Abstract
Probiotics are considered the preferred alternatives to antibiotics for growth promotion and disease prevention. Previous studies have confirmed that Diutina rugosa SD-17 has the potential as a probiotic. We evaluated the probiotic effect of D. rugosa SD-17 on 360 one-day-old Hy-line brown chickens that were divided into 2 groups, and each group contained 6 replicate pens with 30 birds per pen. The chickens were fed with basal diet supplemented with or without D. rugosa SD-17, and the effects of D. rugosa SD-17 on growth performance, intestine morphology, and immune status were assessed. Body weight was significantly improved from week 3 to 6 (P < 0.05), and the feed conversion ratio was significantly improved in weeks 1 and 2 (P < 0.001). The length of the duodenum was lengthened significantly in week 3 (P < 0.05), and supplementation of D. rugosa SD-17 significantly increased villus height and villus height to crypt depth ratio in the ileum in week 3 (P < 0.05). Expressions of tight-junction-related genes of zonula occludens-2 and occludin in the ileum were significantly increased (P < 0.05). The proliferation capacity of blood lymphocytes stimulated by concanavalin A was significantly enhanced (P < 0.05), and the proportion of helper T (Th) cells increased significantly (P < 0.05). Expressions of Th1 cell markers IL-2 and interferon (IFN)-γ and immune-related genes of IL-1β, transforming growth factor-β, and IFN-γ in ileum were significantly increased (P < 0.05). These results indicated that D. rugosa SD-17 improved the growth and regulated immunity of chickens, and could be optimized for use as a feed additive for livestock and poultry.
key words: Diutina rugosa SD-17, growth performance, intestine morphology, immunity
INTRODUCTION
In recent years, the safety of animal-derived food has been questioned due to the abuse of antibiotics (Yeping et al., 2014). To eliminate safety hazards at the source, some feed additives, such as antibiotics and hormones, which seriously threaten food safety, have been banned from animal feed (Castanon, 2007; Millet and Maertens, 2011; Mohsina et al., 2015). Since antibiotics and hormones can prevent disease and promote the growth of livestock and poultry (Dibner and Richards, 2005), prohibition of their use will inevitably lead to economic losses in animal husbandry. It is an urgent problem to find feed additives that are harmless to livestock and poultry and can resist disease and promote growth, instead of antibiotics and hormones (Seal et al., 2013). Studies have shown that probiotics are good substitutes for antibiotics or hormones (Reid and Friendship, 2002; Kritas and Morrison, 2005).
Probiotics are defined as live microorganisms that confer a health benefit on the host when administered in adequate amounts (FAO/WHO, 2006). It is worth noting that probiotic effects are strain specific (Araya et al., 2002). Ramos et al. (2013) found that a total of 234 Lactobacillus isolates from Brazilian food products were strain specific and 3 isolates exhibited potential probiotic properties. Our previous study also reached a similar conclusion. Diutina rugosa SD-17 isolated from chicken feces had significant probiotic performance in vitro, while the type strain D. rugosa ATCC10571 had no potential as a probiotic (Wang et al., 2019).
Diutina rugosa is a hemiascus, asporogenic, and nonpathogenic yeast. Although it is found extensively in the environment, it is mainly used for the industrial production of lipases (Benjamin and Pandey, 1998; Hasan et al., 2006). So far, there are no reports on the use of D. rugosa for livestock production. Our previous studies have shown that D. rugosa SD-17 has strong adaptability in the simulated gastrointestinal environment in vitro and can be temporarily retained in the intestine (Wang et al., 2019), but these results only indicated that D. rugosa SD-17 has potential as a probiotic. In the present study, we determined the effects ofD. rugosa SD-17 on growth performance, intestinal morphology, and the immune system of chickens to demonstrate its probiotic effects and clarify its probiotic mechanisms.
MATERIALS AND METHODS
Animal Ethics Statement
All animal experimental protocols were approved by the Shandong Agricultural University Animal Care and Use Committee (SDAUA-2017–38).
Experimental Design and Animal Management
A total of 360 one-day-old Hy-Line Brown chickens were purchased from Dongyue Breeding Poultry Co. Ltd. (Shandong, China). The chickens were randomly divided into 2 experimental groups: group 1, control diet; and group 2, D. rugosa SD-17-supplemented diet. Each group contained 6 replicate pens with 30 birds per pen, and animals were fed a balanced, unmedicated corn and soybean meal-based mash diet that contained either 0 (control) or 1 × 107 CFU/g D. rugosa SD-17. Diutina rugosa SD-17 used in the experiments was provided by our laboratory. The composition of the basal diet and nutrient levels are presented in Table 1. The room temperature was maintained at 33°C during the first 5 D and then gradually decreased by 3°C each week until it reached 24°C. Chickens had free access to feed and water, and were housed in wire cages, received continuous light for the first 24 h, and were then maintained under 23 L: 1 D for the remainder of the study.
Table 1.
Ingredients and nutrient composition of diets.
| Ingredient (%) | Energy and nutrient content | ||
|---|---|---|---|
| Corn | 61.7 | Metabolizable energy (Kcal/kg) | 3,236 |
| Wheat bran | 4.5 | Crude protein (%) | 16.96 |
| Bean pulp | 24 | Crude fiber (%) | 3.12 |
| Fish meal | 2 | Methionine (%) | 0.49 |
| Rapeseed meal | 5 | Lysine (%) | 0.88 |
| Calcium phosphate | 1.3 | ||
| Limestone | 1.2 | ||
| Salt | 0.3 | ||
Growth Performance
Chickens and feed intake were group weighed by cage at 1, 2, 3, 4, 5, and 6 wk of age. ADG, ADFI, and feed conversion ratio (FCR) were calculated for each period and for the overall experiment. These performance parameters were corrected according to mortality.
