Abstract
Takotsubo cardiomyopathy (TTS) has become a recognised clinical entity since the Japanese scientist Sato first described it in 1990.
Despite an increasing number of confirmed cases, especially during the COVID-19 pandemic, its pathophysiology remains incompletely understood, and decision-making differs in the diagnosis and treatment. In addition, it is not evident whether a significant increase in TTS is due to better understanding among practitioners and widespread access to coronary angiography, or if it is a reflection of an actual increase in incidence.
We analysed a series of international research studies from 1990 to 2021. Beyond epidemiology and clinical presentation, we evaluated and summarised fundamental knowledge about various predisposing factors, with particular attention to the iatrogenic impact of certain drugs, namely antidepressants, chemotherapy, and antiarrhythmics.
Furthermore, we highlighted the main pathophysiological theories to date. In addition, based on published studies and clinical cases, we investigated the role of numerous diagnostic approaches in the differential diagnosis of TTS and identified predictors of TTS complications, such as cardiogenic shock, ventricular fibrillation, and left ventricular thrombi. Accordingly, we sought to propose a diagnostic algorithm and further treatment management of TTS under the presence of possible complications to help practitioners make more informed decisions, as the initial presentation continues to pose a challenge due to its close similarity to acute coronary syndrome with ST-elevation.
In conclusion, this article examines Takotsubo cardiomyopathy from different perspectives and, along with future systematic reviews and meta-analyses, can be of particular interest to practising cardiologists and researchers in developing clinical guidelines.
Keywords: Takotsubo, Cardiomyopathy, Risk factors, Diagnostics, Complication, Treatment
1. Introduction
Takotsubo syndrome (TTS), also known as stress-induced cardiomyopathy or broken heart syndrome, is reversible cardiomyopathy characterised by acute transient left ventricular (LV) dysfunction and is mostly associated with LV apical distension visualised during systole [1].
It was initially thought to be a benign condition, but it is now recognised to be associated with severe complications such as life-threatening ventricular arrhythmias and cardiogenic shock. In addition, the incidence of Takotsubo syndrome has been increasing [2], [3], and the process appears to be multifactorial. Recognition and increased awareness, along with improved technologies, have helped the diagnostic evaluation of TTS. However, there are still no generally established clinical guidelines for diagnosing, treating, and preventing TTS.
This article aims to review the current situation of TTS, briefly summarize pathophysiological mechanisms, discuss various risk factors, propose a diagnostic algorithm and different treatment strategies of the patients with stress-induced cardiomyopathy, and highlight future challenges.
2. Epidemiology
The exact prevalence of TTS is uncertain because it can be misdiagnosed and hardly distinguished from acute coronary syndrome (ACS) without advanced diagnostic tools. In the United States Nationwide Inpatient Sample discharge records the reported prevalence of TTS was 5.2/100,000 for females and 0.6/100,000 for males, thus accounting for 0,02% of hospitalizations [4], [5]. It has also been reported that the combined annual incidence of principal and secondary TTS hospitalizations increased from 5.7/100,000 person-years in 2007 to 17.4/100,000 in 2012 [2], [3]. Coronary artery disease (CAD) was frequently present in patients with TTS, and according to the HORIZONS-AMI trial in 2014, TTS was identified in 2.1% of female ACS patients and 0.5% of all ACS patients [6].
Important to note a considerable increase in the incidence of TTS during the COVID-19 pandemic. As reported in the retrospective large cohort Cleveland Clinic study, the proportion of TTS cases among all ACS patients before and during the pandemic was 1,8% and 7,8%, respectively [7].
The multicenter GEIST (German Italian Stress Cardiomyopathy) Registry analysed the recurrence rate of TTS which accounted for 4.0% among 749 consecutive patients with TTS and a median follow-up of 830 days. Relatively younger age and the presence of cardiovascular risk factors such as arterial hypertension were significantly higher in patients with recurrence episodes [8].
According to the International Expert Consensus Document on Takotsubo Syndrome, about 90% of TTS patients are women aged 67–70 [5]. Although women are more predisposed to stress-induced cardiomyopathy caused by emotional triggers, TTS tends to develop more often among male patients after a stressful physical triggering event with a higher mortality rate because of underlying critical illnesses [9], [10].
Based on the analyses of various types of studies, Okura et al. have demonstrated that emotional stress was strongly related with TTS development in about 20–39%, while physical stress was seen in 35–55% of all cases [11].
Moreover, TTS has been described in children, including premature neonates [5]. A retrospective analysis of the Healthcare Cost and Utilisation 2012 and 2016 Kids' Inpatient Database revealed TTS in 3.1 young patients per 100,000 discharges, aged 12–20. TTS occurrence was mainly associated with psychiatric illnesses, substance use disorder, and sepsis. Currently, there is no specific guideline regarding the diagnosis and management of TTS in children. Although it is an uncommon condition among children, it is essential to be aware of its association with other comorbidities [12].
3. Predisposing factors
The main predisposing factor includes female sex in a postmenopausal period. Some researchers linked the predominance of women to the absence of cardioprotective effects of androgens, which are observed in men. In particular, testosterone inhibits oxidative stress by activating cardiomyocyte antioxidant enzymes via androgen receptors [13] or by converting to estradiol [14].
In addition to hormonal changes, genetic and psychogenic factors, mental disorders, and other comorbidities influence TTS development (Table 1).
Table 1.
Predisposing factors.
| Predisposing factors | Description | Authors, year of paper |
|---|---|---|
| Genetic factors | People carrying the T allele at the rs2234693 locus of the ESR1 and rs1271572 locus of the ESR2 gene have a higher risk of TTS development. | Pizzino et al., 2017 [185] |
| The Gln27Glu substitution at the rs1042714 within the adrenergic receptor B2 was observed more frequently in healthy controls than in TTS patients. | Vriz et al., 2011 [186] | |
| The Arg389Gly substitution at the rs1801253 of the adrenergic receptor B1 was more frequently found in TTS patients. | Vriz et al., 2011 [186] | |
| There is no significant difference between TTS and healthy controls in the Arg389Gly substitution at the rs1801253 of the adrenergic receptor B1. | Figtree et al., 2013 [187] Mattsson et al., 2018 [188] |
|
| Each patient carried predicted deleterious variants affecting known cardiomyopathy genes. | Kalani et al., 2016 [189] | |
| A patient with TTS was detected with a heterozygous mutation in exon 9 of the TTN gene: c.1489G > T (p. E497X). | Keller et al., 2018 [190] | |
| APOE, MFGE8, ALB, APOB, SAA1, A2M, and C3 genes were classified as key genes of TTS, could be helpful either as diagnostic biomarkers or molecular targets for the treatment of TTS. | Pan et al., 2020 [191] | |
| Postmenopausal women/ hormonal changes | Oestrogen may be considered a relative protective hormone; its decline may predispose to TTS development. | Pelliccia et al., 2017 [56] |
| Oestradiol has been reported to be protective against catecholamine surge; reducing oestrogen levels may increase the risk of acquired long QT syndrome in TTS. | El-Battrawy et al., 2018 [179] | |
| Oestradiol deficiency was not identified as a risk factor for TTS. | Möller et al., 2018 [156] | |
| Vitamin D deficiency was more prevalent in patients with TTS. Probably, lack of Vitamin D leads to suboptimal myocardial reserve and worse hemodynamics in affected female patients. | Dande et al., 2013 [192] | |
| Psychogenic factors/ psychiatric disorders | Higher rates of neurologic or psychiatric disorders (55.8% vs. 25.7%) were seen in patients with TTS than those with acute coronary syndrome. | Templin et al., 2015 [75] |
| Common psychiatric disorders among patients with TTS included depression (n = 98; 39%), anxiety (n = 44, 17%), alcohol exposure (n = 35, 14%), suicidal thoughts (n = 30, 12%), and severe mental conditions (n = 25, 10%). Psychiatric illnesses were reported to be triggers for TTS development in 61% cases. | Carroll et al., 2020 [15] | |
| Among psychiatric events, long-lasting psychological distress and anxiety appeared to play a significant role in TTS predisposition. | Galli et al., 2019 [193] | |
| Anxiety disorders were reported to have a higher predisposition to TTS compared to myocardial infarction. Conversely, the prevalence of depression was the same between TTS and myocardial infarction groups. Role of personality appeared to not influence TTS development compared to myocardial infarction. | Salmoirago-Blotcher et al., 2016 [194] | |
| Comorbidities | Concomitant diabetes mellitus in TTS patients is associated with an increased risk for worst outcomes. | Abe et al., 2020 [182] |
| Underlying critical illness contributed most to mortality. Male patients, who have underlying critical illness more frequently, had a significantly increased mortality rate than female patients. | Brinjikji et al., 2012 [10] | |
| Underlying atrial fibrillation in TTS patients has a significantly higher all‐cause mortality rate than patients without atrial fibrillation (OR = 2.19, 95% CI: 1.57–3.06, p < 0.001). | Prasitlumkum et al., 2018 [195] | |
| TTS triggered by physical stress (i.e., asthma, surgery, trauma, drugs) had worse short and long-term outcomes, higher mortality rates, recurrences, and readmissions. |
Núñez-Gil et al., 2015 [73] |
Table summarising main predisposing factors in the TTS development.
TTS — Takotsubo cardiomyopathy, ESR1 – Estrogen Receptor 1, ESR2 – Estrogen Receptor 2.
Of note, despite the clear presence of mental disorder as a clinical substrate and trigger of TTS, psychiatric treatment during hospitalisation was provided in only 32% of cases. Furthermore, psychiatric disorders were not frequently managed during follow-up [15].
The effect of race on the incidence and prognosis of TTS has also been studied. For example, small-sampled research has demonstrated an increased in-hospital mortality rate among patients of African-American (AA) descent [16], [17]; however, a large population-based study has not reported racial differences for mortality [10]. Similarly, after a fully adjusted analysis, a recent study involving 97,650 patients, which included differences in age, comorbidities, and socioeconomic factors, has demonstrated that the African-American race was not associated with the worse in-hospital outcome than Caucasians.
In 2020, Jabri et al. carried out a cohort study that showed a significant increase in the number of confirmed TTS associated with the COVID-19 pandemic [7].
In addition, based on retrospective case series, complications and mortality rates in secondary TTS associated with COVID-19 are higher in older patients (>70 years), patients with lower blood pressure (<110 mm Hg), lower left ventricular ejection fraction (LVEF < 45%), presence of right ventricle (RV) involvement, and mitral regurgitation [18].
4. Drugs as risk factors for TTS
4.1. Antidepressants
Despite the high prevalence of depression and other psychiatric disorders among patients with TTS, certain antidepressants may still contribute to TTS development. Therefore, a series of clinical cases were analysed to identify the drugs contributing to TTS (Table 2). According to this data review, the TTS risk is highest in serotonin-norepinephrine reuptake inhibitors use, i.e., venlafaxine, desvenlafaxine, duloxetine, milnacipran. In addition, the use of selective serotonin reuptake inhibitors (SSRIs) like fluoxetine or selective norepinephrine reuptake inhibitors (SNRIs) as atomoxetine, or tetracyclic antidepressants such as maprotiline, may also be associated with TTS development.
Table 2.
Antidepressants as risk factors for TTS development.
| Drugs | Drugs for the treatment | Number of patients | Author, year |
|---|---|---|---|
| Venlafaxine, Desvenlafaxine | — | 6 | Neil et al., 2012 [196] |
| Desvenlafaxine | Bisoprolol, perindopril (combination therapy of β-blockers and ACE inhibitors) |
1 (F) | Gurunathan, 2018 [197] |
| Duloxetine | Carvedilol (the patient used it before the TTS), the addition of ACE inhibitors | 1 (F) | Selke et al., 2011 [198] |
| Duloxetine | — | 1 (F) | Rotondi et al., 2011 [199] |
| Maprotiline | Bisoprolol, verapamil, warfarin (already used by the patient), therapy with medosalam, cyproheptadine | 1 (F) | Sasaki et al., 2012 [200] |
| Milnacipran | Enalapril, carvedilol, ACE inhibitors (combination therapy of β-blockers and ACE inhibitors) | 1 (F) | Forman et al., 2011 [201] |
| Venlafaxine | ILE, ECLS and CytoSorb® | 1 (F) | Schroeder et al., 2017 [202] |
| Venlafaxine | Aspirin, enalapril, metoprolol (combination therapy of β-blockers and ACE inhibitors) | 1 (F) | Vasudev et al., 2016 [203] |
| Venlafaxine | Combination therapy of β-blockers and ACE inhibitors | 1 (F) | Christoph et al., 2010 [204] |
| Venlafaxine | Ramipril, carvedilol, diuretics | 1 (F) | Elikowski et al., 2019 [205] |
| Atomoxetine, Fluoxetine | — | 1 (F) | Naguy, 2016 [206] |
| Fluoxetine | Heparin, clopidogrel, a chewable aspirin, atorvastatin, lisinopril (only ACE inhibitors) | 1 (F) | Conrad et al., 2016 [207] |
| Atomoxetine, Fluoxetine | — | 2 | Verduin, 2016 [208] |
| Fluoxetine | Metoprolol, ramipril (combination therapy of β-blockers and ACE inhibitors) | 1 (F) | Prasad, 2009 [209] |
Table summarising studies on the role of antidepressants in the TTS development.
ACE inhibitor — Angiotensin-converting enzyme inhibitor, TTS — Takotsubo cardiomyopathy, ILE — Intravenous Lipid Emulsion, ECLS — Extracorporeal Life Support.
SNRIs block the capture of neurotransmitters in the presynaptic membrane, which increases the level of noradrenaline. This process leads to activation of the sympathoadrenal system. The mechanism of action of SSRIs on the development of TTS is not fully understood, although overdoses and drug interactions have been reported. In 2002, a study showed that only fluoxetine increased norepinephrine concentrations among SSRIs, contributing to the development of TTS. In addition, it was found that its extracellular concentrations in the prefrontal cortex at a dose that increased extracellular monoamines (in this case, serotonin) were 242 nM, enough to block 5-HT(2C) receptors, which is a possible mechanism for fluoxetine-mediated catecholamine increase [19].
Therefore, before starting antidepressant therapy, physicians are advised to obtain a comprehensive medical and family history, paying attention to sudden cardiac death and heart failure. Furthermore, according to the analysed data, tricyclic antidepressants, SSRIs, and SNRIs should not be prescribed in patients with heart disease due to a high risk of drug-drug interaction resulting in an increased sensitivity of cardiomyocytes to catecholamines. For that reason, in case of drug-induced TTS, these drugs should be withdrawn and, if possible, replaced with other medications (for example, paroxetine, sertraline, or plant-based drugs such as valerian or motherwort).
4.2. Chemotherapy
Carbone A. et al. have found that TTS development was associated with a broad spectrum of antitumoral drugs used in various cancers. For example, treatment with 5-fluorouracil, capecitabine, trastuzumab, and immune checkpoint inhibitors was found in 36.5%, 9.7%, 9.7%, 9.7% of TTS cases, respectively [20]. The exact mechanism of chemotherapy-induced cardiotoxicity of 5-fluorouracil and capecitabine is not fully known. However, coronary spasm, thromboxane A2 activation, and electrolyte imbalances are the most likely effects [21], [22], [23], [24]. Trastuzumab prompts extracellular signal-regulated kinase activation, leading to increased regulation of the mammalian target of rapamycin (mTOR) [25]. Activated mTOR phosphorylates Unc51-like kinase that inhibits autophagy, thereby disrupting the ability of cardiomyocytes to utilise toxic cellular substrates, leading to direct myocardial damage [26]. Bevacizumab disrupts cardiomyocyte survival via vascular endothelial growth factor (VEGF) signalling inhibition [27]. It is hypothesised that inhibition of VEGF reduces nitric oxide production in the endothelium, leading to vasoconstriction, increased peripheral vascular resistance, and blood pressure. Reduced nitric oxide levels contribute to the expression of plasminogen activator inhibitor 1, leading to a further increase in blood pressure and cardiac stress [28]. The cardiotoxic effect of immune checkpoint inhibitors is still unknown.
4.3. Antiarrhythmic drugs
In addition, based on a series of clinical cases, antiarrhythmic drugs have been identified as risk factors for TTS development, especially drugs such as flecainide, sotalol, amiodarone, lidocaine, and xylocaine (Table 3). Flecainide leads to marked inhibition of the upstroke of the cardiac action potential, delayed inactivation of the slow sodium channel, and blocks the delayed rectifier potassium channels (IKr3), resulting in a prolonged QT interval, potentially preceding a TTS [29]. Amiodarone by blocking potassium rectifier currents leads to an increase in the action potential duration and prolongation of the effective refractory period in cardiomyocytes and therefore can prolong QTc interval. Amiodarone also interferes with beta-adrenergic receptors (e.g., beta-1), calcium and sodium channels, which can induce arrhythmias and worsen the course of TTS [30].
Table 3.
Potential drugs as risk factors for TTS development.
| Antineoplastic drugs | ||||||
|---|---|---|---|---|---|---|
| 5-Fluorouracil | Age, sex | Evaluation criteria | Duration of observation | Relapse /complications | Additions | Reference |
| 48, M | Chest pain ECG: abnormal ST Echo-CG: severe LV dysfunction, hypokinesia in the apical and median segments, LVEF 15% |
5 months and 3 weeks | Relapse after 1.5 months with cardiac arrest and acute HF | oxaliplatin, calcium folinate | Basselin C et al., 2011 [210] | |
| 58, F | Increased serum troponin T levels by 0.39 mg / L, creatine kinase 156U / L, Echo-CG: severe diffuse hypokinesis of the LV, LVEF 15%; ECG: non- specific lateral ST changes and poor R wave progression |
3 months | No | oxaliplatin, folinic acid | Stewart T et al., 2010 [211] | |
| 48, M | Tachycardia, troponin-I 2,87 ng / ml ECG: negative T at V4,5; Echo-CG: severe LV dysfunction with hyperkinesis of the mid-apical segments and hyperkinesis of the basal segments, LVEF 15% |
13.5 months | Ventricular fibrillation, death | docetaxel, cisplatin, irinotecan, folinic acid | Ozturk M et al., 2013 [21] | |
| 35, M | Echo-CG: severe LV dysfunction, LVEF 19% | 6 months | pulmonary oedema | oxaliplatin, folinic acid | Saif M et al., 2016 [212] | |
| 42, F | ECG: elevation of the ST segment in the anterior leads and depression of the ST segment in the inferolateral leads Echo-CG: LVEF 17%, general hypokinesis with apical akinesia |
3 months | LV thrombus | No | Kumar D et al., 2021 [213] | |
| Capecitabine | 80, F | ECG: hyperacute T waves in the anterior precordial leads; Ventriculography: apical ballooning with a hyperdynamic base; Echo-CG: LVEF 55–60%, apical akinesia |
6 weeks | No | clonazepam, atorvastatin, meclizine | Bhardwaj P et al., 2019 [214] |
| 55, M | Troponin T 89 ng / l ECG: elevation of the ST segment by 1–2 mm in V2-6 and about 1 mm in -aVR, II and aVF Echo-CG: LVEF 15–20%, severe LV hypokinesis; |
1 week | No | No | Y-Hassan S et al., 2013 [215] | |
| 47, M | Serum troponin I increased to 0.19 ng/ml; ECG: ST-segment elevations in inferolateral leads I, II, aVL and V6, and ST depression and T wave inversion in leads V1-V2; Ventriculography: anomaly of movement of the anterior apical wall with LVEF 35%; Echo-CG: general hypokinesia |
6 weeks | No | doxorubicin, paclitaxel, vinorelbine, tamoxifen, and anastrozole | Qasem A et al., 2016 [216] | |
| Gemcitabine | 65, F | TnT 111 ng / ml; ECG: T wave inversion in precordial leads; Echo-CG: LV apical balloon, LVEF 25–30% |
Still now | No | vinorelbine | Ozbay B et al., 2021 [217] |
| 62, F | troponin I − 9552 ng / l, BNP − 175 pg/ml, NT-proBNP − 2691 pg/ml ECG: inversion of T waves in leads above the anterior and lateral walls; Ventriculography: akinesia of the apex, apical and middle segment of the anterior wall, LVEF 38%; | 4 days | No | cisplatin | Zalewska-Adamiec M et al., 2021 [218] | |
| Trastuzumab | 65, M | Troponin I 0.219 ng / ml, creatinine kinase (CC) 104 U / l; Fever, shortness of breath, chest pain; ECG: negative T waves in V2 and ST-segment elevation in V3 - V6, apical akineдsia and LV hypokinesia with an apical balloon, LVEF 33,1% |
23 days | RDS, death (as a result of carcinoma) | oxaliplatin | Matsumoto T et al., 2019 [219] |
| 40, F | Troponin 2.64 μg / L;HR 105 btm/min, arterial hypotension (98/50 mm Hg); Echo-CG: LVEF 45%; left ventriculography: severe hypokinesia of the middle LV segment |
1 year and 8 months | No | carboplatin, docetaxel | Burgy M et al., 2014 [220] | |
| 50, F | Chest pain, sweating, nausea, increased troponin T levels (0.15 pkg/ml); ECG: negative T waves in leads V1-3, I, aVL. |
6 weeks | No | carboplatin, docetaxel | Khanji M et al., 2013 [221] | |
| Antiarrhythmic drugs | ||||||
| Flecainide | 48, M | ECG: initially QT prolongation (QTc 624 ms), then negative T in leads I, aVL, V2 - V6 | A few months | No | Emotional stress before hospitalisation | Bodziock G et al., 2019 [222] |
| Sotalol | 82, M | Echo-CG: LV hypokinesis with LVEF 25%; ECG: QT prolongation with abnormal T waves |
3 weeks | No | Emotional stress before hospitalisation | Friedman P et al., 2010 [223] |
| Amiodarone | 79, F | Echo-CG: akinesia of the apical and middle segments with hypokinesia in the basal segments; ventriculography: apical dyskinesia, with the apical balloon and preserved LVEF | 3 months | New episode of ischemic colitis with bowel perforation, generalised sepsis, and death | Hyperthyroidism type I | Capel I et al., 2017 [224] |
| Lidocaine | 36, F | Palpitations, nausea, troponin-T 1.03 ng / ml; NT-pro-BNP 717 pg / ml; ECG: ST-segment elevation and negative T wave in aVL; Ultrasound: hypokinesia of the basal segments and hyperkinesis of the apex with moderate mitral regurgitation |
1 month | No | No | Tomcsányi J et al., 2008 [225] |
| 14, F | Hypotension (89/56 mm Hg); troponin I 2.42 ng / ml; proBNP 8284 pg / ml; total creatine kinase 217UI / l; Echo-CG: dilated LV with hypokinesia of the middle and basal segments, LVEF < 30%; ECG: non-specific ST wave abnormalities in V4-V5; |
9 days | No | Propofol, Atropine | Faleiro Oliveira J et al., 2016 [226] | |
| Xylocaine | 18, F | HR 140 bpm; BP 86/52 mm Hg.; increased troponin and creatine kinase ECG: non-specific ST wave abnormalities; Echo-CG: LV apical hypokinesis with anomalies of the anterior wall movement, LVEF 15–20% |
6 days | No | Epinephrine | Glamore M et al., 2012 [227] |
Table summarising studies on various drugs as potential risk factors for TTS.
