Abstract
Objectives
The objective of our systematic review was to identify the effective interventions to prevent or mitigate social isolation and/or loneliness in older adults who experienced a fall.
Design
Systematic review.
Data sources
MEDLINE, Embase, the Cochrane Central Register of Controlled Trials and Ageline were searched (from inception to February 2020).
Methods
Studies were eligible if they described any intervention for social isolation in older adults living in a community setting who experienced a fall, and reported outcomes related to social isolation or loneliness.
Two independent reviewers screened citations, abstracted data and appraised risk of bias using the Cochrane risk of bias tool. The results were summarised descriptively.
Results
After screening 4069 citations and 55 full-text articles, four studies were included. The four studies varied in study design, including a randomised controlled trial, non-randomised controlled trial, an uncontrolled before-after study and a quasiexperimental study. Interventions varied widely, and included singing in a choir, a patient-centred, interprofessional primary care team-based approach, a multifactorial assessment targeting fall risk, appropriate medication use, loneliness and frailty, and a community-based care model that included comprehensive assessments and multilevel care coordination. Outcome measures varied and included scales for loneliness, social isolation, social interaction, social networks and social satisfaction. Mixed results were found, with three studies reporting no differences in social isolation or loneliness after the intervention. Only the multifactorial assessment intervention demonstrated a small positive effect on loneliness compared with the control group after adjustment (B=−0.18, 95% CI −0.35 to −0.02).
Conclusions
Few studies examined the interventions for social isolation or loneliness in older adults who experienced a fall. More research is warranted in this area.
PROSPERO registration number
CRD42020198487.
Keywords: rehabilitation medicine, geriatric medicine, preventive medicine
Strengths and limitations of this study.
We conducted a comprehensive search of four databases, using a search strategy which was peer reviewed by a second librarian, and supplemented this by searching grey literature and scanning references of included studies and relevant reviews.
We followed the methodology outlined by the Cochrane Handbook, with screening, data abstraction and risk of bias appraisal being conducted in duplicate by independent reviewers, and our findings were reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses 2020 checklist.
We deviated from our protocol slightly due to the limited data on older adults in a community setting who had experienced a fall and expanded our inclusion criteria to include studies where some participants (not all) had a history of falling.
Our included studies were plagued by risk of bias across several components, including poor allocation concealment, lack of random sequence generation and a lack of blinding of participants, personnel and outcome assessors.
A lack of standardisation was observed across the outcomes assessed in the included studies due to lack of consensus on measures for social isolation and loneliness.
Introduction
Worldwide, more than 37 million falls occur requiring medical attention every year.1 Almost 650 000 people die every year from a fall, with those aged 65 years and older experiencing the greatest number of fatal falls.1 Falls are associated with considerable negative outcomes on older adults, such as physical inactivity, anxiety, depressive symptoms and fear of falling.2 3
Social isolation is a serious consequence among older adults who have experienced a fall.4 Social isolation is a complex phenomenon that can be characterised by five key attributes: decreased number of social contacts, decreased feeling of belonging, reduced or lack of fulfilling relationships, decreased engagement with others and reduced quality of the members in one’s network.5 Loneliness is another consequence that may occur after a fall and can be defined as ‘the unpleasant experience that occurs when a person’s network of social relations is deficient in some way, either quantitatively or qualitatively’.6 Some research has focused on the risk of social isolation and loneliness after experiencing a fall, since people who have experienced a fall are less likely to continue their activities of daily living.4 For example, one study reported a statistically significant relationship between feelings of loneliness and social exclusion after experiencing a fall.4
Although social isolation and loneliness are related, it is important to note that they are two distinct concepts.7 Social isolation is more objective, as it can be measured by examining the presence or absence of relationships with other people, whereas loneliness is a person’s subjective experience and is more difficult to measure. This distinction is important, as different interventions might be required for each of these outcomes after experiencing a fall.
Social isolation and loneliness among older adults is associated with many adverse health outcomes, including cognitive decline, depression, anxiety and dementia.8 Interventions to mitigate social isolation and loneliness after older adults experience a fall are of paramount importance. Examples of interventions may include participating in social activities, outreach calls from peers or healthcare workers and group exercise. We are unaware of a previous systematic review that examined this important issue. As such, the objective of our systematic review was to identify the effective interventions to mitigate social isolation and loneliness in older adults who lived independently in a community setting with a history of falling.