Intestinal Morphology
At 2, 3, and 4 wk, 6 birds from each replicate pen were randomly selected and killed. The gastrointestinal tract was removed and the small intestine was divided into 3 parts: duodenum (from the gizzard outlet to the end of the pancreatic loop); jejunum (from the pancreatic loop to Meckel's diverticulum); and ileum (from Meckel's diverticulum to the ileo-ceco-colic junction), and the length of each section was measured. At 3 wk, 1-cm-long segments were taken from the center of each part and fixed in 10% buffered formalin. Tissues were serial dehydrated by transferring through alcohols with increasing concentrations and embedded in paraffin. Tissue sections were cut by a microtome and stained with hematoxylin and eosin. Images were obtained using a microscope, and histomorphometric measurement was performed by using Photoshop software. A total of 10 well-oriented, intact villi and crypts were randomly selected in duplicate from each tissue sample and the average of 20 values obtained for each chicken was taken.
Immune Organ Index
Six birds from each replicate pen were randomly selected and killed by cervical dislocation at 2, 3, and 4 wk. The bursa of Fabricius, thymus, and spleen were dissected out, surface moisture was removed with a filter paper, and pathological changes to the organ surface were recorded. Finally, the organs were weighed and the immune organ index was calculated.
Blood Lymphocyte Proliferation Assay and Subpopulations
At 3 wk, 6 birds from each group were randomly selected, weighed, and wing venous blood was collected in a 1-mL injection syringe containing 4% sodium citrate. Peripheral blood lymphocytes (PBLs) were isolated using the lymphocyte separation medium (Solarbio, Beijing, China) (Fair et al., 2008). The PBLs were seeded into 96-well microtiter plates (Costar, Cambridge, MA) at 105 cells per well in sextuplicate, with or without concanavalin A (Con A) (0.5 mg/mL; Sigma-Aldrich, St. Louis, MO). The plates were incubated in 5% CO2 at 37°C for 66 h. Cell Counting Kit-8 reagent (Solarbio) was added to each well, followed by incubation for 2 h at 37°C, and optical density at 450 nm (OD450) was measured using an automated microplate reader (Biotek Instruments, Winooski, VT). The results of the lymphocyte proliferation assay were expressed as stimulation indices, which were presented as the ratio of absorbance of stimulated cells to that of unstimulated cells from the same chicken. To measure the percentage of CD4+ and CD8+ cells, the isolated PBLs were incubated with mouse anti-chicken CD3-PE/Cy5 (Southern Biotech, Birmingham, AL) and mouse anti-chicken CD8a- FITC (Southern Biotech) or mouse anti-chicken CD4-FITC (Southern Biotech) at 4°C for 20 min and analyzed using flow cytometry.
Detection of Cytokines
At 3 wk, 2-cm-long segments were taken from the center of the ileum and quickly transferred to a mortar precooled with liquid nitrogen, and ground to powder with a pestle. The sample homogenate amount of RNAiso Plus (Takara, Dalian, China) was added to the mortar for RNA extraction. Blood lymphocytes were directly treated with RNAiso Plus for RNA extraction. cDNA synthesis was conducted using a PrimeScript RT Reagent Kit with gDNA Eraser (Takara). Quantitative real-time polymerase chain reaction (qPCR) was performed using an Applied Biosystems 7500 Real-Time PCR System (Invitrogen Life Technologies, Carlsbad, CA) using TB Green Premix Ex Taq (Takara) with appropriate primers (Supplementary data). Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was used as an endogenous control for data normalization. Based on expression of target genes normalized to GAPDH levels, relative ΔΔ Ct values were calculated and the results presented as fold change compared to controls.
Statistical Analysis
The data were evaluated by unpaired t -tests using Graph Pad Prism version 3.00. The data are expressed as the mean ± standard error.
RESULTS
Growth Performance
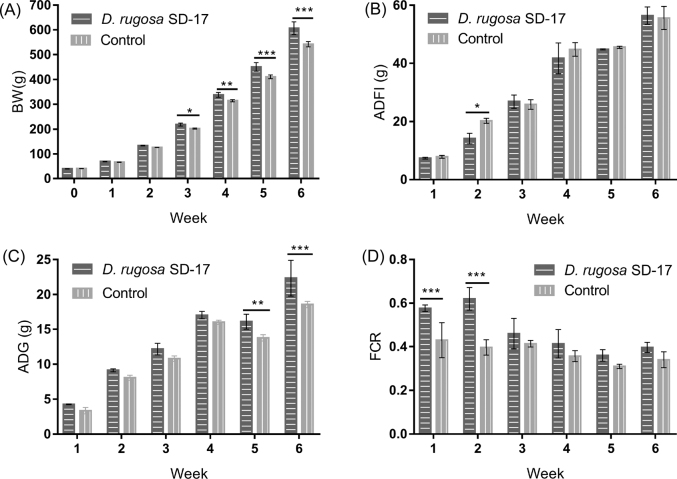
None of the chickens in the D. rugosa SD-17 group died or showed obvious pathological changes. Two and one chicken died in the control group on days 6 and 7, respectively, although no obvious pathological changes were seen macroscopically appearance or through pathological examination. Birds fed D. rugosa SD-17 diets had significantly greater body weight than those in the control group at weeks 3 (P < 0.05), 4 (P < 0.01), 5 (P < 0.001), and 6 (P < 0.001) (Figure 1 A). ADFI decreased significantly at week 2 (P < 0.05; Figure 1 B). In addition, ADG increased significantly at weeks 5 and 6 (P < 0.01 and P < 0.001; Figure 1 C). FCR was significantly improved at weeks 1 and 2 (P < 0.001; Figure 1 D).