M — Male, F — Female, ECG — Electrocardiography, Echo-CG — Echocardiography, LVEF — Left ventricular ejection fraction, LV — Left ventricle, TnT — Troponin-T, BNP — Brain natriuretic peptide, NT-proBNP — N-terminal-pro brain natriuretic peptide, RDS — Respiratory distress syndrome, HR — Heart rate, BP — Blood pressure.
Although it was difficult to distinguish which factor may have played a significant role in TTS development, a detailed cardiovascular assessment, prior to initiating antiarrhythmic therapy, and routine ECG screening for QT interval prolongation will minimise the risks of life-threatening arrhythmia resulting in the development of “stunned” myocardium with the features of apical ballooning syndrome in susceptible patients.
5. Pathogenesis
The pathogenesis of TTS remains elusive and unclear. However, the main pathogenic hypotheses include catecholamine surge, switching in G-coupled proteins, systemic inflammation, endothelial dysfunction, coronary vasospasm and excessive activation of the sympathetic nervous system (SNS) (Table 4).
Table 4.
Pathogenesis.
| Pathogenetic pathways | Description | Authors, year of paper |
|---|---|---|
| Excessive activation of the sympathetic nervous system | Sympathetic nervous system activation in response to stress leads to increased catecholamine release via the hypothalamic–pituitaryadrenal axis. | Wang et al., 2020 [31] |
| The role of the limbic system | The presence of dysregulated neural networks in several stress-associated limbic brain regions such as the amygdala, insula, anterior cingulate cortex, prefrontal cortex, and hippocampus was highlighted among patients with TTS. | Suzuki et al., 2014 [35] Radfar et al., 2021 [36] Hiestand et al., 2018 [37] Pereira et al., 2016 [38] |
| Catecholamine effects | A higher level of circulating catecholamines was found in patients with stress-associated TTS than patients with myocardial infarction. | Wittstein et al., 2005 [47] |
| Elevated concentrations of norepinephrine in coronary sinuses were found in patients with TTS. | Kume et al., 2008 [46] | |
| No elevated plasma catecholamine concentrations were detected in TTS patients. | Madhavan et al., 2009 [48] | |
| Intravenous administration of adrenaline or beta-receptor agonists can cause TTS symptoms. | Abraham et al., 2009 [228] | |
| Nearly 68% of drug-induced TTS cases were associated with catecholamine stimulation. | Kido et al., 2017 [49] | |
| Catecholamines can affect sarcoplasmic-Ca2 + -ATPase (SERCA2a) by stimulating β-adrenoreceptors and reducing sarcolipin concentrations. | Nef et al., 2009 [45] Nef et al., 2010 [44] |
|
| The effect of catecholamines on β2-adrenoreceptors leads to activation of nitric oxide synthase, which stimulates nitric oxide synthesis. This results in the formation of peroxynitrite, which damages DNA and stimulates the DNA repairing enzyme poly(ADP-ribose) polymerase to be released. | Dawson et al., 2015 [52] | |
| Activation of adrenoreceptors enhances the differentiation of cardiomyocytes from iPSC-CMs. The main pathway of iPSC-CMs differentiation regulation is mediated through the alpha1-receptors. |
Li et al., 2017 [55] | |
| Switching in G-coupled proteins | Switching epinephrine affinity from beta2-adrenoreceptors-Gs at low epinephrine concentration to Gi at high epinephrine concentration leads to acute apical cardiac depression in a Takotsubo rat model. This epinephrine-affinity switching seems to be cardioprotective and decrease catecholamine-induced myocardial toxicity during acute stress. | Paur et al., 2012 [42] |
| In the basal myocardium, norepinephrine contributes to hypercontractility due to the high density of sympathetic nerve endings. Conversely, the apical myocardium has an increased density of beta-adrenoreceptors. Thus, high free epinephrine leads to switching to beta2-receptors-Gi followed by apical myocardium dilatation. | Yoshikawa, 2015 [229] | |
| Systemic inflammation | TTS is associated with a low-grade chronic inflammatory state. It consists of a myocardial macrophage inflammatory infiltrate and an increase in systemic proinflammatory cytokines (i.e., serum interleukin-6, chemokine ligand 1, and classic CD14++CD16-). | Scally et al., 2019 [62] |
| Endothelial dysfunction | Endothelial dysfunction is significantly increased in TTS patients compared to healthy controls. | Naegele et al., 2016 [57] |
| TTS is significantly associated with migraine and the Raynaud phenomenon, which suggest a vasomotor dysfunction pathway in the TTS pathogenesis. | Scantlebury et al., 2013 [230] |
Table summarising main pathogenetic pathways of TTS.
TTS — Takotsubo cardiomyopathy, DNA — Deoxyribonucleic acid, ADP — Adenosine diphosphate, iPSC-CMs — Induced pluripotent stem-cell-derived cardiomyocytes.
One of the most popular theories of pathogenesis is activation of the sympathetic nervous system (SNS) in response to stress, which results in over-release of catecholamines [31]. Increased SNS activity was first demonstrated in a study by Akashi et al. who used 123I-metaiodobenzylguanidine (MIBG) myocardial scintigraphy [32]. Ten years later, Vaccaro et al. confirmed the presence of increased SNS activity in patients with TTS, using the evaluation of spontaneous baroreflex control of sympathetic activity and microneurography [33]. Although the part of the sympathetic nervous system is heavily discussed, the role of the parasympathetic nervous system (PNS) often has been neglected. Norcliffe-Kaufmann et al. assessed sympathetic and parasympathetic activity using baroreflex, cognitive, and emotional stimulation; their results showed a reduction in parasympathetic modulation of heart rate in patients with TTS [34]. Some recent neuroimaging studies provide strong evidence that alterations in the central autonomic network (CEN) are found to be present in patients with TTS. Other studies have demonstrated the presence of dysregulated neural networks in several stress-associated limbic brain regions such as the amygdala, insula, anterior cingulate cortex, prefrontal cortex, and hippocampus among patients with TTS [35], [36], [37], [38]. Although alterations were found, it is still unclear whether they are predisposing or causal factors for TTS development. It was also observed that when the spinal cord was transected at the C7-Th1 level in rats, followed by adrenaline administration, myocardial damage was significantly reduced, confirming the role of the central nervous system in the pathogenesis of TTS [39], [40].
There are two phases in the catecholamine hypothesis. The first phase is characterised by a massive release of catecholamines in response to stress. The second phase reflects cardiovascular reaction to a rapid increase in plasma level of catecholamines. As a result, apical dysfunction, myocardial stunning, and paradoxical vasodilation develop, culminating in a decrease in cardiac output, systemic hypotension, and acute heart failure [41]. These changes are considered as a cardioprotective mechanism that is caused by beta-receptors Gs-Gi switching [42]. Although Gi-pathway inhibition was associated with decreased cardiac akinesia in a rat model, it significantly increased mortality [43]. With reference to these findings, TTS patients may benefit from beta-blockers because they bind to and inhibit the Gs-protein metabolic pathway in cardiomyocytes via beta-adrenoreceptors downregulation. In addition, it has been shown that catecholamines can affect sarcoplasmic-Ca2 + -ATPase (SERCA2a) by stimulating β-adrenoreceptors and reducing sarcolipin concentrations. At the same time, phospholamban is dephosphorylated and decreases the affinity of Ca2 + -ATPase for calcium. A subsequent increase in phospholamban/SERCA2a ratio leads to contractile dysfunction [44], [45].
Even though a high level of circulating catecholamines was found in patients with stress-associated TTS, the role of catecholamine effects is still not entirely understood [46], [47]. Contradicting research demonstrated no differences in elevated plasma catecholamine concentrations between TTS and STEMI patients, which the following factors can explain: first of all, TTS patients are a heterogeneous group with variable mechanisms of systolic dysfunction; in addition, laboratory data discrepancies can be attributed to the difficulty in measuring catecholamines, differences in assays, and cut-off values for what is considered normal [48]. Conversely, the systematic review of 157 cases demonstrated that 68.2% of drug-induced TTS cases were associated with catecholamine stimulation, while 8.9% were due to chemotherapy-induced coronary vasospasm [49].
It has been demonstrated that the effect of catecholamines on β2-adrenoreceptors leads to activation of nitric oxide synthase (NOS), which stimulates nitric oxide (NO) synthesis [50]. In addition, the synthesis of reactive oxygen species is increased in patients with TTS. This results in the formation of peroxynitrite - a product of the reaction of NO and reactive oxygen species superoxide [51]. Peroxynitrite damages DNA and stimulates the DNA repairing enzyme poly(ADP-ribose) polymerase (PARP) to be released. However, it is important to mention that this enzyme requires significant energy for its activation, and therefore impairment of myocardial energetics is seen in patients with TTS [52]. Therefore, further studies are needed to investigate the role of a catecholamine surge in TTS development.
Several studies have shown that activation of β-adrenoreceptors stimulates the proliferation of neonatal cardiomyocytes [53], mesenchymal stem cells [54], as well as the differentiation of cardiac embryonic stem cells (ESC). These studies suggested that the stimulation of β-adrenoreceptors can promote the differentiation and proliferation of induced pluripotent stem cell-derived cardiomyocytes (iPSC-CMs). Li et al. showed that activation of adrenoreceptors enhances the differentiation of cardiomyocytes from iPSC-CMsh, which is regulated through the alpha1-receptors pathway [55]. Further studies are needed to confirm these results.
Another hypothesis of TTS pathogenesis is endothelial dysfunction, which may represent an essential link between stress and myocardial dysfunction. Endothelial dysfunction has been suggested as a plausible causative factor explaining the subepicardial and/or microvascular vasospasm. In a prospective observational study, authors investigated changes in endothelial function and concluded that 22 TTS patients demonstrated impaired flow-mediated vasodilatation compared to 21 matched controls (p = 0,016). Transient myocardial ischemia related to endothelial dysfunction and subsequent cardiomyocyte stunning might be the possible causes of the reversible LV dysfunction in TTS [56], [57]. Recently, plaque rupture and thrombosis followed by transient ischaemia were considered as one of the possible mechanisms of TTS development. The basis for this hypothesis was the detection of atherosclerotic plaques in some patients using optical coherence tomography in patients with TTS. However, Haghi et al. rejected this hypothesis as they detected no ruptured plaque in any patient [58]. Similar results were obtained 6 years later by Eitel et al. in a single-centre study [59]. In the meantime, it should be noted that obstructive coronary lesions can be observed approximately in 1 out of 10 TTS patients pointing to the possible association of TTS with CAD [60], [61].
TTS was also associated with a chronic inflammatory state [62] in a multicenter study, and increased endothelial and vasomotor dysfunction was found among TTS patients [57], [63]. To date, elevated levels of IL-6 and IL-10 in TTS have been explained by the fact that catecholamines activate endothelial cells and vascular smooth muscle cells, which produce these cytokines. In a rat model of hypoxic myocardial stress, Yamauchi-Takihara et al. found that several factors, including epinephrine, can induce IL-6 mRNA expression [64]. The correlation of IL-10 with elevated epinephrine levels was also shown in a study by T. Ohtsuka et al. [65]. Therefore, the inflammatory cascade may be proportionally enhanced by catechol-aminergic myocardial endothelial damage due to severe peripheral vasoconstriction.
The growth of TTS during the COVID-19 pandemic can not be overlooked and is explained by three leading theories to date:
-
1.
The cytokine storm leads to increased release of tumour necrosis factor-α, IL-6, IL-1β, and catecholamines into the bloodstream, contributing to TTS development [66]. The exact mechanism of the effect of proinflammatory interleukins on catecholamine release is unknown. However, a systematic review has shown that a cytokine storm (observed in Covid-19) can lead to direct catecholamine toxicity and myocardial damage, contributing to TTS development [67]. This hypothesis is also supported by a clinical case of a patient with TTS who recovered after IL-6 inhibitor administration [68].
-
2.
Activation of the sympathetic nervous system causes catecholamine-induced myocardial stunning and, as a result, TTS [69] and microvascular dysfunction [70].
-
3.
An immense emotional stress caused by a cataclysm and a high mortality rate may trigger TTS development. In comparison, according to the US nationwide study, the highest incidence of TTS cases was identified in Vermont and Missouri (the Tropical Storm Irene and Joplin Tornado struck these states in the year of the study, and these natural disasters claimed hundreds of lives) [71].
Furthermore, the series of ongoing research on the pathogenetic mechanisms of TTS attempts to explain the development of the syndrome at the molecular level. In particular, overexpression of microRNA-16 and microRNA-26a specifically reduced baseline contractility of apical but not basal cardiomyocytes in vitro and functionally interacted to predispose to the cardiac depression seen in TTS [72]. Thus, it is vital to learn more about pathogenetic mechanisms of the condition to develop new ways of its prevention and treatment.
6. Classification
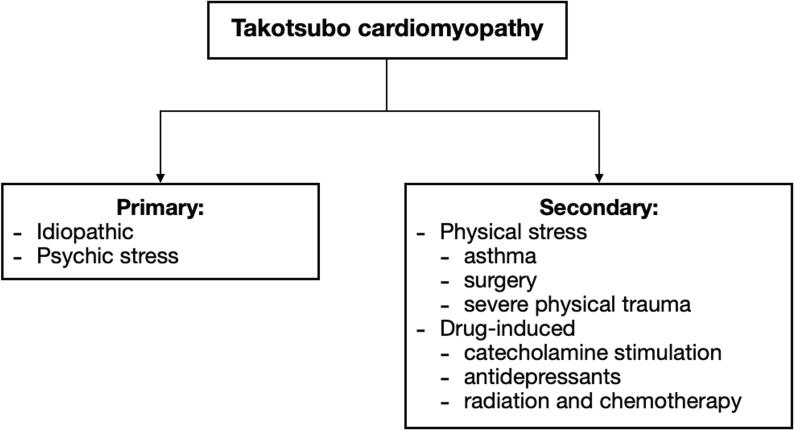
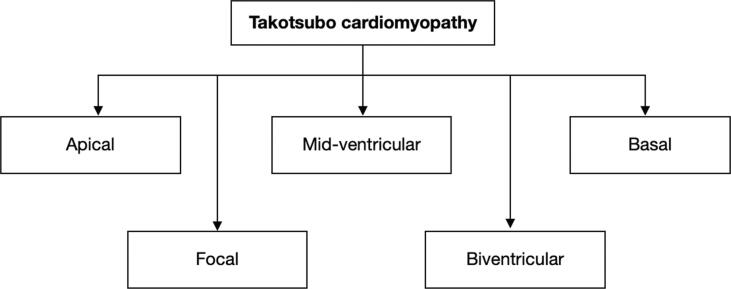
Today TTS is commonly divided into two clinical subtypes: primary and secondary (Fig. 1a). Primary TTS is a leading cause of hospital admission, commonly triggered by psychosocial stress, although emotional stress may not be identifiable in some cases. Secondary TTS develops among patients already admitted to hospitals due to other various conditions, such as asthma attack, surgical intervention, or severe physical trauma and may also involve drug-induced TTS (i.e., catecholamine stimulation, antidepressants, antiarrhythmics, radiation, and chemotherapy) [49], [73]. In addition, there is a clinically used classification based on the wall motion abnormality (WMA) location (Fig. 1b), which subdivides TTS into apical, mid-ventricular, basal, focal, and biventricular TTS [74].
Fig. 1a.
Classification of TTS based on etiology.
Fig. 1b.
Classification of TTS based on the location of WMA.
7. Clinical profile: Typical vs atypical TTS patient
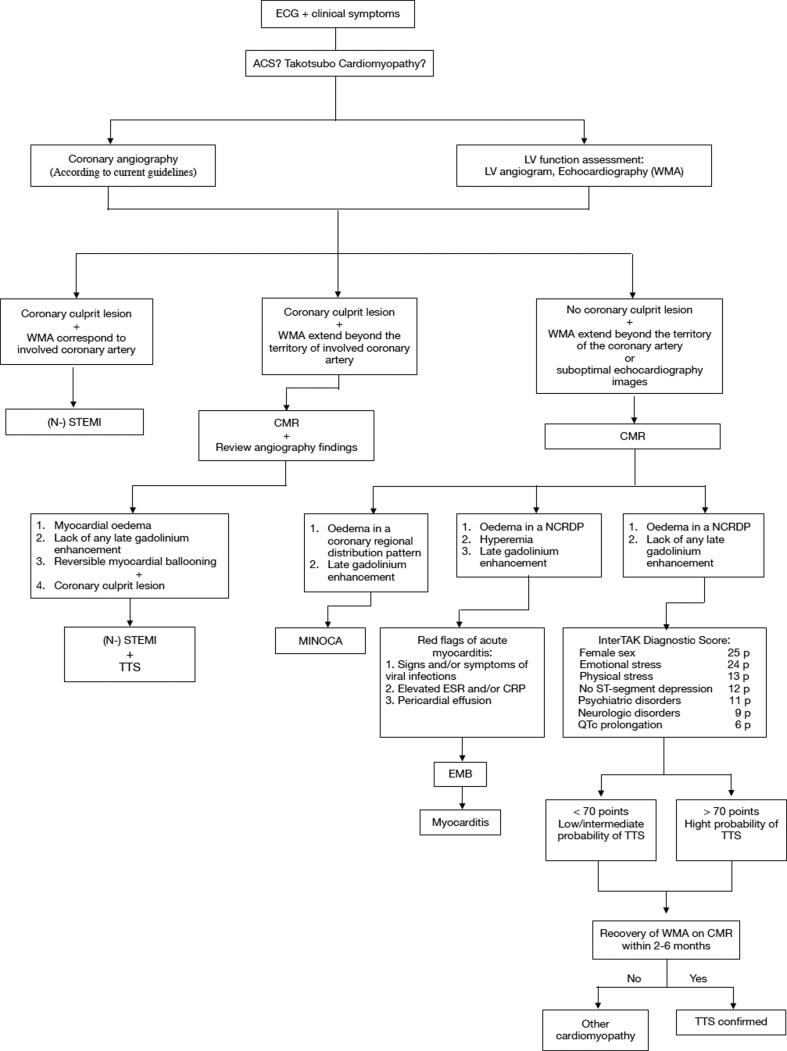
As described above, a typical TTS patient is a postmenopausal woman over 50 years old with symptoms similar to myocardial infarction, such as sudden onset chest pain, dyspnea, or syncope, provoked by emotional stress and characterized by the development of apical ballooning. In the meantime, concomitant CAD is reported among patients with TTS, with a prevalence ranging from 10 to 29%. Therefore, patients with TTS and obstructive CAD are often misdiagnosed as a classical acute coronary syndrome, and differentiation can be challenging [75]. In addition, there are various scenarios where clinicians need to differentiate TTS from myocarditis, myocardial infarction with nonobstructive coronary arteries (MINOCA) (Fig. 2).
Fig. 2.
Diagnostic algorithm for undifferentiated chest pain and/or shortness of breath: Takotsubo Cardiomyopathy and/or Acute Coronary Syndrome. ECG – Electrocardiography, ACS – Acute coronary syndrome, LV – Left ventricle, WMA – Wall motion abnormalities, (N-) STEMI – (Non-) ST-elevation myocardial infarction, CMR – Cardiac magnetic resonance, NCRDP – Noncoronary regional distribution pattern, MINOCA – Myocardial infarction with nonobstructive coronary arteries, ESR – Erythrocyte sedimentation rate, CRP – C-reactive protein, EMB – Endomyocardial biopsy, TTS – Takotsubo cardiomyopathy, p – points.
Underlying chronic conditions (e.g., diabetes mellitus, asthma), cerebrovascular events (e.g., ischemic stroke, transient ischemic attack), or seizures may often predispose to TTS, which underpins the role of extracardiac factors in the development of the disease. In this regard, symptoms may include atypical clinical manifestations (loss of consciousness, neurologic signs, or blood pressure dropping). Besides, TTS can manifest at a younger age, and patients are often admitted with the symptoms of acute heart failure and cardiogenic shock, pulmonary edema, or stroke [5].
According to the International Takotsubo Registry, among 1750 patients from 9 countries, atypical presentation, including younger age, neurologic symptoms, ST depression, and lower level of B-type natriuretic peptide (BNP), accounted for 20% of all cases, while outcomes and prognosis were comparable between patients with a typical and atypical presentation [76]. Therefore, notwithstanding a better understanding of TTS diagnosis, it is of critical value to closely monitor patients with both typical and atypical clinical presentation, as a diagnostic reasoning bias cannot be eliminated.
