Abstract
Real-life mobility, also called “enacted” mobility, characterizes an individual’s activity and participation in the community. Real-life mobility may be facilitated or hindered by a variety of factors, such as physical abilities, cognitive function, psychosocial aspects, and external environment characteristics. Advances in technology have allowed for objective quantification of real-life mobility using wearable sensors, specifically, accelerometry and global positioning systems (GPSs). In this review article, first, we summarize the common mobility measures extracted from accelerometry and GPS. Second, we summarize studies assessing the associations of facilitators and barriers influencing mobility of community-dwelling older adults with mobility measures from sensor technology. We found the most used accelerometry measures focus on the duration and intensity of activity in daily life. Gait quality measures, e.g., cadence, variability, and symmetry, are not usually included. GPS has been used to investigate mobility behavior, such as spatial and temporal measures of path traveled, location nodes traversed, and mode of transportation. Factors of note that facilitate/hinder community mobility were cognition and psychosocial influences. Fewer studies have included the influence of external environments, such as sidewalk quality, and socio-economic status in defining enacted mobility. Increasing our understanding of the facilitators and barriers to enacted mobility can inform wearable technology-enabled interventions targeted at delaying mobility-related disability and improving participation of older adults in the community.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40520-022-02096-x.
Keywords: Physical activity and participation, Spatial movement, Wearable technology
Introduction
Mobility is essential for completion of many instrumental activities of daily living and promotes physical function, social engagement, independent living, and quality of life [1]. By 2040, the United States is expected to have more than 81 million older adults, and 15.4 million of them will be unable to walk even 2–3 blocks in their neighborhood [2]. Active mobility (e.g., walking) is a key source of physical activity in older adults. Mobility limitations, such as inability to walk without support and prevalence of sedentary behavior, would lead to about $42 billion additional annual healthcare costs [2]. Moreover, a sedentary lifestyle can increase the risk of obesity, cardiovascular disease [3], and diabetes [4]. Mobility behaviors are risk factors for cognitive and neurodegenerative diseases, such as Parkinson’s and Alzheimer’s [5, 6]
Many research studies have focused on measurement of physical functioning in laboratory environments, referred to as “experimental” assessments. These assessments reflect the capacity and capability of a person [7]. In the last two decades, focus has increased on assessing real-life mobility and participation, also called “enacted” mobility [8]. There are popular self-reported mobility assessment questionnaires, such as the Life Space Assessment (see Taylor et al. [9], review), to measure enacted mobility. Self-reported measures are quick and easy tools; however, they are prone to recall bias, individual perception of neighborhood, and present challenges among individuals with cognitive impairment. Self-reported measures are not good at capturing dimensions of activity, such as duration and day-to-day variability.
The use of accelerometry and GPS as objective measures to record temporal activity and spatial movements during community ambulation is growing. We conceptualize enacted mobility in the community as (1) quantity and performance of physical activity and (2) spatial navigation and activity location. Accelerometers can be used to record change in body movements, steps per day, intensity of activity, and quality of walking, i.e., gait characteristics, such as step time variability and symmetry; GPS can record location, mode, path, and destinations. Together, these two technologies complement each other in measuring enacted mobility. Existing systematic reviews in the literature are focused on methodological issues, such as sensor properties, device placement, and sedentary and physical activity level cut-offs for older adults [10–12]. Additionally, studies utilizing GPS to monitor location of activity and participation in older adults (above 50 years) have been reviewed [13]. However, no existing reviews have assessed the factors associated with accelerometry and GPS-based measures of mobility in natural environments.
An individual’s enacted mobility may be facilitated or hindered by a variety of factors, such as physical abilities, cognitive function, psychosocial aspects, and external environment characteristics [14, 15]. In this review article, we summarize the research studies that focus on these facilitators and barriers to enacted mobility in community-dwelling older adults, via accelerometry and GPS. Studying these associations will further our understanding of these quantitative mobility measures. We address the following questions in this qualitative review: (1) What metrics extracted from accelerometry and GPS quantify real-world enacted mobility? (2) To what extent are accelerometer and GPS devices being used to assess enacted mobility? (3) What is current knowledge and where are the gaps in assessing associations of facilitators and barriers to enacted mobility?
Search strategy method
PubMed, Web of Science, and IEEE Xplore databases were used to search for research studies with keywords “Mobility” AND “Older Adults” AND (“Accelerometer” OR “GPS” OR “Global Positioning System”). Studies published from January 2000 to March 2021 have been included. A study was included if association of at least one facilitator or barrier to enacted mobility quantified by either GPS or accelerometer or both was assessed. There was no restriction on study design or country where the research was conducted as long as community-dwelling older adults (> 60 years) participated. Disabilities, such as Parkinson’s, dementia, and other neuromotor disorders, can limit mobility of older adults, by default. In this review article, we want to include general populations of community-dwelling older adults rather than patient populations with conditions that would severely impair mobility. This will help in understanding facilitators and barriers influencing mobility during the normal aging process. Therefore, studies assessing individuals with existing physical disabilities, severe cognitive impairments, and other neurodegenerative disorders are not included in this review.
Results for data extraction and study synthesis
A total of n = 459 records were identified using the keyword combination “mobility” AND “older adults” AND (“accelerometer” OR “GPS” OR “global positioning system”) in PubMed, Web of Science, and IEEE Xplore, between 01/01/2000 and 03/31/2021. We removed duplicates (n = 126). We next excluded studies based on titles and abstracts (n = 151). These consisted of individuals with patient population (n = 103). Some excluded studies were focused on individuals residing in-care facilities, were hospitalized, or had major surgeries, and fractures (n = 36). Further, reviews and protocols were excluded (n = 12). The remaining full-text articles (n = 182) were assessed for eligibility, out of which n = 49 articles were included in this final review. The excluded articles (n = 133) either did not record daily life/real-life mobility using sensors (n = 50) or did not assess any facilitator or barrier (n = 57) or included individuals with age less than 60 years (n = 26). For detailed literature identification and screening process, refer to Supplementary Table 1 and Supplementary Fig. 1.
Most studies were cross-sectional in design and used sensors at the lower back position. A total of about n = 19,267 older adults (≥ 60 years) were assessed in these studies (age 76.2 ± 4.7 years, 40% females). These studies analyzed 3–10 days of sensor data. The study sizes typically varied from about 100 to 1000 participants. The studies were from different countries, all notably developed (United States, United Kingdom, Canada, Japan, Finland, the Netherlands, Germany). Detailed participant characteristics for studies are given in Supplementary Table 2. The sections below provide synthesized takeaways from these studies.
Quantification of enacted mobility
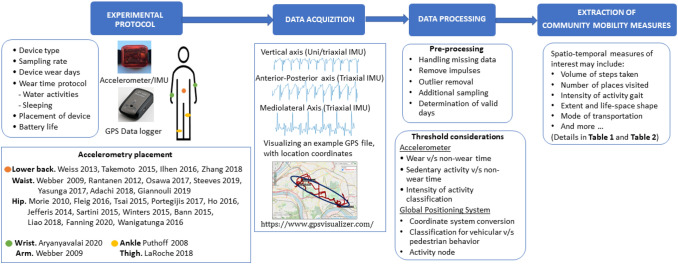
Enacted mobility can be captured using Inertial Measurement Units/accelerometers and GPS. These two modalities complement each other with regard to the information provided. A general framework of processing accelerometer and GPS data consists of four steps: (1) determine the protocol, (2) acquire data, (3) data processing, and (4) extract the quantitative measures of enacted mobility. Measures that have been used include activity characteristics (intensity, duration, frequency, walking quality) and spatial navigation behavior (Fig. 1).
Fig. 1.