Figure 1.
Effects of Diutina rugosa SD-17 on growth performance in chickens. Effects of D. rugosa SD-17 on (A) BW; (B) ADFI; (C) ADG; and (D) feed conversion ratio (FCR). Control = birds fed a basal diet; D. rugosa SD-17 = birds fed a basal diet supplemented with 1 × 107 cfu/kg D. rugosa SD-17. Each mean represents 10 replicates.*P < 0.05; **P < 0.01; ***P < 0.001.
Intestinal Morphology
Intestinal Development
By visual and histopathological observation, no bleeding, injury, and other lesions were found in the intestinal tract of the chickens in the 2 groups. The duodenal lengths of the D. rugosa SD-17 group were significantly longer than that of the control group at 3 and 4 wk (P < 0.05, Table 2). There was no significant difference in the length of jejunum and ileum between the groups at 2, 3, and 4 wk (P > 0.05). The D. rugosa SD-17 group had normal intestinal structure; the highest villi were in the duodenum followed by lower villi in the jejunum, and the lowest being in the ileum (Table 3). The intestinal villi were slim and finger-shaped and the intestinal mucosa revealed no histopathological changes in chickens from both groups. At 3 wk, D. rugosa SD-17 significantly increased villus height and villus height to crypt depth ratio in the ileum (P < 0.05). However, crypt depth was not affected by dietary supplementation of D. rugosa SD-17 (P > 0.05).
Table 2.
Change in intestinal length with or without D. rugosa SD-17 supplementation.1
| Intestine | Age | Control | D. rugosa SD-17 | P-value |
|---|---|---|---|---|
| Duodenum | 2 | 14.5 ± 0.58 | 16 ± 1.10 | 0.313 |
| 3 | 14.0 ± 0.63 | 16.78 ± 0.97 | 0.023 | |
| 4 | 16.67 ± 0.82 | 19.44 ± 1.13 | 0.023 | |
| Jejunum | 2 | 31.75 ± 1.71 | 29.17 ± 2.79 | 0.084 |
| 3 | 38.33 ± 3.62 | 39.44 ± 3.36 | 0.359 | |
| 4 | 38.67 ± 1.97 | 40.89 ± 3.41 | 0.069 | |
| Ileum | 2 | 21.5 ± 3.00 | 23.00 ± 2.53 | 0.313 |
| 3 | 27.00 ± 1.58 | 28.78 ± 1.99 | 0.167 | |
| 4 | 32.83 ± 3.06 | 32.89 ± 2.15 | 0.963 |
Results are reported as the means ± SD.
Each mean represents the data of 6 birds.
Table 3.
Effects of level of supplementation of D. rugosa SD-17 on small intestinal morphology in chickens.
| Control | D. rugosa SD-17 | P-value | |
|---|---|---|---|
| Duodenum | |||
| VH1 (μm) | 1262.2 ± 77.74 | 1294.1 ± 15.86 | 0.245 |
| CD2 (μm) | 318.2 ± 11.85 | 306.3 ± 21.02 | 0.661 |
| VH/CD ratio | 3.97 ± 0.15 | 4.23 ± 0.24 | 0.129 |
| Jejunum | |||
| VH (μm) | 828.3 ± 28.52 | 845.7 ± 32.11 | 0.520 |
| CD (μm) | 119.2 ± 8.49 | 123.83 ± 6.17 | 0.865 |
| VH/CD ratio | 6.95 ± 0.25 | 6.83 ± 0.09 | 0.472 |
| Ileum | |||
| VH (μm) | 409.6 ± 29.34 | 477.0 ± 50.72 | 0.019 |
| CD (μm) | 103.2 ± 7.76 | 103.0 ± 17.39 | 0.993 |
| VH/CD ratio | 3.97 ± 0.04a | 4.66 ± 0.30b | 0.001 |
Results are reported as the means ± SD.
Villus height.
Crypt depth.
Expression of Tight-Junction-Related Genes
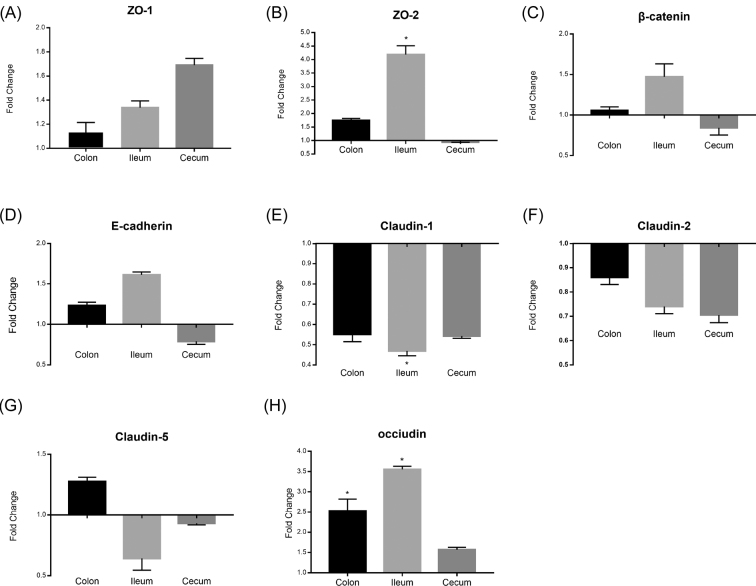
We detected changes in the mRNA expression of tight-junction-related genes in the duodenum, ileum, and cecum. Expression of zonula occludens (ZO)-2 and occludin was significantly upregulated by 4.19-fold (P < 0.05, Figure 2 B) and 3.55-fold (P < 0.05, Figure 2 H), respectively, in the ileum. Expression of claudin-1 was significantly reduced by 2.13-fold (P < 0.05, Figure 2 E). Expression of occludin in the duodenum was significantly upregulated by 2.53-fold (P < 0.05, Figure 2 H). Expressions of the other of genes of ZO-1, β-catenin, E-cadherin, claudin-1, and claudin-5 were not significantly changed (P > 0.05, Figure 2 A, C, D, F, and G).
