Abstract
Follicular helper T (TFH) cells provide help to B cells, supporting the formation of germinal centres that allow affinity maturation of antibody responses. Although usually located in secondary lymphoid organs, T cells bearing features of TFH cells can also be identified in human blood, and their frequency and phenotype are often altered in people with autoimmune diseases. In this Perspective article, I discuss the increase in circulating TFH cells seen in autoimmune settings and explore potential explanations for this phenomenon. I consider the multistep regulation of TFH cell differentiation by the CTLA4 and IL-2 pathways as well as by regulatory T cells and highlight that these same pathways are crucial for regulating autoimmune diseases. The propensity of infection to serve as a cue for TFH cell differentiation and a potential trigger for autoimmune disease development is also discussed. Overall, I postulate that alterations in pathways that regulate autoimmunity are coupled to alterations in TFH cell homeostasis, suggesting that this population may serve as a core sentinel of dysregulated immunity.
Subject terms: Peripheral tolerance, Germinal centres, Autoimmunity
Individuals with autoimmunity often have an increased frequency of T cells bearing features of follicular helper T cells in their blood. Lucy Walker proposes that alterations in pathways that regulate autoimmunity are coupled to alterations in follicular helper T cell homeostasis.
Introduction
Coordinated interaction between different immune cells is crucial for the development of protective immunity. Nowhere is this more obvious than in the emergence of high affinity antibody responses, where carefully orchestrated contacts between dendritic cells (DCs), T cells and B cells culminate in a refined and long-lived antibody response. The critical go-between in this cellular trio is the follicular helper T (TFH) cell that liaises first with the DC, before migrating to the B cell follicle for repeated interaction with B cells1. Such TFH cells bear a characteristic phenotype including expression of markers such as CXC-chemokine receptor 5 (CXCR5; which promotes homing to the B cell follicle), programmed cell death protein 1 (PD1), inducible T cell costimulator (ICOS) and the transcription factor BCL-6 (ref.2) (Box 1). TFH cells are classically found in secondary lymphoid organs with a small population of similar cells present in the blood (referred to as circulating TFH (cTFH) cells). Curiously, multiple studies have revealed that cTFH cells are present at increased frequencies in many autoimmune diseases, including systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), Sjogren syndrome (SS), autoimmune thyroid diseases, myasthenia gravis, type 1 diabetes (T1D) and multiple sclerosis (MS)3. Consistent with elevations in cTFH cell numbers, autoantibodies are commonly associated with these conditions and their presence often precedes symptomatic disease.
In this Perspective, I discuss core mechanisms controlling TFH cell differentiation and highlight that these same pathways are linked to the regulation of autoimmune disease. I also discuss the potential for infection to serve as a link between TFH cells and autoimmunity. Overall, I postulate that regulation of TFH cells and regulation of autoimmunity are tightly coupled, perhaps explaining why increases in cTFH cell numbers are evident across multiple autoimmune diseases.
Box 1 Transcription factors controlling TFH cell development.
BCL-6 is an essential transcription factor for follicular helper T (TFH) cell differentiation143–145, and its repression of BLIMP1 is necessary144 but not sufficient146 for the TFH cell fate. Other key transcription factors include MAF, which is upregulated by inducible T cell costimulator (ICOS) ligation147, and BATF, which controls expression of BCL-6 and MAF148,149. ASCL2 promotes early TFH cell differentiation by upregulating the expression of genes such as CXCR5 (ref.150), whereas repression of KLF2 expression is required to maintain the TFH cell phenotype151. STAT proteins play a major role in influencing TFH cell differentiation in response to cytokines: STAT5 inhibits TFH cell differentiation following IL-2 exposure and, conversely, STAT3, STAT1 and STAT4 promote TFH cell differentiation in response to cytokines such as IL-6, IL-21 and IL-12 (refs81,152,153).
Discovery of cTFH-like cells
In 2005, a seminal publication from Vinuesa et al. showed that mutant mice with dysregulated TFH cell differentiation exhibited systemic autoimmunity4. The causative mutation in these animals mapped to the Roquin (Rc3h1) gene, the product of which repressed ICOS expression and negatively regulated TFH cell differentiation. These sanroque mice exhibited lupus-like pathology and robust development of T1D when crossed to a T cell receptor (TCR) transgenic mouse model. Impairing TFH cell differentiation, by rendering sanroque mice heterozygous for BCL-6 or deficient for SLAM-associated protein (SAP, an adaptor protein required for TFH cell–B cell interactions5), ameliorated the autoimmune phenotype, leading to reduced autoantibody production and decreased renal pathology6. These findings sparked interest in whether TFH cell differentiation might be connected to lupus pathology in humans, leading to the demonstration that cells with a TFH cell phenotype were elevated in the blood of patients with SLE7. Reports documenting cTFH-like cells in numerous other autoimmune diseases rapidly followed (reviewed in ref.8).
The spotlight was then turned on the true identity of these blood-borne TFH-like cells, specifically on their relationship to germinal centre (GC)-resident TFH cells. Important work from the Ueno group revealed that circulating CD4+CXCR5+ T cells shared functional properties with TFH cells from secondary lymphoid organs and could provide help to B cells via IL-21 production9. This led to the idea that blood-borne CD4+CXCR5+ T cells were a memory counterpart of lymphoid TFH cells, and a substantial body of evidence has since emerged to support this view10–14. Consistent with this notion, individuals with defects in GC formation due to deficiency in ICOS or CD40L, or a developmental block in B cell development (BTK deficiency), have fewer circulating CD4+CXCR5+ cells, and they are absent altogether from the cord blood of newborns15,16. Of note, many TFH cell markers are downregulated in the memory phase12,17–19, perhaps explaining early controversies over the existence of a TFH cell memory pool. Experiments involving the adoptive transfer of mouse TFH cells into antigen-free hosts indicate that CXCR5 expression is least affected by the phenomenon of TFH cell marker loss20, suggesting it may be the most reliable marker for tracking cTFH cells. Painstaking experiments in which cTFH cells were purified from mouse blood revealed that these cells can home to secondary lymphoid tissues upon re-challenge and participate in GC reactions, providing direct evidence of their functional capacity upon antigen re-encounter18. Thus, the consensus view is that TFH cells have a circulating memory compartment that retains expression of CXCR5 and, to a variable extent, other TFH cell markers and can be recalled to participate in the memory phase of humoral responses.
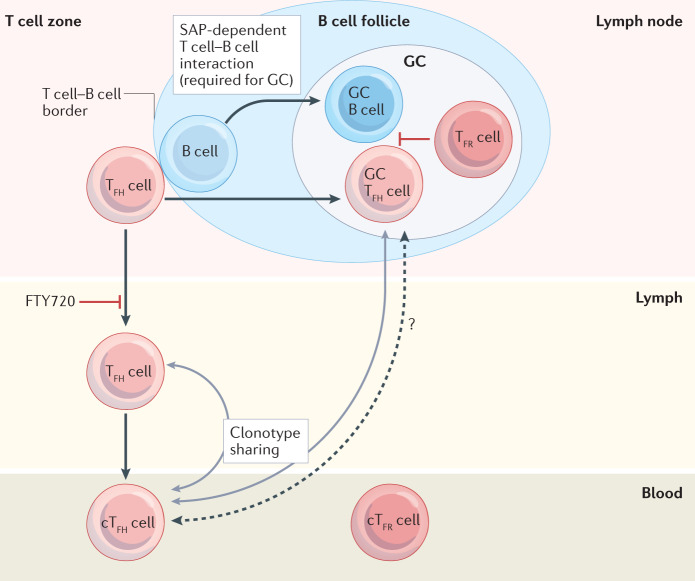
Somewhat unexpectedly, the majority of cTFH cells do not seem to derive from the GC environment itself. In fact, imaging studies have shown that, although GC TFH cells frequently move between GCs, their egress to the circulation is rare21. Instead, it appears that circulating CXCR5+ cells arise mainly from TFH cells that have not yet undergone sustained interaction with B cells. In line with this, the frequency of cTFH cells appears undiminished in mice and humans that lack SAP expression and consequently exhibit impaired T cell–B cell interactions22. The link between lymphoid tissue TFH cells and cTFH cells has been compellingly demonstrated both by mass cytometric comparison of blood and tonsillar tissue with dimensionality reduction approaches23 and by vaccination studies showing that blood CD4+CXCR5+ICOS+PD1+ cells24 or CD4+CXCR5+PD1hi cells25 are clonally related to lymph node GC TFH cells. Overall, this suggests a model in which TFH cells at the T cell–B cell border can give rise to both GC-resident TFH cells and cTFH cells that travel through efferent lymph to the blood (Fig. 1). Consistent with this, T cells with TFH cell features can be detected in thoracic duct lymph of mice and humans, and treatment with the drug FTY720, which prevents lymph node exit, dramatically decreases cTFH cells in both species18,26,27.
Fig. 1. Blood-borne cTFH cells are clonally related to their lymphoid counterparts.
Follicular helper T (TFH) cells classically reside in secondary lymphoid organs where they support germinal centre (GC) B cell responses; however, T cells with similar markers can be detected in the lymph and blood. These circulating TFH (cTFH) cells have a memory phenotype and do not depend on GCs as they can arise in the context of SLAM-associated protein (SAP) deficiency, which abrogates sustained T cell–B cell interactions22. However, they do require B cells, as cTFH cell frequencies are greatly reduced in individuals with B cell deficiency16. Blocking lymph node exit, by treatment with FTY720, dramatically decreases cTFH cells in mice and humans18,26,27. Clonotype sharing reveals a developmental relationship between TFH cells found in the GC and the blood24,25 and those found in the lymph and the blood26, suggesting that T cell–B cell interactions at the T cell–B cell border give rise to both GC TFH cells and cTFH cells. It is possible that some GC TFH cells enter the circulation from GCs but this is likely to be rare21. Follicular regulatory T (TFR) cells also have circulating counterparts (cTFR); however, these have an immature phenotype and differentiate from regulatory T cells without the requirement for contact with B cells164.
