Abstract
Comorbid symptoms such as post-traumatic stress and pain are common barriers to optimal self-management among veterans with type 2 diabetes. Additionally, self-management behaviors occur in the context of veterans’ daily routines and social environments. This study evaluated the feasibility and acceptability of ecological momentary assessment (EMA) among veterans with type 2 diabetes. Ten veterans with type 2 diabetes were asked to respond to random EMA surveys during preprogrammed intervals five times per day for 14 days. EMA surveys were delivered via a mobile application and assessed momentary physical location, activities, social interactions, mood, stress, and pain. The last survey of each day included additional items about daily post-traumatic stress symptoms, diabetes distress, social support, physical activity, self-management behaviors, and functioning. Participants completed interviews assessing their experience in the study and barriers to responding and indicated their likelihood of participating in similar studies. The mean survey response rate was 96%, providing 675 observations. The majority of participants completed the five momentary surveys in <1 minute and the daily EMA surveys in <5 minutes. Results revealed substantial individual day-to-day variability across symptoms and self-management behaviors that is not captured by aggregated means across all participants. Participants generally reported enjoying responding to surveys and experiencing few barriers. Nine of 10 participants reported being “extremely likely” to participate in a similar study. These pilot data suggest that intensive EMA designs are feasible and acceptable for veterans with type 2 diabetes and can inform the design of future larger studies.
The prevalence of diabetes among veterans is nearly 25%, or about double that in the general population (1). Even after adjusting for age and other demographic factors, diabetes is more common in veterans than in civilians (1). Diabetes outcomes are substantially improved when patients engage in regular self-management behaviors such as getting physical activity, taking prescribed medications, following dietary recommendations, and monitoring blood glucose levels (2). However, many veterans with type 2 diabetes do not engage in consistent self-management (3). Therefore, a more granular understanding is needed of veteran-specific barriers to daily engagement in diabetes self-management behaviors, such as comorbid symptoms and social context.
Symptoms of comorbid medical and mental health conditions represent one set of barriers to daily engagement in diabetes management of particular relevance to the veteran population, which is characterized by high comorbidity rates (4). Suboptimal type 2 diabetes management is often asymptomatic, yet it is a leading cause of cardiovascular disease, kidney disease, blindness, and amputations in the long term (5). However, many veterans with type 2 diabetes have at least one comorbid condition that is more symptomatic than diabetes (e.g., pain) (4). While symptoms of common comorbid conditions such as depressed mood, stress, and pain garner more attention from patients, they also have been associated with poor functioning in type 2 diabetes (6–8). Although type 2 diabetes self-management can benefit comorbid condition symptoms, these behaviors often become a low priority (6,9).
Social context is another source of potential barriers or facilitators to daily diabetes management that is especially pertinent to veterans, who may have more limited social networks compared with civilians (10). Social support has been associated with more engagement in diabetes self-management behaviors for veterans (11). Research among civilians suggests that social support is positively associated with target blood glucose levels, better mood, and quality of life (12). Conversely, those with low social support have higher symptoms of depression and functional disability (13), all of which may be barriers to daily diabetes self-management.
The majority of prior research in this area has involved cross-sectional studies of between-person relationships between retrospective reports of diabetes self-management behavior and global indicators of hypothesized barriers to daily engagement. Conversely, there has been little research on the moment-to-moment associations between comorbid condition symptoms, other psychological states, social support, and daily engagement in type 2 diabetes self-management behaviors. That is, while evidence exists for these cross-sectional associations at the between-person level, few studies have examined links between comorbid condition symptoms and daily diabetes self-management within an individual over time.
Given that diabetes self-management activities take place primarily outside of medical visits and in the context of individuals’ daily physical and social environments, more work is needed to capture and model within-person variability in diabetes self-management using ecologically valid methods that sample daily life. A handful of daily diary studies have shown that various social contextual factors are positively related to diabetes self-management behaviors (14–16), but none have focused on the veteran population, and these studies, such as one by Khan et al. (14), have typically focused on daily occurrences and events rather than momentary factors. Thus, understanding how daily barriers to diabetes self-management actually unfold within and across an individual’s everyday life is crucial to developing person-centered interventions designed to improve diabetes outcomes for veterans.
Real-world, ambulatory assessment methods, such as ecological momentary assessment (EMA) can build on past cross-sectional and daily diary work to understand the dynamics of daily diabetes self-management behaviors and psychosocial factors of veterans with type 2 diabetes. EMA is a mobile health technology that assesses mood, behavior, and environmental factors in the moment in participants’ own physical and social contexts, where barriers to self-management occur. Whereas daily diary methods typically involve a single daily assessment wherein participants report on events of the day, EMA typically involves multiple within-day assessments that are more focused on momentary states and behaviors (17). A 2021 review (18) found few published studies using EMA methodology to assess diabetes self-management and contextual factors. Of the 10 studies included in the review, only two focused on type 2 diabetes (vs. type 1 diabetes) (18). Since this review was published, additional conference abstracts and study protocols have examined the use of EMA to assess self-management among people with type 2 diabetes in the general population (19–21), underscoring the emerging interest in and the need for best practices and standardized measures when using this methodology.