Figure 2.
Expression of tight-junction-related genes in the colon, ileum, and cecum of chickens. (A) Zonula occludens (ZO)-1, (B) ZO-2, (C) β-catenin, (D) E-cadherin, (E) claudin-1, (F) claudin-3, (G) claudin-5, and (H) occludin. The fold change represents gene expression in diet with D. rugosa SD-17 compared to that of the controls. Bars represent the mean ± SD of 3 independent experiments, *P < 0.05.
Changes in the Immune System
Immune Organ Index
The immune organ indices of the thymus, spleen, and bursa of Fabricius of the D. rugosa SD-17 group at weeks 2, 3, and 4 showed no significant difference compared with those of the control group.
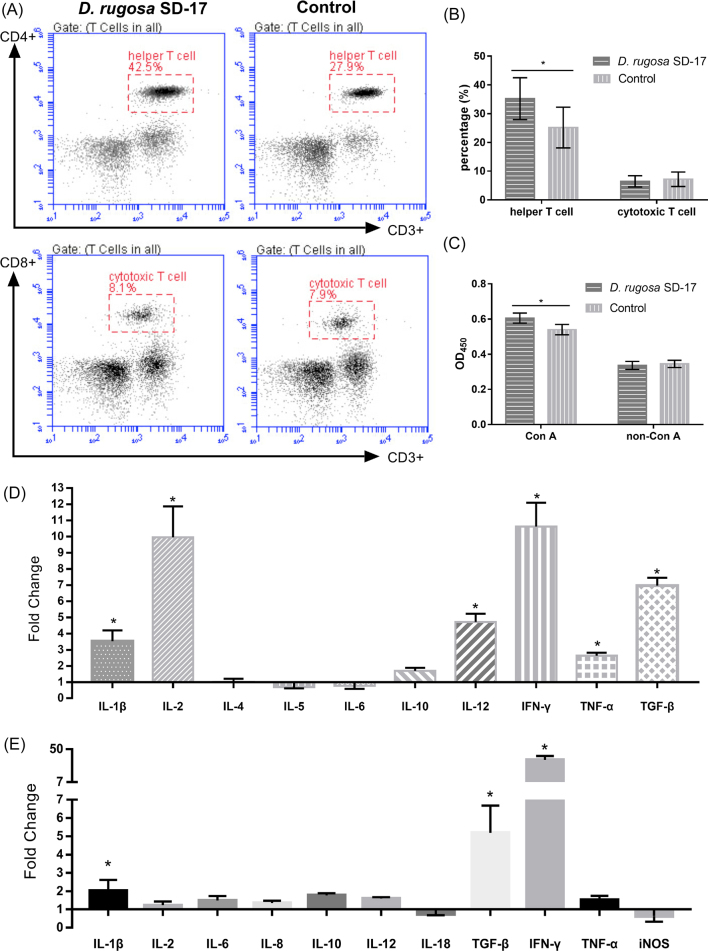
Subpopulations and Proliferation of Blood Lymphocytes
The percentage of CD3+ CD4+ Th cells in the D. rugosa SD-17 group was significantly higher than in the control group (P < 0.05), but there was no significant change in CD3+ CD8+ cytotoxic T cells (P > 0.05; Figure 3 A and B). Lymphocyte proliferation in response to ConA is shown in Figure 3 C. The D. rugosa SD-17 group displayed significantly higher lymphocyte proliferation in response to ConA than that of the control group (P < 0.05).
Figure 3.
(A) T-lymphocyte sorting through fluorescence activated cell sorting (FACS). Each dot in the plot indicates a single cell. (B) The percentages of CD4+ and CD8+ cells in the blood. (C) Blood lymphocyte proliferation responses to ConA. (D) Expression of immune-related genes in blood lymphocytes of chickens. (E) Expression of immune-related genes in ileum of chickens. Con A, concanavalin A; IFN-γ, interferon-γ; TNF-α, tumor necrosis factor-α; TGF-β, transforming growth factor-β; iNOS, inducible nitric oxide synthase. Each bar represents the mean ± SD (n = 3) and each bird sample was analyzed in triplicate. *P < 0.05.
Expression of Cytokines in T-Lymphocytes
Changes in the mRNA expressions of cytokines in T lymphocytes are shown in Figure 3 D. The expressions of Th1 cell markers IL-2 and interferon (IFN)-γ were significantly upregulated by 9.96- and 10.62- fold (P < 0.05), respectively, while expressions of the Th2 cell markers IL-4 and IL-5 were not significantly changed. Expressions of IL-1β, IL-12, tumor necrosis factor (TNF)-α, and transforming growth factor (TGF)-β were upregulated by 3.52-, 4.72-, 2.64-, and 6.98-fold, respectively (P < 0.05), but expressions of IL-6 and IL-10 were not obviously changed.
