Abstract
To investigate psychological response of Chinese public during the regular prevention and control of Corona Virus Disease 2019 (COVID-19), and explore the relationship among income loss, social support and mental health.
Five hundred twenty-six participants were randomly selected by snowball sampling method. Chinese version of Perceived Psychological Stress Scale, Perceived Social Support Scale, self-rating anxiety scale, and the PTSD Checklist for DSM-5 were used to measure the levels of psychological stress, social support, anxiety, and post-traumatic stress disorder (PTSD) symptoms. Demographic variables, income loss and income satisfaction during the outbreak period were also collected.
The prevalence rate of anxiety, PTSD symptoms and stress problems were 19.8%, 23.8%, and 24.7% respectively. Multiple Regression Analysis illustrated that social support associated with stress, anxiety and PTSD after controlling demographic variables; for non-student samples, stress, anxiety, and PTSD were corelated with change in income and social support.
During the regular prevention and control of COVID-19, social support might help reducing stress, anxiety, and PTSD symptoms. In addition to social support, change of income level was also an important factor for mental health. This study suggested the importance of maintaining a steady income after acute outbreak of COVID-19.
Keywords: anxiety, COVID-19, income, PTSD, social support, stress
1. Introduction
The outbreak of Corona Virus Disease 2019 (COVID-19) has caused various mental health problems in China and throughout the world. Among the problems, high level of stress, anxiety, and posttraumatic disorder (PTSD) symptoms were most serious in the general public group. For example, it was reported that 24% and 22.3% of the general public in Saudi Arabia reported anxiety and stress symptoms[1]; 21.6% and 15.8% residents in Spain suffered from anxiety and PTSD symptoms respectively.[2] In China, more than 90,000 cases were confirmed,[3] the impact of COVID-19 on psychological health was also quite severe. Evidence has showed that the pooled prevalence rate of psychological morbidities includes poor sleep quality (40%), stress (34%), psychological distress (34%), insomnia (30%), post-traumatic stress symptoms (27%), anxiety (26%), depression (26%) in Chinese.[4]
The opening of Chinese “two sessions” on May 20, 2020 showed that epidemic prevention and control had become normal and that the outbreak of COVID-19 was initially under control. However, from June to August, there were small outbreaks of COVID-19 happened in the cities of Beijing, Dalian, and Urumchi in China,[5] causing fear and psychological distress in the general public. And these small outbreaks were signals that the influence of COVID-19 was far from over. Previous studies mainly focused on the psychological responses during the initial stage of COVID-19, and the present study aimed to illustrate mental health status during the beginning of “normal control” time: Whether general public in China still showed problems of anxiety, stress and PTSD symptoms when the control of COVID-19 became normal? Also, as the response to public health events in Wuhan city declined to Level-2,[6] Wuhan was not the most influenced area of COVID-19 in China, and previous findings that Wuhan expose history was negatively related with mental health should be re-examined.[7]
The outbreak of COVID-19 in China has a significant negative impact on economic development. According to the National Bureau of Statistics of China, the gross domestic product of China had shrunk 6.8 percent in the first quarter of 2020, which was the worst decline in the last 3 decades.[8] On an individual level, COVID-19 might result in a loss of income, and lead to mental problems.[9] Numerous studies has showed that individual's anxiety, trauma, psychological stress were soaring with the decline of income.[10–12] A research conducted following the 2003 outbreak of severe acute respiratory syndrome has illustrated that mental health problems among the general public in East Asian region was closely related to income losses.[13] However, there were currently few studies investigate the link between change in income and psychological response during the outbreak of COVID-19. Thus, the present study aimed to explore the possible relationship.
Social support was one of the most important protective factors to psychological well-being, which can help mitigate or buffer adverse psychological factors caused by negative events. Cohen et al[14] acknowledged that social support was extremely beneficial for individuals with high stress level. Studies had found social support were closely related to dreadful emotional experience during the COVID-19 outbreak.[15,16] Although financial support was a part of social support, there was evidence that income and social support might has distinct effects on mental health. For example, a recent study has reported that economic status would impact the association between positive social support and depressive symptoms among Korean adults.[17] As a result, it was reasonable to hypothesize that income change during COVID-19 and social support might have sperate contribution to the development of mental health problems.