Given the limited prior EMA studies to examine psychosocial and contextual barriers to self-management in adults with type 2 diabetes and the lack of prior studies in the high-risk veteran population, additional work is needed to understand the feasibility and acceptability of these methods and the utility of included measures to inform the design of future studies. Thus, the primary aim of this study was to pilot test an EMA protocol to assess the feasibility and acceptability of EMA assessment among veterans with type 2 diabetes who are treated through the VA health care system. We also assessed the utility of our EMA survey items among veterans with type 2 diabetes by examining the between-person versus the within-person variability of our study measures.
Research Design and Methods
Participants
Veterans with type 2 diabetes were recruited for a pilot research study from a list of participants who previously participated in diabetes research at a Southern California VA health care system. Participants were required to have a diagnosis of type 2 diabetes as confirmed by electronic health record (EHR) review, own a smartphone, be ≥18 years of age, and understand to and respond in English. Of 19 participants screened, 16 were eligible and 10 agreed to participate. Only one of the 19 participants screened did not own a smartphone. One participant had type 1 diabetes, two were not interested, and six were interested but not available for our data collection window (e.g., because they were going to be out of town). Participants were screened until we met our target sample size (N = 10). The study was approved by the health care systems institutional review board, and participants provided informed consent. This article was prepared according to the standard Checklist for Reporting EMA Studies (22).
Procedures
All EMA survey questions were programmed using the LifeData platform, a Web-based program for creating mobile assessments that can be downloaded to smartphones via the associated RealLife Exp mobile application (app) and does not require consistent internet access. Participants completed informed consent and a brief research visit/instruction session either virtually or in person before beginning a single 14-day EMA period. Data collection occurred between 7 October and 23 October 2020.
After consent, a research assistant helped eligible participants download the app to their personal smartphones and access the study protocol. All EMA survey questions were reviewed with participants during the instruction session. Participants were given a 24-hour trial period to further familiarize themselves with the protocol and troubleshoot any issues with the study team. The protocol delivered momentary surveys containing up to nine items through an app notification five times a day randomly within preprogrammed 2-hour intervals between 8:00 a.m. and 8:00 p.m. for each of the 14 days. Daily end-of-the-day surveys containing up to 24 items were delivered once daily in combination with the last momentary survey. Participants were given up to three reminder notifications for each survey until they completed it. Participants had 90 minutes from the notification time to respond to each survey, after which time the survey expired. A research assistant also called each participant after 7 days to assess barriers to participation and answer any questions.
Participants were compensated up to $150 in VA canteen coupons based on their survey response rate. The compensation schedule was discussed with participants during the instruction session, and coupons were mailed to participants after they completed the study. Participants received $10 for completing the instruction session, $1 for each momentary EMA survey, and $2 for each end-of-day survey (encompassing the last momentary EMA survey and daily EMA survey). Participants received an additional $20 for a 75% survey response rate and an additional $22 for a 100% response rate.
Measures
Feasibility
Feasibility was assessed by survey response rate, with an average response rate >80% (completion of 56 of 70 possible EMA surveys) as a target. We also assessed time to complete surveys and number of reminders before responses.
Acceptability
Participants were asked to respond to four open-ended questions and one Likert-scale question about their experiences completing the EMA surveys via individual interview with a research assistant. These questions included “What did you like?,” “What did you not like?,” “What made it difficult to respond to questions?,” “What did you think about the number of questions? Too many?,” “What other feedback or suggestions do you have for us?,” and “Would you be willing to participate in a future similar study?” (with the latter ranked on a scale from 1 = unlikely to 5 = extremely likely). The interviewer probed for clarification as necessary and took detailed notes of each participant’s response, including direct quotations.
Demographic and Medical Characteristics
Participants’ demographic information including, age, sex, race, and ethnicity, was obtained through self-report for a previous study. Medical information, including A1C, BMI, mental health diagnoses, and chronic pain diagnoses, was obtained from participants’ EHR.
EMA Momentary Survey Items
EMA momentary surveys focused on constructs expected to fluctuate throughout a day, including activities, comorbid symptoms, and social and physical contexts. Specifically, these included:
Daily activities. Participants responded to the question “What are you doing?” using a list of possible daily activities (e.g., watching TV, physical activity/exercise, or working). If participants selected “other,” they could type in a free-text response. Subscales were created based on conceptually grouped activities adapted from Moore et al. (23).
Physical activities. If participants selected “physical activity/exercise” from the options above, they were asked to indicate “What type of physical activity/exercise?” Response choices included running/jogging, walking, weightlifting/strength training, using cardiovascular equipment, bicycling, or other (free-text response) (24).
Comorbid symptoms. Participants were asked to rate their current mood (depressed, happy, or anxious), stress, and pain levels on a 0–10 Likert scales. For example, for “I feel depressed,” 0 = not at all to 10 = extremely.
Social context. Participants were asked to indicate who they were currently with (e.g., spouse) using a dropdown menu (25) and the number of social interactions, with the question, “Since the last alarm, how many times did you socialize with someone else (e.g., spent more than 5 minutes talking/communicating with someone else)?” (23). In light of coronavirus disease 2019 (COVID-19) restrictions, participants were instructed to include virtual contact (i.e., phone or video).