A framework for accelerometer and GPS data processing. A Experimental protocol B Acquisition of data C Data processing D Extraction of spatio-temporal measures
Accelerometer
Studies have utilized uniaxial as well as triaxial accelerometers to record daily activity, typically for 3–10 days. A considerable number of studies using accelerometry and assessing at least one facilitator or barrier were found. Sedentary behavior includes sitting, reclining, or lying position; light physical activities are mostly indoor activities of daily living, such as walking inside the home, bathing, or changing one’s clothes, whereas moderate-vigorous physical activity (MVPA) includes outdoor activities, such as active walking and exercises. Standard accelerometer activity counts range is 1–100 per minute (<1.5 metabolic equivalents) for sedentary, 100–1951 activity counts per minute (1.5–3.0 metabolic equivalents) for light physical activity, and >1952 counts per minute (>3 metabolic equivalents) for MVPA [11, 16]. We adapted the dimensions of physical activity [17], categorizing the accelerometry-based measures into volume, activity intensity, and gait quality, and have summarized the studies that utilized each measure (Table 1). “Volume” includes counts or quantities of steps, walking bouts, activity, and transitions. These likely account for light intensity activity, such as casual walking. “Activity intensity” focuses on time spent in MVPA, energy equivalents, and accumulation of MVPA. “Gait quality” includes cadence, variability, and other aspects of walking. Studies utilizing accelerometry have primarily focused on recording physical activity, for which signal in vertical direction provides accurate and sufficient information. Potentially useful signals for gait analysis in the mediolateral and anterior-posterior [18] directions were often not analyzed. Placement of the sensors is usually on the waist, lower back, or right hip (Figure 1).
Table 1.
Categorization of accelerometer-based measures and associated studies
| Volume | Accelerometer-based measures | Gait Quality |
|---|---|---|
| Moderate-Vigorous Activity | ||
|
Step count (34, 35, 37, 39, 42–44, 46, 47, 49, 50, 57, 60–62, 65, 70, 79, 80, 87, 99) Walking bouts count (37) Mean daily activity counts (33, 43, 62) Transitions from high-low activity (62) Up-down transitions (41, 56) |
Minutes (33, 34, 38, 42–44, 46, 48–50, 52, 57, 65, 69, 79, 80) METsa (40, 53, 57, 64, 85, 91) Accumulation (52, 55) |
Step and stride time (37) Smoothness (37) Complexity (44, 46) Entropy (37, 46) Acceleration range (37, 38) Cadence (38, 39, 44) |
aMETs metabolic equivalents in energy
Global positioning system
There were fewer GPS-based studies to measure enacted mobility. Most of these studies used both GPS and accelerometer. Spatial (count, extent, and shape) and temporal (duration) aspects were the focus, motivated from the detailed GPS measure classification [19, 20] (Table 2). “Count” refers to the number of mobility-related events, such as number of visited locations and number of trips made (on foot or vehicular). “Extent” refers to the spatial size of mobility-related behavior, for example, distance traveled, life-space area, etc. “Shape” is a measure of distribution of activity locations and can be quantified using circularity or compactness of life space. “Duration” captures temporal aspects, such as time out of home and time spent as pedestrian vs in vehicle. In addition to the variables tabulated, GPS devices can record walking speed and driving speed [21].
Table 2.
Classification of GPS acquired spatio-temporal measures of enacted mobility and associated studies
| Spatial measures | Temporal measures | ||
|---|---|---|---|
| Count | Extent | Shape | Duration |
|
Activity nodes (59, 74, 82) Pedestrian trips (21, 58) Vehicular trips (58) Total trips (45) Driving episodes (21) Walking tracks (59) |
Total distance (34, 45, 63, 74) Vehicle distance (58, 100) Pedestrian distance (58, 59) Distance traveled per episode (21) Ellipse standard deviation (71, 82) Convex hull–life-space area (34, 63) Maximum action range (34, 45, 59, 63) Daily path area (71, 82) |
Min. convex polygon (71, 74, 82) Life-space circularity and compactness (71, 82) |
Time out of home (59) Walking time (21, 59) Time walking for transport (70) Time spent driving (21) Vehicle time (58, 100) Time spent per activity node (74) |
Activity nodes: number of places visited (sometimes a threshold on the amount of time spent is considered for the node to qualify as an activity node) Ellipse standard deviation: measures the directional distribution of a series of GPS points Convex hull –life-space area: Area of convex hull containing all GPS coordinates Maximum action range: maximum distance traveled from home Daily path area: Builds buffers (generally 200 m) around all of individual’s trips to give geographic extent of travel Minimum convex polygon: Convex polygon (of minimum edges) around set of points containing all GPS coordinates Life-space circularity/compactness: measure of how circular a polygon of activity space is; can be indicative of capacity of neighborhoods to provide opportunities to carry day-to-day activities and role of driving
Facilitators and Barriers to enacted mobility
Factors that impact enacted mobility of older adults have been identified using the associations of self-reported mobility, specifically the Life-Space Assessment [22, 23] with (a) physical capacity and functions [18, 24, 25], (b) cognition [26, 27], (c) psychosocial factors [28, 29], (d) the environment [30, 31], and (e) socio-economic status of the individual and community [32]. A canonical framework emphasizing the role of these facilitators and barriers as mobility extends from the home to outdoors, the neighborhood, the surrounding community, and beyond has been proposed [15]. Gender and cultural and biographical factors also influence one’s mobility. The multidimensional nature of mobility and interrelationships among these dimensions is important. We will now explore the relation between physical, cognitive, psychosocial, and environmental factors to enacted mobility captured by accelerometry and GPS.
Individual physical function
Our discussion of physical aspects of mobility is limited to functional measures of gait, balance, walking endurance, posture transfers, and fall history. These aspects of function integrate across multiple body systems, so we chose not to include system-specific measures, such as muscle strength. The relationships between physical function and enacted mobility are tabulated by modality, accelerometers (Table 3a), and GPS (Table 4a).
Table 3.
Association of accelerometry quantified enacted mobility with facilitators and barriers–physical function, cognitive function, psychosocial factors, and external environment
| Category | Laboratory assessment | Accelerometry | ||
|---|---|---|---|---|
| Volume | Moderate-vigorous intensity | Gait quality | ||
| a. Physical function | ||||
| Gait | Walk speed |
a (33),a (34), b (36), b (40), |
a (35), a (36), a (34), b (40) |
a (37), a (38) a (39) |
| Walking Endurance | Aerobic capacity (VO2max) | a (33), b (41) | b (41) | |
| 400 m walk Test | a (38) | a (38), a (39) | ||
| 5 Minute walk test | a (35) | |||
| 6 Minute walk test | a (55) | |||
| 10 Minute walk test | a (42) | a (42) | ||
| Walking effort | a (41) | a (41) | ||
| Balance | One leg standing | a (42) | a (35) | a (37) |
| Balance and mobility Scale | a (45) | a (44) | ||
| Transfers | Five Times Sit to Stand Test | a (55) | ||
| Fall history | Faller/non-faller | a (47), a (48), | a (47), a (48) | a (37), a (46) |
| a (49), b (37) | ||||
| Combined function assessments | a (50), a (52), | |||
| Performance-based | Short physical performance battery | a (33), a (50), a (51) | a (53) | a (38)c |
| Timed up and go | a (54), a (42), a (34), a (45), b (56) | a (35), a (54), a (55), a (34) | a (37) | |
| Self-reported | 10 item physical function | a (57) | ||
| Physical functioning interview | a (43) | |||
| b. Cognitive function | ||||
| Executive function | Trail making test | a (34) | ||
| Digital symbol code | a (62) | |||
| n-back (1 and 2 back) | a (62) | |||
| Task switching paradigm | a (62) | |||
| Erickson Flanker task | a (62) | |||
| Planning ability | HOTAP.A | a (34) | ||
| Visuospatial attention | Attention window test | a (34) | ||
| Spatial memory | Grid span test | b (45) | a (34) | |
| Literacy/IQ | National adult reading test | b (45) | b (56) | |
| Episodic memory | Hopkins verbal Learning test | a (62) | ||
| c. Psychosocial factors | ||||
| Psychological | ||||
| Depression | Geriatric depression scale | a (34) | a (34), a (64) | |
| Negative affect | Momentary negative affect | a (65) | ||
| Anxiety | State-trait anxiety inventory | a (45) | ||
| Confidence and attitudes | ||||
| Walking confidence | Gait Efficacy Scale | a (34) | a (34), a (68) | |
| Balance confidence | Activities-specific Balance Confidence | a (34) | a (34) | |
| Fear of falling | Fall Efficacy Scale | a (45), a (48) | a (48), a (40) | |
| Attitude toward walking | Walking-like scale | a (68) | ||
| Physical activity intentions | a (69) | a (69) | ||
| Social network | Lubben Scale | a (64) | ||
| People in network | a (45) | |||
| Ageism | Ageism survey scale | a (34) | a (34) | |
| Personality | Personality test | a (34) | a (34) | |
| d. Environmental factors | ||||
| Weather |
Temperature Rain |
b (34) a (69) |
a (70), o (34) a (69), a (70) |
|
| Neighborhood | Walkability | a (51) | a (53)* | |
| NEWS-SNQL | a (68) | |||
| Satisfaction survey | a (72), a (68) | |||
| PENFOM | b (51) | a (64) | ||
| Facilities | a (64) | |||
HOTAP attention and planning assessment scale, NEWS-SNQL neighborhood quality of life survey, PENFOM perceived environmental facilitators for outdoor mobility
*Mediating effect of high income, high walkable neighborhood in association between physical functioning and activity
aAssociation in expected direction
bNo association found
cAssociation found for acceleration range but not cadence
Table 4.