Methods
Protocol
The protocol for this systematic review was developed in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) checklist, with consultation from knowledge users from the Public Health Agency of Canada who commissioned this work and clinical experts on the team and was registered on PROSPERO. This systematic review was conducted according to the methodology outlined in the Cochrane Handbook,9 and the PRISMA checklist (online supplemental file 1) was used to guide the reporting of our results.10
bmjopen-2021-056540supp001.pdf (39.2KB, pdf)
Search strategy and selection criteria
A comprehensive literature search strategy was developed by an experienced information specialist and peer reviewed by a second information specialist using the Peer Review of Electronic Search Strategies checklist.11 MEDLINE, Embase, the Cochrane Central Register of Controlled Trials and Ageline were searched from inception until 25 February 2020 (online supplemental appendix 1). The reference lists of included studies and relevant reviews were also scanned. A search for grey literature was conducted using the Canadian Agency for Drugs and Technologies in Health’s Grey Matters checklist.12
bmjopen-2021-056540supp002.pdf (142.9KB, pdf)
Our eligibility criteria are summarised in table 1. Studies were eligible for inclusion if they described any intervention for social isolation or feelings of loneliness in older adults (mean age 65 years and older) with any participant reporting a history of falling (ie, regardless of the proportion of the sample who fell). The knowledge users from the Public Health Agency of Canada requested that we focus this systematic review on participants who lived independently in a community setting. Eligible study designs included randomised controlled trials (RCTs), cohort studies, case–control studies, non-RCTs, quasiexperimental studies, interrupted time series or controlled/uncontrolled before-after studies. Case reports, case series, cross-sectional studies, qualitative studies and reviews were not eligible for inclusion. Outcomes of interest included any changes in social isolation or loneliness as measured using validated scales, such as the De Jong Gierveld Loneliness Scale13 and the Bude and Lantermann Scale for social exclusion,14 or any other quantitative measure of social isolation or loneliness. Social isolation was defined as a decrease in the number of social contacts, decreased feeling of belonging, reduced or lack of fulfilling relationships, decreased engagement with others and reduced quality of the members in one’s network.5 Loneliness was defined as ‘the unpleasant experience that occurs when a person’s network of social relations is deficient in some way, either quantitatively or qualitatively’.6
Table 1.
Screening eligibility criteria
| Population | Older adults (mean age 65 years and older) living independently in a community setting with any participant reporting a history of falling (ie, regardless of the proportion of the sample who fell) |
| Intervention | Any intervention for social isolation or loneliness |
| Comparator | Usual care or another intervention for social isolation or loneliness |
| Outcomes | Any quantitative measures of changes in social isolation or loneliness Examples: the quantity of social interactions, Lubben Social Network Scale for social isolation, De Jong Gierveld Loneliness Scale, Bude and Lantermann Scale for social exclusion, etc |
| Study designs | Randomised controlled trial (RCT), non-RCT, quasiexperimental, interrupted time series, controlled or uncontrolled before-after studies, case–control studies, cohort studies |
| Time | No time restrictions |
All citations were screened by independent reviewers who worked in pairs after the entire team completed a training exercise on 50 citations and 78% agreement was achieved. Full-text screening by independent reviewers who worked in pairs began after a training exercise on 22 articles among the team with an agreement of 75%. Discrepancies for both levels of screening were resolved by a third reviewer or through discussion.
Data abstraction and risk of bias appraisal
Data abstraction and risk of bias appraisal were also conducted independently by reviewers who worked in pairs after a training pilot exercise reached sufficient agreement, and discrepancies were resolved by a third reviewer. The risk of bias appraisal was conducted using the Cochrane Effective Practice and Organisation of Care risk of bias tool, as it was expected that a mixture of study designs would be included.15
Synthesis
The findings of this review were summarised descriptively, reporting study and patient characteristics, quality appraisal assessment and intervention details. As outlined in our review protocol, we planned to conduct a meta-analysis if more than one study evaluated the same intervention, and a network meta-analysis for connected networks of trials with prespecified intervention nodes if over 10 trials were available and the number of trials was greater than the number of interventions. However, as these conditions were not met, no statistical analyses were conducted.
