Abstract
Identifying signaling pathways and molecules involved in SARS-CoV-2 pathogenesis is pivotal for developing new effective therapeutic or preventive strategies for COVID-19. Pannexins (PANX) are ATP-release channels in the plasma membrane essential in many physiological and immune responses. Activation of pannexin channels and downstream purinergic receptors play dual roles in viral infection, either by facilitating viral replication and infection or inducing host antiviral defense. The current review provides a hypothesis demonstrating the possible contribution of the PANX1 channel and purinergic receptors in SARS-CoV-2 pathogenesis and mechanism of action. Moreover, we discuss whether targeting these signaling pathways may provide promising preventative therapies and treatments for patients with progressive COVID-19 resulting from excessive pro-inflammatory cytokines and chemokines production. Several inhibitors of this pathway have been developed for the treatment of other viral infections and pathological consequences. Specific PANX1 inhibitors could be potentially included as part of the COVID-19 treatment regimen if, in future, studies demonstrate the role of PANX1 in COVID-19 pathogenesis. Of note, any ATP therapeutic modulation for COVID-19 should be carefully designed and monitored because of the complex role of extracellular ATP in cellular physiology.
Keywords: ATP, COVID-19, Drug repurposing, Pannexins, Purinergic receptors, SARS-CoV-2
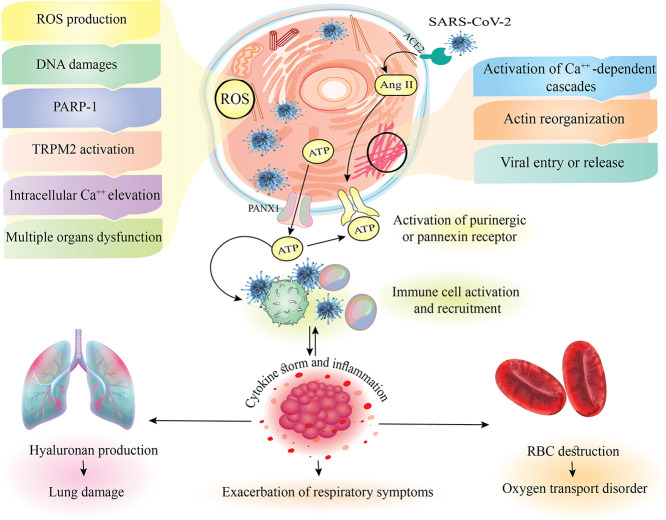
Graphical abstract
1. Introduction
At the beginning of 2020, a new virus with an unknown source was found in the bronchoalveolar lavage of a person affected by pneumonia. It was named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by the International Committee on Taxonomy of Viruses. The related disease, which is spread via contact with affected individuals or fluids, has been named 2019 Coronavirus Disease (COVID-19) [1], [2], and the World Health Organization (WHO) declared it as a pandemic on March 11, 2020 [1], [2], [3].
Because of the lack of effective medicines or preventive strategies for COVID-19, the identification of signaling pathways important for COVID-19 pathogenesis is essential for developing novel effective treatments. Pannexins (PANX) are mammalian vertebrate ATP (adenosine triphosphate)-release channels, consisting of three proteins (PANX1, 2, and 3), among which PANX1 being the most ubiquitously expressed [4], [5], [6].
There is a high concentration of ATP in the cell cytoplasm in normal physiological conditions, which can be released in response to pathological, mechanical, temperature, or ischemic stress, or secretion via pannexin and connexin hemichannels. The release of ATP in response to the activation of the PANX1 channel enables increases in extracellular ATP that facilitates calcium and potassium fluxes [6], [7], [8]. PANX1 channel activation during pathological conditions occurs due to cleavage of its C-terminal tail by caspases [6], increased intracellular Ca2+, and extracellular K+, hypoxia, immune responses, and airway defense [6], [9], [10], [11]. It has been shown that cystic fibrosis transmembrane conductance regulator (CFTR), which its homozygous gene mutations result in clinical cystic fibrosis (CF), modulates PANX1-mediated ATP release through bicarbonate entry. Upon bicarbonate entry, ATP and cytochrome c release from mitochondria is stimulated, leading to cytochrome c activation of caspase 3, which in turn activates PANX1 and ATP is released into the extracellular compartment through the opened PANX1 channel [12].
PANX1 channel regulation is also achieved through interactions with purinergic 2 (P2) receptors classified into P2X1–7 and P2Y1, 2, 4, 6, 11, 12, 13, 14. [13], [14], [15]. When the PANX1 channel is opened, signaling molecules such as ATP are released into the extracellular space, resulting in the activation of purinergic receptors. These receptors can detect ATP and other nucleotides, including ADP, UTP, and UDP, to activate intracellular signaling events [10], [11].
A growing body of data suggests that a cascade of ATP release through the PANX1 channel and purinergic receptors activation play dual roles, resulting in viral infection and replication and induction of inflammatory and antiviral responses contributing to the host antiviral defense. The level of ATP release from pannexin channels determines the outcome: minor and massive release of ATP in normal and pathogenic conditions, respectively [6], [16]. Homeostatic cell function depends on low levels of extracellular ATP and K+. By contrast, under pathological conditions, high levels of extracellular ATP and K+ and high concentration of Ca2+ in the intracellular space result in overactivation of the PANX1-P2X7 complex contributing to inflammation and inducing Caspase 1/11-dependent pyroptotic cell death (Fig. 1 ) [6].
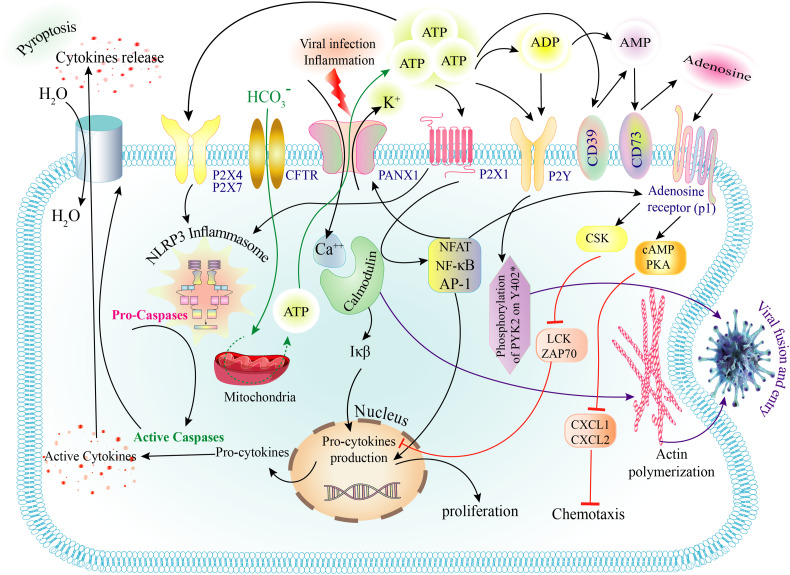
Fig. 1.
Purinergic receptors, downstream signaling and their role in the pathogenesis of viral infections. Viral infection and inflammation stimulate Panx1 and the release of ATP and K+ and the entry of Ca++. On the other hand, bicarbonate enters the cell through CFTR and during a series of steps in the mitochondria leads to increased ATP production, which leaves the cell through Panx1 channel. ATP and ADP bind to P2Y and P2X receptors. AMP produced by CD39 is also converted to adenosine by binding to CD73. On the other hand, the binding of intracellular Ca++ to calmodulin activates IkB, which in turn produces the precursor of inflammatory cytokines. Ca++-calmodulin activates NFAT, NF-κB and AP-1 transcription factors. These factors also activate the AR following adenosine binding. Activation of this receptor inhibits inflammatory cytokines and chemotaxis by activating CSK, CAMP, and PKA and inhibiting LCK, ZAP70, CXCL1, and CXCL2. The binding of ATP to P2X4 and P2X7 activates the NLRP3 inflammasome. NLRP3 converts pro-capsases to active caspases. Active caspases convert the precursor of cytokines to the active form. Cytokines are then released from the cell via gasdermin and pyroptosis occurs. Activation of the P2Y receptor by PYK2 phosphorylation and Ca++-calmodulin complex by actin polymerization causes the virus entry. ADP, Adenosine diphosphate; AMP, Adenosine monophosphate; AP-1, Activator protein 1; AR, adenosine receptor; ATP, Adenosine triphosphate; CAMP, Cyclic adenosine monophosphate; CFTR, Cystic fibrosis transmembrane conductance regulator; CSK, C-Terminal Src Kinase; CXCL1, C-X-C motif ligand 1; GSDMD, Gasdermin D; Iκβ, I-kappa-B; LCK, lymphocyte specific protein tyrosine kinase; NFAT, Nuclear factor of activated T-cells; NF-κB, Nuclear factor kappa B; NLRP3, NOD-like receptors family pyrin domain containing 3; Panx1, Pannexin 1; PKA, protein kinase A; ZAP70, Zeta Chain Of T Cell Receptor Associated Protein Kinase 70.
Of note, ATP can be converted to adenosine in two steps with the help of CD39 and CD73 ectonucleotidases [17]. Adenosine applies its various effects through the interaction with four subtypes of adenosine receptors (AR) [18], Among them, A2A subtype mainly mediates the anti-inflammatory action of adenosine [19]. Due to the well-recognized anti-inflammatory action of adenosine and lack of specific antiviral treatment for COVID-19, Caracciolo et al. hypothesized that adenosine treatment may decrease inflammation and cytokine storm in COVID-19 patients. The use of inhaled adenosine in COVID19 patients resulted in the reduction of length of stay and SARS-CoV-2 positive days. An improvement in arterial oxygen partial pressure (PaO2)/fractional inspired oxygen (FiO2) as well as a decrease in inflammation parameters such as C-reactive protein (CRP) levels was furthermore evident upon adenosine treatment [20].
Upon viral infection, PANX1 channels trigger the release of high amounts of ATP from the cells, serving as pro-inflammatory or danger-associated molecular patterns (DAMPs) through purinergic receptor signaling and recruiting the immune cells to damaged cells/tissues to start/amplify defensive responses [14], [21].
Thus, in this review, we discuss the possible contribution of extracellular ATP, pannexin channels, specially PANX1 and P2 purinergic receptors in the mechanism of action and pathogenesis of SARS-CoV-2 and their potential as promising therapeutic targets in COVID-19 patients.
2. Possible mechanisms of Pannexin 1 channel/purinergic receptors involvement in the COVID-19 pathogenesis
According to recent studies, critical mechanisms involved in the pathogenesis of SARS-CoV-2 include dysregulation of the immune response and cytokines storm, dysregulation of the renin-angiotensin (RAS) signaling pathway, oxidative stress and cell death, and endothelial dysfunction [22]. Here, we hypothesize how the PANX1/purinergic pathway could contribute to the mechanisms of COVID-19 pathogenesis.
2.1. Dysregulation of the immune response and cytokines storm
In the first exposure to the SARS-CoV-2 virus, a well-coordinated and rapid innate immune response is critical to defend against the virus and protect from disease progression to severe stages [23]. PANX1/purinergic receptors signaling has been suggested to mediate the switch between pro- and anti-inflammatory states [6]. They have been reported to have dual roles in viral infections: as proviral as well as antiviral factors [24].
High extracellular ATP release triggers the rapid release of pro-inflammatory mediators. In contrast, low-dose ATP suppresses inflammation due to the induction of dendritic cells, macrophages' activation, and secretion of anti-inflammatory cytokines, including interleukin (IL)-10 and IL-1 receptor antagonist [6].
2.1.1. Proviral responses
Upon binding to eukaryotic cells, many viruses induce low, localized, and regulated extracellular ATP release via the PANX1 channel that could facilitate viral penetration and replication [14]. In the cells infected by viruses, Ca2+-dependent intracellular cascades activated by the purinergic receptors facilitate the formation of membrane ruffles and viral particle endocytosis by triggering actin reorganization [14]. Activation of P2X or P2Y receptors through extracellular ATP is essential for hepatitis B, C, and D viruses, human immunodeficiency virus (HIV), and virus entry into the cells [25]. Extracellular ATP is linked to other events related to the viral infection processes, including release from infected cells, for example, in the case of vesicular stomatitis virus and HIV-1 [26] and is also linked to acute respiratory distress syndrome (ARDS) [27].
There are no known links between extracellular ATP and coronaviruses, including SARS-CoV-2. Membrane fusion through the plasma membrane or at endosomes is recruited by coronaviruses, including SARS-CoV-2, to facilitate their entry into cells through macropinocytosis, clathrin- and caveolin-independent endocytic pathways [28]. PANX1 and P2X7 receptors interactions and their entry into endosomes via a process reminiscent of caveolin- and clathrin-independent endocytosis is initiated by the increased extracellular ATP [27] (Fig. 1).
Pharmacological stimulation of this pathway before viral contact or pretreatment of host cells with high ATP concentrations causes an increase in cell membrane stress and/or cell death; thus, antiviral immunity is enhanced, leading to a reduction in the efficiency of viral infection and replication [14].
