Abstract
Objectives
Financial risk protection (FRP) is an indicator of the Sustainable Development Goal 3 universal health coverage (UHC) target. We sought to characterise what is known about FRP in the UHC context and to identify evidence gaps to prioritise in future research.
Design
Scoping overview of reviews using the Arksey & O’Malley and Levac & Colquhoun framework and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews reporting guidelines.
Data sources
MEDLINE, PsycINFO, CINAHL-Plus and PAIS Index were systematically searched for studies published between 1 January 1995 and 20 July 2021.
Eligibility criteria
Records were screened by two independent reviewers in duplicate using the following criteria: (1) literature review; (2) focus on UHC achievement through FRP; (3) English or French language; (4) published after 1995 and (5) peer-reviewed.
Data extraction and synthesis
Two reviewers extracted data using a standard form and descriptive content analysis was performed to synthesise findings.
Results
50 studies were included. Most studies were systematic reviews focusing on low-income and middle-income countries. Study periods spanned 1990 and 2020. While FRP was recognised as a dimension of UHC, it was rarely defined as a concept. Out-of-pocket, catastrophic and impoverishing health expenditures were most commonly used to measure FRP. Pooling arrangements, expansion of insurance coverage and financial incentives were the main interventions for achieving FRP. Evidence gaps pertained to the effectiveness, cost-effectiveness and equity implications of efforts aimed at increasing FRP. Methodological gaps related to trade-offs between single-country and multicountry analyses; lack of process evaluations; inadequate mixed-methods evidence, disaggregated by relevant characteristics; lack of comparable and standardised measurement and short follow-up periods.
Conclusions
This scoping overview of reviews characterised what is known about FRP as a UHC dimension and found evidence gaps related to the effectiveness, cost-effectiveness and equity implications of FRP interventions. Theory-informed mixed-methods research using high-quality, longitudinal and disaggregated data is needed to address these objectives.
Keywords: health policy, public health, international health services
Strengths and limitations of this study.
This is the first scoping overview of reviews synthesising the evidence gaps related to the conceptualisation of financial risk protection, interventions aimed at increasing financial risk protection, and outcomes used to measure financial risk protection in the context of universal health coverage.
This study was guided by a prospectively registered protocol and systematic searching and evidence review methods.
Study searches were limited by language (English and French) and publication year (1995–2021); however, the study periods of the individual included reviews ranged from 1990 to 2020.
In order to characterise the published evidence base, this research relied on academic peer-reviewed literature.
As recommended in scoping review guidelines, we relied on the interpretations of the authors of the included reviews, rather than impose our own meanings.
Introduction
At the 58th World Health Assembly in 2005, Member States committed to transitioning to universal coverage to guarantee access to necessary health services to the entire population, while protecting against financial risk (WHA58.33).1 This objective was reaffirmed in the 2015 ratification of the United Nations 2030 Agenda for Sustainable Development, which outlined 17 Sustainable Development Goals (SDGs) and 169 targets that aim to provide ‘peace and prosperity for people and the planet’.2 Specifically, SDG 3 called on Member States to ensure healthy lives and promote well-being for all at all ages through the ‘achieve(ment) of universal health coverage (UHC), including financial risk protection (FRP), access to quality essential healthcare services and access to safe, effective, quality and affordable essential medicines and vaccines for all’ (target 3.8).2 The countries’ progress towards the UHC target through FRP is monitored using indicators 3.8.1 (coverage of essential health services among the general and most disadvantaged populations) and 3.8.2 (proportion of population with large household expenditures on health as a share of total household expenditure or income).2
The WHO 13th General Programme of Work (GPW13), which provides a framework for measuring progress towards the health-related SDG targets, specified a goal of one billion more people benefiting from UHC by the year 2023.3 However, despite notable progress towards UHC over the past 30 years, nearly 90 million people are pushed into extreme poverty due to healthcare expenditures each year,4 and only an estimated 389 million additional people will benefit from UHC by 2023, significantly undershooting the GPW13 target.5 While nearly all countries impose direct user payments for health services, this form of healthcare financing is especially predominant in low-income and middle-income countries (LMIC),6 7 and is more prohibitive to populations rendered socially and economically marginalised by systemic barriers in both LMIC and high-income countries (HIC).6 Indirect payments related to transportation and lost wages further increase the risk of financial catastrophe and exacerbate inequities.6
Bibliometric analyses suggest that the release of SDGs has stimulated considerable scholarly research on UHC, with nearly half of the studies published after 2015.8 Nonetheless, substantial debate remains on the conceptualisation of FRP as a dimension of UHC, the established metrics for measuring FRP and its absence, and the mechanisms for achieving UHC through FRP.9–12 These ambiguities complicate the decision-makers’ ability to translate UHC from an aspirational objective into practical public policy.11
Identifying research priorities through evidence synthesis is an important function of health policy and systems research that ensures alignment between evidence needs, research funding and research efforts.13–16 While some recent studies have outlined priority research gaps related to SDGs implementation,17 18 no studies have focused on research priorities related to the achievement of UHC through FRP. In this study, we performed a scoping overview of reviews (1) to synthesise the existing knowledge on FRP in the UHC context and (2) to identify evidence gaps to prioritise in future research on UHC.
Methods
Study design and rationale
Since there is no single accepted methodology for identifying evidence gaps,15 our approach requires some justification. Overviews of literature reviews (‘overviews’), where secondary studies are the unit of analysis, have been described as the preferred review methodology when the evidence base is vast and when policy-makers or decision-makers are the intended knowledge users.19 20 As identifying inconsistent or insufficient evidence is already implicit in syntheses of primary studies,15 21 overviews are able to summarise this information as evidence gaps that are generalisable and applicable in future research.19 20 Although standardised recommendations for the conduct of overviews are not available, existing review methodologies for primary studies can be adapted.19 20 22 Scoping review methodologies are better suited to exploratory and descriptive objectives, such as mapping of the evidence and identification of key concepts, while systematic review methodologies have more narrow objectives that are explanatory or analytical in nature.23 Consequently, scoping overviews of the academic literature have been frequently used for global health services and systems research agenda-setting.14 17 18 24
In conducting this scoping overview, we used the five-step scoping review methodological framework by Arksey & O’Malley and Levac & Colquhoun.25–27 We adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews reporting guidelines23 28 and were guided by a research protocol published prospectively on Open Science Framework.29
Information sources and search strategy
The search strategy (see online supplemental file 1) was developed in consultation with a public health information specialist. We searched MEDLINE (Ovid), APA PsycINFO (Ovid), CINAHL-Plus (EBSCO) and PAIS Index (ProQuest) for English and French-language sources published between 1 January 1995 and 20 July 2021. This date cut-off was chosen because >97% of the literature on UHC was published after 1995,8 likely due to the adoption of the Millennium Development Goals (MDGs) in 2000, in which MDGs 1 and 4–7 expressed a need for universal access to treatment for select health issues.30 We used pretested search filters to identify review articles.31 The search terms included controlled vocabulary and keywords for the concepts of (1) UHC, (2) FRP and (3) equity or impoverishment.32 We used a broad set of synonyms for each concept, as, for example, UHC-related terms have evolved over time and usage has varied between HIC (‘universal healthcare’) and LMIC (‘UHC’).10 12 To capture possible variation in FRP definitions, search concepts were combined using the following logic: (UHC AND FRP) OR (UHC AND equity). The bibliographic searches were supplemented by a review of forward and backward citations.33
bmjopen-2021-052041supp001.pdf (104.4KB, pdf)
Study selection process
Search strategies were imported into a web-based systematic review management software, Covidence (www.covidence.org), to remove duplicate citations and perform citation screening against the predefined selection criteria (described in detail in online supplemental file 2). Studies were eligible if they (1) employed a literature review methodology (where an explicit methodology section was provided to confirm that a literature review was undertaken); (2) focused on the achievement of UHC through FRP; (3) were written in English or French; (4) were published after 1995; (5) were an original peer-reviewed published work and (6) could be retrieved through the University of Toronto library. The selection criteria were first piloted on a sample of 100 citations by two independent reviewers (DB and SM). Citations were then screened in full by the two independent reviewers in two phases: (1) titles and abstracts and (2) full-text articles. The average Cohen’s kappa was calculated to be 0.5, reflecting fair inter-rater agreement.34 Conflicting votes at both screening phases were resolved through discussion with the research team.
Data extraction and synthesis
The data were extracted verbatim from the included articles. A data charting template was first piloted by two independent reviewers (DB and SM) on a random selection of 15 articles and discrepancies were discussed with the other coauthors. Data extraction on the remaining set of articles was divided between the two reviewers. Data items included publication information; study methodology; study objectives; descriptive characteristics; definitions of FRP (concepts, measurements and interventions); and evidence gaps. By ‘FRP interventions’, we broadly mean the implementation of policies, programmes, reforms and mechanisms aimed at reducing health-related financial burden among health system users. Evidence gaps were defined as research findings or propositions identified as insufficient and meriting further study by the research community (ie, authors of the included studies).15 Evidence gaps were retrieved from the results, discussion, and limitations sections of the included articles.
To address the first objective, we summarised what is currently known in the literature about FRP, including its conceptualisation, measurement and implementation as an intervention. To address the second objective, we performed a descriptive content analysis of the extracted data to describe and summarise the evidence gaps identified by the research community, classified as gaps related to the evidence base and to methodology. Similar to the approaches taken by other studies on research priority-setting in global health,17 18 24 this information was framed more broadly to enable applicability to multiple contexts and research topics. Descriptive approaches to content analysis involve staying close to the data; consequently, this synthesis is more summative than interpretive, compared with other meta-aggregative approaches (eg, grounded theory or meta-ethnography).35 36 Descriptive synthesis is recommended for scoping reviews, as scoping reviews seek to describe the state of the literature.23
Patient and public involvement
No patients or members of the public were involved in this study.
