Abstract
Background:
Defining the optimal conduction of percutaneous-coronary-intervention (PCI) to treat bifurcation lesions has been the subject of many clinical studies showing that the applied stenting technique may influence clinical outcome. Accordingly, bifurcation stenting classifications and technical sequences should be standardized to allow proper reporting and comparison.
Methods:
The European Bifurcation Club (EBC) is a multidisciplinary group dedicated to optimize the treatment of bifurcations and previously created a classification of bifurcation stenting techniques that is based on the first stent implantation site. Since some techniques have been abandoned, others have been refined and dedicated devices became available, EBC promoted an international task force aimed at updating the classification of bifurcation stenting techniques as well as at highlighting the best practices for most popular techniques. Original descriptive images obtained by drawings, bench tests and micro-computed-tomographic reconstructions have been created in order to serve as tutorials in both procedure reporting and clinical practice.
Results:
An updated Main-Across-Distal-Side (MADS)-2, classification of bifurcation stenting techniques has been realized and is reported in the present article allowing standardized procedure reporting in both clinical practice and scientific studies. The EBC-promoted task force deeply discussed, agreed on and described (using original drawings and bench tests) the optimal steps for the following major bifurcation stenting techniques: (a) 1-stent techniques (“provisional” and “inverted provisional”) and (b) 2-stent techniques (“T/TAP,”“culotte,” and “DK-crush”).
Conclusions:
The present EBC-promoted paper is intended to facilitate technique selection, reporting and performance for PCI on bifurcated lesions during daily clinical practice.
Keywords: bifurcation lesions, DES, PCI, personalized medicine, stenting technique
1 |. INTRODUCTION
Initiated in 2004, the European Bifurcation Club (EBC) has focused on improving bifurcation PCI practice by organizing annual meetings and promoting general consensus statements1–9 and consensus documents dedicated to specific bifurcation-related topics.10–17 One of the most important concept arose from EBC events was the recognition that the final confirmation of stent struts into a bifurcated coronary lesion is strongly influenced by different factors including stent characteristics,18 technique selection and procedural steps. Accordingly, technical standardization represents a major clinical need. This recognition resulted in an EBC-promoted task force of international experts who collaborated on this document.
2 |. BIFURCATION STENTING TECHNIQUES CLASSIFICATION: MADS-2
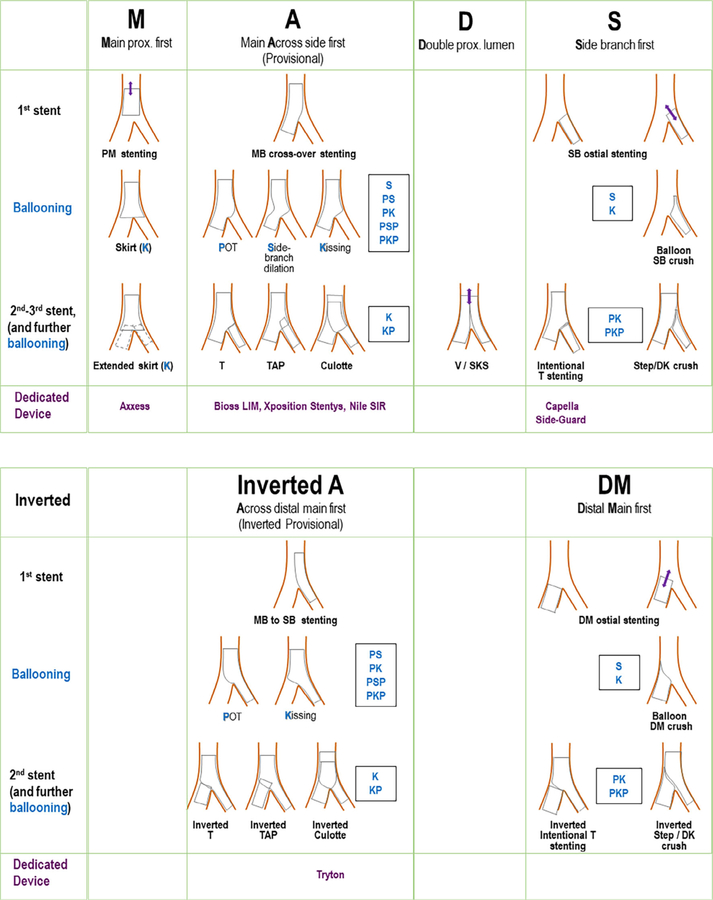
The list of proposed, applied or simply theorized techniques to implant tubular stents in bifurcated coronary lesions is continuously expanding. In 2008, the EBC organized a dedicated international task force led by Yves Louvard (with Ran Kornowski’s significant contribution) that conceived a classification based on the position of the first stent and was called “MADS” (main vessel or across side branch or double lumen in proximal main vessel or side branch).10 The efficacy of this classification for reporting technique during procedures has recently been confirmed by the large (more than 15,000 patients) GLOBAL LEADERS trial.19 During the past decade some techniques have been abandoned or proven not effective, others have been refined. Thus, the original classification has been updated to generate the MADS-2 technique classification reported in Figure 1. Among the novelties, three types of balloon dilation techniques have been inserted in the MADS-2 using the following single letter ballooning technique code:
P: post-dilation of the proximal main vessel (usually reported as proximal optimization technique, POT);
S: balloon dilation of the SB ostium;
K: balloon inflation in the MV and SB (usually reported as kissing balloon inflation technique).
FIGURE 1.
MADS-2 classification of bifurcation stenting techniques. The figure comprises two panels. Upper panel shows the standard techniques while the lower panel shows the “inverted” techniques. Blue capital letters describe ballooning techniques (see text for explanation). Common combinations of ballooning techniques are described as the sequential blue capital letters
Combinations of the ballooning techniques can be easily highlighted by appropriately ordered ballooning letter sequences. As an example, “PKP” stands for POT, followed by kissing, followed by new POT. Another possible ballooning technique is the post-dilation of distal MV, also called “distal balloon optimization” (DOT) and can be reported as D.
Finally, MADS-2 classification is flexible enough to host bifurcation-dedicated devices. This may facilitate the understanding of the technical sequence that is “facilitated” by each specific future or contemporary device. As an example, the Tryton stent (a bare metal bifurcation device which was tested in a large prospective randomized trial20) is depicted in MADS-2 as a device aimed at facilitating an “inverted culotte” (Figure 1).