Common pathways regulate TFH cell differentiation and autoimmunity
TFH cell differentiation and provision of help to B cells is a tightly controlled process. B cell tolerance relies heavily on restricting T cell help, in part because the developmental regulation of T cells is more stringent; nascent T cells are screened against self-antigens during their thymic development, with transcription factors, such as autoimmune regulator (AIRE), ensuring a broad representation of peripheral self-antigens. By contrast, peripheral self-antigens may be less available to B cells developing in the bone marrow, and it has been reported that around 20% of mature naive B cells exhibit low levels of self-reactivity28. B cell antigen specificity is also prone to diversification within GCs, superseding any developmental constraints on self-reactivity. Thus, denying T cell help to self-reactive B cells is necessary to prevent the initiation of potentially damaging autoimmune humoral responses. Ensuring that T cell–B cell collaboration is tightly regulated is also important for optimal protective immunity (Box 2).
In considering the mechanisms controlling TFH cell differentiation, three core and interconnected pathways emerge involving cytotoxic T lymphocyte antigen 4 (CTLA4), regulatory T (Treg) cells and IL-2. Curiously, these same pathways are well recognized for their ability to regulate autoimmunity. Below, I explore evidence indicating that these pathways control TFH cell differentiation and highlight their connection to autoimmune disease susceptibility.
Box 2 Optimal germinal centre B cell selection relies on restricting follicular helper T cell numbers.
Upon antigen engagement, B cells migrate to the T cell–B cell border in search of T cell help154. Restricting the number of T cells available limits how many B cells can seed germinal centres (GCs)155, reducing the number of clones exposed to hypermutation. T cell–B cell interactions at the T cell–B cell border support the extrafollicular response156 and dysregulation of extrafollicular T cells may lead to autoimmunity157. In the follicular response, B cells compete again for T cell help in the GC light zone, with those expressing the highest affinity receptors able to capture more antigen and present higher peptide concentrations. Immunoglobulin gene mutations resulting in enhanced antigen affinity trigger GC B cells to upregulate CCL22 and CCL17 expression, allowing them to preferentially attract T cell help158. Limiting the number of T cells available and ensuring that their cytokine output remains ‘stingy’159 are crucial features of the competitive environment required for affinity maturation to occur.
CTLA4-mediated regulation of TFH cells
CTLA4 controls T cell CD28 costimulation and is a crucial regulator of T cell responses (Box 3). Multiple lines of evidence pinpoint the CTLA4–CD28 axis as a key modulator of TFH cell responses (Box 3). In mice, genetic deficiency or antibody-mediated blockade of CTLA4 triggers spontaneous TFH cell differentiation and GC formation29. GCs that form following CTLA4 blockade are dependent on CD28 (ref.29), consistent with the established role of CTLA4 in regulating CD28 engagement and the importance of the CD28 pathway for TFH cells and GCs30,31. Experiments with CD28 heterozygous mice revealed a relationship between the amount of CD28 engagement and propensity for TFH cell differentiation29, suggesting that CTLA4 may regulate this fate by policing access of CD28 to its ligands. CD28 likely promotes TFH cell differentiation in multiple ways, including increasing ICOS expression, which drives strong phosphoinositide 3-kinase (PI3K) activation important for TFH cell formation32, as well as regulating microRNAs implicated in TFH cell fate29,33.
There is also evidence that the CTLA4 pathway regulates TFH cells in humans. Individuals deficient in LRBA, that show defective CTLA4 trafficking and function, exhibit increases in circulating T cells expressing TFH cell markers (CXCR5 and PD1)34. In addition, patients with cancer receiving anti-CTLA4 antibody immunotherapy show an increase in circulating T cells with TFH cell markers (E. Ntavli, N. M. Edner and L.S.K. Walker, unpublished observations). Conversely, cTFH cells are decreased following treatment with soluble CTLA4 molecules, such as the CTLA4–immunoglobulin fusion protein abatacept, in individuals with SS35, RA36, MS37 or T1D38. Thus, the CTLA4 pathway negatively regulates TFH cell homeostasis in mice and humans, likely by restricting CD28 engagement.
Box 3 CTLA4 function.
Cytotoxic T lymphocyte antigen 4 (CTLA4) acts as a competitive inhibitor for the T cell costimulator CD28 as both receptors bind to the same ligands, CD80 and CD86, but CTLA4 binds with higher affinity. Furthermore, CTLA4 and CD80 form high-avidity dimer–dimer interactions160. CTLA4 can function in a cell-extrinsic manner to remove CD80 and CD86 from antigen-presenting cells by a process known as transendocytosis161. Expression of CTLA4 by regulatory T (Treg) cells is required to prevent fatal autoimmune disease in mice162, and Treg cells can use CTLA4 to control the levels of CD80 and CD86 on dendritic cells trafficking from peripheral tissues to lymph nodes117. As the biological role of CTLA4 is to regulate the CD28 pathway, phenotypes associated with CTLA4 deficiency are lost in the absence of their shared ligands163.
Follicular helper T (TFH) cells are reciprocally regulated by CTLA4 and CD28. Mice lacking CTLA4 systemically or in Treg cells exhibit exaggerated TFH cell differentiation and this is recapitulated by injection of blocking anti-CTLA4 antibodies29,45,48 (see figure, part a). Humans with CTLA4 trafficking defects also exhibit increases in TFH cell numbers34. Conversely, soluble CTLA4 fusion proteins decrease TFH cell numbers in mice and humans35,36,38. Mice with wild-type CD28 expression have intact TFH cell development, and those with lower CD28 expression due to Cd28 gene heterozygosity show a reduced propensity for TFH cell development, whereas complete CD28 deficiency abrogates TFH cell development29,31 (see figure, part b).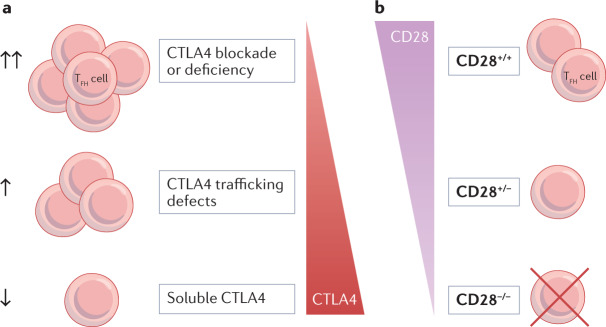
CTLA4 and autoimmunity
The association between CTLA4 and autoimmunity is well documented. Genetic variation at the CTLA4 locus is linked to numerous autoimmune diseases, including T1D, RA, SLE, myasthenia gravis, autoimmune thyroid diseases, coeliac disease, alopecia areata and vitiligo (see GWAS Catalogue). Mice genetically deficient for Ctla4 develop lethal lymphoproliferation and multiorgan immune cell infiltration39,40, and heterozygous CTLA4 mutations in humans are associated with an immune dysregulation syndrome with multiple autoimmune manifestations41,42. Targeting the CTLA4 pathway by immunotherapy in patients with cancer can also elicit autoimmune side effects. CTLA4 function may be altered indirectly by mutations in genes encoding CTLA4 pathway regulators. For example, mutations in LRBA lead to reduced CTLA4 expression and autoimmune outcomes43.
Treg cell-mediated control of TFH cells
Treg cells express the transcription factor FOXP3 and play a crucial role in the maintenance of immune homeostasis. Scurfy mice, which lack functional Treg cells owing to a frameshift mutation disrupting Foxp3, exhibit a marked expansion of BCL-6+CXCR5+ TFH cells in secondary lymphoid tissues44. Consistent with this, in mice expressing diphtheria toxin receptor under the control of the Foxp3 promoter, short-term depletion of Treg cells enhances the generation of antigen-specific TFH cells in response to immunization45,46. Similar to mice, patients with IPEX (immune dysregulation, polyendocrinopathy, enteropathy, X-linked) that have mutations in FOXP3 also exhibit an increased frequency of CXCR5+PD1+ cTFH cells47. Thus, FOXP3+ Treg cells appear to control TFH cell numbers in both mice and humans.
Treg cells constitutively express CTLA4. Interestingly, the enhanced TFH cell differentiation associated with CTLA4 deficiency29 can be recapitulated by loss of CTLA4 expression in Treg cells alone45,48. To avoid widespread immune dysregulation, Sage et al.48 used mice in which tamoxifen-inducible Foxp3-Cre was used to excise the floxed Ctla4 gene in Treg cells immediately prior to immunization, whereas Wing et al.45 probed the impact of partial loss of CTLA4 expression using heterozygous Ctla4-flox/wt mice expressing Foxp3-Cre. In both settings, increases in TFH cells were observed after immunization. Collectively, these findings illustrate that Treg cells are a non-redundant population mediating CTLA4-dependent regulation of TFH cells.