Patient and public involvement
A patient partner with previous experience of a fall was identified and involved in this study from the protocol development stage. The patient partner provided input on our research question and outcome measures to ensure that the patient perspective was incorporated. They also participated in the screening training exercises for citations and full-text articles, provided feedback on screening eligibility criteria and reviewed the manuscript as a coauthor (JB).
Results
Study flow
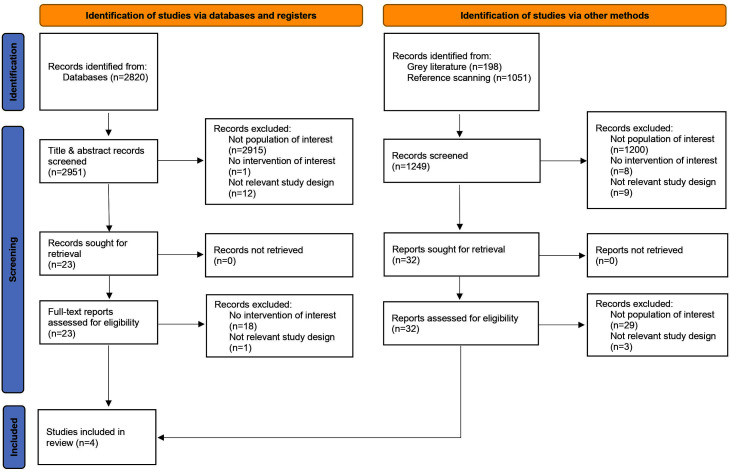
After screening 4069 citations and 55 full-text articles against our eligibility criteria, four studies16–19 met the eligibility criteria and were included in this review (figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) study flow of included studies (n=4).
Study and patient characteristics
Study and patient characteristics are summarised in table 2 and detailed characteristics are reported in online supplemental appendices 2 and 3. The mean age of participants across included studies was 77.8 years (range: 76–79.6 years). Three of the included studies were conducted in North America (75.0%) and one in Europe (25.0%), and they were conducted in a variety of settings including the community setting, a combination of participant homes and community setting, a combination of primary care and community setting or a combination of participant homes and primary care. Only one study provided data on frailty of the included participants, reporting 20.2% of participants with frailty (online supplemental appendix 3). The four studies varied in study design, including an RCT, a non-RCT, an uncontrolled before-after study and a quasiexperimental study in which data from one randomised site were combined with data from four controlled before-after sites. Two of the studies had a study duration of 12 months, and the other two had a duration of 6 months. The sample size in the studies ranged from 21 to 2325 and, on average, 71.3% of participants were female.
Table 2.
Study and patient characteristics
| Summary characteristics | |
| Mean age (range) | 77.8 (76–79.6)* |
| Mean % of female participants (range) | 71.3 (60.8–91)† |
| Mean sample size (range) | 837.3 (21–2325) |
| Mean % of participants living alone (range) | 52.6 (38.1–67)* |
| Mean % of participants with a history of falling (range) | 19.6 (9.3–30.2)* |
| Individual study details | |
|
Cohen et al16 → Chorale intervention Country of conduct: USA Study design: non-randomised controlled trial Study duration: 12 months Sample size: 166 Intervention setting: community | |
|
Scharlach et al17 → ElderHelp Concierge Club (CC) intervention Country of conduct: USA Study design: uncontrolled before-after study Study duration: 6 months Sample size: 21 Intervention setting: participant homes and community | |
|
Franse et al18 → Urban Health Centres Europe (UHCE) approach Country of conduct: UK, Greece, Croatia, the Netherlands, Spain Study design: quasiexperimental (one site randomised, four sites controlled before-after studies) Study duration: 12 months Sample size: 2325 Intervention setting: primary care and community settings | |
|
Dolovich et al19 → Health Teams Advancing Patient Experience: Strengthening Quality (Health TAPESTRY) intervention Country of conduct: Canada Study design: randomised controlled trial Study duration: 6 months Sample size: 312 Intervention setting: participant homes and primary care | |
*Only two of four studies reported on these variables.