Taken together, the present study aimed to illustrate mental health problems among Chinese public when the COVID-19 was initially under control and the “normal control” condition began. Wuhan-expose history, income change, and social support were potential influence factors that explored.
2. Materials and methods
2.1. Participants
This web-based cross-sectional study was carried out in China by snowball sampling. Participants answered the questionnaires anonymously on an online survey platform from May 20, 2020 to June 5, 2020. The link of the questionnaire was broadcasted through mainstream social media or online communities to recruit participants. In doing so, cell-phone verification was used to avoid second submission from a single participant. A total of 552 respondents participated in this study. 95.3% of them (526 out of 552 people) completed the whole survey, and were considered for the ultimate statistical analyses. There were 234 males (44.5% out of the sample) and 292 females (55.5% out of the sample). The mean age of the participants was 32.81 (standard deviation = 14.01).
All the study participants were provided with written informed consent. This project was approved by the Ethics Committee of the Naval Military Medical University.
2.2. Questionnaires
2.2.1. Demographic questionnaire and income status
The first section of the survey collected information about demographic variables, including sex, age, education, occupation, place of residence, and whether the participant was the only child. The participants were asked to evaluate their satisfaction with income and change of income during outbreak of COVID-19 if they were non-students. Income satisfaction and income loss was evaluated with 1-5 points. Individuals would score higher if they were more satisfying with their income and they would score lower if they had greater income loss because of COVID-19.
2.2.2. Perceived social support scale (PSSS)
PSSS was developed by Jiang[18] to evaluate the family support, friend support, and other support. The scale contained 12 items, using Likert 7-level scoring, from 1 point (strongly disagree) to 7 points (strongly agree). Higher scores indicated better social support systems. In this study, Cronbach α of PSSS scale was 0.92.
2.2.3. Chinese version of perceived psychological stress scale (CPSS)
Perceived stress scale was compiled by Cohen, and was translated into Chinese by Yang et al.[19] CPSS had a total of 14 items and each item ranged from 0 points (never) to 4 points (always). The total score of the scale ranged from 0 to 56 points and higher scores indicated greater the psychological stress. The Cronbach α of CPSS was 0.78 in the present study.
2.2.4. Self-rating anxiety scale (SAS)
This scale was compiled by Zung[20] in 1971 and contained 20 items reflecting subjective feelings of anxiety in the past week. Each item was scored on a 0 to 4 point and the total raw score should be multiplied by 1.25 and then rounded to get the standard score which ranged from 25 to 100. The higher the score, the more anxious one felt. According to the Chinese norm, the cut-off value of SAS standard score was 50 points, and 50 to 59 points indicated mild anxiety, 60 to 69 points indicated moderate anxiety, and 69 points or more indicated severe anxiety. The Cronbach α coefficient of SAS was 0.93.
2.2.5. The PTSD checklist for DSM-5 (PCL-5)
The PTSD checklist for DSM-5[21] was adopted to assess the participants’ PTSD symptom during the epidemic. The scale had 20 items, each of which ranged from 0 (not at all) to 4 (very severe), representing the degree to which a person had been troubled by post-traumatic stress disorder in the past month. The scale had a total score of 80 points. The higher the score, the stronger the post-traumatic stress symptom. In this study, the Cronbach α coefficient of PCL-5 was 0.91.
2.3. Statistical analyses
SPSS version 26 (International Business Machines Corporation, Armonk, New York, USA) was used for statistical analysis. Independent-sample t test (two-tailed) and one-way variance analysis were conducted to compare the psychological responses between individuals of different demographic characteristics. Multiple regression analyses were conducted to analyze the link between income loss, social support, and mental health problems. The measurement data conformed to the normal distribution, and expressed as mean (standard deviation).
3. Results
3.1. Demographic characteristics and psychological impact of the sample
The prevalence of PTSD and anxiety was 23.8% and 19.8% respectively. Table 1 showed the comparison between groups of different demographic characteristics in CPSS scores, SAS scores, PCL-5 scores, and PSSS scores. Respondents from 18 to 29-year old had statistically significant higher CPSS and PCL-5 scores than other adult respondents (P < .05), a multiple comparison with Bonferroni correction was applied to test; and groups with different occupation also showed significant difference in CPSS and PCL-5 scores (all P < .05). Compared with the non-only child group, the only child group had significantly higher PCL-5 scores (P < .05). And higher level of education was related with higher CPSS and PSSS scores (all P < .05). Gender as well as residential district did not influence social support and psychological outcome.