The above observations could potentially reflect the role of CTLA4 in follicular regulatory T (TFR) cells, the subset of Treg cells that exhibit TFH cell features and enter GCs44,46,49. For Treg cells to acquire the TFR cell programme they downregulate CD25 (IL-2Rα) expression, permitting them to express BCL-6, which would otherwise be antagonized by IL-2-driven BLIMP1 expression50,51. TFR cells are thought to optimize protective antibody responses while suppressing the generation of antibodies to self-antigens and allergens44,46,49,52–54 and, like TFH cells, TFR cells have a circulating counterpart that can be altered in autoimmunity55,56 (Fig. 1). Interestingly, selective depletion of TFR cells, either in mice with floxed Bcl6 and Foxp3-driven Cre expression54,57,58 or in mice with STOP-floxed Cxcr5-DTR and Foxp3-Cre53, results in only minor or transient increases in TFH cells despite marked effects on B cell differentiation. As loss of CTLA4 expression in FOXP3+ cells increases TFH cells but loss of TFR cells does not, it is possible that substantial CTLA4 activity occurs outside of the B cell follicle during the initial encounter between T cells and DCs. At the T cell–B cell border and within the follicle, TFR cells may employ additional suppressive mechanisms such as expression of the neuropeptide neuritin57 or targeting of B cell metabolic pathways59.
In a fascinating twist, it appears that FOXP3-based regulation of TFH cells can also operate in a cell-intrinsic manner. TFH cells themselves upregulate FOXP3 expression in late-stage GCs, and this is associated with loss of expression of the T cell help-associated genes IL21 and CD40L and GC collapse60. These FOXP3+ TFH cells express high levels of CTLA4 and are reminiscent of the CD25– TFR cells described by Wing et al.61, the transcriptional profiles of which place them equidistant between TFH cells and activated Treg cells. The division of labour between Treg cells, TFR cells and FOXP3+ TFH cells will need to be dissected by further experimentation. Taken together, Treg cell populations play a key role in controlling TFH cell numbers in both mice and humans, potentially via the CTLA4 pathway.
Treg cells and autoimmunity
Many of the genes associated with susceptibility to autoimmunity are expressed in Treg cells62 and the pre-eminent role for Treg cells in regulating autoimmunity is well recognized. Mice lacking Treg cells develop lethal autoimmunity63 and humans with an impaired Treg cell compartment as a result of mutations in FOXP3 develop the aggressive early-onset immune dysregulation syndrome IPEX64. Interestingly, deficits in Treg cells can interfere with normal costimulatory control of T cell immunity — the unexpected exacerbation of disease in CD28-deficient non-obese diabetic mice was reconciled by the discovery of the role of CD28 in Treg cell development65, and recent findings suggest CD28 also contributes to Treg cell homeostasis in humans66. A replete Treg cell compartment is therefore key to the normal regulation of immune responses, and strategies aimed at augmenting Treg cell numbers, by low-dose IL-2 treatment or Treg cell therapy, are being actively pursued in settings of autoimmunity.
IL-2-mediated regulation of TFH cells
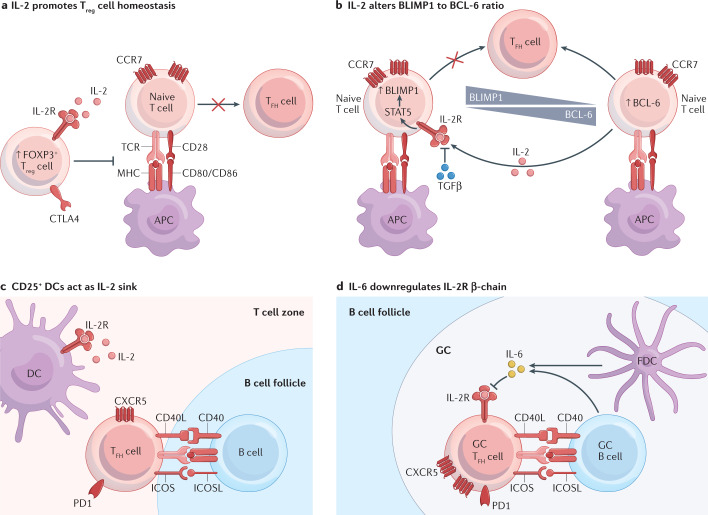
The IL-2 pathway is recognized as a major regulator of TFH cell differentiation (Fig. 2). In mice, exogenous provision of IL-2 has been shown to suppress TFH cell differentiation both in the context of viral infection67 and autoimmunity68. In humans, IL-2 is also a known regulator of TFH cell differentiation69, and low-dose IL-2 therapy can decrease numbers of cTFH cells in individuals with autoimmune disease70.
Fig. 2. IL-2-based inhibition of TFH cells and adaptations to subvert this.
a | IL-2 plays an important role in promoting FOXP3+ regulatory T (Treg) cell homeostasis; Treg cell-deficient mice44 and humans47 exhibit increased follicular helper T (TFH) cell numbers. b | During T cell priming, IL-2-induced signalling through the IL-2 receptor (IL-2R) upregulates BLIMP1 expression, skewing the BLIMP1 to BCL-6 ratio and inhibiting TFH cell differentiation74–77. Transforming growth factor-β (TGFβ) decreases IL-2R signalling by suppressing CD25 (IL-2Rα) expression80. c | CD25-expressing dendritic cells (DCs) in the outer T cell zone can capture local IL-2, favouring TFH cell differentiation82. d | Within the germinal centre (GC), IL-6 can desensitize IL-2R signalling in mature TFH cells by downregulating the IL-2R subunit CD122 (IL-2Rβ)83. APC, antigen-presenting cell; CTLA4, cytotoxic T lymphocyte antigen 4; CXCR5, CXC-chemokine receptor 5; FDC, follicular dendritic cell; ICOS, inducible T cell costimulator; ICOSL, ICOS ligand; PD1, programmed cell death protein 1; TCR, T cell receptor.
One potential mechanism by which IL-2 inhibits TFH cells is by enhancing Treg cell homeostasis as IL-2 is a key cytokine for Treg cell expansion and maintenance71–73. However, it is clear that IL-2 can also act directly on conventional T cells to inhibit TFH cell differentiation. During T cell priming, IL-2 signalling can alter the balance between TFH cell and non-TFH cell effector differentiation74,75 via STAT5-mediated skewing of the BLIMP1 to BCL-6 ratio76,77. In an interesting twist, T cells induced to make IL-2 are not those that respond to it — instead, the producers become TFH cells while using IL-2 in a paracrine manner to preclude their neighbours from this fate78. This finding establishes a biological role for the synaptic-based delivery of IL-2 between adjacent T cells undergoing activation79.
Such is the threat to TFH cell differentiation posed by IL-2 that a variety of mechanisms exists to subvert this inhibition. Transforming growth factor-β (TGFβ) insulates T cells from IL-2 signals by suppressing CD25 (IL-2Rα) expression80, which may contribute to its ability to promote TFH cell differentiation81. Activated DCs in the outer T cell zone upregulate CD25, allowing developing TFH cells to approach the B cell follicle in an environment quenched of local IL-2 (ref.82). Mature TFH cells can be shielded from IL-2 in a different manner, becoming desensitized to IL-2 signalling via IL-6-mediated downregulation of the IL-2 receptor subunit CD122 (IL-2Rβ)83. The local availability of IL-2 and other cytokines is therefore an important factor in controlling TFH cell numbers. Intriguingly, in conditions of limiting IL-2, T helper 1 cells can increase their BCL-6 to T-bet ratio and assume a partial TFH cell phenotype84. Thus, some cells bearing TFH cell markers in autoimmune settings could conceivably have arisen via this route.
The intersection between IL-2-mediated and Treg cell-mediated control of TFH cell differentiation is a complex one. Treg cells might be expected to promote TFH cell differentiation by serving as an IL-2 sink85,86 but they can also limit TFH cell formation by CTLA4-dependent regulation of costimulation29,45,48. One way to view this is that avoiding IL-2 signals may be necessary but not sufficient for TFH cell differentiation and, as highlighted above, this can be achieved through a variety of means. By contrast, there seems to be little redundancy in control of CD28 costimulation, with CTLA4-expressing Treg cells being required to restrict TFH cell numbers45,48. Thus, in the absence of Treg cells, the effects of dysregulated CD28 costimulation may dominate over the lack of IL-2 consumption as other populations can compensate for the latter.
IL-2 and autoimmunity
The IL-2 pathway is strongly implicated in susceptibility to autoimmune disease. Single nucleotide polymorphisms (SNPs) in IL2RA are associated with multiple autoimmune diseases, including T1D, RA, IBD, MS, Crohn’s disease, alopecia areata and vitiligo (see GWAS catalogue). In addition to Il2RA SNPs87, autoimmune-associated variants have been identified in IL2, IL2RB and PTPN2. PTPN2 is a phosphatase involved in many signalling pathways, including IL-2 receptor signalling. T cell-specific deficiency in Ptpn2 increased frequencies of TFH cells and GC B cells in non-obese diabetic mice and was associated with exacerbated diabetes88. It is likely that multiple pathways control IL-2 receptor signalling as defects are evident in T1D and MS even after controlling for IL2RA and PTPN2 genotypes89. Mice deficient in IL-2 or the IL-2 receptor subunits CD122 (IL-2Rβ) or CD25 (IL-2Rα) develop lethal autoimmunity90–92 and mutations in IL-2Rβ cause life-threatening immune dysregulation in humans93. Importantly, although IL-2 pathway genes can clearly modulate autoimmunity via effects on Treg cell homeostasis, they can also act in conventional T cells: for example, a SNP at the Il2RA locus associated with protection from T1D and MS was linked to higher levels of CD25 expression on conventional memory CD4+ T cells94. Consistent with the role of the IL-2 pathway in the regulation of autoimmunity, low-dose IL-2 can be used therapeutically across a wide range of autoimmune diseases95.
