Abstract
This paper discusses the growing problem of persisting pain after successful treatment of breast cancer and presents recommendations for improving pain-related outcomes for this group. We discuss the dominant treatment approach for persisting pain post-breast cancer treatment and draw contrasts with contemporary treatment approaches to persistent pain in non-cancer-related populations. We discuss modern application of the biopsychosocial model of pain and the notion of variable sensitivity within the pain system, moment by moment and over time. We present the implications of increasing sensitivity over time for treatment selection and implementation. By drawing on transformative changes in treatment approaches to persistent non-cancer-related pain, we describe the potentially powerful role that an intervention called pain science education, which is now recommended in clinical guidelines for musculoskeletal pain, may play in improving pain and disability outcomes after successful breast cancer treatment. Finally, we present several research recommendations that centre around adaptation of the content and delivery models of contemporary pain science education, to the post-breast cancer context.
Keywords : Pain; Breast neoplasms; Pain science education; Models, biopsychosocial
Introduction
Breast cancer is the most common cancer amongst women. Seventy-three percent of people diagnosed with breast cancer have their cancer successfully treated, defined here as being alive 5 years after diagnosis [1], but 19.5–21.8% of them experience persisting moderate-to-severe pain [2, 3]. Breast cancer survivors with persistent pain report worse scores on assessments of mental health, social functioning and vitality than pain-free survivors do [4, 5]. Epidemiological data also show that the prevalence and burden of post-breast cancer pain on activities of daily life, quality of life and fulfilment of a person’s role in society are substantial and comparable to those of chronic back pain, fibromyalgia [6, 7] or arthritis [8].
Management of persisting pain problems in non-cancer populations has moved beyond medication-based approaches. Education, active and psychological therapies and self-management skills are now considered and recommended as frontline interventions and are endorsed as such in clinical guidelines almost wherever they exist [9–12]. This is in stark contrast to how persisting pain after successful breast cancer treatment is usually approached. There seem to be no officially endorsed clinical guidelines for managing post-breast cancer pain. Existing guidelines of the European Society of Medical Oncology (ESMO) and American Society of Clinical Oncology (ASCO) focus either on pain management during the cancer treatment period [13–16] or on pharmacological treatments of pain post-cancer in general without specifying the oncology population [17]. Physical and psychological therapies are only occasionally mentioned, mostly as part of management of cancer treatment side effects in general and not specifically for pain [13–17]. The role of pain-related education during cancer treatment is relatively well studied [18] but we contend this is not the case for persisting pain post-cancer treatment. We suggest that the development, refinement and implementation of pain-related education in non-cancer pain management provide an excellent model to guide a similar approach to pain post-breast cancer. Based on current understanding of post-breast cancer pain, it seems reasonable to expect similar impacts to those observed for non-cancer pain, which would greatly improve outcomes for those 19.5–21.8% of survivors currently living with persisting pain.
In this perspectives piece, we will discuss (1) the current approach for persisting pain post-breast cancer treatment; (2) contemporary understanding of the biopsychosocial model of pain and the notion of variable sensitivity; (3) biopsychosocial considerations for post-cancer persistent pain; and (4) the potentially powerful role that contemporary pain science education might play in improving outcomes after successful breast cancer treatment.
-
Current approach for persisting pain post-breast cancer treatment
Although pain is common after finishing breast cancer treatment [2, 3], empirical data suggest that it is often underreported, under-assessed and undertreated [19, 20]. Two issues seem particularly relevant here. First, some patients feel uncomfortable discussing their symptoms or do not want to distract clinicians from other health issues and the necessary post-cancer follow-up trajectory [21]. As such, health care provider impressions of the patient’s pain may differ substantially from the true experience of the patient, resulting in more underreporting [22]. Notably, in palliative cancer care, patient and provider perspectives on pain appear concordant [23]. This may be because medication-based pain management protocols are supported by authoritative systematic reviews (albeit with incomplete high-quality evidence) [24] and widely endorsed. Second, although some clinicians will draw on a wider clinical skillset and experience to tailor pain management to specific patients, the lack of clear evidence for any particular pain management approach undermines other clinicians’ confidence in delivering effective pain management solutions. This situation has been reported for other symptoms common post-cancer, for example depression [25]. Regardless of clinician confidence, there seems a critical need for an expanded toolbox for managing pain post-breast cancer.
Clinical guidelines for the management of persistent pain in non-cancer populations endorse non-pharmacological approaches [9–12]. This reflects in part the evidence against pharmacological approaches and significant concerns of harm [26]. For opioids specifically, recent guidelines stress their limited role in persistent non-cancer pain [26]—empirical data show limited benefit and unacceptable risk [27, 28]. For post-(breast) cancer pain, the role of opioids and other types of analgesics is less studied such that long-term safety and effectiveness remain to be demonstrated [17]. There may be a role in neuropathic pain post-breast cancer and generic internationally endorsed guidelines for the management of neuropathic pain are available and broadly applicable [29]. Even with guideline-conformant pharmacological management of neuropathic pain, only 40 to 60% of patients will reach 30% pain reduction [30]. As such, it seems critical and timely that the field prioritizes research into (additional) innovative, high value pain reduction approaches in people who have successfully completed breast cancer treatment.
-
The biopsychosocial model of pain and the notion of variable sensitivity
The biopsychosocial model was first proposed over 50 years ago [31]. It was grounded in the early Biological Systems Theory [32, 33], remains consistent with the contemporary General Systems Theory [34] and for the first time accounted for the missing dimensions of the biomedical model. While traditional biomedical models focus on pathophysiology and other biological approaches to disease, the biopsychosocial model emphasises the importance of understanding human health and illness in their fullest contexts [31]. The biopsychosocial approach systematically considers biological, psychological and social factors and their complex interactions in understanding health, illness and health care delivery.