Results
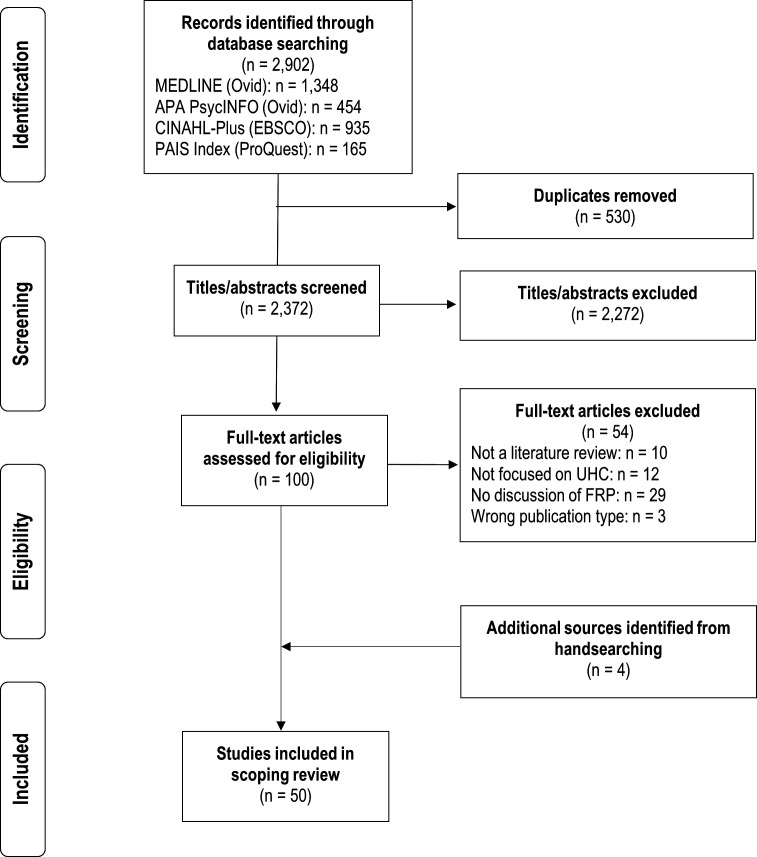
Following the review of 2902 records and handsearching, 50 peer-reviewed articles were included (figure 1), with their characteristics presented in tables 1 and 2. Publication years ranged from 2010 to 2021, with most papers (n=39, 78%) published between 2015 and 2021 and study periods covering 1990 and 2020. Most study designs were systematic reviews (n=34, 68%), followed by narrative reviews (n=4, 8%), and review-based comparative analyses (n=4, 8%). Among the geographical regions covered by the included reviews, 62% considered countries in the African region, 56% in the South-East Asian region, 54% Western-Pacific region, 44% in the Pan-American region, 24% in the European region, and 8% in the Eastern-Mediterranean region. Over half the studies (n=30, 60%) included two or more world regions. Nearly three-quarters (n=36, 72%) of the reviews focused on LMIC, one review (2%) focused on HIC, and 12 (24%) considered both LMIC and HIC. Fifteen studies (30%) focused on FRP in specific populations, including women and children, low-income groups, individuals with multimorbidity, those with mental health issues, and surgical, cancer and tuberculosis patients.
Figure 1.
Study selection flow chart.
Table 1.
Characteristics of the included studies
| Study | Study design | Resource level | Geographical regions | FRP defined? | FRP interventions | FRP measures | Number of studies | Number of databases | Study period |
| Acharya 201270 | SR | LMIC | AFR, EUR, PAR, SEAR, WPR | No | PA | CHE, OOPE | 24 | ten academic, 3 grey | ≤2010 |
| Adebayo 201575 | SR | LMIC | AFR, PAR, SEAR, WPR | No | EC | OOPE | 25 | 17 | 2003–2013 |
| Angell 201969 | SR, Delphi | HIC, LMIC | SEAR, WPR | No | PA | CHE, OOPE | 31 studies, 10 grey | three academic, 14 grey | 2008–2018 |
| Aragão 202180 | SR | LMIC | AFR, PAR, SEAR | No | EC, FI | NS | 9 | 5 | ≤2019 |
| Artignan 202147 | RR | LMIC | AFR | Yes | PA | NS | 16 | 3 | ≤2019 |
| Bazyar 202171 | CA | HIC, LMIC | EUR, SEAR, WPR | No | PA | NS | NS | three academic, 3 grey | ≤2020 |
| Bellows 201383 | NR | LMIC | AFR, EMR, EUR, WPR | No | FI | NS | 28 voucher programmes | NS | 1995–2011 |
| Bhanvadia 202148 | SR | HIC, LMIC | EUR, PAR, WPR | Yes | NS | OOPE | 23 | 5 | ≤2020 |
| Bright 201738 | SR | LMIC | AFR, PAR, SEAR, WPR | Yes | FI | NS | 57 | 4 | ≤2015 |
| Bucagu 201278 | SR | LMIC | AFR | No | EC | CHE | 14 | 1 | 2005–2011 |
| Christmals 202074 | ScR | LMIC | AFR | No | PA | NS | 77 | 5 | 2003–2018 |
| Comfort 201358 | SR | LMIC | AFR, EUR, PAR, SEAR, WPR | Yes | EC, FI | NS | 29 | NS | 1997–2012 |
| Docrat 202085 | SR | LMIC | AFR, PAR, SEAR, WPR | No | EC | OOPE | 18 | 9 | ≤2018 |
| Doshmangir 202049 | MA | LMIC | EMR | Yes | NS | CHE | 53 | 6 | ≤2019 |
| Erlangga 201965 | SR | LMIC | AFR, PAR, SEAR, WPR | No | EC | CHE, IHE, OOPE | 68 | five academic, 3 grey | 2010–2016 |
| Fadlallah 201841 | SR | LMIC | AFR, PAR, SEAR, EUR, WPR | Yes | EC | OOPE | 51 | 6 | 1992–2015 |
| Grainger 201484 | NR | LMIC | AFR, PAR, SEAR, WPR | No | FI | NS | 40 voucher programmes | NS | ≤2011 |
| Hunter 201782 | SR | LMIC | AFR, PAR, SEAR, WPR | No | FI | OOPE | 98 | 19 | 1990–2015 |
| Hussien 202150 | SR | LMIC | AFR, SEAR | Yes | PA | CHE, IHE, OOPE | 27 | three academic, 1 grey | 2005–2020 |
| Ifeagwu 202151 | SR | LMIC | AFR | Yes | PA | CHE, IHE, OOPE | 39 | 7 | 2005–2019 |
| Izzanie 201972 | SR | LMIC | SEAR, WPR | No | EC | CHE, IHE, OOPE | 13 | 4 | 1993–2017 |
| Koch 201745 | SR | LMIC | PAR | Yes | EC | CHE, IHE, OOPE | 16 | 3 | 2008–2015 |
| Lagomarsino 201246 | CA | LMIC | AFR, SEAR, WPR | Yes | EC, FI, PA | IHE, OOPE | NS | 3 | NS |
| Longo 202052 | SR | HIC, LMIC | EUR, PAR, WPR | Yes | NS | OOPE | 32 | 6 | 2005–2019 |
| Mathauer 201968 | CA | NS | NS | No | PA | OOPE | NS | 2 | NS |
| Meng 201181 | SR | HIC, LMIC | AFR, PAR, SEAR, WPR | No | EC | NS | 86 | 45 | 1995–2007 |
| Motaze 202153 | CR | HIC | PAR | Yes | PA | CHE, OOPE | 7 | seven academic, 9 grey | ≤2019 |
| Myint 201963 | SR | HIC, LMIC | SEAR, WPR | No | PA | CHE, OOPE | 77 | 2 | 2010–2017 |
| Njagi 201844 | ScR | LMIC | AFR | Yes | NS | CHE, IHE | 34 | 5 | 2006–2017 |
| Odeyemi 201476 | SR | LMIC | AFR | No | EC | CHE | 26 | 2 | 2003–2012 |
| Odeyemi 201364 | CA | LMIC | AFR | No | EC | OOPE | 16 | 3 | 2000–2012 |
| Odoch 202154 | ScR | HIC, LMIC | AFR, EMR, SEAR, WPR | Yes | PA, EC | CHE, IHE, OOPE | 12 | 5 | 2012–2020 |
| Okedo-Alex 201961 | SR | LMIC | AFR | Yes | EC | CHE | 20 | 5 | 2003–2018 |
| Ökem 201560 | SR | LMIC | EUR | Yes | EC | OOPE | 76 | ≥10 | 2000–2012 |
| Okoroh 201857 | SR | LMIC | AFR | Yes | EC | CHE, OOPE | 7 | 6 | 2003–2017 |
| Platt 202155 | SR | LMIC | AFR, PAR, SEAR | Yes | NS | CHE, OOPE | 31 | 2 | ≤2019 |
| Prinja 201786 | SR | LMIC | SEAR | No | EC | CHE, OOPE | 14 | 4 | 2005–2015 |
| Ravindran 202056 | NR | LMIC | AFR, PAR, SEAR, WPR | Yes | PA, EC, FI | OOPE | 253 | two academic, 7 grey | 2010–2019 |
| Rezaei 201962 | MA | LMIC | EMR | Yes | NS | CHE | 24 | 6 | 2001–2015 |
| Salmi 201779 | SR, survey | HIC, LMIC | EUR | No | EC | NS | 108 | 4 | 2000–2010 |
| Sanogo 201977 | SR | LMIC | AFR, EUR, PAR, SEAR, WPR | No | EC | NS | 12 | 4 | 2005–2018 |
| Spaan 201273 | SR | LMIC | AFR, SEAR, WPR | No | PA | NS | 159 | 19 | ≤2011 |
| Sum 201843 | SR | HIC, LMIC | PAR, SEAR, WPR | Yes | NS | OOPE | 14 | 5 | 2000–2016 |
| Uzochukwu 201542 | SR | LMIC | AFR | Yes | PA | IHE, OOPE | NS | 6 | 2009–2014 |
| Vaidya 202166 | SR | HIC, LMIC | EUR, PAR, SEAR | No | PA | CHE, OOPE | 50 | three academic, 4 grey | 2000–2019 |
| van Hees 201940 | SR | LMIC | AFR, PAR, SEAR, WPR | Yes | EC | CHE | 44 | 11 | 1995–2018 |
| van Minh 201459 | NR | HIC, LMIC | SEAR, WPR | Yes | NS | CHE, IHE, OOPE | NS | 8 | 1995–2017 |
| Wiysonge 201737 | CR | LMIC | AFR, PAR, SEAR, WPR | Yes | FI, PA | CHE, OOPE | 15 | 20 | 2005–2016 |
| Wu 202067 | SR | LMIC | WPR | No | PA, EC | CHE, OOPE | 44 | 3 | 2000–2018 |
| Yerramilli 201839 | SR | HIC, LMIC | EUR | Yes | NS | CHE, IHE, OOPE | 54 | 4 | 1990–2017 |
Country resource level was self-identified by studies or assigned based on the 2020 World Bank country resource level classification. Geographical regions were assigned according to the World Health Organization country region classification.