Physical context. Participants indicated their current location by answering, “Where are you right now?” using a dropdown menu of 13 options adapted from Moore et al. (23) (e.g., “at hospital” or “at my home”).
EMA Daily Survey Measures
EMA daily surveys focused on constructs expected to fluctuate on a day-to-day basis, including post-traumatic stress symptoms (PTSS), diabetes distress, diabetes-related support, self-management behaviors, health-related functioning, and diabetes-related quality of life. Specifically, these included:
PTSS. These symptoms were assessed using four items corresponding to each of the post-traumatic stress disorder symptom clusters: re-experiencing, avoidance, negative cognitions and mood, and arousal (26). Participants indicated how much they were bothered by each item from 0 = not at all to 10 = extremely, through questions such as “Avoiding thoughts, activities, or feelings related to a traumatic event?” Participants were instructed to select “0” if they had never experienced a traumatic event.
Diabetes distress. Daily diabetes distress was assessed using an item adapted from the 17-item Diabetes Distress Scale (27): “Today, how overwhelmed have you felt by the demands of diabetes?” Participants rated the item from 0 = not at all to 10 = extremely. This item was selected because it has the highest correlation with total scores from the full Diabetes Distress Scale (28).
Diabetes-related support. This was assessed with three items about participants’ diabetes-related interactions with others. One item was from a prior study protocol: “When a problem related to your diabetes condition arose, to what extent did someone else help you solve it?” (21), rated from 0 = not at all to 10 = extremely. Two items were developed for the current study and included, “Did you talk to someone about your diabetes today?” (yes/no) and, if yes was selected, “How helpful was that person?” rated from 0 = not at all helpful to 10 = very helpful.
Diabetes self-management behaviors. These behaviors were assessed with the Summary of Diabetes Self-Care Activities measure (29), modified for daily use (21), by replacing the question asking how many were performed in “the last 7 days” with “today.” Self-management behaviors assessed included dietary behaviors, physical activity, exercise, blood glucose monitoring, foot care, medication-taking, and smoking. We also included two questions adapted for daily use from the Diabetes Self-Management Questionnaire (30). These included “Did you take your recommended insulin injections today?” (yes/no/not taking insulin) and “Did you eats lots of sweets or other foods rich in carbohydrates today?”
Health-related functioning. This was assessed using items from the Diabetes Quality of Life Clinical Trial Questionnaire (31), adapted for daily use. Three items were selected as a balance between capturing overall health-related quality of life and functioning and minimizing participant burden. These included, “Today, how would you say your health is?” rated from 0 = poor to 10 = excellent; “How much difficulty did you have doing your daily work because of your physical health or emotional problems today?” rated from 0 = none at all to 5 = could not do daily work; and “Compared to others your age, were your social activities more or less limited because of your physical health today?” rated from 0 = much less limited to 4 = much more limited.
Diabetes-related quality of life. This was assessed using an item from the Diabetes Quality of Life Clinical Trial Questionnaire (31), modified for daily use: “How satisfied are you with the amount of time it took to manage diabetes today?” rated from 0 = very dissatisfied to 5 = very satisfied.
Data Analysis
Data analysis was performed using the statistical software SPSS v. 27 (32) and Mplus v. 8.5 (33). Descriptive statistics were computed to characterize the sample with respect to demographic and medical characteristics and study constructs. Descriptive statistics were also used to assess the feasibility and acceptability indicators. To examine the proportion of the total variance in each EMA survey item attributable to between-person differences versus within-person (i.e., day-to-day) variability, we computed intraclass correlation coefficients (ICCs). Responses to open-ended interview questions were summarized and reviewed multiple times by two study authors to identify patterns among responses.
Results
Participant Characteristics
On average, participants were about 54 years of age (SD 4.2 years) and were mostly male veterans (80%), the majority of whom identified as White (70%), with an annual income ≥$30,000 (70%) and a bachelor’s or graduate/professional degree (60%). Time since being diagnosed with diabetes ranged from 5.9 to 28.8 years (mean 9.8, SD 6.9 years). The average BMI was 32.9 kg/m2 (SD 6.3 kg/m2), falling into the obese range. Mean A1C was 7.2% (SD 1.8%), indicating blood glucose levels close to the standard target of <7.0% (34). The average systolic blood pressure was 130 mmHg (SD 16 mmHg), and the average diastolic blood pressure was 76 mmHg (SD 6 mmHg), with most participants falling in the elevated or stage 1 hypertension range. Per EHR, 60% of participants were using insulin, 70% were taking metformin, and 30% were taking an additional oral diabetes medication. Furthermore, 80% had a chronic pain diagnosis, and 60% had at least one mental health diagnosis.
Feasibility
Participants reported no difficulties after the 24-hour trial period or at the 1-week check-in. In total, 700 prompts were delivered to participants, and no participants dropped out.
The mean response rate across all participants was 96% (range 90–100%), providing a total of 675 EMA observations, with no significant difference between the first 7 days of participation (mean 96%, SD 20.2%) and the second 7 days of study participation (mean 96%, SD 20.4%) (t[698] = 0.05, P = 0.957). The response rate was significantly higher on weekdays (mean 97%, SD 18.1%) than on weekends (mean 94%, SD 24.7%) (t[698] = 1.83, P <0.001). Response rate was not significantly correlated with age, time since diabetes diagnosis, A1C, blood pressure, or mean ratings of stress, mood, and diabetes distress.