3 |. FROM TECHNIQUES CLASSIFICATION COMPREHESIVENESS TO IDEAL TECHNICAL SEQUENCES FOR MAJOR TECHNIQUES
A 1-stent technique, also called “the provisional approach (the implantation of one drug-eluting stent in the MV with additional balloon dilation/stent implantation within the SB only in the case of need) is recognized as the gold standard approach for the majority of bifurcation lesions.9,21 Yet, the use of 2-stent implantation techniques is advised to treat in selected patients with complex bifurcated lesions with relevant and significantly diseased SB.9,21
The EBC considers that:
When using a 1-stent technique, some specific procedural steps may reduce SB complications and need for second stent implantation;
When using a 2-stent technique, the performance of final kissing balloon inflation may reduce target lesion complications and is probably more important than the specific technique adopted to implant the stents.
Some technical sequences may increase efficacy of stenting techniques. These steps are reported in the present article for the major 1-stent and 2-stent techniques. To facilitate interpretation, dedicated bench tests have been performed collecting both fluoroscopy images and micro-CT. Bench tests have been performed according to EBC recommendations14 in a catheterization laboratory equipped by Allura X-ray imaging technology (Philips Healthcare, Best, The Netherlands). Silicone phantoms were constructed with angles between the MV and SB of 60 and sizes mimicking a possible left main bifurcation (proximal MV diameter of 5 mm, distal MV diameter of 3.5 mm, and the SB diameter of 3.0). The stents implanted were Resolute Onyx (Medtronic, Santa Rosa, CA). The balloons used were Euphora (Medtronic, Santa Rosa, California) semi-compliant or non-compliant in the different needed sizes and Trek 5 × 12 mm (Abbott, Abbott Vascular, Redwood City, CA) for proximal MV. Following deployment, the stents were imaged using micro-computed tomography (CT). The micro-CT images obtained were electronically colored (black and blue color code for the two stents in double stenting techniques to facilitate interpretation).
4 |. ONE-STENT TECHNIQUES (“PROVISIONAL” AND “INVERTED PROVISIONAL”) STEP-BY-STEP
One-stent techniques may be applied to many bifurcation anatomies (Table 1) and represent the gold standard for the vast majority of non-complex bifurcated lesions. Of note, 1-stent technique may be practiced according to “provisional” (more commonly adopted) and “inverted provisional” (selected cases).
TABLE 1.
Major bifurcation stenting techniques and anatomic conditions that may favor their adoption
| Favorable settings | Specific issues | |
|---|---|---|
| One-stent techniques | ||
| Provisional | Any non-complex bifurcation lesion Complex bifurcation lesions provided that risk of SB occlusion or difficulty in its bail-out management have been ruled out |
SB occlusion risk |
| Inverted provisional | Medina 0,0,1 lesion of a bifurcation with very large SB like ostial left circumflex lesion or ostial diagonal lesion | Distal MV occlusion risk Distal MV patency is dependent on the stent’s side-cell Distal MV integrity (absence of dissections) should be carefully ascertained |
| Two-stent techniques | ||
| T/TAP stenting | Bail-out management of any SB in the course of provisional Complex bifurcations without very acute angle Complex bifurcations with large and diseased SB (in that case, inverted technique advised) |
Meticulous attention to SB stent implantation is critical to avoid long protrusion or SB ostium uncoverage |
| Culotte stenting | Bail-out management of large-sized SB in the course of provisional Complex bifurcations with SB size comparable with distal MV size |
Multiple steps required Double stent layers in the proximal MV |
| DK-crush | Complex bifurcations, with extensive side-branch disease and/or anticipated difficulty in re-accessing an important SB | Multiple steps required So far, efficacy proven only when practiced by operators with high experience with the technique Triple stent layers in the lateral wall of proximal MV |
Abbreviations: MV, main vessel; SB, side branch.
The recommended steps for “provisional” (Figure 2) are:
Stent implantation across the side-branch (also called “crossover stenting”) following these rules: DES diameter selected 1:1 according to the distal MV size, DES length selected (even in the absence of relevant disease) allowing for proximal MV coverage of a segment equal or longer than the shortest available balloon (usually 8 mm).
Systematic post-dilation of the stent at the level of proximal MV up to the carina level with a balloon diameter sized 1:1 according to the proximal MV (POT technique). Although both semi-compliant and non-compliant balloons can be selected, non-compliant balloon is favored in the presence of st under-expansion and ascertained proximal MV reference size. Semi-compliant balloons have been found to be able to appropriately displace the stent struts obtaining vessel wall apposition in the absence of disease. Of note, meticulous attention should be paid to POT balloon position since when its distal shoulder is positioned accurately at the carina better results are expected.22
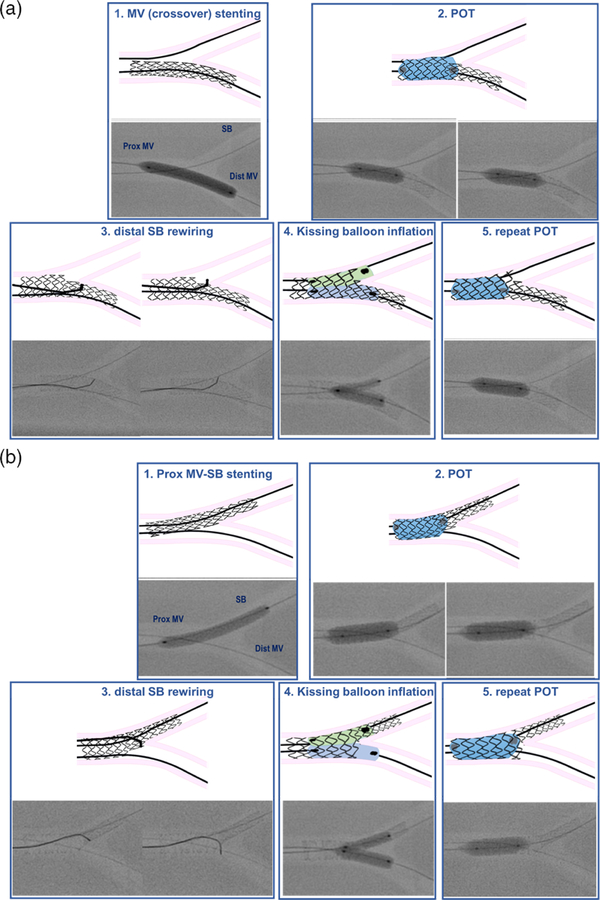
FIGURE 2.