†Only three of four studies reported on this variable.
Risk of bias results
An overall summary of risk of bias across the four studies can be found in online supplemental appendix 4, and detailed risk of bias assessments can be found in online supplemental appendix 5. All studies had low risk of bias for baseline outcome measurements (100% low, 0% unclear, 0% high) and other bias (mainly funding bias; 100% low, 0% unclear, 0% high). Two of the studies had low risk and two had unclear risk of bias for selective reporting (50% low, 50% unclear, 0% high). One study had high risk, two studies had unclear risk and one had low risk of bias for incomplete outcome data (25% low, 50% unclear, 25% high). However, three of four studies had high risk of bias for blinding of outcome assessment (25% low, 0% unclear, 75% high), blinding of participants and personnel (25% low, 0% unclear, 75% high), random sequence generation (25% low, 0% unclear, 75% high) and allocation concealment (25% low, 0% unclear, 75% high).
Outcome results
The relevant findings from the four included studies are summarised in online supplemental appendix 6. Cohen et al16 conducted a non-RCT in the USA assessing the effects of singing in a chorale to reduce loneliness compared with usual care in 166 older adults. The chorale intervention involved attendance at weekly singing rehearsals and several public performances, while the usual care group continued their usual activities. Both groups had a similar baseline history of falling over the past 12 months (average of 0.40 falls per person in the intervention group and 0.36 falls per person in the control group). After 12 months of follow-up, they noted a reduction in loneliness (as measured using the University of California, Los Angeles (UCLA) Loneliness Scale III) in both groups (chorale: baseline mean 35.1 (SD 8.1) and follow-up mean 34.6 (SD 7.9); usual care: baseline mean 38.3 (SD 10.1) and follow-up mean 37.0 (SD 10.3)). While the chorale intervention reported lower loneliness scores than the usual care group after 12 months of follow-up, no statistically significant difference was observed (F(1,126)=3.08; p=0.08).
Scharlach et al17 conducted an uncontrolled before-after study in the USA assessing the effectiveness of their ElderHelp Concierge Club intervention on social isolation in a sample of 21 participants. The Concierge Club intervention was a community-based care model that provided different tiers of services to their members including information and referrals, transportation or in-house assessments. The baseline mean number of falls over the past 6 months was 1.3. They noted that social isolation, as measured using an unnamed three-item scale,20 did not change significantly after 6 months of follow-up (baseline mean: 8.7 (SD 3.2) and follow-up mean: 7.0 (SD 3.8)). Similarly, although all participants reported having contact with friends/relatives after the intervention, this was not found to be a significant change from baseline (baseline: 76% of participants, follow-up: 100% of participants).
Franse et al18 conducted a quasiexperimental study comparing the effectiveness of the Urban Health Centres Europe (UHCE) approach to usual care on loneliness in a sample of 1844 older adults across the UK, Greece, Croatia, the Netherlands and Spain. The UHCE approach involved a preventative multidimensional health assessment, which informed the coordination of specific care pathways targeting the individual’s needs (such as fall risk, appropriate medication use, loneliness and frailty). The usual care group received their usual care and had access to any already existing services. At baseline, 30.2% of participants reported having experienced a fall in the past 12 months. Their adjusted analysis found a small positive effect of the UHCE approach on loneliness, as measured using the short De Jong Gierveld Loneliness Scale,21 when compared with usual care (B=−0.18, 95% CI −0.35 to −0.02).
Dolovich et al19 conducted an RCT comparing the effectiveness of the Health Teams Advancing Patient Experience: Strengthening Quality (Health TAPESTRY) intervention to usual care on social isolation in a sample of 312 older adults in Canada. This intervention involved the collection of information on patients’ health goals and needs by trained volunteers, who then summarised these findings in a report for the interprofessional primary care team. The primary care team used these reports to generate and act on plans of care for how the team, community agencies and volunteers could help address each patient’s goals. The control group received usual care. Approximately 9.3% of participants reported experiencing at least one fall. After 6 months of follow-up, they found no statistically significant difference between the intervention and control groups in terms of their social network scores (mean difference 0.038; 95% CI –0.25 to 0.33) and social satisfaction scores (mean difference 0.102; 95% CI –0.35 to 0.55), as measured using the Duke Social Support Index.22
Discussion
We conducted a comprehensive systematic review of interventions to mitigate social isolation and loneliness in older adults living independently in a community setting who experienced a fall. Very few studies were identified that fulfilled our eligibility criteria, indicating a dearth of evidence on this important topic. Only four studies were included and as each examined the different types of interventions, this precluded any statistical pooling of results. Furthermore, studies varied on the proportion of participants who reported experiencing a fall, and multiple types of outcomes were assessed for loneliness and social isolation, making it challenging to provide any meaningful interpretation of results.
