Abstract
Purpose
To describe the objective and design of the Fujian Eye Study and to introduce the general characteristics and vision condition of this study.
Methods
The Fujian Eye Study (FJES) is a population-based cross-sectional survey on the public eye health status of residents over 50 years old in the entire Fujian Province of Southern China, which contains both urban and rural areas and coastal and inland regions. 10,044 participants were enrolled using a two-stage cluster sampling design and underwent a questionnaire and a series of standard examinations both physical and ocular. The main subgroups of data collection included age, sex, region, refractive error, education background, income, eating habits, smartphone usage in the dark, complaints of eye discomfort, history of chronic diseases, consumption of tobacco, alcohol, or tea.
Results
8211 (81.8%) participants were finally included and were divided into urban populations (4678 subjects) and rural populations (3533 subjects) and coastal residents (6434 subjects) and inland residents (1777 subjects); 4836 participants were female. The mean age was 64.39 (SD 8.87) years (median 64 years; range 50–98 years). 227 (3.33%) had vision impairment (VI), 195 (2.87%) had low vision and 14 (0.21%) were blind. The mean presenting near visual acuity (PNVA) was 0.28 (0.17), the mean presenting distance visual acuity (PDVA) was 0.61 (0.30), and the mean best corrected visual acuity (BCVA) was 0.82 (0.28).
Conclusions
The FJES collected detailed questionnaire information and overall ocular and physical examinations, which provide the opportunity to identify risk factors and images of VI and eye diseases and to evaluate their associations with chronic diseases and basic personal information.
Keywords: Cross sectional, Epidemiology, Urban and rural, Coastal and inland, Eye diseases, Related factor, Visual acuity, Vision impairment
Introduction
Population-based studies could usually deliver the evidence for findings and hypotheses formulated on the basis of hospital-based investigations and provide new exploration directions and practical basis for basic experimental research. Previous major population-based studies in the field of Ophthalmology were mostly from United States [1, 2], Australia [3, 4], Western Europe [5, 6], South America [7], Middle East [8], Singapore [9, 10] and Japan [11]. China has a large population and great geographical differences. Although there have been several population-based surveys conducted in China, these have primarily been conducted in inland cities or nearby areas or coastal metropolitan area [12–14]. Eighty percent of Fujian Province is in a mountainous area, where transportation is inconvenient and economic and medical resources are limited. The lack of eye health data in Fujian Province attracted the attention of a National Natural Science Foundation of China (NSFC) applicant. Due to the specific geographical advantages of this location, we can obtain valuable ophthalmic survey data that may be a main focus of future attention.
The Fujian Eye Study (FJES) is a population-based cross-sectional on-site survey of eye health projects in public health of more than 10,000 residents in Fujian Province, southeastern China, which was part of the national “active health and aging science and technology response” key project. Our team crossed over 20,000 km and performed a field survey of more than 50 towns that covered both urban and rural areas and coastal and inland regions. This is the first ophthalmologic epidemiological survey of an entire coastal province of China to date. Previous eye surveys in China were in northern areas [12, 13], urban areas of southern China [14], eastern areas [15] and a national survey in nine inland provinces [16]. Our study was designed to examine the prevalence, relative factors and impact of eye diseases in noninstitutionalized, community-dwelling persons aged 50 years or older in Fujian Province to determine both modifiable and nonmodifiable risk factors that may be associated with ocular diseases and to understand the differences in and barriers to eye care services in these coastal and inland regions. At the same time, lectures about eye health and medical consulting services were provided for residents.
Methods
Study design
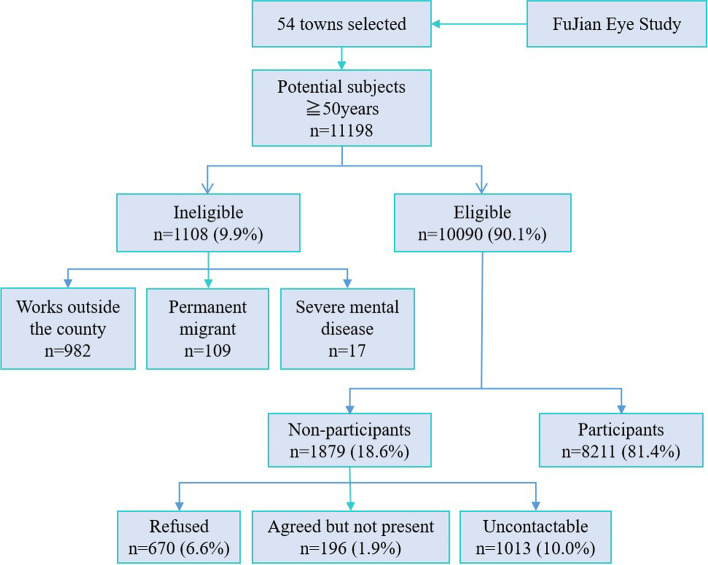
The FJES was performed from May 2018 to October 2019 as an ophthalmologic epidemiologic on-site survey on a random sample of coastal and inland, urban and rural Southern Chinese adults, reflecting the current eye health status of local Chinese people. The location of the study is illustrated in Fig. 1. We aimed to examine the distribution, trends and risk factors for eye diseases between different areas to explore the influence of genetic and environmental factors and the appropriate intervention measures for eye diseases. This research involved the digitization of image data, standardization of diagnosis, assistance by artificial intelligence and a combined study of genetic and environmental factors. It provides an overview of indigenous physical and eye health and is beneficial for global health management. A clinical study registry was obtained for the 2018–2019 FJES study (register number: ChiCTR2100043349) and the study protocol was approved by the Ethics Committee of Xiamen Eye Center affiliated with Xiamen University (Acceptance number: XMYKZX-KY-2018-001), and written informed consent was obtained from all participants. All residents in a community are officially registered at the local mayor’s office. Using this register as the sampling frame, all residents of the communities who were aged over 50 years were eligible for the study. We used a two-stage cluster sampling design where the clusters were first selected with probability proportional to cluster number, and then subjects are randomly sampled inside selected clusters. According to the data of the National Bureau of Statistics and Fujian Provincial Department Of Finance in 2017 (http://czt.fujian.gov.cn/zfxxgk/fdzdgknr/czzjgl/zjfpwj/201803/t20180329_4563507.htm), the permanent residents of Fujian Province was approximately 38.74 million and there were 2153 communities. Our finally total sample was 10,044 subjects, so we randomly selected 54 communities in an equal proportion manner, including 33 urban communities and 21 rural communities. Then we randomly selected subjects based on the register from each community according to the community size. Figure 2 summarizes the survey design and implementation details for the completed survey administration, including the survey field period, survey mode, total sample size and final sample size.