Recommended steps for provisional and inverted provisional technique. (a) provisional technique. (1) MV stenting across SB take-off with DES sized 1:1 according to distal MV diameter. (2) POT with balloon sized 1:1 to proximal MV. Note that, due to long stented area in the proximal MV, two inflations were needed to appropriately post-dilate the entire proximal MV stent segment. (3) Distal SB rewiring according to the pullback technique. Note the double bended guidewire tip shape that allows entering easily the distal part of SB ostium. (4) Simultaneous kissing balloon inflation with MV balloon sized 1:1 according to distal MV and SB balloon sized 1:1 according to SB diameter. (5) Repeat POT with balloon sized 1:1 to proximal MV. (b) Inverted provisional technique. (1) Stent implantation from proximal MV into the SB across distal MV with DES sized 1:1 according to SB. (2) POT with balloon sized 1:1 to proximal MV. Note that, due to long stented area in the proximal MV, two inflations were needed to appropriately post-dilate the whole proximal MV. (3) Distal MV rewiring according to the pullback technique. Note the double bended guidewire tip shape that allows entering easily the distal MV ostium. (4) Simultaneous kissing balloon inflation with MV balloon sized 1:1 according to distal MV and SB balloon sized 1:1 according to SB diameter. (5) Repeat POT with balloon sized 1:1 to proximal MV
These initial two steps are regarded as mandatory, whereas the possible adoption of further steps is a matter of discussion. When an important SB is jeopardized after MV stenting, further intervention has to be performed and the kissing balloon technique is the usual initial approach. Recently, the alternative to perform SB dilation and then repeated POT has been described23 but confirmatory clinical validation is awaited.9
When SB intervention is required during a provisional approach to a bifurcation, the following steps are advised (Figure 2):
Perform SB rewiring with the aim of crossing the “distal” stent struts9 close to bifurcation carina (maneuver usually called “distal re-wiring”). A pullback rewiring technique with appropriately bended guidewire tip shape24 may facilitate this “distal re-wiring.”
Perform kissing balloon inflation using short balloons and MV balloon sized 1:1 according to the distal MV diameter. According to bench test data, minimal balloon overlap in the proximal MV,25 with sequential balloon inflation (alternate inflation of MV and SB balloon followed by simultaneous inflation/deflation) using non-compliant balloons26 seems the best option.
Perform post-dilation of the stent at the level of proximal MV up to the carina level with a balloon diameter sized 1:1 according to the proximal MV (repeat POT or re-POT).
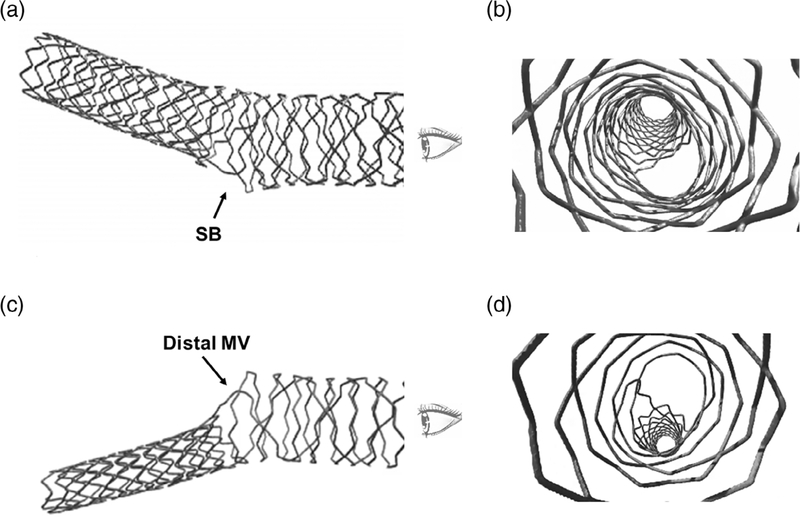
In selected anatomic conditions, the provisional 1-stent technique may be practiced according to the “inverted provisional” approach (Table 1). This specific sequence is summarized in Figure 2b. Notably, the selection of inverted provisional approach might require implantation of a smaller stent platform size as compared with the standard provisional technique. For instance, such selection of a smaller stent with different structure may result in a different proximal MV metallic coverage in the same bifurcation (Figure 3).
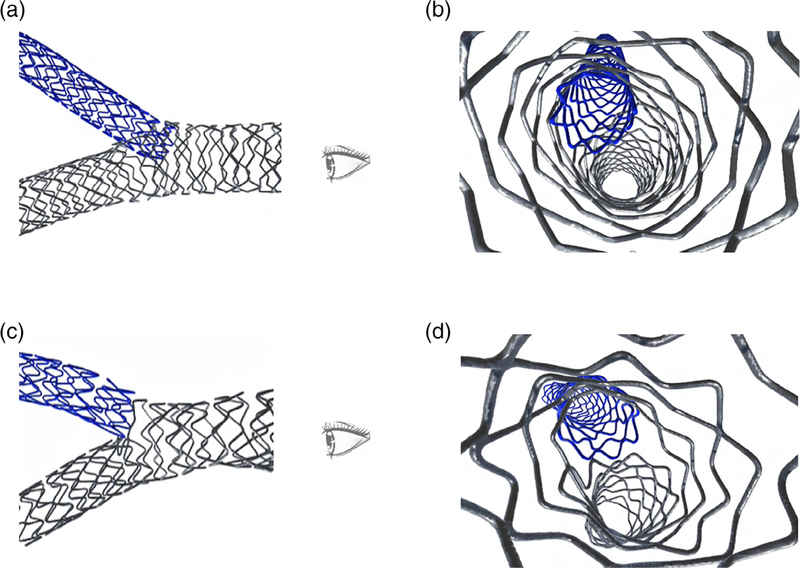
FIGURE 3.
Micro-CT image of stent deformation obtained by provisional and inverted provisional in the same bifurcation model. (a,b) Result after provisional using a 3.5 mm DES (this micro-CT has been obtained in the bench test reported in Figure 2). (c,d) Result after inverted provisional using a 3.0 DES (this micro-CT has been obtained in the bench test reported in this Figure 2)
5 |. T/TAP STENTING STEP-BY-STEP
The potential to implant a second stent during a provisional (or inverted provisional) approach to a bifurcation lesion is one of the major assets of this approach. T and TAP stenting represent the easiest way to implant the second stent.