8. Diagnostics
TTS was first classified as primary cardiomyopathy in 2006 [77]. Since then, several diagnostic criteria have been proposed for TTS diagnosis. One of the most widespread diagnostic tools is the revised version of Mayo Clinic Diagnostic Criteria for TTS (2008), which incorporates transient wall-motion abnormalities, absence of a potential coronary culprit, myocarditis, and pheochromocytoma [63]. In addition, the European Society of Cardiology (ESC) combined up-to-date data and created the International Diagnostic Takotsubo Criteria (InterTAK diagnostic criteria) in 2018 [5], which included pheochromocytoma as a possible trigger and a secondary cause of TTS. Most importantly, coronary artery disease does not rule out TTS because of the possible coexistence of these two illnesses, and according to some data, ACS can instigate TTS [75], [78], [79], [80]. Therefore, in 2019 Heart Failure Association proposed the updated diagnostic criteria, where the presence of obstructive coronary lesion is no longer considered an exclusion, and among such patients, WMA may extend beyond the culprit lesion. Also, the ventricular systolic function recovery on imaging in 3–6 months was added to the criteria [81]. The comparison of the diagnostic criteria of Revised Mayo Clinic Diagnostic Criteria, InterTAK, and Heart Failure Association criteria 2019 are presented in Table 5.
Table 5.
Comparison of the main diagnostic criteria.
| Diagnostic criteria | Revised Mayo Clinic Diagnostic Criteria 2008 [63] | InterTAK Diagnostic Criteria 2018 [5] | Heart Failure Association criteria 2019 [81] |
|---|---|---|---|
| Transient Wall Motion Abnormalities | + | + | + |
| Stress as a trigger | + | + | + |
| Neurological disorders as a trigger | not specified | + | not specified |
| New ECG abnormalities | + | + | + |
| Cardiac biomarkers elevation | + | + | + |
| Serum natriuretic peptide elevation | not specified | + | + |
| Coronary artery disease | Absence of obstructive coronary disease | Significant coronary artery disease is not a contradiction | Absence of culprit atherosclerotic CAD to explain the pattern of temporary LV dysfunction observed |
| Pheochromocytoma | Absence | May serve as a trigger | not specified |
| Absence of Infectious myocarditis | + | + | + |
| Postmenopausal women | not specified | Predominantly affected | not specified |
| Systolic function recovery | not specified | not specified | Within 3–6 months |
Table summarising three main diagnostic criteria: Revised Mayo Clinic Diagnostic Criteria 2008, InterTAK Diagnostic Criteria 2018, Heart Failure Association criteria 2019.
ECG — Electrocardiography; CAD – coronary artery disease; LV – left ventricle.
It should be noted that patients with TTS are presented with the same set of clinical features as patients with ACS. Therefore, it is assumed that the characteristic clinical signs and ECG patterns allow the diagnosis of ACS and coronary angiography per the current guidelines [82] to exclude myocardial infarction in the first place. Based on InterTAK diagnostic criteria, we propose a practical diagnostic algorithm, modified after Napp and Bauersachs [83], including invasive visualisation of coronary arteries, echocardiography, and InterTAK Diagnostic Score (Fig. 2). Subsequently, three clinical scenarios are possible based on the results of coronary angiography and echocardiography.
The first scenario is the presence of coronary culprit lesion plus WMA corresponding to the involved coronary artery, which confirms (N-)STEMI. The second scenario is characterised by the coronary culprit lesion with WMA, which extends beyond the involved coronary artery, which may be due to the coexistence of two conditions, both (N-)STEMI and TTS. Finally, the third scenario is the absence of coronary culprit lesion, but the presence of WMA, which extends beyond a single epicardial coronary distribution, which subsequently requires a differential diagnosis of MINOCA, myocarditis, and cardiomyopathy, including TTS, by performing cardiac magnetic resonance (CMR) [82].
The laboratory and various instrumental methods for the diagnosis of TTS have different diagnostic values.
8.1. Biomarkers
In addition to slightly elevated Troponin T, as a result of acute myocardial damage, Takotsubo cardiomyopathy is characterised by a marked increase in plasma levels of B-type natriuretic peptide (BNP) and N-terminal prohormone of B-type natriuretic peptide (NT-proBNP) with its subsequent peak elevation within 24–48 h after onset of initial symptoms. Furthermore, the ratio of peak levels of NT-proBNP/troponin T was demonstrated to be most accurate in identifying patients with TTS among those admitted with (N)-STEMI [84].
Besides, in an acute phase of TTS, a higher elevation of growth differential factor-15 and proinflammatory cytokines has been described compared to STEMI. On the other side, many cardiac markers, such as troponins, creatine kinase-MB, or markers of vascular stress (i.e., copeptin), are lower in TTS patients than in STEMI [85]. Biomarkers of chronic Takotsubo stage have also been reported. According to Scally et al., high sensitivity troponin I, IL-6, IL-8, and BNP may be identified five months after TTS onset [62]. The summary data of biomarkers in TTS at admission versus STEMI and in the chronic phase of TTS are presented in Table 6.
Table 6.
Main biomarkers in the acute and chronic phase of TTS [85].
| Biomarkers | Acute phase (at admission) | Chronic phase (at 5 month) |
|---|---|---|
| Cardiac injury | NT-proBNP/troponin T ratio, BNP, Troponins, hs-TnT/CK-MB | Troponin I; BNP |
| Immune response/inflammation | Il-2; Il-4; Il-6; Il-10; TNF-a; Leukocytosis and high CRP; |
Il-6; Il-8 |
| Growth factor | Growth differential factor-15; endothelial growth factor | Not described |
| Markers of vascular stress | Copeptin | Not described |
| Messenger markers | microRNA-16 and microRNA-26a specifically reduced baseline contractility of apical cardiomyocytes | Not described |
Table summarising main biomarkers in both acute and chronic phases of TTS.
NT-proBNP – N-terminal prohormone of B-type natriuretic peptide; BNP – B-type natriuretic peptide; hs-TnT – Troponin T, high sensitivity; CK-MB – Creatine kinase-MB; TNF-a – Tumour necrosis factor α.
8.2. Electrocardiography (ECG)
ECG has a low value for TTS diagnostics due to its similar criteria to acute coronary syndrome. In TTS, ECG patterns of ST-elevation (STE) or T-wave depression (if present) demonstrate dynamic changes with the gradual resolution of ST-segment elevation, subsequent T-wave inversion, and QTc prolongation over days to weeks [86]. All these findings primarily require the exclusion of myocardial infarction. In 2016 a retrospective analysis was performed that included 200 patients with TTS and 200 patients with ACS. The authors proposed a practical ECG algorithm that diagnoses STE-TTS, STEMI, NSTE-TTS, or NSTEMI with >95% specificity, stating that ECG criteria could distinguish the two entities [86]. However, coronary angiography and ventriculography are needed to confirm the diagnosis.
Also, some differences in ECG features among AA patients with TTS have been described with the prevalence of diffuse T-wave inversion and more prolonged QTc [87].
8.3. Echocardiography
In contrast, echocardiography is essential in visualising WMA extending beyond the territory of the involved coronary artery, which is the main indication of TTS. Therefore, echocardiography criteria may include the following [76], [88], [89], [90]:
-
a)
LV regional WMA, which frequently involves apical and midventricular segments with the ballooning pattern. Conversely, the basal myocardial segments are often hyperkinetic. As a rule, WMA extends beyond a single epicardial coronary distribution;
-
b)
Transient LV dysfunction, often with a circumferential pattern, and a complete resolution of LV systolic function over 3–6 months;
-
c)
Improvement in E/e ratio during follow-up may be considered an additional useful indicator of LV function recovery;
-
d)
Distal Left Anterior Descending artery flow visualisation.
Moreover, echocardiography is a valuable method for diagnosing and visualising acute and long-term TTS complications, such as wall rupture, acute mitral regurgitation, left ventricle outflow tract obstruction (LVOTO), and RV involvement, pericardial effusion, thrombus formation, heart failure [91], [92].
8.4. Coronary angiography and left ventriculography
Although coronary anatomy in most TTS cases is normal or near-normal, it is crucial to evaluate coronary arteries in TTS diagnostic workup to exclude alternative diagnoses [93]. It should be noted that a one-vessel obstructive coronary artery disease does not exclude TTS, as LV wall motion abnormalities are often beyond the vascularisation zone of the involved vessel in TTS (Fig. 2). Conversely, nonobstructive lesions still may cause ACS [91], [94].
When echocardiography is inconclusive or unavailable, the angiographic biplane left ventriculography helps evaluate both LV function and its morphology by identifying the characteristic TTS patterns [90]. According to Desmet W et al., in almost one-third of observed TTS cases, the presence of a “very small zone of contractility in the most apical portion of the LV” coined as the “apical nipple” was identified during the biplane left ventriculography. At the same time, this sign was not seen among STEMI cases [95]. In addition, ventriculography helps identify the fluoroscopic “hawk’s beak” sign, which represents mid-ventricular region systolic ballooning with preserved LV apical contractility in TTS and can be used as an early diagnostic marker in differential diagnosis with ACS [96], [97].
The biplane left ventriculography is recommended along with cardiac catheterization through LV opacification in case of suspected ACS and non-obstructive coronary lesions [89]. Besides, left ventriculography may be helpful in detecting complications including acute mitral regurgitation or LV apical thrombi, as well as in determining intraventricular pressure gradients to detect LVOTO, particularly in haemodynamically unstable patients [98], [99].
8.5. Cardiac magnetic resonance (CMR)
CMR is an essential instrumental method due to its value for differential diagnosis and exclusion of myocarditis or myocardial infarction. The main CMR signs of TTS are the absence of late gadolinium enhancement and the presence of edema in a noncoronary regional distribution pattern (NCRDP). Complete CMR criteria include the following [100], [101], [102], [103]:
-
a)
LV dysfunction in a noncoronary regional distribution pattern with or without RV involvement;
-
b)
Myocardial edema located in the segments with WMA (akinesia or hypokinesia);
-
c)
Absence of significant necrosis or fibrosis;
-
d)
Absence of high-signal areas (>5 SD above normal) in late gadolinium enhancement images;
-
e)
Complete normalisation of LV ejection fraction on the follow-up CMR imaging.
Therefore, CMR is the gold standard for determining myocardial status [104]. In the future, the broader use of CMR may help in the early diagnosis of TTS and prediction of complications at admission.
8.6. Coronary computed tomography angiography (CCTA)
CCTA provides information on both coronary arteries and regional LV contraction [105]. Therefore, it may be recommended as an alternative diagnostic method in patients with suspected TTS and co-existing life-threatening conditions such as terminal malignancy, intracranial bleeding, sepsis since coronary angiography can add a considerable risk for complications [106]. In addition, considering quick accessibility to CCTA as a less invasive modality, it can be promptly used in the emergency settings for stable patients with low suspicion for ACS and strong clinical and echocardiographic findings compatible with TTS [107].
Beyond coronary artery disease itself, multislice computed tomography (MSCT) helps detect myocardial fibrosis and late iodine enhancement, thus is effectively used as an additional diagnostic tool in differential diagnosis with myocardial infarction and acute myocarditis [108], [109]. The method through multiplanar imaging also provides greater visualisation of LV thrombi, a not so infrequenlty seen TTS complication [110].
Routine CCTA can also provide a quantitative measurement of the coronary artery inflammation process by calculating the weighted pericoronary fat attenuation index (pFAI) [111], [112]. Galbazzi et al. have demonstrated an association between the significantly higher values of pFAI and coronary artery inflammation among patients with MINOCA and TTS than in the controls undergoing CCTA for atypical chest pain and no signs of obstructive coronary artery disease and no follow-up cardiac events [113]. Earlier, in a post-hoc analysis by Oikinomou et al., high values of pFAI were associated with increased all-cause and cardiac mortality and, therefore, can enhance prediction of cardiac risks along with coronary calcium in the current CCTA assessment [114]. Integration of pFAI into standard CCTA may advance cardiac risk-stratification in the presence of nonobstructive coronary plaques.
8.7. Cardiac nuclear imaging
Cardiac nuclear imaging has been successfully used in evaluation of myocardial perfusion and its metabolic activity [115]. It involves single-photon emission computed tomography (SPECT), positron emission tomography (PET), scintigraphy, combined PET/CMR, and combined PET/computed tomography (CT) scanners [116], [117].
SPECT demonstrates perfusion reduction due to regional myocardial wall thinning at the apex, which helps diagnose TTS [118]. Furthemore, the adrenergic hyperactivity seen among TTS patinets leads to “decreased uptake and increased washout of 123I metaiodobenzyl guanidine (MIBG) from the heart” during 123I-MIBG scintigraphy [32], [119]. Therefore, simultaneous use of 123I-MIBG and myocardial perfusion scintigraphy can help in the differential diagnosis of TTS from ACS in case regional innervation and myocardial scarring are parallel and matched [91].
Cardiac positron emission tomography (PET) features a mismatch between impaired myocardial glucose metabolism and normal myocardial perfusion in TTS, also known as «inverse flow metabolism mismatch» and can be employed in differential diagnosis with ACS [120]. The abnormal glucose metabolism and impaired sympathetic innervation detected by PET and 123I-MIBG scintigraphy, respectively, might help diagnose TTS in patients with delayed presentation during the LV wall motion recovery [121], [122].
Combined PET/CMR scanners can also provide a more comprehensive and non-invasive modality in the differential diagnosis of TTS from myocarditis, which is critical as the clinical course and prognosis vary considerably [123], [124], [125]. Combined PET-CT/CMR imaging is more informative than CMR alone in differential diagnosis with myocarditis, as it helps in quantifying the extent of inflammation along with the late gadolinium enhancement seen in patients with suspected myocarditis [126].
8.8. Autopsy
Some microscopic changes of TTS have been found in recent studies [127], [128].
-
a)
An extensive area of myocardial thinning;
-
b)
Evidence of Lewy body-like cytoplasmic inclusions in dorsal nuclei of the nervus vagus;
-
c)
Interstitial oedema with the accumulation of mononuclear leukocytes, lymphocytes, macrophages, polymorphonuclear leukocytes, mast cells, and eosinophils;
-
d)
Focal myocardial fibre degeneration and necrosis with foci of inflammatory cells (histiocytes, plasma cells, and polymorphonuclear leukocytes);
-
e)
Contraction bands with or without overt myocyte necrosis.
Researchers hypothesise that it is possible to make a differential diagnosis at autopsy and to diagnose TTS. Therefore, it is crucial for forensic medical examinations, treating physicians, and close relatives to understand the actual cause of the patient's death. Unfortunately, to date, there are few reports on the pathomorphological features of the heart (both macroscopic and microscopic), which means that more research is needed to look more closely at the pathophysiology of TTS and to identify independent predictors of fatal complications.
9. Management
9.1. TTS without any complications
There are currently several approaches to TTS pharmacotherapy. Table 7 summarises the results of significant clinical trials, including authors, years of publication, number of patients participating in the study, groups of prescribed drugs, follow-up time, side effects, and summary. The most commonly used therapy is a combination of angiotensin-converting enzyme (ACE) inhibitors and beta blockers. Despite the rapid recovery of left ventricular function with the beta-blockers monotherapy [129], the latter did not decrease mortality [130]. Nevertheless, data shows that the combination of beta blockers and ACE inhibitors can be more appropriate and beneficial [131], as ACE inhibitors prevent vasospasm, consequently reducing hypertension, and beta blockers inhibit the Gs-protein metabolic pathway preventing recurrence of TTS development.
Table 7.
Drug therapy for TTS.
| Medication group | Adverse Reactions | Conclusion | Number of patients | Follow-up duration | Authors, year of publication |
|---|---|---|---|---|---|
|
Beta-blockers and ACE inhibitors (17.1% of patients had a history of using antidepressants) |
3% — ventricular tachycardia 1,3% — ventricular thrombus 0,2% — rupture of the ventricular |
ACE inhibitors improve annual survival over a year, and Beta-blockers did not show any significant effect | 1750 (retrospective study) | Ten years | Templin et al. 2015 [75] |
| Aspirin, clopidogrel, statins, beta-blockers, ACE inhibitors | 2,8% — death 2,8% — congestive heart failure |
Refuse antiplatelet therapy; there are repeated hospitalizations (2,8%) |
117 | One year | Yayehd et al. 2016 [133] |
| Antiplatelet therapy, beta-blockers, ACE inhibitors, or statins | 7,3% — death 7,3% — apoplexy 26,7% — congestive heart failure |
Antiplatelet therapy is effective. No significant effect of beta-blockers and statins is shown | 206 (retrospective study) | Before patient’s discharge |
Dias et al. 2016 [132] |
| Beta-blockers, ACE inhibitors | 28% — relapse after six years 11% -- dyspnoea 14% — chest pain |
Reduction of TTS relapse rate | 1664 (multiple meta-regression analysis) |
Two years | Brunetti et al. 2016 [131] |
| Beta-blockers | 2% — death (early therapy) 2,4% — death (therapy during hospitalisation) |
Beta-blockers show equal efficacy both in the early stages and in later stages of the disease | 2110 (retrospective study) |
From the start of medication to condition improvement/death | Isogai et al. 2016 [130] |
| Levosimendan | No serious complications observed | Levosimendan infusion at 0.1 mcg/kg/min with its loading dose of 10 mcg/ kg added to standard medication therapy shortened the recovery time of the myocardium. | 42 (retrospective study) |
Hospitalisation period | Yaman et al. 2016 [231] |
| Enoxaparin, Warfarin | 2,2% — left ventricle thrombosis | Effective in the acute phase. It could be used up to 3 months for apoplexy prevention. | 12 | 984 days (about three years) | Santoro et al. 2017 [147] |
| Catecholamines | 3,2% — death | The use of catecholamines for maintaining blood circulation increases the risk of death | 114 | Four years | Ansari et al. 2018 [232] |
| Beta-blockers | 26,6% — death 7,7% — death resulting from heart diseases |
Hemodynamical and ECG monitoring of the condition of patients is necessary. Preference should be given to short-acting beta-blockers | 154 (retrospective study) |
One year | Madias et al. 2018 [233] |
| Beta-blockers | 95% — improvement of LV systolic function | Complex treatment of TTS with beta-blockers restores the systolic function of the left ventricle in a significantly higher number of patients | 124 (retrospective study) |
Three years | Ghalyoun et al. 2019 [129] |
| Beta-blockers, ACE inhibitors | 7,8% — arrhythmia 11,9% — cardiogenic shock 14,6% — thromboembolism 4% — transfer to the intensive care unit |
Combination of beta-blockers and ACE inhibitors is not an effective and safe method of managing TTS | 103 | Five years | Kummer et al. 2020 [234] |
Table summarising studies on pharmacological drugs used for TTS treatment.
ACE inhibitors — Angiotensin-converting enzyme inhibitor, TTS — Takotsubo cardiomyopathy, ECG — Electrocardiography, LV — Left ventricle.
Also, some studies suggest that haemodynamically stable patients should be given anticoagulants (heparin) or dual antiplatelet therapy (aspirin and clopidogrel) to prevent complications and recurrent TTS [132], [133]. However, there is controversy about the timing of their use, with some authors emphasising their use in the presence of a thrombus and others saying that they should be given as soon as the diagnosis of TTS has been made. Thus, more research is needed to determine the role of anticoagulants and dual antiplatelet therapy in TTS treatment.
It has been shown that single antiplatelet therapy with aspirin or dual therapy with aspirin plus clopidogrel can reduce major adverse cardiovascular events during hospital admission, including stroke [134]. However, in a study by Bertaina et al., it was shown that aspirin did not reduce the risk of recurrent TTS among patients discharged without subsequent use of beta-blockers and ACE inhibitors [135]. The same results were obtained by researchers who published the first meta-analysis to investigate the efficacy of drug therapy after patients were discharged [136]. A second meta-analysis and systematic review protocol studying the effect of aspirin on Takotsubo Syndrome have now been published [137]. In 2020, a study involving 1,533 patients with TTS demonstrated that aspirin use had no significant effect on the prognosis and development of complications after discharge [135].
9.2. TTS and heart failure (HF)
HF is treated with standard therapy, including beta blockers in a compensated condition, ACE inhibitors, or angiotensin receptor blockers (ARBs), and diuretics [138]. Respiratory support may be used if necessary. According to Kumar S et al., beta blockers reduce the incidence of cardiac rupture in TTS [139]. However, they are contraindicated in decompensated HF. The duration of treatment, on average, is up to 4 weeks if there is a visible improvement of the heart contractility, but treatment duration may vary depending on comorbidities and other risk factors. A study by Abanador-Kamper et al. concluded that treatment of HF is most effective during the first 1–2 months after hospital admission [140].
9.3. TTS and cardiogenic shock (CS).
According to 2020 Mayo Clinic data, 11% of patients develop CS in the first 72 h after admission, and 20–25% develop LVOTO [141].
-
1.
Without left ventricular outflow tract obstruction (LVOTO).
These patients usually develop hypotension. Either sympathomimetics or inotropic therapy can restore blood pressure. Given the pathogenesis of TTS, sympathomimetics (for example, norepinephrine or ephedrine) can worsen the patient's condition, so dobutamine/dopamine is the drug of choice because of their positive inotropic effect. If the patient develops moderate to severe LVOTO, inotropic therapy should be discontinued. If there is evidence of decreased blood supply to internal organs and persistent hypotension, vasopressor therapy can be used, which increases cardiac output and thus blood pressure. Severe hypotension and cardiogenic shock can lead to left ventricular dysfunction. In this case, mechanical circulatory support must be used to keep patients alive [142].
-
2.
With left ventricular outflow tract obstruction (LVOTO).
As already mentioned, inotropic therapy must be discontinued. Fluid resuscitation and beta-blockers are the therapy of choice in this case (in the absence of pulmonary congestion). In addition, an alpha-agonist (phenylephrine) can be used to increase the blood pressure and therefore the afterload, which may improve the patient's condition. Mechanical circulatory support (particularly intra-aortic balloon pump) should be used if the conservative therapy is ineffective [143].
Levosimendan, a non-catecholamine inotrope that does not increase myocyte uptake of cytoplasmic oxygen, is a rational therapeutic option in cardiogenic shock associated with TTS. In addition to its direct action as a calcium-sensitising agent, levosimendan has been found to mediate the opening of adenosine triphosphate (ATP)-dependent potassium channels in vascular smooth muscle cells [144]. Through this mechanism, levosimendan causes increased blood perfusion in crucial organs and systemic vasodilation. Furthermore, levosimendan also opens ATP-dependent potassium channels on the inner mitochondrial membrane, which is considered a cardioprotective effect of the drug [145].