Table 1.
Demographic characteristics of the participants and differences in mental health states.
| Variables | n (%) | Stress (CPSS) | Anxiety (SAS) | Post-traumatic stress disorder (PCL-5) | Social support (PSSS) |
| Gender | 526 (100%) | 23.99 (7.816) | 41.52 (10.539) | 23.22 (13.708) | 58.25 (17.024) |
| Male | 234 (44.5%) | 23.53 (8.450) | 41.11 (11.390) | 23.43 (23.055) | 58.03 (17.667) |
| Female | 292 (55.5%) | 24.36 (7.262) | 41.85 (9.812) | 23.05 (13.144) | 58.42 (16.520) |
| t | −1.22 | −0.79 | 0.31 | −0.26 | |
| P | .224 | .427 | .754 | .792 | |
| Age | 526 (100%) | 23.99 (7.816) | 41.52 (10.539) | 23.22 (13.708) | 58.25 (17.024) |
| 18-29 | 270 (51.3%) | 26.29 (7.518) | 42.44 (11.069) | 25.77 (15.384) | 58.83 (16.703) |
| 30-49 | 174 (33.0%) | 21.71 (7.052) | 40.59 (9.277) | 20.32 (11.390) | 56.79 (17.671) |
| >=50 | 82 (15.6%) | 21.24 (8.096) | 40.48 (11.109) | 21.00 (10.502) | 59.43 (16.67) |
| F | 26.55 | 2.12 | 9.95 | 1.00 | |
| P | <.001 | .121 | <.001 | .370 | |
| Only child | 526 (100%) | 23.99 (7.816) | 41.52 (10.539) | 23.22 (13.708) | 58.25 (17.024) |
| Yes | 227 (43.2%) | 25.01 (7.364) | 41.48 (10.583) | 24.50 (14.182) | 59.66 (17.137) |
| No | 299 (56.8%) | 23.21 (8.070) | 41.55 (10.524) | 22.25 (13.279) | 57.180 (16.889) |
| t | 2.66 | −0.07 | 1.86 | 1.66 | |
| P | .008 | .941 | .063 | .099 | |
| Education | 526 (100%) | 23.99 (7.816) | 41.52 (10.539) | 23.22 (13.708) | 58.25 (17.024) |
| Until high School | 144 (27.4%) | 22.85 (8.278) | 41.99 (11.025) | 21.65 (13.670) | 55.05 (19.419) |
| Undergraduate or above | 382 (72.6%) | 24.42 (7.603) | 41.34 (10.360) | 23.81 (13.694) | 59.46 (15.890) |
| t | −2.05 | 0.63 | −1.62 | −2.43 | |
| P | .041 | .527 | .107 | .016 | |
| Occupation | 526 (100%) | 23.99 (7.816) | 41.52 (10.539) | 23.22 (13.708) | 58.25 (17.024) |
| Student | 225 (42.8%) | 26.27 (7.542) | 42.25 (11.313) | 26.02 (15.323) | 59.43 (16.206) |
| Unemployed | 6 (1.1%) | 27.00 (5.020) | 43.00 (8.025) | 24.33 (10.690) | 44.67 (15.680) |
| Employed | 285 (54.2%) | 22.07 (7.508) | 40.67 (9.625) | 20.80 (11.843) | 57.65 (17.646) |
| Retired | 10 (1.9%) | 25.70 (9.989) | 48.40 (15.643) | 28.60 (14.661) | 56.90 (15.337) |
| F | 13.47 | 2.46 | 6.82 | 1.78 | |
| P | <.001 | .062 | <.001 | .150 | |
| Residential district | 526 (100%) | 23.99 (7.816) | 41.52 (10.539) | 23.22 (13.708) | 58.25 (17.024) |
| Hubei Province | 83 (15.8%) | 24.02 (8.687) | 42.35 (11.543) | 22.05 (13.901) | 58.51 (17.761) |
| Other Province | 443 (84.2%) | 23.98 (7.653) | 41.36 (10.347) | 23.44 (13.677) | 58.20 (16.903) |
| t | 0.05 | 0.78 | −0.85 | 0.15 | |
| P | .964 | .435 | .396 | .881 |
CPSS = Chinese version of perceived psychological stress scale, PCL-5 = PTSD checklist for DSM-5, PSSS = perceived social support scale, SAS = self-rating anxiety scale.