AFR, African region; CA, comparative analysis; CHE, catastrophic health expenditure; CR, Cochrane review; EC, expanding coverage; EMR, Eastern Mediterranean region; EUR, European region; FI, financial incentives; FRP, financial risk protection; HIC, high-income countries; IHE, impoverishing health expenditures; LMIC, low-income and middle-income countries; MA, meta-analysis; NR, narrative review; NS, not specified; OOPE, out-of-pocket expenditures; PA, pooling arrangements; PAR, Pan American region; RR, rapid review; ScR, scoping review; SEAR, South East Asian region; SR, systematic review; WPR, Western Pacific region.
Table 2.
Summary of the characteristics of the included studies
| Study characteristic | Number of studies (N=50) |
References |
| Publication year | ||
| 1995–1999 | 0 (0%) | – |
| 2000–2004 | 0 (0%) | – |
| 2005–2009 | 0 (0%) | – |
| 2010–2014 | 11 (22%) | 46 58 59 64 70 73 76 78 81 83 84 |
| ≥2015 | 39 (78%) | 37–45 47–57 60–63 65–69 71 72 74 75 77 79 80 82 85 86 |
| Study period* | ||
| 1990–1994 | 16 (32%) | 38 39 41 47–49 53 55 70–73 80 82 84 85 |
| 1995–1999 | 21 (42%) | 38–41 47–49 53 55 58 59 70–73 80–85 |
| 2000–2004 | 33 (66%) | 38–41 43 47–49 53 55 57–62 64 66 67 70–76 79–85 |
| 2005–2009 | 43 (86%) | 37–45 47–53 55 57–62 64 66 67 69–86 |
| 2010–2020 | 48 (96%) | 37–45 47–67 69–86 |
| Not specified | 2 (4%) | 46 68 |
| Resource level | ||
| LMIC | 36 (72%) | 37 38 40–42 44–47 49–51 55–58 60–62 64 65 67 70 72–78 80 82–86 |
| HIC | 1 (2%) | 53 |
| HIC and LMIC | 12 (24%) | 39 43 48 52 54 59 63 66 69 71 79 81 |
| Not specified | 1 (2%) | 68 |
| Geographical regions* | ||
| African region | 31 (62%) | 37 38 40–42 44 46 47 50 51 54–58 61 64 65 70 73–78 80–85 |
| European region | 12 (24%) | 39 41 48 52 58 60 66 70 71 77 79 83 |
| Eastern-Mediterranean region | 4 (8%) | 49 54 62 83 |
| South-East Asian region | 28 (56%) | 37 38 40 41 43 46 50 54–56 58 59 63 65 66 69–73 75 77 80–82 84–86 |
| Western-Pacific region | 27 (54%) | 37 38 40 41 43 46 48 52 54 56 58 59 63 65 67 69–73 75 77 81–85 |
| Pan-American region | 22 (44%) | 37 38 40 41 43 45 48 52 53 55 56 58 65 66 70 75 77 80–82 84 85 |
| ≥2 world regions | 30 (60%) | 37 38 40 41 43 46 48 50 52 54–56 58 59 63 65 66 69–73 75 77 80–85 |
| Not specified | 1 (2%) | 68 |
| Study design | ||
| Systematic review | 34 (68%) | 38–43 45 48 50–52 55 57 58 60 61 63 65–67 69 70 72 73 75–82 85 86 |
| Comparative analysis | 4 (8%) | 46 64 68 71 |
| Narrative review | 4 (8%) | 56 59 83 84 |
| Scoping review | 3 (6%) | 44 54 74 |
| Meta-analysis | 2 (4%) | 49 62 |
| Cochrane review | 2 (4%) | 37 53 |
| Rapid review | 1 (2%) | 47 |
| Target population | ||
| Women and children | 5 (10%) | 38 56 58 78 83 |
| Low-income groups | 4 (8%) | 40 76 77 81 |
| Cancer | 2 (4%) | 48 52 |
| Multimorbidity | 1 (2%) | 43 |
| Mental health | 1 (2%) | 85 |
| Tuberculosis | 1 (2%) | 80 |
| Surgery | 1 (2%) | 55 |
| Studies with concept definitions* | ||
| Defined universal health coverage | 31 (62%) | 37 38 40–42 45 46 49–51 53–59 61–65 67 68 72 75 77 83–86 |
| Defined financial risk protection | 26 (52%) | 37–62 |
| Defined equity | 14 (28%) | 39 40 43 45 57 63 64 66 69 72 77 79 81 84 |
| Financial risk protection measures* | ||
| Out-of-pocket expenditures | 31 (62%) | 37 39 41–43 45 46 48 50–57 59 60 63–70 72 75 82 85 86 |
| Catastrophic health expenditures | 25 (50%) | 37 39 40 44 45 49–51 53–55 57 59 61–63 65–67 69 70 72 76 78 86 |
| Impoverishing health expenditures | 11 (22%) | 39 42 44–46 50 51 54 59 65 72 |
| Financial risk protection interventions* | ||
| Pooling arrangements | 18 (36%) | 37 42 46 47 50 51 53 54 56 63 66–71 73 74 |
| Expanding insurance coverage | 23 (46%) | 40 41 45 46 54 56–58 60 61 64 65 67 72 75–81 85 86 |
| Financial incentives | 9 (18%) | 37 38 46 56 58 80 82–84 |
Country resource level was self-identified by studies or assigned based on the 2020 World Bank country resource level classification. Geographical regions were assigned according to the World Health Organization country region classification.
*Overlapping categories.
HIC, high-income countries; LMIC, low-income and middle-income countries.
What is known in the literature about FRP?
FRP as a concept
Twenty-six (52%) studies defined FRP as a concept,37–62 with 23 (46%) studies specifically referring to FRP as a necessary step to achieving UHC.37–46 49–51 53–62 Some studies suggested that FRP is achieved when households are able to use safe, effective and high-quality health services, without sacrificing other necessities for well-being, such as nutrition.37–39 45 49 51 53 54 Others considered FRP more narrowly as a means of reducing illness-related expenditures.40–42 48 52 57–60 This includes the concept of ‘financial toxicity’, which describes the distress and financial hardship experienced by patients and their caregivers following a cancer diagnosis.48 52 Studies further suggested that a lack of FRP may exacerbate health and socioeconomic inequities by reducing access to health services and discouraging or delaying care-seeking.39 47 50 56
FRP as a measure
Thirty-eight studies (76%) used one or more of the following FRP measures: (1) out-of-pocket expenditures (OOPE) (n=31, 62%), (2) catastrophic health expenditures (CHE) (n=25, 50%) and (3) impoverishing health expenditures (IHE) (n=11, 22%), with 21 (42%) studies mentioning at least two measures, and eight (16%) considering all three. These measures may be calculated for all health-related expenditures or for specific categories of services, such as chronic disease, infectious disease or maternal health.44 48 52 55 As CHE and IHE are measured against thresholds, some studies may also calculate the mean positive overshoot of the threshold to quantify the intensity of financial hardship.44 45 61
Out-of-pocket expenditures
OOPE include payments, not reimbursed by insurance, made by individuals or households to meet health-related needs.39 46 53 56 57 63 64 Direct payments include health service costs and indirect payments may include transportation costs and losses in productivity or income when accessing health services.39 48 52 55 57 63 64 OOPE indicators may be measured as changes in spending due to illness46 53 55 65; as the proportion of annual wages or disposable income43; or as a proportion of the ability to pay, defined as basic need expenditures (with food often used as a proxy for basic needs).39 44 55 62 The occurrence of OOPE may reflect a low degree of FRP because even small OOPE can cause financial hardship for poor households.39 56 66
Catastrophic health expenditures
CHE was defined as excess spending on health that may cause financial catastrophe, measured as health-related OOPE in the numerator and total income or consumption (budget share method) or spending on basic needs (ability to pay method) in the denominator.39 44 45 49 57 62 65 Thresholds of 10%–25% are used for the budget share method (10% of total household expenditures or 20%–25% of total household income),39 45 49 55 57 and 25%–40% for the ability to pay method.39 49 53 55 57 61 62 67 Some studies use the normative food spending approach to define ability to pay, where a household’s food-related expenditures are subtracted from total consumption and the remaining amount is used in the denominator to calculate CHE.39 45 49 53 57 62 An advantage of CHE indicators is that they can be calculated for all income groups; however, these indicators do not capture descent into poverty owed to healthcare expenditures.45
Impoverishing health expenditures
To understand whether health needs push households into poverty, health-related OOPE may be measured against predefined poverty lines.39 44–46 59 61 65 Poverty lines represent the level at which the basic needs of life cannot be met.45 Absolute poverty lines may be used, such as the World Bank international poverty line (currently, US$1.90 per person per day)39 61 or national poverty lines based on the World Bank poverty assessment, food poverty (cost of minimum food requirements) or basic needs (cost of the basket of goods considered to satisfy basic biological needs).39 Relative thresholds may also be considered, calculated as household income over the national mean or median income.39
FRP as an intervention
Among the included studies, the following interventions were employed to increase FRP in the population: (1) pooling arrangements (n=18, 36%), (2) expanding insurance coverage (including either the benefit package or the proportion of the population or costs covered) (n=23, 46%) and (3) implementing financial incentives (n=9, 18%).
