Abstract
Inertial measurement units (IMUs) can be used to monitor running biomechanics in real-world settings, but IMUs are often used within a laboratory. The purpose of this scoping review was to describe how IMUs are used to record running biomechanics in both laboratory and real-world conditions. We included peer-reviewed journal articles that used IMUs to assess gait quality during running. We extracted data on running conditions (indoor/outdoor, surface, speed, and distance), device type and location, metrics, participants, and purpose and study design. A total of 231 studies were included. Most (72%) studies were conducted indoors; and in 67% of all studies, the analyzed distance was only one step or stride or <200 m. The most common device type and location combination was a triaxial accelerometer on the shank (18% of device and location combinations). The most common analyzed metric was vertical/axial magnitude, which was reported in 64% of all studies. Most studies (56%) included recreational runners. For the past 20 years, studies using IMUs to record running biomechanics have mainly been conducted indoors, on a treadmill, at prescribed speeds, and over small distances. We suggest that future studies should move out of the lab to less controlled and more real-world environments.
Keywords: biomechanics, wearable devices, injury, running conditions
1. Introduction
Wearable technology has been adopted among sports science researchers and practitioners to capture movement in the conditions in which sports take place [1]. Inertial measurement units (IMUs) are a type of wearable technology that can be used to measure running biomechanics [2]. The use of IMUs for real-world monitoring of running biomechanics may provide insights that are different from observations in controlled conditions [3,4,5]. Historically, the space and computational costs of onboard data storage and processing have created challenges for long-term monitoring of running biomechanics [2]. However, as device capabilities and approaches to big data have improved, the large amounts of data produced by IMUs have changed from a liability to an opportunity for real-world running biomechanical analyses.
While several editorials and commentaries have indicated the capability of IMUs to study running biomechanical gait patterns out of the laboratory and recommend that investigators do so [2,3,4,6,7], these suggestions were not based on systematic evidence. Therefore, we do not know how many studies are using IMUs to record running biomechanics and in which settings. In 2018, a systematic review identified only 14 studies that used wearables for running gait analysis for distances greater than 200 m [8]. As the use of wearables is a trending topic in the field of running biomechanics, we expect the number of studies that analyze running gait using IMUs in real-world settings to dramatically increase.
Thus, the purpose of this review is to systematically identify the scope of how IMUs are used to record running biomechanics in all settings. Our primary focus is on the conditions (i.e., location, surface, speed, and distance) in which IMUs capture running quality. Our secondary objectives were to identify the devices and sensors used, the calculated metrics and analyses from the IMU signals, the characteristics of the participants in the studies, and the study details such as the purpose and study design. By identifying the scope of IMU-based running biomechanical studies, we aim to mark the progress made and the steps that remain for analyzing running gait in real-world settings.
2. Materials and Methods
2.1. Registration
The review protocol was registered through the Open Science Framework on 24 August 2020 (https://osf.io/gsmvj/?view_only=cc97d0034c5341bca4ac181878770ec7, accessed on 16 February 2022).
2.2. Eligibility Criteria
This review was designed to capture all journal articles that used IMUs to assess gait quality during running, published in English since 2001. Exclusion criteria were: not original research article (e.g., review papers, conference proceedings, and dissertations); the study did not involve human subjects; the study did not involve running; running quality was analyzed as part of another athletic task (e.g., change of direction and playing a team sport); only spatiotemporal variables were analyzed (e.g., speed, cadence, and step length); there was no use of IMUs; the sole purpose of the study was the use of IMUs for any purpose other than gait analysis; the study primarily focused on development of new technology or methods rather than gait analysis; and running was only with the use of robotic orthoses, exoskeletons, or virtual reality environments.
2.3. Search Strategy
The search was executed in the scientific databases CINAHL, Embase, HealthSTAR, MEDLINE, PsycINFO, PubMed, SPORTDiscus and Web of Science. Databases were searched for articles related to IMUs and running using the following terms and logic: (Wearable Electronic Devices/OR Accelerometry/OR wearable* OR inertial sensor* OR inertial measurement unit* OR imu OR imus OR gyroscope* OR magnetometer* OR acceleromet*) AND (Running/OR running OR jogging), where/indicates a MESH term and * indicates the search term can have any ending. The final search was conducted on 24 April 2021.
2.4. Study Selection
One author (LCB) searched each database, combined the resulting records from each database, and performed initial screening for duplicates, format, and language. The records that passed initial screening were uploaded to an online review management platform (Covidence, Melbourne, Australia). Two authors (LCB and AMR) screened the title and abstract of all records for eligibility, with one author (CAC) serving as the tiebreaker. One author (LCB) obtained and uploaded the full text of the records that passed the title and abstract screening. The full-text review was conducted by two authors (LCB and AMR), and the reason for exclusion was indicated for articles deemed ineligible. In the case where multiple exclusion criteria were relevant, the criterion highest in the list above was chosen. One author (CAC) served as the tiebreaker for conflicts on whether an article should be included or excluded as well as conflicts on the selected reason for exclusion.
2.5. Data Extraction
Each included study was assigned to an author (LCB, AMR, and CAC) who extracted data related to the study, participants, conditions, device(s), and analysis.
2.5.1. Conditions
Location
Categorized as: indoor, outdoor, or indoor and outdoor.
Running Surface
Categorized as: track, pavement or sidewalk, grass (includes real or artificial), trail (includes gravel), treadmill, floor or platform, or not controlled.
Speed
Categorized as: exact (minimum speed of 1.67 m/s except for incremental runs that started with walking but ended with running; recorded in units of m/s), relative—calculated (based on a race time or a specific test [e.g., VO2max and heart rate]), relative—subjective (self-selected or based on participant interpretation [e.g., maximal, slow, and moderate]), and not controlled (races or training runs).
Full Distance or Duration
For each surface, the complete distance or duration was calculated by multiplying the distance or duration by the number of trials and number of days and reported using units from the study. Exceptions for using the reported units for the full distance or duration include more than 180 s (converted to minutes) and more than 5000 m (converted to km).
Analyzed Distance
For each surface, the amount of IMU data analyzed was categorized as: single step or stride per trial for one or more trials, consecutive steps for less than 200 m per trial for one or more trials, consecutive steps over 200 m to 1000 m per trial for one or more trials, consecutive steps over more than 1000 m for one trial, consecutive steps over more than 1000 m for multiple trials. A trial was a repeated run on the same or different course, or a repeated or different segment run on the same or different days. If not provided, the analyzed distance was calculated from the reported speed. If only the number of steps or insufficient information was reported for determining the analyzed distance, equivalences between 200 m, 60 s, and 150 steps/min were used—200 m in 60 s corresponds with a speed of 3.33 m/s, which is a common intermediate running speed [9,10], and 150 steps/min is on the low end of preferred running cadence [11,12,13,14], representing a low threshold of number of steps that equates to 200 m.
2.5.2. Device(s)
Brand and Model
As reported.
Device Location(s)
Categorized as: foot (any portion of foot or shoe), shank (includes tibia/shin, calf, ankle), thigh, lower back (includes pelvis, lumbar spine), upper back (includes thoracic, cervical spine), chest, arm (includes wrist), head. If multiple devices were placed on the same location (e.g., both feet), the location was only recorded once.
Sensors
The number of axes were recorded for each type of sensor: Accelerometer, gyroscope, magnetometer.
2.5.3. Analysis
Statistical Approach
Categorized as: descriptive, inferential, or machine learning. Descriptive was only used when it was the only type of analysis performed. Machine learning was included only when it was used as part of the statistical approach and not to generate metrics (e.g., estimated ground reaction forces from accelerations using an artificial neural network).
Metrics
Categorized as: vertical/axial magnitude (e.g., peak and RMS), anterior–posterior magnitude (e.g., peak and RMS), medial–lateral magnitude (e.g., peak, RMS), resultant magnitude (e.g., peak and RMS), axis ratio (e.g., axis RMS/resultant RMS), variability—any axis (e.g., SD and CV), loading rate, power, PlayerLoad, shock attenuation—time domain, shock attenuation—frequency domain, frequency content, spectral power or spectral energy, stiffness, joint angles or ROM, joint angular velocity, segment rotation, segment rotation velocity, COM displacement (e.g., bounce, oscillation, and trajectory), COM change in velocity (e.g., braking), symmetry or regularity (based on autocorrelation of signal), stability (e.g., Lyapunov exponent), or entropy. Due to the large number of studies investigating shock absorption using an accelerometer placed on the tibia, when the axis for tibial acceleration magnitude was not specified, it was assumed to be vertical. For other situations where the axis of acceleration magnitude was not reported, it was assumed to be the resultant.
2.5.4. Participants
Sex
Females, males, or females and males.
Type
Non-runner (includes sedentary, adults, recreational team sport athletes), recreational runner (described as a runner; includes runners with defined weekly mileage, well-trained runners), and competitive runner (competes at a high level; includes elite, member of a collegiate or higher sports team).
Injury Status
Injured or uninjured.
Age
The central tendency and variability of age were recorded across all participant types. If the study only reported age for each participant group, the overall mean age was calculated.
2.5.5. Study Details
Country
Based on ethics approval, or if not reported, the first author’s first affiliation.
Study Design
Randomized controlled trial, quasi-experimental, case study, case series, case control, prospective cohort, retrospective cohort, or cross-sectional.
Purpose
Equipment intervention, training intervention, validity or reliability of metric(s), compare metrics, compare groups, identify changes due to fatigue, identify changes between sessions, identify changes between conditions, associate with injury or associate with performance. Some studies had multiple purposes.
2.6. Quality Assessment
A formal quality assessment was not part of this scoping review. However, we evaluated the amount of information reported (adequate or lacking) and the relevance to running and IMUs (appropriate or not appropriate) for each set of data extracted (study, participants, conditions, device(s), and analysis) of each study.
3. Results
3.1. Study Selection
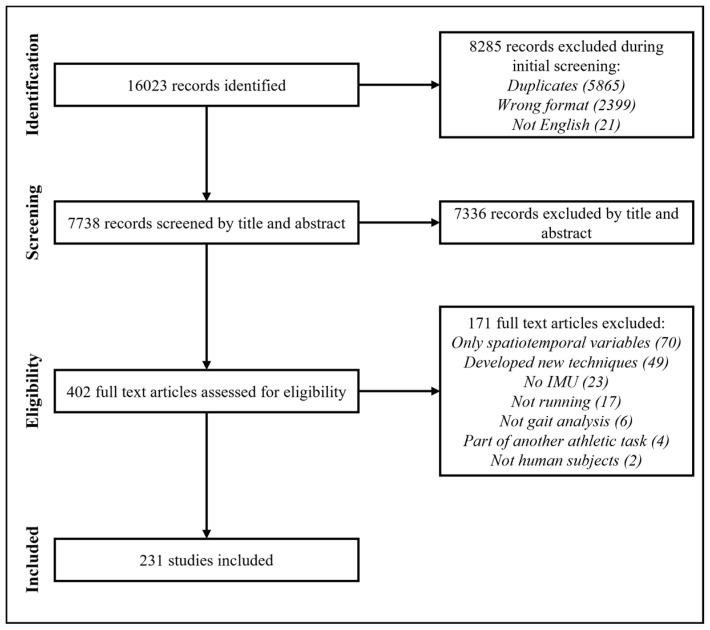
A total of 16,023 records were identified across all databases (Figure 1) and 7336 records were excluded during title and abstract screening. Of the 402 full-text articles that were assessed, 171 were excluded and 231 studies met all eligibility criteria and were included.
Figure 1.
Flowchart of the study selection process.
3.2. Data Extraction
The complete data extracted for each included study are reported as an appendix. The conditions, devices, analysis, participants, and study details are summarized here with key details provided in Table 1, Table 2, Table 3, Table 4, Table 5 and Table 6.
Table 1.
Study characteristics where the analyzed distance is one step/stride.
| Ref. | Author | Year | Location | Surface | Speed | Distance/Duration | Type | Number (Sex) | Overall Age | Metric(s) |
|---|---|---|---|---|---|---|---|---|---|---|
| [15] | Aubol, et al. | 2020 | Indoor | Floor | 3.0 m/s | 30 m | Rec. | 19 (10 F, 9 M) | Mean: 31; SD: 6 | VT, Res. |
| [16] | Blackah, et al. | 2013 | Indoor | Treadmill | 3.83 m/s | 2 min | Rec. | 9 (0 F, 9 M) | Mean: 19; SD: 1 | VT, Shock-time, Shock-frequency |
| [17] | Boyer and Nigg | 2006 | Indoor | Floor | 3 m/s | 320 m | Non | 5 (0 F, 5 M) | Mean: 24.6; SD: 2.5 | VT, Shock-frequency |
| [18] | Chadefaux, et al. | 2019 | Indoor | Floor | 3.1 m/s | 175 m | Rec. | 10 (0 F, 10 M) | Mean: 21; SD: 3 | VT, AP, ML, Res., Freq. |
| [19] | Clansey, et al. | 2012 | Indoor | Floor | 4.5 m/s | 270 m | Rec. | 21 (0 F, 21 M) | Mean: 36.2; SD: 12.5 | VT, Loading Rate |
| [20] | Crowell and Davis | 2011 | Indoor | Floor | 3.7 m/s | 230 m | Rec. | 10 (6 F, 4 M) | Mean: 26; SD: 7 | VT, Loading Rate |
| [21] | Edwards, et al. | 2019 | Indoor | Floor | 3.3., 5.0, and 6.7 m/s | ≥450 m | Comp. | 10 (0 F, 10 M) | Mean: 21; SD: 2 | VT |
| [22] | Gil-Rey, et al. | 2021 | Indoor | Track | incremental from 1.69 m/s | ≥40 min | Non | 82 (82 F, 0 M) | Mean: 59.1; SD: 5.4 | VT, AP, ML |
| [23] | Hagen, et al. | 2009 | Indoor | Floor | 3.3 m/s | NR | Rec. | 20 (0 F, 20 M) | Mean: 32; SD: 10 | VT |
| [24] | Havens, et al. | 2018 | Indoor | Floor | self-selected | 90 m | Non | 14 (7 F, 7 M) | Mean: 29; SD: 12 | VT |
| [25] | Higgins, et al. | 2021 | Indoor | Floor | self-selected | 368 m | Non | 30 (15 F, 15 M) | Mean: 23.0; SD: 4.5 | VT, Res. |
| [26] | Lam, et al. | 2018 | Indoor | Floor | 3.0 and 6.0 m/s | 230 m | Comp. | 18 (0 F, 18 M) | Mean: 25.0; SD: 2.3 | VT |
| [27] | Laughton, et al. | 2003 | Indoor | Floor | 3.7 m/s | ≥57 m | Rec. | 15 (NS) | Mean: 22.46; SD: 4 | VT |
| [28] | Mavor, et al. | 2020 | Indoor | Floor | self-selected | 30 m | Non | 18 (9 F, 9 M) | Mean: 23.7; SD: 3.44 | Joint ROM |
| [29] | Meinert, et al. | 2016 | Indoor | Floor | 2.9 m/s | 30 m | Rec. | 20 (0 F, 20 M) | Mean: 22.7; SD: 2.9 | VT, Res., Shock-frequency, Spectral Energy |
| Indoor | Treadmill | 2.9 m/s | 10 s | |||||||
| [30] | Mercer, et al. | 2005 | Indoor | Floor | comfortable, faster, slower | 800 m | Non | 6 (NS) | Mean: 26; SD: 4.0 | VT, Shock-time |
| [31] | Milner, et al. | 2020 | Indoor | Floor | 3.0 m/s | ≥30 m | Rec. | 19 (10 F, 9 M) | Mean: 31; SD: 6 | VT, AP, ML, Res., Seg. Rot. |
| [32] | Milner, et al. | 2006 | Indoor | Floor | 3.7 m/s | 115 m | Rec. | 40 (40 F, 0 M) | Mean: 26; SD: 9 | VT |
| [33] | Nedergaard, et al. | 2018 | Indoor | Floor | 2, 3, 4, and 5 m/s | ≥64 m | Non | 20 (0 F, 20 M) | Mean: 22; SD: 4 | Res. |
| [34] | Ogon, et al. | 2001 | Indoor | Floor | slow | 144 m | Non | 12 (5 F, 7 M) | Mean: 32.9; SD: 7.9 | Loading Rate |
| [35] | Rowlands, et al. | 2012 | Indoor | Floor | self-selected | 320 m | Non | 10 (5 F, 5 M) | Mean: 29.4; SD: 7.3 | VT, Res., Loading Rate |
| [36] | Sayer, et al. | 2020 | Indoor | Floor | 2.8–3.2 m/s | NR | Non | 64 (64 F, 0 M) | Mean: 13.7; SD: 2.3 | VT, AP |
| [37] | Sinclair and Dillon | 2016 | Indoor | Floor | 4 m/s | 110 m | Rec. | 12 (0 F, 12 M) | Mean: 23.59; SD: 2 | VT, Loading Rate |
| [38] | Sinclair and Sant | 2017 | Indoor | Floor | 4 m/s | NR | Non | 13 (0 F, 13 M) | Mean: 27.81; SD: 7.02 | VT, Loading Rate |
| [39] | Sinclair, et al. | 2016 | Indoor | Floor | 4 m/s | NR | Rec. | 12 (0 F, 12 M) | Mean: 23.11; SD: 5.01 | VT, Loading Rate |
| [40] | Sinclair, et al. | 2015 | Indoor | Floor | 4 m/s | 110 m | Rec. | 12 (12 F, 0 M) | Mean: 21.45; SD: 2.98 | VT, Loading Rate |
| [41] | Sinclair, et al. | 2017 | Indoor | Grass | 4 m/s | NR | Comp. | 12 (0 F, 12 M) | Mean: 22.47; SD: 1.13 | VT |
| [42] | Thompson, et al. | 2016 | Indoor | Floor | self-selected | 450 m | Rec. | 10 (5 F, 5 M) | Mean: 26; SD: 7.3 | Res. |
| [43] | Trama, et al. | 2019 | Indoor | Track | 2.22, 2.92, 3.61, and 4.31 m/s | ≥60 m | Rec. | 20 (0 F, 20 M) | Mean: 23.9; SD: 2.1 | VT, Shock-frequency, Freq., Spectral Energy |
| [44] | Van den Berghe, et al. | 2019 | Indoor | Floor | 2.55, 3.20, and 5.10 m/s | 768 m | Rec. | 13 (NS) | NR | VT, Res. |
| [45] | Wundersitz, et al. | 2013 | Indoor | Floor | maximal | 50 m | Non | 17 (5 F, 12 M) | Mean: 21; SD: 2 | VT, Res. |
Note: NR = not reported; Pavement = pavement or sidewalk; Floor = floor or platform; Rec. = recreational; Comp. = competitive; Non = non-runners; Disp. = displacement; Δv = change in velocity; Sym. or Reg. = symmetry or regularity; Res. = resultant magnitude; VT = vertical/axial magnitude; AP = anterior–posterior magnitude; ML = medial–lateral magnitude; Seg. Rot. = segment rotation; Shock—time = shock attenuation—time domain; Shock—frequency = shock attenuation—frequency domain; Joint ROM = joint angles or range of motion; Joint ω = joint angular velocity; Freq. = frequency content.
Table 2.