2.1.2. Antiviral responses
High doses of extracellular ATP released by virus-infected cells are interpreted as a danger signal to the immune cells to trigger/increase defensive responses [29]. ATP plays a role in the inflammation by the recruitment of components of innate immunity, including monocytes, macrophages, and dendritic cells, into the damaged areas, leading to the upregulation of PANX1 expression and activation of purinergic signaling, thereby facilitating the release of ATP as an inflammatory signaling molecule into the extracellular space (ATP-induced ATP release) [3], [25], [26]. Extracellular ATP contributes to the activation of inflammasome (NLRP3) mediated by the PANX-1/P2X7 receptor (Fig. 1). Moreover, the P2X7 receptor plays a pivotal role in the immunity against viral infections by regulating the secretion of pro-inflammatory mediators including IL-1, IL-6, and IL-18, inducing inflammasome, recruiting immune cells to infected tissues, activating specific T cells, producing reactive oxygen species (ROS) and inducing apoptosis.
However, purinergic receptors can furthermore lead to the direct elimination of viruses through prevention of their replication within the cells and/or by killing infected cells as a result of inflammatory cell death (pyroptosis) [11], [30]. In addition, tumor necrosis factor-alpha (TNF-α) is considered to promote the opening of the PANX1 channel, allowing for extracellular ATP release associated with inflammatory cell recruitment. The opening of PANX1 channels leads to an influx of extracellular Ca2+, which produces a feed-forward effect on NF-κβ (Nuclear factor kappa B), NFAT (Nuclear factor of activated T-cells) and AP-1 (Activator protein 1) to amplify IL-1β synthesis and release by the endothelium to promote the inflammatory response [31] (Fig. 1).
The level of immune system activation determines if this immune response has beneficial or detrimental effects on tissues [14]. A growing body of evidence shows that high extracellular ATP levels result in exacerbation of inflammatory responses through PANX1/P2 receptor activation lead to chronic inflammatory disorders or acute systemic inflammatory reactions such as asthma and septic shock, respectively [32]. For example, during influenza virus infection, activation of P2 receptors due to elevated levels of extracellular ATP worsens immune response, distinguished by the massive production of pro-inflammatory cytokines, induction of apoptosis, the elevation of airway neutrophils and consequently lung disease [30]. Furthermore, the production of several cytokines, including IL-6, IL-1β, IFN-γ, TNF-α, and CXCL-10 involved in SARS-CoV-2 pathogenesis, is mediated via the activation of P2Y2 receptors. Interestingly, IFN-γ is associated with a gene signature proposed in a recent study for SARS-CoV-2 early infection, suggesting a possible role for P2Y2R in the SARS- CoV-2 pathogenesis [33].
Dysregulated innate immunity leading to hyper-inflammation and systemic inflammatory response syndrome (cytokine storm) can have devastating consequences on tissues which are well-known in patients with severe COVID-19 [22]. Hence, in this group of COVID-19 patients displaying hyper-inflammation, immunosuppression treatment could decrease disease progression and viral entry [34], [35]. Disruption (both deletion and inhibition) of the Panx1/P2 receptor is shown to improve animals' survival in the rodent models of ischemia-reperfusion injury as a result of reduced production of inflammatory mediators and decreased neutrophil infiltrations [36], [37], [38], [39], [40].
The SARS-CoV-2 entry has been shown to develop lung inflammatory storm, augmented by smoking [41]. It has been shown that the inflammation induced by cigarette smoke is triggered by the PANX1 channel activation and release of extracellular ATP leading to the activation of P2X7 receptor and inflammasome [42], [43]. On the other hand, there are contradictory and inconclusive data on whether smoking increase or decrease susceptibility to SARS-CoV-2, rate of hospitalization and the severity of the disease [44], [45].
It has been shown that the transient receptor potential (TRP) and pannexin-1 channels have a key role in the smoking-induced dose-related increase in extracellular ATP and induction of airway inflammation [46]. Thus, as a result of viral infection and over-activation of pannexin-1 channel, excessive immune response and consequently serious health consequences are expected. On the other hand, it could be hypothesized that smoking may protect against the COVID-19 due to the protective effect of exposure to high levels of ATP before viral infection and inhibition of virus entry and replication.
2.2. The renin-angiotensin (RAS) signaling pathway
SARS-CoV-2 mainly infects cells through binding to ACE2 (angiotensin-converting enzyme 2) receptors. ACE2 is the enzyme responsible for angiotensin II cleavage to generate angiotensin 1–7, which have antifibrotic, anti-proliferative and vasodilator properties [47]. Attachment of the virus to ACE2 leads to the exhaustion of this receptor, an increase in angiotensin II and inhibition of the vasodilatory activity of angiotensin 1–7 [48], [49]. This process negatively regulates the RAS signaling, which plays a pivotal role in blood pressure regulation, blood vessel permeability, the balance of body fluid and electrolytes and tissue growth, and would lead to exacerbation of inflammatory lung disease [50], [51].
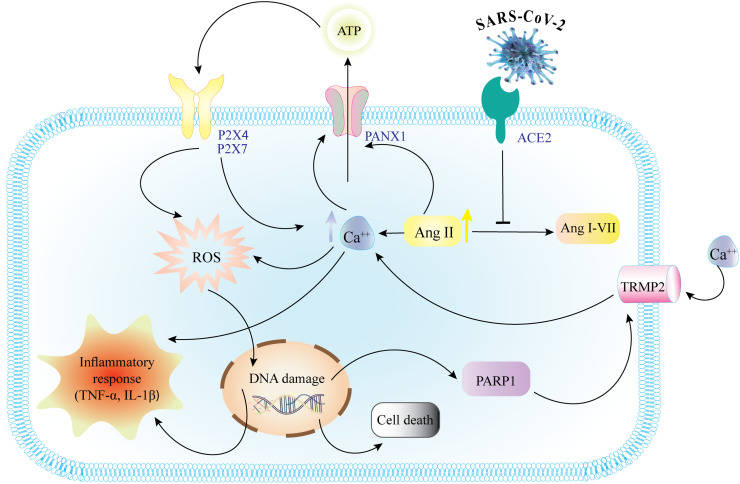
Interestingly, angiotensin II not only causes a dose-dependent activation of PANX1 currents but also causes a sustained increase in intracellular Ca2+, leading to sustained PANX1 channels activity, which releases ATP to the extracellular milieu [52], [53]. In addition, the coexistent increase in intrarenal angiotensin II and activation of PANX1 and subsequently purinergic P2 receptors and Ang II type 1 (AT1) receptors have been considered in pathophysiological conditions such as hypertension. In fact, if the initial angiotensin II-induced alterations in ATP levels are permanent by a constant production and release of ATP, it leads to activation of several signaling pathways promoting oxidative stress and tissue injury as a result of inflammation as it is reported in COVID-19 complications (Fig. 2 ) [53], [54].
Fig. 2.
Inflammatory response through AngII. The binding of ACE2 to the coronavirus prevents the conversion of AngII to AngI-VII and so increases intracellular AngII. AngII stimulates Panx1 to induce ATP release from the cell. Extracellular ATP binds to P2 receptors, increases intracellular Ca++, NF-κB, and ROS. ROS cause DNA damages, producing PARP1 and then TRMP2. TRMP2 also increases intracellular Ca++. Increased intracellular Ca++, NF-κB, and DNA damage trigger inflammatory responses, including the production of cytokines such as TNF-α and IL-1Β. DNA damage also induces cell death. ACE2, Angiotensin-converting enzyme 2; AngII, angiotensin II; ATP, Adenosine triphosphate; IL-1Β, Interleukin 1 Beta; NF-κB, Nuclear factor kappa B; Panx1, Pannexin 1; PARP1, Poly [ADP-ribose] polymerase 1; ROS, Reactive oxygen species; TNF-α, Tumor necrosis factor-alpha; TRMP2, Transient receptor potential cation channel subfamily M member 2.
Accordingly, as PANX1 and angiotensin II-related pathways have an essential role in viral infections and the associated clinical manifestations, more study to identify potential links of these two pathways to COVID-19 pathogenesis is required.
2.3. Oxidative stress and cell death
Free radicals derived from oxygen are essential in biological systems [55]. The disparity between the production and clearance of ROS is called oxidative stress [4]. In response to viral infection, ROS production can be triggered by cytokines and often results in destructive effects [56]. The pathological consequences of oxidative stress through viral infections include damages in macromolecules such as proteins, lipids, and DNA that cause cell death, immune-inflammatory injury, and adverse effects on the function of multiple organs [55], [56], [57].
Overproduction of ROS and disturbance of antioxidant defense have been shown to be involved in the COVID-19 pathogenesis and the severity of its respiratory complications. Researchers have suggested that oxidative stress machinery activation can initiate lung disease in patients with COVID-19. Oxidative stress machinery plays a vital role in the innate immunity and worsens pro-inflammatory host response as a result of activation of transcription factors such as NF-κB [58].
Interestingly, ATP release through PANX1 activates P2 receptors that stimulate Ca2+ influx and production of inflammatory mediators such as ROS, thereby resulting in oxidative stress-related complications [4], [11]. Excessive release of ATP via activated PANX1 channel (resulting from the activation of caspases, DNA damage and oxidative stress) induces some proapoptotic mechanisms [16], [59], [60].
Moreover, DNA damage induces poly (ADP-ribose) polymerase-1 (PARP-1) activation and subsequently transient receptor potential melastatin 2 (TRPM2) activation [61], leading to intracellular Ca2+ elevation [61], [62]. A high level of cytosolic Ca2+ results in PANX1 channel and P2X7 receptor-dependent ATP release, followed by the activation of the P2Y receptor, inducing the DNA damage and apoptosis (Fig. 2) [22], [42], [46], [63]. Therefore, it might be possible to block the PANX1/purinergic pathway components to reduce PANX1/purinergic-mediated oxidative stress and apoptosis, and related pathological consequences during later stages of infection.
2.4. Endothelial dysfunction
Endothelial dysfunction is one of the possible mechanisms of pathogenesis of COVID-19 when the endothelium fails to promote vasodilation, fibrinolysis, and anti-aggregation [64]. This systemic condition induces organ ischemia, increased oxidative stress, inflammation with associated tissue edema, pro-coagulant and anti-fibrinolytic states [65], [66].
Endothelial cell function in health and disease states could be regulated via the ATP release within endothelial cells mediated by the Pannexin channels. Pannexins could also regulate vasodilation and inflammatory cell adhesion in endothelial cells [67]. In this way, inflammatory cells migration into the site of inflammation is facilitated by adhering to the vessel wall. Localization of the PANX1 channel in endothelial cells is promoted by the TNF signaling pathway, resulting in Ca2+ increase and inflammatory cell recruitment [68]. Dysfunction of endothelial cells and the trans-endothelial migration of neutrophils are regulated by TNF- mediated PANX1 activation. Following lung ischemia/reperfusion (I/R), alveolar macrophages activate PANX1 channels via TNF as an initial signal. PANX1 activation helps the release of ATP to the extracellular space, leading to increased leukocyte trafficking and subsequent inflammation and tissue damage [7], [68]. Further investigation is needed to assess whether these channels and receptors lead to endothelial dysfunction in COVID-19 or not.
3. Pannexin 1 channel/purinergic receptors contribution in COVID-19 clinical manifestations
COVID-19 is characterized by a broad clinical spectrum, ranging from an asymptomatic to severe and systemic disease. The severe disease course characterized by ARDS is accompanied by sepsis, septic shock, and multiple organ failure and mortality [47], [69], [70]. In addition to the respiratory system, other affected organs by SARS-CoV-2 include cardiovascular, renal, digestive, nervous, ocular, and integumentary systems [71].
PANX1 is a ubiquitously expressed gene in almost all cell types. It is involved in various physiological functions, such as regulation of cellular differentiation and migration, cell proliferation, wound healing, cytokine secretion, inflammation, control of blood flow, platelet aggregation, endothelial-mediated vasodilation, mucociliary lung clearance, cell death, tissue development and regeneration, potentiation of muscle contraction, glucose uptake in insulin-stimulated adipocytes, differentiation of olfactory sensory neurons, neuromodulation and neuroprotection [4], [6]. As a result, PANX1-mediated signaling has been implicated in several disease processes [9]. In this section, we provide hypotheses about how PANX1 and purinergic signaling may be associated with clinical manifestations of SARS-CoV-2 infection (Table 1 ).
Table 1.