Initially, all the steps of the provisional technique including distal rewiring and kissing should be performed. Then if the bifurcation angle is very close to 90°, placement of the second stent in a T configuration is possible and this allows stent strut coverage of the bifurcation without the need of floating or overlapping stent struts.27 Obviously, achieving the optimal angiographic view (eventually facilitated by stent enhancement tools) is critical for successful T stenting. However, extensive clinical experience, supported by bench test data, has documented the important pitfalls in T stenting. Commonly, the angle is not 90° and this might result in incomplete SB ostium scaffolding or stent protrusion inside the proximal MV. A suboptimal SB ostium coverage may lead to restenosis while protruding struts may jeopardize access to distal MV.
Recognition of these limitations of T stenting resulted in the develpment of the TAP technique.28 The TAP technique creates a metallic neocarina in the center of bifurcation but aims to ensure the systematic and complete stent coverage of the SB ostium. During the performance of TAP, operators should systematically aim to create the shortest neocarina that is possible, while still achieving full coverage of the side-branch ostium.
To electively perform effective T/TAP, all the initial steps for provisional up to kissing inflation are needed (since they allow for good SB ostium opening and bifurcation area scaffolding). Then, after having found the best view to assess the SB ostium, the recommended steps are:
Advancement of a DES of the appropriate length and size into the SB.
Placement of a balloon into the MV (sized 1:1 according to the distal MV diameter—this will be used for final kissing balloon).
After having carefully selected the best position of the SB stent to fully cover the proximal (or “upper”) part of the SB ostium (and minimizing protrusion inside the MV), the stent is inflated while the MV balloon is kept un-inflated into the MV.
After SB stent deployment, the balloon of the stent is slightly pulled back and repeated inflation at high pressure is performed in order to warrant optimal stent expansion at the level of SB ostium (the balloon inside the MV is still kept uninflated during this phase).
After alignment of the MV balloon and SB stenťs delivery balloon, kissing balloon inflation is performed by inflating simultaneously these two balloons. Some bench tests suggest “sequential” high pressure inflation with non-compliant balloons can be considered as an option but simultaneous inflation should follow and the kissing balloon deflation should be simultaneous (to keep the neocarina in a central position).
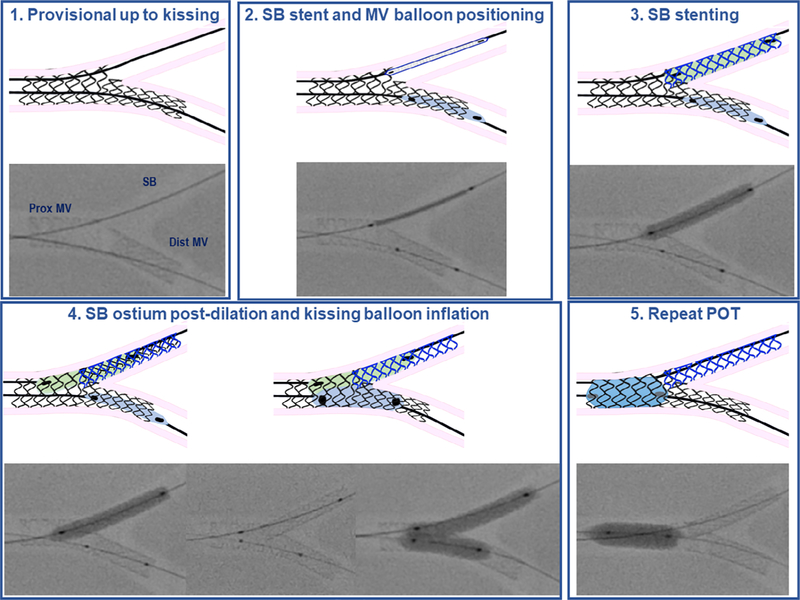
A repeat final POT is considered when a long segment of stent in the MV is present and long overlaps between the balloons during kissing have occurred (this can result in an oval MV result). Of note, with TAP, meticulous attention must be paid during POT balloon placement to do nor reach neocarina. Indeed, the metallic neocarina can be easily displaced causing its removal from central position achieved with kissing balloon inflation.29
Figure 4 illustrates the recommended steps for TAP. The T and TAP can be considered as a continuum and Figure 5 shows (by micro-CT) the different final appearance of neocarina achieved in two different tests by following the same recommended sequence with the same DES. Despite a different neocarina length, optimal ostium scaffolding and stent expansion has been achieved in both cases. Consequently, if during an intended T stent the operator feels doubtful about the efficacy of distal recrossing and/or the perfection of SB stent positioning, switching to a TAP is recommended as this will facilitate procedure completion (i.e., kissing balloon inflation after SB stenting).
FIGURE 4.
Recommended steps for T/TAP stenting technique. (1) The recommended steps of provisional have been followed up to kissing balloon inflation. (2) SB stent and MV balloon positioning: an appropriately sized SB stent is placed in the SB and a balloon sized 1:1 according to the distal MV is advanced in the distal MV. (3) SB stenting: when the best position (to allow cover the SB ostium and minimally protruding inside the MV) for SB stent has been selected, the SB stent is delivered with the MV balloon left uninflated. (4) SB ostium post-dilation and kissing balloon inflation: after SB stent deployment, the balloon of the stent is slightly pulled back and repeated inflation at high pressure is performed in order to warrant optimal stent expansion at the level of SB ostium (the balloon inside the MV is still kept uninflated during this phase). Then, after alignment of the MV balloon and SB stenťs balloon, kissing balloon inflation is performed by inflating simultaneously the two balloons. (5) Repeat POT. This step is not mandatory. If this step is adopted, the POT balloon is inflated in the proximal MV in a position that is far from the metallic neocarina
FIGURE 5.
Micro-CT image of T/TAP stenting with different neocarina length. (a,b) T/TAP stenting sequence applied successfully and resulting in full bifurcation coverage and appreciable neocarina (this micro-CT has been obtained in the bench test reported in this figure). (c,d) T/TAP stenting sequence applied successfully and resulting in full bifurcation coverage and virtual absence of neocarina (true T configuration)
6 |. CULOTTE STENTING STEP-BY-STEP
The culotte technique was first reported by Chevalier et al30 as a technique to complement the provisional approach when a second stent was required (Table 1). This is also called “classic” culotte. Yet, in the clinical practice, culotte is often performed by implanting the first stent in the SB and this sequence is usually called “inverted” culotte.
The recommended steps for inverted culotte are:
After appropriate predilation of both branches, first stent is implanted in the SB protruding inside the proximal MV. The stent is sized according to the diameter of the distal SB and long enough to allow POT in the proximal MV.
Post-dilation of the stent at the level of proximal MV up to the carina level is performed with a balloon sized 1:1 according to the proximal MV (POT technique).
Rewiring of the MV close to the carina is performed using the pullback technique from SB.