Pooling arrangements
Risk pooling involves delinking health-related financial contributions from health risk by enabling lower-need (and by extension, healthier and/or wealthier) individuals to subsidise higher-need (and by extension, sicker and/or poorer) individuals.37 42 50 53 54 63 68–71 Consequently, health-related financial risk is spread to a pool of individuals, rather than being borne by a single person experiencing ill health.68 70 71 The design of pooling arrangements, including the source of funds and extent of government subsidisation; whether contributions are compulsory or voluntary; and the size, number and competitiveness of pools, affects the extent to which risk pooling is achieved.37 42 47 50 53 66 68 70 71 The pooling arrangements examined by the included studies comprised national or social health insurance (SHI; compulsory schemes operated by the state, which are publicly financed through taxation or social security schemes)37 46 51 56 66 69–74; community-based health insurance (CBHI; voluntary schemes operated by non-profit and non-governmental insurers, in which insurers apply community-rated premiums)37 41 47 50 51 73 75 76; and private health insurance (PHI; voluntary schemes operated by private for-profit insurers with little to no state involvement, in which insurers apply risk-rated premiums).37 51 53 66 67 72 73 PHI schemes can be further classified as complementary (covering residual OOPE, such as copayments, or additional health services, excluded from the state benefit package), supplementary (providing enhanced provider choice and access) or substitutional (providing coverage to those unable to receive state benefits).53 66–68
Expanding insurance coverage
Several studies examined the effects of expanding the benefit package (ie, the health services covered by insurance schemes) and extending insurance coverage to a greater proportion of the population or healthcare costs.45 46 54 56–58 60 61 64 67 76–80 Limited health service coverage may result in greater OOPE, thereby reducing FRP.46 57 60 61 80 Populations experiencing socioeconomic marginalisation may also be more vulnerable to increased OOPE due to barriers to insurance enrollment, such as premiums.40 67 78 81 While previously, many health benefits packages tended to prioritise coverage for low-probability, high-cost inpatient services, there has been increasing recognition that outpatient chronic disease prevention and management, including prescription drugs, drive health-related OOPE.43 45 46
Financial incentives
Financial incentives, including general and conditional cash transfers, vouchers, removal of user fees and other subsidies, seek to reduce financial barriers to specific health services and facilitate utilisation, adherence to short-term and long-term treatments, and health-promotive behaviours among health system users and targeted populations experiencing marginalisation.37 38 46 56 58 80 82–84
Which evidence gaps remain in the literature on FRP?
Studies identified evidence gaps related to the effectiveness of FRP interventions, their equity implications, and their cost-effectiveness. The identified research evidence gaps are summarised in table 3.
Table 3.
Evidence gaps identified from the literature
| Category / Number of studies (N=50) |
Specific evidence need | References |
| Evidence of effectiveness N=27 (54%) |
Impact on health service utilisation
|
37 46–48 53 54 56 58 65 69–71 73 82 85 |
Impact on FRP
|
39 43–45 48 51 52 55–57 65 69 70 73 86 | |
Impact on experience of care
|
57 77 84 | |
Impact on health status
|
37 58 65 69 70 73 83 84 | |
| Equity considerations N=13 (26%) |
Stratification of FRP intervention coverage
|
46 47 67 70 73 84 |
Stratification of FRP indicators and other outcomes
|
37–40 44 47 70 73 79 85 | |
| Evidence of cost-effectiveness N=9 (18%) |
Estimating resource requirements and input costs
|
57 69 82 83 |
Mobilising and managing resources
|
42 46 69 | |
Establishing cost-effectiveness
|
38 51 69 82–84 |
CHE, catastrophic health expenditures; DALYs, disability-adjusted life-years; FRP, financial risk protection; IHE, impoverishing health expenditures; OOPE, out-of-pocket expenditures; QALYs, quality-adjusted life-years; UHC, universal health coverage.
Evidence of effectiveness
Studies (n=27, 54%) recognised that implementation of FRP interventions should be informed by evidence of their effectiveness in relation to health service use, FRP, patient experiences and health status.
Impact on health service utilisation
Expansion of health insurance through SHI and CBHI had mixed effects on general health service use.37 46 65 70 73 Among reviews that considered the types of health services, SHI and CBHI were associated with increases in the use of antenatal47 58 70 74 and outpatient (including curative, disease management and preventive care)47 65 69 70 73 74 services, as well as increases in73 or no association with inpatient service use.47 The included reviews further noted that few studies examined the effects of PHI on health service use.37 73 In the USA and China, PHI was associated with increased use of preventive care,53 67 but was not associated with the use of inpatient or outpatient care.67 Other reviews found that financial incentives may improve adherence to long-term but not short-term treatments.37 70 As countries are expanding coverage to outpatient chronic disease and mental healthcare and pharmaceuticals, several reviews noted that future studies should investigate whether this yields increased access to and utilisation of these services.37 45–47 85 It also remains unclear what proportion of the observed increases in utilisation may represent health service overuse, particularly for high-cost invasive procedures.58 70 82
Impact on FRP
The impact of FRP interventions on measures of FRP, including OOPE, CHE and IHE, has been characterised as inconsistent.45 65 69 70 86 SHI, CBHI and financial incentives have been associated with reductions in OOPE in some reviews65 69 73 74 80 86 and no significant effect in others.65 70 86 Studies have provided the following suggestions for future research to clarify impacts: (1) investigating the specific health services that drive high OOPE39 45 55; (2) the role of chronic illness and multimorbidity in driving high OOPE43 44 48; (3) the role of non-medical services, such as transportation and food, in exacerbating health-related OOPE44 48 55 57 and (4) whether the cost of premiums or entry fees into insurance schemes (which are presently not included in health-related OOPE calculations) affect FRP.70
Impact on experience of care
Reviews suggested the need to monitor patient experiences and perceptions of care, as these outcomes are relevant to care-seeking but are not typically considered among FRP intervention impact evaluations.57 77 84 In one review that reported on this outcome, enrollment in SHI was associated with the perception that care is more affordable, compared with uninsured individuals.74
Impact on health status
Several reviews noted that population health outcomes, including morbidity, mortality, disability or health utility measures (quality-adjusted life-years or disability-adjusted life-years) should be considered in FRP impact evaluations.37 58 65 69 83 84 Among reviews that evaluated health outcomes, FRP interventions were associated with improvements in tuberculosis treatment rates and perinatal maternal and infant outcomes in some reviews74 80 and were not significantly associated with perinatal infant outcomes and general health status in others.37 70 73 74 Health outcomes may also be tailored to target populations and health system contexts. For example, the impact of maternal and neonatal FRP interventions may be measured by stratifying maternal and neonatal health status by home-based and facility-based deliveries, as FRP interventions may lead to more facility-based deliveries.58 83
Equity considerations
Studies noted that evaluations of effectiveness should assess whether FRP intervention impacts are equitable (n=13, 26%). Specifically, studies recommended stratifying (1) FRP intervention coverage and (2) FRP indicators and other outcomes across subgroups experiencing marginalisation. Poverty, chronic illness and older age were observed to be the most frequent strata reported by primary studies,39 40 42 43 45 85 possibly because these subgroups are more readily identifiable in most data sources.40 Several reviews have suggested considering additional subgroups for stratification, including area of residence, gender, citizenship/migration status, ethnicity, employment status, homelessness and institutionalisation39 40 42 43 45 85; however, these facets of marginalisation remain more challenging to operationalise due to variation in political and cultural contexts.40
Stratification of FRP intervention coverage
Reviews suggested monitoring new enrollees in FRP interventions and estimating what proportion of the population covered was part of a marginalised group, as overall enrollment estimates may mask inequities in coverage among marginalised populations.46 47 70 73 84 For instance, fewer PHI selling agencies, lower availability of PHI information and poor access to healthcare providers in rural and low-income areas may underlie disparities in PHI enrollment.47 Others have suggested that while affordable premiums may support CBHI enrollment among poorer segments of the population, higher copayments may discourage care seeking, resulting in poorer households subsidising wealthier enrollees.47 Disparities in coverage may further exacerbate inequities in downstream outcomes (eg, OOPE or health status).46 70 73 84
Stratification of FRP intervention impacts
The included reviews observed a need to collect and analyse disaggregated OOPE, CHE or IHE data to investigate whether FRP interventions reduce inequities in health-related expenditures among subgroups experiencing marginalisation, compared with the general population.37–39 45 47 79 85 Interestingly, among reviews that identified studies with disaggregated data, high expenditures persisted among individuals with chronic illnesses, older adults and individuals with disabilities.40 44
As it is hypothesised that removing financial barriers to healthcare would improve population health, reviews highlighted a need to also disaggregate intervention impacts across other outcomes, including health service utilisation and health status.70 73 79 85 Among reviews that identified studies that disaggregated health service utilisation, CBHI has been associated with more equitable need-based healthcare use across income quartiles, compared with those who were uninsured.47 73 SHI has been associated with greater health service use among low-income groups, though differences remained in the use of public versus private healthcare facilities.51 73 PHI has shown mixed effects on cancer screening uptake in the US across race-based subgroups,53 while in China, PHI has been associated with greater healthcare utilisation only among urban residents.67
Evidence of cost-effectiveness
In addition to demonstrating effectiveness, studies (n=9, 18%) noted that cost-effectiveness of FRP interventions should be considered, given its relevance to decision-makers. This involves gaining a comprehensive understanding of intervention resource requirements, resource management and comparative cost-effectiveness.