Symptoms of purinergic receptor dysregulation and suggested therapeutic options.
| System | Effect of PANX signaling dysregulation | Therapeutic options | Ref. |
|---|---|---|---|
| Pulmonary | Acute pulmonary inflammation, edema, and lung dysfunction, Mucus hypersecretion | TRPV4 inhibitors, controlling of MUC5AC, carbenoxolone, Spironolactone | [35], [74], [147] |
| Cardiovascular | Vasodilation, vasoconstriction, cardiomyocyte apoptosis | Clopidogrel, prasugrel, Spironolactone | [82], [86], [146] |
| Coagulopathies | Thrombosis, coagulation, hemolysis | Probenecid, carbenoxolone | [90] |
| Renal | Kidney injury | NA | – |
| Gastrointestinal | Enteric neuron death, IBD | Carbenoxolone | [7] |
| Hepatic | Hepatic ischemia-reperfusion injury, fibrosis and cirrhosis | Tenofovir | [148] |
| Sepsis | Sepsis | Probenecid | [9] |
| Neurological | Myelination and neurite outgrowth, epilepsy, seizure, depression | P2X7 selective antagonists | [113] |
| Olfactory | Suppresses odor responsiveness | NA | – |
| Endocrinological | Obesity, insulin resistance, lipolysis | NA | – |
| Dermatological | Fibrotic scars, collagen production, contact dermatitis, psoriasis, cutaneous GVHD | Tenofovir | [148] |
NA: not available data.
3.1. Pulmonary manifestations
Pneumonia, a common complication in COVID-19 patients, may progress to hypoxemia and potentially acute lung injury and ARDS [72]. During acute lung injury and hypoxia, PANX1 channel activation leads to extracellular ATP release, which acts as a signaling molecule via binding to P2 receptors [7]. Elevated extracellular ATP (as a result of PANX1 channel upregulation) has been demonstrated to play an essential role in acute pulmonary inflammation, edema, and lung dysfunction after ischemia/reperfusion injury [73].
One strategy to control the pulmonary edema and limit the severity of COVID-19-associated ARDS is through transient receptor potential vanilloid 4 (TRPV4) inhibitors [74]. Interestingly, TRPV4 channels are shown to induce PANX1 channel activity [39], [75], [76]. Hence, we hypothesize that pharmacological antagonism of PANX1 activity may help for the management of COVID-19 pathogenesis.
Mucosal damage is suggested as a pathological consequence of PANX1 and P2X7R activities [77]. The outer mucus is excessively produced and secreted, accompanied by a periciliary fluid decrease in pathological situations such as infection and inflammation. Stretching the cell membrane due to osmolality and viscosity alterations creates a mechanical stimulation inducing PANX1 opening, ATP, and H2O releasing into the periciliary fluid layer and increasing the periciliary fluid volume [78]. Additionally, MUC5AC, airway mucin, is expressed and released via ATP-activated P2Y2R. Mucus hypersecretion after viral infection could be managed by controlling of MUC5AC expression pathway [35].
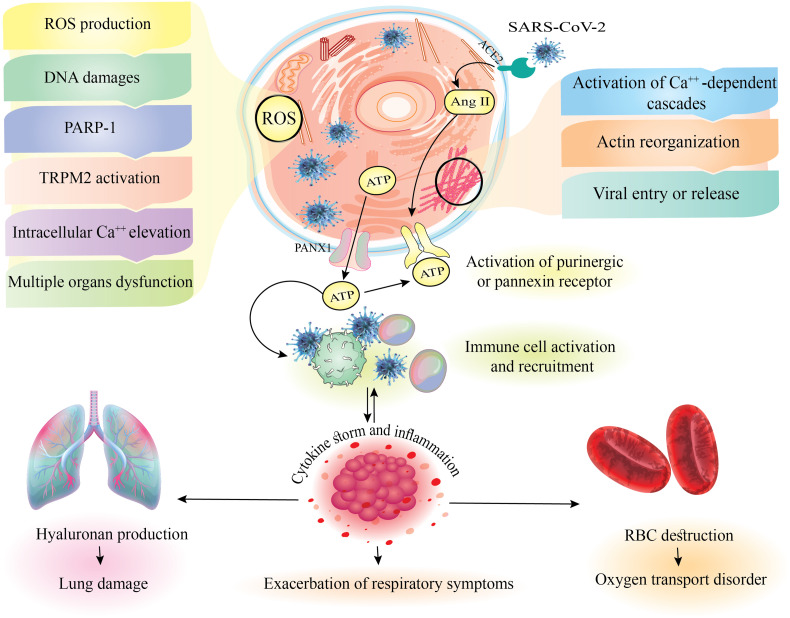
Production of hyaluronan (Hyaluronic acid, HA) as a significant component of the extracellular matrix associated with ARDS is affected by SARS-CoV-2 infection. Potent stimulators of HA-synthase-2 (HAS2), including inflammatory cytokines IL-1 and TNF, are increased in the lungs of patients with COVID-19 [79]. Furthermore, extracellular ATP is considered to mediate pro-inflammatory signals. Therefore, it could upregulate the HAS2 expression and hyaluronan secretion (Fig. 3 ) (Rauhala et al., 2018), suggesting reducing the HA level or inhibiting its production in COVID-19 patients may be achieved through inhibition of PANX1 channel.
Fig. 3.
Mechanisms of virus entry, cell death, immune response, cytokine storm and coronavirus pathogenesis. Following the entrance of the virus through the ACE2 receptor, AngII activates purinergic or pannexin receptors. ROS production following viral infection, through the path shown, eventually induces cell death pathways and organ failure. Activation of Ca++-dependent signaling cascades also facilitates virus entry into the cell through actin polymerization. On the other hand, activation of purinergic and pannexin receptors activates and recruits immune cells. Following this event, inflammatory processes and cytokine storms, with the production of hyaluronan and RBC damage, caused lung damage and lack of oxygen transfer, respectively, which together exacerbate the respiratory symptoms of the COVID-19. ACE2, Angiotensin-converting enzyme 2; AngII, angiotensin II; ATP, Adenosine triphosphate; COVID-19, Coronavirus disease 2019; Panx1, Pannexin 1; PARP1, Poly [ADP-ribose] polymerase 1; RBC, Red blood cells; ROS, Reactive oxygen species; TRMP2, Transient receptor potential cation channel subfamily M member 2. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3.2. Cardiovascular manifestations
The cardiovascular system, especially the heart, is affected by SARS-CoV-2 [69]. In COVID-19, cytokine storms and the hypoxic state are among the putative mechanisms of myocardial injury, which can induce excessive extracellular Ca2+ levels leading to myocyte apoptosis [80], [81].
ATP release and activation of PANX1/P2 signaling contribute to several processes involved in both the physiology and pathophysiology of the cardiovascular system. This signaling pathway is a primary contributing factor in many inflammation-associated cardiovascular diseases [4], [82].
Ischemic cardiomyocytes, activated platelets, and/or inflammatory cells in the interstitium can release extracellular ATP triggering the activation of the P2X7 receptor and thereby pro-inflammatory cascade [83]. ATP release is also known to play an essential role in vasodilation induced by hypoxia, vasoconstriction, and hypertension-induced vasodilation [67].
During myocardial ischemia, the activation of cardiac spinal afferents is controlled by endogenously released ATP mediated by P2X [84]. ATP release and its effect on P2X receptors to mediate cardiomyocyte apoptosis have been reported to be induced by rat atrial myocytes stretch [82]. In addition, a wave of Ca2+ via autocrine ATP release acting on P2Y1 receptors in rat atrial myocytes is caused by shear stress [85]. ATP can also control cardiomyocyte contractility via binding to the P2X receptors [83].
Mechanisms and receptors involved in ATP release are potential targets for treating vascular complications such as heart failure, atherosclerosis, thrombosis and hypertension. Clopidogrel, prasugrel, and other P2Y12R blockers are widely used in the treatment of thrombosis, stroke, and myocardial infarctions as platelet inhibitors [82], [86]. Interestingly, these antiplatelet agents are proposed for arterial thromboprophylaxis in COVID-19 patients [87].
3.3. Coagulopathies and hematological manifestations
Coagulation abnormalities, such as thrombotic microangiopathy or disseminated intravascular coagulation, are observed in many patients with severe COVID-19 [88]. The inflammatory changes, along with hypoxia and infection-mediated endothelial damage and endothelialitis, promote thrombotic complications in COVID-19 [71].
The release of pro-thrombotic granule contents and thrombin formation is triggered by platelet activation [89], [90]. The surface of human platelets contains PANX1. Probenecid (PBN) and carbenoxolone (CBX) are PANX1 inhibitors that might act through P2X1 signaling to impair collagen, thrombin, and thromboxane A2 analog-induced Ca2+ influx [90]. The platelet P2Y12 receptor regulates platelet activation by the impact of platelet agonists. This explains the importance of this purinergic receptor in thrombosis [89]. Moreover, in human coronary artery endothelial cells, ATP or UTP activates the P2Y2 receptor, resulting in the upregulation of tissue factor, a primary initiator of the coagulation cascade [82].
In COVID-19, hemolysis as a result of a significant increase in ATP release from RBCs (Red Blood Cell) via the PANX1 channel could be a possible explanation for reduced erythrogenesis and increased destruction of RBCs [91], [92], [93], [94] (Fig. 3).
3.4. Renal manifestations
Sudden kidney failure within seven days is called acute kidney injury (AKI) observed in patients infected with MERS-CoV, SARS-CoV and SARS-CoV-2. Moreover, in COVID-19, multi-organ failure, sepsis and shock accompany AKI [69].
The severity of AKI is determined by mitochondria dysfunction, excess ROS production, apoptosis, and necrosis caused by metabolic stress in the kidneys induced by decreased intracellular ATP pool. AKI could be developed by the changes in ATP concentration in extracellular and intracellular spaces via PANX1 channels. A high concentration of ATP in the extracellular space exacerbates inflammation, and depletion of intracellular ATP changes cellular energetics, which, subsequently, causes irreversible cellular damage, apoptosis, and necrosis [95].
Factors such as elevation of sheer stress, excessive interstitial ATP concentration, increased renal interstitial Ang II, and P2 receptors activation lead to the development of hypertensive renal injury by release of interleukins and growth factors [54].
3.5. Gastrointestinal (GI) involvement
Gastrointestinal symptoms such as diarrhea, abdominal pain, nausea and vomiting are observed in some patients with COVID-19 [69], [96]. The PANX1 channel plays a pivotal role in the GI system to mediate various actions, including gut function and pathophysiology of IBD (inflammatory bowel disease) [4], [97]. PANX1 is involved in enteric neuron death induced by inflammation which leads to abnormalities in gut motility in IBD. This channel also contributes to IBD by increasing ROS production [4]. However, the link between the level of PANX1 channel activity and gastrointestinal complications of COVID-19 remains to be elucidated.
3.6. Hepatic manifestations
In patients with severe COVID-19, liver injury or liver failure could be attributed to immune-mediated inflammation [98]. Hepatic ischemia-reperfusion injury (IRI) affecting multiple tissues and organs is followed by PANX1-mediated inflammasome activation [7], [99]. Chronic cellular damage could lead to severe liver diseases such as fibrosis and cirrhosis by triggering an aberrant repair process mediated by ATP [100]. Therefore, it could be hypothesized that liver injury or failure in COVID-19 patients may be triggered by PANX1-mediated inflammation.
3.7. Sepsis and septic shock
One of the clinical manifestations of COVID-19 is sepsis [69], [101]. Adenosine plays a role in sepsis-associated hemodynamic changes [82]. ATP release following PANX1 activation results in dysregulated inflammation leading to sepsis pathogenesis. Inflammation triggers inflammasome activation through P2X7R activation, the release of HMGB1 (high mobility group box 1), and the production of NO (nitric oxide). Lethal systemic inflammation is linked to excessive macrophage PANX1 hemichannel activation [102].
3.8. Neurological manifestations
Ataxia, seizure, neuralgia, unconsciousness, acute cerebrovascular disease, encephalopathy, and neuropsychiatric symptoms are clinical manifestations in patients with COVID-19 whose central nervous system (CNS) is invaded by the virus [103]. Some of these neurological manifestations can prove COVID-19 neurovirulence. Excess cytokine can trigger the pro-inflammatory and pro-thrombotic cascade affecting brain vasculature and the blood-brain barrier (BBB) that may lead to inflammatory damage in the brain tissue in patients with COVID-19 [71], [104].
PANX1 and P2 receptors are linked to peripheral sensitization (pain) pathways in both CNS and peripheral nervous system (PNS). Other processes in the PNS, such as myelination and neurite outgrowth, are mediated by purinergic pathways [13]. Regulation of neuronal excitability by the release of glutamate, gamma-Aminobutyric acid (GABA), and ATP is triggered by the binding of ATP to purinergic receptors. A massive increase of the extracellular ATP concentrations has been reported during pathological conditions, including ischemia, inflammation, trauma and epilepsy. For example, during a seizure, the ATP excitatory effects on neurons are linked to P2X, and the inhibitory effects are mediated through the activation of P1 purinergic receptors [105]. Indeed, seizure prevention by the opening of the PANX1 channel during metabolic stress (e.g., ketogenic diet) or in the pilocarpine model has been reported can result from activation of P1 receptors [105].
Signaling in the CNS is triggered by the ATP release from synaptic terminals and mediated by the P2Y receptors initiating intracellular Ca2+ release and proliferating Ca2+ waves, a substrate for glial excitability. P2X1–4 and P2X6 receptors are expressed and translated in astrocytes in situ, and P2X-mediated currents are produced in astroglial cell cultures that may be critical during pathological conditions [106].