Expression of Immune-Related Genes in the Ileum
The expression of immune-related genes in the ileum was detected. Expressions of IL-1β, TGF-β, and IFN-γ were significantly upregulated by 2.02-, 5.19-, and 36.11-fold, respectively (P < 0.05), but expressions of IL-2, IL-6, IL-8, IL-10, IL-12, IL-18, TNF-α, and inducible nitric oxide synthase were not significantly changed (Figure 3 E).
DISCUSSION
Evidence has been presented that probiotics promote the growth of poultry, but the exact mechanism through which this occurs is considered to be complex (Bai et al., 2017; Forte et al., 2018), and could include the production of nutrients, stimulation of intestinal development, and/or fermentation of the feed. In this study, the basal diet supplemented with D. rugosa SD-17 significantly increased BW and FCR, and significantly decreased ADFI, which may be related to D. rugosa lipase. Diutina rugosa is a strong lipase producer (Tan et al., 2003), and D. rugosa lipase has excellent traits, such as stability at high temperatures and activity at a broad range of pH values (Treichel et al., 2010; Geoffry and Achur, 2018). Therefore, D. rugosa SD-17 can break down lipids to produce fatty acids in poor gastrointestinal environments. Short-chain fatty acids can regulate intestinal mucosal homeostasis and modulate neuronal excitability (Soret et al., 2010; Ríos-Covián et al., 2016), thereby improving gastrointestinal motility and promoting digestion and absorption of feed. Previous studies have shown that β-glucan is an immunomodulator that can be extracted from the cell walls of yeast, which can be directly absorbed and utilized by the gut and can significantly improve growth performance and enhance the innate immune system (Rouhier et al., 1995; Tian et al., 2016). In our previous study, we found that the content of glucan in D. rugosa SD-17 was higher than that of another type strain, which may be an important reason for the growth promotion effect of D. rugosa SD-17 in chickens (Chae et al., 2006).
Improving the intestinal morphology is another way by which probiotics play a probiotic role, and the height of the villi in the small intestine is strongly associated with their intestinal absorption (Yamauchi, 2002). Many studies have shown that probiotics can promote normal development of the intestinal villi, including Bacillus subtilis (Sen et al., 2012), Lactobacillus (Awad et al., 2009), and Enterococcus faecalis (Cao et al., 2013). Similarly, D. rugosa SD-17 increased the height of ileal villi in the present study. Crypt depth is associated with infection, which represents the ability of intestinal epithelial cells to renew and repair themselves in the event of infection. Cao et al. (2013) have reported that Escherichia coli K88 increased jejunal crypt depth by infecting broiler chickens, and Enterococcus faecium reduced infection and jejunal crypt depth. It has been reported that probiotics have no significant effect on the depth of the crypt under healthy conditions (Awad et al., 2009). Likewise, in our study D. rugosa SD-17 had no effect on the crypt depth of duodenum, jejunum, and ileum. This suggested that D. rugosa SD-17 did not invade the intestinal epithelial cells and cause intestinal infection. In addition, D. rugosa SD-17 promoted duodenal development and the length of the duodenum increased significantly, which was conducive to improving digestion and absorption. Tight junctions are an important part of the epithelial barrier, and probiotics have been shown to promote intestinal barrier integrity in vitro and in vivo (Yu et al., 2012; Wang et al., 2018). Tight junctions are complex protein structures composed of transmembrane proteins (Ma et al., 2018). Treatment of epithelial cells with E. coli Nissle 1917 leads to increased expression of ZO-2 tight junction protein and redistribution of ZO-2 from the cytosol to cell boundaries (Ukena et al., 2007; Zyrek et al., 2007). In addition, Ewaschuk et al. (2008) and Anderson et al. (2010) found that treatment of epithelial cells with the probiotic product VSL#3 increased transcription of occludin and ZO-1 gene expression while reducing claudin gene expression. A similar effect was observed in our study; supplementation of D. rugosa SD-17 increased transcription of ZO-2 and occludin and decreased transcription of claudin-1, suggesting that D. rugosa SD-17 altered the expression of tight junction proteins to regulate intestinal barrier function.
T lymphocytes and their functions are important components of the immune system (Burnette and Weichselbaum, 2013; Yahfoufi et al., 2018). Previous studies have shown that probiotics promote proliferation of lymphocytes (Kirjavainen et al., 1999; Bujalance et al., 2007). Our study confirmed this. D. rugosa SD-17 promoted the proliferation of T lymphocytes, which indicated that it stimulated nonspecific immunity. Th cells and cytotoxic T cells are the main types of blood T lymphocytes, and their proportion directly reflects the level of specific immunity (Zhu et al., 2010; Kaech and Cui, 2012). Studies have confirmed that Th cells play central roles in the function of the immune system by orchestrating immune responses against a wide variety of pathogenic microorganisms (Biedermann et al., 2004; Zhou et al., 2008; Sant et al., 2018). In our study, D. rugosa SD-17 increased the proportion of Th cells but had no effect on cytotoxic T cells. This showed that D. rugosa SD-17 could help improve resistance to external microorganisms. Th1 cells represent one of the different subsets of the heterogeneous Th CD4+ population, and these cells are characterized by the production of IL-2, IFN-γ, and lymphotoxin as signature cytokines (Annunziato and Romagnani, 2016), whereas these lymphokines are not detectably expressed in Th2 clones. Conversely, only Th2 clones synthesize detectable amounts of IL-4 and IL-5 (Mosmann and Coffman, 1989). It has been shown that probiotics stimulate the secretion of cytokines by Th1 cells (Ghadimi et al., 2008). Similar conclusions were reached in the present study. The expressions of IL-2 and IFN-γ at the transcript levels were significantly increased but expression of IL-4 was not significantly affected. These results indicated that D. rugosa SD-17 changed the direction of lymphocyte differentiation toward Th1 cells. It has been shown that probiotics stimulate immune cells to release proinflammatory cytokines, including IL-1β, TNF-α, and IFN-γ (Tsai et al., 2010). The expressions of IL-1β and IFN-γ were significantly increased in this study. In addition, the expression of TGF-β was significantly increased, which suggests that TGF-β is a regulator of cytokines and plays an important role in regulating immunity (Wahl, 2007; Kubiczkova et al., 2012).