Fig. 1.
The geographical location of the Fujian Eye Study
Fig. 2.
Flowchart of recruitment in the Fujian Eye Study
Inclusion and exclusion criteria
Inclusion criteria
-
I.
Officially registered at the local mayor’s office
-
II.
Age over 50 years
-
III.
Live and work in the county right now
-
IV.
Good mental state, and able to cooperate with the examination
Exclusion criteria
-
I.
Not officially registered at the local mayor’s office
-
II.
Age less than 50 years
-
III.
Not live or work in the county right now
-
IV.
Permanent migrant
-
V.
Have severe mental disease which can not cooperate the inspection
Sample size considerations
The following calculation formula was used to estimate the sample size: n = deff×μα2 × p × (1-p)/d2. The present study can achieve a precision of 0.05 (d), considering confidence interval of 95% (bilateral), μα2 of 1.96, design effect of 2, relative error of 0.15 and d = r × p. The sample size was targeted to achieve an adequate precision around estimates of prevalence and to allow for risk factor analyses to be carried out. As the prevalence of the main eye diseases in cross-sectional baseline surveys were estimated to be greater than 2.0% [6, 17–20]. Based on the data above and the response rate of pilot study (about 85%), 10,044 subjects would be recruited in this study. According to the data of the National Bureau of Statistics in 2017 [21], the permanent population of Fujian Province was about 38.74 million with 14.0% aged 50 to 59 years, 10.0% aged 60 to 69 years, 4.3% aged 70 to 79 years, and 1.8% aged 80 years and older, including 24.64 million urban population and 14.1 million rural population (58.1%: 41.9%) or a coastal population of 30.90 million and an inland population of 7.84 million (79.8%: 20.2%). Therefore, a total of 5836 urban and 4208 rural residents or 8015 coastal and 2029 inland residents were needed.
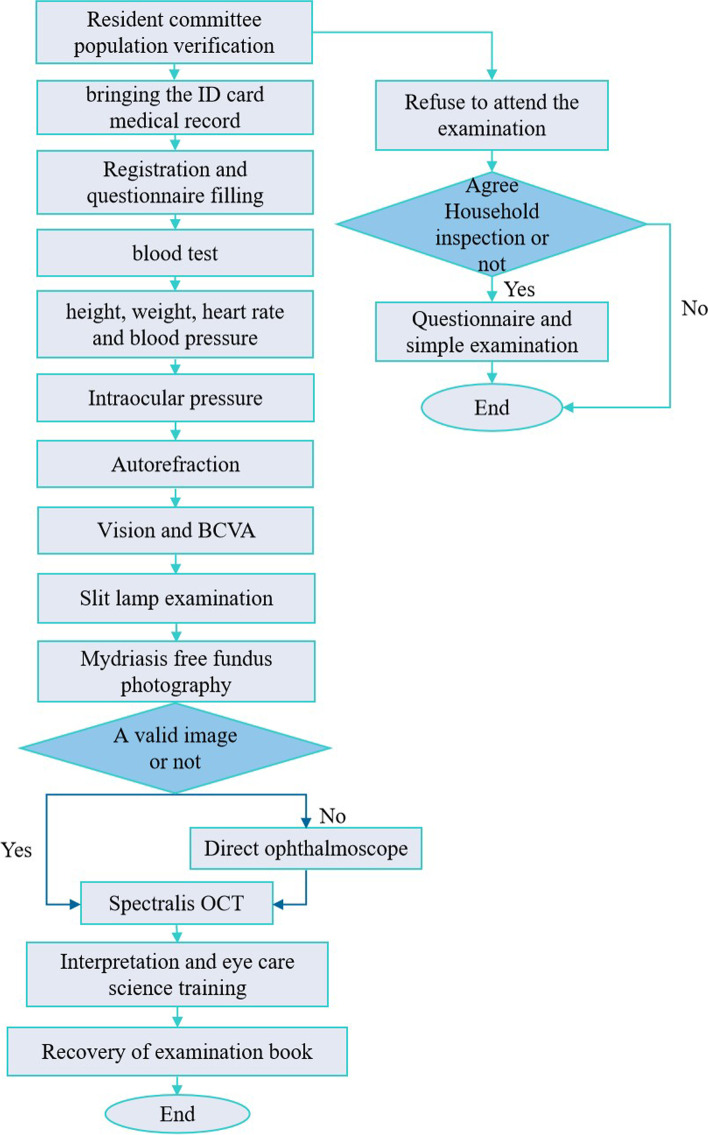
Survey constructs and measures
The FJES provides exhaustive longitudinal information including sociodemographic and administrative data (sex, age, nationality, etc.), physical data (height, weight, body mass index (BMI), heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), blood index) and ocular data (presenting near visual acuity (PNVA); presenting distance visual acuity (PDVA); refractive state; best corrected visual acuity (BCVA); intraocular pressure (IOP); slit lamp examination and fundus examinations (nonmydriatic color fundus photography and multicolour optical coherence tomography (OCT)) data. The process of on-site inspection is shown schematically in Fig. 3.
Fig. 3.
Flowchart of on site inspection in the Fujian Eye Study
PDVA and BCVA were measured using E Standard Logarithmic Visual Acuity Chart (GB 11533—1989) at a distance of 5 m. For results less than 0.1, PDVA and BCVA at a distance of 1 m were tested. If that was not possible, finger counting, hand movement, and light perception were tested.
NVA was measured by logarithmic visual acuity chart at a distance of 30 cm, followed the WHO definitions of VI as BCVA in better eyes of < 20/60 or worse (equaled with 0.3 in E Standard Logarithmic Visual Acuity Chart (GB 11533—1989)) and blindness as BCVA in better eyes worse than 20/400 (equaled with 0.05 in E Standard Logarithmic Visual Acuity Chart (GB 11533—1989)), defined PNVI as PNVA worse than 20/50 (equaled with 0.4 in our logarithmic near visual acuity chart) and defined presbyopia as PNVA worse than 20/50 and BCVA better than 20/40 (equaled with 0.5 in E Standard Logarithmic Visual Acuity Chart (GB 11533—1989)).