In depression, excessive release of inflammatory cytokines, such as IL-1β, is triggered by the overactivation of P2X7 receptor and NOD-, LRR- and pyrin domain-containing protein 3 (NLRP3) inflammasome [107]. Depression is a consequence of CNS neuroinflammation due to the activation of P2X7 receptors by microglia after increasing the extracellular ATP level in the brain under psychological stress [107], [108]. Adverse stimuli such as stress lead to the activation of P2X7 ion channels in the brain, stimulating the release of pro-inflammatory factors induced by NLRP3, causing CNS neuroinflammation and subsequently, depression [109], [110], [111]. In a chronic stress model, inhibition of the P2X7–NLRP3–IL-1β pathway by P2X7 selective antagonists penetrating the BBB reduces the immune-inflammatory effect of microglia cells, CNS neuroinflammation, and depression [112], [113]. Therefore, the role of this pathway which might also involve PANX1 activation in depression, as one of the neuropsychiatric manifestations of COVID-19, should be elucidated.
3.9. Olfactory disturbances
Olfactory disturbances have been reported primarily on asymptomatic COVID-19 patients [114]. The highest expression of ACE2 in the respiratory system is observed in nasal epithelial cells, which might explain the altered sense of taste or smell [71]. The olfactory epithelium (OE) and olfactory bulb (OB) constitute the main olfactory system (MOS). The regulation of olfactory sensations is mediated by purinergic signaling [115]. MOS signaling in the olfactory epithelium is mediated by ATP release through PANX1, which is also critical for the proliferation and differentiation of olfactory sensory neurons [116]. ATP induces inward currents and Ca2+ increase in sensory neurons via P2X receptors activation, which suppresses odor responsiveness [116].
3.10. Endocrinological manifestations
The severity of COVID-19 could be higher in patients with pre-existing endocrinological conditions such as diabetes mellitus and/or obesity [74]. The severe form of COVID-19 could be linked to increased levels of cytokines which cause pancreatic β-cell dysfunction and apoptosis, leading to decreased insulin production and ketosis [117], [118]. Another possible mechanism could be a rapid fat breakdown in COVID-19 patients [119]. Clinical manifestations of COVID-19 in other body organs other than lungs could be interlinked with diabetic complications [120].
Another risk factor for severe COVID-19 is obesity [121]. Increased pro-inflammatory cytokines exacerbating the inflammatory response are related to elevated adiposity [71], [122], [123], [124]. β-cell functions and survival are modulated by purinergic signaling. The P2X7 receptor and PANX-1 are involved in the release of ATP and insulin from pancreatic β-cells by regulating signaling pathways in the pancreatic islets [125], [126].
A growing body of data shows that the metabolism of lipids, control of endocrine activity, and glucose uptake are linked to purinergic receptors. Adipogenesis and lipid metabolism are regulated by purinergic P2 receptors [114]. P2X7-deficient mice exhibit accumulation of lipids, abnormal fat distribution, and, finally, weight gain [127]. In contrast, energy expenditure increases by the P2X7 stimulation. Overall, the P2X7 signaling plays a prominent role in obesity and insulin resistance [128].
Extracellular nucleotide release from adipocytes is mediated by the PANX1 channels indicating their role in controlling metabolic homeostasis. Activation of insulin-induced glucose uptake in adipocytes is triggered by PANX1-dependent ATP release, and the PANX1 channel is activated by insulin [129].
There is a growing body of evidence showing that insulin-PANX1-purinergic signaling crosstalk exists in adipose tissue. It is suggested that deregulation of this signaling may contribute to lipolysis in adipocytes and adipose tissue inflammation [130]. The increased release of pro-inflammatory factor IL-1β is a result of the activation of the P2X7–NLRP3 inflammasome stimulated by chronic hyperglycemia. Type 2 diabetes induction and aggravation through β cell death and insulin resistance are related to the elevated NLRP3-dependent IL-1β [112].
3.11. Dermatological manifestations
Rare incidence of dermatological manifestations in patients with COVID-19 [74] could potentially be a consequence of hypersensitivity reactions to SARS-CoV-2 RNA, cytokine-release syndrome, deposition of microthrombi, and vasculitis [131]. Histopathological examination of skin rashes has revealed dyskeratotic keratinocytes and superficial perivascular dermatitis [132], [133]. Acro cutaneous lesions biopsy has displayed dense diffuse lymphoid infiltrates as well as signs of endothelial inflammation. Rarely, small thrombi are also observed in blood vessels of the dermis [71], [132], [133].
In various layers of the adult human skin, the PANX1 expression with different localization profiles is reported [134], [135]. The channel regulates the cellular properties of keratinocytes and fibroblasts in the early stages of skin development. It is also upregulated in wound repair after injury and downregulated in aged skin. The migration of keratinocytes and regulation of dermal fibroblasts differentiation into myofibroblasts for appropriate wound contraction are also attributed to PANX1. Panx1-deficiency results in excessive proliferation of fibroblasts and the development of fibrotic scars as a result of improper differentiation of fibroblasts in response to TGF-β. The migration of keratinocytes is also dysregulated after the Panx1 deletion [136].
Proliferation, differentiation, and apoptosis of various types of skin cells could be regulated by the ATP release from PANX1 channels. ATP binds to the purinergic receptors triggering activation of downstream signaling [137]. Reaction to mechanical stimulation and cell damage can lead to the ATP release in wound healing [138]; therefore, it is considered that PANX1 and purinergic receptors play an important role in the proper signaling cascade during wound healing [136]. Recently, it has been shown that macrophage trafficking, in situ proliferation, and collagen production increase drastically within the wound after intracellular ATP delivery [6].
P2X7 might have a role in some skin disorders, including contact dermatitis, psoriasis, cutaneous GVHD (Graft-versus-host disease). It is also involved in skin processes such as wound healing and transplantation [139].
Hence, these channels and receptors represent a potential target in inflammatory conditions and could emerge as new therapeutic opportunities for the pathologies which result from cytokine storm in patients with COVID-19.
4. Targeting PANX1 channel and/or purinergic signaling in COVID-19 therapy
Targeting PANX1 channel and purinergic receptors may emerge as a novel therapeutic option for COVID-19 prevention and treatment. In this regard, we focus here on summarizing the antiviral activities of PANX1 and purinergic receptors` inhibitors and highlighting their therapeutic potential in combating COVID-19.
4.1. Repurposed FDA-approved drugs which target PANX1 in COVID-19 therapy
Due to the time-consuming de novo drug discovery process, it would be wise to consider drug repositioning in the epidemic of sudden infectious diseases [140]. ATP decrease in vivo and in vitro by PANX1 antagonists such as CBX and PBN hinders the downstream purinergic signaling mediated by ATP, leading to inflammation [7]. PBN is an FDA-approved drug for gout which blocks PANX1 hemichannels, ATP release, β toxin-induced cell death, human erythrocytes (RBCs) swelling, the inflammatory mediator's release, the ATP-induced T-cell mortality, aggregation of platelets, formation of thrombus and oxygen-glucose deprivation injury [4].
Following PBN treatment, attenuation of influenza A viral infection and lung viral load has been observed both in vitro and in vivo [141]. PBN decreases the inflammatory response in sepsis by reducing inflammasome-dependent IL-1β secretion from macrophages in vitro [9]. In addition, treatment by PBN decreases the required dose of Oseltamivir, antiviral medication for influenza [141] possibly by increasing its plasma levels [142]. Another possible explanation for the antiviral and anti-inflammatory activities of PBN is its ability to inhibit P2X7 receptors [143]. PBN also inhibits the secretion of the lysosomal cathepsin proteases providing a protective effect in ischemia/reperfusion injury [144]. This mechanism of protection can also be utilized in SARS-CoV-2 infection since coronavirus infection is also facilitated by cathepsins cleaving the spike protein [145]. Therefore, PBN could be potentially used for COVID-19 treatment because of its tolerance, demonstrated effect on viral infection-associated inflammation, and lowered required doses of other antiviral drugs [27].
Furthermore, ATP release through Pannexin hemichannels can be inhibited by a water-soluble blocker of PANX1 channels, CBX [4]. CBX has also been used for gastric ulcers and other types of inflammation treatment. Significant mitigation of lung dysfunction, injury, and edema after I/R is observed after treatment by both PBN and CBX [7].
Spironolactone is an aldosterone antagonist inhibiting the PANX1 channel, which can potentially be used to treat COVID-19. Spironolactone is initially used as a diuretic for high blood pressure treatment [146]. Its use in COVID-19-associated ARDS patients with hypertension is suggested in addition to its potential benefit as a PANX1 blocker [147]. A possible mechanism of action for Spironolactone is increasing the ACE2 levels, the spike protein receptor, in plasma, which increases its proportion in plasma to pulmonary endothelial cell membrane resulting in lung infection reduction [147]. More studies are needed to prove Spironolactone's mechanism of action and the effectiveness of its PANX1-inhibiting function in the context of COVID-19 [27].
Furthermore, nucleoside analog antivirals such as Tenofovir disrupt the virus life cycle by incorporating into newly synthesized viral nucleic acid molecules resulting in synthesis inhibition and chain termination. Mechanism of action of Tenofovir in the treatment of hepatitis B (HBV) and HIV in RAW264.7 and HepG2 cells (a mouse macrophage and a human liver cell lines, respectively) is through inhibition of PANX1-mediated ATP release [27]. Importantly, downregulation of adenosine levels by Tenofovir inhibits liver and skin fibrosis [148].
Tenofovir is metabolized into a nucleotide analog within the cell and its inhibitory action on the PANX1 channel could be through an intracellular mechanism [149]. Inhibition and internalization of the channel by excessive extracellular ATP have led to another possible hypothesis for the Tenofovir mechanism of action, which is the release of active tenofovir into the extracellular space and blocking the PANX1 from an external site [27], [150], [151].
Inhibition of ATP release by Tenofovir is hypothesized to be mediated by the intracellular accumulation of the drug and possibly its polyphosphated metabolites [148]. Tenofovir is absorbed into the cell and converted to the active form of the drug (Tenofovir diphosphate, TFV-DP) [152]. In HIV infections, Tenofovir diphosphate competes with deoxyadenosine 5′-triphosphate for inclusion into a new synthesized HIV DNA, a mechanism reminiscent of that of NRTIs (Nucleoside reverse transcriptase inhibitors). DNA synthesis is interrupted after Tenofovir diphosphate insertion [148].
A recent molecular docking study has suggested Tenofovir as a potent drug against SARS-CoV-2 through tightly binding to its RNA-dependent RNA polymerase (RdRp), with binding energies similar to those of native nucleotides. Hence, it may inhibit the SARS-CoV polymerase function [153]. Moreover, using polymerase extension experiments, it has been shown that the Tenofovir diphosphate can be incorporated by SARS-CoV-2 RdRp terminating polymerase extension. Previous studies have indicated the potential activity of Tenofovir for inhibiting HIV and HBV polymerase but not host nuclear and mitochondrial polymerases [154], [155]. Tenofovir diphosphate has a smaller size than natural nucleoside triphosphates; therefore, it could easily fit in the active site of SARS-CoV-2 RdRp. In addition, TFV-DP is a non-cyclic nucleotide without a normal sugar ring configuration which might not be detectable by the 3′-exonucleases, which are necessary for SARS-CoV-2 proofreading processes [156].
Furthermore, computational analysis of potential drugs for COVID-19 has shown that Tenofovir might bind to nonstructural protein 1 (Nsp1), a coronavirus virulence factor interacting with host 40S ribosomal subunit and thus lead to host mRNA degradation, and also inhibition of type-I interferon production [157].
Several cohorts have recently shown that Tenofovir disoproxil fumarate plus emtricitabine accelerate the natural clearance of nasopharyngeal SARS-CoV-2 viral burden and thus contribute to a less likely severe form of COVID-19 [158], [159]. Hence, it would be wise to consider the inclusion of tenofovir-based therapies in multi-armed therapeutic trials for the prevention and early treatment of COVID-19.
Remdesivir is extensively used in the treatment of COVID-19 patients; however, it is not known if it interferes with PANX1 activity and possibly PANX1-associated inflammatory signaling in COVID-19. Since Remdesivir is also a nucleoside analog, it would be interesting to investigate whether it blocks PANX1 channels like Tenofovir or not [27].
4.2. Directly targeting of PANX1 channels
It is not known whether PANX1 is linked to the SARS-CoV-2 mechanism of infection and inflammatory responses. If further studies proved their link, developing new drugs for directly targeting the channel may be worthwhile for preventive and therapeutic purposes. Currently, there is a PANX1-specific inhibitor peptide, Pannexin intracellular loop 2 peptide (PxIL2P), which is composed of a short sequence mimicking the IL2 region of PANX1 linked to an HIV-TAT transactivation protein [68], [160]. PxIL2P was shown to effectively reduce inflammatory responses by regulating intracellular calcium in human umbilical vein endothelial cells (HUVECs) in vitro and in vivo; however, it is not yet approved by the FDA [68]. PxIL2P blocks ATP release from the PANX1 channel by binding to the second intracellular loop of PANX1 and, consequently, changing intracellular Ca2+ flux. The use of PxIL2P in cultured endothelial cells inhibits the expression and release of cytokines IL-1β and CxCL10 regulated by PANX1, and in the vasculature limits monocyte adhesion [27]. Therefore, reducing the susceptibility to SARS-CoV-2 infection and vascular inflammation in patients with COVID19 can be attained by directly targeting the PANX1 channel.