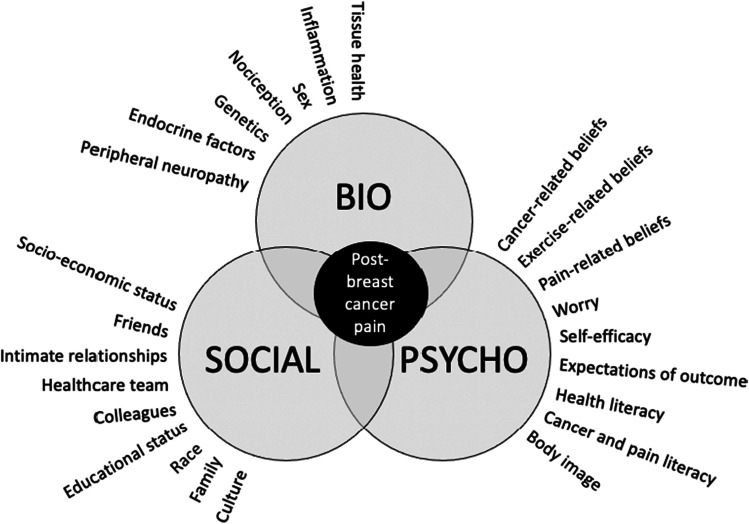
Application of the biopsychosocial model to pain asserts that pain results from the interaction and integration of these biological, psychological and social factors (Fig. 1) [35]. A vast body of literature suggests that this integration occurs primarily, although not exclusively, within the brain [36, 37]. That many variables across these domains can influence pain is relevant to the International Association for the Study of Pain (IASP) developing a classification system whereby pain is considered nociceptive (associated with demonstrable or likely tissue inflammation or damage), neuropathic (associated with demonstrable nerve injury or disease) or ‘nociplastic’ (associated with neither) [38]. ‘Nociplastic pain’ was proposed as a third ‘mechanistic descriptor’ but it does not reflect a particular mechanism [39] and seems to be a classification of exclusion. Perhaps unsurprisingly, it has had a mixed response from the field. This classification system is of great relevance to post-breast cancer pain because nociceptive and neuropathic criteria are sometimes met, but seldom explain the full pain experience. Of course, this situation is not unique—the most common and burdensome painful conditions seem to reflect ‘mixed pain states’ [40], such that it may be more helpful from a clinical reasoning perspective to consider nociceptive, neuropathic and nociplastic ‘contributions’ to a pain state. Such an approach may well reduce the risk that those for whom non-neural tissue or neural injury is not clearly evident are put in an ‘other’ category, potentially returning us to the inference of ‘real’ and ‘not real’ pains. That all three contributions are often involved in post-breast cancer pain is probably one reason that single modality or medication-only treatment approaches are often ineffective.
The other trigger for suggesting a ‘nociplastic pain’ classification is the potentially profound dynamics of pain system sensitivity. There is now compelling evidence that variations in system responsiveness occur across time scales, from seconds [41] to years [42]. These changes are mediated by both real-time interaction between sensory, environmental, psychological and social factors and a range of changes that constitute one form or another of learning [43]. Persisting pain is characterised by the latter—increased sensitivity within the pain-relevant neuroimmune axis. This realization was triggered by the discovery of enhanced stimulus–response profiles of spinal nociceptive neurons in animal models of nerve injury [44], and is now thought to be mediated by similar enhanced responses throughout the spinal cord, brain and immune and endocrine systems. The manifestation of this widespread learning is that rather than pain serving to protect tissue and promote healing, it comes to ‘overprotect’ tissue and limit recovery [45].
-
3.
Biopsychosocial contributors to pain post-breast cancer treatment
In the early stage of cancer treatment, acute pain caused by surgery, radiotherapy and/or chemotherapy is present in many cases [47]. After surgery and radiotherapy in particular, (painful) dysfunctions related to the musculoskeletal system are often described [48]. Chemotherapy-induced peripheral neuropathy is a common sequela with certain types of chemotherapy (e.g. taxanes). In this case, nerves may become sensitized and this results in positive and negative sensory signs and symptoms, including pain [49]. The most commonly described radiotherapy-related side effect is fibrosis of the skin and soft tissues [50]. This is typically a late and painful effect, with the onset varying up to many years after radiotherapy. It is hypothesised that ionizing radiation causes reactive oxygen and nitrogen molecules that lead to localized inflammation. This inflammatory process can ultimately evolve into a fibrotic one with increased collagen deposition, poor vascularity and scarring, often associated with pain [50]. Hormone therapy–related arthralgia reportedly affects 36–80% of women treated with aromatase inhibitors, leading up to 13–22% of women to quit hormone therapy [51]. The exact mechanism of arthralgia with aromatase inhibitors has still to be unravelled, but fundamental (animal) studies reveal a possible role of oestrogen deprivation in peripheral and central nociceptive processing pathways [51, 52].
A wide range of psychological variables have been found to influence pain in cancer, including mood states such as anxiety, depression, worry and distress [53, 54], including cognitive variables related to appraisal of the likely cause or impact of tissue injury. In musculoskeletal pain, such variables might include the perceived vulnerability of the body part to mechanical load (e.g. ‘my back is damaged’, or ‘it’s bone on bone’). In post-cancer pain, these variables might also apply (e.g. ‘my skin is damaged’) but perceived vulnerability to returning cancer might be considered a more potent cognitive variable. There are two parts to this: reduced threshold (allodynia) and enhanced responsiveness (hyperalgesia) for pain in response to changes in tissue environment and enhanced behavioural responses when pain occurs. For example, everyday aches and pains can be attributed to recurrent or new cancer [55]. While recent research has shown this mostly within the context of childhood cancer survival [56, 57], studies indicate that survivors of breast cancer also worry about everyday aches and pains as indicating a recurrence of their disease [58, 59]. One can easily draw the comparison here with back pain: the individual with back pain who perceived that they have a ‘slipped disc’ that may well slip further will be more likely to experience pain on mechanical loading of the back and more likely to attribute any back pain they do have as reflecting further ‘slipping of the disc’. The clinical implication for pain science education after breast cancer is to improve understanding of the multiple contributors to pain, including psychological factors.
Fig. 1.
The biopsychosocial contributors to pain post-breast cancer treatment (adapted from Explain Pain Supercharged [46]). The experience of pain is determined not only by the stimulation of tissues such as muscles or nerves (biological level), but also by how a person is feeling and thinking about the pain (psychological level) as well as one’s personal environment and how one feels supported within it (social level) [35]
Social factors influence pain. Here, social factors can be proximal (who you are with, your immediate relationships) and distal (the ‘social determinants’ of health). There are many studies that show immediate relationships affect pain [60, 61], but comparatively little is understood about the influence of one’s wider social context on pain-related outcomes. There are some data primarily centred on back pain [62] and back surgery outcomes [63]. Those data imply that the demonstrated effects of social determinants of health on other conditions also apply when it comes to pain. Finally, as is the case for musculoskeletal pain, consideration of social factors associated with post-cancer pain must also include the social impacts of living with persistent post-breast cancer pain.
