Background
Food is a vital determinant of both health and disease [1]. National and international organizations alike recognize that food is directly related to morbidity and premature mortality [2]. In the United States, the rising prevalence of non-communicable, chronic diseases that drive morbidity and mortality, such as obesity, diabetes, and hypertension, is directly related to low dietary quality [3]. This relationship between food insecurity, defined as a “household-level economic and social condition of limited or uncertain access to adequate food [4],” and chronic disease is well characterized in patient populations with low socioeconomic status [5]. As a result, food insecurity is associated with diabetes, hypertension, hyperlipidemia, and obesity [6,7]. In addition to limited access to nutritious foods that promote health, individuals who experience food insecurity could be forced to adopt coping strategies, such as food/medication trade-offs, that further worsen chronic disease management and increase acute healthcare utilization [4,8,9].
The evidence base for the health impact of food security interventions is still developing. Recent studies in the United States and abroad highlight the promise of food security interventions for improving a wide range of outcomes, including food security and dietary quality [10,11], HIV care [12,13], diabetes [11,14] and blood pressure [15] control, and skilled nursing facility and hospital admission rates [16,17]. It is important to work in parallel with ongoing research efforts to develop practical models for addressing both food insecurity and chronic disease.
The COVID-19 pandemic has exacerbated the devastating impact of food insecurity [18,19]. In Massachusetts, food banks and food pantries reported record levels of demand during the peak of the pandemic. In response to this, the charitable food system is distributing more food than ever before. In eastern Massachusetts, The Greater Boston Food Bank (GBFB) has distributed an unprecedented quantity of food and has also engaged in innovative collaborations with healthcare systems [20,21].
Given that food insecurity may affect chronic disease risk and progression, the COVID-19 pandemic could be negatively impacting the health of populations with low socioeconomic status. As a result, rates of diet-related chronic diseases, such as diabetes and pediatric obesity, might be worsening [22,23]. Such deterioration of health could result from reductions in both access to and the ability to afford healthy foods. This risk occurs in a context of other ongoing threats to health due to the pandemic, such as loss of health insurance tied to employment and limited transportation.
Worsening levels of food insecurity and diet-related chronic disease necessitate interventions that empower patients and communities to access healthy foods. One promising approach focuses on increasing consumption of plant-based foods [24]. Plant-based diets consist of either a majority of plant-based foods (e.g., the Mediterranean and Dietary Approaches to Stop Hypertension [DASH] diets) or exclusive plant composition (i.e., vegan). High intake of plant-based foods has been shown to be beneficial for prevention and treatment of many conditions, including cardiovascular disease [25–30], hypertension [31,32], and diabetes [33–35]. Major health organizations including the American Heart Association [36] and the American Diabetes Association recommend plant-based diets as one of several healthy dietary patterns [37]. Beyond the broad recommendations for plant-based diets, patients with food insecurity have demonstrated broad acceptance of plant-based food security interventions [38].
This study aimed to address the high prevalence of food insecurity and chronic disease by starting a plant-based food pantry at an academic medical center community clinic.
Organizational Context: A partnership between Massachusetts General Hospital Revere Healthcare Center and The Greater Boston Food Bank
This project took place over a 10-month period from January 2020 to October 2020. It was located at the Massachusetts General Hospital (MGH) Revere Healthcare Center, which is a community-based academic medical center clinic located in Revere, Massachusetts. Revere is a city located approximately five miles north of Boston and is comprised of a racially, ethnically, and socioeconomically diverse community with a large immigrant population. Patients at the MGH Revere Healthcare Center had high rates of food insecurity (13%) before the onset of the COVID-19 pandemic [39].
GBFB is the largest food bank in New England. In Fiscal Year 2020, it distributed 99 million pounds of food to approximately 600 partner agencies, the majority of which are food pantries that distribute food to people in need [40,41]. GBFB is a member organization of Feeding America, a network of over 200 food banks throughout the country [42]. To support the health of food insecure populations, GBFB incorporates a color-coded stoplight nutrition ranking system: Supporting Wellness at Pantries (SWAP) [43]. SWAP colors help food banks and food pantries make informed decisions about the nutritional quality of their food purchases based on saturated fat, sugar, and sodium contents [44].
This project was undertaken as a Quality Improvement Initiative at MGH, and as such did not undergo Institutional Review Board review per the hospital’s policies.
Personal Content
The development of the MGH Revere Food Pantry stemmed from food security intervention work conducted at MGH by Dr. Seth A. Berkowitz, including research studies with patients from the MGH Revere Healthcare Center [11,45]. Dr. Jacob B. Mirsky is a primary care physician at MGH Revere Healthcare Center and has a longstanding interest in healthy lifestyle change and structural approaches to addressing food insecurity and health inequities. Dr. Lauren Fiechtner is a pediatrician at MGH and also serves as the Senior Health and Research Advisor at GBFB, where she partners with epidemiologist and Senior Data Analyst Dr. Rachel M. Zack to increase understanding of food insecurity, its impact on health, and the benefits of food security interventions.