3.2. Associations of social support with stress, anxiety, and PTSD during COVID-19 outbreak
Multiple regressions analysis was conducted with social support as independent variable, stress, anxiety, and PTSD as dependent variables after controlling demographic variables. Table 2 showed the associations of social support with psychological stress, anxiety, and PTSD symptoms for the public during the regular prevention and control of COVID-19 in China. Results illustrated that social support was negatively associated with stress, anxiety and PTSD symptom, indicating the protective effect of social support on mental health.
Table 2.
The association between social support and psychological stress, anxiety, and post-traumatic stress disorder.
| Dependent variable | Independent variable | F | P | R2 | B | β | t | P |
| Stress (CPSS) | Social support | 21.285 | <.001 | 0.213 | −0.174 | −0.378 | −9.669 | <.001 |
| Anxiety (SAS) | Social support | 9.818 | <.001 | 0.105 | −0.207 | −0.334 | −8.015 | <.001 |
| Post-traumatic stress disorder (PCL-5) | Social support | 5.683 | <.001 | 0.059 | −0.16 | −0.199 | −4.651 | <.001 |
Sex, age, education, occupation, residential district, and only child were controlled.
CPSS = Chinese version of perceived psychological stress scale, PCL-5 = PTSD checklist for DSM-5, SAS = self-rating anxiety scale.
3.3. The influence of income on mental health
To explore the influence of income on mental health and to exclude the influence of occupation, we first coded non-student samples’ occupations into 2 categories. One type was called “stable occupation” (n = 168, 55.8%), for example, workers of state-owned enterprises, civil servant et al; the other was “unstable occupation” (n = 133, 44.2%), for example, employees of private enterprises, freelance et al. In China, socioeconomic situations generally had a great influence on the income of individuals with unstable occupations but not on individuals with stable occupations. Independent t test showed that participants with stable occupation showed less income loss (t = 6.14, P < .001) and were more satisfied with income after COVID-19 massive outbreak (t = 5.50, P < .001).
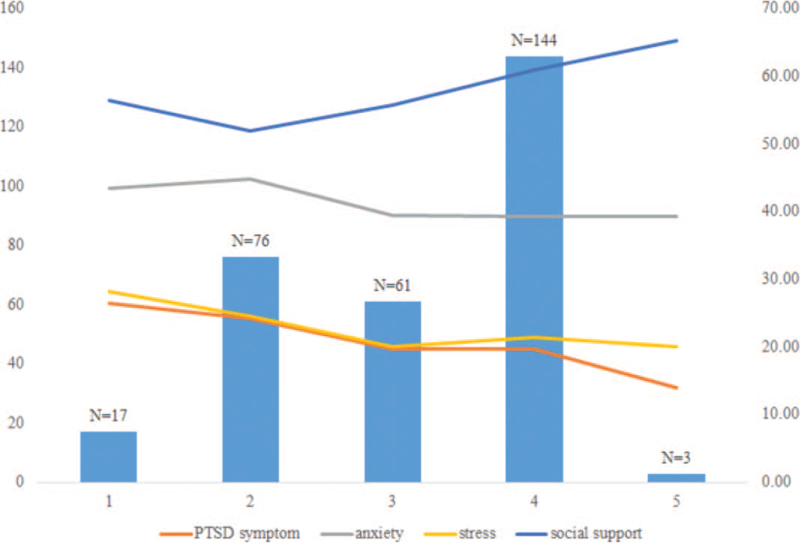
Figure 1 showed how the psychological responses changed with social support and income loss. To analyze the association between income and mental health, multiple regression analyses was conducted with income loss, income satisfaction, and social support as independent variable, stress, anxiety, and PTSD as dependent variables. Demographic variables including the occupation code were controlled. The results were showed in Table 3 social support and income loss were dependent predictors of stress, anxiety, and PTSD. However, the association between income satisfaction and mental health was not significant.
Figure 1.
Change of psychological responses with social support and income loss. Bar chart represents number of income loss of different levels; line chart represents social support, PTSD (Post-traumatic stress disorder) symptoms, anxiety and stress, respectively. X-axis represents levels of income loss. Y-axis (left) represents sample sizes; Y-axis (right) represent the scores of scales.