Estimating resource requirements and input costs
Studies highlighted the need to estimate start-up,57 82 operating82 83 and scale-up69 83 costs of FRP interventions to ensure adequate coverage of the target population and to inform intervention sustainability. This includes standardising intervention costing approaches to enable robust comparisons.57 83
Mobilising and managing resources
Other key evidence gaps related to articulating clear approaches to mobilising resources to meet the needs of FRP interventions; determining optimal intervention financing models, including the roles of governments and other payers; and understanding how to best manage resources once programmes are funded.42 69 73
Establishing comparative cost-effectiveness
Cost-effectiveness includes a broad class of analyses that seek to estimate the benefit of programmes, such as improvements in health status or changes in health service use, relative to their resource inputs.38 51 83 84 In addition to estimating the cost-effectiveness of individual FRP interventions, researchers should consider how cost-effective programmes are relative to alternative programmes seeking to achieve the same impacts.69 82 83
Which methodological gaps remain in the literature on FRP?
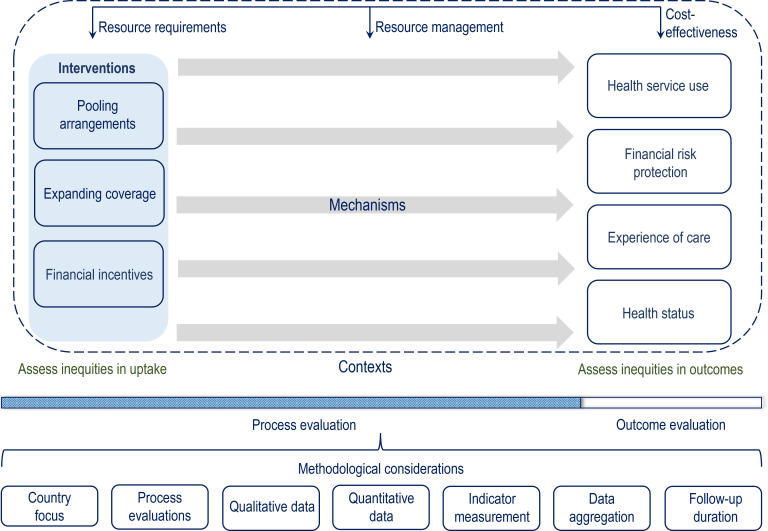
A number of methodological issues should be considered when designing studies to address the identified evidence gaps. A concept map outlining the evidence gaps and methodological considerations is presented in figure 2.
Figure 2.
Concept map of financial risk protection interventions, impacts, evidence gaps and methodological considerations.
Country focus
Researchers should consider the trade-offs of performing single-country versus multicountry analyses. While multicountry studies provide a snapshot of a large body of evidence, these analyses tend to lack depth in terms of time-trends and contextual features within and outside of the healthcare system.39 40 In addition, countries may be unequally represented in multicountry reviews, leading to biased conclusions.39 41 50 69 73 81 On the other hand, although findings from single-country case studies may not be generalisable to other settings,39 51 61 62 77 they may provide more detailed contextual information.39 46 73 Multijurisdictional case-studies and health system comparative research may provide an opportunity to capitalise on the strengths of both approaches.39 54 66
Process evaluations
Despite the widespread political commitment to UHC through FRP, studies noted that implementation of these aims has been suboptimal and there remains a lack of understanding of how contextual factors, including the political environment, social welfare policies, culture, population size and characteristics, historical investment in the healthcare system, economic growth and the number of payers (eg, government, private and users), may facilitate or hinder financing, implementing, operating and scaling up of FRP interventions.39 40 46 47 59 69 73 More research is also needed to elucidate how implementation of new FRP interventions, such as CBHI or incentive-based programmes, could complement the existing health financing arrangements to progress towards UHC.41 67 In addition to implementation issues, studies highlighted the current limited understanding of the reasons why FRP interventions do not achieve their intended impacts after implementation.47 65 This is especially relevant when considering the failures of some FRP interventions to reduce inequities in coverage; incurred OOPE, CHE and IHE; and poor health outcomes among marginalised segments of the population.60 63 72
Process evaluation could address explanatory research questions related to how contexts affect the implementation and success of FRP interventions.47 54 56 86 Realist evaluation methods may be particularly well-suited to addressing such aims, as realist evaluation seeks to identify context-mechanism-outcome configurations that describe what works, for whom and in which circumstances.40 56 Finally, two reviews noted that it is unclear whether FRP programmes and their evaluations are informed by specific conceptual frameworks or theories of change.38 79 Consensus should also be reached regarding the relevant process indicators to enable process evaluation comparability.86
Qualitative data
Reviews acknowledged the limited availability of qualitative evidence, including key stakeholder perspectives.40 54 65 86 Qualitative data can support process and realist evaluations by illuminating how implementation issues, contexts and mechanisms of change may influence the intervention–outcome associations observed in the quantitative data, including inequitable impacts.40 54 65 69 Hunter and Murray82 also cautioned that many studies with qualitative components tend to be situated within large mixed-methods evaluations, in which more attention is devoted to reporting the quantitative findings.82 Future qualitative and mixed-methods studies should thus provide more thorough descriptions of and rationale for the chosen data collection and analytical methods, as well as reflections on the role of the researcher in generating the results.82
Quantitative data
Poorly controlled observational study designs—particularly, self-reported cross-sectional household surveys—are abundant in the evidence base.38 40 43 45 47 48 57 58 65 70 72 73 75 81–83 This limits the ability to make causal inferences about FRP interventions and leaves the possibility of residual confounding related to population and health system factors.41 57 82 83 While the use of randomised controlled trials may clarify intervention impacts,53 58 65 using such study designs to evaluate government reforms or SHI schemes may not be feasible or ethical, compared with evaluating CBHI or incentive-based interventions.38 65 Future studies may consider alternative designs, such as well-controlled quasi-experimental studies, to evaluate programmes.52 53 56 70 81 Further, since countries may employ multiple complex interventions to implement FRP, studies may need to evaluate combinations of interventions over individual programmes.67 81
Indicator measurement
Reviews note that many studies focus on the incidence of OOPE or CHE, but few consider IHE.39 44 The number of households estimated to be experiencing CHE or IHE is also contingent on the choice of thresholds, which has implications for analyses related to the equity of FRP intervention impacts.39 44–46 For instance, IHE measures are affected by poverty lines, and while international poverty lines may be more suitable for comparative studies, they may result in less sensitive indicators for HIC and some middle-income countries.39 44 Using national poverty lines may overcome this issue, but hinder international comparisons.39 In regard to CHE, studies have shown that the budget share method tends to find that health-related financial hardship is concentrated among wealthier households.39 As such, ability to pay approaches for estimating CHE have been recommended, particularly when considering equity in the analysis.39 One review recommended that costs should be consistently converted to US dollars to improve comparability.55 Two reviews also noted a lack of validated disease-specific measures of financial risk, such as cancer-related financial toxicity, which limits comparability.48 52
Data aggregation
Meta-analyses could not be performed in many quantitative reviews.40 50 57 58 62 65 67 79 80 Robust inferences also could not be drawn due to different data sources,44 57 different data scope (eg, national versus targeted population surveys),44 different recall periods,57 unclear documentation of data collection processes,39 45 57 and lack of standardisation in data collection and outcome measures across survey cycles and countries.39 45 50 In some countries, the wait period to receive insurance coverage for new enrollees or migrants may also result in information bias due to misclassification, as this wait period would effectively render these groups uninsured and expose them to higher healthcare expenditures.57 Finally, it is unclear how the data collected for purposes other than FRP assessment, such as administrative data, may affect estimates of incurred costs.44
Follow-up duration
Most quantitative studies were conducted early in FRP intervention implementation, particularly those evaluating programme pilots.39 44 59 72 82 83 This may, in part, explain the aforementioned evidence gaps related to evaluations of impact on health status and equity, as well as the lack of clarity regarding long-term trends in FRP indicators, such as OOPE, CHE or IHE.44 59 83 Future studies should consider using longitudinal and panel data to provide sufficient variation to analyse FRP intervention impacts over time.39 44 45 47 48 59 72
Discussion
In this scoping overview of 50 academic literature reviews, we described the current state of knowledge on FRP in the UHC context and evidence gaps that should be prioritised in future research. We found that although FRP is recognised as a necessary dimension for achieving UHC, it remains unclear whether interventions increase FRP and optimise health service utilisation, experience of care and health status. The lack of disaggregated information across measures of social marginalisation may further explain the limited understanding regarding how to equitably increase FRP among subgroups at greatest risk of poor health and its financial consequences. Finally, there is little evidence regarding the resources required to implement and sustain FRP interventions and regarding their cost-effectiveness. These evidence gaps are further compounded by methodological challenges.