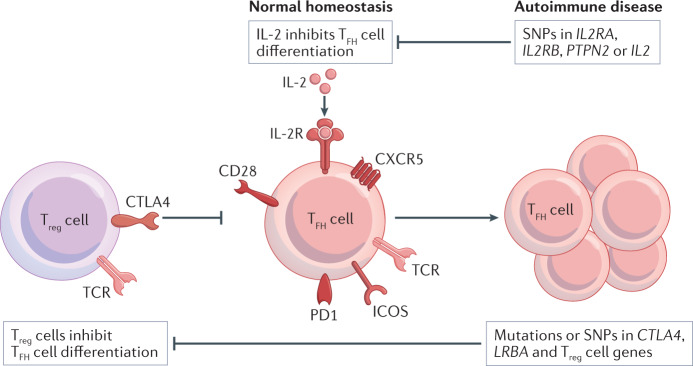
Collectively, these studies highlight the connection between control of TFH cell differentiation and the genetic regulation of autoimmunity. Notably, genes in the CTLA4 and IL-2 pathways are consistently highlighted in genetic analyses across a broad range of common autoimmune conditions96,97, and SNPs associated with autoimmunity are enriched in CpG demethylated regions specifically found in Treg cells62. This places CTLA4, IL-2 and Treg cells at the heart of the shared genetic susceptibility to autoimmune disease that underpins heritability. Importantly, any defects in the CTLA4 or IL-2 pathways or deficits in Treg cell homeostasis or function would lead to a dysregulated TFH cell compartment as well as to the propensity to autoimmune disease (Fig. 3). This could be one reason for increases in cTFH cells being seen across multiple autoimmune disease settings.
Fig. 3. Common pathways control autoimmune susceptibility and TFH cell homeostasis.
In healthy individuals, follicular helper T (TFH) cell homeostasis is maintained by the CTLA4 pathway and regulatory T (Treg) cells as well as by IL-2. Defects in the IL-2–IL-2R pathway can increase TFH cell numbers, and single nucleotide polymorphisms (SNPs) in the IL-2 pathway are associated with autoimmune disease. Altered CTLA4 expression or trafficking (for example, owing to LRBA mutations) or defects in Treg cells can increase TFH cell numbers and are also associated with autoimmune disease susceptibility. CTLA4, cytotoxic T lymphocyte antigen 4; CXCR5, CXC-chemokine receptor 5; ICOS, inducible T cell costimulatory; PD1, programmed cell death protein 1; TCR, T cell receptor.
Infection as a link between TFH cell differentiation and autoimmunity
The principal biological role for TFH cells lies in protection from infectious disease. TFH cell differentiation in response to viral, bacterial, parasitic or fungal antigens is key for the generation of protective antibody responses, in particular affinity-matured neutralizing antibodies98. Mimicking infection by vaccination also induces TFH cells, with transient increases in cTFH cells being detectable in the blood99.
Notably, infectious triggers have been postulated for many autoimmune diseases100–104. Lyme disease is the quintessential example whereby immune responses to tick-borne Borrelia burgdorferi can give rise to Lyme arthritis with autoimmune T cell and B cell responses105. In most of the common autoimmune diseases, a clear link to an individual pathogen is lacking; however, circumstantial evidence is often strong. For example, there is a known association between enteroviral infections and T1D106, and enteroviral capsid protein107 and an antiviral signature108 have been detected in the pancreatic islets of people with T1D. Furthermore, recent data show a clear link between Epstein–Barr virus infection and the development of MS109,110.
Persistent TFH cells in chronic infection: helpers for autoreactive B cells
Although TFH cell increases are short-lived in acute infection, chronic viral infections elicit persistent TFH cell responses111,112. Such increases in TFH cells could interfere with competitive selection within the GC, potentially allowing the survival of self-reactive B cells. Indeed, persistent viral infection can elicit polyclonal B cell activation and production of autoantibodies113. In light of this, it is interesting that prolonged enteroviral infection, rather than multiple short-duration infections, is associated with islet autoimmunity in T1D114.
The ability of self-reactive B cells to take up viral antigens, via pinocytosis, Fc receptors or complement receptors, may allow them to present viral peptides and solicit help from virus-specific TFH cells113. In experimental systems, B cells specific for the central nervous system self-antigen myelin oligodendrocyte glycoprotein (MOG) can co-capture influenza virus haemagglutinin and MOG from cell membranes and obtain help from haemagglutinin-specific T cells to produce anti-MOG antibodies115. Interestingly, the ability of TFH cells to provide help to bystander B cells and elicit autoantibody production appears to be enhanced by lymphopenia20, a state long associated with autoimmunity. Conceivably, lymphopenia in the context of SARS-CoV-2 infection could contribute to the generation of autoantibodies documented in patients with COVID-19 (ref.116).
Potential for infection to unleash self-reactive TFH cells
Chronic infections may alter T cell activation thresholds via the upregulation of costimulatory ligands in response to Toll-like receptor engagement or pro-inflammatory cytokines. This costimulatory ligand upregulation may outpace CTLA4-dependent ligand downregulation, permitting the activation of self-reactive T cells normally censored by insufficient CD28 engagement117. Prolonged increases in TFH cells could exacerbate this by increasing levels of IL-21, the archetypal TFH cell-associated cytokine, which can counteract Treg cell suppression118,119 and may reinforce TFH cell differentiation120. IL-21 is overexpressed in several autoimmune diseases, including SLE, RA, SS and T1D121, and although it can also derive from other cells, significant correlations between IL-21 production and TFH cell frequencies have been noted122,123. Thus, chronic infectious settings associated with elevated IL-21, blunted Treg cell function and increased costimulation could permit self-reactive T cells to acquire a TFH cell phenotype.
Infection may play a role in epitope spreading, which is a feature of many autoimmune diseases and is frequently associated with disease progression. One mechanism that may contribute to this phenomenon is the invasion and reuse of existing GCs by B cells bearing a different specificity, particularly in the context of shared T cell help (for example, when B cells specific for distinct regions of a protein interact with the same TFH cell owing to presentation of a common peptide)124. Cross-reactive recognition of bacterial antigens by self-reactive T cells could conceivably form the basis of shared T cell help in autoimmune settings125. Notably, the presence of adjuvants, including the bacterial molecule lipopolysaccharide, can enhance GC invasion and reuse124, suggesting that, in addition to unleashing new cohorts of TFH cells, infection may also enhance the sharing of T cell help between B cells of different specificities.
The type 1 interferon connection
Infection and autoimmunity may also intersect mechanistically at involvement of the type 1 interferon pathway. Type 1 interferons provide the key ‘early warning’ signal of viral infection and play complex roles in protection or pathology following infection with viruses, bacteria, parasites and fungi126. The type 1 interferon pathway has been widely associated with autoimmune diseases, most notably in the case of SLE but also in T1D, MS, RA and others127–130. There are conflicting reports on the impact of type 1 interferons on TFH cell differentiation. There is evidence that type 1 interferons promote acquisition of at least some aspects of the TFH cell phenotype131, although other data suggest that they support T helper 1 cells at the expense of TFH cells132. Studies focusing on DCs as the target cells for type 1 interferons point to a positive role in TFH cell differentiation following immunization or vaccination133,134 but a negative role in the setting of Plasmodium infection135. As might be expected for the type 1 interferon pathway, timing, location and context are likely to be key in determining outcome136.
Future directions
Different autoimmune diseases are highly distinct in their presentation, with unique tissue-specific features: for example, bone erosion in RA, renal pathology in SLE and metabolic abnormalities in T1D. Given the striking differences in disease processes and clinical presentation, it is remarkable that increases in cTFH cells appear to be a unifying theme across a large number of autoimmune diseases. In this article, I highlight that CTLA4, IL-2 and Treg cells are key modulators of TFH cell differentiation and are also major players in the regulation of autoimmunity. This fundamental connection may go some way to explaining why dysregulated TFH cell homeostasis is a feature of so many different autoimmune diseases. Reinforcing this connection, several other TFH cell-associated genes (including CXCR5, CCR7, ICOSL, PD1, IL4R, IL21R and CD40) are linked to autoimmune disease susceptibility. The notion that genetic predisposition to autoimmunity may be coupled to genetic predisposition to TFH cell formation provides a new perspective on the cTFH cell changes widely reported in autoimmune settings.
As infection can lead to TFH cell differentiation, it is conceivable that infectious triggers occurring on autoimmune-susceptible backgrounds may cause discernible changes to TFH cell populations that precede autoimmunity. Thus, TFH cells may represent the consummate biomarker in autoimmunity, neatly integrating genetic and environmental risk. Accordingly, TFH cell profiling may be increasingly important in the prediction of autoimmune disease development and in monitoring and predicting clinical response to immunotherapies38.
The precise contribution of TFH cells, and their circulating counterparts, to pathology likely differs between autoimmune diseases. Dysregulated TFH cell homeostasis may allow the production of autoantibodies that mediate diverse effector functions — for example, enhancing cross-presentation of islet antigens in T1D137, driving renal pathology in SLE138, and promoting osteoclastogenesis and bone loss in RA139,140. As well as acting on B cells, the capacity for TFH cells to produce IL-21 and CXCL13 (ref.8) may influence CD8+ T cell activation and ectopic lymphoid structure formation, respectively, whereas dysregulated IFNγ production by TFH cells141 has been shown to drive autoimmune GCs and systemic autoimmune disease142.
Altogether, closer study of TFH cell populations in blood, lymphoid organs and tissues promises to yield new insight into autoimmune pathogenesis as well as allowing us to harness the full biomarker potential of this population.
Acknowledgements
I am grateful to M. A. Linterman, P. Tolar, N. M. Edner, C. J. Wang and L. Petersone for valuable feedback on the manuscript draft and for assistance with the figures. I am supported by a Medical Research Council Programme Grant and a Wellcome Trust Investigator Award.