Study characteristics where the analyzed distance is <200 m.
| Ref. | Author | Year | Location | Surface | Speed | Distance/Duration | Type | Number (Sex) | Overall Age | Metric(s) |
|---|---|---|---|---|---|---|---|---|---|---|
| [46] | Adams, et al. | 2016 | Indoor | Treadmill | comfortable | 2 min | Rec. | 20 (8 F, 12 M) | Mean: 30.0; SD: 7.0 | COM Disp. |
| [47] | Adams, et al. | 2018 | Indoor | Treadmill | comfortable | 90 s | Rec. | 20 (NS) | NR | COM Disp. |
| [48] | Argunsah Bayram, et al. | 2021 | Indoor | Treadmill | preferred | 15 min | Non | 24 (10 F, 14 M) | Mean: 22.2; SD: 0.9 | Joint ROM, COM Disp., Sym. or Reg. |
| [49] | Armitage, et al. | 2021 | Indoor | Floor | sprint | 21 m | Non | 16 (0 F, 16 M) | Mean: 17; SD: 1 | Res. |
| Indoor | Treadmill | 3.0 m/s | 1 min | |||||||
| [50] | Backes, et al. | 2020 | Indoor | Treadmill | 2.78 and 3.33 m/s | 2 min | Rec. | 39 (6 F, 33 M) | Mean: 41.8; SD: 9.8 | COM Disp. |
| [51] | Bailey and Harle | 2015 | Indoor | Treadmill | 2.3, 2.7, 3.0, and 3.4 m/s | 6 min | Rec. | 3 (1 F, 2 M) | NR | Res., Seg. Rot. |
| Outdoor | Grass | steady state | 100 m | |||||||
| Outdoor | Pavement | steady state | 100 m | |||||||
| Outdoor | Track | steady state | 100 m | |||||||
| Outdoor | Trail | steady state | 100 m | |||||||
| [52] | Barnes, et al. | 2021 | Outdoor | Grass | 2.1, 2.9, and 4.4 m/s | 140 m | Comp. | 29 (0 F, 29 M) | Mean: 25.2; SD: 3.5 | PlayerLoad |
| [53] | Bastiaansen, et al. | 2020 | NR | NR | maximal sprint | 90 m | Non | 5 (0 F, 5 M) | Mean: 22.5; SD: 2.1 | Joint ROM, Joint ω |
| [54] | Benson, et al. | 2018 | Indoor | Treadmill | preferred | 2 min | Rec. | 44 (18 F, 26 M) | Mean: 13.9; SD: 12.3 | VT, AP, ML, Res. |
| [55] | Bergamini, et al. | 2012 | Outdoor | Track | sprint | 180 m | Comp. | 5 (2 F, 3 M) | NR | Res., Joint ω |
| Rec. | 6 (2 F, 4 M) | |||||||||
| [56] | Boey, et al. | 2017 | NR | Pavement | 3.06 m/s | 90 m | Rec. | 23 (11 F, 12 M) | Mean: 23.3; SD: 3.0 | VT |
| NR | Track | 3.06 m/s | 90 m | Non | 12 (6 F, 6 M) | |||||
| NR | Trail | 3.06 m/s | 90 m | |||||||
| [57] | Boyer and Nigg | 2007 | Indoor | Track | 4.8 m/s | NR | Non | 13 (NS) | NR | VT, Freq. |
| [58] | Boyer and Nigg | 2004 | Indoor | Floor | 2.0, 3.0, 4.0, and 5.5 m/s | 960 m | Non | 10 (0 F, 10 M) | Mean: 25; SE: 4.2 | VT, Freq. |
| [59] | Brayne, et al. | 2018 | Indoor | Treadmill | 2.5, 3.5, and 4.5 m/s | 120 s | Rec. | 13 (0 F, 13 M) | Mean: 30; SD: 7 | VT |
| [60] | Buchheit, et al. | 2015 | Indoor | Treadmill | 2.78, 4.72, and 6.67 m/s | 450 s | Non | 1 (0 F, 1 M) | Exact: 36; NA | Stiffness |
| [61] | Butler, et al. | 2003 | Indoor | Floor | 3.4 m/s | 375 m | Rec. | 15 (NS) | NR; Range: 18–45 | VT |
| [62] | Camelio, et al. | 2020 | Indoor | Treadmill | preferred | 36 min | Rec. | 17 (9 F, 8 M) | Mean: 27; SD: 7 | VT |
| [63] | Carrier, et al. | 2020 | Indoor | Treadmill | self-selected | 6 min | Rec. | 17 (8 F, 9 M) | Mean: 28.1; SD: 7.38 | COM Disp. |
| [64] | Castillo and Lieberman | 2018 | Indoor | Treadmill | 3.0 m/s | 2 min | Non | 27 (13 F, 14 M) | NR; Range: 18–45 | Shock-frequency, Spectral Energy, Joint ROM, Joint ω |
| [65] | Chen, et al. | 2021 | Indoor | Treadmill | 2.5 m/s | 3 min | Non | 24 (0 F, 24 M) | NR | Spectral Energy |
| [66] | Cheung, et al. | 2018 | Indoor | Treadmill | typical | 12 min | Rec. | 16 (5 F, 11 M) | Mean: 28.3; SD: 6.2 | VT, Loading Rate |
| [67] | Cheung, et al. | 2019 | Indoor | Treadmill | 2.78 m/s | 10 min | Rec. | 14 (7 F, 7 M) | Mean: 26.4; SD: 11.2 | VT, Loading Rate |
| [68] | Ching, et al. | 2018 | Indoor | Treadmill | self-selected | 20 min | Rec. | 16 (9 F, 7 M) | Mean: 25.1; SD: 7.9 | VT, Loading Rate |
| [69] | Chu and Caldwell | 2004 | Indoor | Treadmill | 4.17 m/s | ≥75 s | Rec. | 10 (0 F, 10 M) | Mean: 26; SD: 6 | VT, Shock-frequency, Spectral Energy |
| [70] | Clark, et al. | 2010 | Indoor | Treadmill | 2.78 m/s | 12 min | Non | 36 (36 F, 0 M) | Mean: 30.3; SD: 5.8 | VT, AP, ML |
| [71] | Creaby and Frattenovich Smith | 2016 | Indoor | Treadmill | 3 m/s | 50 min | Rec. | 22 (0 F, 22 M) | Mean: 25.4; SD: 6.2 | VT |
| [72] | Crowell, et al. | 2010 | Indoor | Treadmill | self-selected | 25 min | Rec. | 5 (5 F, 0 M) | Mean: 26; SD: 2 | VT, Loading Rate |
| [73] | Day, et al. | 2021 | Indoor | Treadmill | 3.8, 4.1, 4.9, and 5.4 m/s | NR | Comp. | 30 (21 F, 9 M) | NR | VT, Spectral Energy |
| [74] | De la Fuente, et al. | 2019 | Indoor | Treadmill | typical | 10 min | Rec. | 20 (0 F, 20 M) | Mean: 30.5; SD: 9.3 | VT, Res., Freq. |
| [75] | Deflandre, et al. | 2018 | Indoor | Treadmill | 2.22 and 4.44 m/s | 6 min | Rec. | 20 (0 F, 20 M) | Mean: 26; SD: 9.5 | Stiffness, Joint ROM, COM Disp., Sym. or Reg. |
| Outdoor | Grass | 2.22, 2.78, and 3.33 m/s | 720 m | Non | 10 (0 F, 10 M) | |||||
| [76] | DeJong and Hertel | 2020 | Indoor | Treadmill | 2.68 and 3.6 m/s | 180 s | Comp. | 20 (12 F, 8 M) | Mean: 20; SD: 2 | Joint ROM |
| [77] | Derrick, et al. | 2002 | Indoor | Treadmill | 3.2 km pace | run to exhaustion | Rec. | 10 (NS) | Mean: 25.8; SD: 7.0 | VT, Shock-time, Shock-frequency, Spectral Energy, Joint ω, Seg. Rot. |
| [78] | Dufek, et al. | 2009 | Indoor | Treadmill | preferred, 10% slower | 102 s | Rec. | 14 (7 F, 7 M) | Mean: 24.9; SD: 4 | VT, Shock-time |
| [79] | Eggers, et al. | 2018 | Indoor | Track | 3.33 m/s | 400 m | Non | 17 (7 F, 10 M) | NR; Range: 18–40 | VT, Stiffness, COM Disp. |
| [80] | Encarnación-Martínez, et al. | 2020 | Indoor | Treadmill | 3.89 m/s | 4 min | Rec. | 17 (0 F, 17 M) | Mean: 28.7; SD: 8.3 | VT, Shock-frequency, Spectral Energy |
| [81] | Encarnación-Martínez, et al. | 2018 | Outdoor | Grass | 3.33 and 4.00 m/s | 480 m | Non | 12 (0 F, 12 M) | Mean: 24.3; SD: 3.7 | VT, Shock-time |
| [82] | Encarnación-Martínez, et al. | 2021 | Indoor | Treadmill | 2.78 m/s | 10 min | Non | 30 (10 F, 20 M) | Mean: 26.3; SD: 7.0 | VT |
| [83] | Friesenbichler, et al. | 2011 | Outdoor | NR | 10 km pace | run to exhaustion | Rec. | 10 (7 F, 3 M) | Mean: 31.7; SD: 7.3 | VT, AP, ML, Freq., Spectral Energy |
| [84] | Fu, et al. | 2015 | Indoor | Treadmill | 3.33 m/s | 6 min | Rec. | 13 (0 F, 13 M) | Mean: 23.7; SD: 1.2 | VT |
| Outdoor | Grass | 3.33 m/s | 90 m | |||||||
| Outdoor | Pavement | 3.33 m/s | 90 m | |||||||
| Outdoor | Track | 3.33 m/s | 90 m | |||||||
| [85] | Gantz and Derrick | 2018 | Indoor | Treadmill | self-selected | ≥6 min | Rec. | 16 (7 F, 9 M) | Mean: 22.9; SD: 3.3 | VT, Shock-frequency, Spectral Energy |
| [86] | Garcia, et al. | 2021 | Outdoor | Pavement | self-selected | 200 m | Rec. | 15 (12 F, 3 M) | Mean: 27.7; SD: 9.1 | VT, AP, ML, Res., Shock-time |
| Outdoor | Trail | self-selected | 400 m | |||||||
| [87] | García-Pérez, et al. | 2014 | Indoor | Treadmill | 4 m/s | 800 m | Rec. | 20 (9 F, 11 M) | Mean: 34; SD: 8 | VT, Loading Rate, Shock-time |
| Outdoor | Track | 4 m/s | 800 m | |||||||
| [88] | Giandolini, et al. | 2014 | Indoor | Treadmill | 3.89 and 4.44 m/s | 8 min | Rec. | 48 (18 F, 30 M) | Mean: 38.4; SD: 6.7 | VT |
| Outdoor | Trail | 2.78 and 3.33 m/s | 6 min | |||||||
| [89] | Giandolini, et al. | 2013 | Indoor | Treadmill | self-selected | 60 min | Non | 30 (8 F, 22 M) | Mean: 18.3; SD: 4.5 | VT |
| [90] | Glassbrook, et al. | 2020 | Indoor | Treadmill | 60%–100% of maximal | 435 s | Non | 16 (6 F, 10 M) | Mean: 24.5; SD: 4.5 | Res. |
| [91] | Gullstrand, et al. | 2009 | Indoor | Treadmill | 2.78, 3.33, 3.89, 4.44, 5.00, 5.56, and 6.11 m/s | ≥210 s | Rec. | 13 (0 F, 13 M) | Mean: 22.7; NR | COM Disp. |
| [92] | Hardin and Hamill | 2002 | Indoor | Treadmill | 3.4 m/s | 30 min | Rec. | 24 (0 F, 24 M) | NR | VT |
| [93] | Iosa, et al. | 2014 | Indoor | Floor | self-selected | 10 m | Non | 25 (NS) | Mean: 15.3; SD: 3.9 | VT, AP, ML, Stability |
| [94] | Iosa, et al. | 2013 | Indoor | Floor | self-selected | 10 m | Non | 40 (16 F, 24 M) | Mean: 5.5; SD: 2.5 | VT, AP, ML, Res., Freq. |
| [95] | Johnson, et al. | 2020 | Indoor | Treadmill | 90% marathon pace | 30 s | Rec. | 192 (87 F, 105 M) | Mean: 44.9; SD: 10.8 | VT, Res. |
| Outdoor | Pavement | not controlled | 42.2 km | |||||||
| [96] | Johnson, et al. | 2021 | Indoor | Treadmill | self-selected | 16 s | Rec. | 18 (8 F, 10 M) | Mean: 33; SD: 11 | AP, ML |
| [97] | Johnson, et al. | 2020 | Indoor | Treadmill | self-selected | 32 s | Rec. | 18 (8 F, 10 M) | Mean: 33; SD: 11 | VT, Res., Loading Rate |
| [98] | Kawabata, et al. | 2013 | Indoor | Treadmill | slow, preferred, fast | 18 min | Non | 13 (0 F, 13 M) | Mean: 23.3; SD: 0.6 | VT, AP, ML |
| Outdoor | Track | slow, preferred, fast | 4800 m | |||||||
| [99] | Kenneally-Dabrowski, et al. | 2018 | Indoor | Track | maximal sprint | 120 m | Comp. | 13 (0 F, 13 M) | Mean: 23.8; SD: 2.4 | VT |
| [100] | Khassetarash, et al. | 2015 | Indoor | Treadmill | 4 m/s | run to exhaustion (10 km max) | Comp. | 8 (0 F, 8 M) | Mean: 26; SD: 3.6 | Shock-frequency |
| [101] | Kobsar, et al. | 2014 | Indoor | Treadmill | self-selected | 135 s | Rec. | 42 (42 F, 0 M) | Mean: 33; SD: 6 | VT, AP, ML, Res., Freq., Axis Ratio, Sym. or Reg. |
| [102] | Koldenhoven and Hertel | 2018 | Indoor | Treadmill | comfortable | 1.5 miles | Rec. | 12 (6 F, 6 M) | Mean: 23.1; SD: 5.5 | Seg. Rot., Seg. Rot. Velocity |
| [103] | Le Bris, et al. | 2006 | NR | Track | maximal aerobic | run to exhaustion | Comp. | 6 (0 F, 6 M) | Mean: 21.6; SD: 4 | Res., Freq., Spectral Energy, Sym. or Reg. |
| [104] | Leduc, et al. | 2020 | Outdoor | NR | 5.00 m/s | 240 m | Comp. | 17 (0 F, 17 M) | Mean: 21.0; SD: 1.3 | VT, AP, ML, Res., PlayerLoad |
| [105] | Lee, et al. | 2010 | Indoor | Treadmill | self-selected, 0.28 m/s above and below | 15 min | Comp. | 10 (4 F, 6 M) | Mean: 30; SD: 8 | VT |
| [106] | Lee, et al. | 2015 | Indoor | Treadmill | 2.0 and 3.5 m/s | 30 s | Non | 15 (0 F, 15 M) | Mean: 26.9; SD: 3.1 | VT, AP, ML, Res., Seg. Rot. Velocity |
| [107] | Lin, et al. | 2014 | Indoor | Treadmill | 1.67, 2.22, 2.50, and 3.33 m/s | 4 min | Comp. | 10 (0 F, 10 M) | Mean: 50.30; SD: 9.40 | VT, AP, ML |
| Outdoor | Not Controlled | not controlled | 12 hours | |||||||
| [108] | Lindsay, et al. | 2016 | Indoor | Treadmill | 2.22, 2.78, and 3.33 m/s | 8.5 min | Non | 15 (4 F, 11 M) | Mean: 23.7; SD: 4.7 | VT, AP, ML, Res. |
| [109] | Lindsay, et al. | 2014 | Indoor | Treadmill | 2.22, 2.78, and 3.33 m/s | 180 s | Non | 18 (0 F, 18 M) | Mean: 24.0; SD: 4.2 | VT, AP, ML, Res. |
| [110] | Lucas-Cuevas, et al. | 2017 | Indoor | Treadmill | 2.22, 2.78, and 3.33 m/s | 6 min | Rec. | 30 (0 F, 30 M) | Mean: 27.3; SD: 6.4 | VT, Shock-time, Shock-frequency, Freq., Spectral Energy |
| [111] | Lucas-Cuevas, et al. | 2016 | Indoor | Treadmill | 60% maximal aerobic | 3 min | Rec. | 22 (NS) | Mean: 28.4; SD: 5.8 | VT, Loading Rate, Shock-time |
| [112] | Lucas-Cuevas, et al. | 2017 | Indoor | Treadmill | 3.33 m/s | 16 min | Rec. | 38 (18 F, 20 M) | Mean: 29.8; SD: 5.3 | VT, Loading Rate, Shock-time |
| [113] | Macadam, et al. | 2019 | Indoor | Track | maximal sprint | 160 m | Comp. | 1 (0 F, 1 M) | Exact: 32; NA | Seg. Rot., Seg. Rot. Velocity |
| [114] | Macadam, et al. | 2020 | NR | NR | sprint | 200 m | Comp. | 15 (0 F, 15 M) | Mean: 21.0; SD: 2.5 | Seg. Rot., Seg. Rot. Velocity |
| [115] | Macadam, et al. | 2020 | Indoor | Treadmill | maximal sprint | 80 s | Non | 14 (NS) | Mean: 24.9; SD: 4.2 | Seg. Rot., Seg. Rot. Velocity |
| [116] | Macdermid, et al. | 2017 | Indoor | Treadmill | 2.61 m/s | 9 min | Rec. | 8 (NS) | Mean: 25; SD: 12 | Res., Loading Rate |
| [117] | Mangubat, et al. | 2018 | Indoor | Treadmill | preferred | 90 s | Rec. | 13 (5 F, 8 M) | Mean: 27.1; SD: 5.1 | VT |
| [118] | Masci, et al. | 2013 | Indoor | Floor | maximal | 15 m | Non | 54 (NS) | Mean: 5; SD: 3 | VT, AP, ML, Res., Stiffness |
| [119] | McGregor, et al. | 2009 | Indoor | Treadmill | incremental from 0.56 m/s | run to exhaustion | Comp. | 7 (0 F, 7 M) | Mean: 21.4; SD: 1.7; Range: 19–24 | VT, AP, ML, Res., Entropy |
| [120] | Mercer and Chona | 2015 | Indoor | Treadmill | 100%, 110%, 120%, and 130% of preferred | 16 min | Non | 10 (6 F, 4 M) | Mean: 21.4; SD: 2.0 | VT |
| [121] | Mercer, et al. | 2002 | Indoor | Treadmill | 50%, 60%, 70%, 80%, 90%, and 100% of maximal | 120 s | Non | 8 (0 F, 8 M) | Mean: 25; SD: 4.6 | VT, Shock-frequency |
| [122] | Mercer, et al. | 2003 | Indoor | Treadmill | 3.8 m/s | 140 s | Rec. | 10 (0 F, 10 M) | Mean: 24; SD: 5.8 | Shock-frequency, Spectral Energy |
| [123] | Mercer, et al. | 2010 | Indoor | Floor | preferred | 200 m | Non | 18 (7 F, 11 M) | Mean: 10.3; SD: 1 | VT, Shock-time |
| Indoor | Treadmill | preferred, 0.5 m/s faster and slower | 6 min | |||||||
| [124] | Mercer, et al. | 2003 | Indoor | Treadmill | 3.1 and 3.8 m/s | 40 s | Non | 10 (0 F, 10 M) | Mean: 24; SD: 6 | VT, Shock-frequency, Spectral Energy |
| [125] | Meyer, et al. | 2015 | Indoor | Floor | 1.67 and 2.78 m/s | 140 m | Non | 13 (3 F, 10 M) | Mean: 10.1; SD: 3.0; Range: 5–16 | VT |
| [126] | Meyer, et al. | 2018 | Indoor | Track | 3.5 m/s | 900 m | Non | 36 (18 F, 18 M) | Mean: 25.4; SD: 3.5 | VT, AP, ML, Variability-any axis |
| Indoor | Treadmill | 3.0 m/s | 1 min | |||||||
| Outdoor | Grass | 3.0 m/s | 1 min | |||||||
| Outdoor | Pavement | 3.0 m/s | 1 min | |||||||
| [127] | Mitschke, et al. | 2017 | Indoor | Track | 2.5 and 3.5 m/s | 450 m | Rec. | 24 (NS) | Mean: 24.7; SD: 4.1 | Seg. Rot. Velocity |
| [128] | Mitschke, et al. | 2017 | Indoor | Track | 3.5 m/s | 450 m | Rec. | 21 (0 F, 21 M) | Mean: 28.9; SD: 10.8 | VT, Seg. Rot., Seg. Rot. Velocity |
| [129] | Mitschke, et al. | 2018 | Indoor | Track | self-selected | 225 m | Rec. | 21 (0 F, 21 M) | Mean: 24.4; SD: 4.2 | VT, Seg. Rot. |
| [130] | Montgomery, et al. | 2016 | Indoor | Floor | natural jog, natural run | 40 m | Non | 15 (NS) | Mean: 24.2; SD: 3.8 | VT, Loading Rate |
| Indoor | Treadmill | natural jog, natural run | 1 min | |||||||
| [131] | Moran, et al. | 2017 | Indoor | Treadmill | 75% of maximum HR | 37 min | Rec. | 15 (6 F, 9 M) | Mean: 20.4; SD: 2.4 | VT |
| [132] | Morrow, et al. | 2014 | Indoor | Floor | slow, normal, fast | ≥504 m | Non | 11 (8 F, 3 M) | Mean: 33.4; SD: 10.5 | VT, AP, ML |
| [133] | Neugebauer, et al. | 2012 | Indoor | Floor | consistent | 540 m | Non | 35 (20 F, 15 M) | Mean: 11.6; SD: 0.7 | Res. |
| [134] | Nüesch, et al. | 2017 | Indoor | Treadmill | self-selected | 6 min | Rec. | 20 (12 F, 8 M) | Mean: 27.4; SD: 8.3 | Joint ROM |
| [135] | O’Connor and Hamill | 2002 | Indoor | Treadmill | 3.8 m/s | 4 min | Non | 12 (0 F, 12 M) | Mean: 27.6; SD: 5.3 | VT |
| [136] | Provot, et al. | 2017 | Indoor | Treadmill | 2.22, 2.78, 3.33, 3.89, 4.44, and 5.00 m/s | 7 min | Non | 1 (0 F, 1 M) | Exact: 33; NA | Res., Spectral Energy |
| [137] | Provot, et al. | 2019 | Indoor | Treadmill | 2.22, 2.50, 2.78, 3.06, 3.33, 3.61, 3.89, 4.44, and 5.00 m/s | 9 min | Rec. | 18 (8 F, 10 M) | Mean: 31.4; SD: 8.9 | Res., Freq., Spectral Energy, Stiffness |
| [138] | Rabuffetti, et al. | 2019 | Indoor | Treadmill | 1.8 and 2.2 m/s | 140 s | Non | 25 (11 F, 14 M) | Mean: 26.5; SD: 4.5; Range: 20–40 | Sym. or Reg. |
| [139] | Raper, et al. | 2018 | Indoor | Track | slow, medium, fast | 50 m | Comp. | 10 (6 F, 4 M) | Mean: 26.90; SD: 4.03 | VT |
| [140] | Reenalda, et al. | 2019 | Outdoor | Track | 10 km pace | 20 min | Rec. | 10 (0 F, 10 M) | Mean: 31; SD: 5 | VT, Shock-time, Joint ROM |
| [141] | Schütte, et al. | 2015 | Indoor | Treadmill | 3.2 km pace | run to exhaustion | Rec. | 20 (8 F, 12 M) | Mean: 21.05; SD: 2.14 | VT, AP, ML, Axis Ratio, Sym. or Reg., Entropy |
| [142] | Schütte, et al. | 2016 | Outdoor | Pavement | self-selected | 180 m | Rec. | 28 (14 F, 14 M) | Mean: 22.62; SD: 3.07 | VT, AP, Freq., Axis Ratio, Sym. or Reg., Entropy |
| Outdoor | Track | self-selected | 180 m | |||||||
| Outdoor | Trail | self-selected | 180 m | |||||||
| [143] | Schütte, et al. | 2018 | Indoor | Treadmill | incremental from 2.22 or 2.50 m/s | run to exhaustion | Rec. | 30 (14 F, 16 M) | Mean: 21.75; SD: 1.40 | VT, AP, ML, Axis Ratio, Sym. or Reg., Entropy |
| [144] | Setuain, et al. | 2017 | Indoor | Floor | maximal sprint | 60 m | Comp. | 1 (0 F, 1 M) | Exact: 19; NA | VT, AP, Res., COM Disp., COM Δv |
| [145] | Setuain, et al. | 2018 | Indoor | Floor | maximal sprint | 80 m | Rec. | 16 (8 F, 8 M) | Mean: 28.8; SD: 5.35 | AP, Res., COM Δv, Power |
| [146] | Sheerin, et al. | 2018 | Indoor | Treadmill | 2.7, 3.0, 3.3, and 3.7 m/s | 8 min | Rec. | 14 (0 F, 14 M) | Mean: 33.6; SD: 11.6 | Res. |
| [147] | Sheerin, et al. | 2018 | Indoor | Treadmill | 2.7, 3.0, 3.3, and 3.7 m/s | 8 min | Rec. | 85 (20 F, 65 M) | Mean: 39.51; SD: 8.92 | Res. |
| [148] | Shiang, et al. | 2016 | Indoor | Treadmill | 1.94, 2.78, and 3.61 m/s | 6 min | Non | 6 (0 F, 6 M) | Mean: 25.4; SD: 1.7 | Seg. Rot. |
| [149] | Simoni, et al. | 2020 | Indoor | Treadmill | self-selected | 1 min | Rec. | 87 (28 F, 59 M) | Mean: 41; SD: 10 | VT, AP, ML |
| [150] | Stickford, et al. | 2015 | Indoor | Treadmill | 3.88, 4.47, and 5.00 m/s | 12 min | Comp. | 16 (0 F, 16 M) | Mean: 22.4; SD: 3 | Stiffness, COM Disp. |
| [151] | TenBroek, et al. | 2014 | Indoor | Treadmill | 3 m/s | 90 min | Rec. | 10 (0 F, 10 M) | NR; Range: 18–55 | VT, Shock-frequency |
| [152] | Tenforde, et al. | 2020 | Indoor | Treadmill | self-selected | 3 min | Rec. | 169 (74 F, 95 M) | Mean: 38.7; SD: 13.1 | VT, Res. |
| [153] | Thomas and Derrick | 2003 | Indoor | Treadmill | preferred | 10 min | Comp. | 12 (6 F, 6 M) | Mean: 20.9; SD: 2.3 | VT, Shock-time, Spectral Energy, Joint ROM, Joint ω |
| [154] | Tirosh, et al. | 2019 | Indoor | Treadmill | 20% above walking | 27 min | Non | 37 (NS) | Mean: 9.2; SD: 1.3 | VT |
| [155] | Tirosh, et al. | 2017 | Indoor | Treadmill | 20% above walking | 2 min | Non | 24 (NS) | Mean: 8.5; SD: 0.9 | VT |
| [156] | Tirosh, et al. | 2020 | Indoor | Treadmill | 20% above walking | 2 min | Non | 32 (15 F, 17 M) | Mean: 9.26; SD: 1.18 | VT, Shock-time |
| [157] | van Werkhoven, et al. | 2019 | Indoor | Treadmill | comfortable | 3 min | Non | 12 (NS) | NR; Range: 18–45 | Joint ROM, Joint ω, Seg. Rot. |
| [158] | Walsh | 2021 | Indoor | Treadmill | 100% and 120% of preferred | 12 min | Non | 18 (9 F, 9 M) | Mean: 29; SD: 6.5 | Stability, Entropy |
| [159] | Waite, et al. | 2021 | Outdoor | Grass | 80% of 1 mile pace | 180 m | Rec. | 13 (5 F, 8 M) | Mean: 20.07; SD: 0.95 | VT |
| Outdoor | Pavement | 80% of 1 mile pace | 360 m | |||||||
| [160] | Winter, et al. | 2016 | Indoor | Floor | self-selected | 8.2 km | Rec. | 10 (4 F, 6 M) | Mean: 27.5; SD: 9.5 | VT, AP, ML |
| [161] | Wixted, et al. | 2010 | Outdoor | Track | race effort | 1500 m | Comp. | 2 (NS) | NR | VT, AP, ML |
| [162] | Wood and Kipp | 2014 | Indoor | Treadmill | comfortable fast jog | 25 min | Rec. | 9 (6 F, 3 M) | Mean: 20; SD: 1.5 | VT, AP, Res. |
| [163] | Wundersitz, et al. | 2015 | Indoor | Treadmill | 3.3, 5.0, and 5.9 m/s | 90 s | Non | 39 (11 F, 28 M) | Mean: 24.2; SD: 2.5 | Res. |
| [164] | Zhang, et al. | 2019 | Indoor | Treadmill | 90%, 100%, and 110% of preferred | 9 min | Rec. | 13 (3 F, 10 M) | Mean: 41.1; SD: 6.9 | VT |
| [165] | Zhang, et al. | 2016 | Indoor | Treadmill | preferred, 15% faster and slower | 18 min | Non | 10 (2 F, 8 M) | Mean: 23.6; SD: 3.8 | VT |
Note: NR = not reported; Pavement = pavement or sidewalk; Floor = floor or platform; Rec. = recreational; Comp. = competitive; Non = non-runners; Disp. = displacement; Δv = change in velocity; Sym. or Reg. = symmetry or regularity; Res. = resultant magnitude; VT = vertical/axial magnitude; AP = anterior–posterior magnitude; ML = medial–lateral magnitude; Seg. Rot. = segment rotation; Shock—time = shock attenuation—time domain; Shock—frequency = shock attenuation—frequency domain; Joint ROM = joint angles or range of motion; Joint ω = joint angular velocity; Freq. = frequency content.