Interpretation and future directions
Previous work has suggested that the theory of change for SDG 3 has some limitations, as not all input, process and impact indicators align.87 This included an omission of impact indicators for FRP (where impacts are defined as long-term changes occurring in communities or systems as a result of FRP),87 which may explain the limited evidence of effectiveness of FRP interventions in relation to health service utilisation, experience of care and health status, in addition to financial risk. Reliance on cross-sectional self-reported household surveys in LMIC may partially underpin some methodological issues, such as the lack of longitudinal follow-up and poor interjurisdictional comparability, and contribute to the inconclusiveness of existing effectiveness evaluations.9 88–90 Furthermore, the problem of unmeasured confounding persists even among well-designed observational studies, limiting causal interpretations.91 The growing use of routine health information systems (RHIS) for research in LMIC may present an opportunity to conduct higher-quality FRP intervention evaluations.45 92 For instance, RHIS data have been successfully used to support longitudinal programme impact evaluations in relation to health service use and disease-related outcomes using time series and difference-in-difference designs (though it should be noted that RHIS may not provide information on FRP metrics like household OOPE, CHE and IHE).92 In addition, ambiguities in the quantitative evidence of effectiveness of FRP interventions may be owed to the inherent complexities of implementing and evaluating public health interventions within dynamic settings,93 rather than a limited evidence base. As such, our findings suggest that process evaluations using qualitative and mixed methods should accompany impact evaluations to elucidate FRP mechanisms of action across different health system contexts and population subgroups.94
Inconsistencies in concept definitions may underlie methodological issues. While there is general agreement on the importance of UHC, interpretations of the concepts of universality, health, and coverage vary in breadth, affecting the scope of FRP interventions and the choice of indicators used to monitor progress.10 11 95 The common indicators of FRP—OOPE, CHE and IHE—may also not sufficiently capture the FRP concept, as these measures rely on healthcare utilisation and do not account for individuals deterred from care-seeking by financial barriers, those opting for lower-quality health services, and those resorting to borrowing or selling assets to afford health services.9 46 55 96 In addition, while equity has often been thought to be implicit in the goal of UHC and an assumed consequence of its achievement,11 97 98 there is increasing recognition that striving for health for all and reducing disparities are two separate aims, warranting the need to explicitly measure and monitor equity in UHC efforts (including FRP interventions) using disaggregated data.97 Although there is no agreement on which stratifying variables should be selected when measuring inequities,97 the reviews included in this overview highlighted a need to disaggregate data across several social determinants of health (eg, area of residence and migration status), in addition to income status.
Strengths and limitations
We conducted the first scoping overview to identify research needs in the FRP knowledge base. A strength of our study is our use of systematic searching and evidence review methods. Several limitations should also be considered. First, we limited our search by language and publication dates. Relevant studies in languages other than English or French may thus have been missed. We believe our inclusion of evidence published after 1995 to be reasonable, as bibliometric analyses have shown that UHC publications began to increase after the adoption of MDGs in 2000,8 and the study periods of the included reviews spanned 1990 and 2020. Second, since our objective was to describe knowledge gaps within the academic evidence base, we relied on published peer-reviewed work, rather than grey literature. Third, we employed descriptive content analysis methods, which involve greater reliance on the original study authors’ interpretations. Importantly, as performing a critical appraisal of the quality of the evidence is outside the scope of a scoping review,23 we are unable to make robust conclusions regarding the evidence of intervention effectiveness.99 The identified evidence gaps should be interpreted as a descriptive summary of research needs characterised by the authors of the included reviews, rather than our own inferences. Participatory approaches, such as Delphi panels and stakeholder interviews, should follow the present work in order to rank the identified research priorities and further develop the UHC research agenda.14 Fourth, while an advantage of overviews is their provision of an overall picture of a research field or phenomenon,20 most of the included reviews were multicountry and/or multiregion studies with limited information on the sociopolitical, legal and fiscal contexts within which FRP efforts were undertaken. Fifth, while we did not select for specific literature review study designs, the over-representation of LMIC among the included studies may be owed to more evidence syntheses on UHC in these settings, but not necessarily a lack of primary studies in HIC.
Conclusion
This scoping overview of reviews summarised what is known about achieving UHC through FRP and found evidence gaps related to the effectiveness, cost-effectiveness and equity implications of FRP interventions. Theory-informed, high-quality mixed-methods research using longitudinal and disaggregated data is needed to address the identified gaps.
Supplementary Material
Acknowledgments
We gratefully acknowledge Vincci Lui (Gerstein Science Information Centre, University of Toronto) for providing expert advice on the bibliographic database search strategy. We also thank our grant collaborators, Drs Beverley Essue, Garry Aslanyan, Miguel Gonzalez Block, Gregory Marchildon, and Jeremy Veillard, for their helpful comments on earlier versions of this work.
Footnotes
Twitter: @ed4socialchange
Contributors: DB: conceptualisation, methodology, data curation, investigation, formal analysis, writing-original draft, writing-review and editing, project administration. SM: conceptualisation, methodology, data curation, investigation, formal analysis, writing-original draft, writing-review and editing. AK: conceptualisation, methodology, writing-review and editing. BY: conceptualisation, methodology, writing-review and editing. SA: conceptualisation, methodology, resources, funding acquisition, supervision,
writing-review and editing. EDR: conceptualisation, methodology, resources, funding acquisition, supervision, writing-review and editing. EDR and SA are the senior authors of this work. EDR is the guarantor of this research and accepts full responsibility for the finished work and the conduct of the study, had access to the data and controlled the decision to publish.
Funding: This research was supported by a grant to Drs. Erica Di Ruggiero and Sara Allin from the Canadian Institutes for Health Research (CIHR) (#407149) for the project titled 'Towards Equitable Universal Health Coverage in a Globalised Era: A Research Agenda-Setting Workshop'.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study. This work analysed secondary sources, which are cited and are accessible publicly or with academic institutional credentials. Search strategies are provided in the online supplemental material.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.World Health Assembly . WHA58.33 Sustainable health financing, universal coverage and social health insurance [Internet]. World Health Organization, 2005. Available: http://apps.who.int/iris/bitstream/handle/10665/20383/WHA58_33-en.pdf?sequence=1
- 2.Department of Economic and Social Affairs, Sustainable Development . Goal 3: Ensure healthy lives and promote well-being for all at all ages [Internet]. United Nations, 2021. Available: https://sdgs.un.org/goals/goal3
- 3.World Health Organization . Thirteenth General Programme of Work 2019−2023 [Internet]. World Health Organization, 2019. Available: https://www.who.int/about/what-we-do/thirteenth-general-programme-of-work-2019-2023
- 4.World Health Organization . Primary health care on the road to universal health coverage: 2019 monitoring report: executive summary [Internet]. World Health Organization, 2019. Available: https://www.who.int/docs/default-source/documents/2019-uhc-report-executive-summary
- 5.Lozano R, Fullman N, Mumford JE, et al. Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet 2020;396:1250–84. 10.1016/S0140-6736(20)30750-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization . The world health report: health systems financing: the path to universal coverage. Geneva, Switzerland: World Health Organization, 2010. https://apps.who.int/iris/bitstream/handle/10665/44371/9789241564021_eng.pdf?sequence=1&isAllowed=y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Global Burden of Disease Health Financing Collaborator Network . Health sector spending and spending on HIV/AIDS, tuberculosis, and malaria, and development assistance for health: progress towards sustainable development goal 3. Lancet 2020;396:693–724. 10.1016/S0140-6736(20)30608-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ghanbari MK, Behzadifar M, Doshmangir L, et al. Mapping research trends of universal health coverage from 1990 to 2019: bibliometric analysis. JMIR Public Health Surveill 2021;7:e24569. 10.2196/24569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saksena P, Hsu J, Evans DB. Financial risk protection and universal health coverage: evidence and measurement challenges. PLoS Med 2014;11:e1001701. 10.1371/journal.pmed.1001701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abiiro GA, De Allegri M. Universal health coverage from multiple perspectives: a synthesis of conceptual literature and global debates. BMC Int Health Hum Rights 2015;15:17. 10.1186/s12914-015-0056-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O'Connell T, Rasanathan K, Chopra M. What does universal health coverage mean? The Lancet 2014;383:277–9. 10.1016/S0140-6736(13)60955-1 [DOI] [PubMed] [Google Scholar]
- 12.Stuckler D, Feigl A, Basu S. The political economy of universal health coverage. Background paper for the global symposium on health systems research. In: Science to accelerate universal health coverage. Montreux, Switzerland: World Health Organization, 2010. [Google Scholar]
