialysis outcomes practice patterns study survey. Kidney Int Rep. 2022;7:397–409. doi: 10.1016/j.ekir.2021.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.The World Bank The World Bank by income and region. The World Bank. https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html Published 2020. Accessed September 25, 202.
- 24.Bong C.-L., Brasher C., Chikumba E., et al. The COVID-19 pandemic: effects on low- and middle-income countries. Anesth Analg. 2020;131:86–92. doi: 10.1213/ANE.0000000000004846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krouse H.J. COVID-19 and the widening gap in health inequity. Otolaryngol Head Neck Surg. 2020;163:65–66. doi: 10.1177/0194599820926463. [DOI] [PubMed] [Google Scholar]
- 26.Blumenthal D., Fowler E.J., Abrams M., Collins S.R. Covid-19—implications for the health care system [published correction appears in N Engl J Med. 2020;383:1698] N Engl J Med. 2020;383:1483–1488. doi: 10.1056/NEJMsb2021088. [DOI] [PubMed] [Google Scholar]
- 27.Nikolai L.A., Meyer C.G., Kremsner P.G., Velavan T.P. Asymptomatic SARS coronavirus 2 infection: invisible yet invincible. Int J Infect Dis. 2020;100:112–116. doi: 10.1016/j.ijid.2020.08.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Torres I., Sippy R., Sacoto F. Assessing critical gaps in COVID-19 testing capacity: the case of delayed results in Ecuador. BMC Public Health. 2021;21:637. doi: 10.1186/s12889-021-10715-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zare H., Bai G., Albrecht C., et al. Hospital inpatient charges of COVID-19 diagnostic tests ranged from $10 to $1390. Popul Health Manag. 2021;24:433–435. doi: 10.1089/pop.2020.0283. [DOI] [PubMed] [Google Scholar]
- 30.Ikizler T.A., Kliger A.S. Minimizing the risk of COVID-19 among patients on dialysis. Nat Rev Nephrol. 2020;16:311–313. doi: 10.1038/s41581-020-0280-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arenas M.D., Villar J., González C., et al. Protection of nephrology health professionals during the COVID-19 pandemic. Nefrol (Engl Ed) 2020;40:395–402. doi: 10.1016/j.nefro.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dore B. Covid-19: collateral damage of lockdown in India [published correction appears in BMJ. 2020;369:m1797] BMJ. 2020;369:m1711. doi: 10.1136/bmj.m1711. [DOI] [PubMed] [Google Scholar]
- 33.Tannor E.K. Challenges in kidney care in a lower middle income country during the COVID-19 pandemic—the Ghanaian perspective. Kidney Int Rep. 2021;6:2014–2016. doi: 10.1016/j.ekir.2021.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Prasad N., Bhatt M., Agarwal S.K., et al. The adverse effect of COVID pandemic on the care of patients with kidney diseases in India. Kidney Int Rep. 2020;5:1545–1550. doi: 10.1016/j.ekir.2020.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yamada T., Mikami T., Chopra N., et al. Patients with chronic kidney disease have a poorer prognosis of coronavirus disease 2019 (COVID-19): an experience in New York City. Int Urol Nephrol. 2020;52:1405–1406. doi: 10.1007/s11255-020-02494-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang D., Xiao Y., Chen J., et al. COVID-19 and chronic renal disease: clinical characteristics and prognosis. QJM. 2020;113:799–805. doi: 10.1093/qjmed/hcaa258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gallo Marin B., Aghagoli G., Lavine K., et al. Predictors of COVID-19 severity: a literature review. Rev Med Virol. 2021;31:1–10. doi: 10.1002/rmv.2146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hittesdorf E., Panzer O., Wang D., et al. Mortality and renal outcomes of patients with severe COVID-19 treated in a provisional intensive care unit. J Crit Care. 2021;62:172–175. doi: 10.1016/j.jcrc.2020.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jöbges S., Vinay R., Luyckx V.A., Biller-Andorno N. Recommendations on COVID-19 triage: international comparison and ethical analysis. Bioethics. 2020;34:948–959. doi: 10.1111/bioe.12805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vukoja M., Riviello E., Gavrilovic S., et al. A survey on critical care resources and practices in low- and middle-income countries. Glob Heart. 2014;9:337–342.e1-e5. doi: 10.1016/j.gheart.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 41.Salluh J.I., Burghi G., Haniffa R. Intensive care for COVID-19 in low- and middle-income countries: research opportunities and challenges. Intensive Care Med. 2021;47:226–229. doi: 10.1007/s00134-020-06285-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288:112936. doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tsamakis K., Rizos E., Manolis A.J., et al. [Comment] COVID-19 pandemic and its impact on mental health of healthcare professionals. Exp Ther Med. 2020;19:3451–3453. doi: 10.3892/etm.2020.8646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mackworth-Young C.R., Chingono R., Mavodza C., et al. Community perspectives on the COVID-19 response, Zimbabwe. Bull World Health Organ. 2021;99:85–91. doi: 10.2471/BLT.20.260224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Uvais NA, Aziz F, Hafeeq B. COVID-19-related stigma and perceived stress among dialysis staff. Springer; 2020:1–2. [DOI] [PMC free article] [PubMed]
- 46.Choi E.M. COVID-19 vaccines for low- and middle-income countries. Trans R Soc Trop Med Hyg. 2021;115:447–456. doi: 10.1093/trstmh/trab045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Asundi A., O’Leary C., Bhadelia N. Global COVID-19 vaccine inequity: the scope, the impact, and the challenges. Cell Host Microbe. 2021;29:1036–1039. doi: 10.1016/j.chom.2021.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.