Distal MV balloon dilation (or kissing balloon inflation) is performed to open the struts into distal MV direction.
Second stent implantation in the distal MV covering up to proximal MV is performed. DES diameter is selected 1:1 according to the distal MV size, DES length selected to ensure proximal MV lesion coverage.
Systematic post-dilation of the stent at the level of proximal MV up to the carina level with a balloon diameter sized 1:1 according to the proximal MV (repeat POT) is recommended.
Distal rewiring of the SB according to the pullback technique is performed.
Kissing balloon inflation (using short non-compliant balloons) is systematically needed. Usually, after having placed the two ballons in the proper position, sequential inflation at high pressure followed by simultaneous kissing balloon inflation is suggested.
Post-dilation of the stent at the level of proximal MV up to the carina level with a balloon diameter sized 1:1 according to the proximal MV (final POT) is performed.
The EBC strongly recommends systematic POT immediately after each stent deployment in order to avoid the presence of malapposed struts in the proximal MV that may cause abluminal rewiring. Figure 6a reports the graphic demonstration of a possible sequence of technical steps to perform culotte when double stenting is planned according to “inverted culotte”. Figure 6b,c shows (by micro-CT) the final appearance of culotte stenting.
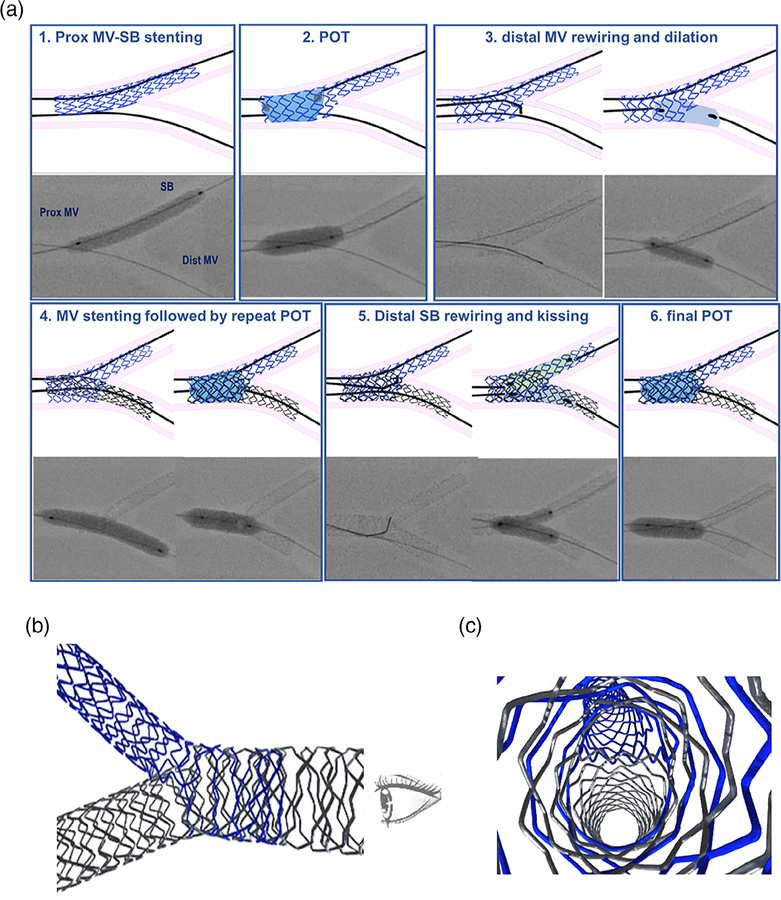
FIGURE 6.
Culotte stenting. (a) Recommended steps for culotte stenting (in the case of elective double stenting). (1) Stent implantation from proximal MV into the SB across distal MV with DES sized 1:1 according to SB. When culotte is used for elective double stenting, usually a short proximal MV coverage may be selected in order to limit the area with overlapping stents. (2) POT with balloon sized 1:1 to proximal MV. (3) Distal MV rewiring and dilation. Distal MV rewiring is performed according to the pullback technique. Distal MV dilation may be performed either using kissing balloon inflation (see inverted provisional) or by simple balloon dilation with balloon selected 1:1 according to distal MV size. (4) MV stenting followed by repeat POT: after SB guidewire removal, stent implantation across the side-branch with DES diameter selected 1:1 according to the distal MV size is performed. Thereafter, repeat POT with balloon sized 1:1 to proximal MV is done. (5) Distal SB rewiring and kissing: distal SB rewiring is performed according to the pullback technique. Simultaneous kissing balloon inflation (usually with non-compliant balloons at high pressure) is performed selecting MV balloon sized 1:1 according to distal MV and SB balloon sized 1:1 according to SB diameter. 5. Final POT: performed with balloon sized 1:1 to proximal MV. (b,c) Micro-CT image of stent conformation obtained by culotte
The main limitation of the culotte technique is the fact that both stents (needed to cover the two bifurcation branches: distal MV and SB) also have to cover the proximal MV. Consequently, care is required to select DES that can be expanded enough to reach the MV diameter. Accordingly, culotte may not be the optimal technique for bifurcation lesions with very different branch sizes (Table 1).
7 |. DK-CRUSH STENTING STEP-BY-STEP
The firstly crush technique was reported by Colombo in 2003.31 Subsequently, clinical experience recognized a lack of predictability in wire/balloon recrossing after deployment of the second stent and performance of final kissing was identified as a main modulator for crush technique safety.32 Thus, several modifications were proposed33 and Chen and colleagues developed the DK-crush.34 A series of landmark trials has documented the efficacy of this technique, that reached a IIb recommendation in the European clinical guidelines for revasculari-zation.21 EBC recognizes the importance of the practice DK-crush but highlights the potential complexity of the technique. Accordingly, careful lesion selection (Table 1) and appropriate training is advocated for interventional cardiologists willing to adopt this technique.
The recommended steps for “DK-crush” are:
Optimal balloon pre-dilation of both branches, then advancement in the SB of a DES (appropriate length to cover SB disease and sized 1:1 according to the SB). The stent should protrude into the MV but such protrusion should be limited to 2–3 mm.
Placement of a balloon in the MV to crush the SB stent (size selected in order to achieve appropriate crush, see below).
The SB stent is inflated whilst the MV balloon is kept uninflated in the MV.
After SB stent deployment, the balloon of the stent might be slightly pulled back and repeated inflation at high pressure can be performed (the balloon inside the MV is still kept un inflated during this phase). This step (called “SB optimization” by Dr Francesco Lavarra in his oral communication at EBC meeting 201835) is aimed at achieving the best stent apposition and expansion at the SB ostium.