Table 3.
Study characteristics where the analyzed distance is 200–1000 m.
| Ref. | Author | Year | Location | Surface | Speed | Distance/Duration | Type | Number (Sex) | Overall Age | Metric(s) |
|---|---|---|---|---|---|---|---|---|---|---|
| [166] | Aubry, et al. | 2018 | Indoor | Treadmill | 3.06–5.00 m/s | 6 min | Comp. | 11 (0 F, 11 M) | Mean: 33.4; SD: 6.6 | COM Disp., Power |
| Outdoor | Track | 3.06–5.00 m/s | 12 min | Rec. | 13 (0 F, 13 M) | |||||
| [167] | Austin, et al. | 2018 | Indoor | Treadmill | 85–89% VO2max | 8 min | Comp. | 17 (8 F, 9 M) | Mean: 20.6; SD: 2.3 | Power |
| [168] | Barrett, et al. | 2014 | Indoor | Treadmill | incremental from 1.94 m/s | 2 runs to exhaustion | Comp. | 44 (NS) | Mean: 22; SD: 3 | PlayerLoad |
| [5] | Benson, et al. | 2020 | Indoor | Treadmill | preferred | 5 min | Rec. | 69 (31 F, 38 M) | Mean: 33.7; SD: 11.5 | VT, AP, ML, Res., Sym. or Reg. |
| Outdoor | Pavement | preferred | 600 m | |||||||
| [169] | De Brabandere, et al. | 2018 | Indoor | Treadmill | incremental from 2.5 m/s to 4.58 m/s | run to exhaustion | Rec. | 28 (16 F, 12 M) | Mean: 21.8; SD: 1.3 | VT, AP, ML |
| [170] | Cher, et al. | 2017 | Indoor | Treadmill | slow, medium, fast | 60 min | Non | 12 (4 F, 8 M) | Mean: 29.4; SD: 6.8 | VT, AP, ML, Res. |
| [171] | Clansey, et al. | 2016 | Indoor | Treadmill | 95% of onset of blood lactate accumulation | 40 min | Rec. | 13 (0 F, 13 M) | Mean: 35.1; SD: 10.2 | VT, Shock-frequency |
| [172] | Clermont, et al. | 2019 | Indoor | Treadmill | preferred | 5 min | Rec. | 41 (16 F, 25 M) | Mean: 32.5; SD: 12.7 | VT, AP, ML, Res., Sym. or Reg. |
| [173] | Clermont, et al. | 2020 | Indoor | Track | self-selected | 21 min | Rec. | 17 (10 F, 7 M) | Mean: 39.8; SD: 9.6 | VT, AP, ML, Res., Sym. or Reg. |
| Outdoor | Track | not controlled | 6 km | |||||||
| [174] | Deriaz, et al. | 2010 | Indoor | Treadmill | comfortable | 15 min | Rec. | 65 (0 F, 65 M) | Mean: 36.0; SD: 6.8 | VT |
| Non | 16 (0 F, 16 M) | |||||||||
| [175] | Enders, et al. | 2014 | Indoor | Treadmill | 3.5 m/s | 20 min | Rec. | 12 (0 F, 12 M) | Mean: 25.56; SD: 2.88 | VT, Shock-frequency, Freq., Spectral Energy |
| [176] | Garcia-Byrne, et al. | 2020 | Indoor | Floor | 2.22 m/s | 400 m | Comp. | 36 (0 F, 36 M) | Mean: 25; SD: 3 | PlayerLoad |
| [177] | Giandolini, et al. | 2016 | Outdoor | Pavement | self-selected | 6.5 km | Rec. | 23 (0 F, 23 M) | Mean: 39; SD: 11 | VT, ML, Res., Shock-time, Shock-frequency |
| Outdoor | Trail | self-selected | 6.5 km | |||||||
| [178] | Giandolini, et al. | 2017 | Outdoor | Pavement | self-selected | 6.5 km | Rec. | 23 (0 F, 23 M) | Mean: 39; SD: 11 | VT |
| Outdoor | Trail | self-selected | 6.5 km | |||||||
| [179] | Horvais, et al. | 2019 | Indoor | Treadmill | 3.9 m/s | 14 min | Rec. | 10 (0 F, 10 M) | Mean: 27.3; SD: 5.4 | VT, AP, Res., Spectral Energy |
| [180] | Hughes, et al. | 2019 | Indoor | Treadmill | 3.89 and 5.00 m/s | 9 min | Comp. | 16 (NS) | Mean: 17.36; SD: 1.25 | VT |
| [181] | Koska, et al. | 2018 | Indoor | Treadmill | 2.78, 3.33, and 4.17 m/s | 9 min | Rec. | 51 (15 F, 36 M) | Mean: 33.9; SD: 8.2 | Seg. Rot., Seg. Rot. Velocity |
| [182] | Melo, et al. | 2020 | Indoor | Treadmill | 10 km pace | 20 km | Rec. | 13 (5 F, 8 M) | Mean: 36; SD: 4 | COM Disp. |
| [183] | Moltó, et al. | 2020 | Indoor | Treadmill | typical | 3 min | Rec. | 38 (16 F, 22 M) | Mean: 26.7; SD: 7.7 | Seg. Rot. |
| [184] | Morio, et al. | 2016 | Indoor | Treadmill | 3.06 m/s | 12 min | Rec. | 8 (0 F, 8 M) | Mean: 26; SD: 2 | VT, AP, ML |
| [185] | Murray, et al. | 2017 | Indoor | Treadmill | incremental to reach [La]b concentration of 4 mmol/L | run to exhaustion | Comp. | 6 (0 F, 6 M) | Mean: 15.6; SD: 1.2 | VT, AP, ML, Entropy |
| [186] | Navalta, et al. | 2019 | Outdoor | Trail | self-selected | 10 min | Non | 20 (8 F, 12 M) | Mean: 22.2; SD: 5.8 | Stiffness, COM Disp., Power |
| [187] | Olin and Gutierrez | 2013 | Indoor | Treadmill | comfortable | 21 min | Rec. | 18 (12 F, 6 M) | Mean: 31.2; SD: 7.9 | VT |
| [188] | Perrotin, et al. | 2021 | Outdoor | Pavement | not controlled | 1 km | Rec. | 30 (3 F, 27 M) | Mean: 36.4; SD: 8 | Stiffness, COM Disp., Power |
| [189] | Provot, et al. | 2016 | Indoor | Treadmill | 3.33 m/s | 40 min | Rec. | 1 (0 F, 1 M) | Exact: 22; NA | Res., Freq., Spectral Energy, Stiffness |
| [190] | Reenalda, et al. | 2016 | Outdoor | Pavement | not controlled | 42.2 km | Rec. | 3 (0 F, 3 M) | Mean: 38.7; SD: 8.2; Range: 31–50 | VT, Joint ROM, COM Disp. |
| [191] | Seeley, et al. | 2020 | Indoor | Treadmill | 2.68, 3.13, and 3.58 m/s | 12 min | Non | 31 (14 F, 17 M) | Mean: 23; SD: 3 | VT, AP, ML, Res. |
| [192] | Shih, et al. | 2014 | Indoor | Treadmill | 70% of maximal | 30 min | Rec. | 15 (NS) | Mean: 24.5; SD: 1.7 | Joint ROM, Joint ω |
| [193] | Tirosh, et al. | 2019 | Indoor | Floor | 20% above walking | 1 km | Non | 10 (NS) | Mean: 10.7; SD: 1.27 | VT |
| Outdoor | Grass | 3.33, 3.89, 4.44, and 5.00 m/s | 12 min | |||||||
| Outdoor | Pavement | 3.33, 3.89, 4.44, and 5.00 m/s | 12 min | |||||||
| Outdoor | Track | 3.33, 3.89, 4.44, and 5.00 m/s | 12 min | |||||||
| Outdoor | Track | 4.78 m/s | 6 km | |||||||
| [194] | Ueberschar, et al. | 2019 | Indoor | Treadmill | incremental from 1.67 m/s | run to exhaustion | Rec. | 15 (0 F, 15 M) | Mean: 30; SD: 7 | VT, Res. |
| [195] | Van den Berghe, et al. | 2021 | Indoor | Track | 3.2 m/s | 20 min | Rec. | 10 (NS) | Mean: 33; SD: 9; Range: 24–49 | VT |
| [196] | van der Bie and Krose | 2015 | Indoor | Treadmill | ventilatory threshold | run to exhaustion | Non | 18 (14 F, 4 M) | Mean: 23; SD: 3 | VT, AP, ML, Variability-any axis, Entropy |
| [9] | Watari, et al. | 2016 | Indoor | Treadmill | 2.7, 3.0, 3.3, 3.6, and 3.9 m/s | 5 min | Rec. | 22 (8 F, 14 M) | Mean: 28.2; SD: 10.1 | COM Disp. |
| [197] | Weich, et al. | 2019 | Indoor | Track | 95% anaerobic threshold | 5000 m | Rec. | 25 (NS) | Mean: 26.64; SD: 6.86 | VT, AP, ML |
| Non | 9 (NS) |
Note: NR = not reported; Pavement = pavement or sidewalk; Floor = floor or platform; Rec. = recreational; Comp. = competitive; Non = non-runners; Disp. = displacement; Δv = change in velocity; Sym. or Reg. = symmetry or regularity; Res. = resultant magnitude; VT = vertical/axial magnitude; AP = anterior–posterior magnitude; ML = medial–lateral magnitude; Seg. Rot. = segment rotation; Shock—time = shock attenuation—time domain; Shock—frequency = shock attenuation—frequency domain; Joint ROM = joint angles or range of motion; Joint ω = joint angular velocity; Freq. = frequency content.
Table 4.
Study characteristics where the analyzed distance is >1000 m over a single run.
| Ref. | Author | Year | Location | Surface | Speed | Distance/Duration | Type | Number (Sex) | Overall Age | Metric(s) |
|---|---|---|---|---|---|---|---|---|---|---|
| [198] | Bigelow, et al. | 2013 | Indoor | Track | self-selected | 4 miles | Rec. | 12 (NS) | Mean: 32.8; SD: 9.8 | VT, ML |
| Indoor | Treadmill | self-selected | 4 miles | |||||||
| [199] | Brahms, et al. | 2020 | Indoor | Track | 5 km pace | run to exhaustion | Comp. | 16 (NS) | Mean: 24; SD: 3.9 | Res. |
| Rec. | 16 (NS) | |||||||||
| Indoor | Treadmill | incremental from 2.5 m/s | run to exhaustion | |||||||
| Outdoor | Track | 2.78 m/s | 9 min | |||||||
| Outdoor | Track | incremental from 2.5 m/s | run to exhaustion | |||||||
| [200] | Clermont, et al. | 2019 | Outdoor | Not Controlled | not controlled | 42.2 km | Rec. | 27 (15 F, 12 M) | Mean: 45.1; SD: 11.5 | Joint ROM, Seg. Rot., COM Disp., COM Δv |
| [201] | DeJong and Hertel | 2020 | Outdoor | Pavement | not controlled | 6–21.1 km | Comp. | 5 (4 F, 1 M) | Mean: 30.2; SD: 3.3 | VT, AP, Joint ω |
| Outdoor | Trail | not controlled | 5 km | |||||||
| [202] | Giandolini, et al. | 2015 | Outdoor | Trail | not controlled | 45 km | Comp. | 1 (0 F, 1 M) | Exact: 26; NA | VT, AP, Res., Freq. |
| [203] | Gómez-Carmona, et al. | 2020 | Indoor | Treadmill | incremental from 2.22 m/s | run to exhaustion | Rec. | 20 (0 F, 20 M) | Mean: 27.32; SD: 6.65 | PlayerLoad |
| Outdoor | Track | incremental from 2.22 m/s | run to exhaustion | |||||||
| [204] | Hoenig, et al. | 2019 | NR | Track | maximal | 5000 m | Rec. | 30 (0 F, 30 M) | Mean: 27; SD: 6.0 | Stability |
| [205] | Provot, et al. | 2019 | Indoor | Treadmill | 3.75 m/s | run to exhaustion | Rec. | 10 (5 F, 5 M) | Mean: 38.0; SD: 11.6 | VT, AP, ML, Res., Freq., Spectral Energy, Stiffness |
| [206] | Rojas-Valverde, et al. | 2019 | Outdoor | Trail | not controlled | 35.27 km | Rec. | 20 (0 F, 20 M) | Mean: 38.95; SD: 9.99 | Res., Entropy, PlayerLoad |
| [207] | Rojas-Valverde, et al. | 2020 | Outdoor | Not Controlled | not controlled | 36 km | Rec. | 18 (NS) | Mean: 38.78; SD: 10.38 | Res. |
| [208] | Schütte, et al. | 2018 | Outdoor | Track | 3.2 km pace | 3200 m | Rec. | 16 (6 F, 10 M) | Mean: 20.23; SD: 0.78 | VT, Shock-frequency, Spectral Energy, Axis Ratio, Sym. or Reg., Entropy |
| Rec. | 14 (6 F, 8 M) | |||||||||
| [209] | Ueberschar, et al. | 2019 | Outdoor | Trail | 3.17 m/s | 10 km | Non | 10 (NS) | Mean: 10.7; SD: 1.27 | VT |
Note: NR = not reported; Pavement = pavement or sidewalk; Floor = floor or platform; Rec. = recreational; Comp. = competitive; Non = non-runners; Disp. = displacement; Δv = change in velocity; Sym. or Reg. = symmetry or regularity; Res. = resultant magnitude; VT = vertical/axial magnitude; AP = anterior–posterior magnitude; ML = medial–lateral magnitude; Seg. Rot. = segment rotation; Shock—time = shock attenuation—time domain; Shock—frequency = shock attenuation—frequency domain; Joint ROM = joint angles or range of motion; Joint ω = joint angular velocity; Freq. = frequency content.
Table 5.