Most participants responded to EMA surveys after the initial notification (67.3%), followed by after the first reminder (18.8%), after the second reminder (7.2%), and after the third reminder (6.7%). Participants responded to prompts after an average of 12 minutes, 8 seconds (SD 17 minutes, 42 seconds), after the notification. More than half (57.9%) of the momentary surveys were completed in <1 minute (mean 1.30 minutes, SD 2.30 minutes), and most (76.3%) end-of-day surveys were completed in <5 minutes (mean 5.42 minutes, SD 8.52 minutes).
Acceptability
In open-ended interview questions, participants generally reported enjoying participation and the opportunity to reflect on their mood throughout the day. Three participants specifically stated that survey items reminded them about self-management behaviors, including medication, diet, and foot care. Participants reported encountering very few barriers to engaging in study protocols. Most participants (80%) said that the lengths of EMA momentary and end-of-day surveys were reasonable; however, two participants reported that the end-of-day survey was too long. Two participants said they would be willing to answer additional questions. Two participants said the questions did not fit into their waking hours and suggested custom time windows.
Participants provided additional suggestions for including a question about hypoglycemic episodes, additional activities such as outdoor labor, and more reminder alarms. One participant asked if she could share her results with her diabetes health care team. One participant reported that the allowable response time was adequate when a prompt was sent during exercising and a response could not be sent immediately. Several participants (80%) mentioned that survey items helped them be more aware of their moods or behaviors. Nine participants reported that they would be “extremely likely” to participate in a similar study, and the remaining participant reported being “likely” to participate.
Descriptive Statistics for EMA Survey Items
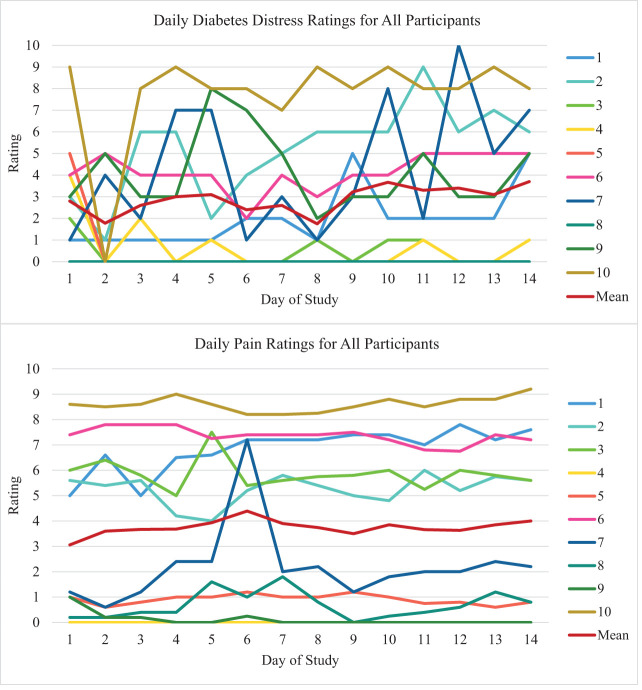
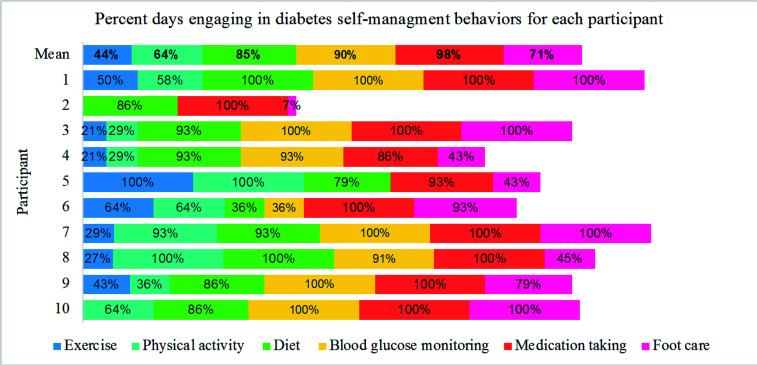
Descriptive statistics for EMA survey items are presented in Table 1. Results show that participants spend most of their time in sedentary behaviors (60.3%) and spend over one-third of their time alone (37.5%). On average, participants reported speaking to someone about diabetes 41% of days; one participant never reported talking to someone about diabetes during the 14 days, and another endorsed doing so on all 14 days, with the remaining participants endorsing the item on 10–80% of days). Of note, only five participants ever endorsed currently engaging in physical activity. Individual variability of two example comorbid symptoms (diabetes distress and pain) compared with the means across all participants is shown in Figure 1. This figure depicts a substantial amount of intraindividual (within-person) day-to-day variability across symptoms that is not captured by means across all participants. Figure 2 shows engagement in diabetes self-management behaviors for each participant compared with the mean percentage of engagement across all participants, indicating that individual patterns of engagement in self-management behaviors are not captured by the mean.
Table 1.