In conclusion, supplementation with D. rugosa SD-17 improved growth performance, intestinal morphology, and immunity in chickens. Because this study was conducted on healthy chickens, whether D. rugosa SD-17 would also show beneficial effects on sick chickens is worthy of further study.
ACKNOWLEDGMENTS
This work was supported by grants from National Key Research and Development Program of China (Grant No. 2017YFD0500400), National Natural Science Foundation of China (No. 31172314) and Funds of Shandong “Double Tops” Program (SYL2017YSTD11).
Footnotes
Supplementary data are available at Poultry Science online.
Table S1. Gene-specific sequences primers used in real-time quantitative PCR.
Contributor Information
F. Wang, Email: wangfangkun1980@163.com.
X. Zhao, Email: xmzhao66@163.com.
Supplementary Material
REFERENCES
- Anderson R.C., Cookson A.L., McNabb W.C., Park Z., McCann M.J., Kelly W.J., Roy N.C. Lactobacillus plantarum MB452 enhances the function of the intestinal barrier by increasing the expression levels of genes involved in tight junction formation. BMC Microbiol. 2010;10:316. doi: 10.1186/1471-2180-10-316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annunziato F., Romagnani S. Encyclopedia of Immunobiology. Elsevier; Irvine, CA: 2016. Th1 cells; pp. 287–293. [Google Scholar]
- Araya M., Morelli L., Reid G., Sanders M.E., Stanton C., Pineiro M., Ben Embarek P. Guidelines for the evaluation of probiotics in food. Joint FAO/WHO Working. Group Report on Drafting Guidelines for the Evaluation of Probiotics in Food, London, Ontario, Canada. 2002;1:1–11. [Google Scholar]
- Awad WA, Ghareeb K., Abdel-Raheem S., Bohm J. Effects of dietary inclusion of probiotic and synbiotic on growth performance, organ weights, and intestinal histomorphology of broiler chickens. Poult. Sci. 2009;88:49–56. doi: 10.3382/ps.2008-00244. [DOI] [PubMed] [Google Scholar]
- Bai K., Huang Q., Zhang J., He J., Zhang L., Wang T. Supplemental effects of probiotic Bacillus subtilis fmbJ on growth performance, antioxidant capacity, and meat quality of broiler chickens. Poult. Sci. 2017;96:74–82. doi: 10.3382/ps/pew246. [DOI] [PubMed] [Google Scholar]
- Benjamin S., Pandey A. Candida rugosa lipases: molecular biology and versatility in biotechnology. Yeast. 1998;14:1069–1087. doi: 10.1002/(SICI)1097-0061(19980915)14:12<1069::AID-YEA303>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- Biedermann T., Röcken M., Carballido J.M. TH1 and TH2 lymphocyte development and regulation of TH cell–mediated immune responses of the skin. J. Investig. Dermatol. Symp. Proc. 2004;9:5–14. doi: 10.1111/j.1087-0024.2004.00829.x. [DOI] [PubMed] [Google Scholar]
- Bujalance C., Moreno E., Jimenez-Valera M., Ruiz-Bravo A. A probiotic strain of Lactobacillus plantarum stimulates lymphocyte responses in immunologically intact and immunocompromised mice. Int. J. Food Microbiol. 2007;113:28–34. doi: 10.1016/j.ijfoodmicro.2006.07.014. [DOI] [PubMed] [Google Scholar]
- Burnette B., Weichselbaum R.R. Radiation as an immune modulator. Semin. Radiat. Oncol. 2013;23:273–280. doi: 10.1016/j.semradonc.2013.05.009. [DOI] [PubMed] [Google Scholar]
- Cao G.T., Zeng X.F., Chen A.G., Zhou L., Zhang L., Xiao Y.P., Yang C.M. Effects of a probiotic, Enterococcus faecium, on growth performance, intestinal morphology, immune response, and cecal microflora in broiler chickens challenged with Escherichia coli K88. Poult. Sci. 2013;92:2949–2955. doi: 10.3382/ps.2013-03366. [DOI] [PubMed] [Google Scholar]
- Castanon J.I.R. History of the use of antibiotic as growth promoters in European poultry feeds. Poult. Sci. 2007;86:2466–2471. doi: 10.3382/ps.2007-00249. [DOI] [PubMed] [Google Scholar]
- Chae B.J., Lohakare J.D., Moon W.K., Lee S.L., Park Y.H., Hahn T.W. Effects of supplementation of β-glucan on the growth performance and immunity in broilers. Res. Vet. Sci. 2006;80:291–298. doi: 10.1016/j.rvsc.2005.07.008. [DOI] [PubMed] [Google Scholar]
- Dibner J.J., Richards J.D. Antibiotic growth promoters in agriculture: history and mode of action. Poult. Sci. 2005;84:634–643. doi: 10.1093/ps/84.4.634. [DOI] [PubMed] [Google Scholar]
- Ewaschuk J.B., Diaz H., Meddings L., Diederichs B., Dmytrash A., Backer J., Looijer-van Langen M., Madsen K.L. Secreted bioactive factors from Bifidobacterium infantis enhance epithelial cell barrier function. Am. J. Physiol. Liver Physiol. 2008;295:G1025–G1034. doi: 10.1152/ajpgi.90227.2008. [DOI] [PubMed] [Google Scholar]