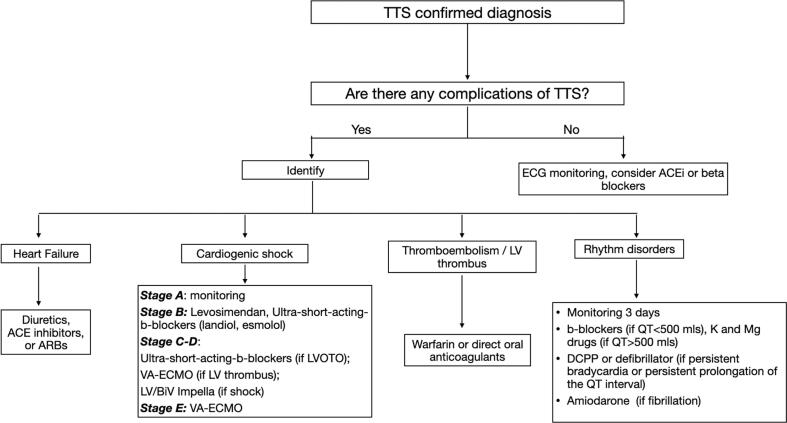
Depending on the stage of CS [146], relevant treatment measures should be applied (Fig. 3) [83]:
-
1.
Stage A (At risk): no tachycardia, hypotension, and normal lactate values. At this stage, only close monitoring of the patient's condition is necessary;
-
2.
Stage B (Beginning): hypotension (relative), tachycardia without hypoperfusion, and normal lactate values. Levosimendan and ultra-short-acting beta blockers (landiolol, esmolol) should be administered;
-
3.
Stage C (Classic): hypoperfusion, elevated lactate values, cardiac index < 2.2 L/min/m*2. In the absence of LVOTO, venoarterial extracorporeal membrane oxygenation (VA-ECMO) is required if there is a left ventricular thrombus, and LV or BiV Impella if no thrombus is found. If LVOTO is developed, the inotropic therapy should be discontinued, and ultra-short-acting beta blockers (landiolol, esmolol) should be prescribed instead. However, if the patient does not improve, VA-ECMO or LV/Biventricular (BiV) Impella should be started, depending on the presence or absence of thrombus, respectively;
-
4.
Stage D (Deteriorating): hypoperfusion and deterioration (Not refractory shock). Treatment is the same as for stage C;
-
5.
Stage E (Extremis): hypoperfusion, deterioration, refractory shock. VA-ECMO is needed at this stage;
Fig. 3.
Treatment of TTS complications. TTS - Takotsubo cardiomyopathy, ECG - Electrocardiography, ACEi - Angiotensin-converting enzyme inhibitor, ARB - Angiotensin II receptor blocker, LVOTO - Left ventricular outflow tract obstruction, VA-ECMO -Venoarterial extracorporeal membrane oxygenation, LV - Left ventricle, BiV - Biventricular, DCPP - Dual-chamber permanent pacemaker.
9.4. TTS and thromboembolism
The most commonly used drug for treating thrombosis in TTS is warfarin, a vitamin K antagonist. The optimal duration of treatment is three months, but depending on the size and location of LV thrombi, it can be prolonged [147]. To date, no studies are investigating the role of novel oral anticoagulants, so the question of their efficacy remains unresolved.
9.5. TTS and rhythm disorders
According to 2018 data, the prevalence of arrhythmias among 286 patients with TTS demonstrated that ventricular tachycardia (VT) and ventricular fibrillation (VF) accounted for two-thirds of the arrhythmic episodes [148]. In general, arrhythmias in TTS last for several days and stop under the influence of beta-blockers. However, there are a few recommendations that practising physicians should follow when managing a patient with TTS-associated arrhythmia [149]:
-
1.
Telemetry monitoring should be carried out for at least three days (1–2 days if the QT interval is restored);
-
2.
Beta-blockers should be discontinued, and potassium and magnesium should be given in patients with a QT interval > 500 ms;
-
3.
It is advisable to be alert to the list of antiarrhythmic drugs that prolong QT interval. Although intravenous amiodarone is the most commonly prescribed medication for treating life-threatening arrhythmia, a few cases of torsade de pointes have been reported [150], [151]. Early detection of concurrent electrolyte disturbances, careful QT interval monitoring, and awareness of drug interaction profiles can be helpful;
-
4.
In the case of torsades de pointes, intravenous magnesium is the first-line pharmacological treatment approach. In patients with prolonged QT interval and unresponsive to magnesium treatment, isoproterenol was shown to prevent torsades de pointes. Synchronised cardioversion is the preferred method for hemodynamically unstable patients who have a pulse. Patients with pulseless torsades should be defibrillated [152];
-
5.
A dual-chamber permanent pacemaker or defibrillator may be considered in persistent bradycardia or persistent prolongation of the QT interval. Bradyarrhythmias can be dangerous if they lead to complete atrioventricular heart block (AV-block). In the Stiermaier T et al. study, researchers suggested that patients in this situation need a permanent ventricular pacemaker with long-term follow-up, indicating that bradyarrhythmias in TTS require implantation of a permanent pacemaker [153]. In contrast, according to this study, polymorphic ventricular arrhythmias were restricted to the acute and subacute phase until repolarisation recovery, suggesting a temporary treatment approach (e.g., transient pacemaker, wearable defibrillators). However, further studies on device implantation in TTS are needed to confirm these results.
10. What lies ahead for the TTS treatment?
NACRAM trial is a multicenter, randomised, placebo-controlled trial consecutively testing the early use of intravenous N-acetylcysteine followed by oral administration of ramipril for 12 weeks in TTS management. The use of these medications is reasoned by their inhibiting effects on nitrosative stress and expression of the activator thioredoxin interacting protein. Both processes are presumably related to TTS pathogenesis. NACRAM evaluates the reduction of myocardial edema on magnetic resonance imaging of the heart. It also analyses the improvement of LV systolic function measured by global longitudinal strain on echocardiography, evaluates the quality of life and inflammation markers. NACRAM is likely to become the first prospective study that will evaluate treatment options of acute attacks of stress-induced cardiomyopathy [154].
Also, hormone therapy is currently being researched. The advantages of estradiol are still being studied and assessed in treating the chronic phase of TTS. Animal experimental trials have demonstrated a significant reduction in stress-induced LV dysfunction and arrhythmias. It indicates the importance of the sex hormone in the clinical management of TTS after complete recovery of LV function established by echocardiography. It has also been demonstrated that oestrogen has a cardioprotective effect against myocardial damage in the context of ischemia or reperfusion [155]. However, the available data about the role of estrogens is limited and contradictory. For instance, Möller et al. demonstrated no difference in sex hormones concentration among postmenopausal females with TTS and ACS, nor did they identify a protective effect of estradiol among those females under hormone replacement therapy (HRT) [156]. Further studies are needed to evaluate the role of hormones and the potential benefits of HRT in TTS.
To date, mineralocorticoid receptor antagonists and angiotensin-neprilysin receptor inhibitors (sacubitril/valsartan), which are effectively used in patients with chronic systolic heart failure, have not been studied among patients with TTS. However, these drugs may be of scientific interest for further research [157], [158].
A randomised interventional controlled trial involving 90 patients who have recovered from TTS is currently underway. The researchers are conducting a three-arm pilot trial of early rehabilitation, including standardised physical exercise training, cognitive behavioural therapy, and comparing the results with the standard clinical care. Key indicators are the “restored cardiac energetic status assessed by 31P-magnetic resonance spectroscopy, cortisol awakening response, global longitudinal strain by echocardiography, and the 6-minute walk test” [159].
11. Complications and their possible predictors
The most common complications of TTS are cardiogenic shock, rhythm disturbances, and thrombosis. We established the most likely independent predictors of various complications based on the data from multicenter studies, meta-analyses, and clinical cases (Table 8).
Table 8.
Independent predictors for TTS complications.
| Complication | HR (bpm) |
BP (mmHg) |
ST-changes | T changes | QT-interval (ms) |
Peak NTproBNP or BNP (pg/mL) |
Peak troponin (ng/mL) |
AB or dyskinesia, akinesia, hypokinesia | Basal function | EF (%) | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|
| VF | 100 | 94/70 | — | Elevation (V2-4) | 728 | 3.192 (NT proBNP) | — | Dyskinesia | Hyper | — | Taguchi M et al. 2020 [235] |
| VF | 110 | 147/98 | Elevation (II, III, aVF, V3-V6) | — | — | 3431.5 (BNP) | 0.813 | Dyskinesia | Hyper | — | Mizutani K et al. 2020 [236] |
| VF | — | 104/73 | Normal | inversion (V4-V6) | 539 | — | 0.143 | Akinesia | Hyper | 53 | Wakatsuki D et al. 2020 [237] |
| VF | 153 | 170/100 | Depression (V4-V6) | inversion (V3-V5) | 705 | 145. (BNP) | — | Hypokinesia | Hyper | — | Ishida T et al. 2017 [238] |
| AF | — | 110/65 | Depression | inversion (V2-V5) | 520 | 1437 (NT proBNP) | 670 | Akinesia | Hyper | 30 | O’Brien et al. 2021 [239] |
| AT and ischaemic stroke | 73 | 110/70 | Elevation (V1-V6) | — | 496 | — | 937 | Akinesia | Hyper | 38 | Iuliano G et al. 2021 [240] |
| AF | 114 | 133/64 | — | inversion (V5-V6) | — | — | 0.423 | AB and akinesia | — | 30 | Sattar Y et al. 2020 [241] |
| LVOTO | 110 | 90/60 | Elevation (III – aVF) | — | — | 3254 (BNP) | 5 | Akinesia | — | 30 | Attisano T et al. 2020 [242] |
| AT | 110 | 100/60 | Elevation (I-III, aVL, aVF, V2-V6) | — | — | — | 2,2 | Hypokinesia | — | 40 | Herath H et al. 2017 [243] |
| AT | — | — | Normal | inversion (all leads) | More than normal | — | 3827 | Akinesia | Hyper | 36 | Pongbangli N et al. 2019 [244] |
| AT | 118 | 119/75 | Elevation (II, III, aVF, V3-V6) | — | Normal | 5435 (NT proBNP) | More than normal | Akinesia | Hyper | — | Nonaka D et al. 2019 [245] |
| LVT | — | — | Elevation (V3-V5) | inversion | Normal | — | 528 | Akinesia | Normal | — | Y-Hassan S et al. 2019 [246] |
| Hepatic artery thrombosis | 120 | — | Elevation (V2) | — | — | 1660 (BNP) | 0,45 | Hypokinesia | — | 15–20 | Luu L et al. 2020 [247] |
| LVT | 165 | 60/30 | Elevation (II-III, aVF, V3-V6) | — | — | — | 500 | Akinesia | — | 20 | Joki T et al. 2020 [248] |
Table summarising studies on the independent predictors for various TTS complications.
Hyper — Hypercontraction, VF — Ventricular fibrillation, AF — Atrial fibrillation, AT — Apical thrombus, LVT — Left ventricular thrombus, HR — Heart rate, BP — Blood pressure, EF — Ejection fraction, AB — Apical ballooning, LVOTO — Left ventricular outflow tract obstruction.
Independent predictors of cardiogenic shock [160] :
-
a.
Male;
-
b.
Asian or Hispanic;
-
c.
Comorbidities, including congestive heart failure, chronic lung condition, and chronic diabetes.
Independent predictors of LV thrombus [94] and thromboembolic complications [161] :
-
a.
Apical ballooning TTS;
-
b.
Previous vascular disease;
-
c.
LVEF ≤ 30%;
-
d.
First WBC > 10 × 10*3 cells/μL;
-
e.
Troponin I level > 10 ng/mL.
Independent predictors of cardiac arrest [162] :
-
a.
High peak brain natriuretic peptide (BNP) values;
-
b.
ST-segment elevation;
-
c.
Atrial fibrillation;
-
d.
High C-reactive protein.
Independent predictors of atrial fibrillation [163] :
-
a.
Peak BNP 1620 ± 1459 ng/L;
-
b.
Peak CRP 116 ± 96 mg/L;
-
c.
LVEF 48 ± 15 %.
Independent predictors of ventricular fibrillation (VF):
-
a.
Increased heart rate and blood pressure;
-
b.
T-wave inversion (V4-V5);
-
c.
QT interval prolongation;
-
d.
Left ventricular basal hypercontraction.
A recent study showed that neutrophil/lymphocyte ratio is an independent predictor of hospital-acquired complications, including pulmonary edema, cardiogenic shock, death, stroke, and LV thrombi [164]. However, further studies are needed to determine the diagnostic and prognostic role of the general blood test.
Interleukins (IL) are hypothesised to influence TTS development, and their role as independent predictors of complications is also considered. For example, in 2016, Santoro et al. found that elevated levels of IL-6 and IL-10 on admission to hospital correlated with a high incidence of in-hospital complications. Patients with IL-6 > 51 pg/ml and/or IL-10 > 1.3 pg/ml were more likely to develop cardiogenic shock, pulmonary oedema, stroke, and recurrent TTS [165]. It has also been reported that IL infusion may contribute to the development of TTS [166]. Based on a study that involved 136 patients, the levels of anti-inflammatory cytokines (IL-2, IL-4, IL-10), two inflammatory cytokines (tumour necrosis factor (TNF)-a and interferon gamma (INF-g)) and the chemo-attract component epidermal growth factor (EGF) were higher among patients with TTS [167]. The higher levels of anti-inflammatory interleukins (IL-2, IL-4, and IL-10) found in TTS can be explained by the presence of macrophages M2 surrounding the damaged tissue [168]. For example, Nef et al. in their study of myocardial biopsy samples from TTS, immunohistochemical staining revealed the presence of several extracellular macrophage clusters (CD68) both in the acute phase and in the “recovered” myocardium [169]. As known, macrophages are cells of the immune system that can induce and suppress inflammation by secreting different groups of molecules.
In comparison to ACS, lower levels of IL-6 and higher levels of TNF-a and INF-g were found in patients with TTS, indicating a different response of cellular molecules in the two pathological processes. Researchers suggested that the higher levels of TNF-a and INF-g in patients with TTS may be related to their ability to remove damaged cells, while the higher levels of IL-6 in patients with ACS may indicate the process of atherosclerosis [167].
12. Prognosis
TTS is usually favourable and resolves with complete recovery in 4–8 weeks in>90% of patients. Relapses are rare. Thus, in a study by Templin et al. relapse rate was 1.8% per year [75]. A meta-analysis of 31 studies involving 1664 patients reported a 5% relapse after six years [170]. In a meta-analysis involving 3513 patients, Kato et al. reported a relapse rate from 0 to 10% [171]. Furthermore, in a study by Lau et al. with 519 patients, TTS recurred in 7.5% of patients over 5.2 years of follow-up [172].
Risk factors for developing relapses are severe LV dysfunction, increased susceptibility to emotional stress, dynamic fluctuations in the sensitivity of cardiac adrenergic receptors, and women over 50 years old [173]. Moreover, long-term mortality in TTS patients was significantly higher compared with the matched STEMI patients (24.7% vs. 15.1%, 95% confidence interval 1.07–2.33; P = 0.02). Masculinity, high Killip grade on admission, and diabetes mellitus were identified as independent predictors of mortality in TTS patients [174]. As such, preventive measures should be required to reduce the risk of complications and TTS recurrence.
According to Matabuena Gomez-Limon J et al. (1.8–6.6 years), long-term consequences include LV wall movement abnormalities, myocardial infarction, recurrent events of TTS, heart failure, and others [175]. Furthermore, independent predictors of in-hospital complications, according to Bento D et al. (234 patients), include chronic kidney disease, coronary artery disease, lower LVEF on admission (mean LVEF was 43 ± 11%), dyspnea at presentation [176], [177]. Also, it was shown that TTS might trigger rhythm disorders. Meanwhile, ventricular arrhythmias were the most common [178]. Rhythm disturbances mainly occurred in the first 48 h after admission to hospital, but asystole and AV-block were mainly out-hospital (before the hospitalisation). Cardiogenic shock and prolongation of the QT interval were identified as independent predictors of rhythm disturbances. The QT interval change could be explained by the role of increased late sodium current and decreased transient outward current (i.e., impaired depolarisation and repolarisation) [179] or by myocardial oedema (with QT prolongation 72 h after admission) [101]. Researchers have concluded that rhythm disturbances in TTS may indicate myocardial vulnerability in the acute phase so that patients with TTS and independent predictors of complications should probably be referred to the intensive care unit within 48 h of admission.
Moreover, atrial fibrillation is known to increase the risk of ventricular arrhythmias and cardiac arrest [180]. Therefore, such patients require longer hospital lengths of stay and careful monitoring after discharge.
In 2016 the retrospective study demonstrated paradoxical results of better intrahospital and long-term outcomes for patients with underlying diabetes mellitus who suffered from TTS [181]. However, in 2020 these results were not supported by Temidayo et al. It was demonstrated that TTS patients with DM had a higher risk for poor outcomes in a larger sample size [182]. At the same time, the 2021 research on “Diabetes Paradox” with a large Nationwide inpatient sample showed that TTS patients have a low prevalence of DM compared to patients without TTS. Moreover, complicated DM patients were found to have lower in-hospital mortality, probably secondary to blunted catecholamine mediated response caused by chronic hyperglycemia [183]. Therefore, further prospective research is warranted to evaluate the impact of DM on stress-induced cardiomyopathy.
13. Prevention
13.1. Pharmacological prevention
Until now, there has been no consensus regarding the pharmacological prevention of TTS. Thus, Santoro et al. found that the recurrence rate was lower with the use of beta-blockers (1.81%) compared with the control group (2.86%). The relapse rate with ACE inhibitors, aspirin, and statins was statistically less significant and amounted to 0.5% compared to 0% in the control group [136]. Contradicting results were obtained by Singh et al. in a meta-analysis showing that ACE inhibitors, and not beta-blockers, reduce the risk of recurrence [170]. Researchers suggested that β2-adrenoceptors are involved in the TTS pathogenesis so that the action of selective β1-adrenoblockers is neither practical nor helpful. In contrast, ACE inhibitors, according to the researchers, may reduce the risk of recurrent TTS through anti-inflammatory or sympathetic activity. The same results were obtained by Brunetti et al. in a 2016 study [131]. In 2021, a study was carried out to investigate the long-term effects of TTS. Patients were followed up for 5.2 years, and it was noted that recurrence and mortality were lower after therapy with beta blockers alone compared with patients taking ACE inhibitors only [172].
13.2. Taking antidepressants with caution
It is necessary to alleviate stress in everyday life to prevent TTS, and antidepressants should not be taken, especially SNRI, without prescription. Thus, obtaining proper medical history and identifying susceptible patients before starting antidepressants are vital in clinical practice. In addition, close follow-up care with a psychiatrist and a cardiologist is recommended to reduce TTS recurrences and long-term complications.
13.3. Changing lifestyle
As a preventive measure, it is advised to reduce the consumption of caffeine drinks and quit smoking since these are the risk factors that impair endothelial function and/or coronary blood flow reserve and increase adrenergic stimulation [184].