Peer review
Peer review information
Nature Reviews Immunology thanks the anonymous reviewers for their contribution to the peer review of this work.
Competing interests
The author is an inventor on a patent relating to TFH cell profiles and predicting response to costimulation blockade in autoimmunity.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
GWAS Catalogue: https://www.ebi.ac.uk/gwas
References
- 1.Victora GD, Nussenzweig MC. Germinal centers. Annu. Rev. Immunol. 2012;30:429–457. doi: 10.1146/annurev-immunol-020711-075032. [DOI] [PubMed] [Google Scholar]
- 2.Vinuesa CG, Linterman MA, Yu D, MacLennan IC. Follicular helper T cells. Annu. Rev. Immunol. 2016;34:335–368. doi: 10.1146/annurev-immunol-041015-055605. [DOI] [PubMed] [Google Scholar]
- 3.Ueno H, Banchereau J, Vinuesa CG. Pathophysiology of T follicular helper cells in humans and mice. Nat. Immunol. 2015;16:142–152. doi: 10.1038/ni.3054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vinuesa CG, et al. A RING-type ubiquitin ligase family member required to repress follicular helper T cells and autoimmunity. Nature. 2005;435:452–458. doi: 10.1038/nature03555. [DOI] [PubMed] [Google Scholar]
- 5.Qi H, Cannons JL, Klauschen F, Schwartzberg PL, Germain RN. SAP-controlled T-B cell interactions underlie germinal centre formation. Nature. 2008;455:764–769. doi: 10.1038/nature07345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Linterman MA, et al. Follicular helper T cells are required for systemic autoimmunity. J. Exp. Med. 2009;206:561–576. doi: 10.1084/jem.20081886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simpson N, et al. Expansion of circulating T cells resembling follicular helper T cells is a fixed phenotype that identifies a subset of severe systemic lupus erythematosus. Arthritis Rheum. 2010;62:234–244. doi: 10.1002/art.25032. [DOI] [PubMed] [Google Scholar]
- 8.Ueno H. T follicular helper cells in human autoimmunity. Curr. Opin. Immunol. 2016;43:24–31. doi: 10.1016/j.coi.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 9.Morita R, et al. Human blood CXCR5+CD4+ T cells are counterparts of T follicular cells and contain specific subsets that differentially support antibody secretion. Immunity. 2011;34:108–121. doi: 10.1016/j.immuni.2010.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weber JP, Fuhrmann F, Hutloff A. T-follicular helper cells survive as long-term memory cells. Eur. J. Immunol. 2012;42:1981–1988. doi: 10.1002/eji.201242540. [DOI] [PubMed] [Google Scholar]
- 11.Choi YS, et al. Bcl6 expressing follicular helper CD4 T cells are fate committed early and have the capacity to form memory. J. Immunol. 2013;190:4014–4026. doi: 10.4049/jimmunol.1202963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hale JS, et al. Distinct memory CD4+ T cells with commitment to T follicular helper- and T helper 1-cell lineages are generated after acute viral infection. Immunity. 2013;38:805–817. doi: 10.1016/j.immuni.2013.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Locci M, et al. Human circulating PD-1+CXCR3-CXCR5+ memory Tfh cells are highly functional and correlate with broadly neutralizing HIV antibody responses. Immunity. 2013;39:758–769. doi: 10.1016/j.immuni.2013.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schmitt N, Bentebibel SE, Ueno H. Phenotype and functions of memory Tfh cells in human blood. Trends Immunol. 2014;35:436–442. doi: 10.1016/j.it.2014.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bossaller L, et al. ICOS deficiency is associated with a severe reduction of CXCR5+CD4 germinal center Th cells. J. Immunol. 2006;177:4927–4932. doi: 10.4049/jimmunol.177.7.4927. [DOI] [PubMed] [Google Scholar]
- 16.Ma CS, et al. Monogenic mutations differentially affect the quantity and quality of T follicular helper cells in patients with human primary immunodeficiencies. J. Allergy Clin. Immunol. 2015;136:993–1006.e1. doi: 10.1016/j.jaci.2015.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kitano M, et al. Bcl6 protein expression shapes pre-germinal center B cell dynamics and follicular helper T cell heterogeneity. Immunity. 2011;34:961–972. doi: 10.1016/j.immuni.2011.03.025. [DOI] [PubMed] [Google Scholar]
- 18.Sage PT, Alvarez D, Godec J, von Andrian UH, Sharpe AH. Circulating T follicular regulatory and helper cells have memory-like properties. J. Clin. Invest. 2014;124:5191–5204. doi: 10.1172/JCI76861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Asrir A, Aloulou M, Gador M, Perals C, Fazilleau N. Interconnected subsets of memory follicular helper T cells have different effector functions. Nat. Commun. 2017;8:847. doi: 10.1038/s41467-017-00843-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baumjohann D, et al. Persistent antigen and germinal center B cells sustain T follicular helper cell responses and phenotype. Immunity. 2013;38:596–605. doi: 10.1016/j.immuni.2012.11.020. [DOI] [PubMed] [Google Scholar]
- 21.Shulman Z, et al. T follicular helper cell dynamics in germinal centers. Science. 2013;341:673–677. doi: 10.1126/science.1241680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.He J, et al. Circulating precursor CCR7loPD-1hi CXCR5+ CD4+ T cells indicate Tfh cell activity and promote antibody responses upon antigen reexposure. Immunity. 2013;39:770–781. doi: 10.1016/j.immuni.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 23.Wong MT, et al. Mapping the diversity of follicular helper T cells in human blood and tonsils using high-dimensional mass cytometry analysis. Cell Rep. 2015;11:1822–1833. doi: 10.1016/j.celrep.2015.05.022. [DOI] [PubMed] [Google Scholar]
- 24.Heit A, et al. Vaccination establishes clonal relatives of germinal center T cells in the blood of humans. J. Exp. Med. 2017;214:2139–2152. doi: 10.1084/jem.20161794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hill DL, et al. The adjuvant GLA-SE promotes human Tfh cell expansion and emergence of public TCRbeta clonotypes. J. Exp. Med. 2019;216:1857–1873. doi: 10.1084/jem.20190301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vella LA, et al. T follicular helper cells in human efferent lymph retain lymphoid characteristics. J. Clin. Invest. 2019;129:3185–3200. doi: 10.1172/JCI125628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huber JE, et al. Fingolimod profoundly reduces frequencies and alters subset composition of circulating T follicular helper cells in multiple sclerosis patients. J. Immunol. 2020;204:1101–1110. doi: 10.4049/jimmunol.1900955. [DOI] [PubMed] [Google Scholar]
- 28.Wardemann H, et al. Predominant autoantibody production by early human B cell precursors. Science. 2003;301:1374–1377. doi: 10.1126/science.1086907. [DOI] [PubMed] [Google Scholar]
- 29.Wang CJ, et al. CTLA-4 controls follicular helper T-cell differentiation by regulating the strength of CD28 engagement. Proc. Natl Acad. Sci. USA. 2015;112:524–529. doi: 10.1073/pnas.1414576112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferguson SE, Han S, Kelsoe G, Thompson CB. CD28 is required for germinal center formation. J. Immunol. 1996;156:4576–4581. [PubMed] [Google Scholar]
- 31.Walker LS, et al. Compromised OX40 function in CD28-deficient mice is linked with failure to develop CXCR5-positive CD4 cells and germinal centers. J. Exp. Med. 1999;190:1115–1122. doi: 10.1084/jem.190.8.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rolf J, et al. Phosphoinositide 3-kinase activity in T cells regulates the magnitude of the germinal center reaction. J. Immunol. 2010;185:4042–4052. doi: 10.4049/jimmunol.1001730. [DOI] [PubMed] [Google Scholar]
- 33.Baumjohann D, et al. The microRNA cluster miR-17 approximately 92 promotes TFH cell differentiation and represses subset-inappropriate gene expression. Nat. Immunol. 2013;14:840–848. doi: 10.1038/ni.2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alroqi FJ, et al. Exaggerated follicular helper T-cell responses in patients with LRBA deficiency caused by failure of CTLA4-mediated regulation. J. Allergy Clin. Immunol. 2018;141:1050–1059.e10. doi: 10.1016/j.jaci.2017.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Verstappen GM, et al. Attenuation of follicular helper T cell-dependent B cell hyperactivity by abatacept treatment in primary Sjogren’s syndrome. Arthritis Rheumatol. 2017;69:1850–1861. doi: 10.1002/art.40165. [DOI] [PubMed] [Google Scholar]
- 36.Piantoni S, Regola F, Scarsi M, Tincani A, Airo P. Circulating follicular helper T cells (CD4+CXCR5+ICOS+) decrease in patients with rheumatoid arthritis treated with abatacept. Clin. Exp. Rheumatol. 2018;36:685. [PubMed] [Google Scholar]
- 37.Glatigny S, et al. Abatacept targets T follicular helper and regulatory T cells, disrupting molecular pathways that regulate their proliferation and maintenance. J. Immunol. 2019;202:1373–1382. doi: 10.4049/jimmunol.1801425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Edner NM, et al. Follicular helper T cell profiles predict response to costimulation blockade in type 1 diabetes. Nat. Immunol. 2020;21:1244–1255. doi: 10.1038/s41590-020-0744-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tivol EA, et al. Loss of CTLA-4 leads to massive lymphoproliferation and fatal multiorgan tissue destruction, revealing a critical negative regulatory role of CTLA-4. Immunity. 1995;3:541–547. doi: 10.1016/1074-7613(95)90125-6. [DOI] [PubMed] [Google Scholar]
- 40.Waterhouse P, et al. Lymphoproliferative disorders with early lethality in mice deficient in Ctla-4. Science. 1995;270:985–988. doi: 10.1126/science.270.5238.985. [DOI] [PubMed] [Google Scholar]