Study characteristics where the analyzed distance is >1000 m over multiple runs.
| Ref. | Author | Year | Location | Surface | Speed | Distance/Duration | Type | Number (Sex) | Overall Age | Metric(s) |
|---|---|---|---|---|---|---|---|---|---|---|
| [210] | Ahamed, et al. | 2019 | Outdoor | Not Controlled | not controlled | 29 km | Rec. | 11 (10 F, 1 M) | Mean: 44.1; SD: 9.1 | Joint ROM, Seg. Rot., COM Disp., COM Δv |
| [211] | Ahamed, et al. | 2018 | Outdoor | Pavement | not controlled | ≥24 km | Rec. | 6 (5 F, 1 M) | Mean: 44.4; NR | Seg. Rot., COM Disp., COM Δv |
| [212] | Ahamed, et al. | 2019 | Outdoor | Not Controlled | not controlled | 7 runs | Rec. | 35 (25 F, 10 M) | Mean: 49.7; SD: 9.6 | Joint ROM, Seg. Rot., COM Disp., COM Δv |
| [213] | Benson, et al. | 2019 | Outdoor | Not Controlled | not controlled | 10 runs | Rec. | 12 (9 F, 3 M) | Mean: 48.5; SD: 12.0 | Joint ROM, Seg. Rot., COM Disp., COM Δv |
| [214] | Carton-Llorente, et al. | 2021 | Indoor | Treadmill | submaximal | 120 min | Rec. | 22 (0 F, 22 M) | Mean: 34; SD: 7.5 | Power |
| [215] | Cerezuela-Espejo, et al. | 2020 | Indoor | Treadmill | 2.78 m/s | 24 min | Rec. | 12 (0 F, 12 M) | Mean: 25.7; SD: 7.9 | Power |
| [216] | Colapietro, et al. | 2020 | Outdoor | Track | slow, fast | 3200 m | Rec. | 18 (10 F, 8 M) | Mean: 22.7; SD: 4.7 | VT, AP, Joint ROM, Joint ω |
| [217] | Gregory, et al. | 2019 | Outdoor | Track | hard | 1600 m | Non | 12 (6 F, 6 M) | Mean: 22.0; SD: 1.9 | VT, AP, Joint ROM, Joint ω |
| [218] | Hollander, et al. | 2021 | Indoor | Treadmill | 70% VO2max | 105 min | Non | 41 (20 F, 21 M) | Mean: 25.2; SD: 3.1 | Stability |
| [219] | Hollis, et al. | 2019 | Outdoor | Grass | moderate, hard | 3200 m | Rec. | 15 (8 F, 7 M) | Mean: 20; SD: 3.1 | VT, AP, Joint ROM, Joint ω |
| Outdoor | Track | moderate, hard | 3200 m | |||||||
| [220] | Kiernan, et al. | 2018 | Outdoor | Not Controlled | not controlled | 60 day training period | Comp. | 9 (0 F, 9 M) | Mean: 18.7; SD: 1.0 | VT |
| [221] | Koldenhoven, et al. | 2020 | Outdoor | Not Controlled | not controlled | 3 runs | Rec. | 16 (8 F, 8 M) | Mean: 23.5; SD: 5 | AP, Res., Seg. Rot., Seg. Rot. Velocity |
| [116] | Macdermid, et al. | 2017 | Indoor | Treadmill | 2.83 m/s | 30 min | Comp. | 6 (NS) | Mean: 29.8; SD: 13.0 | Loading Rate, Shock-time, COM Disp. |
| [222] | McGregor, et al. | 2009 | Indoor | Treadmill | incremental from 0.56 m/s | 2 runs to exhaustion | Comp. | 7 (0 F, 7 M) | Mean: 26.5; SD: 5.7 | VT, AP, ML, Res. |
| Non | 7 (NS) | |||||||||
| [223] | Nüesch, et al. | 2019 | Indoor | Treadmill | self-selected | 15 min | Rec. | 19 (11 F, 8 M) | Mean: 27.7; SD: 8.6 | Joint ROM |
| [224] | Olcina, et al. | 2019 | NR | Track | maximal | 24 min | Comp. | 10 (2 F, 8 M) | Mean: 25.7; SD: 8.9 | COM Disp. |
| Outdoor | Trail | not controlled | 4.1 km | |||||||
| [225] | Rochat, et al. | 2019 | Outdoor | Trail | not controlled | 15 km | Rec. | 9 (0 F, 9 M) | Mean: 37.8; SD: 7 | VT, COM Disp. |
| [226] | Ruder, et al. | 2019 | Outdoor | Pavement | not controlled | 42.2 km | Rec. | 222 (103 F, 119 M) | Mean: 44.1; SD: 10.8 | VT |
| [227] | Ryan, et al. | 2021 | Outdoor | Not Controlled | not controlled | 10–12 runs | Rec. | 12 (0 F, 12 M) | NR; Range: 14–18 | Res. |
| [228] | Strohrmann, et al. | 2012 | Indoor | Treadmill | 85% of maximal | 45 min | Rec. | 21 (NS) | NR | Res., Joint ω, Seg. Rot., COM Disp. |
| Outdoor | Track | 85% of maximal | 45 min | |||||||
| [209] | Ueberschar, et al. | 2019 | Outdoor | Pavement | 3.64 and 6.67 m/s | 10.7 km | Comp. | 2 (0 F, 2 M) | Mean: 17.6; SD: 1.13 | VT |
| [229] | Van den Berghe, et al. | 2020 | Indoor | Track | 3.2 m/s | 24.5 min | Rec. | 10 (5 F, 5 M) | Mean: 33; SD: 9 | VT |
| [230] | Vanwanseele, et al. | 2020 | Indoor | Treadmill | 2.22, 3.33, and 4.44 m/s | 3 min | Rec. | 68 (NS) | Mean: 29.5; SD: 8.1 | VT, AP, ML |
| Outdoor | Not Controlled | not controlled | 3 month training period | |||||||
| [231] | Willis, et al. | 2019 | Indoor | Treadmill | 2.50, 2.78, 3.61, and 4.17 m/s | 10 min | Comp. | 12 (NS) | Mean: 33.6; SD: 4.3 | Stiffness |
Note: NR = not reported; Pavement = pavement or sidewalk; Floor = floor or platform; Rec. = recreational; Comp. = competitive; Non = non-runners; Disp. = displacement; Δv = change in velocity; Sym. or Reg. = symmetry or regularity; Res. = resultant magnitude; VT = vertical/axial magnitude; AP = anterior–posterior magnitude; ML = medial–lateral magnitude; Seg. Rot. = segment rotation; Shock—time = shock attenuation—time domain; Shock—frequency = shock attenuation—frequency domain; Joint ROM = joint angles or range of motion; Joint ω = joint angular velocity; Freq. = frequency content.
Table 6.
Study characteristics where the analyzed distance is not reported.
| Ref. | Author | Year | Location | Surface | Speed | Distance/Duration | Type | Number (Sex) | Overall Age | Metric(s) |
|---|---|---|---|---|---|---|---|---|---|---|
| [232] | Bielik | 2019 | Outdoor | Track | 2.78, 3.33, and 4.17 m/s | 15 min | Rec. | 73 (24 F, 49 M) | Mean: 29.2; SD: 4.1 | COM Disp. |
| Outdoor | Treadmill | incremental from 0.28 m/s | run to exhaustion | |||||||
| [233] | Bielik and Clementis | 2017 | Indoor | Treadmill | incremental from 2.22 m/s | run to exhaustion | Comp. | 30 (NS) | NR | COM Disp. |
| Rec. | 24 (NS) | |||||||||
| [234] | Butler, et al. | 2007 | Indoor | Treadmill | self-selected | 2 runs | Rec. | 24 (NS) | Mean: 21.4; SD: 3.1 | VT |
| [235] | Cooper, et al. | 2009 | Indoor | Treadmill | incremental from 0.45 m/s to 2.24 m/s | 5 min | Non | 7 (2 F, 5 M) | Mean: 30; SD: 6 | Joint ROM |
| [236] | de Fontenay, et al. | 2020 | Indoor | Treadmill | self-selected | NR | Non | 32 (13 F, 19 M) | Mean: 27.0; SD: 5.5 | AP, Loading Rate, Joint ROM, COM Disp. |
| [237] | Dufek, et al. | 2008 | Indoor | Treadmill | self-selected | 90 s | Rec. | 31 (31 F, 0 M) | Mean: 26.7; SD: 3.8 | VT, Shock-time |
| [238] | Garrett, et al. | 2019 | NR | NR | 6.25 m/s | 450 m | Comp. | 23 (0 F, 23 M) | Mean: 22.4; SD: 3.6 | PlayerLoad |
| [239] | Gurchiek, et al. | 2017 | Indoor | Floor | sprint | NR | Non | 15 (3 F, 12 M) | Mean: 23.2; SD: 2.11 | Seg. Rot. |
| [240] | Sheerin, et al. | 2020 | Indoor | Treadmill | comfortable | NR | Rec. | 18 (7 F, 11 M) | Mean: 35.2; SD: 9.6 | Res. |
| Outdoor | Track | comfortable | 800 m | |||||||
| [241] | Ueberschar, et al. | 2019 | Indoor | Treadmill | incremental | run to exhaustion | Comp. | 53 (18 F, 35 M) | Mean: 20.07; SD: 3.65 | VT, Shock-time |
| [242] | Zadeh, et al. | 2020 | Outdoor | Not Controlled | not controlled | 36 physical training sessions | Non | 55 (16 F, 39 M) | Mean: 20.8; SD: 3.32 | VT, Res., Loading Rate |
Note: NR = not reported; Pavement = pavement or sidewalk; Floor = floor or platform; Rec. = recreational; Comp. = competitive; Non = non-runners; Disp. = displacement; Δv = change in velocity; Sym. or Reg. = symmetry or regularity; Res. = resultant magnitude; VT = vertical/axial magnitude; AP = anterior–posterior magnitude; ML = medial–lateral magnitude; Seg. Rot. = segment rotation; Shock—time = shock attenuation—time domain; Shock—frequency = shock attenuation—frequency domain; Joint ROM = joint angles or range of motion; Joint ω = joint angular velocity; Freq. = frequency content.
3.2.1. Conditions
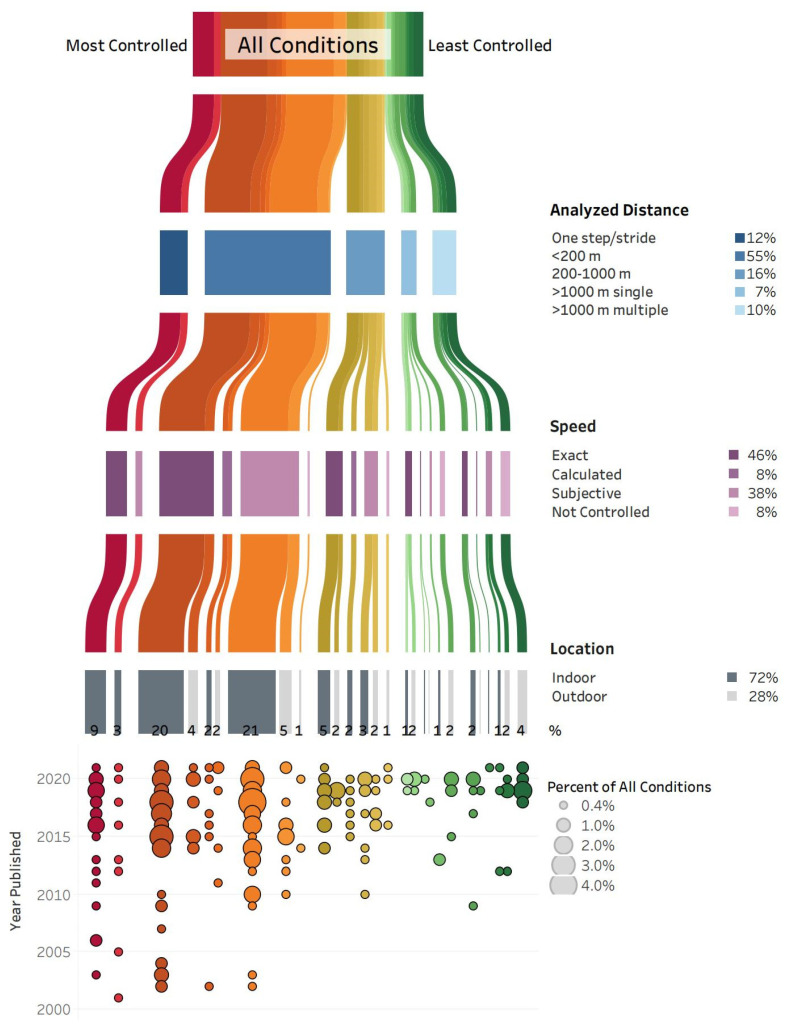
Across the 231 included studies, running gait was analyzed in 286 different conditions; however, for 24 conditions, the analyzed distance, speed and/or location could not be classified due to lack of information. The 262 running conditions that could be classified consisted of 27 unique combinations of the specified categories for analyzed distance (one step or stride, <200 m, 200–1000 m, >1000 m single trial, >1000 m multiple trials), speed (exact, calculated, subjective, not controlled) and location (indoor, outdoor) (Figure 2).
Figure 2.
All conditions (262 across 231 studies) are grouped according to the analyzed distance, speed, and location. The condition groups are ranked from most controlled (red, on the left) to least controlled (green, on the right), and the width of each line corresponds to the percent of all conditions within that group. The degree of control is based on the analyzed distance (one step/stride is more controlled than >1000 m), speed (exact is more controlled than not controlled), and location (indoor is more controlled than outdoor). The percent of all conditions for each category of analyzed distance (shades of blue), speed (shades of purple), and location (shades of grey) is reported. In the bottom panel, the percent of all conditions within each group are further separated by year the study was published, with larger circles corresponding to a greater percent of all conditions. Note: 24 conditions that could not be categorized due to lack of information are not included in this figure.
The most common running condition was indoors at an exact speed with <200 m analyzed, accounting for 21% of all 262 conditions. Indoor running at a subjective speed with <200 m analyzed was the second most common condition at 20%. Indoor running at an exact or subjective speed with one step or stride analyzed accounted for 12% of all conditions. Overall, 72% of all conditions were indoors; and in 67% of all conditions, the analyzed distance was one step or stride or <200 m. Most of those studies were published between 2015 and 2021.
Studies with less controlled running conditions were primarily published after 2018. A total of 17% of all conditions included runs of >1000 m in a single or multiple trials, and speed was not controlled in races or training runs for 8% of all conditions. The least controlled condition—outdoor running with speed not controlled for multiple trials > 1000 m—accounted for 4% of all conditions.
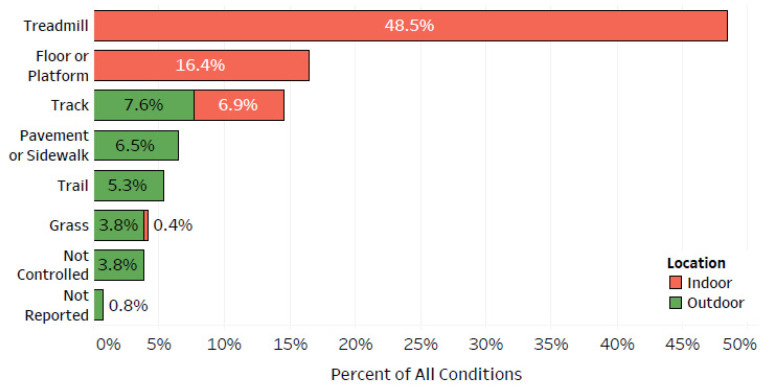
The running conditions were grouped by surface and location (Figure 3). Overall, 49% of all conditions were indoors on a treadmill, and an additional 16% were indoors on a floor or platform. Outdoor pavement or sidewalk, trail, grass, and not controlled running surfaces combined for 19% of all conditions.
Figure 3.
The percent of all conditions (262 across 231 studies) by running surface and location (indoor, outdoor).
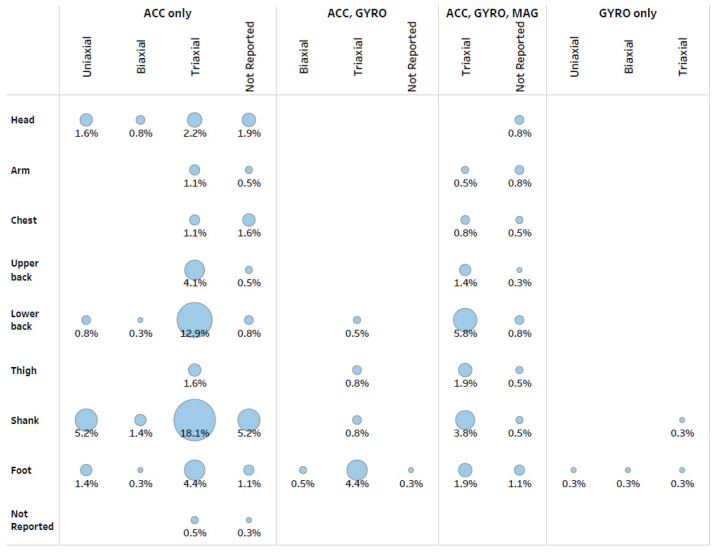
3.2.2. Device(s)
There were 365 combinations of devices with specific sensor/axis composition and device locations on the body (Figure 4). The most common combination was a triaxial accelerometer on the shank (18% of all combinations) followed by a triaxial accelerometer on the lower back (13%). Across all sensors with any number of axes, the top three device locations were the shank, lower back and foot, accounting for 35%, 22% and 16% of all combinations, respectively. Across any number of axes, 70% of all combinations used an accelerometer only, and 22% of all combinations used all three sensors. A gyroscope was the only sensor for 1% of all combinations and was placed on the foot or shank.
Figure 4.
The percent of all combinations of devices and locations of devices on the body (365 combinations across 231 studies) by body location and sensor/axis composition. The circles are sized relative to percentage to provide visual comparisons for the frequency of device and location combinations. ACC = accelerometer, GYRO = gyroscope, and MAG = magnetometer.
Some studies used multiple devices, bringing the total number of devices to 251. Most devices (82%) were of research-grade. The remaining 18% of devices are commercially available and designed for public use and include adidas Run Genie, Catapult, DorsaVi, Garmin, Google Nexus, Lumo Run, Milestone Pod, Polar, RunScribe, Runteq Zoi, Stryd, and Zephyr BioHarness. These devices were commonly worn on the shoe or lower or upper back.
3.2.3. Analysis
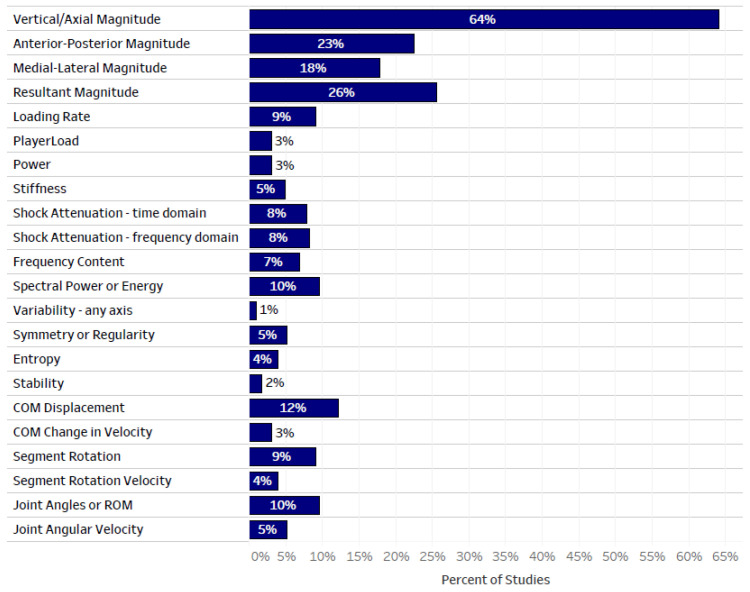
The reported metrics across all studies are shown in Figure 5. The most common metric was accelerometer magnitude, with vertical/axial, anterior–posterior, medial–lateral and resultant magnitude reported in 64%, 23%, 18% and 26% of all studies, respectively. (Note: studies often reported multiple metrics, and therefore the sum of the percentages is greater than 100%.) The acceleration quantity was also reported in metrics such as loading rate, PlayerLoad, power and stiffness, with loading rate being the most common (9% of all studies). Shock attenuation was reported in 7% of all studies using time domain calculations and in 8% of all studies using frequency domain calculations. Signal frequency content was reported in 7% of all studies and the spectral power or energy was reported in 9% of all studies. Signal consistency, represented by metrics such as variability, symmetry or regularity, entropy, and stability, was reported in 5% or less of all studies, each. Segment (including center of mass) or joint kinematics were reported in up to 12% of studies, with measures of displacement more common than measures of velocity.
Figure 5.
The percent of all studies that reported each metric. Note: studies often reported multiple metrics, and therefore the sum of all percentages is greater than 100%. COM = center of mass; ROM = range of motion.
In terms of a statistical approach, 91% of all studies used inferential statistics, 2% used machine learning, and 7% presented results descriptively. The most common metrics reported in studies that used a machine learning statistical approach were vertical/axial magnitude, anterior–posterior magnitude, and joint angles or range of motion.
3.2.4. Participants
Half of the studies included male and female participants, 35% included males only, 3% included females only, and the sex of participants was not specified in 12% of all studies. Participants were uninjured in 99% of all studies. The mean participant age within a study ranged from 5 to 59 years, with an average of 27 years across all studies.
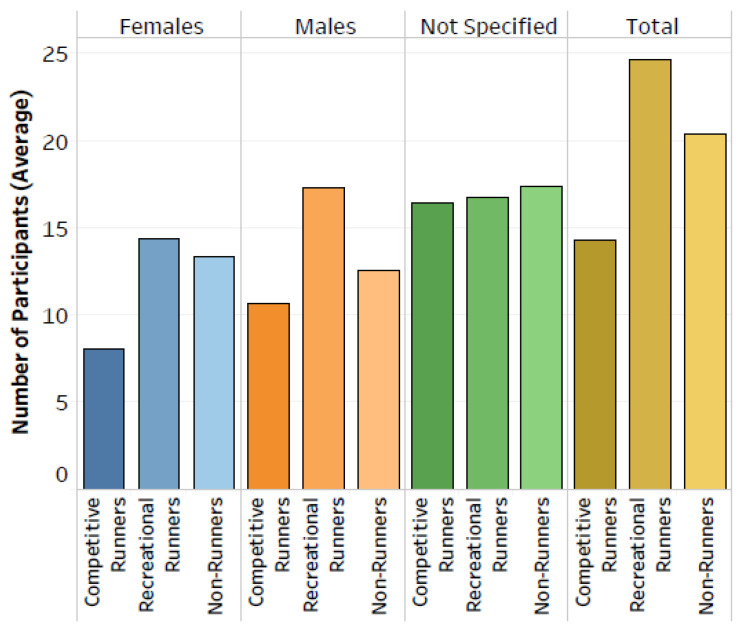
Recreational runners, non-runners and competitive runners were participants in 56%, 30% and 17% of all studies, respectively. (Note: some studies included multiple participant types, and therefore the sum of the percentages is greater than 100%.) The average number of participants reported for each participant type and sex is shown in Figure 6. With an average of 25 participants per study, recreational runners had the greatest number of participants per study, followed by non-runners (n = 20) then competitive runners (n = 14). This pattern was consistent when separated by males and females, and the average number of male recreational and competitive runners was greater than the average number of females in each group.
Figure 6.
The average number of participants for each participant type and sex. Averages are reported across studies that included the given participant type and sex.
3.2.5. Study Details
Studies were conducted in 27 different countries. The USA had the most studies (29%), followed by Canada at 9%. In total, 39% of studies were conducted in 11 European countries.
One-quarter of the studies had interventions: 24% were quasi-experimental and 1% were randomized controlled trials. Two-thirds of the interventions (17% of all studies) were equipment-based and one-third (9% of all studies) involved training interventions. The remaining 75% of studies were observational, and 95% of observational studies (71% of all studies) used a cross-sectional study design. Prospective and retrospective cohorts accounted for 2% and <1% of studies, respectively, and 2% of studies were case studies or case control. The most common purpose (22% of studies) was to determine the validity or reliability of metrics, and 16% of studies compared metrics. In 20% of studies, the purpose was to identify changes in conditions not related to fatigue or different sessions. Differences in gait due to group membership, fatigue and sessions were reported in 13%, 12% and 2% of studies, respectively. Associations of gait metrics with performance and injury were reported for less than 2% of studies, each. (Note: some studies had multiple purposes, and therefore the sum of the percentages is greater than 100%).