14. Conclusion
In summary, TTS is an increasingly recognized condition that can lead to less favourable outcomes comparable to those of acute coronary syndrome despite a self-limiting clinical course. Moreover, the two conditions can coexist, making diagnosis even more challenging. The existing knowledge about this syndrome is primarily based on consensus documents and current international registries. Therefore, controlled clinical trials and further research are needed to determine the optimal diagnostic approach, treatment, and prevention strategies.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Buchmann S.J., Lehmann D., Stevens C.E. Takotsubo Cardiomyopathy—Acute Cardiac Dysfunction Associated With Neurological and Psychiatric Disorders. Front. Neurol. 2019;10:917. doi: 10.3389/fneur.2019.00917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Minhas A.S., Hughey A.B., Kolias T.J. Nationwide Trends in Reported Incidence of Takotsubo Cardiomyopathy from 2006 to 2012. Am. J. Cardiol. 2015;116:1128–1131. doi: 10.1016/j.amjcard.2015.06.042. [DOI] [PubMed] [Google Scholar]
- 3.Murugiah K., Wang Y., Desai N.R., Spatz E.S., Nuti S.V., Dreyer R.P., Krumholz H.M. Trends in Short- and Long-Term Outcomes for Takotsubo Cardiomyopathy Among Medicare Fee-for-Service Beneficiaries, 2007 to 2012. JACC: Heart Failure. 2016;4(3):197–205. doi: 10.1016/j.jchf.2015.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Deshmukh A., Kumar G., Pant S., Rihal C., Murugiah K., Mehta J.L. Prevalence of Takotsubo cardiomyopathy in the United States. Am. Heart J. 2012;164(1):66–71.e1. doi: 10.1016/j.ahj.2012.03.020. [DOI] [PubMed] [Google Scholar]
- 5.Ghadri J.-R., Wittstein I.S., Prasad A., et al. International Expert Consensus Document on Takotsubo Syndrome (Part I): Clinical Characteristics, Diagnostic Criteria, and Pathophysiology. Eur. Heart J. 2018;39(22):2032–2046. doi: 10.1093/eurheartj/ehy076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prasad A., Dangas G., Srinivasan M., Yu J., Gersh B.J., Mehran R., Stone G.W. Incidence and angiographic characteristics of patients With apical ballooning syndrome (takotsubo/stress cardiomyopathy) in the HORIZONS-AMI trial: An analysis from a multicenter, international study of ST-elevation myocardial infarction. Cathet. Cardiovasc. Intervent. 2014;83(3):343–348. doi: 10.1002/ccd.23441. [DOI] [PubMed] [Google Scholar]
- 7.Jabri A., Kalra A., Kumar A., Alameh A., Adroja S., Bashir H., Nowacki A.S., Shah R., Khubber S., Kanaa’N A., Hedrick D.P., Sleik K.M., Mehta N., Chung M.K., Khot U.N., Kapadia S.R., Puri R., Reed G.W. Incidence of Stress Cardiomyopathy During the Coronavirus Disease 2019 Pandemic. JAMA Netw Open. 2020;3(7):e2014780. doi: 10.1001/jamanetworkopen.2020.14780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El‐Battrawy I., Santoro F., Stiermaier T., Möller C., Guastafierro F., Novo G., Novo S., Mariano E., Romeo F., Romeo F., Thiele H., Guerra F., Capucci A., Giannini I., Brunetti N.D., Eitel I., Akin I. Incidence and Clinical Impact of Recurrent Takotsubo Syndrome: Results From the GEIST Registry. J Am Heart Assoc. 2019;8(9) doi: 10.1161/JAHA.118.010753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aizawa K., Suzuki T. Takotsubo Cardiomyopathy. Heart Failure Clinics. 2013;9(2):243–247. doi: 10.1016/j.hfc.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 10.Brinjikji W., El-Sayed A.M., Salka S. to 2009. Am. Heart J. 2012;164(2):215–221. doi: 10.1016/j.ahj.2012.04.010. [DOI] [PubMed] [Google Scholar]
- 11.Okura H. Echocardiographic assessment of takotsubo cardiomyopathy: beyond apical ballooning. J. Echocardiogr. 2016;14(1):13–20. doi: 10.1007/s12574-015-0271-3. [DOI] [PubMed] [Google Scholar]
- 12.Berton E., Vitali-Serdoz L., Vallon P., Maschio M., Gortani G., Benettoni A. Young girl with apical ballooning heart syndrome. Int. J. Cardiol. 2012;161(1):e4–e6. doi: 10.1016/j.ijcard.2012.03.012. [DOI] [PubMed] [Google Scholar]
- 13.Xing X. Testosterone suppresses oxidative stress via androgen receptor-independent pathway in murine cardiomyocytes. Mol. Med. Report. 2011 doi: 10.3892/mmr.2011.539. [DOI] [PubMed] [Google Scholar]
- 14.Kato K., Lyon A.R., Ghadri J.-R., Templin C. Takotsubo syndrome: aetiology, presentation and treatment. Heart. 2017;103(18):1461–1469. doi: 10.1136/heartjnl-2016-309783. [DOI] [PubMed] [Google Scholar]
- 15.Carroll A.J., Goergen J., Wafford Q.E., Flaherty J.D., Grady K.L., Feingold K.L. Psychiatric conditions in patients presenting with Takotsubo syndrome: A systematic review and synthesis of case studies. Gen. Hosp. Psychiatry. 2020;65:54–63. doi: 10.1016/j.genhosppsych.2020.05.010. [DOI] [PubMed] [Google Scholar]
- 16.Dias A., Franco E., Koshkelashvili N., Pressman G.S., Hebert K., Figueredo V.M. Racial and ethnic differences in Takotsubo cardiomyopathy presentation and outcomes. Int. J. Cardiol. 2015;194:100–103. doi: 10.1016/j.ijcard.2015.04.056. [DOI] [PubMed] [Google Scholar]
- 17.Qaqa A., Daoko J., Jallad N., et al. Takotsubo Syndrome in African American vs. Non-African American Women. West J. Emerg. Med. 2011;12:218–223. [PMC free article] [PubMed] [Google Scholar]
- 18.Hegde S., Khan R., Zordok M., Maysky M. Characteristics and outcome of patients with COVID-19 complicated by Takotsubo cardiomyopathy: case series with literature review. Open Heart. 2020;7(2):e001360. doi: 10.1136/openhrt-2020-001360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bymaster F.P., Zhang W., Carter P.A., Shaw J., Chernet E., Phebus L., Wong D.T., Perry K.W. Fluoxetine, but not other selective serotonin uptake inhibitors, increases norepinephrine and dopamine extracellular levels in prefrontal cortex. Psychopharmacology. 2002;160(4):353–361. doi: 10.1007/s00213-001-0986-x. [DOI] [PubMed] [Google Scholar]
- 20.Carbone A., Bottino R., Russo V., D'Andrea A., Liccardo B., Maurea N., Quagliariello V., Cimmino G., Golino P. Takotsubo Cardiomyopathy as Epiphenomenon of Cardiotoxicity in Patients With Cancer: A Meta-summary of Case Reports. J. Cardiovasc. Pharmacol. 2021;78(1):e20–e29. doi: 10.1097/FJC.0000000000001026. [DOI] [PubMed] [Google Scholar]
- 21.Ozturk M.A., Ozveren O., Cinar V., Erdik B., Oyan B. Takotsubo syndrome: an underdiagnosed complication of 5-fluorouracil mimicking acute myocardial infarction. Blood Coagul. Fibrinolysis. 2013;24(1):90–94. doi: 10.1097/MBC.0b013e3283597605. [DOI] [PubMed] [Google Scholar]
- 22.Grunwald M.R., Howie L., Diaz L.A. Takotsubo Cardiomyopathy and Fluorouracil: Case Report and Review of the Literature. JCO. 2012;30(2):e11–e14. doi: 10.1200/JCO.2011.38.5278. [DOI] [PubMed] [Google Scholar]
- 23.Polk A., Vaage-Nilsen M., Vistisen K., Nielsen D.L. Cardiotoxicity in cancer patients treated with 5-fluorouracil or capecitabine: A systematic review of incidence, manifestations and predisposing factors. Cancer Treat. Rev. 2013;39(8):974–984. doi: 10.1016/j.ctrv.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 24.Rateesh S., Luis S.A., Luis C.R., Hughes B., Nicolae M. Myocardial infarction secondary to 5-fluorouracil: Not an absolute contraindication to rechallenge? Int. J. Cardiol. 2014;172(2):e331–e333. doi: 10.1016/j.ijcard.2013.12.274. [DOI] [PubMed] [Google Scholar]
- 25.Kim J., Kundu M., Viollet B., Guan K.-L. AMPK and mTOR regulate autophagy through direct phosphorylation of Ulk1. Nat. Cell Biol. 2011;13(2):132–141. doi: 10.1038/ncb2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mohan N., Shen Y., Endo Y., ElZarrad M.K., Wu W.J. Trastuzumab, but Not Pertuzumab, Dysregulates HER2 Signaling to Mediate Inhibition of Autophagy and Increase in Reactive Oxygen Species Production in Human Cardiomyocytes. Mol. Cancer Ther. 2016;15(6):1321–1331. doi: 10.1158/1535-7163.MCT-15-0741. [DOI] [PubMed] [Google Scholar]
- 27.Economopoulou P., Kentepozidis N., Kotsakis A., et al. Cancer therapy and cardiovascular risk: focus on bevacizumab. CMAR. 2015:133. doi: 10.2147/CMAR.S77400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kamba T., McDonald D.M. Mechanisms of adverse effects of anti-VEGF therapy for cancer. Br. J. Cancer. 2007;96(12):1788–1795. doi: 10.1038/sj.bjc.6603813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moretti A., Polselli M., Carbone I., et al. Takotsubo cardiomyopathy and flecainide toxicity: a case report and brief literature review. Eur. Rev. Med. Pharmacol. Sci. 2021;25:4069–4073. doi: 10.26355/eurrev_202106_26048. [DOI] [PubMed] [Google Scholar]
- 30.J.B. Florek, D. Girzadas, Amiodarone, in: StatPearls, StatPearls Publishing, Treasure Island (FL), 2022. http://www.ncbi.nlm.nih.gov/books/NBK482154/ (accessed February 20, 2022).
- 31.Wang X., Pei J., Hu X. The Brain-Heart Connection in Takotsubo Syndrome: The Central Nervous System, Sympathetic Nervous System, and Catecholamine Overload. Cardiol. Res. Practice. 2020;2020:1–5. doi: 10.1155/2020/4150291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Akashi Y.J., Nakazawa K., Sakakibara M., et al. 123I-MIBG myocardial scintigraphy in patients with “takotsubo” cardiomyopathy. J. Nucl. Med. 2004;45:1121–1127. [PubMed] [Google Scholar]
- 33.Vaccaro A., Despas F., Delmas C., Lairez O., Lambert E., Lambert G., Labrunee M., Guiraud T., Esler M., Galinier M., Senard J.M., Pathak A., Baumert M. Direct Evidences for Sympathetic Hyperactivity and Baroreflex Impairment in Tako Tsubo Cardiopathy. PLoS ONE. 2014;9(3):e93278. doi: 10.1371/journal.pone.0093278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Norcliffe-Kaufmann L., Kaufmann H., Martinez J., Katz S.D., Tully L., Reynolds H.R. Autonomic Findings in Takotsubo Cardiomyopathy. Am. J. Cardiol. 2016;117(2):206–213. doi: 10.1016/j.amjcard.2015.10.028. [DOI] [PubMed] [Google Scholar]
- 35.Suzuki H., Matsumoto Y., Kaneta T., Sugimura K., Takahashi J., Fukumoto Y., Takahashi S., Shimokawa H. Evidence for Brain Activation in Patients With Takotsubo Cardiomyopathy. Circ. J. 2014;78(1):256–258. doi: 10.1253/circj.CJ-13-1276. [DOI] [PubMed] [Google Scholar]
- 36.Radfar A., Abohashem S., Osborne M.T., Wang Y., Dar T., Hassan M.Z.O., Ghoneem A., Naddaf N., Patrich T., Abbasi T., Zureigat H., Jaffer J., Ghazi P., Scott J.A., Shin L.M., Pitman R.K., Neilan T.G., Wood M.J., Tawakol A. Stress-associated neurobiological activity associates with the risk for and timing of subsequent Takotsubo syndrome. Eur. Heart J. 2021;42(19):1898–1908. doi: 10.1093/eurheartj/ehab029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hiestand T., Hänggi J., Klein C., et al. Takotsubo Syndrome Associated With Structural Brain Alterations of the Limbic System. J. Am. Coll. Cardiol. 2018;71:809–811. doi: 10.1016/j.jacc.2017.12.022. [DOI] [PubMed] [Google Scholar]
- 38.Pereira V.H., Marques P., Magalhães R., Português J., Calvo L., Cerqueira J.J., Sousa N. Central autonomic nervous system response to autonomic challenges is altered in patients with a previous episode of Takotsubo cardiomyopathy. Eur. Heart J.: Acute Cardiovasc. Care. 2016;5(2):152–163. doi: 10.1177/2048872615568968. [DOI] [PubMed] [Google Scholar]
- 39.Haft J.I. Cardiovascular injury induced by sympathetic catecholamines. Prog. Cardiovasc. Dis. 1974;17(1):73–86. doi: 10.1016/0033-0620(74)90039-5. [DOI] [PubMed] [Google Scholar]
- 40.Y-Hassan S. Insights into the Pathogenesis of Takotsubo Syndrome, Which with Persuasive Reasons Should Be Regarded as an Acute Cardiac Sympathetic Disease Entity. ISRN Cardiol. 2012;(2012):1–6. doi: 10.5402/2012/593735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gupta S., Gupta M.M. Takotsubo syndrome. Indian Heart J. 2018;70(1):165–174. doi: 10.1016/j.ihj.2017.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Paur H., Wright P.T., Sikkel M.B., Tranter M.H., Mansfield C., O'Gara P., Stuckey D.J., Nikolaev V.O., Diakonov I., Pannell L., Gong H., Sun H., Peters N.S., Petrou M., Zheng Z., Gorelik J., Lyon A.R., Harding S.E. High Levels of Circulating Epinephrine Trigger Apical Cardiodepression in a β 2 -Adrenergic Receptor/G i –Dependent Manner: A New Model of Takotsubo Cardiomyopathy. Circulation. 2012;126(6):697–706. doi: 10.1161/CIRCULATIONAHA.112.111591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shao Y., Redfors B., Scharin Täng M., Möllmann H., Troidl C., Szardien S., Hamm C., Nef H., Borén J., Omerovic E. Novel rat model reveals important roles of β-adrenoreceptors in stress-induced cardiomyopathy. Int. J. Cardiol. 2013;168(3):1943–1950. doi: 10.1016/j.ijcard.2012.12.092. [DOI] [PubMed] [Google Scholar]
- 44.Nef H.M., Möllmann H., Akashi Y.J., Hamm C.W. Mechanisms of stress (Takotsubo) cardiomyopathy. Nat. Rev. Cardiol. 2010;7(4):187–193. doi: 10.1038/nrcardio.2010.16. [DOI] [PubMed] [Google Scholar]
- 45.Nef H.M., Mollmann H., Troidl C., Kostin S., Voss S., Hilpert P., Behrens C.B., Rolf A., Rixe J., Weber M., Hamm C.W., Elsasser A. Abnormalities in intracellular Ca2+ regulation contribute to the pathomechanism of Tako-Tsubo cardiomyopathy. Eur. Heart J. 2009;30(17):2155–2164. doi: 10.1093/eurheartj/ehp240. [DOI] [PubMed] [Google Scholar]
- 46.Kume T., Kawamoto T., Okura H., Toyota E., Neishi Y., Watanabe N., Hayashida A., Okahashi N., Yoshimura Y., Saito K., Nezuo S., Yamada R., Yoshida K. Local Release of Catecholamines From the Hearts of Patients With Tako-Tsubo-Like Left Ventricular Dysfunction. Circ .J. 2008;72(1):106–108. doi: 10.1253/circj.72.106. [DOI] [PubMed] [Google Scholar]
- 47.Wittstein I.S., Thiemann D.R., Lima J.A.C., Baughman K.L., Schulman S.P., Gerstenblith G., Wu K.C., Rade J.J., Bivalacqua T.J., Champion H.C. Neurohumoral Features of Myocardial Stunning Due to Sudden Emotional Stress. N Engl. J. Med. 2005;352(6):539–548. doi: 10.1056/NEJMoa043046. [DOI] [PubMed] [Google Scholar]
- 48.Madhavan M., Borlaug B.A., Lerman A., Rihal C.S., Prasad A. Stress hormone and circulating biomarker profile of apical ballooning syndrome (Takotsubo cardiomyopathy): insights into the clinical significance of B-type natriuretic peptide and troponin levels. Heart. 2009;95(17):1436–1441. doi: 10.1136/hrt.2009.170399. [DOI] [PubMed] [Google Scholar]
- 49.Kido K., Guglin M. Drug-Induced Takotsubo Cardiomyopathy. J. Cardiovasc. Pharmacol. Ther. 2017;22(6):552–563. doi: 10.1177/1074248417708618. [DOI] [PubMed] [Google Scholar]
- 50.Nguyen T.H., Neil C.J., Sverdlov A.L., Ngo D.T., Chan W.P., Heresztyn T., Chirkov Y.Y., Tsikas D., Frenneaux M.P., Horowitz J.D. Enhanced NO signaling in patients with Takotsubo cardiomyopathy: short-term pain, long-term gain? Cardiovasc. Drugs Ther. 2013;27(6):541–547. doi: 10.1007/s10557-013-6481-x. [DOI] [PubMed] [Google Scholar]
- 51.Surikow S.Y., Nguyen T.H., Stafford I., Chapman M., Chacko S., Singh K., Licari G., Raman B., Kelly D.J., Zhang Y., Waddingham M.T., Ngo D.T., Bate A.P., Chua S.J., Frenneaux M.P., Horowitz J.D. Nitrosative Stress as a Modulator of Inflammatory Change in a Model of Takotsubo Syndrome. JACC Basic Transl. Sci. 2018;3(2):213–226. doi: 10.1016/j.jacbts.2017.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dawson D.K., Neil C.J., Henning A., Cameron D., Jagpal B., Bruce M., Horowitz J., Frenneaux M.P. Tako-Tsubo Cardiomyopathy: A Heart Stressed Out of Energy? JACC Cardiovasc. Imaging. 2015;8(8):985–987. doi: 10.1016/j.jcmg.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 53.Yi‐Tang T., Risha K., Joan S.P., et al. β-Adrenergic receptors (ßAR) regulate cardiomyocyte proliferation during early postnatal life. FASEB J. 2001;15(11):1921–1926. doi: 10.1096/fj.01-0151com. [DOI] [PubMed] [Google Scholar]
- 54.Li H., Fong C., Chen Y., Cai G., Yang M. β2- and β3-, but not β1-adrenergic receptors are involved in osteogenesis of mouse mesenchymal stem cells via cAMP/PKA signaling. Arch. Biochem. Biophys. 2010;496(2):77–83. doi: 10.1016/j.abb.2010.01.016. [DOI] [PubMed] [Google Scholar]
- 55.Li X.-L., Zeng D., Chen Y., Ding L., Li W.-J., Wei T., Ou D.-B., Yan S., Wang B., Zheng Q.-S. Role of alpha- and beta-adrenergic receptors in cardiomyocyte differentiation from murine-induced pluripotent stem cells. Cell Prolif. 2017;50(1):e12310. doi: 10.1111/cpr.12310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pelliccia F., Kaski J.C., Crea F., Camici P.G. Pathophysiology of Takotsubo Syndrome. Circulation. 2017;135(24):2426–2441. doi: 10.1161/CIRCULATIONAHA.116.027121. [DOI] [PubMed] [Google Scholar]
- 57.Naegele M., Flammer A.J., Enseleit F., Roas S., Frank M., Hirt A., Kaiser P., Cantatore S., Templin C., Fröhlich G., Romanens M., Lüscher T.F., Ruschitzka F., Noll G., Sudano I. Endothelial function and sympathetic nervous system activity in patients with Takotsubo syndrome. Int. J. Cardiol. 2016;224:226–230. doi: 10.1016/j.ijcard.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 58.Haghi D., Roehm S., Hamm K., Harder N., Suselbeck T., Borggrefe M., Papavassiliu T. Takotsubo Cardiomyopathy Is Not Due to Plaque Rupture: An Intravascular Ultrasound Study. Clin. Cardiol. 2010;33(5):307–310. doi: 10.1002/clc.20747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Eitel I., Stiermaier T., Graf T., Möller C., Rommel K.-P., Eitel C., Schuler G., Thiele H., Desch S. Optical Coherence Tomography to Evaluate Plaque Burden and Morphology in Patients With Takotsubo Syndrome. JAHA. 2016;5(12) doi: 10.1161/JAHA.116.004474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Haghi D., Hamm K., Heggemann F., Walter T., Suselbeck T., Papavassiliu T., Borggrefe M. Coincidence of coronary artery disease and Tako-Tsubo cardiomyopathyKoinzidenz von koronarer Herzkrankheit und Tako-Tsubo Kardiomypathie. Herz. 2010;35(4):252–257. doi: 10.1007/s00059-011-3447-2. [DOI] [PubMed] [Google Scholar]
- 61.Parodi G., Citro R., Bellandi B., Del Pace S., Rigo F., Marrani M., Provenza G., Leoncini M., Salerno Uriarte J.A., Bovenzi F., Bossone E. Tako-tsubo cardiomyopathy and coronary artery disease: a possible association. Coron. Artery Dis. 2013;24(6):527–533. doi: 10.1097/MCA.0b013e3283645c4e. [DOI] [PubMed] [Google Scholar]
- 62.Scally C., Abbas H., Ahearn T., Srinivasan J., Mezincescu A., Rudd A., Spath N., Yucel-Finn A., Yuecel R., Oldroyd K., Dospinescu C., Horgan G., Broadhurst P., Henning A., Newby D.E., Semple S., Wilson H.M., Dawson D.K. Myocardial and Systemic Inflammation in Acute Stress-Induced (Takotsubo) Cardiomyopathy. Circulation. 2019;139(13):1581–1592. doi: 10.1161/CIRCULATIONAHA.118.037975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Scantlebury D.C., Prasad A. Diagnosis of Takotsubo Cardiomyopathy: – Mayo Clinic Criteria –. Circ. J. 2014;78(9):2129–2139. doi: 10.1253/circj.CJ-14-0859. [DOI] [PubMed] [Google Scholar]
- 64.Yamauchi-Takihara K., Ihara Y., Ogata A., Yoshizaki K., Azuma J., Kishimoto T. Hypoxic Stress Induces Cardiac Myocyte-Derived Interleukin-6. Circulation. 1995;91(5):1520–1524. doi: 10.1161/01.CIR.91.5.1520. [DOI] [PubMed] [Google Scholar]
- 65.Ohtsuka T., Hamada M., Hiasa G., Sasaki O., Suzuki M., Hara Y., Shigematsu Y., Hiwada K. Effect of beta-blockers on circulating levels of inflammatory and anti-inflammatory cytokines in patients with dilated cardiomyopathy. J. Am. Coll. Cardiol. 2001;37(2):412–417. doi: 10.1016/S0735-1097(00)01121-9. [DOI] [PubMed] [Google Scholar]