Association of GPS quantified enacted mobility with facilitators and barriers–physical function, cognitive function, psychosocial factors, and external environment
| Category | Laboratory test | GPS | |||
|---|---|---|---|---|---|
| Space | Time | ||||
| Count | Extent | Shape | Duration | ||
| a Physical function | |||||
| Walking endurance | 400 m walk test | a (58)* | a (58)* | ||
| Balance | One leg standing | a (45) | a (45) | ||
| Combined function assessments | |||||
| Performance-based | Short physical performance battery | a (58)* | a (58)* | a (58)* | |
| Timed up and go | a (45) | b (45) | |||
| Self-reported | Short form survey − 36 | a (21) | a (21), a (59) | a (21), a (59) | |
| b. Cognitive function | |||||
| Executive function | Trail making test A and B | b (58) | a (59), b (55) | b (58) | |
| Planning ability | HOTAP | a (63), a (34) | |||
| Visuospatial attention | Attention window test | a (63), a (34) | |||
| Spatial memory | Grid span test | a (45) | a (63), a (34), a (45) | ||
| Working memory | Digit span test (forward and backward) | a (59) | |||
| Episodic memory | Word list learning, word list recall, logical memory-I, logical memory-II | a (59) | a (59) | a (59) | |
| c. Psychosocial factors | |||||
| Psychological | |||||
| Depression |
Geriatric depression scale Geriatric depression scale (Short version) |
a (58)* | a (58)* |
a (58)* a (59) |
|
| Negative affect | Positive and negative affect scale | b (21) | b (21) | b (21) | |
| Anxiety | State-trait anxiety inventory | b (45) | b (45) | ||
| Confidence and attitudes | |||||
| Fear of falling | Fall efficacy scale | a (58)**, b (45) | a (58)*, a (34), b (45) | a (58)* | |
| Ageism | Ageism survey scale | a (34) | |||
| Quality of life | Life satisfaction 1–10 scale | a (21) | a (21) | ||
| d. Environmental factors | |||||
| Weather | Temperature | b (34) | a (70) | ||
| Rain | a (70) | ||||
| Neighborhood | Walkability | a (71)c | |||
HOTAP attention and planning assessment scale
*association only with pedestrian-based measures; **association only with vehicular trips
aAssociation in expected direction
bNo association found
cLarger activity space for less-walkable neighborhood
Faster walking speed measured in the laboratory has been consistently related to higher mobility by accelerometry measures, including volume [33, 34], intensity [34–36], and gait quality [37–39] (Table 3). However, not all studies have found positive associations between gait speed and volume [36, 40]. Gait speed has been associated with the amount of MVPA and gait quality, even after including demographics and step counts as covariates [35–37, 39].
Greater walking endurance was consistently related to better mobility by accelerometry measures, regardless of the duration of the walk tests used for assessment [33, 35, 38, 39, 41–43] (Table 3). Laboratory measures of balance and transfers were related to better mobility by accelerometry [35, 37, 42, 44, 45], though only one study has assessed transfers [43]. Like balance, self-reported fall history has been related to multiple aspects of mobility measured by accelerometry (Table 3). However, there is no consensus on if volume, quality, or both aspects of mobility are important considerations to reduce fall risk. Individuals with two or more falls differed from non-fallers on gait quality as measured by step time and entropy rate. In contrast, fall history was not associated with volume-based accelerometry measures, such as steps per day [37, 46]. This contrasts with studies that showed non-recurrent fallers (less than two fall) took significantly more steps per day than recurrent fallers [47, 48] and that fall risk was reduced in those walking > 5000 steps per day (volume measure) [49]. One study found that adjusting for psychosocial factors attenuated the differences in mobility between fallers and non-fallers [48].
Finally, several studies have shown that combined measures of physical function [i.e., Short Physical Performance Battery [33, 38, 50–53] and Timed Up and Go [34, 35, 37, 42, 54, 55] were related to accelerometry measures of mobility, with only a single study finding no association between the Timed Up and Go and volume aspect of mobility [56] (Table 3). Self-reported physical function is also associated with MVPA [43, 57].
No study has examined gait speed and fall history in relation to spatio-temporal GPS measures. Only one study examined endurance in relation to GPS measures and found that individuals with a faster 400 m walk time made more walking trips [58]; but no association with vehicular trips was found. Interestingly, ability to balance on one leg was a key predictor of mobility in a GPS accelerometry-based study that included physical, cognitive, and psychosocial factors [45]. GPS measures indicated individuals with better physical functioning were more engaged in walking, had greater spatial extent of travel, and had greater time out of home [21, 58, 59].
Overall, volume and activity intensity measures from accelerometry are well studied. Quite a few studies assessed gait quality in real-world environment [37–39, 44, 46], emphasizing a growing interest in quantifying “how we walk” in real-world settings.
Domain-specific cognitive function
Performing daily tasks and navigating the environment (e.g., traffic situations, road-crossings, and using public transportation) require adequate cognitive functioning. Studies have explored potential applications of out-of-home mobility behaviors in older adults as indicators of cognitive deficits [60, 61]. In comparison to the number of studies assessing physical capabilities, fewer studies explored the relationship between cognitive function and enacted mobility measures using accelerometry (Table 3b) and GPS (Table 4b).
Only one study assessed associations between executive function and accelerometry measured volume of mobility, finding a positive relation [34] . In two studies, better cognitive performance across multiple domains, including executive function, planning ability, visuospatial attention, spatial memory, and episodic memory, was associated with greater amounts of MVPA [34, 62] and the associations persisted even after considering covariates, such as socio-demographic, sleep quality, perceived stress, and comorbidities. Interestingly, Wanigatunga and colleagues suggested that older adults with more preserved cognitive function have the capability to be active for longer periods of time needed for completion of a task-oriented test [62]. Studies found no associations between literacy level and mobility measures [45, 56] and there were no studies assessing the relationship between cognitive function and free-living gait quality.
Several studies found associations of cognitive domains, such as executive function, planning ability, visuospatial attention, spatial memory, working memory, and episodic memory with spatial measures of mobility from GPS [34, 45, 59, 63]. Episodic memory was a predictor of GPS measures, such as time spent out of home, number of locations visited, and life-space area; however, no such associations with walking tracks, time, and distance in walking were found by the same study [59]. Surprisingly, two studies did not find associations of executive functioning with GPS measures [58, 61]. Visuospatial attention was found to be the strongest predictor of mobility, establishing a close link between attention and enacted mobility [63].
Psychosocial factors
Studies have explored the relationship between psychosocial factors and enacted mobility measures using accelerometry (Table 3c) and GPS (Table 4c).