Table 3.
The associations between income, social support, and mental health.
| Dependent variable | Independent variable | F | P | R2 | B | β | t | P |
| Stress (CPSS) | Income change | 11.128 | <.001 | 0.233 | −1.185 | −0.155 | −2.612 | .009 |
| Income satisfaction | −0.055 | −0.008 | −0.136 | .892 | ||||
| Social support | −0.178 | −0.413 | −7.843 | <.001 | ||||
| Anxiety (SAS) | Income change | 6.392 | <.001 | 0.139 | −1.521 | −0.152 | −2.425 | .016 |
| Income satisfaction | −0.851 | −0.097 | −1.533 | .126 | ||||
| Social support | −0.171 | −0.304 | −5.458 | <.001 | ||||
| Post-traumatic stress disorder (PCL-5) | Income change | 3.559 | <.001 | 0.071 | −2.138 | −0.177 | −2.716 | .007 |
| Income satisfaction | 0.177 | 0.017 | 0.255 | .799 | ||||
| Social support | −0.164 | −0.241 | −4.156 | <.001 |
Sex, age, education, occupation, residential district and whether is the only child were controlled.
CPSS = Chinese version of perceived psychological stress scale, PCL-5 = PTSD checklist for DSM-5, SAS = self-rating anxiety scale.
4. Discussion
This study sought to explore public mental health status during the “normal prevention and control of COVID-19” in China. Although the breakout of COVID-19 was initially under control in China, the public still showed high levels of anxiety, psychological stress, and posttraumatic disorder symptoms, with the prevalence of 19.8%, 24.7%, and 23.8%, respectively. Age showed a significant impact on mental health in the present study, and this result was consistent with previous studies illustrating the young group (18-29 years) were more vulnerable to psychological disorder compared to the middle aged group (30-49 years) and elder group (>=50 years).[1] However, the present study failed to find a significant different between male and female participants in mental health problems, which was different from some other previous studies.[22–24] But there were other evidences that gender had no impact on mental health.[25,26] However, considering the imbalance of male (44.5%) and female ratio (55.5%) in the present study, this result should be interpreted with caution. Meanwhile, only child and employment status also linked with mental health, but Hubei contact history was not related to any type of psychological problems. There was evidence that being to Wuhan city, the capital of Hubei province during COVID-19 was related with more PTSD symptoms, which was different from the current study.[7] However, considering the time of study, this difference could be a reflection of the changing situation of epidemic prevention and control. In fact, at the beginning of the current study, the public health emergency response level in Hubei Province had changed from Level-1 to Level-2,[6] indicating the situation had greatly improved in Wuhan city and Hubei province.
Using multiple regression analysis, the study showed the protective effect of social support on mental health, which was in line with a number of previous studies.[15,27] Furthermore, by adding the income loss as an independent variable, the study revealed that income loss was negatively related with mental health problems and the association was significant even when social support was added, indicating a separate contribution to mental health of income loss and social support. This result illustrated a protective role of keeping stable income during COVID-19 outbreak. Previous studies had showed that depression was related with disposable income loss of young mothers during the financial crisis in Ireland[28] and that income reduction due to severe acute respiratory syndrome could predict psychological disorders with an odds ratio of 25.0, which was the highest among various risk factors.[13] The previous study had also showed low income was related with mental health after 4 weeks of quarantine in Austria[29] and our study extended previous work by adding a dynamic perspective that not only low income would associated with mental health deficit but income loss would also related with psychological health. These results indicated that during “normal prevention and control of COVID-19”, economic development would be an important factor for mental health.
The current study found income loss was the risk factor and social support was the protective factor of mental health during normal control of COVID-19 and these 2 factors had independent effects on mental health. In previous studies, social support was seen as a mediator between economic status and mental health and happiness. For example, Chu et al[30] showed that social support played a fully mediating role between family income and the well-being in senior high school students. However, in other studies, income not only affected mental health through the mediation effect of social support but also had a direct effect on mental health, indicating the independent effect of income.[31] In the present study, social support mainly referred to subjective support and income loss was an objective index, they might work through different mechanisms. It also should be noticed that in Chu et al's[30] study, high school students with no personal income were researched, and family income and personal income might have different influence on mental health for different population.