Across the four studies in this systematic review, only the quasiexperimental study by Franse et al,18 which assessed the impact of multifactorial health assessments and coordinated care pathways targeting fall risk, medication use, loneliness and frailty, found a small positive effect on loneliness (ie, reduction) when comparing those who received the intervention with the control group. However, given the paucity of data in older adults with a history of falling, the most effective intervention for preventing or reducing social isolation remains unclear. Only one RCT was identified in this review, highlighting the need for more robust research in this important area.
We searched for previous reviews that were related and only one was identified. Gardiner et al conducted an integrative review on interventions for social isolation in older adults.23 While this review was not specific to individuals who had experienced a fall, it discusses characteristics of effective social isolation interventions in the broader older adult population and could be applicable to the subset of this population that experiences falling. While the majority of interventions they identified showed at least a moderate positive effect on social isolation or loneliness, they noted that the quality of the evidence was poor, making it difficult to identify a particular intervention as most effective.23 This is consistent with our determination of the need for more robust research on the effectiveness of social isolation interventions in older adults with a history of falling. They identified adaptability to local contexts, community participation in the design and implementation of the intervention, and productive engagement (as opposed to passive activities) as common features among successful interventions.23 Future studies should consider these factors in the development and evaluation of interventions for social isolation. Finally, we focused on the community setting at the request of the Public Health Agency of Canada who felt that these results were most relevant to their decision-making needs.
Across our included studies, all four interventions appeared to be adapted to their local contexts. The UHCE approach by Franse et al18 and the Health TAPESTRY intervention by Dolovich et al19 also involved strong community participation by tailoring their intervention to each participant’s healthcare needs; however, it is unclear whether the subsequent care pathways or plans allowed for productive engagement. Cohen et al’s16 chorale intervention provided productive engagement to participants but may have benefited from further community participation in the implementation of the intervention.
There are many strengths to our systematic review. Our search strategy was peer reviewed by a second librarian and was comprehensive through the inclusion of four databases, searching grey literature and scanning references of included studies and relevant reviews. Our methodology was informed by the Cochrane Handbook,9 with screening, data abstraction and risk of bias appraisal being conducted in duplicate by independent reviewers, and our findings were reported using PRISMA 2020.10 However, there are some limitations. We deviated from our protocol slightly to allow for inclusion of studies where only some participants had a history of falling, given the paucity of data on older adults in a community setting who had experienced a fall. We were unable to update our literature search due to a lack of sufficient funding. Further, studies were plagued by risk of bias across several components, including the risk of bias from poor allocation concealment, lack of random sequence generation and a lack of blinding of participants, personnel and outcome assessors. A lack of standardisation was observed across the outcomes assessed in the included studies, suggesting that future work could focus on developing consensus on measures for social isolation and loneliness that have already been validated to establish a core outcome data set. Indeed, a study by Cornwell and Waite24 highlights the wide variation in indicators for isolation and loneliness and proposed combining these varying indicators to develop two parsimonious scales to measure social disconnectedness and perceived isolation24; however, these scales were not used by the included studies here. Furthermore, additional examination of tailoring interventions to reduce loneliness and/or social isolation is warranted, as there was a dearth of included studies to examine this fully in this systematic review with two studies each focusing on social isolation and loneliness separately. Further research is warranted on this, as social isolation and loneliness are distinct concepts and different interventions may be required to target each outcome separately. Finally, we focused our review on the community setting at the request of the Public Health Agency of Canada and our results might not be applicable to all older adults living in other settings.