- 41.Schubert D, et al. Autosomal dominant immune dysregulation syndrome in humans with CTLA4 mutations. Nat. Med. 2014;20:1410–1416. doi: 10.1038/nm.3746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kuehn HS, et al. Immune dysregulation in human subjects with heterozygous germline mutations in CTLA4. Science. 2014;345:1623–1627. doi: 10.1126/science.1255904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lo B, et al. Patients with LRBA deficiency show CTLA4 loss and immune dysregulation responsive to abatacept therapy. Science. 2015;349:436–440. doi: 10.1126/science.aaa1663. [DOI] [PubMed] [Google Scholar]
- 44.Chung Y, et al. Follicular regulatory T cells expressing Foxp3 and Bcl-6 suppress germinal center reactions. Nat. Med. 2011;17:983–988. doi: 10.1038/nm.2426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wing JB, Ise W, Kurosaki T, Sakaguchi S. Regulatory T cells control antigen-specific expansion of Tfh cell number and humoral immune responses via the coreceptor CTLA-4. Immunity. 2014;41:1013–1025. doi: 10.1016/j.immuni.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 46.Linterman MA, et al. Foxp3+ follicular regulatory T cells control the germinal center response. Nat. Med. 2011;17:975–982. doi: 10.1038/nm.2425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kinnunen T, et al. Accumulation of peripheral autoreactive B cells in the absence of functional human regulatory T cells. Blood. 2013;121:1595–1603. doi: 10.1182/blood-2012-09-457465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sage PT, Paterson AM, Lovitch SB, Sharpe AH. The coinhibitory receptor CTLA-4 controls B cell responses by modulating T follicular helper, T follicular regulatory, and T regulatory cells. Immunity. 2014;41:1026–1039. doi: 10.1016/j.immuni.2014.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wollenberg I, et al. Regulation of the germinal center reaction by Foxp3+ follicular regulatory T cells. J. Immunol. 2011;187:4553–4560. doi: 10.4049/jimmunol.1101328. [DOI] [PubMed] [Google Scholar]
- 50.Botta D, et al. Dynamic regulation of T follicular regulatory cell responses by interleukin 2 during influenza infection. Nat. Immunol. 2017;18:1249–1260. doi: 10.1038/ni.3837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ritvo PG, et al. Tfr cells lack IL-2Ralpha but express decoy IL-1R2 and IL-1Ra and suppress the IL-1-dependent activation of Tfh cells. Sci. Immunol. 2017;2:eaan0368. doi: 10.1126/sciimmunol.aan0368. [DOI] [PubMed] [Google Scholar]
- 52.Fu W, et al. Deficiency in T follicular regulatory cells promotes autoimmunity. J. Exp. Med. 2018;215:815–825. doi: 10.1084/jem.20170901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Clement RL, et al. Follicular regulatory T cells control humoral and allergic immunity by restraining early B cell responses. Nat. Immunol. 2019;20:1360–1371. doi: 10.1038/s41590-019-0472-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lu Y, et al. CD4+ follicular regulatory T cells optimize the influenza virus-specific B cell response. J. Exp. Med. 2021;218:e20200547. doi: 10.1084/jem.20200547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wing JB, Tekguc M, Sakaguchi S. Control of germinal center responses by T-follicular regulatory cells. Front. Immunol. 2018;9:1910. doi: 10.3389/fimmu.2018.01910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Deng J, Wei Y, Fonseca VR, Graca L, Yu D. T follicular helper cells and T follicular regulatory cells in rheumatic diseases. Nat. Rev. Rheumatol. 2019;15:475–490. doi: 10.1038/s41584-019-0254-2. [DOI] [PubMed] [Google Scholar]
- 57.Gonzalez-Figueroa P, et al. Follicular regulatory T cells produce neuritin to regulate B cells. Cell. 2021;184:1775–1789.e19. doi: 10.1016/j.cell.2021.02.027. [DOI] [PubMed] [Google Scholar]
- 58.Wu H, et al. Follicular regulatory T cells repress cytokine production by follicular helper T cells and optimize IgG responses in mice. Eur. J. Immunol. 2016;46:1152–1161. doi: 10.1002/eji.201546094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sage PT, et al. Suppression by TFR cells leads to durable and selective inhibition of B cell effector function. Nat. Immunol. 2016;17:1436–1446. doi: 10.1038/ni.3578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jacobsen JT, et al. Expression of Foxp3 by T follicular helper cells in end-stage germinal centers. Science. 2021;373:eabe5146. doi: 10.1126/science.abe5146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wing JB, et al. A distinct subpopulation of CD25(-) T-follicular regulatory cells localizes in the germinal centers. Proc. Natl Acad. Sci. USA. 2017;114:E6400–E6409. doi: 10.1073/pnas.1705551114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ohkura N, et al. Regulatory T cell-specific epigenomic region variants are a key determinant of susceptibility to common autoimmune diseases. Immunity. 2020;52:1119–1132.e4. doi: 10.1016/j.immuni.2020.04.006. [DOI] [PubMed] [Google Scholar]
- 63.Brunkow ME, et al. Disruption of a new forkhead/winged-helix protein, scurfin, results in the fatal lymphoproliferative disorder of the scurfy mouse. Nat. Genet. 2001;27:68–73. doi: 10.1038/83784. [DOI] [PubMed] [Google Scholar]
- 64.Wildin RS, Smyk-Pearson S, Filipovich AH. Clinical and molecular features of the immunodysregulation, polyendocrinopathy, enteropathy, X linked (IPEX) syndrome. J. Med. Genet. 2002;39:537–545. doi: 10.1136/jmg.39.8.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Salomon B, et al. B7/CD28 costimulation is essential for the homeostasis of the CD4+CD25+ immunoregulatory T cells that control autoimmune diabetes. Immunity. 2000;12:431–440. doi: 10.1016/S1074-7613(00)80195-8. [DOI] [PubMed] [Google Scholar]
- 66.Beziat V, et al. Humans with inherited T cell CD28 deficiency are susceptible to skin papillomaviruses but are otherwise healthy. Cell. 2021;184:3812–3828. doi: 10.1016/j.cell.2021.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ballesteros-Tato A, et al. Interleukin-2 inhibits germinal center formation by limiting T follicular helper cell differentiation. Immunity. 2012;36:847–856. doi: 10.1016/j.immuni.2012.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ward NC, et al. Persistent IL-2 receptor signaling by IL-2/CD25 fusion protein controls diabetes in NOD mice by multiple mechanisms. Diabetes. 2020;69:2400–2413. doi: 10.2337/db20-0186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Locci M, et al. Activin A programs the differentiation of human TFH cells. Nat. Immunol. 2016;17:976–984. doi: 10.1038/ni.3494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.He J, et al. Low-dose interleukin-2 treatment selectively modulates CD4+ T cell subsets in patients with systemic lupus erythematosus. Nat. Med. 2016;22:991–993. doi: 10.1038/nm.4148. [DOI] [PubMed] [Google Scholar]
- 71.Setoguchi R, Hori S, Takahashi T, Sakaguchi S. Homeostatic maintenance of natural Foxp3+ CD25+ CD4+ regulatory T cells by interleukin (IL)-2 and induction of autoimmune disease by IL-2 neutralization. J. Exp. Med. 2005;201:723–735. doi: 10.1084/jem.20041982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fontenot JD, Rasmussen JP, Gavin MA, Rudensky AY. A function for interleukin 2 in Foxp3-expressing regulatory T cells. Nat. Immunol. 2005;6:1142–1151. doi: 10.1038/ni1263. [DOI] [PubMed] [Google Scholar]
- 73.Webster KE, et al. In vivo expansion of T reg cells with IL-2-mAb complexes: induction of resistance to EAE and long-term acceptance of islet allografts without immunosuppression. J. Exp. Med. 2009;206:751–760. doi: 10.1084/jem.20082824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Choi YS, et al. ICOS receptor instructs T follicular helper cell versus effector cell differentiation via induction of the transcriptional repressor Bcl6. Immunity. 2011;34:932–946. doi: 10.1016/j.immuni.2011.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Pepper M, Pagan AJ, Igyarto BZ, Taylor JJ, Jenkins MK. Opposing signals from the Bcl6 transcription factor and the interleukin-2 receptor generate T helper 1 central and effector memory cells. Immunity. 2011;35:583–595. doi: 10.1016/j.immuni.2011.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Johnston RJ, Choi YS, Diamond JA, Yang JA, Crotty S. STAT5 is a potent negative regulator of TFH cell differentiation. J. Exp. Med. 2012;209:243–250. doi: 10.1084/jem.20111174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Nurieva RI, et al. STAT5 protein negatively regulates T follicular helper (Tfh) cell generation and function. J. Biol. Chem. 2012;287:11234–11239. doi: 10.1074/jbc.M111.324046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.DiToro D, et al. Differential IL-2 expression defines developmental fates of follicular versus nonfollicular helper T cells. Science. 2018;361:eaao2933. doi: 10.1126/science.aao2933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sabatos CA, et al. A synaptic basis for paracrine interleukin-2 signaling during homotypic T cell interaction. Immunity. 2008;29:238–248. doi: 10.1016/j.immuni.2008.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Marshall HD, et al. The transforming growth factor beta signaling pathway is critical for the formation of CD4 T follicular helper cells and isotype-switched antibody responses in the lung mucosa. eLife. 2015;4:e04851. doi: 10.7554/eLife.04851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Schmitt N, et al. The cytokine TGF-beta co-opts signaling via STAT3-STAT4 to promote the differentiation of human TFH cells. Nat. Immunol. 2014;15:856–865. doi: 10.1038/ni.2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Li J, Lu E, Yi T, Cyster JG. EBI2 augments Tfh cell fate by promoting interaction with IL-2-quenching dendritic cells. Nature. 2016;533:110–114. doi: 10.1038/nature17947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Papillion A, et al. Inhibition of IL-2 responsiveness by IL-6 is required for the generation of GC-TFH cells. Sci. Immunol. 2019;4:eaaw7636. doi: 10.1126/sciimmunol.aaw7636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Oestreich KJ, Mohn SE, Weinmann AS. Molecular mechanisms that control the expression and activity of Bcl-6 in TH1 cells to regulate flexibility with a TFH-like gene profile. Nat. Immunol. 2012;13:405–411. doi: 10.1038/ni.2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pandiyan P, Zheng L, Ishihara S, Reed J, Lenardo MJ. CD4+CD25+Foxp3+ regulatory T cells induce cytokine deprivation-mediated apoptosis of effector CD4+ T cells. Nat. Immunol. 2007;8:1353–1362. doi: 10.1038/ni1536. [DOI] [PubMed] [Google Scholar]