Descriptive Statistics for EMA Survey Items
| Variables | Data Points, n | Mean ± SD or % | Observed Range | ICC |
|---|---|---|---|---|
| Daily symptom ratings | ||||
| Happy | 669 | 6.40 ± 2.33 | 0–10 | 0.67 |
| Depressed | 669 | 2.87 ± 2.91 | 0–10 | 0.84 |
| Anxious | 669 | 3.18 ± 3.17 | 0–10 | 0.86 |
| Stress | 669 | 3.40 ± 3.19 | 0–10 | 0.79 |
| Pain | 669 | 3.79 ± 3.29 | 0–10 | 0.92 |
| Diabetes distress | 135 | 2.90 ± 2.93 | 0–10 | 0.74 |
| PTSS | 135 | 1.32 ± 1.19 | 0–4 | 0.84 |
| Where are you? | 669 | |||
| At home | 79.4 | — | ||
| Work | 6.7 | — | ||
| In vehicle | 4.3 | — | ||
| Outside walking | 3.4 | — | ||
| Other | 6.0 | — | ||
| What are you doing? | 669 | |||
| Sedentary activities | 60.3 | — | ||
| Eating or preparing food | 13.0 | — | ||
| Instrumental activities of daily living | 11.7 | — | ||
| Intellectual activities | 10 | — | ||
| Physical activities | 3.6 | — | ||
| Social activities | 1.5 | — | ||
| Who are you with? | 669 | |||
| Alone | 37.5 | — | ||
| Spouse or partner | 33.5 | — | ||
| Friends | 4.0 | — | ||
| Other family members | 7.2 | — | ||
| Pets | 30 | — | ||
| Health care provider | 0.3 | — | ||
| Other known or unknown | 8.2 | — | ||
| Number of daily interactions | 669 | 1.36 ± 1.23 | 0–4 | 0.34 |
| Extent someone helped with a diabetes problem? | 135 | 5.44 ± 3.65 | 0–10 | 0.74 |
| Talked with someone about diabetes today? | 135 | 41.5 | 0.29 | |
| How helpful was that person? | 56 | 7.49 ± 1.91 | 2–10 | 0.36 |
| Diabetes quality of life | 135 | 2.96 ± 1.00 | 0–4 | 0.63 |
| Limitations because of physical health or emotional problems | 135 | 2.55 ± 1.26 | 1–5 | 0.71 |
| Social activities limited because of physical health? | 135 | 2.73 ± 1.20 | 1–5 | 0.76 |
| Today, how would you say your health is? | 135 | 5.73 ± 2.71 | 0–10 | 0.95 |
| Diabetes self-management* | ||||
| Followed a healthful eating plan | 135 | 85.5 | 0.20 | |
| Ate five or more fruits and vegetables | 135 | 44.4 | 0.44 | |
| Ate high-fat foods | 135 | 29.6 | 0.08 | |
| Ate sweets and carbohydrates | 135 | 11.1 | 0.40 | |
| Participated in physical activity | 135 | 57.0 | 0.36 | |
| Participated in exercise | 135 | 35.6 | 0.32 | |
| Monitored blood glucose | 135 | 66.7 | 0.84 | |
| Monitored blood glucose as recommended | 135 | 71.9 | 0.83 | |
| Checked feet | 135 | 71.1 | 0.46 | |
| Took medication | 135 | 98.5 | NA | |
| Took insulin | 82 | 100 | NA | |
| Smoked even one cigarette | 135 | 10.4 | NA |
Diabetes self-management responses are reported as the mean percentage of days participants reported carrying out each item. NA, not applicable. ICC could not be computed due to low variability.
Figure 1.
Daily diabetes distress (top) and daily pain (bottom) ratings for each of the 10 participants, as well as the daily mean for all participants, across the 14-day study period. Diabetes distress and pain were each rated on a 0–10 scale.
Figure 2.
Percentage of 14 study days on which selected diabetes self-management behaviors were endorsed by each study participant (N = 10 individuals), as well as the mean percentage of days each item was reported for all participants. Exercise = “Did you participate in a specific exercise session (such as swimming, walking, biking) other than what you do around the house or as part of your work today?” Physical activity = “Did you participate in at least 30 minutes of physical activity today (total minutes of continuous activity, including walking)?” Diet = “Have you followed a healthful eating plan today?” Blood glucose monitoring = “Did you test your blood sugar the number of times recommended by your health care provider today?” Foot care = “Did you check your feet today?”
Discussion
We aimed to pilot test our EMA protocol and questions to determine the feasibility and acceptability of EMA assessment among veterans with type 2 diabetes. Given the paucity of prior work examining daily diabetes self-management using EMA or similar methods, we also sought to describe the within-person versus between-person variability of our EMA measures to assess the utility of EMA for examining our key constructs. Our results suggest that EMA among veterans with type 2 diabetes is feasible and acceptable. Our results also demonstrate substantial within-person variability in many study measures, including mood, social interactions, diabetes distress, and self-management behaviors, that is not captured by between-person means.
The response rates of EMA surveys were high, suggesting that the number of reminders delivered, compensation schedule, and degree of participant burden are appropriate for this population. Thus, we recommend providing incentives to participants based on their response rates for observational EMA studies. However, for a treatment study, use of financial incentives needs more careful consideration, as this strategy could serve as an intervention in and of itself.