Although the biopsychosocial model is well endorsed for cancer treatment itself [64], the dominant treatment approach for post-cancer pain remains biomedical; pharmacological approaches are often the first and only interventions offered in clinical practice [13–17]. This is surprising in light of the progress in treatment of cancer-related fatigue, which has shifted in the past decades to a comprehensive biopsychosocial framework [65, 66]. Non-pharmacological approaches, including exercise, activity management, psychosocial support and cognitive behavioural therapy, are widely recognized to be effective and important components of contemporary cancer-related fatigue management [65]. Although they are separate conditions, fatigue and pain have strikingly much in common [67, 68]: they are both potentially consuming feelings that urge self-protection and they commonly co-occur in many people living with and beyond cancer [69, 70]. In acute situations, pain and fatigue serve clear protective value, but as either condition persists, their protective value decreases, and they can become a primary cause of disability and other secondary problems. Remarkably, this understanding and established biopsychosocial approach for cancer-related fatigue are not (yet) adopted for management of post-(breast) cancer pain.
-
4.
The potentially powerful role of contemporary pain science education
One transformative learning from people with persistent musculoskeletal pain was that the very treatments that are most helpful—active and psychological therapies and self-management skills—make no sense if one understands pain to be an accurate reflection of the condition of the body [71]. This observation led to the development of a new psychoeducational intervention, which has become known as ‘pain science education’ (see also ‘explaining pain’ or ‘pain neuroscience education’). Over 25 clinical trials conducted over the last two decades have revealed the potentially powerful impact of pain science education. Two features differentiate pain science education from previous and alternative notions of pain education. First, contemporary pain education integrates foundational pain science discoveries within the educational content. This content differentiates from previous educational approaches, which focussed on education about cognitive and behavioural responses to pain, and the structural and functional anatomy of the painful body part (thereby reflecting the underlying structural-pathological model of pain). Contemporary approaches focus instead on understanding ‘how pain works’, including the biological basis of pain’s multifactorial, the notion of variable sensitivity and the ‘over-protective’ nature of persistent pain. Second, contemporary pain education is grounded in educational and learning science principles, moving away from didactic or ‘information provision’ approaches. It is also distinct from ‘cognitive therapy’ because it seeks to raise understanding of the biological processes underpinning pain rather than challenge negative patterns of thought about oneself or the world [72]. Relevant here is that the impetus for developing contemporary pain science education was in part the limitation of cognitive behavioural therapy in challenging unhelpful thoughts and behaviours. Indeed, empirical data clearly show that consumers, and clinicians, often conceptualise pain as a marker of the state of body tissues, which, as suggested earlier, renders a biopsychosocial approach to pain management non-sensical [71]. Meta-analyses show that pain science education has clinical benefit on pain, disability, pain catastrophizing and kinesiophobia in the short to medium term [73, 74]. Extensive empirical support of pain science education has led it to become a cornerstone treatment in musculoskeletal pain management [75, 76] and complex regional pain syndrome management [77] and it is now being integrated into pelvic pain [78] and osteoarthritis pain [79] management programs.
Pain science education has been defined elsewhere as ‘a range of educational interventions that aim to change one’s understanding of the biological processes that are thought to underpin pain’ [14]. That it is also grounded in educational and conceptual change science means that it necessarily progresses in line with those fields. Modern implementation of pain science education draws heavily on principles of self-regulated learning, participatory education and Bayesian learning. Learning objectives broadly cover the idea that pain is a marker of the perceived need to protect body tissue rather than a marker of tissue damage or disease.
Pain science education also applies the principles of deep learning, by targeting learning objectives related to pain biology, or ‘how pain works’, and thus reconceptualising the meaning of pain [14]. This approach is consistent with the common sense model of health—coping decisions will differ as a function of the meaning individuals assign to their symptoms (i.e. their illness representation) and this interpretive process will reflect their past illness experience, societal expectations and information from friends, media and medical practitioners [80]. By positioning the consumer as learner and taking a deep learning approach, pain science education promotes the consumer’s agency and autonomy, enabling and empowering them to evaluate treatment options and make optimal coping decisions.
At this moment, the potential role of education as part of pain care for cancer populations is already being recognized, but the results are underwhelming. This may be because up to now, the tested educational interventions take a biomedical approach to understanding pain. That these interventions show little effect in decreasing pain and disability, possibly increasing fear and anxiety [81–84], both of which also elevate pain and disability [85], mirrors discoveries made in the musculoskeletal field 20 years ago [86] and is therefore not surprising. The misconception—that pain provides an accurate marker of the state of body tissue—applies to persistent post-breast cancer pain just as it applies to persistent back pain. Moreover, this misconception is a dominant although a modifiable barrier to improving outcomes for the 19.5–21.8% of survivors who experience persisting pain and associated disability after cancer treatment [2, 3], just as it is for those who experience persistent back pain after an initial injury. Such comparisons suggest that, in relation to pain-related education, the cancer field is where musculoskeletal pain was over two decades ago. That is, in musculoskeletal pain, it has become clear that the content, delivery principles and strategies of pain education are critical, not just whether or not ‘education’ has occurred. We contend that the same is also likely here and that there is an urgent need to shift consumer and clinician expectations and community norms on what pain education for post-breast cancer pain should look like. At this stage, we suggest that contemporary pain science education provides the most likely candidate model.
The content of pain science education
To reconceptualise the meaning of pain, tailored, individualized education addressing the concepts that are relevant to that person with persistent pain should be provided. A recent mixed-method study in people who had recovered from a range of chronic pain states revealed three key concepts they considered to hold most value [87]. The first concept ‘Pain does not mean my body is damaged’ captures the importance of abandoning pre-existing ideas that pain indicates tissue damage. Second, ‘Thoughts, emotions and experiences affect pain’ captures the value of recognising multifactorial (biopsychosocial) influences on pain. And third, ‘I can retrain my over-protective pain system’ captures the importance of conceptualising persistent pain as a persistently heightened protective response that can be modified [87]. Although these key target concepts identified in non-cancer population certainly hold value in the post-breast cancer population as well, the complexity and unique characteristics of post-breast cancer pain limit simple transfer from the non-cancer population to the cancer population. As such, additional cancer-specific concepts might well be added, just as musculoskeletal-specific concepts (e.g. ‘an intervertebral disc can’t slip’) might be dropped. Tailoring pain science education to the cancer population will need to account for other comorbidities (for which a lot of biomedical information is provided by leaflets, books and the internet), serious unique biopsychosocial factors described earlier, the possible sequelae of cancer treatments and the already long and often intensive follow-up and after-care. Cancer-specific concepts that can be integrated with the key concepts drawn from clinical trials underway [88] that underpin pain science education are listed in Table 1.