- 13.Gluckman PD, Bardsley A, Kaiser M. Brokerage at the science–policy interface: from conceptual framework to practical guidance. Humanit Soc Sci Commun 2021;8:84. 10.1057/s41599-021-00756-3 [DOI] [Google Scholar]
- 14.Ranson MK, Bennett SC. Priority setting and health policy and systems research. Health Res Policy Syst 2009;7:27. 10.1186/1478-4505-7-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nyanchoka L, Tudur-Smith C, Thu VN, et al. A scoping review describes methods used to identify, prioritize and display gaps in health research. J Clin Epidemiol 2019;109:99–110. 10.1016/j.jclinepi.2019.01.005 [DOI] [PubMed] [Google Scholar]
- 16.Lund H, Brunnhuber K, Juhl C, et al. Towards evidence based research. BMJ 2016;355:i5440. 10.1136/bmj.i5440 [DOI] [PubMed] [Google Scholar]
- 17.Bennett S, Jessani N, Glandon D, et al. Understanding the implications of the sustainable development goals for health policy and systems research: results of a research priority setting exercise. Global Health. 2020;16:5. 10.1186/s12992-019-0534-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Qiu M, Jessani N, Bennett S. Identifying health policy and systems research priorities for the sustainable development goals: social protection for health. Int J Equity Health 2018;17:155. 10.1186/s12939-018-0868-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pollock M, Fernandes RM, Becker LA, et al. What guidance is available for researchers conducting overviews of reviews of healthcare interventions? A scoping review and qualitative metasummary. Syst Rev 2016;5:190. 10.1186/s13643-016-0367-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aromataris E, Fernandez R, Godfrey CM, et al. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc 2015;13:132–40. 10.1097/XEB.0000000000000055 [DOI] [PubMed] [Google Scholar]
- 21.Robinson KA, Saldanha IJ, McKoy NA. Development of a framework to identify research gaps from systematic reviews. J Clin Epidemiol 2011;64:1325–30. 10.1016/j.jclinepi.2011.06.009 [DOI] [PubMed] [Google Scholar]
- 22.Gates M, Gates A, Guitard S, et al. Guidance for overviews of reviews continues to accumulate, but important challenges remain: a scoping review. Syst Rev 2020;9:254. 10.1186/s13643-020-01509-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peters MDJ, Marnie C, Tricco AC, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth 2020;18:2119–26. 10.11124/JBIES-20-00167 [DOI] [PubMed] [Google Scholar]
- 24.Glandon D, Meghani A, Jessani N, et al. Identifying health policy and systems research priorities on multisectoral collaboration for health in low-income and middle-income countries. BMJ Glob Health 2018;3:e000970. 10.1136/bmjgh-2018-000970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 26.Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69. 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Colquhoun HL, Levac D, O'Brien KK, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol 2014;67:1291–4. 10.1016/j.jclinepi.2014.03.013 [DOI] [PubMed] [Google Scholar]
- 28.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 29.Mishra S, Bhatia D, Allin S. Financial Risk Protection under Universal Health Coverage: A Scoping Review Protocol [Internet]. Open Science Framework, 2020. Available: https://osf.io/kqamx/?view_only=6315dbae7133475d8a294ff9db45df01
- 30.World Health Organization . Millennium Development Goals (MDGs) [Internet]. World Health Organization, 2018. Available: https://www.who.int/news-room/fact-sheets/detail/millennium-development-goals-(mdgs)
- 31.InterTASC Information Specialists SubGroup . Systematic Reviews: Filters [Internet]. InterTASC Information Specialists SubGroup, 2020. Available: https://sites.google.com/a/york.ac.uk/issg-search-filters-resource/home/systematic-reviews?authuser=0
- 32.Hosking J, Macmillan A, Jones R, et al. Searching for health equity: validation of a search filter for ethnic and socioeconomic inequalities in transport. Syst Rev 2019;8:94. 10.1186/s13643-019-1009-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Connected Papers [Internet], 2021. Available: https://www.connectedpapers.com/about
- 34.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. [Internet]. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available: http://handbook.cochrane.org
- 35.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health 2000;23:334–40. [DOI] [PubMed] [Google Scholar]
- 36.Sandelowski M. What's in a name? Qualitative description revisited. Res Nurs Health 2010;33:77–84. 10.1002/nur.20362 [DOI] [PubMed] [Google Scholar]
- 37.Wiysonge CS, Paulsen E, Lewin S, et al. Financial arrangements for health systems in low-income countries: an overview of systematic reviews. Cochrane Database Syst Rev 2017;9:CD011084. 10.1002/14651858.CD011084.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bright T, Felix L, Kuper H, et al. A systematic review of strategies to increase access to health services among children in low and middle income countries. BMC Health Serv Res. 2017;17:252. 10.1186/s12913-017-2180-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yerramilli P, Fernández Óscar, Thomson S. Financial protection in Europe: a systematic review of the literature and mapping of data availability. Health Policy 2018;122:493–508. 10.1016/j.healthpol.2018.02.006 [DOI] [PubMed] [Google Scholar]
- 40.van Hees SGM, O'Fallon T, Hofker M, et al. Leaving no one behind? social inclusion of health insurance in low- and middle-income countries: a systematic review. Int J Equity Health 2019;18:134. 10.1186/s12939-019-1040-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fadlallah R, El-Jardali F, Hemadi N, et al. Barriers and facilitators to implementation, uptake and sustainability of community-based health insurance schemes in low- and middle-income countries: a systematic review. Int J Equity Health. 2018;17:13. 10.1186/s12939-018-0721-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Uzochukwu BSC, Ughasoro MD, Etiaba E, et al. Health care financing in Nigeria: implications for achieving universal health coverage. Niger J Clin Pract 2015;18:437. 10.4103/1119-3077.154196 [DOI] [PubMed] [Google Scholar]
- 43.Sum G, Hone T, Atun R, et al. Multimorbidity and out-of-pocket expenditure on medicines: a systematic review. BMJ Glob Health 2018;3:e000505. 10.1136/bmjgh-2017-000505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Njagi P, Arsenijevic J, Groot W. Understanding variations in catastrophic health expenditure, its underlying determinants and impoverishment in sub-Saharan African countries: a scoping review. Syst Rev 2018;7:136. 10.1186/s13643-018-0799-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Koch KJ, Cid Pedraza C, Schmid A. Out-Of-Pocket expenditure and financial protection in the Chilean health care system-A systematic review. Health Policy 2017;121:481–94. 10.1016/j.healthpol.2017.02.013 [DOI] [PubMed] [Google Scholar]
- 46.Lagomarsino G, Garabrant A, Adyas A, et al. Moving towards universal health coverage: health insurance reforms in nine developing countries in Africa and Asia. Lancet 2012;380:933–43. 10.1016/S0140-6736(12)61147-7 [DOI] [PubMed] [Google Scholar]
- 47.Artignan J, Bellanger M. Does community-based health insurance improve access to care in sub-Saharan Africa? a rapid review. Health Policy Plan 2021;36:572–84. 10.1093/heapol/czaa174 [DOI] [PubMed] [Google Scholar]
- 48.Bhanvadia SK, Psutka SP, Burg ML, et al. Financial toxicity among patients with prostate, bladder, and kidney cancer: a systematic review and call to action. Eur Urol Oncol 2021;4:396–404. 10.1016/j.euo.2021.02.007 [DOI] [PubMed] [Google Scholar]
- 49.Doshmangir L, Yousefi M, Hasanpoor E, et al. Determinants of catastrophic health expenditures in Iran: a systematic review and meta-analysis. Cost Eff Resour Alloc 2020;18:17. 10.1186/s12962-020-00212-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hussien M, Azage M. Barriers and facilitators of community-based health insurance policy renewal in low- and middle-income countries: a systematic review. Clinicoecon Outcomes Res 2021;13:359–75. 10.2147/CEOR.S306855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ifeagwu SC, Yang JC, Parkes-Ratanshi R, et al. Health financing for universal health coverage in sub-Saharan Africa: a systematic review. Glob Health Res Policy 2021;6:8. 10.1186/s41256-021-00190-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Longo CJ, Fitch MI, Banfield L, et al. Financial toxicity associated with a cancer diagnosis in publicly funded healthcare countries: a systematic review. Support Care Cancer 2020;28:4645–65. 10.1007/s00520-020-05620-9 [DOI] [PubMed] [Google Scholar]
- 53.Motaze NV, Chi PC, Ongolo-Zogo P, et al. Government regulation of private health insurance. Cochrane Database Syst Rev 2021;2:CD011512. 10.1002/14651858.CD011512.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Odoch WD, Senkubuge F, Hongoro C. How has sustainable development goals Declaration influenced health financing reforms for universal health coverage at the country level? A scoping review of literature. Global Health 2021;17:50. 10.1186/s12992-021-00703-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Platt E, Doe M, Kim NE, et al. Economic impact of surgery on households and individuals in low income countries: a systematic review. Int J Surg 2021;90:105956. 10.1016/j.ijsu.2021.105956 [DOI] [PubMed] [Google Scholar]
- 56.Ravindran TKS, Govender V. Sexual and reproductive health services in universal health coverage: a review of recent evidence from low- and middle-income countries. Sex Reprod Health Matters 2020;28:1779632. 10.1080/26410397.2020.1779632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Okoroh J, Essoun S, Seddoh A, et al. Evaluating the impact of the National health insurance scheme of Ghana on out of pocket expenditures: a systematic review. BMC Health Serv Res. 2018;18:426. 10.1186/s12913-018-3249-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Comfort AB, Peterson LA, Hatt LE. Effect of health insurance on the use and provision of maternal health services and maternal and neonatal health outcomes: a systematic review. J Health Popul Nutr 2013;31:81–105. [PubMed] [Google Scholar]
- 59.Van Minh H, Pocock NS, Chaiyakunapruk N, et al. Progress toward universal health coverage in ASEAN. Glob Health Action 2014;7:25856. 10.3402/gha.v7.25856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ökem ZG, Çakar M. What have health care reforms achieved in Turkey? An appraisal of the "Health Transformation Programme". Health Policy 2015;119:1153–63. 10.1016/j.healthpol.2015.06.003 [DOI] [PubMed] [Google Scholar]