We recommend updating this systematic review as more literature becomes available on this topic. Effective interventions are necessary to support older people who are at increased risk of social isolation, particularly after experiencing a fall. In addition, further work is required to examine the relationship between social isolation, loneliness and falling, and whether other variables influence this relationship, as this may warrant different intervention approaches.
In conclusion, we identified four studies examining the interventions for social isolation among older adults with a history of falling. The interventions examined varied widely from singing in a chorale to community-based care coordination, as did the outcome measures used to assess the effectiveness of the interventions. We identified only one quasiexperimental study which demonstrated that multifactorial health assessments and coordinated care pathways resulted in a small positive effect on loneliness in this population. Future research is warranted in this understudied area.
Supplementary Material
Acknowledgments
We thank Jessie McGowan for developing our search strategies, Tamara Rader for peer reviewing the search strategies (PRESS) and Alissa Epworth for running the searches, deduplicating the results and obtaining full-text articles. We thank Joanne Bowater for her input during the earlier stages of the project. Finally, we thank Katrina Chiu, Navjot Mann and Faryal Khan for their support with formatting the manuscript and creating tables and appendices.
Footnotes
Twitter: @GaryMitchellRN
Contributors: Substantial contributions to the conception or design of the work: ACT, SMT, JW, SES. Acquisition, analysis or interpretation of data for the work: all authors. Drafting the work: ACT, SMT. Revising the work critically for important intellectual content: AR, NR, GM, JF, YJ, MdG, KA, JB, AG-B, JW, SES. Final approval of the version to be published: all authors. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: all authors. ACT accepts full responsibility for the conduct of the study as guarantor, had access to the data, and controlled the decision to publish.
Funding: This work was funded through the Strategy for Patient-Oriented Research (SPOR) Evidence Alliance. The SPOR Evidence Alliance is supported by the Canadian Institutes of Health Research (CIHR) under Canada’s Strategy for Patient-Oriented Research (SPOR) initiative, and the generosity of partners from 41 public agencies and organisations across Canada who have made cash or in-kind contributions. ACT is funded by a Tier 2 Canada Research Chair in Knowledge Synthesis. SES is funded by a Tier 1 Canada Research Chair in Knowledge Translation. GM and JF were in part supported by the Health Research Board (Ireland) and the HSC Public Health Agency (Grant number CBES-2018-001) through Evidence Synthesis Ireland and Cochrane Ireland. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Competing interests: None declared.
Patient and public involvement statement: Patients and/or the public were involved in the design, or conduct, reporting or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. The full data set is available from the corresponding author upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study does not involve human participants.
References
- 1.WHO . Falls, 2018. Available: https://www.who.int/news-room/fact-sheets/detail/falls
- 2.Terroso M, Rosa N, Torres Marques A, et al. Physical consequences of falls in the elderly: a literature review from 1995 to 2010. Eur Rev Aging Phys Act 2014;11:51–9. 10.1007/s11556-013-0134-8 [DOI] [Google Scholar]
- 3.Petersen N, König H-H, Hajek A. The link between falls, social isolation and loneliness: a systematic review. Arch Gerontol Geriatr 2020;88:104020. 10.1016/j.archger.2020.104020 [DOI] [PubMed] [Google Scholar]
- 4.Hajek A, König H-H. The association of falls with loneliness and social exclusion: evidence from the DEAS German ageing survey. BMC Geriatr 2017;17:204. 10.1186/s12877-017-0602-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nicholson NR. Social isolation in older adults: an evolutionary concept analysis. J Adv Nurs 2009;65:1342–52. 10.1111/j.1365-2648.2008.04959.x [DOI] [PubMed] [Google Scholar]