- 66.Nishiga M., Wang D.W., Han Y., Lewis D.B., Wu J.C. COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat. Rev. Cardiol. 2020;17(9):543–558. doi: 10.1038/s41569-020-0413-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Singh S., Desai R., Gandhi Z., Fong H.K., Doreswamy S., Desai V., Chockalingam A., Mehta P.K., Sachdeva R., Kumar G. Takotsubo Syndrome in Patients with COVID-19: a Systematic Review of Published Cases. SN Compr. Clin. Med. 2020;2(11):2102–2108. doi: 10.1007/s42399-020-00557-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Taza F., Zulty M., Kanwal A., Grove D. Takotsubo cardiomyopathy triggered by SARS-CoV-2 infection in a critically ill patient. BMJ Case Rep. 2020;13(6):e236561. doi: 10.1136/bcr-2020-236561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chadha S. ‘COVID-19 pandemic’ anxiety-induced Takotsubo cardiomyopathy. QJM: Int. J. Med. 2020;113:488–490. doi: 10.1093/qjmed/hcaa135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Virani S.S., Khan A.N., Mendoza C.E., et al. Takotsubo cardiomyopathy, or broken-heart syndrome. Tex Heart Inst. J. 2007;34:76–79. [PMC free article] [PubMed] [Google Scholar]
- 71.Pant S., Deshmukh A., Mehta K., Patel N., Badheka A., Shah N., Chothani A., Giri S., Dabhadkar K., Mehta J., Rihal C. Clustering of Takotsubo cardiomyopathy cases in United States in 2011. J. Am. Coll. Cardiol. 2014;63(12):A828. doi: 10.1016/S0735-1097(14)60828-7. [DOI] [Google Scholar]
- 72.Couch L.S., Fiedler J., Chick G., Clayton R., Dries E., Wienecke L.M., Fu L.u., Fourre J., Pandey P., Derda A.A., Wang B.X., Jabbour R., Shanmuganathan M., Wright P., Lyon A.R., Terracciano C.M., Thum T., Harding S.E. Circulating microRNAs predispose to takotsubo syndrome following high-dose adrenaline exposure. Cardiovasc. Res. 2021 doi: 10.1093/cvr/cvab210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Núñez-Gil I.J., Almendro-Delia M., Andrés M., Sionis A., Martin A., Bastante T., Córdoba-Soriano J.G., Linares J.A., González Sucarrats S., Sánchez-Grande-Flecha A., Fabregat-Andrés O., Pérez B., Escudier-Villa J.M., Martin-Reyes R., Pérez-Castellanos A., Rueda Sobella F., Cambeiro C., Piqueras-Flores J., Vidal-Perez R., Bodí V., García de la Villa B., Corbí-Pascua M., Biagioni C., Mejía-Rentería H.D., Feltes G., Barrabés J. Secondary forms of Takotsubo cardiomyopathy: A whole different prognosis. Eur. Heart J.: Acute Cardiovasc. Care. 2016;5(4):308–316. doi: 10.1177/2048872615589512. [DOI] [PubMed] [Google Scholar]
- 74.Okura H. Update of takotsubo syndrome in the era of COVID-19. J. Cardiol. 2021;77(4):361–369. doi: 10.1016/j.jjcc.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Templin C., Ghadri J.R., Diekmann J., Napp L.C., Bataiosu D.R., Jaguszewski M., Cammann V.L., Sarcon A., Geyer V., Neumann C.A., Seifert B., Hellermann J., Schwyzer M., Eisenhardt K., Jenewein J., Franke J., Katus H.A., Burgdorf C., Schunkert H., Moeller C., Thiele H., Bauersachs J., Tschöpe C., Schultheiss H.-P., Laney C.A., Rajan L., Michels G., Pfister R., Ukena C., Böhm M., Erbel R., Cuneo A., Kuck K.-H., Jacobshagen C., Hasenfuss G., Karakas M., Koenig W., Rottbauer W., Said S.M., Braun-Dullaeus R.C., Cuculi F., Banning A., Fischer T.A., Vasankari T., Airaksinen K.E.J., Fijalkowski M., Rynkiewicz A., Pawlak M., Opolski G., Dworakowski R., MacCarthy P., Kaiser C., Osswald S., Galiuto L., Crea F., Dichtl W., Franz W.M., Empen K., Felix S.B., Delmas C., Lairez O., Erne P., Bax J.J., Ford I., Ruschitzka F., Prasad A., Lüscher T.F. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N Engl. J. Med. 2015;373(10):929–938. doi: 10.1056/NEJMoa1406761. [DOI] [PubMed] [Google Scholar]
- 76.Ghadri J.R., Cammann V.L., Napp L.C., Jurisic S., Diekmann J., Bataiosu D.R., Seifert B., Jaguszewski M., Sarcon A., Neumann C.A., Geyer V., Prasad A., Bax J.J., Ruschitzka F., Lüscher T.F., Templin C. Differences in the Clinical Profile and Outcomes of Typical and Atypical Takotsubo Syndrome: Data From the International Takotsubo Registry. JAMA Cardiol. 2016;1(3):335. doi: 10.1001/jamacardio.2016.0225. [DOI] [PubMed] [Google Scholar]
- 77.Maron B.J., Towbin J.A., Thiene G., Antzelevitch C., Corrado D., Arnett D., Moss A.J., Seidman C.E., Young J.B. Contemporary Definitions and Classification of the Cardiomyopathies: An American Heart Association Scientific Statement From the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation. 2006;113(14):1807–1816. doi: 10.1161/CIRCULATIONAHA.106.174287. [DOI] [PubMed] [Google Scholar]
- 78.Redfors B., Råmunddal T., Shao Y., et al. Takotsubo triggered by acute myocardial infarction: a common but overlooked syndrome? J. Geriatr. Cardiol. 2014;11:171–173. doi: 10.3969/j.issn.1671-5411.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Y-Hassan S., Böhm F. The causal link between spontaneous coronary artery dissection and takotsubo syndrome: A case presented with both conditions. Int. J. Cardiol. 2016;203:828–831. doi: 10.1016/j.ijcard.2015.11.047. [DOI] [PubMed] [Google Scholar]
- 80.S Y.-H. Takotsubo Syndrome Triggered by Acute Coronary Syndrome in a Cohort of 20 Patients: An often Missed Diagnosis. IJCRR. 2015:28–33. doi: 10.19070/2470-456310.19070/2470-4563-150007. [DOI] [Google Scholar]
- 81.Keramida K., Backs J., Bossone E., Citro R., Dawson D., Omerovic E., Parodi G., Schneider B., Ghadri J.R., Van Laake L.W., Lyon A.R. Takotsubo syndrome in Heart Failure and World Congress on Acute Heart Failure 2019: highlights from the experts, ESC. Heart Failure. 2020;7(2):400–406. doi: 10.1002/ehf2.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Collet J.-P., Thiele H., Barbato E., Barthélémy O., Bauersachs J., Bhatt D.L., Dendale P., Dorobantu M., Edvardsen T., Folliguet T., Gale C.P., Gilard M., Jobs A., Jüni P., Lambrinou E., Lewis B.S., Mehilli J., Meliga E., Merkely B., Mueller C., Roffi M., Rutten F.H., Sibbing D., Siontis G.C.M., Kastrati A., Mamas M.A., Aboyans V., Angiolillo D.J., Bueno H., Bugiardini R., Byrne R.A., Castelletti S., Chieffo A., Cornelissen V., Crea F., Delgado V., Drexel H., Gierlotka M., Halvorsen S., Haugaa K.H., Jankowska E.A., Katus H.A., Kinnaird T., Kluin J., Kunadian V., Landmesser U., Leclercq C., Lettino M., Meinila L., Mylotte D., Ndrepepa G., Omerovic E., Pedretti R.F.E., Petersen S.E., Petronio A.S., Pontone G., Popescu B.A., Potpara T., Ray K.K., Luciano F., Richter D.J., Shlyakhto E., Simpson I.A., Sousa-Uva M., Storey R.F., Touyz R.M., Valgimigli M., Vranckx P., Yeh R.W., Barbato E., Barthélémy O., Bauersachs J., Bhatt D.L., Dendale P., Dorobantu M., Edvardsen T., Folliguet T., Gale C.P., Gilard M., Jobs A., Jüni P., Lambrinou E., Lewis B.S., Mehilli J., Meliga E., Merkely B., Mueller C., Roffi M., Rutten F.H., Sibbing D., Siontis G.C.M. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021;42(14):1289–1367. doi: 10.1093/eurheartj/ehaa575. [DOI] [PubMed] [Google Scholar]
- 83.Napp L.C., Bauersachs J. Takotsubo syndrome: between evidence, myths, and misunderstandingsTakotsubo-Syndrom: Evidenz, Mythen, Missverständnisse. Herz. 2020;45(3):252–266. doi: 10.1007/s00059-020-04906-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Frhlich G.M., Schoch B., Schmid F., Keller P., Sudano I., Lscher T.F., Noll G., Ruschitzka F., Enseleit F. Takotsubo cardiomyopathy has a unique cardiac biomarker profile: NT-proBNP/myoglobin and NT-proBNP/troponin T ratios for the differential diagnosis of acute coronary syndromes and stress induced cardiomyopathy. Int. J. Cardiol. 2012;154(3):328–332. doi: 10.1016/j.ijcard.2011.09.077. [DOI] [PubMed] [Google Scholar]
- 85.Khan H., Gamble D., Mezincescu A., Abbas H., Rudd A., Dawson D. A systematic review of biomarkers in Takotsubo syndrome: A focus on better understanding the pathophysiology. IJC Heart Vasculature. 2021;34:100795. doi: 10.1016/j.ijcha.2021.100795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Frangieh A.H., Obeid S., Ghadri J.-R., Imori Y., D'Ascenzo F., Kovac M., Ruschitzka F., Lüscher T.F., Duru F., Templin C., Diekmann J., Cammann V.L., Jaguszewski M., Dichtl W., Franz W.M., Fijalkowski M., Opolski G., Franke J., Katus H.A., Michels G., Pfister R., Cuculi F. ECG Criteria to Differentiate Between Takotsubo (Stress) Cardiomyopathy and Myocardial Infarction. JAHA. 2016;5(6) doi: 10.1161/JAHA.116.003418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Franco E., Dias A., Koshkelashvili N., Pressman G.S., Hebert K., Figueredo V.M. Distinctive Electrocardiographic Features in African Americans Diagnosed with Takotsubo Cardiomyopathy: Electrocardiographic Racial Differences in Takotsubo. Ann. Noninvasive Electrocardiol. 2016;21(5):486–492. doi: 10.1111/anec.12337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mansencal N., Pellerin D., Lamar A., Beauchet A., El Mahmoud R., Pillière R., McKenna W.J., Dubourg O. Diagnostic value of contrast echocardiography in Tako-Tsubo cardiomyopathy. Arch. Cardiovas. Dis. 2010;103(8-9):447–453. doi: 10.1016/j.acvd.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 89.Patel S.M., Lennon R.J., Prasad A. Regional wall motion abnormality in apical ballooning syndrome (Takotsubo/stress cardiomyopathy): importance of biplane left ventriculography for differentiating from spontaneously aborted anterior myocardial infarction. Int. J. Cardiovasc. Imaging. 2012;28(4):687–694. doi: 10.1007/s10554-011-9911-5. [DOI] [PubMed] [Google Scholar]
- 90.Citro R., Lyon A.R., Meimoun P., Omerovic E., Redfors B., Buck T., Lerakis S., Parodi G., Silverio A., Eitel I., Schneider B., Prasad A., Bossone E. Standard and Advanced Echocardiography in Takotsubo (Stress) Cardiomyopathy: Clinical and Prognostic Implications. J. Am. Soc. Echocardiogr. 2015;28(1):57–74. doi: 10.1016/j.echo.2014.08.020. [DOI] [PubMed] [Google Scholar]
- 91.Citro R., Okura H., Ghadri J.R., Izumi C., Meimoun P., Izumo M., Dawson D., Kaji S., Eitel I., Kagiyama N., Kobayashi Y., Templin C., Delgado V., Nakatani S., Popescu B.A. Multimodality imaging in takotsubo syndrome: a joint consensus document of the European Association of Cardiovascular Imaging (EACVI) and the Japanese Society of Echocardiography (JSE) J. Echocardiogr. 2020;18(4):199–224. doi: 10.1007/s12574-020-00480-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Izumo M., Akashi Y.J. Role of echocardiography for takotsubo cardiomyopathy: clinical and prognostic implications. Cardiovasc. Diagn. Ther. 2018;8:90–100. doi: 10.21037/cdt.2017.07.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Tsuchihashi K., Ueshima K., Uchida T., Oh-mura N., Kimura K., Owa M., Yoshiyama M., Miyazaki S., Haze K., Ogawa H., Honda T., Hase M., Kai R.-I., Morii I. Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. J. Am. Coll. Cardiol. 2001;38(1):11–18. doi: 10.1016/S0735-1097(01)01316-X. [DOI] [PubMed] [Google Scholar]
- 94.Napp L.C., Ghadri J.R., Bauersachs J., Templin C. Acute coronary syndrome or Takotsubo cardiomyopathy: The suspect may not always be the culprit. Int. J. Cardiol. 2015;187:116–119. doi: 10.1016/j.ijcard.2015.03.255. [DOI] [PubMed] [Google Scholar]
- 95.Desmet W., Bennett J., Ferdinande B., De Cock D., Adriaenssens T., Coosemans M., Sinnaeve P., Kayaert P., Dubois C. The apical nipple sign: a useful tool for discriminating between anterior infarction and transient left ventricular ballooning syndrome. Eur. Heart J. Acute Cardiovasc. Care. 2014;3(3):264–267. doi: 10.1177/2048872613517359. [DOI] [PubMed] [Google Scholar]
- 96.Madias J.E. “Nipple” and “hawk’s beak” appearances on contrast left ventricular angiography in Takotsubo syndrome: what’s in a sign? Int. J. Cardiol. 2014;173(2):326. doi: 10.1016/j.ijcard.2014.03.053. [DOI] [PubMed] [Google Scholar]
- 97.Matta A., Roncalli J., Elbaz M., Lhermusier T., Campelo-Parada F., Bouisset F., Elenizi K., Nader V., Carrié D. Mid-Ventricular Takotsubo Cardiomyopathy with Hawk’s Beak Appearance: A Case Report. Am. J. Case Rep. 2020;21 doi: 10.12659/AJCR.919563. [DOI] [PubMed] [Google Scholar]
- 98.Citro R., Rigo F., D'Andrea A., Ciampi Q., Parodi G., Provenza G., Piccolo R., Mirra M., Zito C., Giudice R., Patella M.M., Antonini-Canterin F., Bossone E., Piscione F., Salerno-Uriarte J. Echocardiographic correlates of acute heart failure, cardiogenic shock, and in-hospital mortality in tako-tsubo cardiomyopathy. JACC Cardiovasc. Imaging. 2014;7(2):119–129. doi: 10.1016/j.jcmg.2013.09.020. [DOI] [PubMed] [Google Scholar]
- 99.Citro R., Pontone G., Pace L., Zito C., Silverio A., Bossone E., Piscione F. Contemporary Imaging in Takotsubo Syndrome. Heart Fail Clin. 2016;12(4):559–575. doi: 10.1016/j.hfc.2016.06.005. [DOI] [PubMed] [Google Scholar]
- 100.Eitel I., von Knobelsdorff-Brenkenhoff F., Bernhardt P., Carbone I., Muellerleile K., Aldrovandi A., Francone M., Desch S., Gutberlet M., Strohm O., Schuler G., Schulz-Menger J., Thiele H., Friedrich M.G. Clinical Characteristics and Cardiovascular Magnetic Resonance Findings in Stress (Takotsubo) Cardiomyopathy. JAMA. 2011;306(3) doi: 10.1001/jama.2011.992. [DOI] [PubMed] [Google Scholar]
- 101.Perazzolo Marra M., Zorzi A., Corbetti F., De Lazzari M., Migliore F., Tona F., Tarantini G., Iliceto S., Corrado D. Apicobasal gradient of left ventricular myocardial edema underlies transient T-wave inversion and QT interval prolongation (Wellens’ ECG pattern) in Tako-Tsubo cardiomyopathy. Heart Rhythm. 2013;10(1):70–77. doi: 10.1016/j.hrthm.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 102.Athanasiadis A., Schneider B., Sechtem U. Role of Cardiovascular Magnetic Resonance in Takotsubo Cardiomyopathy. Heart Failure Clinics. 2013;9(2):167–176. doi: 10.1016/j.hfc.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 103.Plácido R., Cunha Lopes B., Almeida A.G., Rochitte C.E. The role of cardiovascular magnetic resonance in takotsubo syndrome. J. Cardiovasc. Magn. Reson. 2017;18(1) doi: 10.1186/s12968-016-0279-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Jensch P.-J., Stiermaier T., Eitel I. Takotsubo Syndrome—Is There a Need for CMR? Curr. Heart Fail Rep. 2021;18(4):200–210. doi: 10.1007/s11897-021-00518-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ghadri J.-R., Wittstein I.S., Prasad A., et al. International Expert Consensus Document on Takotsubo Syndrome (Part II): Diagnostic Workup, Outcome, and Management. Eur. Heart J. 2018;39(22):2047–2062. doi: 10.1093/eurheartj/ehy077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tavakol M., Ashraf S., Brener S.J. Risks and Complications of Coronary Angiography: A Comprehensive Review. GJHS. 2011;4:65. doi: 10.5539/gjhs.v4n1p65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Bossone E., Lyon A., Citro R., Athanasiadis A., Meimoun P., Parodi G., Cimarelli S., Omerovic E., Ferrara F., Limongelli G., Cittadini A., Salerno-Uriarte J.A., Perrone Filardi P., Schneider B., Sechtem U., Erbel R. Takotsubo cardiomyopathy: an integrated multi-imaging approach. Eur. Heart J. Cardiovasc. Imaging. 2014;15(4):366–377. doi: 10.1093/ehjci/jet167. [DOI] [PubMed] [Google Scholar]
- 108.Pergola V., Previtero M., Cecere A., Storer V., Castiello T., Baritussio A., Cabrelle G., Mele D., Motta R., Caforio A.P., Iliceto S., Perazzolo Marra M. Clinical Value and Time Course of Pericoronary Fat Inflammation in Patients with Angiographically Nonobstructive Coronaries: A Preliminary Report. J. Clin. Med. 2021;10(8):1786. doi: 10.3390/jcm10081786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Rodriguez-Granillo G.A. Delayed enhancement cardiac computed tomography for the assessment of myocardial infarction: from bench to bedside. Cardiovasc. Diagn Ther. 2017;7:159–170. doi: 10.21037/cdt.2017.03.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sueta D., Oda S., Izumiya Y., Kaikita K., Kidoh M., Utsunomiya D., Yamashita Y., Tsujita K. Comprehensive assessment of takotsubo cardiomyopathy by cardiac computed tomography. Emerg. Radiol. 2019;26(1):109–112. doi: 10.1007/s10140-018-1610-2. [DOI] [PubMed] [Google Scholar]
- 111.Antonopoulos A.S., Sanna F., Sabharwal N., Thomas S., Oikonomou E.K., Herdman L., Margaritis M., Shirodaria C., Kampoli A.-M., Akoumianakis I., Petrou M., Sayeed R., Krasopoulos G., Psarros C., Ciccone P., Brophy C.M., Digby J., Kelion A., Uberoi R., Anthony S., Alexopoulos N., Tousoulis D., Achenbach S., Neubauer S., Channon K.M., Antoniades C. Detecting human coronary inflammation by imaging perivascular fat. Sci. Transl. Med. 2017;9(398) doi: 10.1126/scitranslmed.aal2658. [DOI] [PubMed] [Google Scholar]
- 112.Kwiecinski J., Dey D., Cadet S., Lee S.-E., Otaki Y., Huynh P.T., Doris M.K., Eisenberg E., Yun M., Jansen M.A., Williams M.C., Tamarappoo B.K., Friedman J.D., Dweck M.R., Newby D.E., Chang H.-J., Slomka P.J., Berman D.S. Peri-Coronary Adipose Tissue Density Is Associated With 18F-Sodium Fluoride Coronary Uptake in Stable Patients With High-Risk Plaques. JACC Cardiovasc Imaging. 2019;12(10):2000–2010. doi: 10.1016/j.jcmg.2018.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Gaibazzi N., Martini C., Botti A., Pinazzi A., Bottazzi B., Palumbo A.A. Coronary Inflammation by Computed Tomography Pericoronary Fat Attenuation in MINOCA and Tako-Tsubo Syndrome. J. Am. Heart Assoc. 2019;8(17) doi: 10.1161/JAHA.119.013235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Oikonomou E.K., Marwan M., Desai M.Y., Mancio J., Alashi A., Hutt Centeno E., Thomas S., Herdman L., Kotanidis C.P., Thomas K.E., Griffin B.P., Flamm S.D., Antonopoulos A.S., Shirodaria C., Sabharwal N., Deanfield J., Neubauer S., Hopewell J.C., Channon K.M., Achenbach S., Antoniades C. Non-invasive detection of coronary inflammation using computed tomography and prediction of residual cardiovascular risk (the CRISP CT study): a post-hoc analysis of prospective outcome data. Lancet. 2018;392(10151):929–939. doi: 10.1016/S0140-6736(18)31114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Takehana K. Takotsubo cardiomyopathy: What should myocardial perfusion imaging reveal. J. Nucl. Cardiol. 2021 doi: 10.1007/s12350-020-02435-3. [DOI] [PubMed] [Google Scholar]
- 116.Lee W.W. Recent Advances in Nuclear Cardiology. Nucl. Med. Mol. Imaging. 2016;50(3):196–206. doi: 10.1007/s13139-016-0433-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Adeboye A., Alkhatib D., Butt A., Yedlapati N., Garg N. A Review of the Role of Imaging Modalities in the Evaluation of Viral Myocarditis with a Special Focus on COVID-19-Related Myocarditis. Diagnostics. 2022;12(2):549. doi: 10.3390/diagnostics12020549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Matsuo S., Nakajima K., Kinuya S., Yamagishi M. Diagnostic utility of 123I-BMIPP imaging in patients with Takotsubo cardiomyopathy. J. Cardiol. 2014;64(1):49–56. doi: 10.1016/j.jjcc.2013.10.019. [DOI] [PubMed] [Google Scholar]
- 119.Christensen T.E., Bang L.E., Holmvang L., Skovgaard D.C., Oturai D.B., Søholm H., Thomsen J.H., Andersson H.B., Ghotbi A.A., Ihlemann N., Kjaer A., Hasbak P. (123)I-MIBG Scintigraphy in the Subacute State of Takotsubo Cardiomyopathy. JACC Cardiovasc. Imaging. 2016;9(8):982–990. doi: 10.1016/j.jcmg.2016.01.028. [DOI] [PubMed] [Google Scholar]