The Lens Opacities Classification System III (LOCS III) was used to evaluate the type of cataract. It consisted of six slit-lamp images for grading nuclear colour (NC) and nuclear opalescence (NO), five retroillumination images for grading cortical cataracts (C), and five retroillumination images for grading posterior subcapsular (P) cataracts [22].
A fundus photograph of each eye was taken using a scanning laser device (Digital Fundus Camera, VISUCAM 524, Goeschwitzer Strasse 51–52, 07745 Jena, Germany), which has a resolution of 20 μm and is able to capture the fundus even through an undilated pupil. Fundus photography was used to take at least two fundus photographs following the operation rules, one centred on the macular disc and one centred on the optic disc.
Multicolour OCT (Spectralis OCT, Heidelberg Engineering GmbH 69,121, Heidelberg, Germany) was used for high-resolution imaging of the optic disc and central retina in both eyes. Prior to imaging, autokeratometry data were entered to correct for ocular magnification effects. The instrument’s eye-tracking software was used to minimize the effects of eye movements. If a lesion was visible, the lesion site was identified with multi-slice scanning images. The protocol for Multicolour OCT imaging for each eye was as follows [23].
Disc-centred scans
Forty-nine-line raster scan of a 15° × 10° area. The average of nine frames for each B-scan was used to improve quality.
Peripapillary retinal nerve fibre layer (RNFL) thickness measurements. A circular B-scan of the peripapillary RNFL was taken along a 3.5 mm-diameter (~ 12°) circle.
Optic nerve head radial and circle (ONH-RC) scan. Forty-eight equidistant (7.5° spaced) radials and three circle B-scans were obtained. Each radial B-scan was averaged from 25 frames and spanned 4.7 mm. The three circular B-scans were 3.5 mm (~ 11.5°–12.5°), 4.1 mm (~ 13.5°–14.5°) and 4.7 mm (~ 15.5°–16.5°) in diameter, and each was averaged from 100 frames. Prior to starting the scans, the ONH-RC programme automatically detected the foveal and Bruch’s membrane opening positions. The examiner checked and, if necessary, manually corrected the positions of these landmarks.
Foveal-centred scans
Thirty-one-line raster scan of a (30° × 25°). Each B-scan was averaged from nine frames.
Enhanced depth imaging of the macular. Each B-scan spanned approximately 8.6 mm (~ 30°), and the average of 100 frames for each scan was recorded for analysis.
Data quality
Before the on-site survey, all technicians and clinicians recruited were trained uniformly and needed to finish an examination, and each survey examination was required to be fixed consistently with the same technician. During our on-site survey, participants were asked to complete all the tests before they can get the final diagnosis report, in order to improve the response rate. In the aspect of data collation, double entry with EpiData v3.1 (EpiData for Windows, version 3.1, the EpiData Association, Denmark, Europe) was used to check the data to ensure the correctness of the data.
Data analysis
Stata/SE statistical software (Stata for Windows, version 15.1, StataCorp LLC, Lakeway Drive, College Station, TX, USA) was used to analyse the data. Data are provided as the mean ± standard deviation (SD). Only one randomly selected eye per subject was obtained for statistical analysis of visual acuity unless intraindividual intereye differences were evaluated. Analysis of variance (ANOVA) was applied to compare the mean among groups of normally distributed parameters. Chi-square (χ2) tests were used to compare proportions. Multiple regression models were used to examine the relation between visual acuity measurements and selected sociodemographic characteristics. Logistic regression was applied for the comparison of binary parameters versus categorical parameters and for the comparison of binary parameters versus continuous normally distributed parameters. Linear regression was applied for the comparison of normally distributed parameters. Logistic regression was used to examine the correlation degree of each group. The statistical correlations was reported as the correlation coefficient r and statistical strength of correlations was described using odds ratio (OR). Confidence intervals (CI, 95%) are presented. All described associations were derived from the multivariable statistical analysis, unless indicated otherwise. All P-values were two sided and less than 0.05 were considered statistically significant.
Results
A total of 8211 residents (response rate, 81.8%, 8211 out of 10,044) aged ≥50 years were eventually included, and 4836 (58.9%) were female. 4678 (57.0%) were from urban area, and 3533 (43.0%) were from rural area. 6434 (78.4%) were from coastal region, and 1777 (21.6%) were from inland region. The response rates were 80.2 and 84.0% for the urban population and rural population, respectively, and 80.3 and 87.6% for the coastal population and inland population, respectively. Mean age was 64.39 (SD 8.87) years (median 64 years; range 50–98 years). The proportion of age group population in this study was similar to that in China on the whole. Per Capital Annual Net Income in this rural area is 16,335 Yuan, approximately $2419 US, which is higher than the average annual income (11,969 Yuan, approximately $1773 US) per Capital of those living in rural areas throughout Mainland China, and 39,001 Yuan in urban area, approximately $5776 US, which is also higher than the average annual income (33,834 Yuan, approximately $5011 US) per Capital of those living in urban areas throughout Mainland China [24]. Table 1 summarizes the general information of the survey, including the total sample size, gender, region, age group, height, weight, body mass index (BMI), heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), refractive error, education and income in more detail.
Table 1.