- 86.Chinen T, et al. An essential role for the IL-2 receptor in Treg cell function. Nat. Immunol. 2016;17:1322–1333. doi: 10.1038/ni.3540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lowe CE, et al. Large-scale genetic fine mapping and genotype-phenotype associations implicate polymorphism in the IL2RA region in type 1 diabetes. Nat. Genet. 2007;39:1074–1082. doi: 10.1038/ng2102. [DOI] [PubMed] [Google Scholar]
- 88.Wiede F, et al. T-cell-specific PTPN2 deficiency in NOD mice accelerates the development of type 1 diabetes and autoimmune comorbidities. Diabetes. 2019;68:1251–1266. doi: 10.2337/db18-1362. [DOI] [PubMed] [Google Scholar]
- 89.Cerosaletti K, et al. Multiple autoimmune-associated variants confer decreased IL-2R signaling in CD4+ CD25hi T cells of type 1 diabetic and multiple sclerosis patients. PLoS One. 2013;8:e83811. doi: 10.1371/journal.pone.0083811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sadlack B, et al. Ulcerative colitis-like disease in mice with a disrupted interleukin-2 gene. Cell. 1993;75:253–261. doi: 10.1016/0092-8674(93)80067-O. [DOI] [PubMed] [Google Scholar]
- 91.Suzuki H, et al. Deregulated T cell activation and autoimmunity in mice lacking interleukin-2 receptor beta. Science. 1995;268:1472–1476. doi: 10.1126/science.7770771. [DOI] [PubMed] [Google Scholar]
- 92.Willerford DM, et al. Interleukin-2 receptor alpha chain regulates the size and content of the peripheral lymphoid compartment. Immunity. 1995;3:521–530. doi: 10.1016/1074-7613(95)90180-9. [DOI] [PubMed] [Google Scholar]
- 93.Zhang Z, et al. Human interleukin-2 receptor beta mutations associated with defects in immunity and peripheral tolerance. J. Exp. Med. 2019;216:1311–1327. doi: 10.1084/jem.20182304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Dendrou CA, et al. Cell-specific protein phenotypes for the autoimmune locus IL2RA using a genotype-selectable human bioresource. Nat. Genet. 2009;41:1011–1015. doi: 10.1038/ng.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Rosenzwajg M, et al. Immunological and clinical effects of low-dose interleukin-2 across 11 autoimmune diseases in a single, open clinical trial. Ann. Rheum. Dis. 2019;78:209–217. doi: 10.1136/annrheumdis-2018-214229. [DOI] [PubMed] [Google Scholar]
- 96.Farh KK, et al. Genetic and epigenetic fine mapping of causal autoimmune disease variants. Nature. 2015;518:337–343. doi: 10.1038/nature13835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Cotsapas C, et al. Pervasive sharing of genetic effects in autoimmune disease. PLoS Genet. 2011;7:e1002254. doi: 10.1371/journal.pgen.1002254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Crotty S. T follicular helper cell biology: a decade of discovery and diseases. Immunity. 2019;50:1132–1148. doi: 10.1016/j.immuni.2019.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bentebibel SE, et al. Induction of ICOS+CXCR3+CXCR5+ TH cells correlates with antibody responses to influenza vaccination. Sci. Transl. Med. 2013;5:176ra132. doi: 10.1126/scitranslmed.3005191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Qiu CC, Caricchio R, Gallucci S. Triggers of autoimmunity: the role of bacterial infections in the extracellular exposure of lupus nuclear autoantigens. Front. Immunol. 2019;10:2608. doi: 10.3389/fimmu.2019.02608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Van Ghelue M, Moens U, Bendiksen S, Rekvig OP. Autoimmunity to nucleosomes related to viral infection: a focus on hapten-carrier complex formation. J. Autoimmun. 2003;20:171–182. doi: 10.1016/S0896-8411(02)00110-5. [DOI] [PubMed] [Google Scholar]
- 102.Rodriguez-Calvo T. Enteroviral infections as a trigger for type 1 diabetes. Curr. Diab Rep. 2018;18:106. doi: 10.1007/s11892-018-1077-2. [DOI] [PubMed] [Google Scholar]
- 103.Konig MF, et al. Aggregatibacter actinomycetemcomitans-induced hypercitrullination links periodontal infection to autoimmunity in rheumatoid arthritis. Sci. Transl. Med. 2016;8:369ra176. doi: 10.1126/scitranslmed.aaj1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Steelman AJ. Infection as an environmental trigger of multiple sclerosis disease exacerbation. Front. Immunol. 2015;6:520. doi: 10.3389/fimmu.2015.00520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lochhead RB, Strle K, Arvikar SL, Weis JJ, Steere AC. Lyme arthritis: linking infection, inflammation and autoimmunity. Nat. Rev. Rheumatol. 2021;17:449–461. doi: 10.1038/s41584-021-00648-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wang K, et al. Association between enterovirus infection and type 1 diabetes risk: a meta-analysis of 38 case-control studies. Front. Endocrinol. 2021;12:706964. doi: 10.3389/fendo.2021.706964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Richardson SJ, Leete P, Bone AJ, Foulis AK, Morgan NG. Expression of the enteroviral capsid protein VP1 in the islet cells of patients with type 1 diabetes is associated with induction of protein kinase R and downregulation of Mcl-1. Diabetologia. 2013;56:185–193. doi: 10.1007/s00125-012-2745-4. [DOI] [PubMed] [Google Scholar]
- 108.Apaolaza PS, et al. Islet expression of type I interferon response sensors is associated with immune infiltration and viral infection in type 1 diabetes. Sci. Adv. 2021;7:eabd6527. doi: 10.1126/sciadv.abd6527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bjornevik K, et al. Longitudinal analysis reveals high prevalence of Epstein-Barr virus associated with multiple sclerosis. Science. 2022;375:296–301. doi: 10.1126/science.abj8222. [DOI] [PubMed] [Google Scholar]
- 110.Lanz TV, et al. Clonally expanded B cells in multiple sclerosis bind EBV EBNA1 and GlialCAM. Nature. 2022 doi: 10.1038/s41586-022-04432-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Greczmiel U, et al. Sustained T follicular helper cell response is essential for control of chronic viral infection. Sci. Immunol. 2017;2:eaam8686. doi: 10.1126/sciimmunol.aam8686. [DOI] [PubMed] [Google Scholar]
- 112.Fahey LM, et al. Viral persistence redirects CD4 T cell differentiation toward T follicular helper cells. J. Exp. Med. 2011;208:987–999. doi: 10.1084/jem.20101773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Hunziker L, et al. Hypergammaglobulinemia and autoantibody induction mechanisms in viral infections. Nat. Immunol. 2003;4:343–349. doi: 10.1038/ni911. [DOI] [PubMed] [Google Scholar]
- 114.Vehik K, et al. Prospective virome analyses in young children at increased genetic risk for type 1 diabetes. Nat. Med. 2019;25:1865–1872. doi: 10.1038/s41591-019-0667-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Sanderson NS, et al. Cocapture of cognate and bystander antigens can activate autoreactive B cells. Proc. Natl Acad. Sci. USA. 2017;114:734–739. doi: 10.1073/pnas.1614472114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wang EY, et al. Diverse functional autoantibodies in patients with COVID-19. Nature. 2021;595:283–288. doi: 10.1038/s41586-021-03631-y. [DOI] [PubMed] [Google Scholar]
- 117.Ovcinnikovs V, et al. CTLA-4-mediated transendocytosis of costimulatory molecules primarily targets migratory dendritic cells. Sci. Immunol. 2019;4:eaaw0902. doi: 10.1126/sciimmunol.aaw0902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Peluso I, et al. IL-21 counteracts the regulatory T cell-mediated suppression of human CD4+ T lymphocytes. J. Immunol. 2007;178:732–739. doi: 10.4049/jimmunol.178.2.732. [DOI] [PubMed] [Google Scholar]
- 119.Clough LE, et al. Release from regulatory T cell-mediated suppression during the onset of tissue-specific autoimmunity is associated with elevated IL-21. J. Immunol. 2008;180:5393–5401. doi: 10.4049/jimmunol.180.8.5393. [DOI] [PubMed] [Google Scholar]
- 120.Vogelzang A, et al. A fundamental role for interleukin-21 in the generation of T follicular helper cells. Immunity. 2008;29:127–137. doi: 10.1016/j.immuni.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 121.Spolski R, Leonard WJ. Interleukin-21: a double-edged sword with therapeutic potential. Nat. Rev. Drug Discov. 2014;13:379–395. doi: 10.1038/nrd4296. [DOI] [PubMed] [Google Scholar]