The SB stent delivery balloon and the SB guidewire are removed.
The MV balloon is positioned at the level of the SB take-off and high pressure inflation is performed in order to crush the stent struts protruding inside the MV (“balloon-crushing”). The balloon size should be adjusted according to amount of atherosclerosis and MV size, but bench tests show that POT technique is needed to achieve complete stent crushing.
The SB is rewired using a guidewire with an appropriately shaped tip aiming at crossing the SB ostium through a non-distal cell.36
Two balloons are advanced in the SB (diameter size 1:1 according to SB) and the MV (diameter size 1:1 according to distal MV) and kissing balloon inflation is performed according to sequential technique (alternating isolated high pressure inflations of each followed by final simultaneous kissing inflation and deflation).
Balloons and SB guidewire are removed. A stent is advanced and inflated in the MV across SB (size 1:1 with distal MV diameter) covering up all proximal MV segment that is intended to be treated.
A Repeat POT is performed with balloon sized 1:1 to proximal MV.
The SB is rewired using a guidewire with an appropriately bent tip aiming to cross the SB ostium through a non-distal cell. Once again, the rewiring should carefully checked to prevent stent strut removal from the SB ostium.37
Simultaneous kissing balloon inflation with two balloons (MV balloon sized 1:1 to distal MV; SB balloon sized 1:1 to SB diameter) according to sequential technique (alternating isolated high-pressure inflations of each followed by final simultaneous kissing inflation and deflation).38
Post-dilation of the stent at the level of proximal MV up to the carina level with a balloon diameter sized 1:1 according to the proximal MV (final POT).
Figure 7a reports the graphic demonstration of an ideal sequence of technical steps to perform DK-crush. Figure 7b,c shows (by micro-CT) the final appearance of DK-crush stenting.
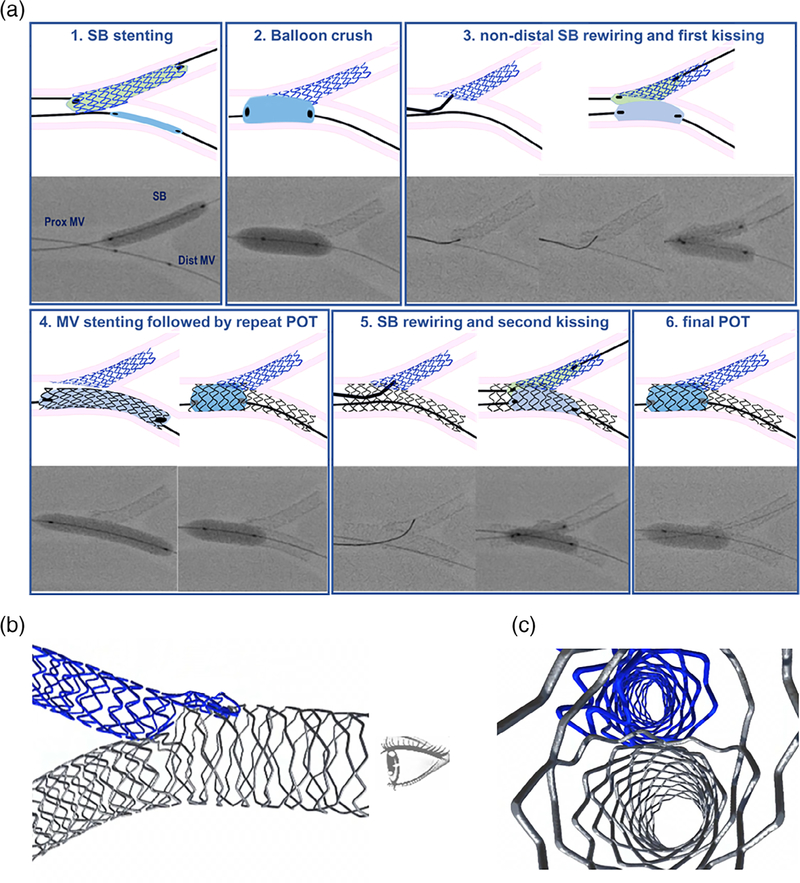
FIGURE 7.
DK-crush. (a) Recommended steps for DK-crush. (1) SB stenting. While the MV balloon is kept un-inflated into the MV, the stent (sized 1:1 according to SB) is implanted in the SB protruding inside the proximal MV for 2–3 mm. After SB stent deployment, the balloon of the stent might be slightly pulled back and repeated inflation at high pressure can be performed (the balloon inside the MV is still kept uninflated during this phase). (2) Balloon crush. After removal of SB stenťs balloon and the SB guidewire, the protruding struts of the SB are crushed by an appropriately sized balloon. Of note, the ideal balloon size to warrant optimal crushing is a balloon sized 1:1 to proximal MV. During the clinical practice, smaller balloons are often selected but this is theoretically associated with risk of incomplete stent crush resulting in floating struts in the MV. (3) Non-distal SB rewiring and first kissing. The SB is rewired using a guidewire with an appropriately bended tip aiming at crossing the SB ostium through a non-distal cell. The absence of unintended distal tracking at the ostium level should be carefully checked before further steps are done. Two non-compliant balloon (eventually after undersized balloon SB dilation) are advanced in the SB (diameter size 1:1 according to SB) and in the MV (diameter size 1:1 according to distal MV) and kissing balloon inflation is performed according to a sequential technique (alternating isolated high pressure inflations of each followed by final simultaneous kissing). (4) MV stenting followed by repeat POT: after SB guidewire removal, stent implantation across the SB take-off with DES diameter selected 1:1 according to the distal MV size is performed. Thereafter, repeat POT with balloon sized 1:1 to proximal MV is done. (5) SB rewiring and second kissing: the SB is rewired using a guidewire with an appropriately bended tip aiming at crossing the SB ostium through a non-distal cell. The “centrality” of rewiring should carefully checked before further steps are done. Simultaneous kissing balloon inflation (usually with non-compliant balloons at high pressure according to the sequential technique) is performed selecting MV balloon sized 1:1 according to distal MV and SB balloon sized 1:1 according to SB diameter. (5) Final POT: performed with balloon sized 1:1 to proximal MV. (b,c) Micro-CT image of stent conformation obtained by DK-crush
8 |. CONCLUSIONS
In the present article, the EBC-promoted expert task force provides an update of a comprehensive bifurcation stenting techniques classification and a detailed description of recommended sequences for both 1- and 2-stent techniques. The present expert consensus may facilitate technique reporting in future studies and provides practical tools for the selection and performance of PCI on bifurcated lesions during the daily clinical practice.