Table 1.
Cancer-specific target concepts for pain science education for persistent post-breast cancer pain
| Cancer-specific target concept | Explanation/Content | Learning goals | Metaphor |
|---|---|---|---|
| Unusual sensations related to scars | The mechanisms involved in scar tissue formation, related sensations, psychological impact, and how to manage and soften scars are addressed [89] |
• Understanding that tissues heal in days/weeks Reinforcement/revisiting of the concept that the brain can produce pain without tissue damage • Introducing the idea that it is now safe (and beneficial) to move • Understanding how to manage and soften scars • Reframing every scar as a story of strength and survival |
‘The skill to heal: cuts heal fast’ ‘Move scars into stars’ |
| Damaged nerves send false danger messages | The mechanisms behind neuropathic pain (and related unusual sensations). This concept is relevant in the context of (painful and non-painful) neuropathies related to surgery, radiotherapy and chemotherapy [49] |
• Understanding the mechanisms behind neuropathic pain • Learning about and setting/updating expectations for recovery time (and implications for helpful or unhelpful strategies) |
‘Nerves heal slow, fuel the grow’ |
| Side effects related to radiotherapy | The mechanisms behind radiotherapy-related fibrosis and related sensations in radiated area are explained [50] |
• Skin and soft tissue effects of radiotherapy • Skin care and scar management following radiotherapy • Understanding flare-ups without re-injury |
‘From radiation to rehabilitation’ ‘Sunburn?’ |
| Side effects of hormone therapy | This session gives information about the mechanisms and side effects of hormone therapy and the role of the endocrine system in (persistent) pain [51, 52] |
• Explaining how these mechanisms can result in and explain unusual symptoms experienced • Importance of movement in managing hormone therapy–related arthralgia |
‘Don’t blame the hormones’ |
| (Physical) deconditioning due to cancer treatments | This session gives information about the toll that breast cancer treatments and inactivity can have on the body’s tolerance for exercise |
• General tips for getting started on becoming more active • Understanding some of the signs and symptoms that people might experience when resuming exercise |
‘Use it or lose it’ |
| Cancer-related fatigue | In case of cancer-related fatigue, this session offers an explanation on the mechanisms of cancer-related fatigue as sign of increased level of protection. [69, 70] |
• Practical strategies for becoming more active, adopting a ‘slow and steady wins the race’ approach • The importance of pacing and planning your activities • Tips and resources for setting goals and introduces the idea of energy-givers and energy-takers (and how to identify these on an individual basis) |
‘How to charge up your batteries’ |
| Living with pain-related uncertainty | Interpreting everyday aches and pains as a sign of cancer recurrence will substantially increase the threat value of pain [58, 59] |
• Beware over-monitoring daily aches and pain • Learning skills and strategies to manage these uncertainties |
‘In the shadow of the volcano’ |
Research agenda
We argue for new innovative collaborative programs that incorporate pain science education. To reduce the burden of post-cancer pain, we should benefit from shifting treatment away from patients as ‘passive therapy receivers’ towards patients enabled by contemporary understanding and empowered by proactive, psychological and self-management skills to master their situation and commence a pain recovery journey. We suggest that this will promote optimal treatment and coping decisions towards less pain, less pain-related disability and greater quality of life.
A pressing need is to establish both key cancer-specific learning objectives or concepts (see Table 1) that are valued by consumers, scientists and clinicians, as has been done in the past decades for the non-cancer pain field [87]. The effects on knowledge, participation, worry, pain and disability that have been established for pain science education in non-cancer pain populations should be tested in those with post-breast cancer pain. When testing these educational interventions, innovative, efficient methods that overcome current barriers to care in breast cancer survivors should be considered. Relevant here is that most cancer survivors are already burdened with long-term follow-up of medical surveillance, and many have limited access to rehabilitation settings and/or reimbursements. Furthermore, personal barriers including health literacy of the learner, their cultural background, their cancer-specific psychosocial needs and the possible underreporting of pain and other symptoms should be considered [90, 91]. With recent developments recognising the critical role of engagement and self-reflection in order to facilitate deep learning, a patient-centred educational approach with individually tailored information may well be needed [73]. Finally, a lesson still being learned in the musculoskeletal pain field is the critical need for adequate training of frontline health care professionals in contemporary pain science education and (after) care delivery. That knowledge growth does not fully capitalise into better care reminds us that health care professionals need knowledge, skills, confidence and support [92, 93]. Finally, that treatment is strongly influenced by consumer expectations implies that attention should also be given to community-level education strategies, for which there are important social considerations [94].
Innovation in delivery
One innovation that may be particularly suited to this population in light of the above is a digital approach for delivering pain science education. The COVID-19 pandemic has forced us to switch to digital health interventions (‘eHealth’) very quickly. The successful integration of digital health interventions in a sustainable way is now encouraged [95], also for pain management [96]. For digitally delivered pain science education, technologies using a conversational agent may offer benefit [97]. Some patients even prefer a digital agent over human practitioners [98] and may be significantly more willing to disclose to them information about themselves than in a clinical context [99]. This could prove to be particularly helpful for people with cancer as they are often reluctant to report pain due to stoicism [100] and fear of distracting medical practitioners from treating the underlying disease [101].
Conclusion
In summary, based on the lessons learned in the non-cancer pain field, pain science education seems a promising intervention approach that could help shift the traditional biomedical model of managing persisting pain after breast cancer, towards a biopsychosocial model. However, the complexity and specific characteristics of post-breast cancer pain warrant an extension and modification of the educational content typically addressed in non-cancer populations with cancer-specific learning objectives. Also, a digital approach may be valuable for this specific population. Learnings from two decades of pain science education in musculoskeletal pain may well lead to useful tools within both the clinician’s pain management skillset and the survivors’ self-management toolkit. We suspect that this will lead directly to better pain, function and quality of life outcomes of successful cancer treatment.
Author contribution
An De Groef: conceptualization, writing original draft
Mira Meeus: conceptualization, writing original draft
Lauren C. Heathcote: conceptualization, writing original draft
Louise Wiles: conceptualization, writing – reviewing and editing
Mark Catley: conceptualization, writing – reviewing and editing
Anna Vogelzang: conceptualization, writing – reviewing and editing
Ian Olver: conceptualization, writing – reviewing and editing
William B. Runciman: conceptualization, writing – reviewing and editing
Peter Hibbert: conceptualization, writing – reviewing and editing
Lore Dams: conceptualization, writing – reviewing and editing
Bart Morlion: conceptualization, writing – reviewing and editing
G. Lorimer Moseley: conceptualization, writing original draft
Declarations
Conflict of interest
In relation to this study, all authors declare no relevant financial relationships and have no relevant conflicts of interest to declare.