- 61.Okedo-Alex IN, Akamike IC, Ezeanosike OB, et al. A review of the incidence and determinants of catastrophic health expenditure in Nigeria: implications for universal health coverage. Int J Health Plann Manage 2019;34:e1387–404. 10.1002/hpm.2847 [DOI] [PubMed] [Google Scholar]
- 62.Rezaei S, Woldemichael A, Hajizadeh M, et al. Catastrophic healthcare expenditures among Iranian households: a systematic review and meta-analysis. Int J Hum Rights Healthc 2019;12:105–15. 10.1108/IJHRH-02-2018-0017 [DOI] [Google Scholar]
- 63.Myint C-Y, Pavlova M, Thein K-N-N, et al. A systematic review of the health-financing mechanisms in the association of Southeast Asian nations countries and the people's Republic of China: lessons for the move towards universal health coverage. PLoS One 2019;14:e0217278. 10.1371/journal.pone.0217278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Odeyemi IAO, Nixon J. Assessing equity in health care through the National health insurance schemes of Nigeria and Ghana: a review-based comparative analysis. Int J Equity Health 2013;12:9. 10.1186/1475-9276-12-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Erlangga D, Suhrcke M, Ali S, et al. The impact of public health insurance on health care utilisation, financial protection and health status in low- and middle-income countries: a systematic review. PLoS One 2019;14:e0219731. 10.1371/journal.pone.0219731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Vaidya S, Boes S. Strategies to mitigate inequity within mandatory health insurance systems: a systematic review. World Med Health Policy 2021;13:272–92. 10.1002/wmh3.446 [DOI] [Google Scholar]
- 67.Wu R, Li N, Ercia A. The effects of private health insurance on universal health coverage objectives in China: a systematic literature review. Int J Environ Res Public Health 2020;17:2049. 10.3390/ijerph17062049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mathauer I, Saksena P, Kutzin J. Pooling arrangements in health financing systems: a proposed classification. Int J Equity Health 2019;18:198. 10.1186/s12939-019-1088-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Angell B, Dodd R, Palagyi A, et al. Primary health care financing interventions: a systematic review and stakeholder-driven research agenda for the Asia-Pacific region. BMJ Glob Health 2019;4:e001481. 10.1136/bmjgh-2019-001481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Acharya A, Vellakkal S, Taylor F, et al. The impact of health insurance schemes for the informal sector in low- and middle-income countries: a systematic review. World Bank Res Obs 2013;28:236–66. 10.1093/wbro/lks009 [DOI] [Google Scholar]
- 71.Bazyar M, Yazdi-Feyzabadi V, Rashidian A, et al. The experiences of merging health insurance funds in South Korea, Turkey, Thailand, and Indonesia: a cross-country comparative study. Int J Equity Health 2021;20:66. 10.1186/s12939-021-01382-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Izzanie M, Khaled N, Aidalina M. Health insurance inequity in selected Asia countries. International Journal of Public Health and Clinical Sciences 2019;6. [Google Scholar]
- 73.Spaan E, Mathijssen J, Tromp N, et al. The impact of health insurance in Africa and Asia: a systematic review. Bull World Health Organ 2012;90:685–92. 10.2471/BLT.12.102301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Christmals CD, Aidam K. Implementation of the National health insurance scheme (NHIS) in Ghana: lessons for South Africa and low- and middle-income countries. Risk Manag Healthc Policy 2020;13:1879–904. 10.2147/RMHP.S245615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Adebayo EF, Uthman OA, Wiysonge CS, et al. A systematic review of factors that affect uptake of community-based health insurance in low-income and middle-income countries. BMC Health Serv Res. 2015;15:543. 10.1186/s12913-015-1179-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Odeyemi IAO. Community-Based health insurance programmes and the National health insurance scheme of Nigeria: challenges to uptake and integration. Int J Equity Health 2014;13:20. 10.1186/1475-9276-13-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sanogo N'doh Ashken, Fantaye AW, Yaya S. Universal health coverage and facilitation of equitable access to care in Africa. Front Public Health. 2019;7:102. 10.3389/fpubh.2019.00102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bucagu M, Kagubare JM, Basinga P, et al. Impact of health systems strengthening on coverage of maternal health services in Rwanda, 2000-2010: a systematic review. Reprod Health Matters 2012;20:50–61. 10.1016/S0968-8080(12)39611-0 [DOI] [PubMed] [Google Scholar]
- 79.Salmi L-R, Barsanti S, Bourgueil Y, et al. Interventions addressing health inequalities in European regions: the air project. Health Promot Int 2017;32:430–41. 10.1093/heapro/dav101 [DOI] [PubMed] [Google Scholar]
- 80.Aragão FBA, Arcêncio RA, Fuentealba-Torres M, et al. Impact of social protection programs on adults diagnosed with tuberculosis: systematic review. Rev Bras Enferm 2021;74:e20190906. 10.1590/0034-7167-2019-0906 [DOI] [PubMed] [Google Scholar]
- 81.Meng Q, Yuan B, Jia L, et al. Expanding health insurance coverage in vulnerable groups: a systematic review of options. Health Policy Plan 2011;26:93–104. 10.1093/heapol/czq038 [DOI] [PubMed] [Google Scholar]
- 82.Hunter BM, Murray SF. Demand-side financing for maternal and newborn health: what do we know about factors that affect implementation of cash transfers and voucher programmes? BMC Pregnancy Childbirth 2017;17:262. 10.1186/s12884-017-1445-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bellows BW, Conlon CM, Higgs ES, et al. A taxonomy and results from a comprehensive review of 28 maternal health voucher programmes. J Health Popul Nutr 2013;31:106–28. [PubMed] [Google Scholar]
- 84.Grainger C, Gorter A, Okal J, et al. Lessons from sexual and reproductive health voucher program design and function: a comprehensive review. Int J Equity Health 2014;13:33. 10.1186/1475-9276-13-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Docrat S, Besada D, Cleary S, et al. The impact of social, National and community-based health insurance on health care utilization for mental, neurological and substance-use disorders in low- and middle-income countries: a systematic review. Health Econ Rev. 2020;10:11. 10.1186/s13561-020-00268-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Prinja S, Chauhan AS, Karan A, et al. Impact of publicly financed health insurance schemes on healthcare utilization and financial risk protection in India: a systematic review. PLoS One 2017;12:e0170996. 10.1371/journal.pone.0170996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Seidman G. Does SDG 3 have an adequate theory of change for improving health systems performance? J Glob Health 2017;7:010302. 10.7189/jogh.07.010302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Aftab W, Siddiqui FJ, Tasic H, et al. Implementation of health and health-related sustainable development goals: progress, challenges and opportunities - a systematic literature review. BMJ Glob Health 2020;5:e002273. 10.1136/bmjgh-2019-002273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Luz A, Santatiwongchai B, Pattanaphesaj J, et al. Identifying priority technical and context-specific issues in improving the conduct, reporting and use of health economic evaluation in low- and middle-income countries. Health Res Policy Syst 2018;16:4. 10.1186/s12961-018-0280-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Griffiths UK, Legood R, Pitt C. Comparison of economic evaluation methods across low-income, middle-income and high-income countries: what are the differences and why? Health Econ 2016;25 Suppl 1:29–41. 10.1002/hec.3312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Levy H, Meltzer D. The impact of health insurance on health. Annu Rev Public Health 2008;29:399–409. 10.1146/annurev.publhealth.28.021406.144042 [DOI] [PubMed] [Google Scholar]
- 92.Hung YW, Hoxha K, Irwin BR, et al. Using routine health information data for research in low- and middle-income countries: a systematic review. BMC Health Serv Res 2020;20:790. 10.1186/s12913-020-05660-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ogilvie D, Cummins S, Petticrew M, et al. Assessing the evaluability of complex public health interventions: five questions for researchers, funders, and policymakers. Milbank Q 2011;89:206–25. 10.1111/j.1468-0009.2011.00626.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.McGill E, Marks D, Er V, et al. Qualitative process evaluation from a complex systems perspective: a systematic review and framework for public health evaluators. PLoS Med 2020;17:e1003368. 10.1371/journal.pmed.1003368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hogan DR, Stevens GA, Hosseinpoor AR, et al. Monitoring universal health coverage within the sustainable development goals: development and baseline data for an index of essential health services. Lancet Glob Health 2018;6:e152–68. 10.1016/S2214-109X(17)30472-2 [DOI] [PubMed] [Google Scholar]
- 96.Thomson S, Cylus J, Evetovits T. Can people afford to pay for health care? New evidence on financial protection in Europe. Copenhagen: World Health Organization, Regional Office for Europe, 2019. https://apps.who.int/iris/bitstream/handle/10665/311654/9789289054058-eng.pdf?sequence=1&isAllowed=y [Google Scholar]
- 97.Rodney AM, Hill PS. Achieving equity within universal health coverage: a narrative review of progress and resources for measuring success. Int J Equity Health 2014;13:72. 10.1186/s12939-014-0072-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Amri MM, Jessiman-Perreault G, Siddiqi A, et al. Scoping review of the world Health organization's underlying equity discourses: apparent ambiguities, inadequacy, and contradictions. Int J Equity Health 2021;20:70. 10.1186/s12939-021-01400-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Green S, Higgins JPT, Schünemann HJ, et al. Response to paper by Lang a, Edwards N, and Fleiszer a. J Clin Epidemiol 2007;60:598–9. 10.1016/j.jclinepi.2007.02.001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-052041supp001.pdf (104.4KB, pdf)
Data Availability Statement
Data sharing not applicable as no datasets generated and/or analysed for this study. This work analysed secondary sources, which are cited and are accessible publicly or with academic institutional credentials. Search strategies are provided in the online supplemental material.