Studies using accelerometry have found that depression, negative affect, and anxiety are associated with less step count and less amounts of MVPA [34, 45, 48, 64, 65]. This supports the activity theory of aging [66, 67] that people with higher positive affect are more active out of home. A greater confidence in walking and balancing and a reduced fear of falling have shown associations with greater volume and MVPA measures of mobility [34, 40, 45, 47, 48, 68]. Interestingly, fear of falling restricted physical activity in older adults, even when they had relatively high physical functioning [40]. Another study found that the association of fear of falling with physical activity was independent of actual fall history [48], indicating that older adults could reduce activity due to fear even without having experienced a fall. Attitude toward walking (i.e., enjoyment of walking) also impacts PA and overall mobility [68, 69]. This suggests that physical activity intentions are potentially modifiable and may be targeted using cognitive behavioral interventions. No study evaluated relation between psychosocial factors and free-living gait quality.
In GPS studies, significant negative associations were found for fear of falling and depressive symptoms with number of pedestrian trips, distance walked, and trip durations [34, 58, 59]. These associations were inconsistent with vehicular trips [45, 58]. Two studies did not find associations of negative affect and anxiety with GPS measures [21, 45], unlike some accelerometry-based studies that reported such associations. Psychosocial factors in relation to enacted mobility are a growing topic of research.
External environmental factors
Few studies have explored the relationship between environmental factors and enacted mobility measures using accelerometry (Table 3d) and GPS (Table 4d) in community-dwelling older adults.
Accelerometry measures of physical activity varied with the weather. As expected, precipitation [69, 70] and temperature extremes [70] were associated with reduced volume (step counts), walking minutes, and activity (duration and intensity), though the support for this was not consistent across studies. For example, no relation between temperature and enacted mobility was found by Giannouli and colleagues[34].
Neighborhood attributes, such as higher street connectivity, greater walkability, proximity to destinations, traffic conditions, presence of parks, and overall diversity of land use, are associated with increased mobility, particularly MVPA, among older adults [64, 68, 71, 72]. However, one study noted that an individual’s perception of diversity in built environment and street connectivity influenced their “confidence to walk outside,” suggesting that association of these factors with enacted mobility was not independent of walking confidence [68]. Further, two studies showed that the presence of lower-extremity physical limitations affected the strength of some person–environment relationships [51, 73]. One study found that higher physical functioning scores were associated with higher MVP only in the high-income, highly walkable neighborhoods, whereas no significant association was observed between physical functioning and MVPA in low-income neighborhoods or in high-income, low-walkable neighborhoods, suggesting the additional role of socio-economic status as an additional determinant of mobility [53].
Only two studies have assessed neighborhood characteristics and temperature in relation to spatial measures of mobility from GPS [34, 71]. One reported individuals in less-walkable neighborhoods to have larger activity spaces [71], while the other found no association of temperature with spatio-temporal measures of mobility [34].
Gaps in the literature and future directions
Forty-nine studies were identified that utilized accelerometry and/or GPS measures of community mobility in older adults. Most studies using accelerometry focused on measurement of step count and minutes in MVPA and studies using GPS focused on distance traveled. In contrast, there is a lack of data on quality of walking and spatial metrics of travel. There is lack of consistency in the data collection methods and quantification of the accelerometry and GPS signals. These inconsistencies make it difficult to compare the studies; however, they do provide insights into the existing gaps in measurement of facilitators and barriers to mobility that future research studies can focus on. In this section we discuss gaps and future directions for accelerometry and GPS sensor-based measurement of enacted mobility. We discuss the facilitators and barriers to enacted mobility that are lacking in literature. Finally, we emphasize the public health implications of sensor technology in mobility assessment of older adults.
Sensor technology for measurement of enacted mobility
Assessment of community mobility by accelerometry and GPS provides objective methods to quantify mobility. Some of the advantages are overcoming recall bias, and providing a detailed understanding of individual spatio-temporal behavior and valuable insights into person–environmental interactions [74]. Valuable insights into environmental facilitators and inhibitors are also being defined. However, using technology to assess enacted mobility comes with technical challenges that must be overcome. Current issues are as follows: (1) limited battery life, (2) relatively low sampling rate for many GPS devices, (3) reliance on the participant to wear and charge the device, and (4) parameterizing the data during processing of accelerometry and GPS signals (Fig. 1). Signal drop in GPS satellites leads to missing data points which require interpolation. Discontinuous data recording can affect comprehensive analysis. The current technical challenges to using accelerometry and GPS for assessment of enacted mobility have been detailed in recent reviews [12, 13, 75]. Even so, the objective information about variability in mobility that these wearable technologies can provide have numerous applications. This detailed spatio-temporal assessment potentially outweighs the current challenges in data processing from these modalities that the research community continues to address.
Gaps and future directions of accelerometry-based enacted mobility assessment
Most studies used a triaxial accelerometer and the activity measures were based on data from only one axis (usually the vertical axis). Only two studies leveraged the full capabilities of accelerometry [37, 46]. The temporal and statistical measures extracted from anterior–posterior and mediolateral signals could provide further information on quality of movement. Studies assessing gait quality in laboratory settings and in real-world settings are not common. Moreover, there is a need to perform analyses beyond the number of steps as it can be a deceiving measure for older adults taking more smaller steps [76]. When assessing, it is difficult but necessary to separate the relative influence of volume versus intensity of physical activity. For example, walking at a higher cadence will increase the number of steps per day if distance is maintained [39]. Accelerometry may also underestimate physical activity among those walking slowly [77]. Most studies in this review utilized single accelerometers placed at lower back or waist. Single accelerometers are limited in that they cannot accurately capture and distinguish between different postures (i.e., standing still, sitting, or lying), which can possibly lead to overestimating or underestimating activity, thereby impacting enacted mobility measures. Some studies have shown that an additional sensor placed on thigh or chest, in combination with sensors on lower back are able to predict postures accurately [78, 79]. More research is needed to understand role of posture as a component in enacted mobility. Further, accelerometry studies in the review have focused on activity monitoring; however, “activity accumulation” through the course of the day is also important and needs more research [52, 55, 56].
Gaps and future directions of GPS-based enacted mobility assessment
GPS has only recently been applied to research studies compared to accelerometry. We only found eight studies that utilized both accelerometer and GPS for older adults (Supplementary Table 3). There is little consensus regarding processing of the GPS data. Parameters of the navigated space in relation to physical, cognitive, psychosocial, and environmental factors impacting mobility have yet to be explored. The distinction between active and passive modes of transportation is necessary and needs to be considered during analysis. For example, if the participants made little use of passive transportation and instead were mainly physically active, the associations of physical factors to life-space mobility will stand out compared to cognitive and psychosocial measures [34]. Destinations and life space may be associated with objectively measured physical activity [71, 80, 81]. Therefore, prospective studies should also assess associations between accelerometry-based activity and GPS-based space [82]. GPS is a popular technology incorporated in most smartphone devices. Validation of spatial measures that can be derived from GPS and their relation to factors influencing enacted mobility have potential to alter intervention strategies to enhance participation of older adults in the community [83].
Bridging semantics and technology output: Mixed-methods approach
Future community outdoor mobility studies could employ both objective and subjective methods to gather in-depth information on individual travel patterns and behaviors. Even the preferred modality of examination (self-reported vs sensor-based) changes with socio-demographic factors. For example, a study examining challenges in using wearable GPS devices in low-income older adults found that older adults with low socio-economic status preferred self-reported Visualization and Evaluation of Route Itineraries, Travel Destinations, and Activity Spaces, (VERITAS) over using GPS [84]. And in another study 46% of older adults who had less of a routine refused to wear an accelerometer [85]. Self-reported outcomes are important because they consider individual perceptions of mobility and effort. Mixed-methods approaches using quantitative (accelerometry or GPS) and qualitative (interviews and diary-based) approaches together can generate different insights and enhance the overall study findings [86, 87]. Another study via ground visualization approach showed that familiarity influences spatial perceptions of neighborhoods and older adults prioritize destinations that allow them to engage in multiple activities [88].