In addition to PANX1 inhibitors, purinergic receptor antagonists could be considered as potential therapeutics for COVID-19. Purinergic receptor blockers including Suramin, pyridoxal-phosphate-6-azophenyl-2′,4′-disulfonate (PPADS), and Brilliant Blue G (BBG), which latter selectively blocks P2X7R, are currently used for the treatment of HBV infection. Furthermore, antiviral effects of Suramin have been demonstrated on other animal viruses [24].
In one of its mechanisms of action, the antibiotic erythromycin, which is used to treat respiratory infections, blocks the P2X receptor-dependent Ca2+ influx [35]. However, its clinical utility in the course of COVID-19 remains to be studied.
4.3. ATP supplementation for treatment of COVID-19
Published evidence to date indicates that although cystic fibrosis patients are at higher risk of acute severity of chronic lung disease, the clinical course of these patients with SARS-CoV-2 infection was milder than initially expected with a potentially new and unknown mechanism of action [161]. In a search to find the factors behind this survival benefit against SARS-CoV-2, Abraham et al. focused on a promising candidate which was ATP, with elevated systemic levels in CF patients and playing crucial roles in intra-cellular metabolism and extracellular signaling [162]. They proposed that as well as the general reduction of ATP levels with age [163], there may be other mechanisms like blood clotting with subsequent decreased local oxygenation and tissue ATP production leading to the general decline of ATP levels in COVID-19 patients. They furthermore hypothesized that ATP supplementation of the general population especially during the first few critical weeks of SARS-CoV-2 infection, may lead to a survival benefit like what was observed in CF patients. Therefore, they initiated a non-randomized trial of oral ATP nutritional supplementation for treatment of clinically significant COVID-19 patients and their short-term results showed a considerable survival benefit conferred by ATP therapy [162].
While at first glance, ATP supplementation for treatment of COVID-19 seems to be a contradiction, considering what we previously hypothesized: ATP reduction via inhibiting PANX1 channel as a therapy for COVID-19, it should be noted that in the early stages of the disease, increased levels of ATP are beneficial, while in the advanced stages of the disease, conversely, by exacerbating the cytokine storm, it has detrimental effects [164]. With this explanation, it can be hypothesized that in patients with cystic fibrosis, due to high levels of ATP, the immune cells are more active than normal population, which prevents from life-threatening consequences of COVID-19. Another crucial factor is the concentration of ATP. Increasing the concentration of ATP will be beneficial to some extent and prevent viral infection, but too much concentration has the opposite effect [165]. In summary, any ATP therapeutic modulation (supplementation/blockage) for COVID-19 should be carefully designed and monitored because of the complex role of extracellular ATP in cellular physiology.
5. Conclusion
The association of PANX1 channels with various signaling molecules and its wide cellular and tissue distribution has attracted increasing attention in disease-related research. Since its discovery in the early 21st century, studies have reported a major contribution of PANX1 in the pathology of various viral infections and their related complications [25], [105].
Here, we hypothesize that pharmacological modulation of the PANX1 (and therefore potentially purinergic P2 receptor signaling pathways) may provide clinical benefit to COVID-19 patients with progressive disease resulting from excessive production of pro-inflammatory cytokines/chemokines. According to the above vision of the role of PANX/P2-receptor in the regulation of inflammatory cascades and viral pathologies, this pathway should be the focus of further investigations to assess potential direct links to COVID-19 molecular pathology and design new preventative therapies and treatments for COVID-19.
PANX1 could be considered a candidate target for treating COVID-19 because of its role in regulating inflammation and viral infection. However, there is no experimentally proved mechanism linking PANX1 to COVID-19. Nucleotide antiviral drugs which exhibit anti-PANX1 activity have been currently used for COVID-19 treatment. PBN is another drug blocking PANX1 having the same effects of PANX1 deletion and could be repurposed as a potential treatment for COVID-19. Specific PANX1 inhibitors could be included as part of the treatment regimen if further studies demonstrate the role of PANX1 in COVID-19 pathogenesis.
CRediT authorship contribution statement
Zakiye Nadeali: Investigation, Writing – original draft. Fatemeh Mohammad-Rezaei: Investigation, Writing – original draft. Hamid Aria: Investigation, Visualization, Writing – original draft. Parvaneh Nikpour: Conceptualization, Project administration, Supervision, Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Liguoro I., Pilotto C., Bonanni M., Ferrari M.E., Pusiol A., Nocerino A., Vidal E., Cogo P. SARS-COV-2 infection in children and newborns: a systematic review. Eur. J. Pediatr. 2020;179:1029–1046. doi: 10.1007/s00431-020-03684-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Espinosa O.A., dos S. Zanetti A., Antunes E.F., Longhi F.G., de Matos T.A., Battaglini P.F. Prevalence of comorbidities in patients and mortality cases affected by SARS-CoV2: a systematic review and meta-analysis. Rev. Inst. Med. Trop. Sao Paulo. 2020;62 doi: 10.1590/S1678-9946202062043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Montalvan V., Lee J., Bueso T., De Toledo J., Rivas K. Neurological manifestations of COVID-19 and other coronavirus infections: a systematic review. Clin. Neurol. Neurosurg. 2020;194 doi: 10.1016/j.clineuro.2020.105921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xu J., Chen L., Li L. Pannexin hemichannels: a novel promising therapy target for oxidative stress related diseases. J. Cell. Physiol. 2018;233:2075–2090. doi: 10.1002/jcp.25906. [DOI] [PubMed] [Google Scholar]
- 5.Makarenkova H.P., Shestopalov V.I. The role of pannexin hemichannels in inflammation and regeneration. Front. Physiol. 2014;5 doi: 10.3389/fphys.2014.00063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Makarenkova H.P., Shah S.B., Shestopalov V.I. The two faces of pannexins: new roles in inflammation and repair. J. Inflamm. Res. 2018;11:273. doi: 10.2147/JIR.S128401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharma A.K., Charles E.J., Zhao Y., Narahari A.K., Baderdinni P.K., Good M.E., Lorenz U.M., Kron I.L., Bayliss D.A., Ravichandran K.S. Pannexin-1 channels on endothelial cells mediate vascular inflammation during lung ischemia-reperfusion injury. Am. J. Physiol. Cell. Mol. Physiol. 2018;315:L301–L312. doi: 10.1152/ajplung.00004.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rauhala L., Jokela T., Kärnä R., Bart G., Takabe P., Oikari S., Tammi M.I., Pasonen-Seppänen S., Tammi R.H. Extracellular ATP activates hyaluronan synthase 2 (HAS2) in epidermal keratinocytes via P2Y2, Ca2+ signaling, and MAPK pathways. Biochem. J. 2018;475:1755–1772. doi: 10.1042/BCJ20180054. [DOI] [PubMed] [Google Scholar]
- 9.Yanguas S.C., Willebrords J., Johnstone S.R., Maes M., Decrock E., De Bock M., Leybaert L., Cogliati B., Vinken M. Pannexin1 as mediator of inflammation and cell death. Biochim. Biophys. Acta (BBA)-Molecular Cell Res. 2017;1864:51–61. doi: 10.1016/j.bbamcr.2016.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Valdebenito S., Barreto A., Eugenin E.A. The role of connexin and pannexin containing channels in the innate and acquired immune response. Biochim. Biophys. Acta Biomembr. 2018;1860:154–165. doi: 10.1016/j.bbamem.2017.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paoletti A., Raza S.Q., Voisin L., Law F., da Fonseca J.P., Caillet M., Kroemer G., Perfettini J.-L. Multifaceted roles of purinergic receptors in viral infection. Microbes Infect. 2012;14:1278–1283. doi: 10.1016/j.micinf.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 12.Wang Y., Zhao J., Cai Y., Ballard H.J. Cystic fibrosis transmembrane conductance regulator-dependent bicarbonate entry controls rat cardiomyocyte ATP release via pannexin1 through mitochondrial signalling and caspase activation. Acta Physiol. (Oxf) 2020;230 doi: 10.1111/apha.13495. [DOI] [PubMed] [Google Scholar]
- 13.Horton S.M., Luna Lopez C., Blevins E., Howarth H., Weisberg J., Shestopalov V.I., Makarenkova H.P., Shah S.B. Pannexin 1 modulates axonal growth in mouse peripheral nerves. Front. Cell. Neurosci. 2017;11:365. doi: 10.3389/fncel.2017.00365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ferrari D., Idzko M., Müller T., Manservigi R., Marconi P. Purinergic signaling: a new pharmacological target against viruses? Trends Pharmacol. Sci. 2018;39:926–936. doi: 10.1016/j.tips.2018.09.004. [DOI] [PubMed] [Google Scholar]
- 15.Freeman T.L., Swartz T.H. Purinergic receptors: elucidating the role of these immune mediators in HIV-1 fusion. Viruses. 2020;12:290. doi: 10.3390/v12030290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Velasquez S., Eugenin E.A. Role of Pannexin-1 hemichannels and purinergic receptors in the pathogenesis of human diseases. Front. Physiol. 2014;5:96. doi: 10.3389/fphys.2014.00096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beavis P.A., Stagg J., Darcy P.K., Smyth M.J. CD73: a potent suppressor of antitumor immune responses. Trends Immunol. 2012;33:231–237. doi: 10.1016/j.it.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 18.Fredholm B.B., IJzerman A.P., Jacobson K.A., Linden J., Müller C.E., International Union of Basic and Clinical Pharmacology LXXXI. Nomenclature and classification of adenosine receptors—an update. Pharmacol. Rev. 2011;63:1–34. doi: 10.1124/pr.110.003285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Milne G.R., Palmer T.M. Anti-inflammatory and immunosuppressive effects of the A2A adenosine receptor. TheScientificWorldJOURNAL. 2011;11:320–339. doi: 10.1100/tsw.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caracciolo M., Correale P., Mangano C., Foti G., Falcone C., Macheda S., Cuzzola M., Conte M., Falzea A.C., Iuliano E., Morabito A., Caraglia M., Polimeni N., Ferrarelli A., Labate D., Tescione M., Di Renzo L., Chiricolo G., Romano L., De Lorenzo A. Efficacy and effect of inhaled adenosine treatment in hospitalized COVID-19 patients. Front. Immunol. 2021;12 doi: 10.3389/fimmu.2021.613070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abouelkhair M.A. Targeting adenosinergic pathway and adenosine A2A receptor signaling for the treatment of COVID-19: a hypothesis. Med. Hypotheses. 2020;144 doi: 10.1016/j.mehy.2020.110012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kouhpayeh S., Shariati L., Boshtam M., Rahimmanesh I., Mirian M., Zeinalian M., Salari-jazi A., Khanahmad N., Damavandi M.S., Sadeghi P. 2020. The Molecular Story of COVID-19; NAD+ Depletion Addresses All Questions in This Infection. [Google Scholar]