Composition of the study population
| Total study | Urban population | Rural population | P value | 95% CI or χ2 | Coastal population | Inland population | P§ value | 95% CI or χ2 | |
|---|---|---|---|---|---|---|---|---|---|
| Number (subjects) | 8211 | 4678 | 3533 | 6434 | 1777 | ||||
| Sex | |||||||||
| Female | 4836 | 2697 | 2139 | 3804 | 1032 | ||||
| Male | 3375 | 1981 | 1394 | 2630 | 745 | ||||
| Age (years) | 64.39 (8.87) | 64.64 (8.66) | 64.05 (9.12) | 0.0028 | 0.2032 to 0.9775 | 64.49 (8.74) | 64.00 (9.30) | 0.0381 | 0.0272 to 0.9585 |
| Median | 64 | 64 | 64 | 64 | 63 | ||||
| Range | 50 to 98 | 50 to 98 | 50 to 95 | 50 to 98 | 50 to 93 | ||||
| Age group (%) | |||||||||
| 50 to 54 | 15.2 | 13.83 | 17.01 | < 0.0001 | 32.59 | 14.45 | 17.9 | < 0.0001 | 33.52 |
| 55 to 59 | 16.86 | 16.14 | 17.8 | 16.34 | 18.74 | ||||
| 60 to 64 | 19.45 | 20.16 | 18.51 | 20.13 | 16.99 | ||||
| 65 to 69 | 20.34 | 21.44 | 18.88 | 21.01 | 17.9 | ||||
| 70 to 74 | 14.54 | 15.24 | 13.61 | 14.78 | 13.67 | ||||
| 75 to 79 | 7.39 | 6.95 | 7.98 | 7.3 | 7.71 | ||||
| 80+ | 6.22 | 6.24 | 6.2 | 5.98 | 7.09 | ||||
| Height (cm) | 160.34 (7.97) | 160.69 (8.02) | 159.88 (7.89) | < 0.0001 | −1.1619 to −0.4578 | 160.32 (8.06) | 160.42 (7.66) | 0.6512 | −0.3289 to 0.5260 |
| Weight (cm) | 61.43 (10.09) | 61.86 (10.14) | 60.84 (9.99) | < 0.0001 | −1.4635 to − 0.5721 | 61.63 (10.14) | 60.67 (9.86) | 0.0005 | −1.4960 to − 0.4147 |
| BMI | 23.85 (3.26) | 23.91 (3.21) | 23.77 (3.33) | 0.0471 | −0.2905 to − 0.0019 | 23.94 (3.29) | 23.52 (3.14) | < 0.0001 | −0.5861 to − 0.2365 |
| HR (beats/min) | 79.08 (11.07) | 78.78 (10.83) | 79.48 (11.37) | 0.0048 | 0.2151 to 1.1966 | 79.12 (11.01) | 78.94 (11.29) | 0.5653 | −0.7702 to 0.4209 |
| SBP | 136.05 (21.24) | 134.27 (20.01) | 138.43 (22.57) | < 0.0001 | 3.2291 to 5.0956 | 136.35 (21.30) | 134.91 (20.99) | 0.0130 | −2.5784 to −0.3033 |
| DBP | 75.83 (12.54) | 75.46 (12.24) | 76.33 (12.91) | 0.0022 | 0.3101 to 1.4167 | 75.97 (12.69) | 75.33 (11.95) | 0.0641 | −1.3061 to 0.0373 |
| IOP | 13.88 (3.46) | 13.74 (3.41) | 14.06 (3.50) | < 0.0001 | 0.1754 to 0.4780 | 13.77 (3.43) | 14.29 (3.52) | < 0.0001 | 0.3396 to 0.7035 |
| Refractive error | 0.52 (2.73) | 0.51 (2.69) | 0.54 (2.78) | 0.68 | −0.1480 to 0.0966 | 0.62 (2.67) | 0.18 (2.90) | < 0.0001 | 0.2886 to 0.5835 |
| Median | 1 | 1 | 1 | 1 | 0.75 | ||||
| Range | −23.75 to + 14.50 | −23.25 to + 14.50 | − 23.75 to + 13.25 | −23.25 to + 14.50 | − 23.75 to + 7.25 | ||||
| Refraction group (D) (%) | |||||||||
| < −10.00 | 1.18 | 1.09 | 1.3 | 0.53 | 7.05 | 1.07 | 1.58 | < 0.0001 | 44.28 |
| − 10.00 to −6.00 | 1.24 | 1.43 | 0.99 | 1.1 | 1.74 | ||||
| − 6.00 to −3.00 | 3.47 | 14.22 | 3.4 | 2.97 | 5.29 | ||||
| − 3.00 to 0.00 | 14.27 | 14.43 | 14.07 | 13.94 | 15.48 | ||||
| 0 | 3.99 | 3.93 | 4.08 | 3.9 | 4.33 | ||||
| 0.00 to + 3.00 | 66.56 | 67.4 | 65.44 | 68.06 | 61.11 | ||||
| + 3.00 to + 5.00 | 3.9 | 3.74 | 4.1 | 3.99 | 3.55 | ||||
| + 5.00 to + 10.00 | 0.54 | 0.51 | 0.57 | 0.56 | 0.45 | ||||
| > + 10.00 | 0.05 | 0.02 | 0.08 | 0.06 | 0 | ||||
| Missing data | 4.8 | 3.91 | 5.97 | 4.34 | 6.47 | ||||
| Level of education (%) | |||||||||
| Illiteracy | 15.59 | 10.3 | 22.59 | < 0.0001 | 262.69 | 17.94 | 7.09 | < 0.0001 | 53.59 |
| Primary school | 18.52 | 16.03 | 21.82 | 20.33 | 11.99 | ||||
| Middle school | 37.72 | 38.24 | 37.02 | 40.95 | 26 | ||||
| College and above | 14.53 | 17.34 | 10.81 | 14.8 | 13.56 | ||||
| Missing data | 13.64 | 18.08 | 7.76 | 5.98 | 41.36 | ||||
| Income (%) | |||||||||
| < =2000 | 29.44 | 25.16 | 35.1 | < 0.0001 | 222.86 | 32.45 | 18.51 | < 0.0001 | 68.68 |
| 2000–5000 | 23.72 | 29.22 | 16.44 | 23.31 | 25.21 | ||||
| > 5000 | 7.21 | 8.49 | 5.52 | 7.82 | 5.01 | ||||
| Missing data | 39.63 | 37.13 | 42.94 | 36.42 | 51.27 | ||||
BMI body mass index, HR heart rate, SBP systolic blood pressure, DBP diastolic blood pressure, IOP intraocular pressure, D diopter, CI confidence intervals, χ2 the valve of Chi-squaire analysis
P Value, statistical significance of the difference between urban population group and rural population group; P§ Value, statistical significance of the difference between coastal population group and inland population group
In the FJES, 4836 were female, and 3375 were male. Among them, 4776 females and 3287 males had PDVA test results, 4257 females and 2566 males had BCVA results, and 4836 females and 3192 males had PNVA results. The mean PNVA was 0.28 (0.17), the mean presenting VA was 0.61 (0.30) and 0.23 (0.27) logMAR units, and the mean BCVA was 0.82 (0.28) and 0.08 (0.19) logMAR units. Table 2 shows the response rate of best corrected visual acuity by age among the study population in geographical populations. Table 3 reveals the frequency of uncorrected distance visual acuity and best corrected visual acuity in the better eye in this study. Based on the WHO definitions using BCVA, 227 (3.33%) had DVI, 195 (2.87%) had low vision and 14 (0.21%) were blind. 5509 (68.58%) had PNVI, 4279 (68.33%) were noted presbyopia, and 193 (2.85%) had combined both PNVI and DVI. Table 4 shows the VI number of different subgroups.