Facilitators and barriers to enacted mobility beyond physical capabilities
Association of accelerometry measured enacted mobility with physical factors has received much attention; however, only a few studies examined the facilitators and barriers categorized as cognitive, psychosocial, or environmental. Specifically, the relation of physical functioning aspects, such as walking endurance and strength in lower extremities to activity and space measures, seems to be well established. However, enacted mobility and its associations to fall history need more investigation as it is unclear whether volume, intensity, or quality of walking is providing more insights into fall risk. Overall, there are inconsistencies regarding the measurement of specific cognition domains and their relationship with mobility behaviors of older adults, thereby requiring further investigation. Interestingly, there is an absence of studies measuring gait quality in the real world and its association with cognitive, psychosocial, and environmental measures.
Moreover, these facilitators are interlinked and the associations among them also should be accounted for in the analysis. For example, recurrent fallers (physical barrier) have increased fear of falling (psychological barrier) reflected in activity-specific balance score [37]. New research studies can focus on exploring the mediating or independent effects of these factors on mobility. For example, apart from BMI and age as determinants of mobility, variance in mobility could not be explained by a wide range of demographic, social, cognitive, and physical factors in the regression analysis [56]. Similarly, another study showed that of all the barriers and facilitators, physical, and psychological factors accounted for a significant but low proportion of variance (between 5 and 30%) in enacted mobility measures [34]. Physical, cognitive, and psychosocial factors predicted 32 to 43% variance in enacted mobility; ability to balance on single leg was found as one of the prime predictors [45].
No studies included the financial aspect (individual or neighborhood), which is also an important factor determining mobility. For example, not having a car or not being able to travel in an airplane can restrict life space. There are some other individual traits, for example, pet ownership [64, 89], car ownership, and driving capabilities [81, 90, 91], that can influence one’s activity and participation in the community. Additionally, living situation can influence enacted mobility as older couples often influence each other’s mobility patterns [92]. All studies included in this review were observed to be from developed countries. Hence, the findings may not generalize well to developing nations where population density, built environment, and economic disparity are challenges as well. Culture is another important influence, for example, restrictive mobility of women in some countries. Thus, future research studies should be more inclusive and account for access to resources, geography, finance, and culture.
While enacted mobility refers to real-life environments and actions, laboratory assessments of gait and function still provide unique and relevant insights [18]. Laboratory assessments that focus on imitating the complexities of the community may best serve the research focus of enacted mobility. A combination of physical and cognitive tasks, such as dual-task walking, changing the surface of the walking path, staircase climbing, and obstacle navigation, should be a part of assessment. The performance on these tasks may translate more into explaining variability in enacted mobility, recorded by accelerometer and GPS.
Public health implications
Within each of these facilitators and barriers, some aspects are more modifiable, and some are less modifiable. For example, balance/gait training and lifestyle changes can be provided as an intervention, but the biology of aging cannot be altered, yet. As another example, environmental determinants, such as rain, temperature, season, and other geographical aspects which are not directly in our control, are considered. However, ensuring walkable neighborhoods and maintaining sidewalk accessibility for older adults are a modifiable aspect. Negative sidewalk features have been identified as a barrier to mobility [93]. This will reduce the risk of falling accidents [70] and also increase walking confidence. While policies that care about promoting physical activity levels among seniors should keep on improving walkability, those that are focused on car-dependent and low-walkable environments could reinforce other forms of physical activity and socialization during cold months, for instance, by reinforcing indoor activities at public or community centers.
With the rising aging population, in near future, hospital facilities may not be sufficiently available for elderly for intimate examination of well-being. More so, the physical access to medical centers may be limited due to unexpected global situations, like a pandemic, as we are experiencing since 2020. Home-based remote monitoring of activity space behavior can help in diagnosis and progression of a mobility-related disability and in monitoring rehabilitation after occurrence of stroke [94, 95], Parkinson’s [96], and Alzheimer’s [61, 97], and may assist in detection of fall incidence.
Limitations of the review
Some studies assessed facilitators and barriers in detail but were not included here because they included individuals below our age thresholds [20, 74]. While this review uncovered a number of studies investigating physical, cognitive, psychosocial, and environmental barriers and facilitators, there may be more domains that this review does not include. Domains related to body system functions, such as brain networks, cardiovascular, cardiopulmonary, and immune systems, are not included. It is important to note that all studies included have assessed the mobility data prior to COVID-19. Since the pandemic, mobility patterns have been drastically affected, especially in the older adult population [98, 99]. Nevertheless, this review article gives a detailed summary of the understanding of facilitators and barriers to mobility in older adults under normal circumstances.
Conclusion
Mobility is a complex concept and leveraging sensor and GPS technology can help in better understanding of associated barriers and facilitators. As the trend in global aging increases, tailoring programs and city planning toward mobility needs of older adults have become important. More research studies in domains outside physical functionalities are needed, since other modifiable factors––cognition, psychosocial elements, external environment, as well as socio-economic considerations––play an important role for increased activity and participation of older adults in the community. In conclusion, future enacted mobility research needs to focus on assessing quality of walking in the real world, quantifying spatial movement of individuals, broader and inclusive of geography, culture and individual/neighborhood financial aspects, and finally simulating real-life complexities in laboratory to understand the physical and cognition barriers simultaneously.
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
This work was supported by the National Institutes of Health grants awarded to Dr. Andrea L Rosso (R01 AG057671, K01 AG053431).
Declarations
Conflict of interest
On behalf of all the authors, the corresponding author states that there is no conflict of interest.
Statement of human and animal rights
Human subjects were not recruited and therefore ethics approval was not required.
Informed consent
This is a review article and informed consent was not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Andrea L. Rosso and Ervin Sejdić equal contribution senior co-authors.