8.1 |. Main messages of the article
Percutaneous treatment of bifurcated lesions is based on the implantation of tubular drug-eluting stents using various techniques. Technique selection (and the different technical steps selected to practice them) are known to determine the final configuration of the implanted stent(s) and have the potential to influence the clinical outcome (restenosis and stent thrombosis).
An original, updated, comprehensive bifurcation stenting techniques classification is provided in order to standardize technique description and reporting.
Since some techniques are more commonly adopted, the recommended sequences for major 1-stent and 2-stent techniques are described and graphically reported to facilitate clinical practice.
ACKNOWLEDGMENTS
The authors wish to thank the physicians who attended the bifurcation techniques meeting held in Brussels on 12 October 2018 for their invaluable help. The bench tests have been done with the help of an independent senior interventional cardiologist (Dr Cristina Aurigemma) using materials donated by Medtronic. Of note, Medtronic did not influence in any way the selection of materials nor the sequences of technical steps performed. In particular, the authors wish to thank Mr Chuck W. O’Neil for his attitude in facilitating the collection and processing of bench test materials. The drawings of the different steps for the described techniques have been personally realized by an independent senior interventional cardiologist (Dr Osama Shoeib).
Abbreviations:
- DES
drug-eluting stent
- DK
double kissing
- EBC
European Bifurcation Club
- MADS
main-across-distal-side
- MV
main vessel
- PCI
percutaneous coronary interventions
- SB
side-branch
- TAP
T and protrusion
Footnotes
CONFLICT OF INTEREST
Burzotta disclosed to have received speaker fees from Medtronic, Abiomed, Abbott. Lassen disclosed to have received speaker fees from Medtronic, Boston Scientific, Biotronik, Abbott and Biosensors. Banning disclosed to have institutional funding of a fellowship form Boston Scientific and Speaker fees Boston, Abbott, Medtronic, Phillips/Volcano and Miracor. Hildick-Smith disclosed to have received Ad Board/Consultancy/Research Funding from Terumo, Medtronic, Abbott, Boston. Pan disclosed to have received speaker fees from Abbott, Terumo and Volcano. Chieffo disclosed to have received speaker fees from Abiomed and GADA. Chatzizisis disclosed to have received speaker fees, consultation fees and research grant from Boston Scientific, and research support from Medtronic. Murasato disclosed to have received speaker fees from Abbott, Terumo, Medtronic, Kaneka, and Orbus Neich. Serruys disclosed to have received personal fees from Abbott Laboratories, AstraZeneca, Biotronik, Cardialysis, GLG Research, Medtronic, Sino Medical Sciences Technology, Société Europa Digital Publishing, Stentys France, Svelte Medical Systems, Philips/Volcano, St Jude Medical, Qualimed, and Xeltis. All other authors reported to have no conflict of interest to disclose.
REFERENCES
- 1.Thomas M, Hildick-Smith D, Louvard Y, et al. Percutaneous coronary intervention for bifurcation disease. A consensus view from the first meeting of the European Bifurcation Club. EuroIntervention. 2006;2: 149–153. [PubMed] [Google Scholar]
- 2.Legrand V, Thomas M, Zelisko M, et al. Percutaneous coronary intervention of bifurcation lesions: state-of-the-art. Insights from the second meeting of the European Bifurcation Club. EuroIntervention. 2007;3:44–49. [PubMed] [Google Scholar]
- 3.Stankovic G, Darremont O, Ferenc M, et al. Percutaneous coronary intervention for bifurcation lesions: 2008 consensus document from the fourth meeting of the European Bifurcation Club. EuroIntervention. 2009;5:39–49. [DOI] [PubMed] [Google Scholar]
- 4.Hildick-Smith D, Lassen JF, Albiero R, et al. Consensus from the 5th European Bifurcation Club meeting. EuroIntervention. 2010;6:34–38. [PubMed] [Google Scholar]
- 5.Stankovic G, Lefèvre T, Chieffo A, et al. Consensus from the 7th European Bifurcation Club meeting. EuroIntervention. 2013;9:36–45. [DOI] [PubMed] [Google Scholar]
- 6.Lassen JF, Holm NR, Stankovic G, et al. Percutaneous coronary intervention for coronary bifurcation disease: consensus from the first 10 years of the European Bifurcation Club meetings. EuroIntervention. 2014;10:545–560. [DOI] [PubMed] [Google Scholar]
- 7.Lassen JF, Holm NR, Banning A, et al. Percutaneous coronary intervention for coronary bifurcation disease: 11th consensus document from the European Bifurcation Club. EuroIntervention. 2016;12: 38–46. [DOI] [PubMed] [Google Scholar]
- 8.Lassen JF, Burzotta F, Banning AP, et al. Percutaneous coronary intervention for the left main stem and other bifurcation lesions: 12th consensus document from the European Bifurcation Club. EuroIntervention. 2018;13:1540–1553. [DOI] [PubMed] [Google Scholar]
- 9.Banning AB, Lassen JL, Burzotta F, et al. Percutaneous coronary intervention for obstructive bifurcation lesions. The 14th consensus document from the European Bifurcation Club. EuroIntervention. 2019;15:90–98. [DOI] [PubMed] [Google Scholar]
- 10.Louvard Y, Thomas M, Dzavik V, et al. Classification of coronary artery bifurcation lesions and treatments: time for a consensus! Catheter Cardiovasc Interv. 2008;71:175–183. [DOI] [PubMed] [Google Scholar]
- 11.Lansky A, Tuinenburg J, Costa M, et al. Quantitative angiographic methods for bifurcation lesions: a consensus statement from the European Bifurcation Group. Catheter Cardiovasc Interv. 2009;73: 258–266. [DOI] [PubMed] [Google Scholar]
- 12.Collet C, Onuma Y, Cavalcante R, et al. Quantitative angiography methods for bifurcation lesions: a consensus statement update from the European Bifurcation Club. EuroIntervention. 2017;13:115–123. [DOI] [PubMed] [Google Scholar]
- 13.Antoniadis AP, Mortier P, Kassab G, et al. Biomechanical modeling to improve coronary artery bifurcation stenting: expert review document on techniques and clinical implementation. JACC Cardiovasc Interv. 2015;8:1281–1296. [DOI] [PubMed] [Google Scholar]