- 23.Birra D., Benucci M., Landolfi L., Merchionda A., Loi G., Amato P., Licata G., Quartuccio L., Triggiani M., Moscato P. COVID 19: a clue from innate immunity. Immunol. Res. 2020;1–8 doi: 10.1007/s12026-020-09137-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pacheco P.A.F., Faria R.X., Ferreira L.G.B., Paixão I.C.N.P. Putative roles of purinergic signaling in human immunodeficiency virus-1 infection. Biol. Direct. 2014;9:21. doi: 10.1186/1745-6150-9-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen S., Shenk T., Nogalski M.T. P2Y2 purinergic receptor modulates virus yield, calcium homeostasis, and cell motility in human cytomegalovirus-infected cells. Proc. Natl. Acad. Sci. 2019;116:18971–18982. doi: 10.1073/pnas.1907562116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Graziano F., Desdouits M., Garzetti L., Podini P., Alfano M., Rubartelli A., Furlan R., Benaroch P., Poli G. Extracellular ATP induces the rapid release of HIV-1 from virus containing compartments of human macrophages. Proc. Natl. Acad. Sci. 2015;112:E3265–E3273. doi: 10.1073/pnas.1500656112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Swayne L.A., Johnstone S.R., Ng C.S., Sanchez-Arias J.C., Good M.E., Penuela S., Lohman A.W., Wolpe A.G., Laubach V.E., Koval M. 2020. Consideration of Pannexin 1 Channels in COVID-19 Pathology and Treatment. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prabhakara C., Godbole R., Sil P., Jahnavi S., Gulzar S.e.J., van Zanten T.S., Sheth D., et al. Strategies to target SARS-CoV-2 entry and infection using dual mechanisms of inhibition by acidification inhibitors. PLOS Pathogens. 2021;17 doi: 10.1371/journal.ppat.1009706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang C., He H., Wang L., Zhang N., Huang H., Xiong Q., Yan Y., Wu N., Ren H., Han H. Virus-triggered ATP release limits viral replication through facilitating IFN-β production in a P2X7-dependent manner. J. Immunol. 2017;199:1372–1381. doi: 10.4049/jimmunol.1700187. [DOI] [PubMed] [Google Scholar]
- 30.Leyva-Grado V.H., Ermler M.E., Schotsaert M., Gonzalez M.G., Gillespie V., Lim J.K., García-Sastre A. Contribution of the purinergic receptor P2X7 to development of lung immunopathology during influenza virus infection. MBio. 2017;8 doi: 10.1128/mBio.00229-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Martin A.G., San-Antonio B., Fresno M. Regulation of nuclear factor κB transactivation implication of phosphatidylinositol 3-kinase and protein kinase C ζ IN c-rel activation by tumor necrosis factor α. J. Biol. Chem. 2001;276:15840–15849. doi: 10.1074/jbc.M011313200. [DOI] [PubMed] [Google Scholar]
- 32.Cauwels A., Rogge E., Vandendriessche B., Shiva S., Brouckaert P. Extracellular ATP drives systemic inflammation, tissue damage and mortality. Cell Death Dis. 2014;5 doi: 10.1038/cddis.2014.70. e1102–e1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li Y., Duche A., Sayer M.R., Roosan D., Khalafalla F.G., Ostrom R.S., Totonchy J., Roosan M.R. SARS-CoV-2 early infection signature identified potential key infection mechanisms and drug targets. BMC Genomics. 2021;22:1–13. doi: 10.1186/s12864-021-07433-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dubyak G.R. Both sides now: multiple interactions of ATP with pannexin-1 hemichannels. Focus on “A permeant regulating its permeation pore: inhibition of pannexin 1 channels by ATP”. Am. J. Physiol. Physiol. 2009;296:C235–C241. doi: 10.1152/ajpcell.00639.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burnstock G. Purinergic signalling: therapeutic developments. Front. Pharmacol. 2017;8:661. doi: 10.3389/fphar.2017.00661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee B.H., Hwang D.M., Palaniyar N., Grinstein S., Philpott D.J., Hu J. Activation of P2X 7 receptor by ATP plays an important role in regulating inflammatory responses during acute viral infection. PLoS One. 2012;7 doi: 10.1371/journal.pone.0035812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Good M.E., Eucker S.A., Li J., Bacon H.M., Lang S.M., Butcher J.T., Johnson T.J., Gaykema R.P., Patel M.K., Zuo Z. Endothelial cell Pannexin1 modulates severity of ischemic stroke by regulating cerebral inflammation and myogenic tone. JCI Insight. 2018;3 doi: 10.1172/jci.insight.96272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jankowski J., Perry H.M., Medina C.B., Huang L., Yao J., Bajwa A., Lorenz U.M., Rosin D.L., Ravichandran K.S., Isakson B.E. Epithelial and endothelial pannexin1 channels mediate AKI. J. Am. Soc. Nephrol. 2018;29:1887–1899. doi: 10.1681/ASN.2017121306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shahidullah M., Mandal A., Delamere N.A. TRPV4 in porcine lens epithelium regulates hemichannel-mediated ATP release and na-K-ATPase activity. Am. J. Physiol. Physiol. 2012;302:C1751–C1761. doi: 10.1152/ajpcell.00010.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wei R., Bao W., He F., Meng F., Liang H., Luo B. Pannexin1 channel inhibitor (10panx) protects against transient focal cerebral ischemic injury by inhibiting RIP3 expression and inflammatory response in rats. Neuroscience. 2020;437:23–33. doi: 10.1016/j.neuroscience.2020.02.042. [DOI] [PubMed] [Google Scholar]
- 41.Kaur G., Lungarella G., Rahman I. SARS-CoV-2 COVID-19 susceptibility and lung inflammatory storm by smoking and vaping. J. Inflamm. 2020;17:1–8. doi: 10.1186/s12950-020-00250-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Belvisi M.G., Birrell M.A. The emerging role of transient receptor potential channels in chronic lung disease. Eur. Respir. J. 2017;50 doi: 10.1183/13993003.01357-2016. [DOI] [PubMed] [Google Scholar]
- 43.Mortaz E., Braber S., Nazary M., Givi M.E., Nijkamp F.P., Folkerts G. ATP in the pathogenesis of lung emphysema. Eur. J. Pharmacol. 2009;619:92–96. doi: 10.1016/j.ejphar.2009.07.022. [DOI] [PubMed] [Google Scholar]
- 44.Zakharov N. 2020. The Protective Effect of Smoking Against COVID-19: A Population-based Study Using Instrumental Variables. [Google Scholar]
- 45.Shastri M.D., Shukla S.D., Chong W.C., Kc R., Dua K., Patel R.P., Peterson G.M., O’Toole R.F. Smoking and COVID-19: what we know so far. Respir. Med. 2020;176 doi: 10.1016/j.rmed.2020.106237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Baxter M., Eltom S., Dekkak B., Yew-Booth L., Dubuis E.D., Maher S.A., Belvisi M.G., Birrell M.A. Role of transient receptor potential and pannexin channels in cigarette smoke-triggered ATP release in the lung. Thorax. 2014;69:1080–1089. doi: 10.1136/thoraxjnl-2014-205467. [DOI] [PubMed] [Google Scholar]
- 47.Kai H., Kai M. Interactions of coronaviruses with ACE2, angiotensin II, and RAS inhibitors—lessons from available evidence and insights into COVID-19. Hypertens. Res. 2020;1–7 doi: 10.1038/s41440-020-0455-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Abdulamir A.S., Hafidh R.R. The possible immunological pathways for the variable immunopathogenesis of COVID–19 infections among healthy adults, elderly and children. Electron. J Gen. Med. 2020;17 [Google Scholar]
- 49.Thompson R.N. Novel coronavirus outbreak in Wuhan, China, 2020: intense surveillance is vital for preventing sustained transmission in new locations. J. Clin. Med. 2020;9:498. doi: 10.3390/jcm9020498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu C., Zhou Q., Li Y., Garner L.V., Watkins S.P., Carter L.J., Smoot J., Gregg A.C., Daniels A.D., Jervey S. 2020. Research and Development on Therapeutic Agents and Vaccines for COVID-19 and Related Human Coronavirus Diseases. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vaduganathan M., Vardeny O., Michel T., McMurray J.J.V., Pfeffer M.A., Solomon S.D. Renin–angiotensin–aldosterone system inhibitors in patients with Covid-19. N. Engl. J. Med. 2020;382:1653–1659. doi: 10.1056/NEJMsr2005760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Murali S., Zhang M., Nurse C.A. Angiotensin II mobilizes intracellular calcium and activates pannexin-1 channels in rat carotid body type II cells via AT1 receptors. J. Physiol. 2014;592:4747–4762. doi: 10.1113/jphysiol.2014.279299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gómez G.I., Fernández P., Velarde V., Sáez J.C. Angiotensin II-induced mesangial cell damage is preceded by cell membrane permeabilization due to upregulation of non-selective channels. Int. J. Mol. Sci. 2018;19:957. doi: 10.3390/ijms19040957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Franco M., Pérez-Méndez O., Kulthinee S., Navar L.G. Integration of purinergic and angiotensin II receptor function in renal vascular responses and renal injury in angiotensin II-dependent hypertension. Purinergic Signal. 2019;1–9 doi: 10.1007/s11302-019-09662-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Reshi M.L., Su Y.-C., Hong J.-R. RNA viruses: ROS-mediated cell death. Int. J. Cell Biol. 2014;2014 doi: 10.1155/2014/467452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Molteni C.G., Principi N., Esposito S. Reactive oxygen and nitrogen species during viral infections. Free Radic. Res. 2014;48:1163–1169. doi: 10.3109/10715762.2014.945443. [DOI] [PubMed] [Google Scholar]
- 57.Y. Zhou Y. Hou J. Shen Y. Huang W. Martin F.C.-C. Discovery , Undefined 2020, Network-based Drug Repurposing for Novel Coronavirus 2019-nCoV/SARS-CoV-2, Nature.Com. (n.d.). https://www.nature.com/articles/s41421-020-0153-3. [DOI] [PMC free article] [PubMed]
- 58.Delgado-Roche L., Mesta F. Oxidative stress as key player in severe acute respiratory syndrome coronavirus (SARS-CoV) infection. Arch. Med. Res. 2020;51:384–387. doi: 10.1016/j.arcmed.2020.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Orellana J.A., Velasquez S., Williams D.W., Saez J.C., Berman J.W., Eugenin E.A. Pannexin1 hemichannels are critical for HIV infection of human primary CD4+ T lymphocytes. J. Leukoc. Biol. 2013;94:399–407. doi: 10.1189/jlb.0512249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Potey P.M.D., Rossi A.G., Lucas C.D., Dorward D.A. Neutrophils in the initiation and resolution of acute pulmonary inflammation: understanding biological function and therapeutic potential. J. Pathol. 2019;247:672–685. doi: 10.1002/path.5221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sumoza-Toledo A., Penner R. TRPM2: a multifunctional ion channel for calcium signalling. J. Physiol. 2011;589:1515–1525. doi: 10.1113/jphysiol.2010.201855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ishii M., Shimizu S., Hagiwara T., Wajima T., Miyazaki A., Mori Y., Kiuchi Y. Extracellular-added ADP-ribose increases intracellular free Ca2+ concentration through Ca2+ release from stores, but not through TRPM2-mediated Ca2+ entry, in rat β-cell line RIN-5F. J. Pharmacol. Sci. 2006;101:174–178. doi: 10.1254/jphs.scj06001x. [DOI] [PubMed] [Google Scholar]
- 63.Tsukimoto M. Purinergic signaling is a novel mechanism of the cellular response to ionizing radiation. Biol. Pharm. Bull. 2015;38:951–959. doi: 10.1248/bpb.b15-00062. [DOI] [PubMed] [Google Scholar]
- 64.Sardu C., Gambardella J., Morelli M.B., Wang X., Marfella R., Santulli G. Clinical and basic evidence. 2020. Is COVID-19 an endothelial disease? [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Varga Z., Flammer A.J., Steiger P., Haberecker M., Andermatt R., Zinkernagel A.S., Mehra M.R., Schuepbach R.A., Ruschitzka F., Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bermejo-Martin J.F., Almansa R., Menéndez R., Mendez R., Kelvin D.J., Torres A. Lymphopenic community acquired pneumonia as signature of severe COVID-19 infection. J. Infect. 2020;80 doi: 10.1016/j.jinf.2020.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Good M.E., Begandt D., DeLalio L.J., Keller A.S., Billaud M., Isakson B.E. 2015. Emerging Concepts Regarding Pannexin 1 in the Vasculature. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yang Y., Delalio L.J., Best A.K., Macal E., Milstein J., Donnelly I., Miller A.M., McBride M., Shu X., Koval M. Endothelial pannexin 1 channels control inflammation by regulating intracellular calcium. J. Immunol. 2020;204:2995–3007. doi: 10.4049/jimmunol.1901089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zaim S., Chong J.H., Sankaranarayanan V., Harky A. COVID-19 and multi-organ response. Curr. Probl. Cardiol. 2020;100618 doi: 10.1016/j.cpcardiol.2020.100618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.X. Yang Y. Yu J. Xu H. Shu H. Liu Y. Wu … L.Z.-T.L.R. , Undefined 2020, Clinical Course and Outcomes of Critically Ill Patients With SARS-CoV-2 Pneumonia in Wuhan, China: A Single-centered, Retrospective, Observational Study, Elsevier. (n.d.). https://www.sciencedirect.com/science/article/pii/S2213260020300795. [DOI] [PMC free article] [PubMed]