3.3. Quality Assessment
There was an adequate amount of information provided for the conditions (92% of studies), devices (91%), analysis (93%), participants (83%) and study details (100%). Additionally, the relevance to running and IMUs was deemed appropriate for the conditions (99% of studies), devices (100%), analysis (100%), participants (98%) and study details (99%).
4. Discussion
The primary purpose of this review was to systematically identify how IMUs are used to record running biomechanics across real-world settings and describe the conditions in which IMU data were collected. Identifying the characteristics of IMU-based running biomechanical studies serves to mark the progress made and the steps that remain for analyzing running gait in real-world settings.
4.1. Running Environments
Laboratory-based conditions are controlled and are often different from typical running conditions, as most runners complete their runs outdoors [243]. Additionally, loads vary with each stride and a runner’s load capacity changes throughout a running session [244], suggesting that assigning the same estimated load to each stride is not a suitable approximation for the cumulative load in a running session. Therefore, it is important to monitor running in actual real-world conditions, including over long distances. Yet, despite the portability of IMUs [6,7], one of the main findings of this review is that running biomechanics are mainly recorded with IMUs indoors, on a treadmill, at prescribed speeds, and over small distances. Furthermore, the majority of studies that investigated running in artificial environments have been published recently; there has not been a trend away from laboratory-based conditions over time. It is unclear why researchers are using IMUs to record running, but still have participants running in the laboratory, at controlled speeds, on treadmills and/or over short distances. If the purpose of these devices is to capture real-world running, we suggest that the research in this area should move out of the lab to less controlled environments.
Several of the included studies compared running quality between surfaces, and the findings underscore the need to observe runners in their actual running environment. More unstable surfaces lead to less regularity and greater variability during running [5,142], and the variance in outdoor data cannot be explained by indoor measures [31,95]. Moreover, it is likely that not all metrics differ between the running conditions [245]. For example, there was no difference in running power on a track compared to a treadmill [166]. Among the four studies that compared tibial acceleration between treadmill and outdoor running, the acceleration magnitude was either lower [241], greater [31,95], or not different [84,241] in outdoor conditions compared to on the treadmill, but in only one case did the outdoor conditions represent an uncontrolled running environment [95]. We suggest that rather than estimating what it is like to run outdoors, it would be helpful to use IMUs during actual training runs, over longer distances and on surfaces that represent real-world running.
To our point, starting from 2015, some studies have followed athletes for uncontrolled training runs or races [188,200,201,202,206,207,210,211,212,213,220,221,225,226,227,230]. A myriad of external factors, such as weather, traffic, and surface conditions, could influence how someone runs and therefore, it is crucial to capture running patterns in the same settings that runners actually run. Additionally, just as multiple trials are often used in a laboratory setting, multiple runs are needed to establish running patterns in uncontrolled settings [213].
4.2. IMU Considerations
The ability to collect accurate and useful metrics from IMUs depends on the desired metrics, the sensor specifications, device placement, running styles, and user capabilities [4]. IMUs intended for long term monitoring need to be user-friendly. The commercial devices in the included studies were worn on the foot or upper or lower back. In contrast, the most common position for devices among all included studies was on the shank, where tibial acceleration in one or multiple axes was recorded. Tibial accelerations have been used in the context of stress fractures as well as to gauge impact forces at the shank and how they are distributed along the kinetic chain [32]. While devices designed for consumer use have not been developed for placement on the shank, a research-grade device was used to record tibial accelerations of nearly 200 runners during a marathon [95]. Future investigations of impact forces in actual running conditions should consider devices and placement that can be easily applied during long-term monitoring.
The metrics reported from accelerometer sensors, such as the magnitude of acceleration, loading rate and shock attenuation, are similar to metrics obtained from force plates. When the gyroscope and/or magnetometer sensors in an IMU are used, the reported metrics provide information on the kinematics, including segment and joint rotations [28,48,51,53,55,76,102,106,113,114,115,127,128,129,134,140,144,145,148,157,181,183,186,188,190,192,200,201,210,211,212,213,216,217,219,221,228,235]. While it is typical for IMUs to contain multiple sensors, most included studies only used an accelerometer sensor, limiting the reported metrics to those that resemble force plate metrics.
Many of the included studies were conducted in indoor settings because the purpose of the study was to evaluate the validity and reliability of IMU-based metrics compared to metrics from force plates or motion capture systems. Assessing strength of the validity and reliability was not within the scope of this review; however, devices that demonstrate adequate validity and reliability can be used in the field. Additionally, while metrics reported from an IMU are often chosen to be similar to metrics from force plates and motion capture systems, it is possible to report metrics specific to IMU signals (e.g., entropy, regularity, and symmetry) that monitor movement quality [246].
4.3. Changing Running Biomechanics
It is expected that equipment or training interventions that lead to changes in running biomechanics are needed to change injury rates. However, there is limited or conflicting evidence on the relationship between modifications of running biomechanics and running injuries [6,72,73]. It is also possible that lack of clarity on running injury risk factors is related to evaluation of biomechanical metrics in a laboratory setting before and after an intervention or injury observation, and not in the runner’s natural environment [2].
Short-term changes, observed within a laboratory session, may show how training or equipment interventions can change running patterns [72,151]. Some studies use an intervention that is more long term to allow for adaptation and assess movement patterns at baseline and follow up to observe changes [20,154]. If biomechanics are only recorded in a single session, or at baseline and follow up, it is possible to use laboratory equipment (e.g., force plates and motion capture), but this does not reflect how runners run during real-world conditions. The benefit of IMUs is that movement patterns can be measured during the intervention period in actual running settings to monitor changes over time. Yet just two of the intervention studies from this review analyzed metrics from IMUs during an intervention (i.e., not just pre- and post-intervention) that was greater than one session, plus the intervention runs were conducted on a treadmill in both studies [154,218].
IMUs can also be used to observe changes in running patterns throughout a single run. In studies investigating changes in running biomechanics due to fatigue, it is common to have participants run to the point of exhaustion. Reaching a state of exhaustion as defined in a study may occur in some training runs or races, but it is likely not a typical running strategy for all runners. Thus, it is important to look at how running patterns change during actual training runs. More prospective or retrospective studies are also needed that look at how running patterns change over time, especially when those changes precede an injury [4,8]. Only five of the included studies included injured runners [24,144,152,208,221]. Due to pain, running in an injured state is likely not representative of running prior to injury. While some included studies involved runners that were previously injured and others looked at runners that were eventually injured, the data on the running patterns were only observed at a point when the runners were not injured. Regardless, IMUs can facilitate continuous monitoring that will allow for observation of changes in running patterns that lead to injury.
4.4. Participant Characteristics
Over 75% of runners use wearables, and most runners use wearable technology to monitor spatiotemporal parameters, such as distance or speed [247,248,249]. Competitive runners are more likely to use wearables to monitor running form or biomechanics than recreational runners [249]. Even if runners are not personally using IMUs that monitor their biomechanics, based on the results of survey studies, runners have a large appetite for using and consuming data from wearable technology [247,249]. Yet the number of participants in the included studies is low. Considering the popularity of running and runners’ attitudes towards wearable technology, investigations of real-world running biomechanics should be able to recruit large numbers of participants. A bigger pool of participants will enable better comparisons across participant types and consider sex differences as injury rates differ between sexes [250]. Based on race participation statistics, there are more female than male runners [251]. However, consistent with previous findings that show females are underrepresented in sport and exercise medicine research [252], we found that the running and IMU literature is also heavily focused on male runners, with only 3% of studies being female specific.
4.5. Limitations
There are some limitations to this review, based on the exclusion criteria. First, the only type of wearable technology considered was IMUs. Limiting the search to only IMUs excluded studies that only utilized GPS devices, which are very common among runners [249]. Additional types of wearable technology that were not included in this review are heart rate monitors, mobile phone apps that did not utilize the phone’s IMU sensors, and pressure-sensing insoles. Second, studies were excluded if they only reported spatiotemporal metrics. IMUs can be used to derive valid and reliable spatiotemporal stride parameters that capture running quantity [253]; however, load magnitude and distribution are also needed on a per stride basis to evaluate injury risk [244]. Finally, we excluded studies that focused on the development of new technology or methods, which eliminated some studies that reported novel machine learning algorithms. Whilst wearable technology is a growing field, future advancements will hopefully improve our ability to monitor real-world running.
There was no meta-analysis or formal quality assessment of each study as these are not expected for a scoping review. Based on our subjective evaluation, nearly all studies were appropriate to the topic of running and IMUs and contained adequate information for inclusion in this scoping review. Most likely, a more rigorous evaluation of study quality would have revealed overall weak levels of evidence across this field of study. We leave it to future systematic reviews and meta-analyses of specific outcomes and populations to use objective protocols for evaluating study quality.
5. Conclusions
Despite the portability of IMUs, one of the main findings of this review is that running biomechanics are mainly recorded with IMUs indoors, on a treadmill, at prescribed speeds, and over small distances. While it is challenging to collect data in real-world conditions due to the myriad of extrinsic factors such as weather, traffic, and surface conditions, our results indicate the vast majority of studies do not capture running biomechanical data in the same settings that runners actually run. Moreover, while it is typical for IMUs to contain multiple sensors, most included studies only used data derived from the accelerometer sensor and most studies involved placement of the IMU at the shank. Finally, the number of participants in the included studies is low and our findings show that research is still heavily focused on male runners, with only 3% of studies being female specific. Overall, considering that the purpose of IMU devices is to capture real-world running, we suggest that future research in this area should move out of the lab to less controlled and more real-world environments.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author Contributions
Conceptualization, L.C.B., A.M.R., C.A.C. and R.F.; methodology, L.C.B., A.M.R., C.A.C. and R.F.; formal analysis, L.C.B., A.M.R. and C.A.C.; data curation, L.C.B.; writing—original draft preparation, L.C.B. and A.M.R.; writing—review and editing, L.C.B., A.M.R., C.A.C. and R.F.; visualization, L.C.B. All authors have read and agreed to the published version of the manuscript.
Funding
This study was partially funded by the NSERC CREATE Wearable Technology Research and Collaboration (We-TRAC) Training Program (Project No. CREATE/511166-2018).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All data are available within this manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Benson L.C., Räisänen A.M., Volkova V.G., Pasanen K., Emery C.A. Workload a-WEAR-ness: Monitoring Workload in Team Sports with Wearable Technology. A Scoping Review. J. Orthop. Sports Phys. Ther. 2020;50:549–563. doi: 10.2519/jospt.2020.9753. [DOI] [PubMed] [Google Scholar]
- 2.Willy R.W. Innovations and pitfalls in the use of wearable devices in the prevention and rehabilitation of running related injuries. Phys. Ther. Sport. 2018;29:26–33. doi: 10.1016/j.ptsp.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Moore I.S., Willy R.W. Use of Wearables: Tracking and Retraining in Endurance Runners. Curr. Sports Med. Rep. 2019;18:437–444. doi: 10.1249/JSR.0000000000000667. [DOI] [PubMed] [Google Scholar]
- 4.Johnston W., Heiderscheit B. Mobile Technology in Running Science and Medicine: Are We Ready? J. Orthop. Sports Phys. Ther. 2019;49:122–125. doi: 10.2519/jospt.2019.0604. [DOI] [PubMed] [Google Scholar]
- 5.Benson L.C., Clermont C.A., Ferber R. New Considerations for Collecting Biomechanical Data Using Wearable Sensors: The Effect of Different Running Environments. Front. Bioeng. Biotechnol. 2020;8:86. doi: 10.3389/fbioe.2020.00086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Hooren B., Goudsmit J., Restrepo J., Vos S. Real-time feedback by wearables in running: Current approaches, challenges and suggestions for improvements. J. Sports Sci. 2020;38:214–230. doi: 10.1080/02640414.2019.1690960. [DOI] [PubMed] [Google Scholar]
- 7.Napier C., Esculier J.-F., Hunt M.A. Gait retraining: Out of the lab and onto the streets with the benefit of wearables. Br. J. Sports Med. 2017;51:1642–1643. doi: 10.1136/bjsports-2017-098637. [DOI] [PubMed] [Google Scholar]
- 8.Benson L.C., Clermont C.A., Bošnjak E., Ferber R. The use of wearable devices for walking and running gait analysis outside of the lab: A systematic review. Gait Posture. 2018;63:124–138. doi: 10.1016/j.gaitpost.2018.04.047. [DOI] [PubMed] [Google Scholar]
- 9.Watari R., Hettinga B., Osis S., Ferber R. Validation of a Torso-Mounted Accelerometer for Measures of Vertical Oscillation and Ground Contact Time During Treadmill Running. J. Appl. Biomech. 2016;32:306–310. doi: 10.1123/jab.2015-0200. [DOI] [PubMed] [Google Scholar]
- 10.Benson L.C., Clermont C.A., Watari R., Exley T., Ferber R. Automated accelerometer-based gait event detection during multiple running conditions. Sensors. 2019;19:1483. doi: 10.3390/s19071483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lenhart R.L., Thelen D.G., Wille C.M., Chumanov E.S., Heiderscheit B.C. Increasing Running Step Rate Reduces Patellofemoral Joint Forces. Med. Sci. Sports Exerc. 2014;46:557–564. doi: 10.1249/MSS.0b013e3182a78c3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hafer J., Brown A.M., DeMille P., Hillstrom H.J., Garber C. The effect of a cadence retraining protocol on running biomechanics and efficiency: A pilot study. J. Sports Sci. 2015;33:724–731. doi: 10.1080/02640414.2014.962573. [DOI] [PubMed] [Google Scholar]
- 13.Bood R.J., Nijssen M., van der Kamp J., Roerdink M. The Power of Auditory-Motor Synchronization in Sports: Enhancing Running Performance by Coupling Cadence with the Right Beats. PLoS ONE. 2013;8:e70758. doi: 10.1371/journal.pone.0070758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Billat V.L., Mille-Hamard L., Petit B., Koralsztein J.P. The Role of Cadence on the V˙O2 Slow Component in Cycling and Running in Triathletes. Int. J. Sports Med. 1999;20:429–437. doi: 10.1055/s-1999-8825. [DOI] [PubMed] [Google Scholar]
- 15.Aubol K.G., Hawkins J.L., Milner C.E. Tibial Acceleration Reliability and Minimal Detectable Difference During Overground and Treadmill Running. J. Appl. Biomech. 2020;36:457–459. doi: 10.1123/jab.2019-0272. [DOI] [PubMed] [Google Scholar]
- 16.Blackah N., Bradshaw E.J., Kemp J.G., Shoushtarian M. The Effect of Exercise-Induced Muscle Damage on Shock Dissipation during Treadmill Running. Asian J. Exerc. Sports Sci. 2013;10:16–30. [Google Scholar]
- 17.Boyer K.A., Nigg B.M. Soft tissue vibrations within one soft tissue compartment. J. Biomech. 2006;39:645–651. doi: 10.1016/j.jbiomech.2005.01.027. [DOI] [PubMed] [Google Scholar]
- 18.Chadefaux D., Gueguen N., Thouze A., Rao G. 3D propagation of the shock-induced vibrations through the whole lower-limb during running. J. Biomech. 2019;96:109343. doi: 10.1016/j.jbiomech.2019.109343. [DOI] [PubMed] [Google Scholar]
- 19.Clansey A.C., Hanlon M., Wallace E.S., Lake M.J. Effects of Fatigue on Running Mechanics Associated with Tibial Stress Fracture Risk. Med. Sci. Sports Exerc. 2012;44:1917–1923. doi: 10.1249/MSS.0b013e318259480d. [DOI] [PubMed] [Google Scholar]
- 20.Crowell H.P., Davis I.S. Gait retraining to reduce lower extremity loading in runners. Clin. Biomech. 2011;26:78–83. doi: 10.1016/j.clinbiomech.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Edwards S., White S., Humphreys S., Robergs R., O’Dwyer N. Caution using data from triaxial accelerometers housed in player tracking units during running. J. Sports Sci. 2018;37:810–818. doi: 10.1080/02640414.2018.1527675. [DOI] [PubMed] [Google Scholar]
- 22.Gil-Rey E., Deere K.C., Maldonado-Martín S., Palacios-Samper N., Azpeitia A., Gorostiaga E.M., Tobias J. Investigation of the Relationship Between Peak Vertical Accelerations and Aerobic Exercise Intensity During Graded Walking and Running in Postmenopausal Women. J. Aging Phys. Act. 2021;29:71–79. doi: 10.1123/japa.2019-0256. [DOI] [PubMed] [Google Scholar]
- 23.Hagen M., Hennig E.M. Effects of different shoe-lacing patterns on the biomechanics of running shoes. J. Sports Sci. 2009;27:267–275. doi: 10.1080/02640410802482425. [DOI] [PubMed] [Google Scholar]
- 24.Havens K.L., Cohen S.C., Pratt K.A., Sigward S.M. Accelerations from wearable accelerometers reflect knee loading during running after anterior cruciate ligament reconstruction. Clin. Biomech. 2018;58:57–61. doi: 10.1016/j.clinbiomech.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 25.Higgins S., Higgins L.Q., Vallabhajosula S. Site-specific Concurrent Validity of the ActiGraph GT9X Link in the Estimation of Activity-related Skeletal Loading. Med. Sci. Sports Exerc. 2021;53:951–959. doi: 10.1249/MSS.0000000000002562. [DOI] [PubMed] [Google Scholar]