- Fair J.M., Taylor-McCabe K.J., Shou Y., Marrone B.L. Immunophenotyping of chicken peripheral blood lymphocyte subpopulations: Individual variability and repeatability. Vet. Immunol. Immunop. 2008;125:268–273. doi: 10.1016/j.vetimm.2008.05.012. [DOI] [PubMed] [Google Scholar]
- FAO/WHO . Food and Agriculture Organization of the United Nations–World Health Organization; Rome, Italy: 2006. Probiotics in food health and nutritional properties and guidelines for evaluation. (FAO/WHO working group report) [Google Scholar]
- Forte C., Manuali E., Abbate Y., Papa P., Vieceli L., Tentellini M., Trabalza-Marinucci M., Moscati L. Dietary Lactobacillus acidophilus positively influences growth performance, gut morphology, and gut microbiology in rurally reared chickens. Poult. Sci. 2018;97:930–936. doi: 10.3382/ps/pex396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geoffry K., Achur R.N. Screening and production of lipase from fungal organisms. Biocatal. Agric. Biotechnol. 2018;14:241–253. [Google Scholar]
- Ghadimi D., Fölster-Holst R., de Vrese M., Winkler P., Heller K.J., Schrezenmeir J. Effects of probiotic bacteria and their genomic DNA on TH1/TH2-cytokine production by peripheral blood mononuclear cells (PBMCs) of healthy and allergic subjects. Immunobiology. 2008;213:677–692. doi: 10.1016/j.imbio.2008.02.001. [DOI] [PubMed] [Google Scholar]
- Hasan F., Shah A.A., Hameed A. Industrial applications of microbial lipases. Enzyme Microb. Technol. 2006;39:235–251. [Google Scholar]
- Kaech S.M., Cui W. Transcriptional control of effector and memory CD8+ T cell differentiation. Nat. Rev. Immunol. 2012;12:749–761. doi: 10.1038/nri3307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirjavainen P.V., El-Nezami H.S., Salminen S.J., Ahokas J.T., Wright P.F.A. The effect of orally administered viable probiotic and dairy lactobacilli on mouse lymphocyte proliferation. FEMS Immunol. Med. Microbiol. 1999;26:131–135. doi: 10.1111/j.1574-695X.1999.tb01380.x. [DOI] [PubMed] [Google Scholar]
- Kritas S.K., Morrison R.B. Evaluation of probiotics as a substitute for antibiotics in a large pig nursery. Vet. Rec. 2005;156:447–448. doi: 10.1136/vr.156.14.447. [DOI] [PubMed] [Google Scholar]
- Kubiczkova L., Sedlarikova L., Hajek R., Sevcikova S. TGF-β – an excellent servant but a bad master. J. Transl. Med. 2012;10:183. doi: 10.1186/1479-5876-10-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma T.Y., Nighot P., Al-Sadi R. Physiology of the Gastrointestinal Tract. 6th ed. Elsevier; Irvine, CA: 2018. Tight junctions and the intestinal barrier; pp. 587–639. [Google Scholar]
- Millet S., Maertens L. The European ban on antibiotic growth promoters in animal feed: from challenges to opportunities. Vet. J. 2011;187:143–144. doi: 10.1016/j.tvjl.2010.05.001. [DOI] [PubMed] [Google Scholar]
- Mohsina Z., Yang S., Tarique T.M., Qiu J. Use of banned veterinary drugs in feed: food safety challenges and strategies in China: a review. Eur. Acad. Res. 2015;3:2871–2892. [Google Scholar]
- Mosmann T., Coffman R. ThI and Th2 cells: different patterns of lymphokine functional properties. Annu. Rev. Immunol. 1989;7:145–173. doi: 10.1146/annurev.iy.07.040189.001045. [DOI] [PubMed] [Google Scholar]
- Ramos C.L., Thorsen L., Schwan R.F., Jespersen L. Strain-specific probiotics properties of Lactobacillus fermentum, Lactobacillus plantarum and Lactobacillus brevis isolates from Brazilian food products. Food Microbiol. 2013;36:22–29. doi: 10.1016/j.fm.2013.03.010. [DOI] [PubMed] [Google Scholar]
- Reid G., Friendship R. Alternatives to antibiotic use: probiotics for the gut. Anim. Biotechnol. 2002;13:97–112. doi: 10.1081/ABIO-120005773. [DOI] [PubMed] [Google Scholar]
- Ríos-Covián D., Ruas-Madiedo P., Margolles A., Gueimonde M., de los Reyes-Gavilán C.G., Salazar N. Intestinal short chain fatty acids and their link with diet and human health. Front. Microbiol. 2016;7:1–9. doi: 10.3389/fmicb.2016.00185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rouhier P., Kopp M., Begot V., Bruneteau M., Fritig B. Structural features of fungal β-d-glucans for the efficient inhibition of the initiation of virus infection on Nicotiana tabacum. Phytochemistry. 1995;39:57–62. doi: 10.1016/0031-9422(94)00852-k. [DOI] [PubMed] [Google Scholar]