Limitation of the present study included sampling method and sample characteristics. On-line survey and snowball sampling resulted in a biased sample in the present study. For example, proportions of young individuals and students were high in the study. Also, as a cross-section study, the casual relationship among income loss, social support and psychological health could not be tested. Further studies could explore the direct effect of income loss and social support on mental health with psychological experiments or longitude studies.
5. Conclusions
The present research revealed the mental health status in Chinese general public during the normal control period of COVID-19. Prevalence of anxiety, PTSD symptoms and stress problems were relatively high, reaching 19.8%, 23.8%, and 24.7% respectively. Social support was a protective factor for mental health, and income change was a risk factor for mental health and had a separate effect on mental health beyond social support. These results indicated the importance of economic development and promoting psychological health during the normal control period of COVID-19.
Author contributions
Conceptualization: Chenwei Huang and Fan Zhang.
Data curation: Zihao Liu and Yuwei Kang.
Formal analysis: Chenwei Huang and Qiyun Feng.
Funding acquisition: Fan Zhang.
Investigation: Chenwei Huang and Borui Zhang.
Methodology: Chenwei Huang, Borui Zhang, and Qiyun Feng.
Resources: Huiguang Ren.
Supervision: Fan Zhang.
Writing – original draft: Chenwei Huang, Borui Zhang, and Qiyun Feng.
Writing – review & editing: Chenwei Huang, Fan Zhang.
Footnotes
Abbreviations: COVID-19 = Corona Virus Disease 2019, CPSS = Chinese version of perceived psychological stress scale, PCL-5 = PTSD checklist for DSM-5, PSSS = perceived social support scale, PTSD = post-traumatic stress disorder, SAS = self-rating anxiety scale.
How to cite this article: Huang C, Feng Q, Zhang B, Ren H, Liu Z, Kang Y, Zhang F. Income and social support related with mental health during COVID-19 outbreak in China. Medicine. 2022;101:10(e29022).
CH, QF, and BZ contributed equally to this work.
This research was funded by Scientific research project of Shanghai Health Commission, grant number 20204Y0287.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Alkhamees AA, Alrashed SA, Alzunaydi AA, Almohimeed AS, Aljohani MS. The psychological impact of COVID-19 pandemic on the general population of Saudi Arabia. Compr Psychiatry 2020;102:152192. 10.1016/j.comppsych.2020.152192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].González-Sanguino C, Ausín B, Castellanos MÁ, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun Health 2020;87:172–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].World Health Organization. Coronavirus Disease (COVID-19) Dashboard. (2020). Available at: https://covid19.who.int/. Accessed July 1, 2020. [Google Scholar]
- [4].Krishnamoorthy Y, Nagarajan R, Saya GK, Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res 2020;293:113382. 10.1016/j.psychres.2020.113382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Xinhua News Agency. Chinese novel coronavirus pneumonia epidemic situation up to June 13th. Available at: http://www.nhc.gov.cn/yjb/s7860/202006/b85d2888ac6e4a96b2a0d5e0a6d66f95.shtml. Accessed June 13, 2020. [Google Scholar]
- [6].Health commission of Hubei Providence. Public health emergency response reduces from Level-1 to Level-2. Available at: http://wjw.hubei.gov.cn/bmdt/dtyw/202005/t20200502_2258014.shtml. Accessed May 2, 2020. [Google Scholar]
- [7].Zhang F, Shang Z, Ma H, et al. Epidemic area contact history and sleep quality associated with posttraumatic stress symptoms in the first phase of COVID-19 outbreak in China. Sci Rep 2020;10:22463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].National Bureau of Statistics of China. Preliminary GDP calculation results for the first quarter of 2020. Available at: http://www.stats.gov.cn/tjsj/zxfb/202004/t20200417_1739602.html. Accessed April 17, 2020. [Google Scholar]