References
- 1.Rosso AL, Taylor JA, Tabb LP, et al. Mobility, disability, and social engagement in older adults. J Aging Health. 2013;25:617–637. doi: 10.1177/0898264313482489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cummings SR, Studenski S, Ferrucci L. A diagnosis of dismobility—giving mobility clinical visibility: a mobility working group recommendation. JAMA. 2014;311:2061–2062. doi: 10.1001/jama.2014.3033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barnes AS. (2012) Obesity and sedentary lifestyles risk for cardiovascular disease in women. Texas Hear Inst J 39(2):224–227. http://www.cdc.gov/dhdsp/maps/national_maps/. Accessed 9 March 2021 [PMC free article] [PubMed]
- 4.Joseph JJ, Echouffo-Tcheugui JB, Golden SH, et al. Physical activity, sedentary behaviors and the incidence of type 2 diabetes mellitus: the multi-ethnic study of atherosclerosis (MESA) BMJ Open Diabetes Res Care. 2016;4:185. doi: 10.1136/bmjdrc-2015-000185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamer M, Chida Y. Physical activity and risk of neurodegenerative disease: A systematic review of prospective evidence. Psychol Med. 2008;39:3–11. doi: 10.1017/S0033291708003681. [DOI] [PubMed] [Google Scholar]
- 6.Montero-Odasso M, Pieruccini-Faria F, Bartha R, et al. Motor Phenotype in neurodegenerative disorders: gait and balance platform study design protocol for the ontario neurodegenerative research initiative (ONDRI) the creative commons attribution non-commercial license (CC BY-NC 4.0) J Alzheimer’s Dis. 2017;59:707–721. doi: 10.3233/JAD-170149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Glass TA. Conjugating the “tenses” of function: discordance among hypothetical, experimental, and enacted function in older adults. Gerontologist. 1998;38:101–112. doi: 10.1093/geront/38.1.101. [DOI] [PubMed] [Google Scholar]
- 8.Tudor-Locke C. Assessment of enacted mobilityin older adults. Top Geriatr Rehabil. 2012;28:33–38. doi: 10.1097/TGR.0b013e3182341791. [DOI] [Google Scholar]
- 9.Taylor JK, Buchan IE, van der Veer SN. Assessing life-space mobility for a more holistic view on wellbeing in geriatric research and clinical practice. Aging Clin Exp Res. 2019;31:439–445. doi: 10.1007/s40520-018-0999-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang CC, Hsu YL. A review of accelerometry-based wearable motion detectors for physical activity monitoring. Sensors. 2010;10:7772–7788. doi: 10.3390/s100807772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gorman E, Hanson HM, Yang PH, Khan KM, Liu-Ambrose T, Ashe MC. Accelerometry analysis of physical activity and sedentary behavior in older adults: a systematic review and data analysis. Eur Rev Aging Phys Act. 2014;11:35–49. doi: 10.1007/s11556-013-0132-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rao AK. Wearable sensor technology to measure physical activity (PA) in the elderly. Curr Geriatr Reports. 2019;8:55–66. doi: 10.1007/s13670-019-0275-3. [DOI] [Google Scholar]
- 13.Gough C, Weber H, George S, et al. (2019) Location monitoring of physical activity and participation in community dwelling older people: a scoping review. Disabil Rehabil. 2019 doi: 10.1080/09638288.2019.1618928. [DOI] [PubMed] [Google Scholar]
- 14.Patla Aftab E, Shumway-Cook A. Dimensions of mobility space: Some subjective aspects of career mobility. J Aging Phys Act. 1999;7:7–19. doi: 10.1177/053901847201100504. [DOI] [Google Scholar]
- 15.Webber SC, Porter MM, Menec VH. Mobility in older adults: a comprehensive framework. Gerontologist. 2010;50:443–450. doi: 10.1093/geront/gnq013. [DOI] [PubMed] [Google Scholar]
- 16.Migueles JH, Cadenas-Sanchez C, Ekelund U, et al. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sport Med. 2017;47:1821–1845. doi: 10.1007/s40279-017-0716-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Strath SJ, Kaminsky LA, Ainsworth BE, et al. Guide to the assessment of physical activity: clinical and research applications: A scientific statement from the American Heart association. Circulation. 2013;128:2259–2279. doi: 10.1161/01.cir.0000435708.67487.da. [DOI] [PubMed] [Google Scholar]
- 18.Suri A, Rosso AL, VanSwearingen J, et al. Mobility of older adults: gait quality measures are associated with life-space assessment scores. J Gerontol Ser A. 2021 doi: 10.1093/gerona/glab151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fillekes MP, Kim EK, Trumpf R, et al. Assessing older adults’ daily mobility: a comparison of GPS-derived and self-reported mobility indicators. Sensors (Switzerland) 2019 doi: 10.3390/s19204551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boissy P, Blamoutier M, Brière S, et al. Quantification of free-living community mobility in healthy older adults using wearable sensors. Front Public Heal. 2018 doi: 10.3389/fpubh.2018.00216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Isaacson M, Wahl HW, Shoval N, et al. The relationship between spatial activity and wellbeing-related data among healthy older adults: an exploratory geographic and psychological analysis. In: Tannistha S, et al., editors. Cross-Cultural and Cross-Disciplinary Perspectives in Social Gerontology Springer. Singapore; 2016. [Google Scholar]
- 22.Peel C, Baker PS, Roth DL, et al. Assessing mobility in older adults: the UAB study of aging life-space assessment. Phys Ther. 2005;85:1008–1019. doi: 10.1093/ptj/85.10.1008. [DOI] [PubMed] [Google Scholar]
- 23.Baker PS, Bodner EV, Allman RM. Measuring life-space mobility in community-dwelling older adults. J Am Geriatr Soc. 2003;51:1610–1614. doi: 10.1046/j.1532-5415.2003.51512.x. [DOI] [PubMed] [Google Scholar]
- 24.Portegijs E, Rantakokko M, Mikkola TM, et al. Association between physical performance and sense of autonomy in outdoor activities and life-space mobility in community-dwelling older people. J Am Geriatr Soc. 2014;62:615–621. doi: 10.1111/jgs.12763. [DOI] [PubMed] [Google Scholar]
- 25.Lo AX, Brown CJ, Sawyer P, et al. Life-space mobility declines associated with incident falls and fractures. J Am Geriatr Soc. 2014;62:919–923. doi: 10.1111/jgs.12787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Uemura K, Shimada H, Makizako H, et al. Factors associated with life-space in older adults with amnestic mild cognitive impairment. Geriatr Gerontol Int. 2013;13:161–166. doi: 10.1111/j.1447-0594.2012.00878.x. [DOI] [PubMed] [Google Scholar]
- 27.Poranen-Clark T, von Bonsdorff MB, Rantakokko M, et al. The Temporal association between executive function and life-space mobility in old age. J Gerontol Ser A. 2017;73:835–839. doi: 10.1093/gerona/glx217. [DOI] [PubMed] [Google Scholar]
- 28.de Guzman AB, Lagdaan LFM, Lagoy MLV. The role of life-space, social activity, and depression on the subjective memory complaints of community-dwelling filipino elderly: a structural equation model. Educ Gerontol. 2015;41:348–360. doi: 10.1080/03601277.2014.970420. [DOI] [Google Scholar]
- 29.Polku H, Mikkola TM, Portegijs E, et al. Life-space mobility and dimensions of depressive symptoms among community-dwelling older adults. Aging Ment Heal. 2015;19:781–789. doi: 10.1080/13607863.2014.977768. [DOI] [PubMed] [Google Scholar]
- 30.Rantakokko M, Iwarsson S, Portegijs E, et al. Associations between environmental characteristics and life-space mobility in community-dwelling older people. J Aging Health. 2015;27:606–621. doi: 10.1177/0898264314555328. [DOI] [PubMed] [Google Scholar]
- 31.Lo AX, Rundle AG, Buys D, et al. Neighborhood disadvantage and life-space mobility are associated with incident falls in community-dwelling older adults. J Am Geriatr Soc. 2016;64:2218–2225. doi: 10.1111/jgs.14353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eronen J, Von Bonsdorff M, Rantakokko M, Portegijs E, Viljanen A, Rantanen T. Socioeconomic status and life-space mobility in old age. J Aging Phys Act. 2016;24:617–623. doi: 10.1123/japa.2015-0196. [DOI] [PubMed] [Google Scholar]
- 33.Morie M, Reid KF, Miciek R, et al. Habitual physical activity levels are associated with performance in measures of physical function and mobility in older men. J Am Geriatr Soc. 2010;58:1727–1733. doi: 10.1111/j.1532-5415.2010.03012.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Giannouli E, Fillekes MP, Mellone S, et al. Predictors of real-life mobility in community-dwelling older adults: an exploration based on a comprehensive framework for analyzing mobility. Eur Rev Aging Phys Act. 2019 doi: 10.1186/s11556-019-0225-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yasunaga A, Shibata A, Ishii K, et al. Associations of sedentary behavior and physical activity with older adults’ physical function: an isotemporal substitution approach. BMC Geriatr. 2017;17:280. doi: 10.1186/s12877-017-0675-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Adachi T, Kono Y, Iwatsu K, et al. Duration of moderate to vigorous daily activity is negatively associated with slow walking speed independently from step counts in elderly women aged 75 years or over_ a cross-sectional study. Arch Gerontol Geriatr. 2017 doi: 10.1016/j.archger.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 37.Weiss A, Brozgol M, Dorfman M, et al. Does the evaluation of gait quality during daily life provide insight into fall risk? a novel approach using 3-day accelerometer recordings. Neurorehabil Neural Repair. 2013;27:742–752. doi: 10.1177/1545968313491004. [DOI] [PubMed] [Google Scholar]