LCH has received advisory fees from Blue Note Therapeutics. BM received over the last 5 years fees for services for consultancy and/or speaker’s activities from Grünenthal, Lilly, Mundipharma, Pfizer, Krka, Ache, Sandoz, Shionogi, TEVA, GSK, Kyowa-Kirin, Boston Scientific and Reckitt and Benckiser. AV is employed as a part-time research assistant at Noigroup, a company that publishes Pain Science Education books and delivers professional courses in Pain Science Education. GLM has received support from Reality Health, ConnectHealth UK, Kaiser Permanente, AIA Australia, Workers’ Compensation Boards and professional sporting organisations in Australia, Europe, South and North America. Professional and scientific bodies have reimbursed him for travel costs related to presentation of research on pain and pain education at scientific conferences/symposia. He has received speaker fees for lectures on pain and pain education. He receives royalties for books on pain and pain education.
Footnotes
An De Groef, Mira Meeus and Lore Dams are members of the Improving Care in Edema and Oncology Research Group (https://www.caredon.org) and Pain in Motion International Research Group (https://www.paininmotion.be). An De Groef is a postdoctoral research fellow of the FWO-Flanders.
An De Groef and Mira Meeus share first authorship
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
An De Groef, Email: an.degroef@uantwerpen.be, https://www.caredon.org, https://www.paininmotion.be.
Mira Meeus, https://www.caredon.org, https://www.paininmotion.be.
Lore Dams, https://www.caredon.org, https://www.paininmotion.be.
References
- 1.Maajani K, et al. The global and regional survival rate of women with breast cancer: a systematic review and meta-analysis. Clin Breast Cancer. 2019;19(3):165–177. doi: 10.1016/j.clbc.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 2.van den Beuken-van Everdingen MH, et al. Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manage. 2016;51(6):1070–1090 e9. doi: 10.1016/j.jpainsymman.2015.12.340. [DOI] [PubMed] [Google Scholar]
- 3.Wang L, et al. Prevalence and intensity of persistent post-surgical pain following breast cancer surgery: a systematic review and meta-analysis of observational studies. Br J Anaesth. 2020;125(3):346–357. doi: 10.1016/j.bja.2020.04.088. [DOI] [PubMed] [Google Scholar]
- 4.Hamood R, et al. Chronic pain and other symptoms among breast cancer survivors: prevalence, predictors, and effects on quality of life. Breast Cancer Res Treat. 2018;167(1):157–169. doi: 10.1007/s10549-017-4485-0. [DOI] [PubMed] [Google Scholar]
- 5.Manfuku M, et al. Comparison of central sensitization-related symptoms and health-related quality of life between breast cancer survivors with and without chronic pain and healthy controls. Breast Cancer. 2019;26(6):758–765. doi: 10.1007/s12282-019-00979-y. [DOI] [PubMed] [Google Scholar]
- 6.Cohen SP, Vase L, Hooten WM. Chronic pain: an update on burden, best practices, and new advances. Lancet. 2021;397(10289):2082–2097. doi: 10.1016/S0140-6736(21)00393-7. [DOI] [PubMed] [Google Scholar]
- 7.Cieza A, et al. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2021;396(10267):2006–2017. doi: 10.1016/S0140-6736(20)32340-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858. [DOI] [PMC free article] [PubMed]
- 9.de Campos TF. Low back pain and sciatica in over 16s: assessment and management NICE Guideline [NG59] J Physiother. 2017;63(2):120. doi: 10.1016/j.jphys.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 10.Carville S, et al. Chronic pain (primary and secondary) in over 16s: summary of NICE guidance. BMJ. 2021;373:n895. doi: 10.1136/bmj.n895. [DOI] [PubMed] [Google Scholar]
- 11.Arden NK, et al. Non-surgical management of knee osteoarthritis: comparison of ESCEO and OARSI 2019 guidelines. Nat Rev Rheumatol. 2021;17(1):59–66. doi: 10.1038/s41584-020-00523-9. [DOI] [PubMed] [Google Scholar]
- 12.Foster NE, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet. 2018;391(10137):2368–2383. doi: 10.1016/S0140-6736(18)30489-6. [DOI] [PubMed] [Google Scholar]
- 13.Bennett MI, et al. Standards for the management of cancer-related pain across Europe—a position paper from the EFIC Task Force on Cancer Pain. Eur J Pain. 2019;23(4):660–668. doi: 10.1002/ejp.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization, WHO guidelines approved by the Guidelines Review Committee, in WHO guidelines for the pharmacological and radiotherapeutic management of cancer pain in adults and adolescents. 2018, World Health Organization 2018. [PubMed]
- 15.Fallon M, et al. Management of cancer pain in adult patients: ESMO Clinical Practice Guidelines. Ann Oncol. 2018;29(Suppl 4):p. iv166–iv191. doi: 10.1093/annonc/mdy152. [DOI] [PubMed] [Google Scholar]
- 16.Lyman GH, Bohlke K, Cohen L. Integrative therapies during and after breast cancer treatment: ASCO endorsement of the SIO Clinical Practice Guideline Summary. J Oncol Pract. 2018;14(8):495–499. doi: 10.1200/JOP.18.00283. [DOI] [PubMed] [Google Scholar]
- 17.Paice JA, et al. Management of chronic pain in survivors of adult cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2016;34(27):3325–3345. doi: 10.1200/JCO.2016.68.5206. [DOI] [PubMed] [Google Scholar]
- 18.Oldenmenger WH, et al. A systematic review of the effectiveness of patient-based educational interventions to improve cancer-related pain. Cancer Treat Rev. 2018;63:96–103. doi: 10.1016/j.ctrv.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 19.Deandrea S, et al. Prevalence of undertreatment in cancer pain. A review of published literature. Ann Oncol. 2008;19(12):1985–91. doi: 10.1093/annonc/mdn419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greco MT, et al. Quality of cancer pain management: an update of a systematic review of undertreatment of patients with cancer. J Clin Oncol. 2014;32(36):4149–4154. doi: 10.1200/JCO.2014.56.0383. [DOI] [PubMed] [Google Scholar]
- 21.van den Beuken-van Everdingen MHJ, et al. Treatment of pain in cancer: towards personalised medicine. Cancers (Basel). 2018;10(12)pii: cancers10120502. 10.3390/cancers10120502 [DOI] [PMC free article] [PubMed]
- 22.Grossman SA, et al. Correlation of patient and caregiver ratings of cancer pain. J Pain Symptom Manage. 1991;6(2):53–57. doi: 10.1016/0885-3924(91)90518-9. [DOI] [PubMed] [Google Scholar]