- 120.Testa M. Usefulness of myocardial positron emission tomography/nuclear imaging in Takotsubo cardiomyopathy. WJR. 2014;6(7):502. doi: 10.4329/wjr.v6.i7.502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Cimarelli S., Sauer F., Morel O., Ohlmann P., Constantinesco A., Imperiale A. Transient left ventricular dysfunction syndrome: patho-physiological bases through nuclear medicine imaging. Int. J. Cardiol. 2010;144(2):212–218. doi: 10.1016/j.ijcard.2009.04.025. [DOI] [PubMed] [Google Scholar]
- 122.Yoshida T., Hibino T., Kako N., Murai S., Oguri M., Kato K., Yajima K., Ohte N., Yokoi K., Kimura G. A pathophysiologic study of tako-tsubo cardiomyopathy with F-18 fluorodeoxyglucose positron emission tomography. Eur. Heart J. 2007;28(21):2598–2604. doi: 10.1093/eurheartj/ehm401. [DOI] [PubMed] [Google Scholar]
- 123.Tanimura M., Dohi K., Imanaka-Yoshida K., Omori T., Moriwaki K., Nakamori S., Yamada N., Ito M. Fulminant Myocarditis With Prolonged Active Lymphocytic Infiltration After Hemodynamic Recovery. Int. Heart J. 2017;58(2):294–297. doi: 10.1536/ihj.16-225. [DOI] [PubMed] [Google Scholar]
- 124.Sulaiman S., Rajesh G.N., Vellani H. Acute myocarditis morphologically mimicking reverse takotsubo cardiomyopathy. IHJ Cardiovasc. Case Reports (CVCR). 2017;1(1):42–45. doi: 10.1016/j.ihjccr.2017.04.001. [DOI] [Google Scholar]
- 125.Hanneman K., Kadoch M., Guo H.H., Jamali M., Quon A., Iagaru A., Herfkens R. Initial Experience With Simultaneous 18F-FDG PET/MRI in the Evaluation of Cardiac Sarcoidosis and Myocarditis. Clin. Nucl. Med. 2017;42(7):e328–e334. doi: 10.1097/RLU.0000000000001669. [DOI] [PubMed] [Google Scholar]
- 126.Lawal I., Sathekge M. F-18 FDG PET/CT imaging of cardiac and vascular inflammation and infection. Br. Med. Bull. 2016;120(1):55–74. doi: 10.1093/bmb/ldw035. [DOI] [PubMed] [Google Scholar]
- 127.Aoki Y., Kodera S., Watanabe T., Miyauchi Y., Kanda J., Ooe K. Autopsy findings in takotsubo cardiomyopathy with special reference to the autonomic nervous system. Int. J. Cardiol. 2016;203:236–237. doi: 10.1016/j.ijcard.2015.10.121. [DOI] [PubMed] [Google Scholar]
- 128.Mitchell A., Marquis F. Can takotsubo cardiomyopathy be diagnosed by autopsy? Report of a presumed case presenting as cardiac rupture. BMC Clin. Pathol. 2017;17:4. doi: 10.1186/s12907-017-0045-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ghalyoun B.A., Guragai N., Garris R., et al. Abstract 11626: Faster Recovery in Takotsubo With Prior Beta-blocker Use. Circulation. 2019;140 Abstract 11626. [Google Scholar]
- 130.Isogai T., Matsui H., Tanaka H., Fushimi K., Yasunaga H. Early β-blocker use and in-hospital mortality in patients with Takotsubo cardiomyopathy. Heart. 2016;102(13):1029–1035. doi: 10.1136/heartjnl-2015-308712. [DOI] [PubMed] [Google Scholar]
- 131.Brunetti N.D., Santoro F., De Gennaro L., Correale M., Gaglione A., Di Biase M. Drug treatment rates with beta-blockers and ACE-inhibitors/angiotensin receptor blockers and recurrences in takotsubo cardiomyopathy: A meta-regression analysis. Int. J. Cardiol. 2016;214:340–342. doi: 10.1016/j.ijcard.2016.03.196. [DOI] [PubMed] [Google Scholar]
- 132.Dias A., Franco E., Koshkelashvili N., Bhalla V., Pressman G.S., Hebert K., Figueredo V.M. Antiplatelet therapy in Takotsubo cardiomyopathy: does it improve cardiovascular outcomes during index event? Heart Vessels. 2016;31(8):1285–1290. doi: 10.1007/s00380-015-0729-2. [DOI] [PubMed] [Google Scholar]
- 133.Yayehd K., N’da N.W., Belle L., Bataille V., Hanssen M., Leddet P., Aupetit J.-F., Commeau P., Filippi E., Georges J.-L., Albert F., Rangé G., Meimoun P., Marcaggi X., Baleynaud S., Nallet O., Dibie A., Barnay C., Jouve B., Legrand M., Cattan S., Mulak G., Simon T., Danchin N., Dujardin J.-J. Management of Takotsubo cardiomyopathy in non-academic hospitals in France: The Observational French SyndromEs of TakoTsubo (OFSETT) study. Arch. Cardiovasc. Dis. 2016;109(1):4–12. doi: 10.1016/j.acvd.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 134.Dias A. Incidence and predictors of stroke during the index event in an ethnically diverse Takotsubo cardiomyopathy population. FN. 2016 doi: 10.11138/FNeur/2016.31.3.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.D'Ascenzo F., Gili S., Bertaina M., Iannaccone M., Cammann V.L., Di Vece D., Kato K., Saglietto A., Szawan K.A., Frangieh A.H., Boffini B., Annaratone M., Sarcon A., Levinson R.A., Franke J., Napp L.C., Jaguszewski M., Noutsias M., Münzel T., Knorr M., Heiner S., Katus H.A., Burgdorf C., Schunkert H., Thiele H., Bauersachs J., Tschöpe C., Pieske B.M., Rajan L., Michels G., Pfister R., Cuneo A., Jacobshagen C., Hasenfuß G., Karakas M., Koenig W., Rottbauer W., Said S.M., Braun‐Dullaeus R.C., Banning A., Cuculi F., Kobza R., Fischer T.A., Vasankari T., Airaksinen K.E.J., Opolski G., Dworakowski R., MacCarthy P., Kaiser C., Osswald S., Galiuto L., Crea F., Dichtl W., Franz W.M., Empen K., Felix S.B., Delmas C., Lairez O., El‐Battrawy I., Akin I., Borggrefe M., Horowitz J.D., Kozel M., Tousek P., Widimský P., Gilyarova E., Shilova A., Gilyarov M., Biondi‐Zoccai G., Winchester D.E., Ukena C., Neuhaus M., Bax J.J., Prasad A., Di Mario C., Böhm M., Gasparini M., Ruschitzka F., Bossone E., Citro R., Rinaldi M., De Ferrari G.M., Lüscher T., Ghadri J.R., Templin C. Impact of aspirin on takotsubo syndrome: a propensity score-based analysis of the InterTAK Registry. Eur. J. Heart Fail. 2020;22(2):330–337. doi: 10.1002/ejhf.1698. [DOI] [PubMed] [Google Scholar]
- 136.Santoro F., Ieva R., Musaico F., Ferraretti A., Triggiani G., Tarantino N., Biase M.D., Brunetti N.D. Lack of Efficacy of Drug Therapy in Preventing Takotsubo Cardiomyopathy Recurrence: A Meta-analysis. Clin. Cardiol. 2014;37(7):434–439. doi: 10.1002/clc.22280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Lin J., Wu B., Lin L., Ding Y., Zhong B., Huang Z., Lin M., Xu D.-P. Effect of aspirin in takotsubo syndrome: protocol of a systematic review and meta-analysis. BMJ Open. 2021;11(8):e046727. doi: 10.1136/bmjopen-2020-046727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Bybee K.A., Kara T., Prasad A., Lerman A., Barsness G.W., Wright R.S., Rihal C.S. Systematic Review: Transient Left Ventricular Apical Ballooning: A Syndrome That Mimics ST-Segment Elevation Myocardial Infarction. Ann. Intern. Med. 2004;141(11):858. doi: 10.7326/0003-4819-141-11-200412070-00010. [DOI] [PubMed] [Google Scholar]
- 139.Kumar S., Kaushik S., Nautiyal A., Choudhary S.K., Kayastha B.L., Mostow N., Lazar J.M. Cardiac Rupture in Takotsubo Cardiomyopathy: A Systematic Review. Clin. Cardiol. 2011;34(11):672–676. doi: 10.1002/clc.20957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Abanador-Kamper N., Kamper L., Wolfertz J., Pomjanski W., Wolf-Pütz A., Seyfarth M. Evaluation of therapy management and outcome in Takotsubo syndrome. BMC Cardiovasc Disord. 2017;17(1) doi: 10.1186/s12872-017-0661-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.O’Keefe E.L., Torres-Acosta N., O’Keefe J.H., Sturgess J.E., Lavie C.J., Bybee K.A. Takotsubo Syndrome: Cardiotoxic Stress in the COVID Era, Mayo Clinic Proceedings: Innovations. Qual. Outcomes. 2020;4(6):775–785. doi: 10.1016/j.mayocpiqo.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Omerovic E. Takotsubo Syndrome—Scientific Basis for Current Treatment Strategies. Heart Failure Clinics. 2016;12(4):577–586. doi: 10.1016/j.hfc.2016.06.008. [DOI] [PubMed] [Google Scholar]
- 143.Nalluri N., Asti D., Anugu V.R., Ibrahim U., Lafferty J.C., Olkovsky Y. Cardiogenic Shock Secondary to Takotsubo Cardiomyopathy in a Patient with Preexisting Hypertrophic Obstructive Cardiomyopathy. CASE. 2018;2(3):78–81. doi: 10.1016/j.case.2017.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Yokoshiki H., Katsube Y., Sunagawa M., Sperelakis N. Levosimendan, a novel Ca2+ sensitizer, activates the glibenclamide-sensitive K+ channel in rat arterial myocytes. Eur. J. Pharmacol. 1997;333(2-3):249–259. doi: 10.1016/S0014-2999(97)01108-4. [DOI] [PubMed] [Google Scholar]
- 145.Du Toit E.F., Genis A., Opie L.H., Pollesello P., Lochner A. A role for the RISK pathway and K ATP channels in pre- and post-conditioning induced by levosimendan in the isolated guinea pig heart: Levosimendan pre- and post-conditioning. Br. J. Pharmacol. 2008;154(1):41–50. doi: 10.1038/bjp.2008.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.D.A. Baran, C.L. Grines, S. Bailey, et al., SCAI clinical expert consensus statement on the classification of cardiogenic shock: This document was endorsed by the American College of Cardiology (ACC), the American Heart Association (AHA), the Society of Critical Care Medicine (SCCM), and the Society of Thoracic Surgeons (STS) in April 2019, Catheter Cardiovasc Interv. (2019) ccd.28329. 10.1002/ccd.28329. [DOI] [PubMed]
- 147.Santoro F., Stiermaier T., Tarantino N., De Gennaro L., Moeller C., Guastafierro F., Marchetti M.F., Montisci R., Carapelle E., Graf T., Caldarola P., Thiele H., Di Biase M., Brunetti N.D., Eitel I. Left Ventricular Thrombi in Takotsubo Syndrome: Incidence, Predictors, and Management: Results From the GEIST (German Italian Stress Cardiomyopathy) Registry. JAHA. 2017;6(12) doi: 10.1161/JAHA.117.006990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Möller C., Eitel C., Thiele H., Eitel I., Stiermaier T. Ventricular arrhythmias in patients with Takotsubo syndrome. J. Arrhythmia. 2018;34(4):369–375. doi: 10.1002/joa3.12029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Brown K.H., Trohman R.G., Madias C. Arrhythmias in Takotsubo Cardiomyopathy, Cardiac Electrophysiology. Clinics. 2015;7(2):331–340. doi: 10.1016/j.ccep.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 150.Nordkin I., Levinas T., Rosenfeld I., Halabi M. Torsades de pointes after prolonged intravenous amiodarone therapy for atrial fibrillation. Clinical Case Reports. 2021;9(1):391–394. doi: 10.1002/ccr3.3539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Shenthar J., Rachaiah J.M., Pillai V., Chakali S.S., Balasubramanian V., Chollenhalli Nanjappa M. Incidence of drug-induced torsades de pointes with intravenous amiodarone. Indian Heart J. 2017;69(6):707–713. doi: 10.1016/j.ihj.2017.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.B. Cohagan, D. Brandis, Torsade de Pointes, in: StatPearls, StatPearls Publishing, Treasure Island (FL), 2022. http://www.ncbi.nlm.nih.gov/books/NBK459388/ (accessed February 20, 2022).
- 153.Stiermaier T., Rommel K.-P., Eitel C., Möller C., Graf T., Desch S., Thiele H., Eitel I. Management of arrhythmias in patients with Takotsubo cardiomyopathy: Is the implantation of permanent devices necessary? Heart Rhythm. 2016;13(10):1979–1986. doi: 10.1016/j.hrthm.2016.06.013. [DOI] [PubMed] [Google Scholar]
- 154.Ong G.J., Nguyen T.H., Stansborough J., Surikow S., Mahadavan G., Worthley M., Horowitz J. The N-AcetylCysteine and RAMipril in Takotsubo Syndrome Trial (NACRAM): Rationale and design of a randomised controlled trial of sequential N-Acetylcysteine and ramipril for the management of Takotsubo Syndrome. Contemporary Clinical Trials. 2020;90:105894. doi: 10.1016/j.cct.2019.105894. [DOI] [PubMed] [Google Scholar]
- 155.Albakri A. Takotsubo cardiomyopathy: a review of literature on clinical status and meta-analysis of diagnosis and medical therapy. J. Integr. Cardiol. 2018;4 doi: 10.15761/JIC.1000248. [DOI] [Google Scholar]
- 156.Möller C., Stiermaier T., Brabant G., Graf T., Thiele H., Eitel I. Comprehensive assessment of sex hormones in Takotsubo syndrome. Int. J. Cardiol. 2018;250:11–15. doi: 10.1016/j.ijcard.2017.10.047. [DOI] [PubMed] [Google Scholar]
- 157.De Vecchis R., Ariano C. Aldosterone receptor antagonists decrease mortality and cardiovascular hospitalizations in chronic heart failure with reduced left ventricular ejection fraction, but not in chronic heart failure with preserved left ventricular ejection fraction: a meta-analysis of randomized controlled trials. Minerva Cardiol. Angiol. 2017;65 doi: 10.23736/S0026-4725.16.04293-6. [DOI] [PubMed] [Google Scholar]
- 158.Medina de Chazal H., Del Buono M.G., Keyser-Marcus L., et al. Stress Cardiomyopathy Diagnosis and Treatment. J. Am. Coll. Cardiol. 2018;72:1955–1971. doi: 10.1016/j.jacc.2018.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.D. Dawson, Physical Exercise and Mental Wellbeing Rehabilitation for Acute Stress-induced Takotsubo Cardiomyopathy: The PLEASE Study (PLEASE), (2021). https://clinicaltrials.gov/ct2/show/NCT04425785.
- 160.Syed M., Khan M.Z., Osman M., Alharbi A., Khan M.U., Munir M.B., Balla S. Comparison of Outcomes in Patients With Takotsubo Syndrome With-vs-Without Cardiogenic Shock. Am. J. Cardiol. 2020;136:24–31. doi: 10.1016/j.amjcard.2020.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Ding K.J., Cammann V.L., Szawan K.A., et al. Intraventricular Thrombus Formation and Embolism in Takotsubo Syndrome: Insights From the International Takotsubo Registry. ATVB. 2020;40(1):279–287. doi: 10.1161/ATVBAHA.119.313491. [DOI] [PubMed] [Google Scholar]
- 162.Gili S., Cammann V.L., Schlossbauer S.A., et al. Cardiac arrest in takotsubo syndrome: results from the InterTAK Registry. Eur. Heart J. 2019;40(26):2142–2151. doi: 10.1093/eurheartj/ehz170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Jesel L., Berthon C., Messas N., Lim H.S., Girardey M., Marzak H., Marchandot B., Trinh A., Ohlmann P., Morel O. Atrial arrhythmias in Takotsubo cardiomyopathy: incidence, predictive factors, and prognosis. EP Europace. 2019;21(2):298–305. doi: 10.1093/europace/euy147. [DOI] [PubMed] [Google Scholar]
- 164.Santoro F., Guastafierro F., Zimotti T., Mallardi A., Leopizzi A., Cannone M., Di Biase M., Brunetti N.D. Neutrophil/lymphocyte ratio predicts in-hospital complications in Takotsubo syndrome. Results from a prospective multi-center registry. Clin. Cardiol. 2020;43(11):1294–1300. doi: 10.1002/clc.23442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Santoro F., Tarantino N., Ferraretti A., Ieva R., Musaico F., Guastafierro F., Di Martino L., Di Biase M., Brunetti N.D. Serum interleukin 6 and 10 levels in Takotsubo cardiomyopathy: Increased admission levels may predict adverse events at follow-up. Atherosclerosis. 2016;254:28–34. doi: 10.1016/j.atherosclerosis.2016.09.012. [DOI] [PubMed] [Google Scholar]
- 166.Damodaran S., Mrozek E., Liebner D., Kendra K. Focal Takotsubo Cardiomyopathy With High-Dose Interleukin-2 Therapy for Malignant Melanoma. J. Natl. Compr. Canc. Netw. 2014;12(12):1666–1670. doi: 10.6004/jnccn.2014.0168. [DOI] [PubMed] [Google Scholar]
- 167.Santoro F., Costantino M.D., Guastafierro F., Triggiani G., Ferraretti A., Tarantino N., Saguner A., Di Biase M., Brunetti N.D. Inflammatory patterns in Takotsubo cardiomyopathy and acute coronary syndrome: A propensity score matched analysis. Atherosclerosis. 2018;274:157–161. doi: 10.1016/j.atherosclerosis.2018.05.017. [DOI] [PubMed] [Google Scholar]
- 168.Akashi Y.J., Nef H.M., Lyon A.R. Epidemiology and pathophysiology of Takotsubo syndrome. Nat. Rev. Cardiol. 2015;12(7):387–397. doi: 10.1038/nrcardio.2015.39. [DOI] [PubMed] [Google Scholar]
- 169.Nef H.M., Mollmann H., Kostin S., Troidl C., Voss S., Weber M., Dill T., Rolf A., Brandt R., Hamm C.W., Elsasser A. Tako-Tsubo cardiomyopathy: intraindividual structural analysis in the acute phase and after functional recovery. Eur. Heart J. 2007;28(20):2456–2464. doi: 10.1093/eurheartj/ehl570. [DOI] [PubMed] [Google Scholar]
- 170.Singh K., Carson K., Usmani Z., Sawhney G., Shah R., Horowitz J. Systematic review and meta-analysis of incidence and correlates of recurrence of takotsubo cardiomyopathy. Int. J. Cardiol. 2014;174(3):696–701. doi: 10.1016/j.ijcard.2014.04.221. [DOI] [PubMed] [Google Scholar]
- 171.Kato K., Kitahara H., Kobayashi Y. Recurrence of Takotsubo Cardiomyopathy. ICFJ. 2016;5 doi: 10.17987/icfj.v5i0.239. [DOI] [Google Scholar]
- 172.Lau C., Chiu S., Nayak R., Lin B., Lee M.-S. Survival and risk of recurrence of takotsubo syndrome. Heart. 2021;107(14):1160–1166. doi: 10.1136/heartjnl-2020-318028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Sager H.B., Schunkert H., Kurowski V. Recurrent mid-ventricular Tako-Tsubo cardiomyopathy: Three episodes of a uniform cardiac response to varying stressors. Int. J. Cardiol. 2011;152(1):e22–e24. doi: 10.1016/j.ijcard.2010.09.081. [DOI] [PubMed] [Google Scholar]
- 174.Stiermaier T., Moeller C., Oehler K., Desch S., Graf T., Eitel C., Vonthein R., Schuler G., Thiele H., Eitel I. Long-term excess mortality in takotsubo cardiomyopathy: predictors, causes and clinical consequences. Eur. J. Heart Fail. 2016;18(6):650–656. doi: 10.1002/ejhf.494. [DOI] [PubMed] [Google Scholar]
- 175.MatabuenaGomez-Limon J., IsazaArana S., Robledo-Carmona J., AlaniaTorres E., TorresLlergo J., Valle-Racero J.I., LopezPardo F., Martinez-Martinez A., Jimenez-Navarro M., Urbano-Moral J.A. Clinical and echocardiographic course in takotsubo cardiomyopathy: Longterm followup from a multicenter study. Int. J. Cardiol. 2017;228:97–102. doi: 10.1016/j.ijcard.2016.11.256. [DOI] [PubMed] [Google Scholar]
- 176.Bento D., Azevedo O., Santos R., Almeida A., Domingues K., Marmelo B., Reis L., Ruivo C., Guerreiro R., Lima R., Faria R., Marreiros A., Marques N. Short- and medium-term prognosis of Takotsubo syndrome in a Portuguese population. Rev. Port. Cardiol. 2019;38(5):349–357. doi: 10.1016/j.repc.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 177.Arcari L., Musumeci M.B., Stiermaier T., El-Battrawy I., Möller C., Guerra F., Novo G., Mariano E., Limite L.R., Cacciotti L., Semeraro R., Volpe M., Romeo F., Caldarola P., Thiele H., Akin I., Brunetti N.D., Eitel I., Santoro F. Incidence, determinants and prognostic relevance of dyspnea at admission in patients with Takotsubo syndrome: results from the international multicenter GEIST registry. Sci. Rep. 2020;10(1) doi: 10.1038/s41598-020-70445-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.El-Battrawy I., Santoro F., Stiermaier T., Möller C., Guastafierro F., Novo G., Novo S., Santangelo A., Mariano E., Romeo F., Romeo F., Thiele H., Guerra F., Capucci A., Giannini I., Caldarola P., Brunetti N.D., Eitel I., Akin I. Prevalence, management, and outcome of adverse rhythm disorders in takotsubo syndrome: insights from the international multicenter GEIST registry. Heart Fail. Rev. 2020;25(3):505–511. doi: 10.1007/s10741-019-09856-4. [DOI] [PubMed] [Google Scholar]
- 179.El-Battrawy I., Zhao Z., Lan H., Schünemann J.-D., Sattler K., Buljubasic F., Patocskai B., Li X., Yücel G., Lang S., Nowak D., Cyganek L., Bieback K., Utikal J., Zimmermann W.-H., Ravens U., Wieland T., Borggrefe M., Zhou X.-B., Akin I. Estradiol protection against toxic effects of catecholamine on electrical properties in human-induced pluripotent stem cell derived cardiomyocytes. Int. J. Cardiol. 2018;254:195–202. doi: 10.1016/j.ijcard.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 180.Yassin A.S., Subahi A., Adegbala O., Abubakar H., Dawdy J., Mishra T., Akintoye E., Shereef H., Ghandour M., Alhusain R., Shokr M., Oviedo C., Afonso L. Clinical Impact of Atrial Fibrillation on Short-Term Outcomes and In-Hospital Mortality in Patients with Takotsubo Syndrome: A Propensity-Matched National Study. Cardiovasc. Revascularization Med. 2020;21(4):522–526. doi: 10.1016/j.carrev.2019.07.022. [DOI] [PubMed] [Google Scholar]