- 38.Urbanek JK, Zipunnikov V, Harris T, et al. Validation of gait characteristics extracted from raw accelerometry during walking against measures of physical function, mobility, fatigability, and fitness. J Gerontol Ser A. 2018;73:676–681. doi: 10.1093/gerona/glx174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gonzales JU, Shephard J, Dubey N. Steps per day, daily peak stepping cadence, and walking performance in older adults. J Aging Phys Act. 2015;23:395–400. doi: 10.1123/japa.2014-0049. [DOI] [PubMed] [Google Scholar]
- 40.Sawa R, Asai T, Doi T, et al. The association between physical activity, including physical activity intensity, and fear of falling differs by fear severity in older adults living in the community. J Gerontol—Ser B Psychol Sci Soc Sci. 2020;75:953–960. doi: 10.1093/geronb/gby103. [DOI] [PubMed] [Google Scholar]
- 41.LaRoche DP, Melanson EL, Baumgartner MP, et al. Physiological determinants of walking effort in older adults: should they be targets for physical activity intervention? GeroScience. 2018;40:305–315. doi: 10.1007/s11357-018-0032-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yoshida D, Nakagaichi M, Saito K, et al. The relationship between physical fitness and ambulatory activity in very elderly women with normal functioning and functional limitations. J Physiol Anthr. 2010;29:211–218. doi: 10.2114/jpa2.29.211. [DOI] [PubMed] [Google Scholar]
- 43.Steeves JA, Shiroma EJ, Conger SA, et al. Physical activity patterns and multimorbidity burden of older adults with different levels of functional status: NHANES 2003–2006. Disabil Health J. 2019;12:495–502. doi: 10.1016/j.dhjo.2019.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang W, Schwenk M, Mellone S, et al. Complexity of daily physical activity is more sensitive than conventional metrics to assess functional change in younger older adults. Sens (Switzerland) 2018 doi: 10.3390/s18072032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McInnes L, Jones E, Rochester L, et al. Mobility in community dwelling older adults: predicting successful mobility using an instrumented battery of novel measures. J Frailty Aging. 2020;9:68–73. doi: 10.14283/jfa.2019.35. [DOI] [PubMed] [Google Scholar]
- 46.Ihlen EAF, Weiss A, Bourke A, et al. The complexity of daily life walking in older adult community-dwelling fallers and non-fallers. J Biomech. 2016;49:1420–1428. doi: 10.1016/j.jbiomech.2016.02.055. [DOI] [PubMed] [Google Scholar]
- 47.Jefferis BJ, Merom D, Sartini C, et al. Physical activity and falls in older men: the critical role of mobility limitations. Med Sci Sports Exerc. 2015;47:2119–2128. doi: 10.1249/MSS.0000000000000635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jefferis BJ, Iliffe S, Kendrick D, et al. How are falls and fear of falling associated with objectively measured physical activity in a cohort of community-dwelling older men? BMC Geriatr. 2014 doi: 10.1186/1471-2318-14-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Aranyavalai T, Jalayondeja C, Jalayondeja W, et al. Association between walking 5000 step/day and fall incidence over six months in urban community-dwelling older people. BMC Geriatr. 2020;20:194. doi: 10.1186/s12877-020-01582-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Trayers T, Lawlor DA, Fox KR, et al. Associations of objectively measured physical activity with lower limb function in older men and women: Findings from the older people and active living (OPAL) study. J Aging Phys Act. 2014;22:34–43. doi: 10.1123/JAPA.2012-0087. [DOI] [PubMed] [Google Scholar]
- 51.Portegijs E, Keskinen KE, Tsai LT, et al. Physical limitations, walkability, perceived environmental facilitators and physical activity of older adults in Finland. Int J Env Res Public Health. 2017 doi: 10.3390/ijerph14030333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fanning J, Rejeski WJ, Chen SH, et al. Relationships between profiles of physical activity and major mobility disability in the LIFE study. J Am Geriatr Soc. 2020;68:1476–1483. doi: 10.1111/jgs.16386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Van Holle V, Van Cauwenberg J, Gheysen F, et al. The association between belgian older adults’ physical functioning and physical activity: what is the moderating role of the physical environment? Lucia A, ed. PLoS One. 2016;11:e0148398. doi: 10.1371/journal.pone.0148398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ho A, Ashe MC, Delongis A, et al. Gender differences in pain-physical activity linkages among older adults: lessons learned from daily life approaches. Pain Res Manag. 2016 doi: 10.1155/2016/1931590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rava A, Pihlak A, Kums T, et al. Associations of distinct levels of physical activity with mobility in independent healthy older women. Exp Gerontol. 2018;110:209–215. doi: 10.1016/j.exger.2018.06.005. [DOI] [PubMed] [Google Scholar]
- 56.Lord S, Chastin SFM, McInnes L, et al. Exploring patterns of daily physical and sedentary behaviour in community-dwelling older adults. Age Ageing. 2011;40:205–210. doi: 10.1093/ageing/afq166. [DOI] [PubMed] [Google Scholar]
- 57.Nathan A, Wood L, Giles-Corti B. Examining correlates of self-reported and objectively measured physical activity among retirement village residents. Australas J Ageing. 2014;33:250–256. doi: 10.1111/ajag.12055. [DOI] [PubMed] [Google Scholar]
- 58.Takemoto M, Carlson JA, Moran K, et al. Relationship between objectively measured transportation behaviors and health characteristics in older adults. Int J Env Res Public Health. 2015;12:13923–13937. doi: 10.3390/ijerph121113923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wettstein M, Wahl HW, Diehl MK. A multidimensional view of out-of-home behaviors in cognitively unimpaired older adults: examining differential effects of socio-demographic, cognitive, and health-related predictors. Eur J Ageing. 2014;11:141–153. doi: 10.1007/s10433-013-0292-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hausdorff JM, Hillel I, Shustak S, et al. Everyday stepping quantity and quality among older adult fallers with and without mild cognitive impairment: Initial evidence for new motor markers of cognitive defcits? J Gerontol—Ser A Biol Sci Med Sci. 2018;73:1078–1082. doi: 10.1093/gerona/glx187. [DOI] [PubMed] [Google Scholar]
- 61.Wettstein M, Wahl HW, Shoval N, et al. Out-of-home behavior and cognitive impairment in older adults: findings of the sentra project. J Appl Gerontol. 2015;34:3–25. doi: 10.1177/0733464812459373. [DOI] [PubMed] [Google Scholar]
- 62.Wanigatunga AA, Manini TM, Cook DR, et al. Community-based activity and sedentary patterns are associated with cognitive performance in mobility-limited older adults. Front Aging Neurosci. 2018 doi: 10.3389/fnagi.2018.00341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Giannouli E, Bock O, Zijlstra W. Cognitive functioning is more closely related to real-life mobility than to laboratory-based mobility parameters. Eur J Ageing. 2018;15:57–65. doi: 10.1007/s10433-017-0434-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jefferis BJ, Sartini C, Lee IM, et al. Adherence to physical activity guidelines in older adults, using objectively measured physical activity in a population-based study. BMC Public Health. 2014;14:382. doi: 10.1186/1471-2458-14-382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pauly T, Michalowski VI, Nater UM, et al. Everyday associations between older adults’ physical activity, negative affect, and cortisol. Heal Psychol. 2019;38:494–501. doi: 10.1037/hea0000743. [DOI] [PubMed] [Google Scholar]
- 66.Longino CF, Kart CS. Explicating activity theory: a formal replication. J Gerontol. 1982;37:713–722. doi: 10.1093/geronj/37.6.713. [DOI] [PubMed] [Google Scholar]
- 67.Lemon BW, Bengtson VL, Peterson JA. An exploration of the activity theory of aging: activity types and life satisfaction among in-movers to a retirement community. J Gerontol. 1972;27:511–523. doi: 10.1093/geronj/27.4.511. [DOI] [PubMed] [Google Scholar]