- 26.Lam W.-K., Liebenberg J., Woo J., Park S.-K., Yoon S.-H., Cheung R.T.H., Ryu J. Do running speed and shoe cushioning influence impact loading and tibial shock in basketball players? PeerJ. 2018;6:e4753. doi: 10.7717/peerj.4753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laughton C.A., Davis I.M., Hamill J. Effect of Strike Pattern and Orthotic Intervention on Tibial Shock during Running. J. Appl. Biomech. 2003;19:153–168. doi: 10.1123/jab.19.2.153. [DOI] [Google Scholar]
- 28.Mavor M.P., Ross G.B., Clouthier A.L., Karakolis T., Graham R.B. Validation of an IMU Suit for Military-Based Tasks. Sensors. 2020;20:4280. doi: 10.3390/s20154280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meinert I., Brown N., Alt W. Effect of Footwear Modifications on Oscillations at the Achilles Tendon during Running on a Treadmill and Over Ground: A Cross-Sectional Study. PLoS ONE. 2016;11:e0152435. doi: 10.1371/journal.pone.0152435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mercer J.A., Bezodis N.E., Russell M., Purdy A., Delion D. Kinetic consequences of constraining running behavior. J. Sports Sci. Med. 2005;4:144–152. [PMC free article] [PubMed] [Google Scholar]
- 31.Milner C.E., Hawkins J.L., Aubol K.G. Tibial Acceleration during Running Is Higher in Field Testing Than Indoor Testing. Med. Sci. Sports Exerc. 2020;52:1361–1366. doi: 10.1249/MSS.0000000000002261. [DOI] [PubMed] [Google Scholar]
- 32.Milner C.E., Ferber R., Pollard C.D., Hamill J., Davis I.S. Biomechanical Factors Associated with Tibial Stress Fracture in Female Runners. Med. Sci. Sports Exerc. 2006;38:323–328. doi: 10.1249/01.mss.0000183477.75808.92. [DOI] [PubMed] [Google Scholar]
- 33.Nedergaard N.J., Verheul J., Drust B., Etchells T., Lisboa P., Robinson M.A., Vanrenterghem J. The feasibility of predicting ground reaction forces during running from a trunk accelerometry driven mass-spring-damper model. PeerJ. 2018;6:e6105. doi: 10.7717/peerj.6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ogon M., Aleksiev A.R., Spratt K.F., Pope M.H., Saltzman C.L. Footwear Affects the Behavior of Low Back Muscles When Jogging. Int. J. Sports Med. 2001;22:414–419. doi: 10.1055/s-2001-16240. [DOI] [PubMed] [Google Scholar]
- 35.Rowlands A., Stiles V. Accelerometer counts and raw acceleration output in relation to mechanical loading. J. Biomech. 2012;45:448–454. doi: 10.1016/j.jbiomech.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 36.Sayer T.A., Hinman R.S., Paterson K.L., Bennell K.L., Hall M., Allison K., Bryant A.L. Running-related muscle activation patterns and tibial acceleration across puberty. J. Electromyogr. Kinesiol. 2020;50:102381. doi: 10.1016/j.jelekin.2019.102381. [DOI] [PubMed] [Google Scholar]
- 37.Sinclair J., Dillon S. The Influence of Energy Boost and Springblade Footwear on The Kinetics and Kinematics of Running. Hum. Mov. 2016;17:112–118. doi: 10.1515/humo-2016-0010. [DOI] [Google Scholar]
- 38.Sinclair J., Sant B. The effects of cross-fit footwear on the kinetics and kinematics of running. Footwear Sci. 2016;9:41–48. doi: 10.1080/19424280.2016.1268212. [DOI] [Google Scholar]
- 39.Sinclair J., Fau-Goodwin J., Richards J., Shore H. The influence of minimalist and maximalist footwear on the kinetics and kinematics of running. Footwear Sci. 2016;8:33–39. doi: 10.1080/19424280.2016.1142003. [DOI] [PubMed] [Google Scholar]
- 40.Sinclair J., Naemi R., Chockalingam N., Taylor P.J., Shore H. The effects of shoe temperature on the kinetics and kinematics of running. Footwear Sci. 2015;7:173–180. doi: 10.1080/19424280.2015.1084389. [DOI] [Google Scholar]
- 41.Sinclair J., Rooney E., Naemi R., Atkins S., Chockalingam N. Effects of Footwear Variations on Three-Dimensional Kinematics and Tibial Accelerations of Specific Movements in American Football. J. Mech. Med. Biol. 2017;17:1750026. doi: 10.1142/S0219519417500269. [DOI] [Google Scholar]
- 42.Thompson M., Seegmiller J., McGowan C.P. Impact Accelerations of Barefoot and Shod Running. Int. J. Sports Med. 2016;37:364–368. doi: 10.1055/s-0035-1569344. [DOI] [PubMed] [Google Scholar]
- 43.Trama R., Blache Y., Hautier C. Effect of rocker shoes and running speed on lower limb mechanics and soft tissue vibrations. J. Biomech. 2019;82:171–177. doi: 10.1016/j.jbiomech.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 44.Berghe P.V.D., Six J., Gerlo J., Leman M., De Clercq D. Validity and reliability of peak tibial accelerations as real-time measure of impact loading during over-ground rearfoot running at different speeds. J. Biomech. 2019;86:238–242. doi: 10.1016/j.jbiomech.2019.01.039. [DOI] [PubMed] [Google Scholar]
- 45.Wundersitz D.W.T., Netto K.J., Aisbett B., Gastin P.B. Validity of an upper-body-mounted accelerometer to measure peak vertical and resultant force during running and change-of-direction tasks. Sports Biomech. 2013;12:403–412. doi: 10.1080/14763141.2013.811284. [DOI] [PubMed] [Google Scholar]
- 46.Adams D., Pozzi F., Carroll A., Rombach A., Zeni J. Validity and Reliability of a Commercial Fitness Watch for Measuring Running Dynamics. J. Orthop. Sports Phys. Ther. 2016;46:471–476. doi: 10.2519/jospt.2016.6391. [DOI] [PubMed] [Google Scholar]
- 47.Adams D., Pozzi F., Willy R.W., Carrol A., Zeni J. Altering Cadence or Vertical Oscillation During Running: Effects on Running Related Injury Factors. Int. J. Sports Phys. Ther. 2018;13:633–642. doi: 10.26603/ijspt20180633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bayram H.A., Yalcin B. The influence of biofeedback on physiological and kinematic variables of treadmill running. Int. J. Perform. Anal. Sport. 2021;21:156–169. doi: 10.1080/24748668.2020.1861898. [DOI] [Google Scholar]
- 49.Armitage M., Beato M., McErlain-Naylor S.A. Inter-unit reliability of IMU Step metrics using IMeasureU Blue Trident inertial measurement units for running-based team sport tasks. J. Sports Sci. 2021;39:1512–1518. doi: 10.1080/02640414.2021.1882726. [DOI] [PubMed] [Google Scholar]
- 50.Backes A., Skejø S.D., Gette P., Nielsen R.Ø., Sørensen H., Morio C., Malisoux L. Predicting cumulative load during running using field-based measures. Scand. J. Med. Sci. Sports. 2020;30:2399–2407. doi: 10.1111/sms.13796. [DOI] [PubMed] [Google Scholar]
- 51.Bailey G.P., Harle R.K. Sampling Rates and Sensor Requirements for Kinematic Assessment During Running Using Foot Mounted IMUs. Interakt. Syst. 2015;556:42–56. doi: 10.1007/978-3-319-25249-0_4. [DOI] [Google Scholar]
- 52.Barnes M., Guy J., Elsworthy N., Scanlan A. A Comparison of PlayerLoadTM and Heart Rate during Backwards and Forwards Locomotion during Intermittent Exercise in Rugby League Players. Sports. 2021;9:21. doi: 10.3390/sports9020021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bastiaansen B., Wilmes E., Brink M., De Ruiter C.J., Savelsbergh G.J., Steijlen A., Jansen K., Van Der Helm F.C., Goedhart E.A., Van Der Laan D., et al. An Inertial Measurement Unit Based Method to Estimate Hip and Knee Joint Kinematics in Team Sport Athletes on the Field. J. Vis. Exp. 2020:e60857. doi: 10.3791/60857. [DOI] [PubMed] [Google Scholar]
- 54.Benson L.C., Clermont C.A., Osis S.T., Kobsar D., Ferber R. Classifying running speed conditions using a single wearable sensor: Optimal segmentation and feature extraction methods. J. Biomech. 2018;71:94–99. doi: 10.1016/j.jbiomech.2018.01.034. [DOI] [PubMed] [Google Scholar]
- 55.Bergamini E., Picerno P., Pillet H., Natta F., Thoreux P., Camomilla V. Estimation of temporal parameters during sprint running using a trunk-mounted inertial measurement unit. J. Biomech. 2012;45:1123–1126. doi: 10.1016/j.jbiomech.2011.12.020. [DOI] [PubMed] [Google Scholar]
- 56.Boey H., Aeles J., Schütte K., Vanwanseele B. The effect of three surface conditions, speed and running experience on vertical acceleration of the tibia during running. Sports Biomech. 2016;16:166–176. doi: 10.1080/14763141.2016.1212918. [DOI] [PubMed] [Google Scholar]
- 57.Boyer K.A., Nigg B.M. Quantification of the input signal for soft tissue vibration during running. J. Biomech. 2007;40:1877–1880. doi: 10.1016/j.jbiomech.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 58.Boyer K.A., Nigg B.M. Muscle activity in the leg is tuned in response to impact force characteristics. J. Biomech. 2004;37:1583–1588. doi: 10.1016/j.jbiomech.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 59.Brayne L., Barnes A., Heller B., Wheat J. Using a wireless consumer accelerometer to measure tibial acceleration during running: Agreement with a skin-mounted sensor. Sports Eng. 2018;21:487–491. doi: 10.1007/s12283-018-0271-4. [DOI] [Google Scholar]
- 60.Buchheit M., Gray A., Morin J.-B. Assessing Stride Variables and Vertical Stiffness with GPS-Embedded Accel-erometers: Preliminary Insights for the Monitoring of Neuromuscular Fatigue on the Field. J. Sports Sci. Med. 2015;14:698–701. [PMC free article] [PubMed] [Google Scholar]
- 61.Butler R.J., Davis I.M., Laughton C.M., Hughes M. Dual-Function Foot Orthosis: Effect on Shock and Control of Rearfoot Motion. Foot Ankle Int. 2003;24:410–414. doi: 10.1177/107110070302400506. [DOI] [PubMed] [Google Scholar]
- 62.Camelio K., Gruber A.H., Powell D.W., Paquette M.R. Influence of Prolonged Running and Training on Tibial Acceleration and Movement Quality in Novice Runners. J. Athl. Train. 2020;55:1292–1299. doi: 10.4085/1062-6050-0491.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Carrier B., Creer A., Williams L.R., Holmes T.M., Jolley B.D., Dahl S., Weber E., Standifird T. Validation of Garmin Fenix 3 HR Fitness Tracker Biomechanics and Metabolics (VO2max) J. Meas. Phys. Behav. 2020;3:331–337. doi: 10.1123/jmpb.2019-0066. [DOI] [Google Scholar]
- 64.Castillo E.R., Lieberman D.E. Shock attenuation in the human lumbar spine during walking and running. J. Exp. Biol. 2018;221:jeb177949. doi: 10.1242/jeb.177949. [DOI] [PubMed] [Google Scholar]
- 65.Chen C.-H., Yang W.-W., Chen Y.-P., Chen V.C.-F., Liu C., Shiang T.-Y. High vibration frequency of soft tissue occurs during gait in power-trained athletes. J. Sports Sci. 2021;39:439–445. doi: 10.1080/02640414.2020.1824366. [DOI] [PubMed] [Google Scholar]
- 66.Cheung R.T.H., An W.W., Au I.P.H., Zhang J.H., Chan Z.Y.S., MacPhail A.J. Control of impact loading during distracted running before and after gait retraining in runners. J. Sports Sci. 2017;36:1497–1501. doi: 10.1080/02640414.2017.1398886. [DOI] [PubMed] [Google Scholar]
- 67.Cheung R.T.H., Zhang J.H., Chan Z.Y.S., An W.W., Au I.P., MacPhail A., Davis I.S. Shoe-mounted accelerometers should be used with caution in gait retraining. Scand. J. Med. Sci. Sports. 2019;29:835–842. doi: 10.1111/sms.13396. [DOI] [PubMed] [Google Scholar]
- 68.Ching E., An W.W.-K., Au I.P.H., Zhang J.H., Chan Z.Y., Shum G., Cheung R.T. Impact Loading During Distracted Running Before and After Auditory Gait Retraining. Int. J. Sports Med. 2018;39:1075–1080. doi: 10.1055/a-0667-9875. [DOI] [PubMed] [Google Scholar]
- 69.Chu J.J., Caldwell G.E. Stiffness and Damping Response Associated with Shock Attenuation in Downhill Running. J. Appl. Biomech. 2004;20:291–308. doi: 10.1123/jab.20.3.291. [DOI] [Google Scholar]
- 70.Clark R.A., Bartold S., Bryant A.L. Tibial acceleration variability during consecutive gait cycles is influenced by the menstrual cycle. Clin. Biomech. 2010;25:557–562. doi: 10.1016/j.clinbiomech.2010.03.002. [DOI] [PubMed] [Google Scholar]
- 71.Creaby M.W., Smith M.M.F. Retraining running gait to reduce tibial loads with clinician or accelerometry guided feedback. J. Sci. Med. Sport. 2016;19:288–292. doi: 10.1016/j.jsams.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 72.Crowell H.P., Milner C.E., Hamill J., Davis I.S. Reducing Impact Loading During Running With the Use of Real-Time Visual Feedback. J. Orthop. Sports Phys. Ther. 2010;40:206–213. doi: 10.2519/jospt.2010.3166. [DOI] [PubMed] [Google Scholar]
- 73.Day E.M., Alcantara R.S., McGeehan M.A., Grabowski A.M., Hahn M.E. Low-pass filter cutoff frequency affects sacral-mounted inertial measurement unit estimations of peak vertical ground reaction force and contact time during treadmill running. J. Biomech. 2021;119:110323. doi: 10.1016/j.jbiomech.2021.110323. [DOI] [PubMed] [Google Scholar]
- 74.De La Fuente C., Henriquez H., Andrade D.C., Yañez A. Running Footwear with Custom Insoles for Pressure Distribution Are Appropriate to Diminish Impacts After Shin Splints. Asian J. Sports Med. 2019;10:1–7. doi: 10.5812/asjsm.82461. [DOI] [Google Scholar]
- 75.Deflandre D., Miny K., Schwartz C., Dardenne N., Leclerc A.F., Bury T. Myotest efficiency in the mechanical analysis of the stride. Gazzetta Medica Ital. Arch. Sci. Mediche. 2018;177:293–300. doi: 10.23736/S0393-3660.17.03568-9. [DOI] [Google Scholar]
- 76.DeJong M.A.F., Hertel J. Validation of Foot-Strike Assessment Using Wearable Sensors During Running. J. Athl. Train. 2020;55:1307–1310. doi: 10.4085/1062-6050-0520.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Derrick T.R., Dereu D., McLean S.P. Impacts and kinematic adjustments during an exhaustive run. Med. Sci. Sports Exerc. 2002;34:998–1002. doi: 10.1097/00005768-200206000-00015. [DOI] [PubMed] [Google Scholar]
- 78.Dufek J.S., Mercer J.A., Griffin J.R. The Effects of Speed and Surface Compliance on Shock Attenuation Characteristics for Male and Female Runners. J. Appl. Biomech. 2009;25:219–228. doi: 10.1123/jab.25.3.219. [DOI] [PubMed] [Google Scholar]
- 79.Eggers T.M., Massard T.I., Clothier P.J., Lovell R. Measuring Vertical Stiffness in Sport With Accelerometers: Exercise Caution! J. Strength Cond. Res. 2018;32:1919–1922. doi: 10.1519/JSC.0000000000002318. [DOI] [PubMed] [Google Scholar]
- 80.Encarnación-Martínez A., Sanchis-Sanchis R., Pérez-Soriano P., García-Gallart A. Relationship between muscular extensibility, strength and stability and the transmission of impacts during fatigued running. Sports Biomech. 2020:1–17. doi: 10.1080/14763141.2020.1797863. [DOI] [PubMed] [Google Scholar]
- 81.Encarnación-Martínez A., García-Gallart A., Gallardo A.M., Sánchez-Sáez J.A., Sánchez-Sánchez J. Effects of structural components of artificial turf on the transmission of impacts in football players. Sports Biomech. 2017;17:251–260. doi: 10.1080/14763141.2017.1285347. [DOI] [PubMed] [Google Scholar]
- 82.Encarnación-Martínez A., Pérez-Soriano P., Sanchis-Sanchis R., García-Gallart A., Berenguer-Vidal R. Validity and Reliability of an Instrumented Treadmill with an Accelerometry System for Assessment of Spatio-Temporal Parameters and Impact Transmission. Sensors. 2021;21:1758. doi: 10.3390/s21051758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Friesenbichler B., Stirling L.M., Federolf P., Nigg B.M. Tissue vibration in prolonged running. J. Biomech. 2011;44:116–120. doi: 10.1016/j.jbiomech.2010.08.034. [DOI] [PubMed] [Google Scholar]
- 84.Fu W., Fang Y., Liu D.M.S., Wang L., Ren S., Liu Y. Surface effects on in-shoe plantar pressure and tibial impact during running. J. Sport Health Sci. 2015;4:384–390. doi: 10.1016/j.jshs.2015.09.001. [DOI] [Google Scholar]
- 85.Gantz A.M., Derrick T.R. Kinematics and metabolic cost of running on an irregular treadmill surface. J. Sports Sci. 2017;36:1103–1110. doi: 10.1080/02640414.2017.1357829. [DOI] [PubMed] [Google Scholar]
- 86.Garcia M.C., Gust G., Bazett-Jones D.M. Tibial acceleration and shock attenuation while running over different surfaces in a trail environment. J. Sci. Med. Sport. 2021;24:1161–1165. doi: 10.1016/j.jsams.2021.03.006. [DOI] [PubMed] [Google Scholar]
- 87.García-Pérez J.A., Pérez-Soriano P., Belloch S.L., Lucas A., Sánchez-Zuriaga D. Effects of treadmill running and fatigue on impact acceleration in distance running. Sports Biomech. 2014;13:259–266. doi: 10.1080/14763141.2014.909527. [DOI] [PubMed] [Google Scholar]
- 88.Giandolini M., Poupard T., Gimenez P., Horvais N., Millet G., Morin J.-B., Samozino P. A simple field method to identify foot strike pattern during running. J. Biomech. 2014;47:1588–1593. doi: 10.1016/j.jbiomech.2014.03.002. [DOI] [PubMed] [Google Scholar]
- 89.Giandolini M., Horvais N., Farges Y., Samozino P., Morin J.-B. Impact reduction through long-term intervention in recreational runners: Midfoot strike pattern versus low-drop/low-heel height footwear. Eur. J. Appl. Physiol. 2013;113:2077–2090. doi: 10.1007/s00421-013-2634-7. [DOI] [PubMed] [Google Scholar]
- 90.Glassbrook D.J., Fuller J.T., Alderson J.A., Doyle T.L.A. Foot accelerations are larger than tibia accelerations during sprinting when measured with inertial measurement units. J. Sports Sci. 2019;38:248–255. doi: 10.1080/02640414.2019.1692997. [DOI] [PubMed] [Google Scholar]
- 91.Gullstrand L., Halvorsen K., Tinmark F., Eriksson M., Nilsson J. Measurements of vertical displacement in running, a methodological comparison. Gait Posture. 2009;30:71–75. doi: 10.1016/j.gaitpost.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 92.Hardin E.C., Hamill J. The Influence of Midsole Cushioning on Mechanical and Hematological Responses during a Prolonged Downhill Run. Res. Q. Exerc. Sport. 2002;73:125–133. doi: 10.1080/02701367.2002.10609001. [DOI] [PubMed] [Google Scholar]
- 93.Iosa M., Morelli D., Nisi E., Sorbara C., Negrini S., Gentili P., Paolucci S., Fusco A. Assessment of upper body accelerations in young adults with intellectual disabilities while walking, running, and dual-task running. Hum. Mov. Sci. 2014;34:187–195. doi: 10.1016/j.humov.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 94.Morelli D., Marro T., Paolucci S., Fusco A., Iosa M. Ability and Stability of Running and Walking in Children with Cerebral Palsy. Neuropediatrics. 2013;44:147–154. doi: 10.1055/s-0033-1336016. [DOI] [PubMed] [Google Scholar]
- 95.Johnson C.D., Outerleys J., Jamison S.T., Tenforde A.S., Ruder M., Davis I.S. Comparison of Tibial Shock during Treadmill and Real-World Running. Med. Sci. Sports Exerc. 2020;52:1557–1562. doi: 10.1249/MSS.0000000000002288. [DOI] [PubMed] [Google Scholar]
- 96.Johnson C.D., Outerleys J., Davis I.S. Relationships between tibial acceleration and ground reaction force measures in the medial-lateral and anterior-posterior planes. J. Biomech. 2021;117:110250. doi: 10.1016/j.jbiomech.2021.110250. [DOI] [PubMed] [Google Scholar]
- 97.Johnson C.D., Outerleys J., Tenforde A.S., Davis I.S. A comparison of attachment methods of skin mounted inertial measurement units on tibial accelerations. J. Biomech. 2020;113:110118. doi: 10.1016/j.jbiomech.2020.110118. [DOI] [PubMed] [Google Scholar]
- 98.Kawabata M., Goto K., Fukusaki C., Sasaki K., Hihara E., Mizushina T., Ishii N. Acceleration patterns in the lower and upper trunk during running. J. Sports Sci. 2013;31:1841–1853. doi: 10.1080/02640414.2013.805884. [DOI] [PubMed] [Google Scholar]
- 99.Kenneally-Dabrowski C.J., Serpell B.G., Spratford W. Are accelerometers a valid tool for measuring overground sprinting symmetry? Int. J. Sports Sci. Coach. 2017;13:270–277. doi: 10.1177/1747954117716790. [DOI] [Google Scholar]
- 100.Khassetarash A., Hassannejad R., Ettefagh M.M., Sari-Sarraf V. Fatigue and soft tissue vibration during prolonged running. Hum. Mov. Sci. 2015;44:157–167. doi: 10.1016/j.humov.2015.08.024. [DOI] [PubMed] [Google Scholar]
- 101.Kobsar D., Osis S.T., Hettinga B.A., Ferber R. Classification accuracy of a single tri-axial accelerometer for training background and experience level in runners. J. Biomech. 2014;47:2508–2511. doi: 10.1016/j.jbiomech.2014.04.017. [DOI] [PubMed] [Google Scholar]
- 102.Koldenhoven R.M., Hertel J. Validation of a Wearable Sensor for Measuring Running Biomechanics. Digit. Biomark. 2018;2:74–78. doi: 10.1159/000491645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Le Bris R., Billat V., Auvinet B., Chaleil D., Hamard L., Barrey E. Effect of fatigue on stride pattern continuously measured by an accelerometric gait recorder in middle distance runners. J. Sports Med. Phys. Fit. 2006;46:227–231. [PubMed] [Google Scholar]
- 104.LeDuc C., Tee J., Lacome M., Weakley J., Cheradame J., Ramirez C., Jones B. Convergent Validity, Reliability, and Sensitivity of a Running Test to Monitor Neuromuscular Fatigue. Int. J. Sports Physiol. Perform. 2020;15:1067–1073. doi: 10.1123/ijspp.2019-0319. [DOI] [PubMed] [Google Scholar]