Table 2.
Response rate of best corrected visual acuity by age in the Fujian Eye Study
| Area | Age (years) | Registered | Examined | Response rate (%) | Region | Age (years) | Registered | Examined | Response rate (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | ||||
| Urban | 50–54 | 211 | 603 | 164 | 450 | 77.70% | 74.60% | Coastal | 50–54 | 313 | 830 | 242 | 641 | 77.30% | 77.20% |
| 55–59 | 247 | 737 | 195 | 528 | 78.90% | 71.60% | 55–59 | 343 | 982 | 262 | 735 | 76.40% | 74.80% | ||
| 60–64 | 372 | 845 | 260 | 545 | 69.90% | 64.50% | 60–64 | 471 | 1146 | 347 | 842 | 73.70% | 73.50% | ||
| 65–69 | 438 | 838 | 309 | 563 | 70.50% | 67.20% | 65–69 | 568 | 1100 | 425 | 903 | 74.80% | 82.10% | ||
| 70–74 | 350 | 518 | 242 | 356 | 69.10% | 68.70% | 70–74 | 445 | 688 | 332 | 500 | 74.60% | 72.70% | ||
| 75–79 | 187 | 229 | 123 | 148 | 65.80% | 64.60% | 75–79 | 275 | 313 | 201 | 219 | 73.10% | 70.00% | ||
| 80+ | 176 | 197 | 101 | 111 | 57.40% | 56.30% | 80+ | 215 | 266 | 140 | 171 | 65.10% | 64.30% | ||
| Total | 5948 | 4095 | 68.80% | Total | 7955 | 5880 | 73.90% | ||||||||
| Rural | 50–54 | 206 | 486 | 176 | 436 | 85.40% | 89.70% | Inland | 50–54 | 104 | 259 | 98 | 245 | 94.20% | 94.60% |
| 55–59 | 225 | 506 | 184 | 436 | 81.80% | 86.20% | 55–59 | 129 | 261 | 117 | 229 | 90.70% | 87.70% | ||
| 60–64 | 222 | 535 | 191 | 484 | 86.00% | 90.50% | 60–64 | 123 | 234 | 104 | 187 | 84.60% | 79.90% | ||
| 65–69 | 257 | 518 | 213 | 449 | 82.90% | 86.70% | 65–69 | 127 | 256 | 97 | 209 | 76.40% | 81.60% | ||
| 70–74 | 210 | 337 | 182 | 300 | 86.70% | 89.00% | 70–74 | 115 | 167 | 92 | 136 | 80.00% | 81.40% | ||
| 75–79 | 156 | 175 | 131 | 151 | 84.00% | 86.30% | 75–79 | 68 | 91 | 53 | 80 | 77.90% | 87.90% | ||
| 80+ | 118 | 148 | 94 | 115 | 79.70% | 77.70% | 80+ | 79 | 79 | 55 | 55 | 69.60% | 69.60% | ||
| Total | 4099 | 3542 | 86.40% | Total | 2092 | 1757 | 84.00% | ||||||||
Table 3.
Number of subjects stratified into groups of uncorrected distance visual acuity (n = 8178) and best corrected visual acuity (n = 6823) in the better eye in the Fujian Eye Study
| E chart | Visual acuity | Best corrected visual acuity | ||
|---|---|---|---|---|
| Frequency | Cumulative percentage | Frequency | Cumulative percentage | |
| 0 | 2 | 0.02 | 2 | 0.03 |
| LP | 4 | 0.07 | 4 | 0.09 |
| HM | 12 | 0.22 | 9 | 0.22 |
| FC | 9 | 0.33 | 4 | 0.28 |
| 0.01 | 5 | 0.39 | 2 | 0.31 |
| 0.02 | 19 | 0.62 | 7 | 0.41 |
| 0.03 | 1 | 0.64 | ||
| 0.04 | 27 | 0.97 | 3 | 0.45 |
| 0.05 | 5 | 1.03 | 1 | 0.47 |
| 0.06 | 30 | 1.39 | 5 | 0.54 |
| 0.07 | 1 | 1.41 | ||
| 0.08 | 25 | 1.71 | 9 | 0.67 |
| 0.09 | 2 | 1.74 | ||
| 0.1 | 78 | 2.69 | 22 | 1 |
| 0.12 | 93 | 3.83 | 25 | 1.36 |
| 0.15 | 146 | 5.61 | 27 | 1.76 |
| 0.2 | 140 | 7.32 | 43 | 2.39 |
| 0.25 | 291 | 10.88 | 64 | 3.33 |
| 0.3 | 353 | 15.2 | 110 | 4.94 |
| 0.4 | 572 | 22.19 | 194 | 7.78 |
| 0.5 | 1004 | 34.47 | 379 | 13.34 |
| 0.6 | 1223 | 49.43 | 606 | 22.22 |
| 0.8 | 2125 | 75.41 | 256 | 25.97 |
| 1 | 1669 | 95.82 | 4709 | 94.99 |
| 1.2 | 304 | 99.54 | 315 | 99.6 |
| 1.5 | 36 | 99.98 | 26 | 99.99 |
| 2 | 2 | 100 | 1 | 100 |
LP light perception, HM hand movements, FC finger counting
Table 4.