- 68.Fleig L, Ashe MC, Voss C, et al. Environmental and psychosocial correlates of objectively measured physical activity among older adults. Heal Psychol. 2016;35:1364–1372. doi: 10.1037/hea0000403. [DOI] [PubMed] [Google Scholar]
- 69.Hoppmann CA, Man Lee JC, Ziegelmann JP, et al. Precipitation and physical activity in older adults: the moderating role of functional mobility and physical activity intentions. J Gerontol—Ser B Psychol Sci Soc Sci. 2017;72:792–800. doi: 10.1093/geronb/gbv107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Delclòs-Alió X, Marquet O, Vich G, et al. Temperature and rain moderate the effect of neighborhood walkability on walking time for seniors in barcelona. Int J Env Res Public Health. 2020 doi: 10.3390/ijerph17010014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hirsch JA, Winters M, Clarke P, et al. Generating GPS activity spaces that shed light upon the mobility habits of older adults: a descriptive analysis. Int J Health Geogr. 2014;13:51. doi: 10.1186/1476-072X-13-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Thompson WW, Curl C, Aspinall A. Do changes to the local street environment alter behaviour and quality of life of older adults? The “DIY streets” intervention. Br J Sport Med. 2014;48:1059–1065. doi: 10.1136/bjsports. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rantanen T, Portegijs E, Viljanen A, et al. Individual and environmental factors underlying life space of older people—study protocol and design of a cohort study on life-space mobility in old age (LISPE) BMC Public Health. 2012 doi: 10.1186/1471-2458-12-1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ho SH, Tan DPS, Tan PJ, et al. The development and validation of a prototype mobility tracker for assessing the life space mobility and activity participation of older adults. BMC Geriatr. 2020;20:251. doi: 10.1186/s12877-020-01649-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lee IM, Shiroma EJ. Using accelerometers to measure physical activity in large-scale epidemiological studies: Issues and challenges. Br J Sports Med. 2014;48:197–201. doi: 10.1136/bjsports-2013-093154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Puthoff ML, Janz KF, Nielsen DH. The relationship between lower extremity strength and power to everyday walking behaviors in older adults with functional limitations. J Geriatr Phys Ther. 2008;31:24–31. doi: 10.1519/00139143-200831010-00005. [DOI] [PubMed] [Google Scholar]
- 77.Hergenroeder AL, Gibbs BB, Kotlarczyk MP, et al. Accuracy and acceptability of commercial-grade physical activity monitors in older adults. J Aging Phys Act. 2019;27:222–229. doi: 10.1123/japa.2018-0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gjoreski H, Luštrek M, Gams M. (2011) Accelerometer placement for posture recognition and fall detection. In: Proceedings—2011 7th International Conference on Intelligent Environments, IE 2011. IEEE Computer Society 47–54 Doi:10.1109/IE.2011.11
- 79.Fortune E, Lugade VA, Kaufman KR. Posture and movement classification: the comparison of tri-axial accelerometer numbers and anatomical placement. J Biomech Eng. 2014;136:0510031. doi: 10.1115/1.4026230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tsai LT, Portegijs E, Rantakokko M, et al. The association between objectively measured physical activity and life-space mobility among older people. Scand J Med Sci Sport. 2015;25:e368–e373. doi: 10.1111/sms.12337. [DOI] [PubMed] [Google Scholar]
- 81.Winters M, Voss C, Ashe MC, et al. Where do they go and how do they get there? older adults’ travel behaviour in a highly walkable environment. Soc Sci Med. 2015;133:304–312. doi: 10.1016/j.socscimed.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 82.Hirsch JA, Winters M, Ashe MC, et al. Destinations that older adults experience within their gps activity spaces relation to objectively measured physical activity. Env Behav. 2016;48:55–77. doi: 10.1177/0013916515607312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Crist K, Jankowska MM, Schipperijn J, et al. Change in GPS-assessed walking locations following a cluster-randomized controlled physical activity trial in older adults, results from the MIPARC trial. Health Place. 2021;69:102573. doi: 10.1016/J.HEALTHPLACE.2021.102573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Schmidt T, Kerr J, Kestens Y, et al. Challenges in using wearable GPS devices in low-income older adults: can map-based interviews help with assessments of mobility? Transl Behav Med. 2019;9:99–109. doi: 10.1093/tbm/iby009. [DOI] [PubMed] [Google Scholar]
- 85.Osawa Y, Arai Y, Oguma Y, et al. Relationships of muscle echo intensity with walking ability and physical activity in the very old population. J Aging Phys Act. 2017;25:189–195. doi: 10.1123/japa.2015-0203. [DOI] [PubMed] [Google Scholar]
- 86.Meijering L, Weitkamp G. Numbers and narratives: developing a mixed-methods approach to understand mobility in later life. Soc Sci Med. 2016;168:200–206. doi: 10.1016/j.socscimed.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 87.Hand CL, Rudman DL, Huot S, et al. Toward understanding person-place transactions in neighborhoods: a qualitative-participatory geospatial approach. Gerontologist. 2018;58:89–100. doi: 10.1093/geront/gnx064. [DOI] [PubMed] [Google Scholar]
- 88.Franke T, Winters M, McKay H, et al. A grounded visualization approach to explore sociospatial and temporal complexities of older adults’ mobility. Soc Sci Med. 2017;193:59–69. doi: 10.1016/j.socscimed.2017.09.047. [DOI] [PubMed] [Google Scholar]
- 89.Peacock M, Netto J, Yeung P, et al. Understanding the relationship between pet ownership and physical activity among older community-dwelling adults—a mixed methods study. J Aging Phys Act. 2020;28:131–139. doi: 10.1123/japa.2019-0056. [DOI] [PubMed] [Google Scholar]
- 90.Phillips CB, Freed SA, Ross LA. Older adult lifespace varies by driving status and residential population density. Transp Res Rec J Transp Res Board. 2019;2673:586–595. doi: 10.1177/0361198119846092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Amagasa S, Fukushima N, Kikuchi H, et al. Drivers are more physically active than non-drivers in older adults. Int J Env Res Public Health. 2018 doi: 10.3390/ijerph15061094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Heatwole Shank KS, Presgraves E. Geospatial Mapping of Late-life couplehood: dimensions of joint participation. OTJR Occup Particip Heal. 2019;39:176–183. doi: 10.1177/1539449218808277. [DOI] [PubMed] [Google Scholar]
- 93.Buman MP, Winter SJ, Sheats JL, et al. The stanford healthy neighborhood discovery tool: a computerized tool to assess active living environments. Am J Prev Med. 2013 doi: 10.1016/j.amepre.2012.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.O’Brien MK, Shawen N, Mummidisetty CK, et al. Activity recognition for persons with stroke using mobile phone technology: toward improved performance in a home setting. J Med Internet Res. 2017;19:e184. doi: 10.2196/jmir.7385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hanke TA, Hwang S, Keller S, et al. Measuring community mobility in survivors of stroke using global positioning system technology: a prospective observational study. J Neurol Phys Ther. 2019;43:175–185. doi: 10.1097/NPT.0000000000000279. [DOI] [PubMed] [Google Scholar]
- 96.Del Din S, Kirk C, Yarnall AJ, et al. Body-worn sensors for remote monitoring of parkinson’s disease motor symptoms: vision, state of the art, and challenges ahead. J Parkinsons Dis. 2021;11(s1):S35–S47. doi: 10.3233/JPD-202471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kaspar R, Oswald F, Wahl HW, et al. Daily mood and out-of-home mobility in older adults: does cognitive impairment matter? J Appl Gerontol. 2015;34:26–47. doi: 10.1177/0733464812466290. [DOI] [PubMed] [Google Scholar]
- 98.Perracini MR, de Amorim JSC, Lima CA, et al. Impact of COVID-19 pandemic on life-space mobility of older adults living in Brazil: REMOBILIZE study. Front Public Heal. 2021;9:643640. doi: 10.3389/fpubh.2021.643640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Yamada M, Kimura Y, Ishiyama D, et al. Effect of the COVID-19 epidemic on physical activity in community-dwelling older adults in Japan: a cross-sectional online survey. J Nutr Heal Aging. 2020 doi: 10.1007/s12603-020-1424-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Webber SC, Porter MM. Monitoring mobility in older adults using global positioning system (GPS) watches and accelerometers: a feasibility study. J Aging Phys Act. 2009;17:455–467. doi: 10.1123/japa.17.4.455. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.