- Sant A.J., Richards K.A., Nayak J. Distinct and complementary roles of CD4 T cells in protective immunity to influenza virus. Curr. Opin. Immunol. 2018;53:13–21. doi: 10.1016/j.coi.2018.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seal B.S., Lillehoj H.S., Donovan D.M., Gay C.G. Alternatives to antibiotics: a symposium on the challenges and solutions for animal production. Anim. Health Res. Rev. 2013;14:78–87. doi: 10.1017/S1466252313000030. [DOI] [PubMed] [Google Scholar]
- Sen S., Ingale S.L., Kim Y.W., Kim J.S., Kim K.H., Lohakare J.D., Kim E.K., Kim H.S., Ryu M.H., Kwon I.K., Chae B.J. Effect of supplementation of Bacillus subtilis LS 1–2 to broiler diets on growth performance, nutrient retention, caecal microbiology and small intestinal morphology. Res. Vet. Sci. 2012;93:264–268. doi: 10.1016/j.rvsc.2011.05.021. [DOI] [PubMed] [Google Scholar]
- Soret R., Chevalier J., De Coppet P., Poupeau G., Derkinderen P., Segain J.P., Neunlist M. Short-chain fatty acids regulate the enteric neurons and control gastrointestinal motility in rats. Gastroenterology. 2010;138:1772–1782. doi: 10.1053/j.gastro.2010.01.053. [DOI] [PubMed] [Google Scholar]
- Tan T., Zhang M., Wang B., Ying C., Deng L. Screening of high lipase producing Candida sp. and production of lipase by fermentation. Process Biochem. 2003;39:459–465. [Google Scholar]
- Tian X., Shao Y., Wang Z., Guo Y. Effects of dietary yeast β-glucans supplementation on growth performance, gut morphology, intestinal Clostridium perfringens population and immune response of broiler chickens challenged with necrotic enteritis. Anim. Feed Sci. Technol. 2016;215:144–155. [Google Scholar]
- Treichel H., de Oliveira D., Mazutti M.A., Di Luccio M., Oliveira J.V. A review on microbial lipases production. Food Bioprocess Technol. 2010;3:182–196. [Google Scholar]
- Tsai Y.T., Cheng P.C., Liao J.W., Pan T.M. Effect of the administration of Lactobacillus paracasei subsp. paracasei NTU 101 on Peyer's patch-mediated mucosal immunity. Int. Immunopharmacol. 2010;10:791–798. doi: 10.1016/j.intimp.2010.04.012. [DOI] [PubMed] [Google Scholar]
- Ukena S.N., Singh A., Dringenberg U., Engelhardt R., Seidler U., Hansen W., Bleich A., Bruder D., Franzke A., Rogler G., Suerbaum S., Buer J., Gunzer F., Westendorf A.M. Probiotic Escherichia coli Nissle 1917 inhibits leaky gut by enhancing mucosal integrity. PLoS One. 2007;2 doi: 10.1371/journal.pone.0001308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahl S.M. Transforming growth factor-β: innately bipolar. Curr. Opin. Immunol. 2007;19:55–62. doi: 10.1016/j.coi.2006.11.008. [DOI] [PubMed] [Google Scholar]
- Wang G., Xu Q., Jin X., Hang F., Liu Z., Zhao J., Zhang H., Chen W. Effects of lactobacilli with different regulatory behaviours on tight junctions in mice with dextran sodium sulphate-induced colitis. J. Funct. Foods. 2018;47:107–115. [Google Scholar]
- Wang J.Z., Zhang H.Y., Du H.J., Wang F.K., Li H.M., Zhao X.M. Identification and characterization of Diutina rugosa SD-17 for potential use as a probiotic. LWT-Food Sci. Technol. 2019;109:283–288. [Google Scholar]
- Yahfoufi N., Mallet J.F., Graham E., Matar C. Role of probiotics and prebiotics in immunomodulation. Curr. Opin. Food Sci. 2018;20:82–91. [Google Scholar]
- Yamauchi K. Review on chicken intestinal villus histological alterations related with intestinal function. J. Poult. Sci. 2002;39:229–242. [Google Scholar]
- Yeping T., Changhua L., Yinong H. SHS Web of Conferences. Vol. 6. EDP Sciences; 2014. Challenges of animal derived food safety and counter-measures; p. 03008. [Google Scholar]
- Yu Q., Wang Z., Yang Q. Lactobacillus amylophilus D14 protects tight junction from enteropathogenic bacteria damage in Caco-2 cells. J. Dairy Sci. 2012;95:5580–5587. doi: 10.3168/jds.2012-5540. [DOI] [PubMed] [Google Scholar]
- Zhou M., Yang B., Ma R., Wu C. Memory Th-17 cells specific for C. albicans are persistent in human peripheral blood. Immunol. Lett. 2008;118:72–81. doi: 10.1016/j.imlet.2008.03.004. [DOI] [PubMed] [Google Scholar]
- Zhu J., Yamane H., Paul W. Differentiation of effector CD4 T cell populations. Annu Rev. Immunol. 2010;28:445–489. doi: 10.1146/annurev-immunol-030409-101212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zyrek A.A., Cichon C., Helms S., Enders C., Sonnenborn U., Schmidt M.A. Molecular mechanisms underlying the probiotic effects of Escherichia coli Nissle 1917 involve ZO-2 and PKCζ redistribution resulting in tight junction and epithelial barrier repair. Cell. Microbiol. 2007;9:804–816. doi: 10.1111/j.1462-5822.2006.00836.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.