- 105.Lee J.B., Sutter K.J., Askew C.D., Burkett B.J. Identifying symmetry in running gait using a single inertial sensor. J. Sci. Med. Sport. 2010;13:559–563. doi: 10.1016/j.jsams.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 106.Lee Y.-S., Ho C.-S., Shih Y., Chang S.-Y., Róbert F.J., Shiang T.-Y. Assessment of walking, running, and jumping movement features by using the inertial measurement unit. Gait Posture. 2015;41:877–881. doi: 10.1016/j.gaitpost.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 107.Lin S.-P., Sung W.-H., Kuo F.-C., Kuo T.B., Chen J.-J. Impact of Center-of-Mass Acceleration on the Performance of Ultramarathon Runners. J. Hum. Kinet. 2014;44:41–52. doi: 10.2478/hukin-2014-0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lindsay T.R., Yaggie J.A., McGregor S.J. A wireless accelerometer node for reliable and valid measurement of lumbar accelerations during treadmill running. Sports Biomech. 2016;15:11–22. doi: 10.1080/14763141.2015.1123760. [DOI] [PubMed] [Google Scholar]
- 109.Lindsay T.R., Yaggie J.A., McGregor S.J. Contributions of lower extremity kinematics to trunk accelerations during moderate treadmill running. J. Neuroeng. Rehabilit. 2014;11:162. doi: 10.1186/1743-0003-11-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lucas-Cuevas A.G., Encarnación-Martínez A., Camacho-García A., Llana-Belloch S., Pérez-Soriano P. The location of the tibial accelerometer does influence impact acceleration parameters during running. J. Sports Sci. 2016;35:1734–1738. doi: 10.1080/02640414.2016.1235792. [DOI] [PubMed] [Google Scholar]
- 111.Lucas-Cuevas A.G., Quesada J.I.P., Giménez J.V., Aparicio I., Jimenez-Perez I., Pérez-Soriano P. Initiating running barefoot: Effects on muscle activation and impact accelerations in habitually rearfoot shod runners. Eur. J. Sport Sci. 2016;16:1145–1152. doi: 10.1080/17461391.2016.1197317. [DOI] [PubMed] [Google Scholar]
- 112.Lucas-Cuevas A.G., García A.C., Llinares R., Quesada J.I.P., Llana-Belloch S., Pérez-Soriano P. Influence of custom-made and prefabricated insoles before and after an intense run. PLoS ONE. 2017;12:e0173179. doi: 10.1371/journal.pone.0173179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Macadam P., Nuell S., Cronin J.B., Diewald S., Neville J. Thigh positioned wearable resistance improves 40 m sprint performance: A longitudinal single case design study. J. Aust. Strength Cond. 2019;27:39–45. [Google Scholar]
- 114.Macadam P., Cronin J.B., Uthoff A.M., Nagahara R., Zois J., Diewald S., Tinwala F., Neville J. Thigh loaded wearable resistance increases sagittal plane rotational work of the thigh resulting in slower 50-m sprint times. Sports Biomech. 2020:1–12. doi: 10.1080/14763141.2020.1762720. [DOI] [PubMed] [Google Scholar]
- 115.Macadam P., Nuell S., Cronin J.B., Diewald S., Rowley R., Forster J., Fosch P. Load effects of thigh wearable resistance on angular and linear kinematics and kinetics during non-motorised treadmill sprint-running. Eur. J. Sport Sci. 2021;21:531–538. doi: 10.1080/17461391.2020.1764629. [DOI] [PubMed] [Google Scholar]
- 116.Macdermid P.W., Fink P.W., Stannard S.R. Shock attenuation, spatio-temporal and physiological parameter comparisons between land treadmill and water treadmill running. J. Sport Health Sci. 2015;6:482–488. doi: 10.1016/j.jshs.2015.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Mangubat A.L.S., Zhang J.H., Chan Z.Y.-S., MacPhail A.J., Au I.P.-H., Cheung R.T.-H. Biomechanical Outcomes Due to Impact Loading in Runners While Looking Sideways. J. Appl. Biomech. 2018;34:483–487. doi: 10.1123/jab.2017-0381. [DOI] [PubMed] [Google Scholar]
- 118.Masci I., Vannozzi G., Bergamini E., Pesce C., Getchell N., Cappozzo A. Assessing locomotor skills development in childhood using wearable inertial sensor devices: The running paradigm. Gait Posture. 2013;37:570–574. doi: 10.1016/j.gaitpost.2012.09.017. [DOI] [PubMed] [Google Scholar]
- 119.McGregor S.J., Busa M.A., Skufca J., Yaggie J.A., Bollt E.M. Control entropy identifies differential changes in complexity of walking and running gait patterns with increasing speed in highly trained runners. Chaos Interdiscip. J. Nonlinear Sci. 2009;19:026109. doi: 10.1063/1.3147423. [DOI] [PubMed] [Google Scholar]
- 120.Mercer J.A., Chona C. Stride length–velocity relationship during running with body weight support. J. Sport Health Sci. 2015;4:391–395. doi: 10.1016/j.jshs.2015.01.003. [DOI] [Google Scholar]
- 121.Mercer J.A., Vance J., Hreljac A., Hamill J. Relationship between shock attenuation and stride length during running at different velocities. Graefe’s Arch. Clin. Exp. Ophthalmol. 2002;87:403–408. doi: 10.1007/s00421-002-0646-9. [DOI] [PubMed] [Google Scholar]
- 122.Mercer J.A., Devita P., Derrick T.R., Bates B.T. Individual Effects of Stride Length and Frequency on Shock Attenuation during Running. Med. Sci. Sports Exerc. 2003;35:307–313. doi: 10.1249/01.MSS.0000048837.81430.E7. [DOI] [PubMed] [Google Scholar]
- 123.Mercer J.A., Dufek J.S., Mangus B.C., Rubley M.D., Bhanot K., Aldridge J.M. A Description of Shock Attenuation for Children Running. J. Athl. Train. 2010;45:259–264. doi: 10.4085/1062-6050-45.3.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Mercer J.A., Bates B.T., Dufek J., Hreljac A. Characteristics of shock attenuation during fatigued running. J. Sports Sci. 2003;21:911–919. doi: 10.1080/0264041031000140383. [DOI] [PubMed] [Google Scholar]
- 125.Meyer U., Ernst D., Schott S., Riera C., Hattendorf J., Romkes J., Granacher U., Göpfert B., Kriemler S. Validation of two accelerometers to determine mechanical loading of physical activities in children. J. Sports Sci. 2015;33:1702–1709. doi: 10.1080/02640414.2015.1004638. [DOI] [PubMed] [Google Scholar]
- 126.Meyer C., Mohr M., Falbriard M., Nigg S.R., Nigg B.M. Influence of footwear comfort on the variability of running kinematics. Footwear Sci. 2017;10:29–38. doi: 10.1080/19424280.2017.1388296. [DOI] [Google Scholar]
- 127.Mitschke C., Öhmichen M., Milani T.L. A Single Gyroscope Can Be Used to Accurately Determine Peak Eversion Velocity during Locomotion at Different Speeds and in Various Shoes. Appl. Sci. 2017;7:659. doi: 10.3390/app7070659. [DOI] [Google Scholar]
- 128.Mitschke C., Zaumseil F., Milani T.L. The influence of inertial sensor sampling frequency on the accuracy of measurement parameters in rearfoot running. Comput. Methods Biomech. Biomed. Eng. 2017;20:1502–1511. doi: 10.1080/10255842.2017.1382482. [DOI] [PubMed] [Google Scholar]
- 129.Mitschke C., Kiesewetter P., Milani T.L. The Effect of the Accelerometer Operating Range on Biomechanical Parameters: Stride Length, Velocity, and Peak Tibial Acceleration during Running. Sensors. 2018;18:130. doi: 10.3390/s18010130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Montgomery G., Abt G., Dobson C., Smith T., Ditroilo M. Tibial impacts and muscle activation during walking, jogging and running when performed overground, and on motorised and non-motorised treadmills. Gait Posture. 2016;49:120–126. doi: 10.1016/j.gaitpost.2016.06.037. [DOI] [PubMed] [Google Scholar]
- 131.Moran M., Rickert B.J., Greer B.K. Tibial Acceleration and Spatiotemporal Mechanics in Distance Runners During Reduced-Body-Weight Conditions. J. Sport Rehabilit. 2017;26:221–226. doi: 10.1123/jsr.2015-0141. [DOI] [PubMed] [Google Scholar]
- 132.Morrow M.M.B., Hurd W.J., Fortune E., Lugade V., Aufman K.R.K. Accelerations of the Waist and Lower Extremities over a Range of Gait Velocities to Aid in Activity Monitor Selection for Field-Based Studies. J. Appl. Biomech. 2014;30:581–585. doi: 10.1123/jab.2013-0264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Neugebauer J.M., Hawkins D.A., Beckett L. Estimating Youth Locomotion Ground Reaction Forces Using an Accelerometer-Based Activity Monitor. PLoS ONE. 2012;7:e48182. doi: 10.1371/journal.pone.0048182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Nüesch C., Roos E., Pagenstert G., Muendermann A. Measuring joint kinematics of treadmill walking and running: Comparison between an inertial sensor based system and a camera-based system. J. Biomech. 2017;57:32–38. doi: 10.1016/j.jbiomech.2017.03.015. [DOI] [PubMed] [Google Scholar]
- 135.O’Connor K.M., Hamill J. Does Running on a Cambered Road Predispose a Runner to Injury? J. Appl. Biomech. 2002;18:3–14. doi: 10.1123/jab.18.1.3. [DOI] [Google Scholar]
- 136.Provot T., Chiementin X., Oudin E., Bolaers F., Murer S. Validation of a High Sampling Rate Inertial Measurement Unit for Acceleration During Running. Sensors. 2017;17:1958. doi: 10.3390/s17091958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Provot T., Chiementin X., Bolaers F., Murer S. Effect of running speed on temporal and frequency indicators from wearable MEMS accelerometers. Sports Biomech. 2021;20:831–843. doi: 10.1080/14763141.2019.1607894. [DOI] [PubMed] [Google Scholar]
- 138.Rabuffetti M., Scalera G.M., Ferrarin M. Effects of Gait Strategy and Speed on Regularity of Locomotion Assessed in Healthy Subjects Using a Multi-Sensor Method. Sensors. 2019;19:513. doi: 10.3390/s19030513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Raper D.P., Witchalls J., Philips E.J., Knight E., Drew M.K., Waddington G. Use of a tibial accelerometer to measure ground reaction force in running: A reliability and validity comparison with force plates. J. Sci. Med. Sport. 2018;21:84–88. doi: 10.1016/j.jsams.2017.06.010. [DOI] [PubMed] [Google Scholar]
- 140.Reenalda J., Maartens E., Buurke J.H., Gruber A.H. Kinematics and shock attenuation during a prolonged run on the athletic track as measured with inertial magnetic measurement units. Gait Posture. 2019;68:155–160. doi: 10.1016/j.gaitpost.2018.11.020. [DOI] [PubMed] [Google Scholar]
- 141.Schütte K.H., Maas E.A., Exadaktylos V., Berckmans D., Venter R., Vanwanseele B. Wireless Tri-Axial Trunk Accelerometry Detects Deviations in Dynamic Center of Mass Motion Due to Running-Induced Fatigue. PLoS ONE. 2015;10:e0141957. doi: 10.1371/journal.pone.0141957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Schütte K.H., Aeles J., De Beéck T.O., van der Zwaard B.C., Venter R., Vanwanseele B. Surface effects on dynamic stability and loading during outdoor running using wireless trunk accelerometry. Gait Posture. 2016;48:220–225. doi: 10.1016/j.gaitpost.2016.05.017. [DOI] [PubMed] [Google Scholar]
- 143.Schütte K.H., Sackey S., Venter R., Vanwanseele B. Energy cost of running instability evaluated with wearable trunk accelerometry. J. Appl. Physiol. 2018;124:462–472. doi: 10.1152/japplphysiol.00429.2017. [DOI] [PubMed] [Google Scholar]
- 144.Setuain I., Lecumberri P., Izquierdo M. Sprint mechanics return to competition follow-up after hamstring injury on a professional soccer player: A case study with an inertial sensor unit based methodological approach. J. Biomech. 2017;63:186–191. doi: 10.1016/j.jbiomech.2017.08.010. [DOI] [PubMed] [Google Scholar]
- 145.Setuain I., Lecumberri P., Ahtiainen J.P., Mero A.A., Häkkinen K., Izquierdo M. Sprint mechanics evaluation using inertial sensor-based technology: A laboratory validation study. Scand. J. Med. Sci. Sports. 2017;28:463–472. doi: 10.1111/sms.12946. [DOI] [PubMed] [Google Scholar]
- 146.Sheerin K.R., Besier T., Reid D., Hume P.A. The one-week and six-month reliability and variability of three-dimensional tibial acceleration in runners. Sports Biomech. 2017;17:531–540. doi: 10.1080/14763141.2017.1371214. [DOI] [PubMed] [Google Scholar]
- 147.Sheerin K.R., Besier T., Reid D. The influence of running velocity on resultant tibial acceleration in runners. Sports Biomech. 2020;19:750–760. doi: 10.1080/14763141.2018.1546890. [DOI] [PubMed] [Google Scholar]
- 148.Shiang T.-Y., Hsieh T.-Y., Lee Y.-S., Wu C.-C., Yu M.-C., Mei C.-H., Tai I.-H. Determine the Foot Strike Pattern Using Inertial Sensors. J. Sens. 2016;2016:1–6. doi: 10.1155/2016/4759626. [DOI] [Google Scholar]
- 149.Simoni L., Pancani S., Vannetti F., Macchi C., Pasquini G. Relationship between Lower Limb Kinematics and Upper Trunk Acceleration in Recreational Runners. J. Healthc. Eng. 2020;2020:1–7. doi: 10.1155/2020/8973010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Stickford A.S., Chapman R.F., Johnston J.D., Stager J.M. Lower-Leg Compression, Running Mechanics, and Economy in Trained Distance Runners. Int. J. Sports Physiol. Perform. 2015;10:76–83. doi: 10.1123/ijspp.2014-0003. [DOI] [PubMed] [Google Scholar]
- 151.TenBroek T.M., Rodrigues P.A., Frederick E.C., Hamill J. Midsole Thickness Affects Running Patterns in Habitual Rearfoot Strikers During a Sustained Run. J. Appl. Biomech. 2014;30:521–528. doi: 10.1123/jab.2012-0224. [DOI] [PubMed] [Google Scholar]
- 152.Tenforde A.S., Hayano T., Jamison S.T., Outerleys J., Davis I.S. Tibial Acceleration Measured from Wearable Sensors Is Associated with Loading Rates in Injured Runners. PM&R. 2020;12:679–684. doi: 10.1002/pmrj.12275. [DOI] [PubMed] [Google Scholar]
- 153.Thomas J.M., Derrick T.R. Effects of Step Uncertainty on Impact Peaks, Shock Attenuation, and Knee/Subtalar Synchrony in Treadmill Running. J. Appl. Biomech. 2003;19:60–70. doi: 10.1123/jab.19.1.60. [DOI] [Google Scholar]
- 154.Tirosh O., Steinberg N., Nemet D., Eliakim A., Orland G. Visual feedback gait re-training in overweight children can reduce excessive tibial acceleration during walking and running: An experimental intervention study. Gait Posture. 2019;68:101–105. doi: 10.1016/j.gaitpost.2018.11.006. [DOI] [PubMed] [Google Scholar]
- 155.Tirosh O., Orland G., Eliakim A., Nemet D., Steinberg N. Tibial impact accelerations in gait of primary school children: The effect of age and speed. Gait Posture. 2017;57:265–269. doi: 10.1016/j.gaitpost.2017.06.270. [DOI] [PubMed] [Google Scholar]
- 156.Tirosh O., Orland G., Eliakim A., Nemet D., Steinberg N. Attenuation of Lower Body Acceleration in Overweight and Healthy-Weight Children During Running. J. Appl. Biomech. 2020;36:33–38. doi: 10.1123/jab.2019-0138. [DOI] [PubMed] [Google Scholar]
- 157.Van Werkhoven H., Farina K., Langley M.H. Using A Soft Conformable Foot Sensor to Measure Changes in Foot Strike Angle During Running. Sports. 2019;7:184. doi: 10.3390/sports7080184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Walsh G.S. Dynamics of Modular Neuromotor Control of Walking and Running during Single and Dual Task Conditions. Neurosci. 2021;465:1–10. doi: 10.1016/j.neuroscience.2021.04.004. [DOI] [PubMed] [Google Scholar]
- 159.Waite N., Goetschius J., Lauver J.D. Effect of Grade and Surface Type on Peak Tibial Acceleration in Trained Distance Runners. J. Appl. Biomech. 2021;37:2–5. doi: 10.1123/jab.2020-0096. [DOI] [PubMed] [Google Scholar]
- 160.Winter S.C., Lee J.B., Leadbetter R.I., Gordon S.J. Validation of a Single Inertial Sensor for Measuring Running Kinematics Overground during a Prolonged Run. J. Fit. Res. 2016;5:14–23. [Google Scholar]
- 161.Wixted A., Billing D.C., James D. Validation of trunk mounted inertial sensors for analysing running biomechanics under field conditions, using synchronously collected foot contact data. Sports Eng. 2010;12:207–212. doi: 10.1007/s12283-010-0043-2. [DOI] [Google Scholar]
- 162.Wood C.M., Kipp K. Use of audio biofeedback to reduce tibial impact accelerations during running. J. Biomech. 2014;47:1739–1741. doi: 10.1016/j.jbiomech.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 163.Wundersitz D., Gastin P.B., Richter C., Robertson S.J., Netto K. Validity of a trunk-mounted accelerometer to assess peak accelerations during walking, jogging and running. Eur. J. Sport Sci. 2015;15:382–390. doi: 10.1080/17461391.2014.955131. [DOI] [PubMed] [Google Scholar]
- 164.Zhang J.H., Chan Z.Y.-S., Au I.P.-H., An W.W., Shull P.B., Cheung R.T.-H. Transfer Learning Effects of Biofeedback Running Retraining in Untrained Conditions. Med. Sci. Sports Exerc. 2019;51:1904–1908. doi: 10.1249/MSS.0000000000002007. [DOI] [PubMed] [Google Scholar]
- 165.Zhang J.H., An W.W., Au I.P., Chen T.L., Cheung R.T. Comparison of the correlations between impact loading rates and peak accelerations measured at two different body sites: Intra- and inter-subject analysis. Gait Posture. 2016;46:53–56. doi: 10.1016/j.gaitpost.2016.02.002. [DOI] [PubMed] [Google Scholar]
- 166.Aubry R.L., Power G.A., Burr J.F. An Assessment of Running Power as a Training Metric for Elite and Recreational Runners. J. Strength Cond. Res. 2018;32:2258–2264. doi: 10.1519/JSC.0000000000002650. [DOI] [PubMed] [Google Scholar]
- 167.Austin C.L., Hokanson J.F., McGinnis P.M., Patrick S. The Relationship between Running Power and Running Economy in Well-Trained Distance Runners. Sports. 2018;6:142. doi: 10.3390/sports6040142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Barrett S., Midgley A., Lovell R. PlayerLoadTM: Reliability, Convergent Validity, and Influence of Unit Position during Treadmill Running. Int. J. Sports Physiol. Perform. 2014;9:945–952. doi: 10.1123/ijspp.2013-0418. [DOI] [PubMed] [Google Scholar]
- 169.De Brabandere A., De Beéck T.O., Schütte K.H., Meert W., Vanwanseele B., Davis J. Data fusion of body-worn accelerometers and heart rate to predict VO2max during submaximal running. PLoS ONE. 2018;13:e0199509. doi: 10.1371/journal.pone.0199509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Cher P.H., Worringham C.J., Stewart I.B. Human runners exhibit a least variable gait speed. J. Sports Sci. 2016;35:2211–2219. doi: 10.1080/02640414.2016.1262053. [DOI] [PubMed] [Google Scholar]
- 171.Clansey A.C., Lake M.J., Wallace E.S., Feehally T., Hanlon M. Can Trained Runners Effectively Attenuate Impact Acceleration During Repeated High-Intensity Running Bouts? J. Appl. Biomech. 2016;32:261–268. doi: 10.1123/jab.2015-0125. [DOI] [PubMed] [Google Scholar]
- 172.Clermont C.A., Benson L.C., Osis S.T., Kobsar D., Ferber R. Running patterns for male and female competitive and recreational runners based on accelerometer data. J. Sports Sci. 2019;37:204–211. doi: 10.1080/02640414.2018.1488518. [DOI] [PubMed] [Google Scholar]
- 173.Clermont C.A., Pohl A.J., Ferber R. Fatigue-Related Changes in Running Gait Patterns Persist in the Days Following a Marathon Race. J. Sport Rehabilit. 2020;29:934–941. doi: 10.1123/jsr.2019-0206. [DOI] [PubMed] [Google Scholar]
- 174.Dériaz O., Najafi B., Ballabeni P., Crettenand A., Gobelet C., Aminian K., Rizzoli R., Gremion G. Proximal tibia volumetric bone mineral density is correlated to the magnitude of local acceleration in male long-distance runners. J. Appl. Physiol. 2010;108:852–857. doi: 10.1152/japplphysiol.00865.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Enders H., von Tscharner V., Nigg B.M. The effects of preferred and non-preferred running strike patterns on tissue vibration properties. J. Sci. Med. Sport. 2014;17:218–222. doi: 10.1016/j.jsams.2013.03.015. [DOI] [PubMed] [Google Scholar]
- 176.Garcia-Byrne F., Wycherley T., Bishop C., Schwerdt S., Porter J., Buckley J. Accelerometer detected lateral sway during a submaximal running test correlates with endurance exercise performance in elite Australian male cricket players. J. Sci. Med. Sport. 2019;23:519–523. doi: 10.1016/j.jsams.2019.12.003. [DOI] [PubMed] [Google Scholar]
- 177.Giandolini M., Horvais N., Rossi J., Millet G., Samozino P., Morin J.-B. Foot strike pattern differently affects the axial and transverse components of shock acceleration and attenuation in downhill trail running. J. Biomech. 2016;49:1765–1771. doi: 10.1016/j.jbiomech.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 178.Giandolini M., Horvais N., Rossi J., Millet G., Morin J.-B., Samozino P. Effects of the foot strike pattern on muscle activity and neuromuscular fatigue in downhill trail running. Scand. J. Med. Sci. Sports. 2016;27:809–819. doi: 10.1111/sms.12692. [DOI] [PubMed] [Google Scholar]
- 179.Horvais N., Samozino P., Chiementin X., Morin J.-B., Giandolini M. Cushioning perception is associated with both tibia acceleration peak and vibration magnitude in heel-toe running. Footwear Sci. 2019;11:35–44. doi: 10.1080/19424280.2018.1555863. [DOI] [Google Scholar]