The number and correlation of present near vision impairment, presbyopia, distance vision impairment and combined vision impairment with different subgroups
| Number of Impairment | PNVI | χ2 | P value | presbyopia | χ2 | P value | DVI | χ2 | P value | Combined VI | χ2 | P value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Areas | Urban | 3057 | 10.29 | 0.001 | 2292 | 0.23 | 0.633 | 108 | 3.02 | 0.082 | 84 | 7.42 | 0.006 |
| Rural | 2452 | 1987 | 119 | 109 | |||||||||
| Coastal | 4300 | 1.34 | 0.247 | 3321 | 1.13 | 0.287 | 146 | 19.95 | < 0.001 | 130 | 9.54 | 0.002 | |
| Inland | 1209 | 958 | 81 | 63 | |||||||||
| Total | 5509 | 4279 | 227 | 193 | |||||||||
| Age group (years) | 50 to 54 | 592 | 334.56 | < 0.001 | 505 | 274.53 | < 0.001 | 21 | 205.8 | < 0.001 | 13 | 219.04 | < 0.001 |
| 55 to 59 | 868 | 740 | 11 | 9 | |||||||||
| 60 to 64 | 1125 | 910 | 29 | 23 | |||||||||
| 65 to 69 | 1244 | 979 | 41 | 34 | |||||||||
| 70 to 74 | 873 | 662 | 36 | 32 | |||||||||
| 75 to 79 | 438 | 288 | 32 | 29 | |||||||||
| 80+ | 369 | 195 | 57 | 53 | |||||||||
| Total | 5509 | 4279 | 227 | 193 | |||||||||
| Refraction group (D) | < −10.00 | 60 | 961.63 | < 0.001 | 26 | 880.36 | < 0.001 | 23 | 346.46 | < 0.001 | 15 | 217.96 | < 0.001 |
| -10.00 to −6.00 | 52 | 40 | 5 | 3 | |||||||||
| -6.00 to −3.00 | 103 | 70 | 9 | 6 | |||||||||
| -3.00 to 0.00 | 428 | 303 | 36 | 29 | |||||||||
| 0 | 143 | 122 | 5 | 5 | |||||||||
| 0.00 to + 3.00 | 4106 | 3333 | 43 | 39 | |||||||||
| + 3.00 to + 5.00 | 273 | 211 | 6 | 6 | |||||||||
| + 5.00 to + 10.00 | 36 | 25 | 3 | 3 | |||||||||
| > + 10.00 | 3 | 0 | 2 | 2 | |||||||||
| Total | 5204 | 4130 | 132 | 108 | |||||||||
| Education | Illiteracy | 1049 | 495.95 | < 0.001 | 794 | 367.64 | < 0.001 | 80 | 74.79 | < 0.001 | 75 | 83.55 | < 0.001 |
| Primary school | 1186 | 879 | 39 | 34 | |||||||||
| Middle school | 1974 | 1553 | 57 | 49 | |||||||||
| College and above | 526 | 417 | 10 | 5 | |||||||||
| Total | 4735 | 3643 | 186 | 163 | |||||||||
| Income | <=2000 | 1830 | 242.02 | < 0.001 | 1293 | 152.98 | < 0.001 | 86 | 18.15 | < 0.001 | 79 | 21.88 | < 0.001 |
| 2000–5000 | 1144 | 801 | 32 | 27 | |||||||||
| > 5000 | 270 | 233 | 7 | 4 | |||||||||
| Total | 3244 | 2327 | 125 | 110 | |||||||||
D diopter, PNVI present near vision impairment, presbyopia uncorrected near visual acuity worse than N6 or N8 at 40 cm and best corrected visual acuity ≥20/40, DVI distance vision impairment, Combined VI combined vision impairment
Discussion
The FJES enrolled 8211 participants from May 2018 to October 2019. The participant baseline characteristics and ocular characteristics were reported. Compared with several cross sectional study before [1–16], our study presented a relatively complete picture of the status quo of vision and ocular diseases and the interrelationship between human, geographical and other physical elements, especially chronic diseases and personal information.
As the study reported, the percentage of blindness and VI in our study was 0.21 and 3.33%, respectively, which was lower than the global data from a Lancet review. The review showed the percentage of blindness and VI was approximately 0.49 and 3.69%, respectively, until 2015 [25]. Besides, the difference was not statistically significant between urban and rural areas in the DVI rate, which was not consistent with some studies, such as the Ireland study [26] and Brazilian Amazon Region Eye Survey [7]. It is necessary to explore the reasons and correlations of these results. To explore the causes in more detail, we included many different groups to collect evidence, such as age, sex, refraction, BMI, SBP, educational background, income, residency, urbanization, history of chronic diseases, tobacco consumption, alcohol consumption, and tea consumption.
In this study, VI was significantly correlated with biological and sociodemographic factors, including age, urban and rural regions, coastal and inland areas, educational background, income and refractive error. Sex was not statistically significantly associated with VI after taking into account the interdependency of the parameters.
Encouragingly, many innovative results were found, such as the difference in VI between coastal and inland regions, a higher DVI rate in the inland population, a higher combined VI rate in both rural and inland populations, and NVA improvement in the tea-drinking population. Dramatic changes have taken place in residents’ lifestyle with the coronavirus disease-19 (COVID-19) outbreak. In particular, near vision at all ages has been affected significantly due to the penetration of electronic products when people reduce outdoor social activities. As a result, future epidemiological research may involve changes to models or performance. Our study only examined eye health status before the epidemic and provides a pre-epidemic sample for future research. The project is the first domestic epidemiological study for eye diseases covering coastal and inland areas in both urban and rural regions and provides evidence for the establishment of policy making and control strategy for eye diseases. The FJES can facilitate collaborations in clinical practice for ophthalmologists and cardiologists or endocrinologists.
There are also some interesting findings. For example, compared with the inland population, the coastal population had less myopia and better vision function overall. Potential differences in economic level, education level, transportation, environmental and lifestyle factors, such as the coastal diet preference for seafood and higher UV levels [27, 28] in coastal areas, may be important factors in the development of vision changes. Another interesting finding was that drinking tea may improve near vision but not distance vision. This discovery may indicate a new direction for basic research. What ingredients in tea may affect vision? The correlations of these factors will be elaborated in the following articles in detail.
The FJES has several strengths and some differential features with regard to other information resources. First, a key strength of the FJES database is the detailed questionnaire information and overall ocular and physical examinations collected in more than 50 towns of all nine cities in an entire province of southern China. Second, many cross-sectional studies have provided a description of VA, but most studies have reported NVA and DVA separately. This study integrated both NVA and DVA and explored the influence of geographic factors, including urban and rural and coastal and inland areas, which have not previously been covered. Third, most comparisons in previous studies were based on various baselines among different studies, whereas the data analysis and comparison in this study used a single baseline, making the correlation more convincing. Fourth, we used advanced measurement instruments, such as multicolour OCT and nonmydriatic colour fundus photography. Furthermore, we designed various subgroups to provide more original information, which can update and complement worldwide epidemiological surveys in ophthalmology.