Although within the range of typical EMA studies, our relatively wide 90-minute window for participants to respond to EMA prompts may have contributed to our high response rate. However, most participants responded after the initial prompt and in <15 minutes, suggesting that participants were generally able to respond quickly and to notifications. Participant interviews reported in Langer et al. (35) suggest that, from the perspective of adult community members, 45 minutes may be too short and 60–90 minutes might be more ideal. However, most standard approaches to modeling EMA data assume that intervals between observations are equal both across time and across participants; thus, wider time windows between EMA surveys can decrease analytic precision. Therefore, in this population, a response window closer to 60 minutes might be a more ideal balance among participant preference, survey response rate, and statical assumptions.
Participants found the study procedures and questions acceptable, and all reported being willing to participate in a similar future study. They were generally able to complete EMA surveys in a relatively short time period, also suggesting a low burden. We are unaware of norms or standards for survey completion times in the EMA literature, but time to complete our momentary surveys was similar to one study that reported it took 1.15 minutes on average for participants to complete randomly administered EMA surveys (36).
We found that smartphone ownership is common in this population, and many participants are familiar with smartphone technology. In addition to being cost-effective, allowing participants to use their own devices may increase survey response rates, as it does not require participants to carry multiple devices or learn how to navigate a new device.
In this study, EMA measures included both general mood, activity, and social interaction variables similar to those administered in prior EMA studies in other samples (16,18), and diabetes-specific measures that are more novel and exploratory given the few prior EMA studies in this population. Several negative affect variables (e.g., depressed and anxious) that were measured five times per day varied much more from person to person than they did from moment to moment within individual participants. Alternately, diabetes self-management behaviors had more within-person (day-to-day) variability than between-person variability. To better understand how to support and improve upon an individual patient’s diabetes management, these day-to-day fluctuations in diabetes self-management and their psychosocial and behavioral correlates are precisely what must be studied in future research. This pilot study supports future studies with larger between-person samples to examine the relationships between daily comorbid symptoms, social interactions, and diabetes self-management behaviors.
Measurement reactivity is an important consideration in all EMA studies (25). Of particular concern in the current study is the participant feedback that questions about self-management behaviors served as reminders to engage in the behaviors on the same day. Future studies may consider constructing items to reflect engagement in behaviors before the prompt rather than “today.” Another consideration is to use open-ended questions or participant-initiated responses to assess daily diabetes self-management behaviors. In addition to providing objective measures of behaviors, passive measures such as blinded accelerometers and continuous blood glucose monitoring (37,38) may reduce measurement reactivity compared with self-report. We had very few responses to our physical activity items, as participants were only prompted to view these questions if they were currently engaging in physical activity. Participants’ feedback that they were less likely to respond while engaging in physical activity, combined with the low frequency of physical activity in this population, suggested that alternative items would better capture this behavior. For example, items asking participants about physical activity that had occurred since that last alarm would better identify activity type and frequency and could be matched with accelerometer data (25). Finally, while a concern in the current study, the reported measurement reactivity suggests that interventions providing reminders at opportune times may help participants increase engagement in diabetes self-management behaviors.
Another challenge when designing EMA studies is the limited availability of previously validated EMA measures (39), and researchers often rely on adapted or abbreviated versions of validated scales. For example, social support is a broad construct with many subdomains, which is difficult to capture with only one to three EMA items. Additionally, there is a distinction between perceived and actual (or enacted) support; perceived support involves beliefs about the availability or reliability of support resources should needs arise, whereas actual support involves the actual receipt of those resources (40). Although most prior work in diabetes uses self-report measures of global perceived support from others, the daily life context of an EMA study is an ideal opportunity to assess actual social support exchanges in real-time with greater precision than a one-time survey of global perceptions (41). In the current study, we selected three EMA items intended to tap both aspects of actual support (i.e., asking participants if someone helped them solve a diabetes-related problem or if they talked to anyone about diabetes) and perceived support (i.e., asking participants how helpful they felt it was) specifically around diabetes management, based on our interest in understanding barriers to daily diabetes self-management. However, future studies may aim to focus more on the emotional aspects of social support or support in broader domains, for which other EMA items may be better suited.
Our study had limitations. The small sample size (N = 10), which produced 675 unique data points, was selected as appropriate for a pilot study (42,43) and to inform larger studies that may examine relationships between study variables. All participants in our small veteran sample had similar survey response rates; however, our results may not generalize to the larger veteran population. Differences in response rates based on demographic and medical characteristics should be examined in future studies. Although it did not come up in our interviews, participants may have been confused by our question “How helpful was that person?” if they talked to more than one person about diabetes. Additionally, our study was conducted during COVID-19 restrictions and may not represent veterans with type 2 diabetes outside of this context. For example, participants may have had more availability to respond to EMA surveys. Use of biological measures such as continuous glucose monitoring, heart rate variability, and salivary cortisol levels may further elucidate relationships among psychosocial factors, self-management behaviors, and health outcomes. Future research may also consider more in-depth qualitative interviews.