- 71.Gupta A., Madhavan M.V., Sehgal K., Nair N., Mahajan S., Sehrawat T.S., Bikdeli B., Ahluwalia N., Ausiello J.C., Wan E.Y. Extrapulmonary manifestations of COVID-19. Nat. Med. 2020;26:1017–1032. doi: 10.1038/s41591-020-0968-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.George P.M., Wells A.U., Jenkins R.G. Pulmonary fibrosis and COVID-19: the potential role for antifibrotic therapy. Lancet Respir. Med. 2020;8:807–815. doi: 10.1016/S2213-2600(20)30225-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Le T.-T., Berg N., Harting M., Li X., Eltzschig H.K., Yuan X. Purinergic signaling in pulmonary inflammation. Front. Immunol. 2019;10:1633. doi: 10.3389/fimmu.2019.01633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kuebler W.M., Jordt S.-E., Liedtke W.B. Urgent reconsideration of lung edema as a preventable outcome in COVID-19: inhibition of TRPV4 represents a promising and feasible approach. Am. J. Physiol. Cell. Mol. Physiol. 2020;318:L1239–L1243. doi: 10.1152/ajplung.00161.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Rahman M., Sun R., Mukherjee S., Nilius B., Janssen L.J. TRPV4 stimulation releases ATP via pannexin channels in human pulmonary fibroblasts. Am. J. Respir. Cell Mol. Biol. 2018;59:87–95. doi: 10.1165/rcmb.2017-0413OC. [DOI] [PubMed] [Google Scholar]
- 76.Seminario-Vidal L., Okada S.F., Sesma J.I., Kreda S.M., van Heusden C.A., Zhu Y., Jones L.C., O’Neal W.K., Penuela S., Laird D.W. Rho signaling regulates pannexin 1-mediated ATP release from airway epithelia. J. Biol. Chem. 2011;286:26277–26286. doi: 10.1074/jbc.M111.260562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Diezmos E.F., Markus I., Perera D.S., Gan S., Zhang L., Sandow S.L., Bertrand P.P., Liu L. Blockade of Pannexin-1 channels and purinergic P2X7 receptors shows protective effects against cytokines-induced colitis of human colonic mucosa. Front. Pharmacol. 2018;9:865. doi: 10.3389/fphar.2018.00865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ohbuchi T., Suzuki H. Synchronized roles of pannexin and connexin in nasal mucosal epithelia. Eur. Arch. Oto-Rhino-Laryngol. 2018;275:1657–1661. doi: 10.1007/s00405-018-4947-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shi Y., Wang Y., Shao C., Huang J., Gan J., Huang X., Bucci E., Piacentini M., Ippolito G., Melino G. 2020. COVID-19 Infection: The Perspectives on Immune Responses. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Aggarwal G., Cheruiyot I., Aggarwal S., Wong J., Lippi G., Lavie C.J., Henry B.M., Sanchis-Gomar F. Association of cardiovascular disease with coronavirus disease 2019 (COVID-19) severity: a meta-analysis. Curr. Probl. Cardiol. 2020;45 doi: 10.1016/j.cpcardiol.2020.100617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Li H., Liu L., Zhang D., Xu J., Dai H., Tang N., Su X., Cao B. SARS-CoV-2 and viral sepsis: observations and hypotheses. Lancet. 2020;395:1517–1520. doi: 10.1016/S0140-6736(20)30920-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Burnstock G. Purinergic signaling in the cardiovascular system. Circ. Res. 2017;120:207–228. doi: 10.1161/CIRCRESAHA.116.309726. [DOI] [PubMed] [Google Scholar]
- 83.Guerra Martinez C. P2X7 receptor in cardiovascular disease: the heart side. Clin. Exp. Pharmacol. Physiol. 2019;46:513–526. doi: 10.1111/1440-1681.13079. [DOI] [PubMed] [Google Scholar]
- 84.Fu L.-W., Longhurst J.C. A new function for ATP: activating cardiac sympathetic afferents during myocardial ischemia. Am. J. Physiol. Circ. Physiol. 2010;299:H1762–H1771. doi: 10.1152/ajpheart.00822.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kim J., Woo S. Shear stress induces a longitudinal Ca2+ wave via autocrine activation of P2Y1 purinergic signalling in rat atrial myocytes. J. Physiol. 2015;593:5091–5109. doi: 10.1113/JP271016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zhou Z., Matsumoto T., Jankowski V., Pernow J., Mustafa S.J., Duncker D.J., Merkus D. Uridine adenosine tetraphosphate and purinergic signaling in cardiovascular system: an update. Pharmacol. Res. 2019;141:32–45. doi: 10.1016/j.phrs.2018.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kow C.S., Hasan S.S. The use of antiplatelet agents for arterial thromboprophylaxis in COVID-19. Rev. Esp. Cardiol. (Engl. Ed). 2021;74:114. doi: 10.1016/j.rec.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Levi M., Thachil J., Iba T., Levy J.H. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet. Haematol. 2020;7 doi: 10.1016/S2352-3026(20)30145-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Storey R.F. New P2Y12 inhibitors. Heart. 2011;97:1262–1267. doi: 10.1136/hrt.2009.184242. [DOI] [PubMed] [Google Scholar]
- 90.Isakson B.E. A review of the current state of pannexin channels as they relate to the blood vessel wall. J. Med. Sci. 2017;37:179. [Google Scholar]
- 91.Sun S., Cai X., Wang H., He G., Lin Y., Lu B., Chen C., Pan Y., Hu X. Abnormalities of peripheral blood system in patients with COVID-19 in Wenzhou, China. Clinica Chimica Acta. 2020;507:174–180. doi: 10.1016/j.cca.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Begandt D., Good M.E., Keller A.S., DeLalio L.J., Rowley C., Isakson B.E., Figueroa X.F. Pannexin channel and connexin hemichannel expression in vascular function and inflammation. BMC Cell Biol. 2017;18:1–16. doi: 10.1186/s12860-016-0119-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Keller A.S., Diederich L., Panknin C., DeLalio L.J., Drake J.C., Sherman R., Jackson E.K., Yan Z., Kelm M., Cortese-Krott M.M. Possible roles for ATP release from RBCs exclude the cAMP-mediated Panx1 pathway. Am. J. Physiol. Physiol. 2017;313:C593–C603. doi: 10.1152/ajpcell.00178.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sikora J., Orlov S.N., Furuya K., Grygorczyk R. Hemolysis is a primary ATP-release mechanism in human erythrocytes, blood. J. Am. Soc. Hematol. 2014;124:2150–2157. doi: 10.1182/blood-2014-05-572024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Poudel N., Okusa M.D. Pannexins in acute kidney injury. Nephron. 2019;143:158–161. doi: 10.1159/000501278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Chen H., Xuan B., Yan Y., Zhu X., Shen C., Zhao G., Ji L., Xu D., Xiong H., Yu T. Profiling ACE2 expression in colon tissue of healthy adults and colorectal cancer patients by single-cell transcriptome analysis. MedRxiv. 2020 doi: 10.1101/2020.02.15.20023457. [DOI] [Google Scholar]
- 97.Diezmos E.F., Bertrand P.P., Liu L. Purinergic signaling in gut inflammation: the role of connexins and pannexins. Front. Neurosci. 2016;10:311. doi: 10.3389/fnins.2016.00311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhang C., Shi L., Wang F.-S. Liver injury in COVID-19: management and challenges. lancetGastroenterol. Hepatol. 2020;5:428–430. doi: 10.1016/S2468-1253(20)30057-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Cannistrà M., Ruggiero M., Zullo A., Gallelli G., Serafini S., Maria M., Naso A., Grande R., Serra R., Nardo B. Hepatic ischemia reperfusion injury: a systematic review of literature and the role of current drugs and biomarkers. Int. J. Surg. 2016;33:S57–S70. doi: 10.1016/j.ijsu.2016.05.050. [DOI] [PubMed] [Google Scholar]
- 100.Velázquez-Miranda E., Díaz-Muñoz M., Vázquez-Cuevas F.G. Purinergic signaling in hepatic disease. Purinergic Signal. 2019;1–13 doi: 10.1007/s11302-019-09680-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Dallan C., Romano F., Siebert J., Politi S., Lacroix L., Sahyoun C. Septic shock presentation in adolescents with COVID-19. Lancet Child Adolesc. Heal. 2020;4:e21–e23. doi: 10.1016/S2352-4642(20)30164-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Chen W., Zhu S., Wang Y., Li J., Qiang X., Zhao X., Yang H., D’Angelo J., Becker L., Wang P. Enhanced macrophage pannexin 1 expression and hemichannel activation exacerbates lethal experimental sepsis. Sci. Rep. 2019;9:1–12. doi: 10.1038/s41598-018-37232-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Altable M., de la Serna J.M. Neuropsychiatry and COVID-19: An Overview. Qeios. 2020 [Google Scholar]
- 104.Norouzi M., Miar P., Norouzi S., Nikpour P. Nervous system involvement in COVID-19: a review of the current knowledge. Mol. Neurobiol. 2021;58:3561–3574. doi: 10.1007/s12035-021-02347-4. [DOI] [PubMed] [Google Scholar]
- 105.Scemes E., Velíšková J. Exciting and not so exciting roles of pannexins. Neurosci. Lett. 2019;695:25–31. doi: 10.1016/j.neulet.2017.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.North R.A., Verkhratsky A. Purinergic transmission in the central nervous system. Pflügers Arch. 2006;452:479–485. doi: 10.1007/s00424-006-0060-y. [DOI] [PubMed] [Google Scholar]
- 107.Franklin T.C., Xu C., Duman R.S. Depression and sterile inflammation: essential role of danger associated molecular patterns. Brain Behav. Immun. 2018;72:2–13. doi: 10.1016/j.bbi.2017.10.025. [DOI] [PubMed] [Google Scholar]
- 108.Bhattacharya A., Jones D.N.C. Emerging role of the P2X7-NLRP3-IL1β pathway in mood disorders. Psychoneuroendocrinology. 2018;98:95–100. doi: 10.1016/j.psyneuen.2018.08.015. [DOI] [PubMed] [Google Scholar]
- 109.Emanuela F., Grazia M., Marco D.R., Maria Paola L., Giorgio F., Marco B. Inflammation as a link between obesity and metabolic syndrome. J Nutr. Metab. 2012;2012 doi: 10.1155/2012/476380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Li Q., Barres B.A. Microglia and macrophages in brain homeostasis and disease. Nat. Rev. Immunol. 2018;18:225. doi: 10.1038/nri.2017.125. [DOI] [PubMed] [Google Scholar]
- 111.Adinolfi E., Giuliani A.L., De Marchi E., Pegoraro A., Orioli E., Di Virgilio F. The P2X7 receptor: a main player in inflammation. Biochem. Pharmacol. 2018;151:234–244. doi: 10.1016/j.bcp.2017.12.021. [DOI] [PubMed] [Google Scholar]
- 112.Wang D., Wang H., Gao H., Zhang H., Zhang H., Wang Q., Sun Z. P2X7 receptor mediates NLRP3 inflammasome activation in depression and diabetes. Cell Biosci. 2020;10:1–9. doi: 10.1186/s13578-020-00388-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bhattacharya A. Recent advances in CNS P2X7 physiology and pharmacology: focus on neuropsychiatric disorders. Front. Pharmacol. 2018;9:30. doi: 10.3389/fphar.2018.00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lechien J.R., Chiesa-Estomba C.M., De Siati D.R., Horoi M., Le Bon S.D., Rodriguez A., Dequanter D., Blecic S., El Afia F., Distinguin L. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter european study. Eur. Arch. Oto-Rhino-Laryngol. 2020:1–11. doi: 10.1007/s00405-020-05965-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Whyte-Fagundes P., Siu R., Brown C., Zoidl G. Pannexins in vision, hearing, olfaction and taste. Neurosci. Lett. 2019;695:32–39. doi: 10.1016/j.neulet.2017.05.010. [DOI] [PubMed] [Google Scholar]
- 116.Kurtenbach S., Whyte-Fagundes P., Gelis L., Kurtenbach S., Brazil É., Zoidl C., Hatt H., Shestopalov V.I., Zoidl G. Investigation of olfactory function in a Panx1 knock out mouse model. Front. Cell. Neurosci. 2014;8:266. doi: 10.3389/fncel.2014.00266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Eizirik D.L., Darville M.I. Beta-cell apoptosis and defense mechanisms: lessons from type 1 diabetes. Diabetes. 2001;50:S64. doi: 10.2337/diabetes.50.2007.s64. [DOI] [PubMed] [Google Scholar]
- 118.Yang J.-K., Lin S.-S., Ji X.-J., Guo L.-M. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol. 2010;47:193–199. doi: 10.1007/s00592-009-0109-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Li J., Wang X., Chen J., Zuo X., Zhang H., Deng A. COVID-19 infection may cause ketosis and ketoacidosis. Diabetes Obes Metab . 2020;22:1935–1941. doi: 10.1111/dom.14057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Fang L., Karakiulakis G., Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir. Med. 2020;8 doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Simonnet A., Chetboun M., Poissy J., Raverdy V., Noulette J., Duhamel A., Labreuche J., Mathieu D., Pattou F., Jourdain M., LICORN and the Lille COVID-19 and Obesity study group High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity (Silver Spring). 2020;28:1195–1199. doi: 10.1002/oby.22831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.McClean K.M., Kee F., Young I.S., Elborn J.S. Obesity and the lung: 1· epidemiology. Thorax. 2008;63:649–654. doi: 10.1136/thx.2007.086801. [DOI] [PubMed] [Google Scholar]