- 180.Hughes T., Jones R.K., Starbuck C., Sergeant J.C., Callaghan M. The value of tibial mounted inertial measurement units to quantify running kinetics in elite football (soccer) players. A reliability and agreement study using a research orientated and a clinically orientated system. J. Electromyogr. Kinesiol. 2019;44:156–164. doi: 10.1016/j.jelekin.2019.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Koska D., Gaudel J., Hein T., Maiwald C. Validation of an inertial measurement unit for the quantification of rearfoot kinematics during running. Gait Posture. 2018;64:135–140. doi: 10.1016/j.gaitpost.2018.06.007. [DOI] [PubMed] [Google Scholar]
- 182.Melo C.C., Carpes F.P., Vieira T.M., Mendes T.T., de Paula L.V., Chagas M.H., Peixoto G.H., de Andrade A.G.P. Correlation between running asymmetry, mechanical efficiency, and performance during a 10 km run. J. Biomech. 2020;109:109913. doi: 10.1016/j.jbiomech.2020.109913. [DOI] [PubMed] [Google Scholar]
- 183.Moltó I.N., Albiach J.P., Amer-Cuenca J.J., Segura-Ortí E., Gabriel W., Martínez-Gramage J. Wearable Sensors Detect Differences between the Sexes in Lower Limb Electromyographic Activity and Pelvis 3D Kinematics during Running. Sensors. 2020;20:6478. doi: 10.3390/s20226478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Morio C., Sevrez V., Chavet P., Berton E., Nicol C. Neuro-mechanical adjustments to shod versus barefoot treadmill runs in the acute and delayed stretch-shortening cycle recovery phases. J. Sports Sci. 2016;34:738–745. doi: 10.1080/02640414.2015.1069379. [DOI] [PubMed] [Google Scholar]
- 185.Murray A.M., Ryu J.H., Sproule J., Turner A.P., Graham-Smith P., Cardinale M. A Pilot Study Using Entropy as a Noninvasive Assessment of Running. Int. J. Sports Physiol. Perform. 2017;12:1119–1122. doi: 10.1123/ijspp.2016-0205. [DOI] [PubMed] [Google Scholar]
- 186.Navalta J.W., Montes J., Bodell N.G., Aguilar C.D., Radzak K., Manning J.W., DeBeliso M. Reliability of Trail Walking and Running Tasks Using the Stryd Power Meter. Int. J. Sports Med. 2019;40:498–502. doi: 10.1055/a-0875-4068. [DOI] [PubMed] [Google Scholar]
- 187.Olin E.D., Gutierrez G.M. EMG and tibial shock upon the first attempt at barefoot running. Hum. Mov. Sci. 2013;32:343–352. doi: 10.1016/j.humov.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 188.Perrotin N., Gardan N., Lesprillier A., Le Goff C., Seigneur J.-M., Abdi E., Sanudo B., Taiar R. Biomechanics of Trail Running Performance: Quantification of Spatio-Temporal Parameters by Using Low Cost Sensors in Ecological Conditions. Appl. Sci. 2021;11:2093. doi: 10.3390/app11052093. [DOI] [Google Scholar]
- 189.Provot T., Munera M., Bolaers F., Vitry G., Chiementin X. Intra and Inter Test Repeatability of Accelerometric Indicators Measured While Running. Procedia Eng. 2016;147:573–577. doi: 10.1016/j.proeng.2016.06.242. [DOI] [Google Scholar]
- 190.Reenalda J., Maartens E., Homan L., Buurke J. (Jaap) Continuous three dimensional analysis of running mechanics during a marathon by means of inertial magnetic measurement units to objectify changes in running mechanics. J. Biomech. 2016;49:3362–3367. doi: 10.1016/j.jbiomech.2016.08.032. [DOI] [PubMed] [Google Scholar]
- 191.Seeley M.K., Evans-Pickett A., Collins G.Q., Tracy J.B., Tuttle N.J., Rosquist P.G., Merrell A.J., Christensen W.F., Fullwood D.T., Bowden A.E. Predicting vertical ground reaction force during running using novel piezoresponsive sensors and accelerometry. J. Sports Sci. 2020;38:1844–1858. doi: 10.1080/02640414.2020.1757361. [DOI] [PubMed] [Google Scholar]
- 192.Shih Y., Ho C.-S., Shiang T.-Y. Measuring kinematic changes of the foot using a gyro sensor during intense running. J. Sports Sci. 2013;32:550–556. doi: 10.1080/02640414.2013.843013. [DOI] [PubMed] [Google Scholar]
- 193.Tirosh O., Orland G., Eliakim A., Nemet D., Steinberg N. Repeatability of tibial acceleration measurements made on children during walking and running. J. Sci. Med. Sport. 2019;22:91–95. doi: 10.1016/j.jsams.2018.04.006. [DOI] [PubMed] [Google Scholar]
- 194.Ueberschär O., Fleckenstein D., Wüstenfeld J.C., Warschun F., Falz R., Wolfarth B. Running on the hypogravity treadmill AlterG® does not reduce the magnitude of peak tibial impact accelerations. Sports Orthop. Traumatol. 2019;35:423–434. doi: 10.1016/j.orthtr.2019.10.001. [DOI] [Google Scholar]
- 195.Berghe P.V.D., Lorenzoni V., Derie R., Six J., Gerlo J., Leman M., De Clercq D. Music-based biofeedback to reduce tibial shock in over-ground running: A proof-of-concept study. Sci. Rep. 2021;11:4091. doi: 10.1038/s41598-021-83538-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.van der Bie J., Kröse B. Happy Running? Hybrid Learn. Educ. 2015;9425:357–360. doi: 10.1007/978-3-319-26005-1_26. [DOI] [Google Scholar]
- 197.Weich C., Jensen R.L., Vieten M. Triathlon transition study: Quantifying differences in running movement pattern and precision after bike-run transition. Sports Biomech. 2017;18:215–228. doi: 10.1080/14763141.2017.1391324. [DOI] [PubMed] [Google Scholar]
- 198.Bigelow E.M., Elvin N.G., Elvin A.A., Arnoczky S.P. Peak Impact Accelerations during Track and Treadmill Running. J. Appl. Biomech. 2013;29:639–644. doi: 10.1123/jab.29.5.639. [DOI] [PubMed] [Google Scholar]
- 199.Brahms C.M., Zhao Y., Gerhard D., Barden J.M. Long-range correlations and stride pattern variability in recreational and elite distance runners during a prolonged run. Gait Posture. 2020;92:487–492. doi: 10.1016/j.gaitpost.2020.08.107. [DOI] [PubMed] [Google Scholar]
- 200.Clermont C.A., Benson L.C., Edwards W.B., Hettinga B.A., Ferber R. New Considerations for Wearable Technology Data: Changes in Running Biomechanics During a Marathon. J. Appl. Biomech. 2019;35:401–409. doi: 10.1123/jab.2018-0453. [DOI] [PubMed] [Google Scholar]
- 201.DeJong M.A.F., Hertel J. Outdoor Running Activities Captured Using Wearable Sensors in Adult Competitive Runners. Int. J. Athl. Ther. Train. 2020;25:76–85. doi: 10.1123/ijatt.2019-0051. [DOI] [Google Scholar]
- 202.Giandolini M., Pavailler S., Samozino P., Morin J.-B., Horvais N. Foot strike pattern and impact continuous measurements during a trail running race: Proof of concept in a world-class athlete. Footwear Sci. 2015;7:127–137. doi: 10.1080/19424280.2015.1026944. [DOI] [Google Scholar]
- 203.Gómez-Carmona C.D., Bastida-Castillo A., González-Custodio A., Olcina G., Pino-Ortega J. Using an Inertial Device (WIMU PRO) to Quantify Neuromuscular Load in Running: Reliability, Convergent Validity, and Influence of Type of Surface and Device Location. J. Strength Cond. Res. 2020;34:365–373. doi: 10.1519/JSC.0000000000003106. [DOI] [PubMed] [Google Scholar]
- 204.Hoenig T., Hamacher D., Braumann K.-M., Zech A., Hollander K. Analysis of running stability during 5000 m running. Eur. J. Sport Sci. 2019;19:413–421. doi: 10.1080/17461391.2018.1519040. [DOI] [PubMed] [Google Scholar]
- 205.Provot T., Chiementin X., Bolaers F., Munera M. A time to exhaustion model during prolonged running based on wearable accelerometers. Sports Biomech. 2021;20:330–343. doi: 10.1080/14763141.2018.1549682. [DOI] [PubMed] [Google Scholar]
- 206.Rojas-Valverde D., Sánchez-Ureña B., Pino-Ortega J., Gómez-Carmona C., Gutierrez-Vargas R., Timón R., Olcina G. External Workload Indicators of Muscle and Kidney Mechanical Injury in Endurance Trail Running. Int. J. Environ. Res. Public Health. 2019;16:3909. doi: 10.3390/ijerph16203909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Rojas-Valverde D., Timón R., Sánchez-Ureña B., Pino-Ortega J., Martínez-Guardado I., Olcina G. Potential Use of Wearable Sensors to Assess Cumulative Kidney Trauma in Endurance Off-Road Running. J. Funct. Morphol. Kinesiol. 2020;5:93. doi: 10.3390/jfmk5040093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Schütte K.H., Seerden S., Venter R., Vanwanseele B. Influence of outdoor running fatigue and medial tibial stress syndrome on accelerometer-based loading and stability. Gait Posture. 2018;59:222–228. doi: 10.1016/j.gaitpost.2017.10.021. [DOI] [PubMed] [Google Scholar]
- 209.Ueberschär O., Fleckenstein D., Warschun F., Walter N., Hoppe M.W. Case report on lateral asymmetries in two junior elite long-distance runners during a high-altitude training camp. Sports Orthop. Traumatol. 2019;35:399–406. doi: 10.1016/j.orthtr.2019.06.002. [DOI] [Google Scholar]
- 210.Ahamed N.U., Kobsar D., Benson L.C., Clermont C.A., Osis S.T., Ferber R. Subject-specific and group-based running pattern classification using a single wearable sensor. J. Biomech. 2019;84:227–233. doi: 10.1016/j.jbiomech.2019.01.001. [DOI] [PubMed] [Google Scholar]
- 211.Ahamed N.U., Kobsar D., Benson L., Clermont C., Kohrs R., Osis S.T., Ferber R. Using wearable sensors to classify subject-specific running biomechanical gait patterns based on changes in environmental weather conditions. PLoS ONE. 2018;13:e0203839. doi: 10.1371/journal.pone.0203839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Ahamed N.U., Benson L.C., Clermont C.A., Pohl A.J., Ferber R. New Considerations for Collecting Biomechanical Data Using Wearable Sensors: How Does Inclination Influence the Number of Runs Needed to Determine a Stable Running Gait Pattern? Sensors. 2019;19:2516. doi: 10.3390/s19112516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Benson L.C., Ahamed N.U., Kobsar D., Ferber R. New considerations for collecting biomechanical data using wearable sensors: Number of level runs to define a stable running pattern with a single IMU. J. Biomech. 2019;85:187–192. doi: 10.1016/j.jbiomech.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 214.Cartón-Llorente A., García-Pinillos F., Royo-Borruel J., Rubio-Peirotén A., Jaén-Carrillo D., Roche-Seruendo L.E. Estimating Functional Threshold Power in Endurance Running from Shorter Time Trials Using a 6-Axis Inertial Measurement Sensor. Sensors. 2021;21:582. doi: 10.3390/s21020582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Cerezuela-Espejo V., Hernández-Belmonte A., Courel-Ibáñez J., Conesa-Ros E., Martínez-Cava A., Pallarés J.G. Running power meters and theoretical models based on laws of physics: Effects of environments and running conditions. Physiol. Behav. 2020;223:112972. doi: 10.1016/j.physbeh.2020.112972. [DOI] [PubMed] [Google Scholar]
- 216.Colapietro M., Fraser J.J., Resch J.E., Hertel J. Running mechanics during 1600 meter track runs in young adults with and without chronic ankle instability. Phys. Ther. Sport. 2019;42:16–25. doi: 10.1016/j.ptsp.2019.11.010. [DOI] [PubMed] [Google Scholar]
- 217.Gregory C.J., Koldenhoven R.M., Higgins M., Hertel J. External ankle supports alter running biomechanics: A field-based study using wearable sensors. Physiol. Meas. 2019;40:044003. doi: 10.1088/1361-6579/ab15ad. [DOI] [PubMed] [Google Scholar]
- 218.Hollander K., Hamacher D., Zech A. Running barefoot leads to lower running stability compared to shod running - results from a randomized controlled study. Sci. Rep. 2021;11:4376. doi: 10.1038/s41598-021-83056-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Hollis C.R., Koldenhoven R.M., Resch J.E., Hertel J. Running biomechanics as measured by wearable sensors: Effects of speed and surface. Sports Biomech. 2021;20:521–531. doi: 10.1080/14763141.2019.1579366. [DOI] [PubMed] [Google Scholar]
- 220.Kiernan D., Hawkins D.A., Manoukian M.A., McKallip M., Oelsner L., Caskey C.F., Coolbaugh C.L. Accelerometer-based prediction of running injury in National Collegiate Athletic Association track athletes. J. Biomech. 2018;73:201–209. doi: 10.1016/j.jbiomech.2018.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Koldenhoven R.M., Virostek M.A., DeJong M.A.F., Higgins M., Hertel J. Increased Contact Time and Strength Deficits in Runners With Exercise-Related Lower Leg Pain. J. Athl. Train. 2020;55:1247–1254. doi: 10.4085/1062-6050-0514.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.McGregor S.J., Busa M.A., Yaggie J.A., Bollt E.M. High Resolution MEMS Accelerometers to Estimate VO2 and Compare Running Mechanics between Highly Trained Inter-Collegiate and Untrained Runners. PLoS ONE. 2009;4:e7355. doi: 10.1371/journal.pone.0007355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Nüesch C., Roos E., Egloff C., Pagenstert G., Mündermann A. The effect of different running shoes on treadmill running mechanics and muscle activity assessed using statistical parametric mapping (SPM) Gait Posture. 2019;69:1–7. doi: 10.1016/j.gaitpost.2019.01.013. [DOI] [PubMed] [Google Scholar]
- 224.Olcina G., Perez-Sousa M. Ángel; Escobar-Alvarez, J.A.; Timón, R. Effects of Cycling on Subsequent Running Performance, Stride Length, and Muscle Oxygen Saturation in Triathletes. Sports. 2019;7:115. doi: 10.3390/sports7050115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Rochat N., Seifert L., Guignard B., Hauw D. An enactive approach to appropriation in the instrumented activity of trail running. Cogn. Process. 2019;20:459–477. doi: 10.1007/s10339-019-00921-2. [DOI] [PubMed] [Google Scholar]
- 226.Ruder M., Jamison S.T., Tenforde A., Mulloy F., Davis I.S. Relationship of Foot Strike Pattern and Landing Impacts during a Marathon. Med. Sci. Sports Exerc. 2019;51:2073–2079. doi: 10.1249/MSS.0000000000002032. [DOI] [PubMed] [Google Scholar]
- 227.Ryan M.R., Napier C., Greenwood D., Paquette M.R. Comparison of different measures to monitor week-to-week changes in training load in high school runners. Int. J. Sports Sci. Coach. 2021;16:370–379. doi: 10.1177/1747954120970305. [DOI] [Google Scholar]
- 228.Strohrmann C., Harms H., Kappeler-Setz C., Troster G. Monitoring Kinematic Changes with Fatigue in Running Using Body-Worn Sensors. IEEE Trans. Inf. Technol. Biomed. 2012;16:983–990. doi: 10.1109/TITB.2012.2201950. [DOI] [PubMed] [Google Scholar]
- 229.Berghe P.V.D., Gosseries M., Gerlo J., Lenoir M., Leman M., De Clercq D. Change-Point Detection of Peak Tibial Acceleration in Overground Running Retraining. Sensors. 2020;20:1720. doi: 10.3390/s20061720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Vanwanseele B., De Beéck T.O., Schütte K., Davis J. Accelerometer Based Data Can Provide a Better Estimate of Cumulative Load During Running Compared to GPS Based Parameters. Front. Sports Act. Living. 2020;2:575596. doi: 10.3389/fspor.2020.575596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Willis S.J., Gellaerts J., Mariani B., Basset P., Borrani F., Millet G.P. Level Versus Uphill Economy and Mechanical Responses in Elite Ultratrail Runners. Int. J. Sports Physiol. Perform. 2019;14:1001–1005. doi: 10.1123/ijspp.2018-0365. [DOI] [PubMed] [Google Scholar]
- 232.Bielik V. Gender differences of running kinematics and economy in trained distance runners. Gazz. Med. Ital. Arch. Sci. Med. 2019;178:403–410. doi: 10.23736/S0393-3660.18.03863-9. [DOI] [Google Scholar]
- 233.Bielik V., Clementis M. Running mechanics in recreational runners, soccer and tennis players. Gazzetta Medica Ital. Arch. Sci. Mediche. 2017;176:461–466. doi: 10.23736/S0393-3660.16.03409-4. [DOI] [Google Scholar]
- 234.Butler R.J., Hamill J., Davis I. Effect of footwear on high and low arched runners’ mechanics during a prolonged run. Gait Posture. 2007;26:219–225. doi: 10.1016/j.gaitpost.2006.09.015. [DOI] [PubMed] [Google Scholar]
- 235.Cooper G., Sheret I., McMillan L., Siliverdis K., Sha N., Hodgins D., Kenney L., Howard D. Inertial sensor-based knee flexion/extension angle estimation. J. Biomech. 2009;42:2678–2685. doi: 10.1016/j.jbiomech.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 236.de Fontenay B.P., Roy J.S., Dubois B., Bouyer L., Esculier J.F. Validating Commercial Wearable Sensors for Running Gait Parameters Estimation. IEEE Sens. J. 2020;20:7783–7791. doi: 10.1109/JSEN.2020.2982568. [DOI] [Google Scholar]
- 237.Dufek J.S., Mercer J.A., Teramoto K., Mangus B.C., Freedman J.A. Impact attenuation and variability during running in females: A lifespan investigation. J. Sport Rehabilit. 2008;17:230–242. doi: 10.1123/jsr.17.3.230. [DOI] [PubMed] [Google Scholar]
- 238.Garrett J., Graham S.R., Eston R.G., Burgess D.J., Garrett L.J., Jakeman J., Norton K. A Novel Method of Assessment for Monitoring Neuromuscular Fatigue in Australian Rules Football Players. Int. J. Sports Physiol. Perform. 2019;14:598–605. doi: 10.1123/ijspp.2018-0253. [DOI] [PubMed] [Google Scholar]
- 239.Gurchiek R.D., McGinnis R., Needle A.R., McBride J.M., van Werkhoven H. The use of a single inertial sensor to estimate 3-dimensional ground reaction force during accelerative running tasks. J. Biomech. 2017;61:263–268. doi: 10.1016/j.jbiomech.2017.07.035. [DOI] [PubMed] [Google Scholar]
- 240.Sheerin K.R., Reid D., Taylor D., Besier T.F. The effectiveness of real-time haptic feedback gait retraining for reducing resultant tibial acceleration with runners. Phys. Ther. Sport. 2020;43:173–180. doi: 10.1016/j.ptsp.2020.03.001. [DOI] [PubMed] [Google Scholar]
- 241.Ueberschär O., Fleckenstein D., Warschun F., Kränzler S., Walter N., Hoppe M.W. Measuring biomechanical loads and asymmetries in junior elite long-distance runners through triaxial inertial sensors. Sports Orthop. Traumatol. 2019;35:296–308. doi: 10.1016/j.orthtr.2019.06.001. [DOI] [Google Scholar]
- 242.Zadeh A., Taylor D., Bertsos M., Tillman T., Nosoudi N., Bruce S. Predicting Sports Injuries with Wearable Technology and Data Analysis. Inf. Syst. Front. 2021;23:1023–1037. doi: 10.1007/s10796-020-10018-3. [DOI] [Google Scholar]
- 243.Taunton J.E., Ryan M.B., Clement D.B., McKenzie D.C., Lloyd-Smith D.R., Zumbo B.D. A prospective study of running injuries: The Vancouver Sun Run “In Training” clinics. Br. J. Sports Med. 2003;37:239–244. doi: 10.1136/bjsm.37.3.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Bertelsen M.L., Hulme A., Petersen J., Brund R.K., Sørensen H., Finch C.F., Parner E., Nielsen R.O. A framework for the etiology of running-related injuries. Scand. J. Med. Sci. Sports. 2017;27:1170–1180. doi: 10.1111/sms.12883. [DOI] [PubMed] [Google Scholar]
- 245.Van Hooren B., Fuller J.T., Buckley J.D., Miller J.R., Sewell K., Rao G., Barton C., Bishop C., Willy R.W. Is Motorized Treadmill Running Biomechanically Comparable to Overground Running? A Systematic Review and Meta-Analysis of Cross-Over Studies. Sports Med. 2020;50:785–813. doi: 10.1007/s40279-019-01237-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Moe-Nilssen R., Helbostad J.L. Estimation of gait cycle characteristics by trunk accelerometry. J. Biomech. 2004;37:121–126. doi: 10.1016/S0021-9290(03)00233-1. [DOI] [PubMed] [Google Scholar]
- 247.Janssen M., Scheerder J., Thibaut E., Brombacher A., Vos S. Who uses running apps and sports watches? Determinants and consumer profiles of event runners’ usage of running-related smartphone applications and sports watches. PLoS ONE. 2017;12:e0181167. doi: 10.1371/journal.pone.0181167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Pobiruchin M., Suleder J., Zowalla R., Wiesner M., Wilson G., Mauriello M.L., Cena F. Accuracy and Adoption of Wearable Technology Used by Active Citizens: A Marathon Event Field Study. JMIR mHealth uHealth. 2017;5:e24. doi: 10.2196/mhealth.6395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Clermont C.A., Duffett-Leger L., Hettinga B.A., Ferber R. Runners’ Perspectives on ‘Smart’ Wearable Technology and Its Use for Preventing Injury. Int. J. Hum.-Comput. Interact. 2019;36:31–40. doi: 10.1080/10447318.2019.1597575. [DOI] [Google Scholar]
- 250.Aderem J., Louw Q.A. Biomechanical risk factors associated with iliotibial band syndrome in runners: A systematic review. BMC Musculoskelet. Disord. 2015;16:356. doi: 10.1186/s12891-015-0808-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Andersen J.J. The State of Running 2019. [(accessed on 26 May 2021)]. Available online: https://runrepeat.com/state-of-running?fbclid=IwAR3x_Z4MeyKxCaLBwOTBL8uSqcAnz64s5H_Lh8aGHbsm72GxRz_G4Su1zcU.
- 252.Costello J., Bieuzen F., Bleakley C. Where are all the female participants in Sports and Exercise Medicine research? Eur. J. Sport Sci. 2014;14:847–851. doi: 10.1080/17461391.2014.911354. [DOI] [PubMed] [Google Scholar]
- 253.Horsley B.J., Tofari P.J., Halson S.L., Kemp J.G., Dickson J., Maniar N., Cormack S.J. Does Site Matter? Impact of Inertial Measurement Unit Placement on the Validity and Reliability of Stride Variables During Running: A Systematic Review and Meta-analysis. Sports Med. 2021;51:1449–1489. doi: 10.1007/s40279-021-01443-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are available within this manuscript.