- 181.Bill V., El-Battrawy I., Behnes M., Baumann S., Becher T., Elmas E., Hoffmann U., Haghi D., Fastner C., Kuschyk J., Papavassiliu T., Borggrefe M., Akin I. “Diabetes paradox” in Takotsubo Cardiomyopathy. Int. J. Cardiol. 2016;224:88–89. doi: 10.1016/j.ijcard.2016.08.136. [DOI] [PubMed] [Google Scholar]
- 182.Abe T., Olaosebikan K., babatunde A., Abe T., Tobun T. Abstract P050: A query of The diabetes paradox in Takotsubo cardiomyopathy. Hypertension. 2020;76(Suppl_1) doi: 10.1161/hyp.76.suppl_1.P050. [DOI] [Google Scholar]
- 183.Ahuja K.R., Nazir S., Jain V., Isogai T., Saad A.M., Verma B.R., Shekhar S., Kumar R., Eltahawy E.A., Madias J.E. Takotsubo syndrome: Does “Diabetes Paradox” exist? Heart Lung. 2021;50(2):316–322. doi: 10.1016/j.hrtlng.2021.01.005. [DOI] [PubMed] [Google Scholar]
- 184.Harris K.M., Rosman L., Burg M.M., Salmoirago-Blotcher E. Modifiable lifestyle factors in women with Takotsubo syndrome: A case-control study. Heart Lung. 2020;49(5):524–529. doi: 10.1016/j.hrtlng.2020.03.001. [DOI] [PubMed] [Google Scholar]
- 185.Pizzino G., Bitto A., Crea P., Khandheria B., Vriz O., Carerj S., Squadrito F., Minisini R., Citro R., Cusmà-Piccione M., Madaffari A., Andò G., Altavilla D., Zito C. Takotsubo syndrome and estrogen receptor genes: partners in crime? J. Cardiovasc. Med. 2017;18(4):268–276. doi: 10.2459/JCM.0000000000000500. [DOI] [PubMed] [Google Scholar]
- 186.Vriz O., Minisini R., Citro R., Guerra V., Zito C., De Luca G., Pavan D., Pirisi M., Limongelli G., Bossone E. Analysis of β1 and β2-adrenergic receptors polymorphism in patients with apical ballooning cardiomyopathy. Acta Cardiol. 2011;66(6):787–790. doi: 10.1080/AC.66.6.2136964. [DOI] [PubMed] [Google Scholar]
- 187.Figtree G.A., Bagnall R.D., Abdulla I., Buchholz S., Galougahi K.K., Yan W., Tan T., Neil C., Horowitz J.D., Semsarian C., Ward M.R. No association of G-protein-coupled receptor kinase 5 or β-adrenergic receptor polymorphisms with Takotsubo cardiomyopathy in a large Australian cohort. Eur. J. Heart Fail. 2013;15(7):730–733. doi: 10.1093/eurjhf/hft040. [DOI] [PubMed] [Google Scholar]
- 188.Mattsson E., Saliba-Gustafsson P., Ehrenborg E., Tornvall P. Lack of genetic susceptibility in takotsubo cardiomyopathy: a case-control study. BMC Med. Genet. 2018;19(1) doi: 10.1186/s12881-018-0544-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Kalani M.Y.S., Siniard A.L., Corneveaux J.J., Bruhns R., Richholt R., Forseth J., Zabramski J.M., Nakaji P., Spetzler R.F., Huentelman M.J. Rare Variants in Cardiomyopathy Genes Associated With Stress-Induced Cardiomyopathy. Neurosurgery. 2016;78(6):835–843. doi: 10.1227/NEU.0000000000001152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Keller H., Neuhold U., Weidinger F., et al. Takotsubo as Initial Manifestation of Non-Myopathic Cardiomyopathy Due to the Titin Variant c.1489G > T. Medicines. 2018;5:80. doi: 10.3390/medicines5030080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Pan X.-Y., Zhang Z.-W. MFGE8, ALB, APOB, APOE, SAA1, A2M, and C3 as Novel Biomarkers for Stress Cardiomyopathy. Cardiovasc. Ther. 2020;2020:1–11. doi: 10.1155/2020/1615826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Dande A.S., Sena S.F., Wasserman H.S., Warshofsky M.K., Belsky J.L. Prevalence and Consequences of Vitamin D Insufficiency in Women With Takotsubo Cardiomyopathy. J. Clin. Endocrinol. Metabol. 2013;98(5):E872–E876. doi: 10.1210/jc.2013-1082. [DOI] [PubMed] [Google Scholar]
- 193.Galli F., Bursi F., Carugo S. Traumatic Events, Personality and Psychopathology in Takotsubo Syndrome: A Systematic Review. Front. Psychol. 2019;10:2742. doi: 10.3389/fpsyg.2019.02742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Salmoirago-Blotcher E., Rosman L., Wittstein I.S., Dunsiger S., Swales H.H., Aurigemma G.P., Ockene I.S. Psychiatric history, post-discharge distress, and personality characteristics among incident female cases of takotsubo cardiomyopathy: A case–control study. Heart Lung. 2016;45(6):503–509. doi: 10.1016/j.hrtlng.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 195.Prasitlumkum N., Kittipibul V., Limpruttidham N., Rattanawong P., Chongsathidkiet P., Boondarikpornpant T. The presence of atrial fibrillation in Takotsubo cardiomyopathy is predictive of mortality: Systematic review and meta-analysis. Ann. Noninvasive Electrocardiol. 2019;24(1):e12566. doi: 10.1111/anec.12566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Neil C.J.A., Chong C.-R., Nguyen T.H., Horowitz J.D. Occurrence of Tako-Tsubo Cardiomyopathy in Association with Ingestion of Serotonin/Noradrenaline Reuptake Inhibitors. Heart, Lung Circulat. 2012;21(4):203–205. doi: 10.1016/j.hlc.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 197.Gurunathan U. Takotsubo Cardiomyopathy and Intraoperative Cardiac Arrest: Is Desvenlafaxine a Contributing Factor? J. Cardiothorac. Vasc. Anesth. 2018;32(1):e16–e18. doi: 10.1053/j.jvca.2017.08.031. [DOI] [PubMed] [Google Scholar]
- 198.Selke K.J., Dhar G., Cohn J.M. Takotsubo cardiomyopathy associated with titration of duloxetine. Tex. Heart Inst. J. 2011;38:573–576. [PMC free article] [PubMed] [Google Scholar]
- 199.Rotondi F., Manganelli F., Carbone G., Stanco G. “Tako-Tsubo” Cardiomyopathy and Duloxetine Use. Southern Medical J. 2011;104(5):345–347. doi: 10.1097/SMJ.0b013e318213f3e5. [DOI] [PubMed] [Google Scholar]
- 200.Sasaki H., Yumoto K., Nanao T., Nishizawa H., Funada S., Aoki H., Kato K. Cardiogenic shock due to takotsubo cardiomyopathy associated with serotonin syndrome. J. Cardiol. Cases. 2013;7(1):e1–e3. doi: 10.1016/j.jccase.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Forman M.B., Sutej P.G., Jackson E.K. Hypertension, tachycardia, and reversible cardiomyopathy temporally associated with milnacipran use. Tex. Heart Inst. J. 2011;38:714–718. [PMC free article] [PubMed] [Google Scholar]
- 202.Schroeder I., Zoller M., Angstwurm M., Kur F., Frey L. Venlafaxine Intoxication with Development of Takotsubo Cardiomyopathy: Successful Use of Extracorporeal Life Support, Intravenous Lipid Emulsion and Cytosorb ®. Int. J. Artif. Organs. 2017;40(7):358–360. doi: 10.5301/ijao.5000595. [DOI] [PubMed] [Google Scholar]
- 203.Vasudev R., Rampal U., Patel H., Patel K., Bikkina M., Shamoon F. Selective serotonin-norepinephrine reuptake inhibitors-induced Takotsubo cardiomyopathy. North Am. J. Med. Sci. 2016;8(7):312. doi: 10.4103/1947-2714.187153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Christoph M., Ebner B., Stolte D., Ibrahim K., Kolschmann S., Strasser R.H., Schön S. Broken heart syndrome: Tako Tsubo cardiomyopathy associated with an overdose of the serotonin–norepinephrine reuptake inhibitor Venlafaxine. Eur. Neuropsychopharmacol. 2010;20(8):594–597. doi: 10.1016/j.euroneuro.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 205.Elikowski W., Małek-Elikowska M., Ganowicz-Kaatz T., et al. Transient left ventricular hypertrophy in a 30-year-old female with chronic emotional stress and depression treated with venlafaxine. Pol. Merkur Lekarski. 2019;47:144–149. [PubMed] [Google Scholar]
- 206.Naguy A., Al-Mutairi H., Al-Tajali A. Atomoxetine-related Takotsubo Cardiomyopathy. J. Psychiatric Practice. 2016;22:232–233. doi: 10.1097/PRA.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 207.Conrad S.K., Catalano M.C., Catalano G. The Use of Fluoxetine in a Patient With Takotsubo Cardiomyopathy. J. Psychiatric Practice. 2016;22:234–238. doi: 10.1097/PRA.0000000000000151. [DOI] [PubMed] [Google Scholar]
- 208.Verduin M.L. Commentary on 2 Cases of Takotsubo Cardiomyopathy Involving Psychotropic Medication. J. Psychiatric Practice. 2016;22:239–240. doi: 10.1097/PRA.0000000000000153. [DOI] [PubMed] [Google Scholar]
- 209.Prasad A., Madhavan M., Chareonthaitawee P. Cardiac sympathetic activity in stress-induced (Takotsubo) cardiomyopathy. Nat. Rev. Cardiol. 2009;6(6):430–434. doi: 10.1038/nrcardio.2009.51. [DOI] [PubMed] [Google Scholar]
- 210.Basselin C., Fontanges T., Descotes J., et al. 5-Fluorouracil–Induced Tako-Tsubo–Like Syndrome. Pharmacotherapy. 2011;31 doi: 10.1592/phco.31.2.226. 226–226. [DOI] [PubMed] [Google Scholar]
- 211.Stewart T., Pavlakis N., Ward M. Cardiotoxicity with 5-fluorouracil and capecitabine: more than just vasospastic angina: Fluoropyrimidine cardiotoxicity. Int. Med. J. 2010;40:303–307. doi: 10.1111/j.1445-5994.2009.02144.x. [DOI] [PubMed] [Google Scholar]
- 212.Saif M.W., Smith M., Maloney A. The First Case of Severe Takotsubo Cardiomyopathy Associated with 5-Fluorouracil in a Patient with Abnormalities of Both Dihydropyrimidine Dehydrogenase (DPYD) and Thymidylate Synthase (TYMS) Genes. Cureus. 2016 doi: 10.7759/cureus.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Kumar D., Warsha F., Mehta A., et al. 5-Fluorouracil Induced Takotsubo Cardiomyopathy Complicated by Left Ventricular Thrombosis. Cureus. 2021 doi: 10.7759/cureus.14049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Bhardwaj P.V., Chaubey V.K., Islam A.M. Capecitabine-Induced Takotsubo Cardiomyopathy: A Case Report. Perm J. 2019;23 doi: 10.7812/TPP/18.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Y-Hassan S., Tornvall P., Törnerud M., Henareh L. Capecitabine caused cardiogenic shock through induction of global takotsubo syndrome. Cardiovasc. Revascularizat. Med. 2013;14(1):57–61. doi: 10.1016/j.carrev.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 216.Qasem A., Bin Abdulhak A.A., Aly A., Moormeier J. Capecitabine-Induced Takotsubo Cardiomyopathy: A Case Report and Literature Review. Am. J .Ther. 2016;23(5):e1188–e1192. doi: 10.1097/MJT.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 217.Ozbay B., Gurses E., Kemal H., Simsek E., Kultursay H. P256 Takotsubo syndrome early after treatment due to non cardiotoxic chemotheraphy agents. Eur. Heart J. - Cardiovasc. Imag. 2020;21(Supplement_1) doi: 10.1093/ehjci/jez319.117. [DOI] [Google Scholar]
- 218.Zalewska-Adamiec M., Klonowska P., Małyszko J., Kuźma Ł., Bachorzewska-Gajewska H., Dobrzycki S. Primary Takotsubo Syndrome as a Complication of Bladder Cancer Treatment in a 62-Year-Old Woman. Am. J. Case Rep. 2021;22 doi: 10.12659/AJCR.930090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Matsumoto T., Oda T., Yoshida Y., Kimura S., Himei H., Tsuduki T., Takagi S., Takatani M., Morishita H. Takotsubo cardiomyopathy caused by infusion reaction to trastuzumab. Int. Cancer Conf. J. 2020;9(1):28–31. doi: 10.1007/s13691-019-00396-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Burgy M., Brossat H., Barthelemy P., et al. First report of trastuzumab treatment after postoperative Takotsubo cardiomyopathy. Anticancer Res. 2014;34:3579–3582. [PubMed] [Google Scholar]
- 221.Khanji M., Nolan S., Gwynne S., et al. Tako-Tsubo Syndrome after Trastuzumab — An Unusual Complication of Chemotherapy for Breast Cancer. Clin. Oncol. 2013;25:329. doi: 10.1016/j.clon.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 222.Bodziock G., Armstrong C., Montgomery J. Flecainide overdose presenting with long QT and acute Takotsubo cardiomyopathy. J. Electrocardiol. 2019;52:7–9. doi: 10.1016/j.jelectrocard.2018.09.010. [DOI] [PubMed] [Google Scholar]
- 223.Friedman P.L., Montgomery S., Matas N. Sotalol and a broken heart. J. Cardiovasc. Electrophysiol. 2010;21:207–210. doi: 10.1111/j.1540-8167.2009.01520.x. [DOI] [PubMed] [Google Scholar]
- 224.Capel I., Tasa-Vinyals E., Cano-Palomares A., Bergés-Raso I., Albert L., Rigla M., Caixàs A. Takotsubo cardiomyopathy in amiodarone-induced hyperthyroidism, Endocrinology. Diabetes Metabol. Case Reports. 2017;2017 doi: 10.1530/EDM-16-0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Tomcsányi J., Arabadzisz H., Frész T., Sármán B., Bózsik B., Zsoldos A., Simor T. Reverse Takotsubo syndrome pattern induced by local anaesthesia. Orv. Hetil. 2008;149(50):2387–2389. doi: 10.1556/oh.2008.28433. [DOI] [PubMed] [Google Scholar]
- 226.Faleiro Oliveira J., Rebelo Pacheco S., Moniz M., et al. Síndrome Takotsubo após procedimento anestésico em idade pediátrica – um caso clínico. Revista Portuguesa de Cardiologia. 2016;35 doi: 10.1016/j.repc.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 227.Glamore M., Wolf C., Boolbol J., Kelly M. Broken Heart Syndrome. Aesthetic Surg. J. 2012;32(1):58–60. doi: 10.1177/1090820X11430500. [DOI] [PubMed] [Google Scholar]
- 228.Abraham J., Mudd J.O., Kapur N., Klein K., Champion H.C., Wittstein I.S. Stress Cardiomyopathy After Intravenous Administration of Catecholamines and Beta-Receptor Agonists. J. Am. Coll. Cardiol. 2009;53(15):1320–1325. doi: 10.1016/j.jacc.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 229.Yoshikawa T. Takotsubo cardiomyopathy, a new concept of cardiomyopathy: Clinical features and pathophysiology. Int. J. Cardiol. 2015;182:297–303. doi: 10.1016/j.ijcard.2014.12.116. [DOI] [PubMed] [Google Scholar]
- 230.Scantlebury D.C., Prasad A., Rabinstein A.A., Best P.J.M. Prevalence of Migraine and Raynaud Phenomenon in Women With Apical Ballooning Syndrome (Takotsubo or Stress Cardiomyopathy) Am. J. Cardiol. 2013;111(9):1284–1288. doi: 10.1016/j.amjcard.2013.01.269. [DOI] [PubMed] [Google Scholar]
- 231.Yaman M., Arslan U., Kaya A., Akyol A., Ozturk F., Okudan Y.E., Bayramoglu A., Bektas O. Levosimendan accelerates recovery in patients with takotsubo cardiomyopathy. Cardiol J. 2016;23(6):610–615. doi: 10.5603/CJ.a2016.0100. [DOI] [PubMed] [Google Scholar]
- 232.Ansari U., El-Battrawy I., Fastner C., Behnes M., Sattler K., Huseynov A., Baumann S., Tülümen E., Borggrefe M., Akin I. Clinical outcomes associated with catecholamine use in patients diagnosed with Takotsubo cardiomyopathy. BMC Cardiovasc Disord. 2018;18(1) doi: 10.1186/s12872-018-0784-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Madias J.E. Cardioselective ultra-short-acting β-blockers for patients with Takotsubo syndrome?: Letters to the Editor. Geriatr. Gerontol. Int. 2018;18(5):816–817. doi: 10.1111/ggi.13282. [DOI] [PubMed] [Google Scholar]
- 234.Kummer M., El-Battrawy I., Gietzen T., Ansari U., Behnes M., Lang S., Zhou X., Borggrefe M., Akin I. The Use of Beta Blockers in Takotsubo Syndrome as Compared to Acute Coronary Syndrome. Front. Pharmacol. 2020;11 doi: 10.3389/fphar.2020.00681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Taguchi M., Sasa T., Izuhara M., Shioji K., Iwamuro A., Uegaito T., Matsuda M. Ventricular Fibrillation Induced by Takotsubo Syndrome with Congenital Long QT Syndrome. Intern. Med. 2020;59(6):789–792. doi: 10.2169/internalmedicine.3484-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Mizutani K., Shioya A., Hirose Y., Saito R., Yamada S. Serious takotsubo cardiomyopathy: an autopsy case presenting severe irreversible myocardial damage after frequent episodes of recurrence. Diagn. Pathol. 2020;15(1) doi: 10.1186/s13000-020-01006-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Wakatsuki D., Asano T., Mase H., Kurata M., Suzuki H. A case of takotsubo cardiomyopathy developing ventricular fibrillation after a pacemaker implantation. J. Cardiol. Cases. 2020;21(4):149–152. doi: 10.1016/j.jccase.2019.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Ishida T., Uchida H., Miyazaki K., Yukawa T., Sugiyama K., Hamabe Y., Mimura M., Suzuki T. A Possible Role of Takotsubo Cardiomyopathy in Ventricular Fibrillation During Delirium Tremens: A Case Report and Literature Review. Psychosomatics. 2018;59(3):293–297. doi: 10.1016/j.psym.2017.11.008. [DOI] [PubMed] [Google Scholar]
- 239.O’Brien J., Mahony S., Byrne R.J., Byrne R.A., Holy E., Borovac J.A., Forouzandeh F., Tardo D., Thomson R. Dynamic left ventricular outflow tract gradient resulting from Takotsubo cardiomyopathy ameliorated by intra-aortic balloon pump counterpulsation: a case report. Eur. Heart J. - Case Reports. 2021;5(3) doi: 10.1093/ehjcr/ytab082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Iuliano G., Napoletano R., Vecchione C., Citro R., Aboumarie H.S., Baghdasaryan L., Panoulas V., Kurdi H., Ahmed N. A case report of takotsubo syndrome complicated by ischaemic stroke: the clinical dilemma of anticoagulation. Eur. Heart J. - Case Reports. 2021;5(3) doi: 10.1093/ehjcr/ytab051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Sattar Y., Connerney M., Ullah W., Philippou A., Slack D., McCarthy B., Kroll S., Luddington S., Ruiz Maya T., Alraies M.C. COVID-19 Presenting as Takotsubo Cardiomyopathy Complicated with Atrial Fibrillation. IJC Heart Vasculature. 2020;29:100580. doi: 10.1016/j.ijcha.2020.100580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Attisano T., Silverio A., Prota C., Briguori C., Galasso G., Citro R. Impella in Takotsubo syndrome complicated by left ventricular outflow tract obstruction and severe mitral regurgitation. ESC Heart Failure. 2020;7(1):307–311. doi: 10.1002/ehf2.12546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Herath H.M.M.T.B., Pahalagamage S.P., Lindsay L.C., Vinothan S., Withanawasam S., Senarathne V., Withana M. Takotsubo cardiomyopathy complicated with apical thrombus formation on first day of the illness: a case report and literature review. BMC Cardiovasc Disord. 2017;17(1) doi: 10.1186/s12872-017-0616-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Pongbangli N., Jae-aue S., Wongcharoen W., et al. Takotsubo Cardiomyopathy Complicated with Left Ventricular Thrombus in Myasthenic Crisis: A Case Report. Am J Case Rep. 2019;20:743–747. doi: 10.12659/AJCR.915415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Nonaka D., Takase H., Machii M., Ohno K. Intraventricular thrombus and severe mitral regurgitation in the acute phase of takotsubo cardiomyopathy: two case reports. J. Med. Case Reports. 2019;13(1) doi: 10.1186/s13256-019-2081-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Y-Hassan S., Holmin S., Abdula G., Böhm F. Thrombo-embolic complications in takotsubo syndrome: Review and demonstration of an illustrative case. Clin. Cardiol. 2019;42(2):312–319. doi: 10.1002/clc.23137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Luu L.A., Rawashdeh B., Goldaracena N., Agarwal A., McCracken E.K., Sahli Z.T., Oberholzer J., Pelletier S.J. Hepatic Artery Thrombosis and Takotsubo Syndrome After Liver Transplantation – Which Came First? Am. J. Case Rep. 2020;21 doi: 10.12659/AJCR.920263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Joki T., Nikus K., Laukkanen J., Papageorgiou N., D'Amario D., Abdelhamid M., Aziz A., Patel P.A. The electrocardiographic ‘triangular QRS-ST-T waveform’ pattern: a marker of severe haemodynamic compromise in Takotsubo syndrome—a case report. Eur. Heart J. - Case Rep. 2020;4(3):1–6. doi: 10.1093/ehjcr/ytaa076. [DOI] [PMC free article] [PubMed] [Google Scholar]