- 23.Strömgren AS, et al. Does the medical record cover the symptoms experienced by cancer patients receiving palliative care? A comparison of the record and patient self-rating. J Pain Symptom Manage. 2001;21(3):189–196. doi: 10.1016/S0885-3924(01)00264-0. [DOI] [PubMed] [Google Scholar]
- 24.Wiffen PJ, et al. Opioids for cancer pain - an overview of Cochrane reviews. Cochrane Database Syst Rev. 2017;7:Cd012592. doi: 10.1002/14651858.CD012592.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gouveia L, et al. Oncologists’ perception of depressive symptoms in patients with advanced cancer: accuracy and relational correlates. BMC Psychol. 2015;3(1):6. doi: 10.1186/s40359-015-0063-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Häuser W, et al. European* clinical practice recommendations on opioids for chronic noncancer pain - Part 1: role of opioids in the management of chronic noncancer pain. Eur J Pain. 2021;25(5):949–968. doi: 10.1002/ejp.1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abdel Shaheed C, et al. Efficacy, tolerability, and dose-dependent effects of opioid analgesics for low back pain: a systematic review and meta-analysis. JAMA Intern Med. 2016;176(7):958–968. doi: 10.1001/jamainternmed.2016.1251. [DOI] [PubMed] [Google Scholar]
- 28.Busse JW, et al. Opioids for chronic noncancer pain: a systematic review and meta-analysis. JAMA. 2018;320(23):2448–2460. doi: 10.1001/jama.2018.18472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Attal N, et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol. 2010;17(9):1113–e88. doi: 10.1111/j.1468-1331.2010.02999.x. [DOI] [PubMed] [Google Scholar]
- 30.Dworkin RH, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain. 2007;132(3):237–251. doi: 10.1016/j.pain.2007.08.033. [DOI] [PubMed] [Google Scholar]
- 31.Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129–36. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- 32.Weiss P. Adaptation. Ithaca: Cornell University Press; 1949. The biological basis of adaptation; pp. 1–22. [Google Scholar]
- 33.von Bertalanffy L. Problems of life. An evaluation of modern biological thought. AIBS Bull. 1952;2(5):14–14. doi: 10.1093/aibsbulletin/2.5.14-h. [DOI] [Google Scholar]
- 34.von Bertalanffy L. General system theory: foundations, development, applications. New York: George Braziller; 1969. [Google Scholar]
- 35.Loeser J. Concepts of pain, in chronic low-back pain. New York: Raven Press; 1982. [Google Scholar]
- 36.Graven-Nielsen T, Arendt-Nielsen L. Assessment of mechanisms in localized and widespread musculoskeletal pain. Nat Rev Rheumatol. 2010;6(10):599–606. doi: 10.1038/nrrheum.2010.107. [DOI] [PubMed] [Google Scholar]
- 37.Arendt-Nielsen L, et al. Assessment and manifestation of central sensitisation across different chronic pain conditions. Eur J Pain. 2018;22(2):216–241. doi: 10.1002/ejp.1140. [DOI] [PubMed] [Google Scholar]
- 38.Kosek E, et al. Do we need a third mechanistic descriptor for chronic pain states? Pain. 2016;157(7):1382–6. doi: 10.1097/j.pain.0000000000000507. [DOI] [PubMed] [Google Scholar]
- 39.Woolf CJ. What to call the amplification of nociceptive signals in the central nervous system that contribute to widespread pain? Pain. 2014;155(10):1911–1912. doi: 10.1016/j.pain.2014.07.021. [DOI] [PubMed] [Google Scholar]
- 40.Freynhagen R, et al. Current understanding of the mixed pain concept: a brief narrative review. Curr Med Res Opin. 2019;35(6):1011–1018. doi: 10.1080/03007995.2018.1552042. [DOI] [PubMed] [Google Scholar]
- 41.Madden VJ, et al. Variability in experimental pain studies: nuisance or opportunity? Br J Anaesth. 2021;126(2):e61–e64. doi: 10.1016/j.bja.2020.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zouikr I, Karshikoff B. Lifetime modulation of the pain system via neuroimmune and neuroendocrine interactions. Front Immunol. 2017;8:276–276. doi: 10.3389/fimmu.2017.00276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Apkarian AV, Baliki MN, Farmer MA. Predicting transition to chronic pain. Curr Opin Neurol. 2013;26(4):360–367. doi: 10.1097/WCO.0b013e32836336ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Woolf CJ. Evidence for a central component of post-injury pain hypersensitivity. Nature. 1983;306(5944):686–8. doi: 10.1038/306686a0. [DOI] [PubMed] [Google Scholar]
- 45.Moseley GL, Butler DS. Fifteen years of explaining pain: the past, present, and future. J Pain. 2015;16(9):807–13. doi: 10.1016/j.jpain.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 46.Butler DS, Lorimer Moseley G. Explain pain supercharged: the clinician’s manual. Adelaide City West: NOI Group Publishers; 2017. [Google Scholar]
- 47.Evenepoel M, et al. Pain Prevalence During Cancer Treatment: A Systematic Review and Meta-Analysis. J Pain Symptom Manage. 2022;63(3):e317–e335. doi: 10.1016/j.jpainsymman.2021.09.011. [DOI] [PubMed] [Google Scholar]
- 48.Stubblefield MD, Keole N. Upper body pain and functional disorders in patients with breast cancer. PM R. 2014;6(2):170–83. doi: 10.1016/j.pmrj.2013.08.605. [DOI] [PubMed] [Google Scholar]
- 49.Mulvey MR, et al. Neuropathic pain in cancer: systematic review, performance of screening tools and analysis of symptom profiles. Br J Anaesth. 2017;119(4):765–774. doi: 10.1093/bja/aex175. [DOI] [PubMed] [Google Scholar]
- 50.Straub JM, et al. Radiation-induced fibrosis: mechanisms and implications for therapy. J Cancer Res Clin Oncol. 2015;141(11):1985–94. doi: 10.1007/s00432-015-1974-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nahm N, Mee S, Marx G. Efficacy of management strategies for aromatase inhibitor-induced arthralgia in breast cancer patients: a systematic review. Asia Pac J Clin Oncol. 2018;14(6):374–382. doi: 10.1111/ajco.12845. [DOI] [PubMed] [Google Scholar]
- 52.Beckwee D, et al. Prevalence of aromatase inhibitor-induced arthralgia in breast cancer: a systematic review and meta-analysis. Support Care Cancer. 2017;25(5):1673–1686. doi: 10.1007/s00520-017-3613-z. [DOI] [PubMed] [Google Scholar]