Conclusion
EMA is feasible and acceptable for veterans with type 2 diabetes and can provide nuanced information about within-person dynamics. Real-time assessment tools developed through EMA can inform clinical decision-making and treatment planning that considers barriers to self-management that occur outside of medical appointments. This research can also be used to develop adaptive, patient-centered mHealth interventions to supplement in-person treatment or as stand-alone interventions.
Article Information
Acknowledgments
This project was supported by the VA San Diego Center of Excellence for Stress and Mental Health. J.S.W. is supported by the VA Office of Academic Affairs Advanced Fellowship in Women’s Health. N.A. is partially supported by grant R01DK106415 from the National Institute of Diabetes and Digestive and Kidney Diseases.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
J.S.W. was responsible for study conceptualization and acquisition and primary analysis of the data and wrote the first draft of the manuscript. E.C.S. contributed to writing the manuscript and data analysis and reviewed/edited the manuscript. D.E.H. contributed to collecting data and reviewed/edited the manuscript. N.A. contributed to the study conceptualization and acquisition of the data and reviewed/edited the manuscript. J.S.W. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1. Eibner C, Krull H, Brown KM, et al. Current and projected characteristics and unique health care needs of the patient population served by the Department of Veterans Affairs. Rand Health Q 2016;5:13. [PMC free article] [PubMed] [Google Scholar]
- 2. Powers MA, Bardsley J, Cypress M, et al. Diabetes self-management education and support in type 2 diabetes: a joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Care 2015;38:1372–1382 [DOI] [PubMed] [Google Scholar]
- 3. Lynch CP, Strom JL, Egede LE. Variation in quality of care indicators for diabetes in a national sample of veterans and non-veterans. Diabetes Technol Ther 2010;12:785–790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pentakota SR, Rajan M, Fincke BG, et al. Does diabetes care differ by type of chronic comorbidity? An evaluation of the Piette and Kerr framework. Diabetes Care 2012;35:1285–1292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Centers for Disease Control and Prevention . National Diabetes Statistics Report, 2020: Estimates of Diabetes and Its Burden in the United States. Available from https://www.cdc.gov/diabetes/data/statistics/statistics-report.html. Accessed 31 July 2020
- 6. Butchart A, Kerr EA, Heisler M, Piette JD, Krein SL. Experience and management of chronic pain among patients with other complex chronic conditions. Clin J Pain 2009;25:293–298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Molsted S, Tribler J, Snorgaard O. Musculoskeletal pain in patients with type 2 diabetes. Diabetes Res Clin Pract 2012;96:135–140 [DOI] [PubMed] [Google Scholar]
- 8. Krein SL, Heisler M, Piette JD, Butchart A, Kerr EA. Overcoming the influence of chronic pain on older patients’ difficulty with recommended self-management activities. Gerontologist 2007;47:61–68 [DOI] [PubMed] [Google Scholar]
- 9. Lehavot K, Hoerster KD, Nelson KM, Jakupcak M, Simpson TL. Health indicators for military, veteran, and civilian women. Am J Prev Med 2012;42:473–480 [DOI] [PubMed] [Google Scholar]
- 10. Campbell SB, Gray KE, Hoerster KD, Fortney JC, Simpson TL. Differences in functional and structural social support among female and male veterans and civilians. Soc Psychiatry Psychiatr Epidemiol 2021;56:375–386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gray KE, Hoerster KD, Reiber GE, Bastian LA, Nelson KM. Multiple domains of social support are associated with diabetes self-management among veterans. Chronic Illn 2019;15:264–275 [DOI] [PubMed] [Google Scholar]
- 12. Strom JL, Egede LE. The impact of social support on outcomes in adult patients with type 2 diabetes: a systematic review. Curr Diab Rep 2012;12:769–781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Levy M, Deschênes SS, Burns RJ, Elgendy R, Schmitz N. Trajectories of social support in adults with type 2 diabetes: associations with depressive symptoms and functional disability. Int J Geriatr Psychiatry 2019;34:480–487 [DOI] [PubMed] [Google Scholar]
- 14. Khan CM, Stephens MAP, Franks MM, Rook KS, Salem JK. Influences of spousal support and control on diabetes management through physical activity. Health Psychol 2013;32:739–747 [DOI] [PubMed] [Google Scholar]
- 15. Stephens MAP, Franks MM, Rook KS, Iida M, Hemphill RC, Salem JK. Spouses’ attempts to regulate day-to-day dietary adherence among patients with type 2 diabetes. Health Psychol 2013;32:1029–1037 [DOI] [PubMed] [Google Scholar]
- 16. Zajdel M, Helgeson VS, Seltman HJ, Korytkowski MT, Hausmann LRM. Daily communal coping in couples with type 2 diabetes: links to mood and self-care. Ann Behav Med 2018;52:228–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mehl MR, Conner TS, Csikszentmihalyi M, Eds. Handbook of Research Methods for Studying Daily Life. New York, Guilford Press, 2012 [Google Scholar]
- 18. Nam S, Griggs S, Ash GI, et al. Ecological momentary assessment for health behaviors and contextual factors in persons with diabetes: a systematic review. Diabetes Res Clin Pract 2021;174:108745. [DOI] [PubMed] [Google Scholar]