- 122.Kenefeck R, et al. Follicular helper T cell signature in type 1 diabetes. J. Clin. Invest. 2015;125:292–303. doi: 10.1172/JCI76238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ferreira RC, et al. IL-21 production by CD4 effector T cells and frequency of circulating follicular helper T cells are increased in type 1 diabetes patients. Diabetologia. 2015;58:781–790. doi: 10.1007/s00125-015-3509-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Schwickert TA, Alabyev B, Manser T, Nussenzweig MC. Germinal center reutilization by newly activated B cells. J. Exp. Med. 2009;206:2907–2914. doi: 10.1084/jem.20091225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Zhao Z, et al. Nature of T cell epitopes in lupus antigens and HLA-DR determines autoantibody initiation and diversification. Ann. Rheum. Dis. 2019;78:380–390. doi: 10.1136/annrheumdis-2018-214125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.McNab F, Mayer-Barber K, Sher A, Wack A, O’Garra A. Type I interferons in infectious disease. Nat. Rev. Immunol. 2015;15:87–103. doi: 10.1038/nri3787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bennett L, et al. Interferon and granulopoiesis signatures in systemic lupus erythematosus blood. J. Exp. Med. 2003;197:711–723. doi: 10.1084/jem.20021553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Hall JC, Rosen A. Type I interferons: crucial participants in disease amplification in autoimmunity. Nat. Rev. Rheumatol. 2010;6:40–49. doi: 10.1038/nrrheum.2009.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ferreira RC, et al. A type I interferon transcriptional signature precedes autoimmunity in children genetically at risk for type 1 diabetes. Diabetes. 2014;63:2538–2550. doi: 10.2337/db13-1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.van Baarsen LG, et al. A subtype of multiple sclerosis defined by an activated immune defense program. Genes. Immun. 2006;7:522–531. doi: 10.1038/sj.gene.6364324. [DOI] [PubMed] [Google Scholar]
- 131.Nakayamada S, et al. Type I IFN induces binding of STAT1 to Bcl6: divergent roles of STAT family transcription factors in the T follicular helper cell genetic program. J. Immunol. 2014;192:2156–2166. doi: 10.4049/jimmunol.1300675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Ray JP, et al. Transcription factor STAT3 and type I interferons are corepressive insulators for differentiation of follicular helper and T helper 1 cells. Immunity. 2014;40:367–377. doi: 10.1016/j.immuni.2014.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Cucak H, Yrlid U, Reizis B, Kalinke U, Johansson-Lindbom B. Type I interferon signaling in dendritic cells stimulates the development of lymph-node-resident T follicular helper cells. Immunity. 2009;31:491–501. doi: 10.1016/j.immuni.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 134.Stebegg M, et al. Rejuvenating conventional dendritic cells and T follicular helper cell formation after vaccination. eLife. 2020;9:e52473. doi: 10.7554/eLife.52473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Sebina I, et al. IFNAR1-signalling obstructs ICOS-mediated humoral immunity during non-lethal blood-stage plasmodium infection. PLoS Pathog. 2016;12:e1005999. doi: 10.1371/journal.ppat.1005999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.De Giovanni M, et al. Spatiotemporal regulation of type I interferon expression determines the antiviral polarization of CD4+ T cells. Nat. Immunol. 2020;21:321–330. doi: 10.1038/s41590-020-0596-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Harbers SO, et al. Antibody-enhanced cross-presentation of self antigen breaks T cell tolerance. J. Clin. Invest. 2007;117:1361–1369. doi: 10.1172/JCI29470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Suurmond J, Diamond B. Autoantibodies in systemic autoimmune diseases: specificity and pathogenicity. J. Clin. Invest. 2015;125:2194–2202. doi: 10.1172/JCI78084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Harre U, et al. Induction of osteoclastogenesis and bone loss by human autoantibodies against citrullinated vimentin. J. Clin. Invest. 2012;122:1791–1802. doi: 10.1172/JCI60975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Engdahl C, et al. Periarticular bone loss in arthritis is induced by autoantibodies against citrullinated vimentin. J. Bone Miner. Res. 2017;32:1681–1691. doi: 10.1002/jbmr.3158. [DOI] [PubMed] [Google Scholar]
- 141.Faliti CE, et al. P2X7 receptor restrains pathogenic Tfh cell generation in systemic lupus erythematosus. J. Exp. Med. 2019;216:317–336. doi: 10.1084/jem.20171976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Jackson SW, et al. B cell IFN-gamma receptor signaling promotes autoimmune germinal centers via cell-intrinsic induction of BCL-6. J. Exp. Med. 2016;213:733–750. doi: 10.1084/jem.20151724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Yu D, et al. The transcriptional repressor Bcl-6 directs T follicular helper cell lineage commitment. Immunity. 2009;31:457–468. doi: 10.1016/j.immuni.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 144.Johnston RJ, et al. Bcl6 and Blimp-1 are reciprocal and antagonistic regulators of T follicular helper cell differentiation. Science. 2009;325:1006–1010. doi: 10.1126/science.1175870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Nurieva RI, et al. Bcl6 mediates the development of T follicular helper cells. Science. 2009;325:1001–1005. doi: 10.1126/science.1176676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Choi J, et al. Bcl-6 is the nexus transcription factor of T follicular helper cells via repressor-of-repressor circuits. Nat. Immunol. 2020;21:777–789. doi: 10.1038/s41590-020-0706-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Bauquet AT, et al. The costimulatory molecule ICOS regulates the expression of c-Maf and IL-21 in the development of follicular T helper cells and TH-17 cells. Nat. Immunol. 2009;10:167–175. doi: 10.1038/ni.1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Betz BC, et al. Batf coordinates multiple aspects of B and T cell function required for normal antibody responses. J. Exp. Med. 2010;207:933–942. doi: 10.1084/jem.20091548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ise W, et al. The transcription factor BATF controls the global regulators of class-switch recombination in both B cells and T cells. Nat. Immunol. 2011;12:536–543. doi: 10.1038/ni.2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Liu X, et al. Transcription factor achaete-scute homologue 2 initiates follicular T-helper-cell development. Nature. 2014;507:513–518. doi: 10.1038/nature12910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Weber JP, et al. ICOS maintains the T follicular helper cell phenotype by down-regulating Kruppel-like factor 2. J. Exp. Med. 2015;212:217–233. doi: 10.1084/jem.20141432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Ma CS, et al. Functional STAT3 deficiency compromises the generation of human T follicular helper cells. Blood. 2012;119:3997–4008. doi: 10.1182/blood-2011-11-392985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Choi YS, Eto D, Yang JA, Lao C, Crotty S. Cutting edge: STAT1 is required for IL-6-mediated Bcl6 induction for early follicular helper cell differentiation. J. Immunol. 2013;190:3049–3053. doi: 10.4049/jimmunol.1203032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Okada T, et al. Antigen-engaged B cells undergo chemotaxis toward the T zone and form motile conjugates with helper T cells. PLoS Biol. 2005;3:e150. doi: 10.1371/journal.pbio.0030150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Schwickert TA, et al. A dynamic T cell-limited checkpoint regulates affinity-dependent B cell entry into the germinal center. J. Exp. Med. 2011;208:1243–1252. doi: 10.1084/jem.20102477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Bentebibel SE, Schmitt N, Banchereau J, Ueno H. Human tonsil B-cell lymphoma 6 (BCL6)-expressing CD4+ T-cell subset specialized for B-cell help outside germinal centers. Proc. Natl Acad. Sci. USA. 2011;108:E488–E497. doi: 10.1073/pnas.1100898108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Odegard JM, et al. ICOS-dependent extrafollicular helper T cells elicit IgG production via IL-21 in systemic autoimmunity. J. Exp. Med. 2008;205:2873–2886. doi: 10.1084/jem.20080840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Liu B, et al. Affinity-coupled CCL22 promotes positive selection in germinal centres. Nature. 2021;592:133–137. doi: 10.1038/s41586-021-03239-2. [DOI] [PubMed] [Google Scholar]
- 159.Dan JM, et al. A cytokine-independent approach to identify antigen-specific human germinal center T follicular helper cells and rare antigen-specific CD4+ T cells in blood. J. Immunol. 2016;197:983–993. doi: 10.4049/jimmunol.1600318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Collins AV, et al. The interaction properties of costimulatory molecules revisited. Immunity. 2002;17:201–210. doi: 10.1016/S1074-7613(02)00362-X. [DOI] [PubMed] [Google Scholar]
- 161.Qureshi OS, et al. Trans-endocytosis of CD80 and CD86: a molecular basis for the cell-extrinsic function of CTLA-4. Science. 2011;332:600–603. doi: 10.1126/science.1202947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Wing K, et al. CTLA-4 control over Foxp3+ regulatory T cell function. Science. 2008;322:271–275. doi: 10.1126/science.1160062. [DOI] [PubMed] [Google Scholar]
- 163.Mandelbrot DA, McAdam AJ, Sharpe AH. B7-1 or B7-2 is required to produce the lymphoproliferative phenotype in mice lacking cytotoxic T lymphocyte-associated antigen 4 (CTLA-4) J. Exp. Med. 1999;189:435–440. doi: 10.1084/jem.189.2.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Fonseca VR, et al. Human blood Tfr cells are indicators of ongoing humoral activity not fully licensed with suppressive function. Sci. Immunol. 2017;2:eaan148. doi: 10.1126/sciimmunol.aan1487. [DOI] [PMC free article] [PubMed] [Google Scholar]