- 53.Edwards RR, et al. Alteration in pain modulation in women with persistent pain after lumpectomy: influence of catastrophizing. J Pain Symptom Manag. 2013;46(1):30–42 13p. doi: 10.1016/j.jpainsymman.2012.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Boakye PA, et al. A critical review of neurobiological factors involved in the interactions between chronic pain, depression, and sleep disruption. Clin J Pain. 2016;32(4):327–36. doi: 10.1097/AJP.0000000000000260. [DOI] [PubMed] [Google Scholar]
- 55.Heathcote LC, Eccleston C. Pain and cancer survival: a cognitive-affective model of symptom appraisal and the uncertain threat of disease recurrence. Pain. 2017;158(7):1187–1191. doi: 10.1097/j.pain.0000000000000872. [DOI] [PubMed] [Google Scholar]
- 56.Tutelman PR, Heathcote LC. Fear of cancer recurrence in childhood cancer survivors: a developmental perspective from infancy to young adulthood. Psychooncology. 2020;29(11):1959–1967. doi: 10.1002/pon.5576. [DOI] [PubMed] [Google Scholar]
- 57.Heathcote LC, et al. Symptom appraisal in uncertainty: a theory-driven thematic analysis with survivors of childhood cancer. Psychol Health. 2021;36(10):1182–1199. doi: 10.1080/08870446.2020.1836180. [DOI] [PubMed] [Google Scholar]
- 58.Cho D, Chu Q, Lu Q. Associations among physical symptoms, fear of cancer recurrence, and emotional well-being among Chinese American breast cancer survivors: a path model. Support Care Cancer. 2018;26(6):1755–1761. doi: 10.1007/s00520-017-4010-3. [DOI] [PubMed] [Google Scholar]
- 59.Whitney CA, et al. Reminders of cancer risk and pain catastrophizing: relationships with cancer worry and perceived risk in women with a first-degree relative with breast cancer. Fam Cancer. 2019;18(1):9–18. doi: 10.1007/s10689-018-0082-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cunningham JL, et al. Associations between spousal or significant other solicitous responses and opioid dose in patients with chronic pain. Pain Med. 2012;13(8):1034–1039. doi: 10.1111/j.1526-4637.2012.01434.x. [DOI] [PubMed] [Google Scholar]
- 61.Newton-John TRO. Solicitousness and chronic pain: a critical review. Pain Rev. 2002;9(1):7–27. doi: 10.1191/0968130202pr186ra. [DOI] [Google Scholar]
- 62.Karran EL, Grant AR, Moseley GL. Low back pain and the social determinants of health: a systematic review and narrative synthesis. Pain. 2020;161(11):2476–2493. doi: 10.1097/j.pain.0000000000001944. [DOI] [PubMed] [Google Scholar]
- 63.Yap ZL, et al. The role of the social determinants of health in outcomes of surgery for low back pain. A systematic review and narrative synthesis. Spine J. 2021;pii: S1529-9430(21)01047-0. 10.1016/j.spinee.2021.11.013 [DOI] [PubMed]
- 64.Gudenkauf LM, Ehlers SL. Psychosocial interventions in breast cancer survivorship care. Breast. 2018;38:1–6. doi: 10.1016/j.breast.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 65.Fabi A, et al. Cancer-related fatigue: ESMO Clinical Practice Guidelines for diagnosis and treatment. Ann Oncol. 2020;31(6):713–723. doi: 10.1016/j.annonc.2020.02.016. [DOI] [PubMed] [Google Scholar]
- 66.Berger AM, et al. Cancer-related fatigue, version 2.2015. J Natl Compr Canc Netw. 2015;13(8):1012–39. doi: 10.6004/jnccn.2015.0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pedersen M. Chronic fatigue syndrome and chronic pain conditions – vitally protective systems gone wrong. Scand J Pain. 2019;19(4):651–657. doi: 10.1515/sjpain-2019-0072. [DOI] [PubMed] [Google Scholar]
- 68.Williams MT, Gerlach Y, Moseley L. The ‘survival perceptions’: time to put some Bacon on our plates? J Physiother. 2012;58(2):73–5. doi: 10.1016/S1836-9553(12)70085-1. [DOI] [PubMed] [Google Scholar]
- 69.Bjerkeset E, Röhrl K, Schou-Bredal I. Symptom cluster of pain, fatigue, and psychological distress in breast cancer survivors: prevalence and characteristics. Breast Cancer Res Treat. 2020;180(1):63–71. doi: 10.1007/s10549-020-05522-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lee L, et al. Symptom clusters in breast cancer survivors: a latent class profile analysis. Oncol Nurs Forum. 2020;47(1):89–100. doi: 10.1188/20.ONF.89-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Moseley L. Unraveling the barriers to reconceptualization of the problem in chronic pain: the actual and perceived ability of patients and health professionals to understand the neurophysiology. J Pain. 2003;4(4):184–9. doi: 10.1016/S1526-5900(03)00488-7. [DOI] [PubMed] [Google Scholar]
- 72.Fordham B, et al. Cognitive-behavioural therapy for a variety of conditions: an overview of systematic reviews and panoramic meta-analysis. Health Technol Assess. 2021;25(9):1–378. doi: 10.3310/hta25090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Watson JA, et al. Pain neuroscience education for adults with chronic musculoskeletal pain: a mixed-methods systematic review and meta-analysis. J Pain. 2019;20(10):11401–114022. doi: 10.1016/j.jpain.2019.02.011. [DOI] [PubMed] [Google Scholar]
- 74.Tegner H, et al. Neurophysiological Pain Education for Patients With Chronic Low Back Pain: A Systematic Review and Meta-Analysis. Clin J Pain. 2018;34(8):778–786. doi: 10.1097/AJP.0000000000000594. [DOI] [PubMed] [Google Scholar]
- 75.Corp N, et al. Evidence-based treatment recommendations for neck and low back pain across Europe: a systematic review of guidelines. Eur J Pain. 2021;25(2):275–295. doi: 10.1002/ejp.1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Lin I, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2020;54(2):79–86. doi: 10.1136/bjsports-2018-099878. [DOI] [PubMed] [Google Scholar]
- 77.Goebel A, et al. Standards for the diagnosis and management of complex regional pain syndrome: results of a European Pain Federation Task Force. Eur J Pain. 2019;23(4):641–651. doi: 10.1002/ejp.1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Vandyken C, Mdt C, Hilton S. The puzzle of pelvic pain: a rehabilitation framework for balancing tissue dysfunction and central sensitization II a review of treatment considerations. J Women’s Health Phys Ther. 2012;36:4T 54. [Google Scholar]
- 79.Stanton TR, Karran EL, Bennell K, Hill C, Moseley GL, Butler D, Cocks T. Does targeting pain-related beliefs in people with knee osteoarthritis increase physical activity? A pilot, feasibility trial. 2018; Available from: https://www.anzctr.org.au/AnzctrAttachments/375526-PROTOCOL_EP%20FOR%20KNEE%20OA_FINAL.pdf.