Problem: How can healthcare systems address food insecurity and chronic disease at the same time?
Healthcare systems are responsible for improving patient health and reducing the burden of chronic disease. Given the prominent role that food insecurity plays as a risk factor for developing and exacerbating chronic disease, healthcare systems are well positioned to implement innovative food security interventions [46]. Moreover, academic medical centers can leverage research infrastructure to answer the important questions necessary to develop food security interventions that are effective and sustainable.
Plant-based food interventions can address both food insecurity and chronic disease care [24]. In addition to improving food access, and thus reducing food insecurity, distributing plant-based food directly to patients offers a novel strategy for improving chronic disease management. Food security research studies often focus on interventions to treat specific conditions such as diabetes [10]. Such an approach can overlook broader health needs, and the role of food in prevention of chronic illness. We recognized an important gap that could be filled by offering plant-based foods to those in need, without focusing on a specific condition.
Solution and Initial Evaluation
We used a team approach to create a plant-based food pantry focused on improving food access and chronic disease prevention and management. Our initial team included a program manager to guide operations, an administrator for regulatory compliance and budgetary planning, a dietitian for onsite education, and a medical director (J.B.M.) to develop the programming. At MGH, our Accountable Care Organization (ACO) colleagues help improve care for patients covered by Medicaid through programming targeted at health-related social needs including food insecurity. For example, all MGH patients with Medicaid ACO insurance are screened yearly for food insecurity with the well-validated and widely adopted two-question hunger vital sign [47,48]. Because this screening takes place as part of routine care, this institutional partnership allowed us to easily identify patients who might benefit from food security interventions. In addition, the team’s medical director secured protected administrative time to organize the team, identify a strategy to start the food pantry, and unite key stakeholders to create a sustainability plan.
The initial steps to build the MGH Revere Food Pantry focused on learning about best practices and existing models for hospital-based food pantry programming. The team toured and learned from our colleagues at the MGH Chelsea Healthcare Center, which had a successful existing food pantry. The team also explored the Boston Medical Center food access program that consists of a food pantry, teaching kitchen, and rooftop farm [46].
The pilot program started in January 2020. The team initially envisioned a 12-week program with weekly food pick-up. The team generated a list of eligible patients using our electronic health record. Pilot patients all screened positive for food insecurity and had a diagnosis of at least one of the following chronic nutrition-dependent diseases: obesity, hypertension, or diabetes. All patients were English-speaking to support early development of in-person nutrition education with the dietitian and to facilitate direct feedback to our program manager regarding operational challenges and successes. The program manager called patients to gauge interest in participation.
The team aspired to meet a high percentage of household food needs [10] and estimated that 1.2 pounds of food was roughly the equivalent of one meal [49]. Patients generally received 15–25 pounds of food per household member per week, depending on the availability and density of procured foods, which was projected to provide food for each household member to eat up to three meals per day for seven days. Food was purchased at local stores from January to March 2020 while a formal arrangement with GBFB was finalized. At the first visit, each participant was given cooking oil, spices, recipes, and cooking equipment (e.g., pot, pan, vegetable steamer) if necessary. At all visits, patients received pre-packaged bags with plant-based foods, recipes, and in-person nutrition education by the pantry’s dietitian in an informal setting (i.e., without appointments, documentation, or billing).
Patients enrolled in the pilot between January 2020 and early March 2020, when the COVID-19 pandemic brought the pilot program to a halt. To match available resources, we targeted serving up to 12 participants on any given week. A total of 18 patients, out of 41 contacted (44%), came at least once during the pilot. Some initial barriers to participation, ascertained during informal discussions with the food pantry staff, included a lack of transportation and conflicting schedules (e.g., work or child care) during business hours.
In response to heightened needs brought on by the pandemic, the team strategized alternative approaches to meeting our core mission of promoting healthy eating through a plant-based diet. Given the very high rates of COVID-19 in the Revere community, a “COVID-19 hotspot” in Massachusetts, the team decided to suspend pilot programming and expand operations to provide food for all patients from the MGH Revere Healthcare Center seeking food assistance. Patients were served regardless of their insurance coverage, documentation of food insecurity or chronic disease, or language spoken. The team modified its food pick-up system to ensure social distancing through curbside operations. The food pantry expanded its hours of operation from four hours on one day per week to a total of 16 hours on two days per week. These expanded operations were made possible by a temporary reallocation of resources as well as an increase in the pantry’s physical space as a result of the cessation of some in-person programming at the MGH Revere Healthcare Center because of the need for social distancing to reduce COVID-19 infection risk. To support homebound patients and patients with transportation barriers, the team secured a grant that funded home deliveries of food pantry bags, which began in September 2020. In-person nutrition education was paused to reduce the risk of COVID-19 transmission.