- [9].Shevlin M, McBride O, Murphy J, et al. Anxiety, depression, traumatic stress, and COVID-19 related anxiety in the UK general population during the COVID-19 pandemic. BJPsych Open 2020;6:e125. 10.1192/bjo.2020.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Cao W, Fang Z, Hou G, Xu X, Dong J, Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res 2020;287:112934. 10.1016/j.psychres.2020.112934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Hamadani JD, Hasan MI, Baldi AJ, et al. Immediate impact of stay-at-home orders to control COVID-19 transmission on socioeconomic conditions, food insecurity, mental health, and intimate partner violence in Bangladeshi women and their families: an interrupted time series. Lancet Glob Health 2020;8:e1380–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Lahav Y. Psychological distress related to COVID-19–the contribution of continuous traumatic stress. J Affect Disord 2020;277:129–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Mihashi M, Otsubo Y, Xin Y, Nagatomi K, Hoshiko M, Ishitake T. Predictive factors of psychological disorder development during recovery following SARS outbreak. Health Psychol 2009;28:91–100. [DOI] [PubMed] [Google Scholar]
- [14].Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull 1985;98:310–57. [PubMed] [Google Scholar]
- [15].Qi M, Zhou S, Guo Z, et al. The effect of social support on mental health in Chinese adolescents during the outbreak of COVID-19. J Adolesc Health 2020;67:514–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Yang X, Yang X, Kumar P, Cao B, Ma X, Li T. 2020. Social support and clinical improvement in COVID-19 positive patients in China. Nurs Outlook 2020;68:830–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Lee H, Oh J, Kawachi I, et al. 2019. Positive and negative social support and depressive symptoms according to economic status among adults in Korea: cross-sectional results from the Health Examinees-Gem Study. BMJ Open 2020;9:e23036. 10.1016/S2214-109X(20)30366-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Jiang Q. Perceived Social Support Scale (PSSS) (In Chinese). Chin Mental Health J 1999;13: (supplementary issue): 131–3. [Google Scholar]
- [19].Yang T, Huang H. 2003. An epidemiological study on stress among urban residents in social transition period. Chin J Epidemiol 2020;24:760–4. [PubMed] [Google Scholar]
- [20].Zung WW. 1971. A rating instrument for anxiety disorders. Psychosomatics 2020;12:371–9. [DOI] [PubMed] [Google Scholar]
- [21]. Weathers, F.W., Litz, B.T., Keane, T.M., Palmieri, P.A., Marx, B.P., Schnurr, P.P. (2013). The PTSD checklist for DSM-5 (PCL-5) – LEC-5 and extended criterion a [Measurement instrument]. Available at: https://www.ptsd.va.gov/. Accessed March 25, 2020. [Google Scholar]
- [22].Li Q, Miao Y, Zeng X, Tarimo CS, Wu C, Wu J. Prevalence and factors for anxiety during the coronavirus disease 2019 (COVID-19) epidemic among the teachers in China. J Affect Disord 2020;277:153–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Liu N, Zhang F, Wei C, Jia Y, Liu W. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res 2020;287:112921. 10.1016/j.psychres.2020.112921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020;17:1729. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Ahmeda MZ, Ahmedb O, Aibaoa Z, Hanbina S, Siyuc L, Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian J Psychiatr 2020;51:102092. 10.1016/j.ajp.2020.102092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res 2020;288:112954. 10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Catabay CJ, Stockman JK, Campbell JC, Tsuyuki K. Perceived stress and mental health: the mediating roles of social support and resilience among black women exposed to sexual violence. J Affect Disord 2019;259:143–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Kiernan FM. Income loss and the mental health of young mothers: evidence from the recession in Ireland. J Ment Health Policy Econ 2019;22:131–49. [PubMed] [Google Scholar]
- [29].Pieh C, Budimir S, Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (COVID-19) lockdown in Austria. J Psychosom Res 2020;136:110186. 10.1016/j.jpsychores.2020.110186 10.1016/j.jpsychores.2020.110186. Epub 2020 Jul 3. Erratum in: J Psychosom Res. 2020 Dec;139:110278. PMID: 32682159; PMCID: PMC7832650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Chu X, Li Y, Wang X, Wang Y, Lei L. The Association between family income and well-being: the mediating role of social support and the moderating role of gender (In Chinese). Psychol Dev Educ 2019;35:478–85. [Google Scholar]
- [31].Schulz AJ, Israel BA, Zenk SN, et al. Psychosocial stress and social support as mediators of relationships between income, length of residence and depressive symptoms among African American women on Detroit's eastside. Soc Sci Med 2006;62:510–22. [DOI] [PubMed] [Google Scholar]