- 19. Sorinao E, Laurenceau J-P. Visible and invisible spousal support in daily diabetes self-care [Abstract]. Diabetes 2020;69:735-P [Google Scholar]
- 20. Jonas VH, Fishman SR, Sears M, et al. Qualitative results from adults with type 2 diabetes using the MyDay smartphone app [Abstract]. Diabetes 2020;69:55-LB [Google Scholar]
- 21. Lüscher J, Kowatsch T, Boateng G, Santhanam P, Bodenmann G, Scholz U. Social support and common dyadic coping in couples’ dyadic management of type II diabetes: protocol for an ambulatory assessment application. JMIR Res Protoc 2019;8:e13685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Liao Y, Skelton K, Dunton G, Bruening M. A systematic review of methods and procedures used in ecological momentary assessments of diet and physical activity research in youth: an adapted STROBE checklist for reporting EMA Studies (CREMAS). J Med Internet Res 2016;18:e151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Moore RC, Kaufmann CN, Rooney AS, et al. Feasibility and acceptability of ecological momentary assessment of daily functioning among older adults with HIV. Am J Geriatr Psychiatry 2017;25:829–840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Dunton GF, Liao Y, Kawabata K, Intille S. Momentary assessment of adults’ physical activity and sedentary behavior: feasibility and validity. Front Psychol 2012;3:260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dunton GF, Liao Y, Intille S, Huh J, Leventhal A. Momentary assessment of contextual influences on affective response during physical activity. Health Psychol 2015;34:1145–1153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Erwin MC, Dennis PA, Coughlin LN, Calhoun PS, Beckham JC. Examining the relationship between negative affect and posttraumatic stress disorder symptoms among smokers using ecological momentary assessment. J Affect Disord 2019;253:285–291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Polonsky WH, Fisher L, Earles J, et al. Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care 2005;28:626–631 [DOI] [PubMed] [Google Scholar]
- 28. Fisher L, Glasgow RE, Mullan JT, Skaff MM, Polonsky WH. Development of a brief diabetes distress screening instrument. Ann Fam Med 2008;6:246–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Toobert DJ, Hampson SE, Glasgow RE. The Summary of Diabetes Self-Care Activities Measure: results from 7 studies and a revised scale. Diabetes Care 2000;23:943–950 [DOI] [PubMed] [Google Scholar]
- 30. Schmitt A, Gahr A, Hermanns N, Kulzer B, Huber J, Haak T. The Diabetes Self-Management Questionnaire (DSMQ): development and evaluation of an instrument to assess diabetes self-care activities associated with glycaemic control. Health Qual Life Outcomes 2013;11:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Shen W, Kotsanos JG, Huster WJ, Mathias SD, Andrejasich CM, Patrick DL. Development and validation of the Diabetes Quality of Life clinical trial questionnaire. Med Care 1999;37(Suppl Lilly):AS45–AS66 [DOI] [PubMed] [Google Scholar]
- 32. Corp IBM. IBM SPSS Statistics for Windows, version 27. Armonk, NY, IBM Corp., 2020 [Google Scholar]
- 33. Muthén LK, Muthén BO. Mplus User’s Guide. 8th ed. Los Angeles, CA, Muthén & Muthén, 2017 [Google Scholar]
- 34. American Diabetes Association . 6. Glycemic targets: Standards of Medical Care in Diabetes—2021. Diabetes Care 2021;44(Suppl. 1):S73–S84 [DOI] [PubMed] [Google Scholar]
- 35. Langer SL, Ghosh N, Todd M, et al. Usability and acceptability of a smartphone app to assess partner communication, closeness, mood, and relationship satisfaction: a mixed methods approach. JMIR Form Res 2020;4:e14161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Yang C, Linas B, Kirk G, et al. Feasibility and acceptability of smartphone-based ecological momentary assessment of alcohol use among African American men who have sex with men in Baltimore. JMIR Mhealth Uhealth 2015;3:e67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Junghaenel DU, Stone AA. Ecological momentary assessment for the psychosocial study of health. In The Wiley Encyclopedia of Health Psychology. Sweeny K, Robbins ML, Cohen LM, Eds. Hoboken, NJ, Wiley & Sons, 2020, p. 105–112 [Google Scholar]
- 38. Soriano EC, Lenhard JM, Gonzalez JS, et al. Spousal influence on diabetes self-care: moderating effects of distress and relationship quality on glycemic control. Ann Behav Med 2021;55:123–132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bolger N, Laurenceau J. Intensive Longitudinal Methods: An Introduction to Diary and Experience Sampling Research. New York, Guilford Press, 2013 [Google Scholar]
- 40. Gottlieb BH, Bergen AE. Social support concepts and measures. J Psychosom Res 2010;69:511–520 [DOI] [PubMed] [Google Scholar]
- 41. Song Y, Nam S, Park S, Shin IS, Ku BJ. The impact of social support on self-care of patients with diabetes: what is the effect of diabetes type? Systematic review and meta-analysis. Diabetes Educ 2017;43:396–412 [DOI] [PubMed] [Google Scholar]
- 42. Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health 2008;31:180–191 [DOI] [PubMed] [Google Scholar]
- 43. Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: getting started and moving on from stage I. Clin Psychol (New York) 2001;8:133–142 [Google Scholar]