There are some limitations of this study. First, there may be information biases due to absent registration (data completeness). Second, the examination was not perfect. Because of time limitations, we only performed DVA correction (namely, BCVA), and we did not perform NVA correction. Unfortunately, we also did not perform ocular biometry, which can obtain structural parameters such as the refractive power of the cornea, the depth of the anterior chamber, the axial length of the eyeball and the thickness of the lens. Third, data quality may be a strength in some databases but also a weakness for certain data, such as the incompleteness of NVA and DVA data, which could slightly affect the integrity and accuracy of the final diagnosis results.
Conclusions
The FJES is a population-based cross-sectional on-site survey on the public eye health status of Chinese residents in Fujian province. The rich data collected from the study provide the opportunity to identify risk factors and associations of VI and eye diseases with chronic diseases and basic personal information. This project will be meaningful for guidance in eye health-related policy-making.
Acknowledgments
We thank the FJES Group members (Zhenglingling Yao, Liting Wang, Yi Liu, Wufu Qiu, Menging Lin, Yanhong Zhang, etc) who made tremendous efforts to make the study successful, especially in the field examinations and data collection.
Abbreviations
- WHO
World Health Organization
- VI
Vision impairment
- NSFC
National Natural Science Foundation of China
- FJES
Fujian Eye Study
- BMI
Body mass index
- HR
Heart rate
- SBP
Systolic blood pressure
- DBP
Diastolic blood pressure
- PNVA
Presenting near visual acuity
- PDVA
Presenting distance visual acuity
- BCVA
Best corrected visual acuity
- IOP
Intraocular pressure
- OCT
Optical coherence tomography
- DVI
Distance vision impairment
- PNVI
Present near vision impairment
- LOCS III
Lens Opacities Classification System III
- NC
Nuclear color
- NO
Nuclear opalescence
- C
Cortical cataract
- P
Posterior subcapsular
- RNFL
Retinal nerve fibre layer
- ONH-RC
Optic nerve head radial and circle
- SD
Standard deviation
- ANOVA
Analysis of variance
- χ2
Chi-square
- OR
Odds ratio
- CI
Confidence internal
- UV
Ultraviolet
- COVID
Coronavirus disease
- VA
Visual acuity
- NVA
Near visual acuity
- DVA
Distance visual acuity
Authors’ contributions
Yang Li and Qinrui Hu took part in all parts of the study, including the study design, data collection, data analysis, the vision impairment survey data preparation, writing and revision. Xueying Qin and Tao Ren reviewed the data, including data examination, data coding, data packet, data summaries and production forms. Bin Wang assisted in plotting and article revision. All authors contributed to the study design, analysis, and writing of the report. Yonghua Hu and Xiaoxin Li oversaw the research, data and article. The author(s) read and approved the final manuscript.
Authors’ information
Yang Li, PhD, graduated from Health Science Center, Peking University, Beijing, China in 2017. Now she is working in the School of Public Health of Peking University and Xiamen Eye Center Affiliated with Xiamen University to train her postdoctoral personnel.
Xiaoxin Li, MD, PhD, academician of International Academy of Ophthalmology, president of the Asia Pacific Vitreoretinal Society, president of Xiamen Eye Center Affiliated with Xiamen University, member of the International League of American ophthalmic Societies, and consultant of International Council of ophthalmic Societies (ICO). She had undertaken the national “10th Five Year Plan”, “11th Five Year Plan”, national “973”, “863”, Peking University “985”, “211” and WHO prevention and treatment of children’s blindness, and she was the chief scientist of senile macular disease in the national key basic research and development program (973 Program) and the director of Ophthalmology program of “985” phase III. She had published more than 270 papers as the first author or corresponding author, including more than 70 SCI papers. And she chief edited or translated 11 monographs so far.
Funding
This study was supported by the National Natural Science Foundation of China (no.81870672 and 81900881) from the National Natural Science Foundation Committee. The funder had no role in the study design, collection, analysis and interpretation of data.
Availability of data and materials
All data generated or analyzed during this study are included in supplementary information files of this published article.
Declarations
Ethics approval and consent to participate
Approval was obtained from the Ethics Committee of Xiamen Eye Center affiliated with Xiamen University (Acceptance number: XMYKZX-KY-2018-001) and written informed consent was obtained from all study participants. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yang Li and Qinrui Hu contributed equally to this work.
Contributor Information
Xiaoxin Li, Email: drlixiaoxin@163.com.
Yonghua Hu, Email: yhhu@bjmu.edu.cn.
References
- 1.Yonekawa Y, Varma R, Choudhury F, Torres M, Azen SP. Los Angeles Latino eye study group. Risk factors for four-year incident visual impairment and blindness: the Los Angeles Latino eye study. Ophthalmology. 2011;118(9):1790–1797. doi: 10.1016/j.ophtha.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodriguez J, Sanchez R, Munoz B, et al. Causes of blindness and visual impairment in a population-based sample of U.S. Hispanics. Ophthalmology. 2002;109(4):737–743. doi: 10.1016/S0161-6420(01)01008-9. [DOI] [PubMed] [Google Scholar]
- 3.Klein R, Lee KE, Gangnon RE, Klein BE. Incidence of visual impairment over a 20-year period: the beaver dam eye study. Ophthalmology. 2013;120(6):1210–1219. doi: 10.1016/j.ophtha.2012.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hong T, Mitchell P, Rochtchina E, Fong CS, Chia EM, Wang JJ. Long-term changes in visual acuity in an older population over a 15-year period: the Blue Mountains eye study. Ophthalmology. 2013;120(10):2091–2099. doi: 10.1016/j.ophtha.2013.03.032. [DOI] [PubMed] [Google Scholar]