- 6.Perlman D, Peplau LA. Toward a social psychology of loneliness. Pers Relatsh 1981;3:31–56. [Google Scholar]
- 7.de Jong Gierveld J, Van Tilburg T, Dykstra PA. Loneliness and social isolation. In: Cambridge Handbook of personal relationships, 2006: 485–500. [Google Scholar]
- 8.National Academies of Sciences, Engineering, and Medicine . Social isolation and loneliness in older adults: opportunities for the health care system. Washington, DC: National Academies Press,, 2020: 316 p. [PubMed] [Google Scholar]
- 9.Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for systematic reviews of interventions version 6.1. Cochrane, 2020. www.training.cochrane.org/handbook [Google Scholar]
- 10.Page MJ, McKenzie JE, Bossuyt PM, et al. Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. J Clin Epidemiol 2021;134:103–12. 10.1016/j.jclinepi.2021.02.003 [DOI] [PubMed] [Google Scholar]
- 11.McGowan J, Sampson M, Salzwedel DM, et al. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J Clin Epidemiol 2016;75:40–6. 10.1016/j.jclinepi.2016.01.021 [DOI] [PubMed] [Google Scholar]
- 12.Wishart DS, Feunang YD, Guo AC, et al. DrugBank 5.0: a major update to the DrugBank database for 2018. Nucleic Acids Res 2018;46:D1074–82. 10.1093/nar/gkx1037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gierveld JDJ, Tilburg TV. A 6-Item Scale for Overall, Emotional, and Social Loneliness:Confirmatory Tests on Survey Data. Research on Aging 2006;28:582–98. 10.1177/0164027506289723 [DOI] [Google Scholar]
- 14.Bude H, Lantermann E-D. Soziale exklusion und exklusionsempfinden. Kolner Z Soz Sozpsychol 2006;58:233–52. 10.1007/s11575-006-0054-1 [DOI] [Google Scholar]
- 15.Cochrane Effective Practice and Organisation of Care (EPOC) . Epoc resources for review authors, 2017. Available: https://epoc.cochrane.org/sites/epoc.cochrane.org/files/public/uploads/Resources-for-authors2017/suggested_risk_of_bias_criteria_for_epoc_reviews.pdf
- 16.Cohen GD, Perlstein S, Chapline J, et al. The impact of professionally conducted cultural programs on the physical health, mental health, and social functioning of older adults. Gerontologist 2006;46:726–34. 10.1093/geront/46.6.726 [DOI] [PubMed] [Google Scholar]
- 17.Scharlach AE, Graham CL, Berridge C. An integrated model of co-ordinated community-based care. Gerontologist 2015;55:677–87. 10.1093/geront/gnu075 [DOI] [PubMed] [Google Scholar]
- 18.Franse CB, van Grieken A, Alhambra-Borrás T, et al. The effectiveness of a coordinated preventive care approach for healthy ageing (UHCE) among older persons in five European cities: a pre-post controlled trial. Int J Nurs Stud 2018;88:153–62. 10.1016/j.ijnurstu.2018.09.006 [DOI] [PubMed] [Google Scholar]
- 19.Dolovich L, Oliver D, Lamarche L, et al. Combining volunteers and primary care teamwork to support health goals and needs of older adults: a pragmatic randomized controlled trial. CMAJ 2019;191:E491–500. 10.1503/cmaj.181173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hughes ME, Waite LJ, Hawkley LC, et al. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging 2004;26:655–72. 10.1177/0164027504268574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.De Jong Gierveld J, Van Tilburg T. The de Jong Gierveld short scales for emotional and social loneliness: tested on data from 7 countries in the un generations and gender surveys. Eur J Ageing 2010;7:121–30. 10.1007/s10433-010-0144-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wardian J, Robbins D, Wolfersteig W, et al. Validation of the DSSI-10 to measure social support in a general population. Res Soc Work Pract 2013;23:100–6. 10.1177/1049731512464582 [DOI] [Google Scholar]
- 23.Gardiner C, Geldenhuys G, Gott M. Interventions to reduce social isolation and loneliness among older people: an integrative review. Health Soc Care Community 2018;26:147–57. 10.1111/hsc.12367 [DOI] [PubMed] [Google Scholar]
- 24.Cornwell EY, Waite LJ. Measuring social isolation among older adults using multiple indicators from the NSHAP study. J Gerontol B Psychol Sci Soc Sci 2009;64 Suppl 1:i38–46. 10.1093/geronb/gbp037 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-056540supp001.pdf (39.2KB, pdf)
bmjopen-2021-056540supp002.pdf (142.9KB, pdf)
Data Availability Statement
Data are available upon reasonable request. The full data set is available from the corresponding author upon reasonable request.