- 80.Leventhal H, et al. Health psychology: the search for pathways between behavior and health. Annu Rev Psychol. 2008;59:477–505. doi: 10.1146/annurev.psych.59.103006.093643. [DOI] [PubMed] [Google Scholar]
- 81.Hirsch MS, Liebert RM. The physical and psychological experience of pain: the effects of labeling and cold pressor temperature on three pain measures in college women. Pain. 1998;77(1):41–48. doi: 10.1016/S0304-3959(98)00080-3. [DOI] [PubMed] [Google Scholar]
- 82.Maier-Riehle B, Härter M. The effects of back schools–a meta-analysis. Int J Rehabil Res. 2001;24(3):199–206. doi: 10.1097/00004356-200109000-00005. [DOI] [PubMed] [Google Scholar]
- 83.Nachemson AL. Newest knowledge of low back pain. A critical look. Clin Orthop Relat Res. 1992;279:8–20. doi: 10.1097/00003086-199206000-00003. [DOI] [PubMed] [Google Scholar]
- 84.Poiraudeau S, et al. Fear-avoidance beliefs about back pain in patients with subacute low back pain. Pain. 2006;124(3):305–311. doi: 10.1016/j.pain.2006.04.019. [DOI] [PubMed] [Google Scholar]
- 85.Morr S, et al. Quality of information concerning cervical disc herniation on the Internet. Spine J. 2010;10(4):350–354. doi: 10.1016/j.spinee.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 86.Moseley GL, Nicholas MK, Hodges PW. A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clin J Pain. 2004;20(5):324–30. doi: 10.1097/00002508-200409000-00007. [DOI] [PubMed] [Google Scholar]
- 87.Leake HB, et al. What do patients value learning about pain? A mixed-methods survey on the relevance of target concepts after pain science education. Pain. 2021;162(10):2558–2568. doi: 10.1097/j.pain.0000000000002244. [DOI] [PubMed] [Google Scholar]
- 88.De Groef A, et al. EduCan trial: study protocol for a randomised controlled trial on the effectiveness of pain neuroscience education after breast cancer surgery on pain, physical, emotional and work-related functioning. BMJ Open. 2019;9(1):e025742. doi: 10.1136/bmjopen-2018-025742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Cohen BE, et al. The role of elastic fibers in scar formation and treatment. Dermatol Surg. 2017;43(Suppl 1):S19–s24. doi: 10.1097/DSS.0000000000000840. [DOI] [PubMed] [Google Scholar]
- 90.Orhan C, et al. Development of culturally sensitive pain neuroscience education for first-generation Turkish patients with chronic pain: a modified Delphi study. Musculoskelet Sci Pract. 2019;39:1–9. doi: 10.1016/j.msksp.2018.10.007. [DOI] [PubMed] [Google Scholar]
- 91.Edward J, et al. The importance and impact of patients’ health literacy on low back pain management: a systematic review of literature. Spine J. 2018;18(2):370–376. doi: 10.1016/j.spinee.2017.09.005. [DOI] [PubMed] [Google Scholar]
- 92.Arumugam V, et al. Attitudes, knowledge and behaviors related to evidence-based practice in health professionals involved in pain management. Int J Evid Based Healthc. 2018;16(2):107–118. doi: 10.1097/XEB.0000000000000131. [DOI] [PubMed] [Google Scholar]
- 93.Ng W, et al. Barriers and enablers influencing healthcare professionals’ adoption of a biopsychosocial approach to musculoskeletal pain: a systematic review and qualitative evidence synthesis. Pain. 2021;162(8):2154–2185. doi: 10.1097/j.pain.0000000000002217. [DOI] [PubMed] [Google Scholar]
- 94.Karran EL, et al. Pain and pain management experiences following spinal cord injury - a mixed methods study of Australian community-dwelling adults. Disabil Rehabil. 2022; p 1–14. [DOI] [PubMed]
- 95.Turolla A, et al. Musculoskeletal physical therapy during the COVID-19 pandemic: is telerehabilitation the answer? Phys Ther. 2020;100(8):1260–1264. doi: 10.1093/ptj/pzaa093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tauben DJ, et al. Optimizing telehealth pain care after COVID-19. Pain. 2020;161(11):2437–2445. doi: 10.1097/j.pain.0000000000002048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Laranjo L, et al. Conversational agents in healthcare: a systematic review. J Am Med Inform Assoc. 2018;25(9):1248–1258. doi: 10.1093/jamia/ocy072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhou S, et al. Agent-User Concordance and Satisfaction with a Virtual Hospital Discharge Nurse. in Intelligent Virtual Agents. 2014. Cham: Springer International Publishing.
- 99.Lucas GM, et al. It’s only a computer: virtual humans increase willingness to disclose. Comput Hum Behav. 2014;37:94–100. doi: 10.1016/j.chb.2014.04.043. [DOI] [Google Scholar]
- 100.Mah K, et al. Do correlates of pain-related stoicism and cautiousness differ in younger and older people with advanced cancer? J Pain. 2018;19(3):301–316. doi: 10.1016/j.jpain.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 101.Saifan A, et al. Patient–and family caregiver–related barriers to effective cancer pain control. Pain Manag Nurs. 2015;16(3):400–410. doi: 10.1016/j.pmn.2014.09.007. [DOI] [PubMed] [Google Scholar]