- 14.Ormiston JA, Kassab G, Finet G, et al. Bench testing and coronary artery bifurcations: a consensus document from the European Bifurcation Club. EuroIntervention. 2018;13:e1794–e1803. [DOI] [PubMed] [Google Scholar]
- 15.Burzotta F, Lassen JF, Banning AP, et al. Percutaneous coronary intervention in left main coronary artery disease: the 13th consensus document from the European Bifurcation Club. EuroIntervention. 2018; 14:112–120. [DOI] [PubMed] [Google Scholar]
- 16.Mintz GS, Lefèvre T, Lassen JF, et al. Intravascular ultrasound in the evaluation and treatment of left main coronary artery disease: a consensus statement from the European Bifurcation Club. EuroIntervention. 2018;14:e467–e474. [DOI] [PubMed] [Google Scholar]
- 17.Onuma Y, Katagiri Y, Burzotta F, et al. Joint consensus on the use of OCT in coronary bifurcation lesions by European and Japanese bifurcation clubs. EuroIntervention. 2019;14:e1568–e1577. [DOI] [PubMed] [Google Scholar]
- 18.Burzotta F, Mortier P, Trani C. Characteristics of drug-eluting stent platforms potentially influencing bifurcated lesion provisional stenting procedure. EuroIntervention. 2014;10:124–132. [DOI] [PubMed] [Google Scholar]
- 19.Katsikis A, Chichareon P, Cavalcante R, et al. Application of the MADS classification system in a "mega mammoth" stent trial: feasibility and preliminary clinical implications. Catheter Cardiovasc Interv. 2019;93:57–63. [DOI] [PubMed] [Google Scholar]
- 20.Généreux P, Kumsars I, Lesiak M, et al. A randomized trial of a dedicated bifurcation stent versus provisional stenting in the treatment of coronary bifurcation lesions. J Am Coll Cardiol. 2015;65:533–543. [DOI] [PubMed] [Google Scholar]
- 21.Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40: 87–165. [DOI] [PubMed] [Google Scholar]
- 22.Dérimay F, Rioufol G, Nishi T, et al. Optimal balloon positioning for the proximal optimization technique? An experimental bench study. Int J Cardiol. 2019;292:95–97. [DOI] [PubMed] [Google Scholar]
- 23.Dérimay F, Finet G, Souteyrand G, et al. Benefit of a new provisional stenting strategy, the re-proximal optimisation technique: the rePOT clinical study. EuroIntervention. 2018;14:e325–e332. [DOI] [PubMed] [Google Scholar]
- 24.Burzotta F, de Vita M, Sgueglia G, Todaro D, Trani C. How to solve difficult side branch access? EuroIntervention. 2010;6(suppl J): J72–J80. [DOI] [PubMed] [Google Scholar]
- 25.Murasato Y, Iwasaki K, Yamamoto T, et al. Optimal kissing balloon inflation after single-stent deployment in a coronary bifurcation model. EuroIntervention. 2014;10:934–941. [DOI] [PubMed] [Google Scholar]
- 26.Mylotte D, Hovasse T, Ziani A, et al. Non-compliant balloons for final kissing inflation in coronary bifurcation lesions treated with provisional side branch stenting: a pilot study. EuroIntervention. 2012;7: 1162–1169. [DOI] [PubMed] [Google Scholar]
- 27.Sawaya FJ, Lefèvre T, Chevalier B, et al. Contemporary approach to coronary bifurcation lesion treatment. JACC Cardiovasc Interv. 2016; 9:1861–1878. [DOI] [PubMed] [Google Scholar]
- 28.Burzotta F, Gwon HC, Hahn JY, et al. Modified T-stenting with intentional protrusion of the side-branch stent within the main vessel stent to ensure ostial coverage and facilitate final kissing balloon: the T-stenting and small protrusion technique (TAP-stenting). Report of bench testing and first clinical Italian-Korean two-Centre experience. Catheter Cardiovasc Interv. 2007;70:75–82. [DOI] [PubMed] [Google Scholar]
- 29.Burzotta F, Džavík V, Ferenc M, Trani C, Stankovic G. Technical aspects of the T And small Protrusion (TAP) technique. EuroIntervention. 2015;11(suppl V):V91–V95. [DOI] [PubMed] [Google Scholar]
- 30.Chevalier B, Glatt B, Royer T, Guyon P. Placement of coronary stents in bifurcation lesions by the "culotte" technique. Am J Cardiol. 1998; 82:943–949. [DOI] [PubMed] [Google Scholar]
- 31.Colombo A, Stankovic G, Orlic D, et al. Modified T-stenting technique with crushing for bifurcation lesions: immediate results and 30-day outcome. Catheter Cardiovasc Interv. 2003;60:145–151. [DOI] [PubMed] [Google Scholar]
- 32.Colombo A Bifurcational lesions and the "crush" technique: understanding why it works and why it doesnť-a kiss is not just a kiss. Catheter Cardiovasc Interv. 2004;63:337–338. [DOI] [PubMed] [Google Scholar]
- 33.Collins N, Dzavik V. A modified balloon crush approach improves side branch access and side branch stent apposition during crush stenting of coronary bifurcation lesions. Catheter Cardiovasc Interv. 2006;68: 365–371. [DOI] [PubMed] [Google Scholar]
- 34.Chen SL, Zhang JJ, Ye F, et al. Study comparing the double kissing (DK) crush with classical crush for the treatment of coronary bifurcation lesions: the DKCRUSH-1 Bifurcation Study with drug-eluting stents. Eur J Clin Invest. 2008;38:361–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lavarra F Proximal side optimization: a modification of the double kissing crush technique. US Cardiology Review. 2020;14:e02. 10.15420/usc.2020.07. [DOI] [Google Scholar]
- 36.Zhang JJ, Chen SL, Ye F, et al. Mechanisms and clinical significance of quality of final kissing balloon inflation in patients with true bifurcation lesions treated by crush stenting technique. Chin Med J (Engl). 2009;122:2086–2091. [PubMed] [Google Scholar]
- 37.Murasato Y, Hikichi Y, Horiuchi M. Examination of stent deformation and gap formation after complex stenting of left main coronary artery bifurcations using microfocus computed tomography. J Interv Cardiol. 2009;22:135–144. [DOI] [PubMed] [Google Scholar]
- 38.Ormiston JA, Webster MW, Webber B, Stewart JT, Ruygrok PN, Hatrick RI. The "crush" technique for coronary artery bifurcation stenting: insights from micro-computed tomographic imaging of bench deployments. JACC Cardiovasc Interv. 2008;1:351–357. [DOI] [PubMed] [Google Scholar]