- 5.Wolfram C, Schuster AK, Elflein HM, et al. The prevalence of visual impairment in the adult population. Dtsch Arztebl Int. 2019;116(17):289–295. doi: 10.3238/arztebl.2019.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Delcourt C, Le Goff M, von Hanno T, et al. The decreasing prevalence of nonrefractive visual impairment in older Europeans: a Meta-analysis of published and unpublished data. Ophthalmology. 2018;125(8):1149–1159. doi: 10.1016/j.ophtha.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Salomão SR, Berezovsky A, Furtado JM, et al. Vision status in older adults: the Brazilian Amazon region eye survey. Sci Rep. 2018;8(1):886. doi: 10.1038/s41598-018-19338-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Katibeh M, Pakravan M, Yaseri M, Pakbin M, Soleimanizad R. Prevalence and causes of visual impairment and blindness in Central Iran; the Yazd eye study. J Ophthalmic Vis Res. 2015;10(3):279–285. doi: 10.4103/2008-322X.170362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong TY, Tham YC, Sabanayagam C, Cheng CY. Patterns and risk factor profiles of visual loss in a multiethnic Asian population: the Singapore epidemiology of eye diseases study. Am J Ophthalmol. 2019;206:48–73. doi: 10.1016/j.ajo.2019.05.006. [DOI] [PubMed] [Google Scholar]
- 10.Majithia S, Tham YC, Chee ML, Teo CL, Chee ML, Dai W, Kumari N, Lamoureux EL, Sabanayagam C, Wong TY, Cheng CY. Singapore Chinese eye study: key findings from baseline examination and the rationale, methodology of the 6-year follow-up series. Br J Ophthalmol. 2020;104(5):610–615. doi: 10.1136/bjophthalmol-2019-314760. [DOI] [PubMed] [Google Scholar]
- 11.Suzuki Y, Yamamoto T, Araie M, Iwase A, Tomidokoro A, Abe H, Shirato S, Kuwayama Y, Mishima HK, Shimizu H, Tomita G, Inoue Y, Kitazawa Y. Tajimi Study review. Nippon Ganka Gakkai Zasshi. 2008;112(12):1039–1058. [PubMed] [Google Scholar]
- 12.Liang YB, Friedman DS, Wong TY, Wang FH, Duan XR, Yang XH, Zhou Q, Tao Q, Zhan SY, Sun LP, Wang NL. Handan eye study group. Rationale, design, methodology, and baseline data of a population-based study in rural China: the Handan eye study. Ophthalmic Epidemiol. 2009;16(2):115–127. doi: 10.1080/09286580902738159. [DOI] [PubMed] [Google Scholar]
- 13.Jonas JB, Xu L, Wang YX. The Beijing eye study. Acta Ophthalmol. 2009;87(3):247–261. doi: 10.1111/j.1755-3768.2008.01385.x. [DOI] [PubMed] [Google Scholar]
- 14.Wang L, Zhu Z, Scheetz J, He M. Visual impairment and ten-year mortality: the Liwan eye study. Eye (Lond). 2021;35(8):2173–9. [DOI] [PMC free article] [PubMed]
- 15.Zou H, Zhang X, Xu X, Wang W, Li G, Yu H. An epidemiological survey of low vision and blindness of senile persons in Beixinjing blocks, Shanghai. Zhonghua Yan Ke Za Zhi. 2002;38(12):744–746. [PubMed] [Google Scholar]
- 16.Zhao J, Xu X, Ellwein LB, et al. Prevalence of vision impairment in older adults in rural China in 2014 and comparisons with the 2006 China Nine-Province survey. Am J Ophthalmol. 2018;185:81–93. doi: 10.1016/j.ajo.2017.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jonas JB, Cheung CMG, Panda-Jonas S. Updates on the epidemiology of age-related macular degeneration. Asia Pac J Ophthalmol (Phila) 2017;6(6):493–497. doi: 10.22608/APO.2017251. [DOI] [PubMed] [Google Scholar]
- 18.Song P, Wang H, Theodoratou E, Chan KY, Rudan I. The national and subnational prevalence of cataract and cataract blindness in China: a systematic review and meta-analysis. J Glob Health. 2018;8(1):010804. doi: 10.7189/jogh.08.010804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thapa R, Bajimaya S, Paudyal G, et al. Prevalence, pattern and risk factors of retinal vein occlusion in an elderly population in Nepal: the Bhaktapur retina study. BMC Ophthalmol. 2017;17(1):162. doi: 10.1186/s12886-017-0552-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li JQ, Welchowski T, Schmid M, et al. Prevalence, incidence and future projection of diabetic eye disease in Europe: a systematic review and meta-analysis. Eur J Epidemiol. 2020;35(1):11–23. doi: 10.1007/s10654-019-00560-z. [DOI] [PubMed] [Google Scholar]
- 21.National Bureau of Statistics People’s Republic of China. Major Figures of the 2010 population census. Available at: http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm. Accessed 03 Mar 2021.
- 22.Chylack LT, Jr, Wolfe JK, Singer DM, Leske MC, Bullimore MA, Bailey IL, Friend J, McCarthy D, Wu SY. The Lens opacities classification system III. The longitudinal study of cataract study group. Arch Ophthalmol. 1993;111(6):831–836. doi: 10.1001/archopht.1993.01090060119035. [DOI] [PubMed] [Google Scholar]
- 23.Lee SS, Lingham G, Yazar S, Sanfilippo PG, Charng J, Chen FK, Hewitt AW, Ng F, Hammond C, Straker LM, Eastwood PR, MacGregor S, Rose KA, Lucas RM, Guggenheim JA, Saw SM, Coroneo MT, He M, Mackey DA. Rationale and protocol for the 7- and 8-year longitudinal assessments of eye health in a cohort of young adults in the Raine study. BMJ Open. 2020;10(3):e033440. doi: 10.1136/bmjopen-2019-033440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.CPIRC. China Population. Annual report of Chinese resident’s income 2017 [in Chinese]. Available at: http://data.stats.gov.cn/easyquery.htm?cn=C01. Accessed 03 Mar 2021.
- 25.Bourne RR, ABourne R, et al. Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. The lancet. Glob Health. 2017;5(9):e888–e897. doi: 10.1016/S2214-109X(17)30293-0. [DOI] [PubMed] [Google Scholar]
- 26.Gallagher BA, Hart PM, O'Brien C, Stevenson MR, Jackson AJ. Mobility and access to transport issues as experienced by people with vision impairment living in urban and rural Ireland. Disabil Rehabil. 2011;33(12):979–988. doi: 10.3109/09638288.2010.516786. [DOI] [PubMed] [Google Scholar]
- 27.Williams KM, Bentham GC, Young IS, et al. Association between myopia, ultraviolet B radiation exposure, serum vitamin D concentrations, and genetic polymorphisms in vitamin D metabolic pathways in a multicountry European study. JAMA Ophthalmol. 2017;135(1):47–53. doi: 10.1001/jamaophthalmol.2016.4752. [DOI] [PubMed] [Google Scholar]
- 28.Bose B, Najwa AR, Shenoy PS. Oxidative damages to eye stem cells, in response to, bright and ultraviolet light, their associated mechanisms, and salvage pathways. Mol Biotechnol. 2019;61(2):145–152. doi: 10.1007/s12033-018-0136-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in supplementary information files of this published article.