- 123.Hibbert K., Rice M., Malhotra A. Obesity and ARDS. Chest. 2012;142:785–790. doi: 10.1378/chest.12-0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Rajala M.W., Scherer P.E. Minireview: the adipocyte—at the crossroads of energy homeostasis, inflammation, and atherosclerosis. Endocrinology. 2003;144:3765–3773. doi: 10.1210/en.2003-0580. [DOI] [PubMed] [Google Scholar]
- 125.Tozzi M., Larsen A.T., Lange S.C., Giannuzzo A., Andersen M.N., Novak I. The P2X7 receptor and pannexin-1 are involved in glucose-induced autocrine regulation in β-cells. Sci. Rep. 2018;8:1–15. doi: 10.1038/s41598-018-27281-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Solini A., Novak I. Role of the P2X7 receptor in the pathogenesis of type 2 diabetes and its microvascular complications. Curr. Opin. Pharmacol. 2019;47:75–81. doi: 10.1016/j.coph.2019.02.009. [DOI] [PubMed] [Google Scholar]
- 127.Beaucage K.L., Xiao A., Pollmann S.I., Grol M.W., Beach R.J., Holdsworth D.W., Sims S.M., Darling M.R., Dixon S.J. Loss of P2X7 nucleotide receptor function leads to abnormal fat distribution in mice. Purinergic Signal. 2014;10:291–304. doi: 10.1007/s11302-013-9388-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Coccurello R., Volonté C. P2X7 receptor in the management of energy homeostasis: implications for obesity, dyslipidemia, and insulin resistance. Front. Endocrinol. (Lausanne) 2020;11:199. doi: 10.3389/fendo.2020.00199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Adamson S.E., Meher A.K., Chiu Y., Sandilos J.K., Oberholtzer N.P., Walker N.N., Hargett S.R., Seaman S.A., Peirce-Cottler S.M., Isakson B.E. Pannexin 1 is required for full activation of insulin-stimulated glucose uptake in adipocytes. Mol. Metab. 2015;4:610–618. doi: 10.1016/j.molmet.2015.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Tozzi M., Hansen J.B., Novak I. Pannexin-1 mediated ATP release in adipocytes is sensitive to glucose and insulin and modulates lipolysis and macrophage migration. Acta Physiol. 2020;228 doi: 10.1111/apha.13360. [DOI] [PubMed] [Google Scholar]
- 131.Wei C., Friedman A.J. COVID-19 pandemic: are there unique cutaneous manifestations in patients infected with SARS-CoV-2? J. Drugs Dermatol. 2020;19:554–555. [PubMed] [Google Scholar]
- 132.Gianotti R., Veraldi S., Recalcati S., Cusini M., Ghislanzoni M., Boggio F., Fox L.P. Cutaneous clinico-pathological findings in three COVID-19-positive patients observed in the metropolitan area of Milan, Italy. Acta Derm. Venereol. 2020;100:1–2. doi: 10.2340/00015555-3490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Recalcati S., Barbagallo T., Frasin L.A., Prestinari F., Cogliardi A., Provero M.C., Dainese E., Vanzati A., Fantini F. Acral cutaneous lesions in the time of COVID-19. J. Eur. Acad. Dermatology Venereol. 2020;34:e346–e347. doi: 10.1111/jdv.16533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Penuela S., Bhalla R., Gong X.-Q., Cowan K.N., Celetti S.J., Cowan B.J., Bai D., Shao Q., Laird D.W. Pannexin 1 and pannexin 3 are glycoproteins that exhibit many distinct characteristics from the connexin family of gap junction proteins. J. Cell Sci. 2007;120:3772–3783. doi: 10.1242/jcs.009514. [DOI] [PubMed] [Google Scholar]
- 135.Cowan K.N., Langlois S., Penuela S., Cowan B.J., Laird D.W. Pannexin1 and Pannexin3 exhibit distinct localization patterns in human skin appendages and are regulated during keratinocyte differentiation and carcinogenesis. Cell Commun. Adhes. 2012;19:45–53. doi: 10.3109/15419061.2012.712575. [DOI] [PubMed] [Google Scholar]
- 136.Penuela S., Kelly J.J., Churko J.M., Barr K.J., Berger A.C., Laird D.W. Panx1 regulates cellular properties of keratinocytes and dermal fibroblasts in skin development and wound healing. J. Invest. Dermatol. 2014;134:2026–2035. doi: 10.1038/jid.2014.86. [DOI] [PubMed] [Google Scholar]
- 137.Burnstock G., Knight G.E., Greig A.V.H. Purinergic signaling in healthy and diseased skin. J. Invest. Dermatol. 2012;132:526–546. doi: 10.1038/jid.2011.344. [DOI] [PubMed] [Google Scholar]
- 138.Wang D., Huang N., Heppel L.A. Extracellular ATP shows synergistic enhancement of DNA synthesis when combined with agents that are active in wound healing or as neurotransmitters. Biochem. Biophys. Res. Commun. 1990;166:251–258. doi: 10.1016/0006-291x(90)91938-o. [DOI] [PubMed] [Google Scholar]
- 139.Geraghty N., Watson D., Adhikary S., Sluyter R. 2016. P2X7 Receptor in Skin Biology and Diseases. [Google Scholar]
- 140.Xu J., Shi P.-Y., Li H., Zhou J. Broad spectrum antiviral agent niclosamide and its therapeutic potential. ACS Infect. Dis. 2020;6:909–915. doi: 10.1021/acsinfecdis.0c00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Perwitasari O., Yan X., Johnson S., White C., Brooks P., Tompkins S.M., Tripp R.A. Targeting organic anion transporter 3 with probenecid as a novel anti-influenza a virus strategy. Antimicrob. Agents Chemother. 2013;57:475–483. doi: 10.1128/AAC.01532-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Rayner C.R., Chanu P., Gieschke R., Boak L.M., Jonsson E.N. Population pharmacokinetics of oseltamivir when coadministered with probenecid. J. Clin. Pharmacol. 2008;48:935–947. doi: 10.1177/0091270008320317. [DOI] [PubMed] [Google Scholar]
- 143.Bhaskaracharya A., Dao-Ung P., Jalilian I., Spildrejorde M., Skarratt K.K., Fuller S.J., Sluyter R., Stokes L. Probenecid blocks human P2X7 receptor-induced dye uptake via a pannexin-1 independent mechanism. PLoS One. 2014;9 doi: 10.1371/journal.pone.0093058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Wei R., Wang J., Xu Y., Yin B., He F., Du Y., Peng G., Luo B. Probenecid protects against cerebral ischemia/reperfusion injury by inhibiting lysosomal and inflammatory damage in rats. Neuroscience. 2015;301:168–177. doi: 10.1016/j.neuroscience.2015.05.070. [DOI] [PubMed] [Google Scholar]
- 145.Zhou Y., Vedantham P., Lu K., Agudelo J., Carrion R., Jr., Nunneley J.W., Barnard D., Pöhlmann S., McKerrow J.H., Renslo A.R. Protease inhibitors targeting coronavirus and filovirus entry. Antivir. Res. 2015;116:76–84. doi: 10.1016/j.antiviral.2015.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Good M.E., Chiu Y.-H., Poon I.K.H., Medina C.B., Butcher J.T., Mendu S.K., DeLalio L.J., Lohman A.W., Leitinger N., Barrett E. Pannexin 1 channels as an unexpected new target of the anti-hypertensive drug spironolactone. Circ. Res. 2018;122:606–615. doi: 10.1161/CIRCRESAHA.117.312380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Cadegiani F.A. Can spironolactone be used to prevent COVID-19-induced acute respiratory distress syndrome in patients with hypertension? Am. J. Physiol. Metab. 2020;318:E587–E588. doi: 10.1152/ajpendo.00136.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Feig J.L., Mediero A., Corciulo C., Liu H., Zhang J., Perez-Aso M., Picard L., Wilder T., Cronstein B. The antiviral drug tenofovir, an inhibitor of Pannexin-1-mediated ATP release, prevents liver and skin fibrosis by downregulating adenosine levels in the liver and skin. PLoS One. 2017;12 doi: 10.1371/journal.pone.0188135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Boyce A.K.J., Swayne L.A. P2X7 receptor cross-talk regulates ATP-induced pannexin 1 internalization. Biochem. J. 2017;474:2133–2144. doi: 10.1042/BCJ20170257. [DOI] [PubMed] [Google Scholar]
- 150.Deng Z., He Z., Maksaev G., Bitter R.M., Rau M., Fitzpatrick J.A.J., Yuan P. Cryo-EM structures of the ATP release channel pannexin 1. Nat. Struct. Mol. Biol. 2020;27:373–381. doi: 10.1038/s41594-020-0401-0. [DOI] [PubMed] [Google Scholar]
- 151.Michalski K., Syrjanen J.L., Henze E., Kumpf J., Furukawa H., Kawate T. The cryo-EM structure of pannexin 1 reveals unique motifs for ion selection and inhibition. elife. 2020;9 doi: 10.7554/eLife.54670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Robbins B.L., Srinivas R.V., Kim C., Bischofberger N., Fridland A. Anti-human immunodeficiency virus activity and cellular metabolism of a potential prodrug of the acyclic nucleoside phosphonate 9-R-(2-phosphonomethoxypropyl) adenine (PMPA), bis (isopropyloxymethylcarbonyl) PMPA. Antimicrob. Agents Chemother. 1998;42:612–617. doi: 10.1128/aac.42.3.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Elfiky A.A. Ribavirin, remdesivir, sofosbuvir, galidesivir, and tenofovir against SARS-CoV-2 RNA dependent RNA polymerase (RdRp): a molecular docking study. Life Sci. 2020;117592 doi: 10.1016/j.lfs.2020.117592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Lou L. Advances in nucleotide antiviral development from scientific discovery to clinical applications: tenofovir disoproxil fumarate for hepatitis B. J. Clin. Transl. Hepatol. 2013;1:33. doi: 10.14218/JCTH.2013.004XX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.De Clercq E. Tenofovir alafenamide (TAF) as the successor of tenofovir disoproxil fumarate (TDF) Biochem. Pharmacol. 2016;119:1–7. doi: 10.1016/j.bcp.2016.04.015. [DOI] [PubMed] [Google Scholar]
- 156.Chien M., Anderson T.K., Jockusch S., Tao C., Xiaoxu L., Kumar S., Russo J.J., Kirchdoerfer R.N., Ju J. Nucleotide Analogues as Inhibitors of SARS-CoV-2 Polymerase, a Key Drug Target for COVID-19. J Proteome Res. 2020;19:4690–4697. doi: 10.1021/acs.jproteome.0c00392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Wu C., Liu Y., Yang Y., Zhang P., Zhong W., Wang Y., Wang Q., Xu Y., Li M., Li X. Analysis of therapeutic targets for SARS-CoV-2 and discovery of potential drugs by computational methods. Acta Pharm. Sin. B. 2020;10:766–788. doi: 10.1016/j.apsb.2020.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Parienti J.-J., Prazuck T., Peyro-Saint-Paul L., Fournier A., Valentin C., Brucato S., Verdon R., Sève A., Colin M., Lesne F. Effect of tenofovir disoproxil fumarate and emtricitabine on nasopharyngeal SARS-CoV-2 viral load burden amongst outpatients with COVID-19: a pilot, randomized, open-label phase 2 trial. EClinicalMedicine. 2021;38 doi: 10.1016/j.eclinm.2021.100993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Del Amo J., Polo R., Moreno S., Díaz A., Martínez E., Arribas J.R., Jarrín I., Hernán M.A. Incidence and severity of COVID-19 in HIV-positive persons receiving antiretroviral therapy: a cohort study. Ann. Intern. Med. 2020;173:536–541. doi: 10.7326/M20-3689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Lohman A.W., Leskov I.L., Butcher J.T., Johnstone S.R., Stokes T.A., Begandt D., DeLalio L.J., Best A.K., Penuela S., Leitinger N. Pannexin 1 channels regulate leukocyte emigration through the venous endothelium during acute inflammation. Nat. Commun. 2015;6:1–12. doi: 10.1038/ncomms8965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Mathew H.R., Choi M.Y., Parkins M.D., Fritzler M.J. Systematic review: cystic fibrosis in the SARS-CoV-2/COVID-19 pandemic. BMC Pulm. Med. 2021;21:1–11. doi: 10.1186/s12890-021-01528-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Abraham E.H., Guidotti G., Rapaport E., Bower D., Brown J., Griffin R.J., Donnelly A., Waitzkin E.D., Qamar K., Thompson M.A. Cystic fibrosis improves COVID-19 survival and provides clues for treatment of SARS-CoV-2. Purinergic Signal. 2021;1–12 doi: 10.1007/s11302-021-09771-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Rabini R.A., Petruzzi E., Staffolani R., Tesei M., Fumelli P., Pazzagli M., Mazzanti L. Diabetes mellitus and subjects’ ageing: a study on the ATP content and ATP-related enzyme activities in human erythrocytes. Eur. J. Clin. Investig. 1997;27:327–332. doi: 10.1046/j.1365-2362.1997.1130652.x. [DOI] [PubMed] [Google Scholar]
- 164.Ribeiro D.E., Oliveira-Giacomelli Á., Glaser T., Arnaud-Sampaio V.F., Andrejew R., Dieckmann L., Baranova J., Lameu C., Ratajczak M.Z., Ulrich H. Hyperactivation of P2X7 receptors as a culprit of COVID-19 neuropathology. Mol. Psychiatry. 2021;26:1044–1059. doi: 10.1038/s41380-020-00965-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Zyma M., Pawliczak R. Characteristics and the role of purinergic receptors in pathophysiology with focus on immune response: purinergic receptors are widely expressed in immune cells and regulate high variety of their functions, taking part in pathogenesis of many diseases. Int. Rev. Immunol. 2020;39:97–117. doi: 10.1080/08830185.2020.1723582. [DOI] [PubMed] [Google Scholar]