To meet the growing needs during the pandemic, the team also focused on broadening food supply sources. The team prioritized providing predominantly shelf-stable plant-based foods (e.g., canned beans and bagged rice), in large part due to philanthropy-supported purchasing at box stores. For fresh produce, the MGH Medicaid ACO office partnered with a local non-profit during the COVID-19 pandemic that provided additional fresh produce beyond what was received from GBFB. The team also created a partnership with a local gleaning organization, which collected unharvested produce from local farms and delivered it to food pantries for distribution.
The MGH Revere Food Pantry created a workflow, which was modified after the COVID-19 pandemic started, that enabled weekly food distribution. This workflow allowed for weekly pick-up and distribution of foods from GBFB (Figure 1) and included weekly ordering of food through “SHOP GBFB,” an online food ordering system that allowed for a scheduled food pick up timeslot. The SHOP GBFB system incorporated SWAP scores (i.e., a green, yellow, and red nutritional ranking system based on sugar, saturated fat, and sodium content) directly into the ordering process (Figure 2). Of note, the bags of food that patients received from the food pantry also included fresh produce from alternative sources, as mentioned above. As an example of how the MGH Revere Food Pantry supported patients during the study period, a representative offering for a family of four in September 2020 (inclusive of foods from GBFB and the gleaning organization) contained four cans of fruit, two cans of vegetables, three cans of beans, two cans of tomatoes, one can of soup, one jar of peanut butter, two boxes of cereal or oats, two boxes of pasta, one bag of rice, and six bottles of applesauce. Soon after the study period, nutrition education resumed virtually with the piloting of weekly YouTube videos demonstrating how to prepare recipes with foods distributed that week [50].
Figure 1.
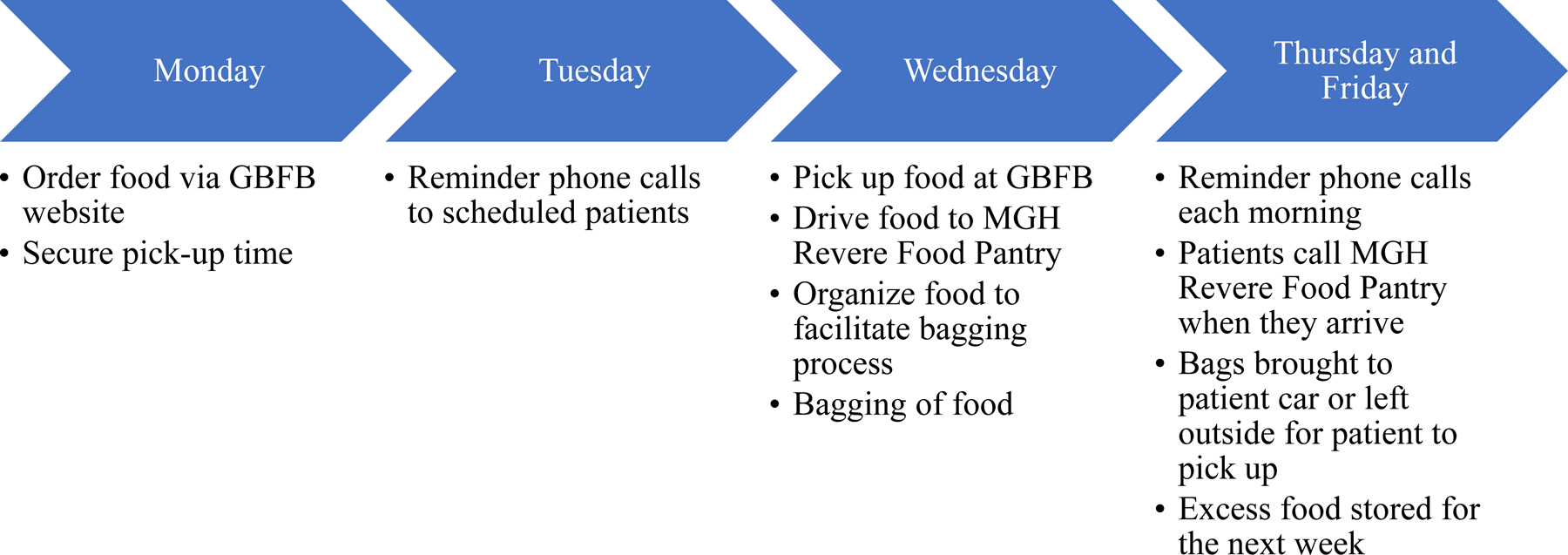
MGH Revere Food Pantry Weekly Workflow. Abbreviations: GBFB = Greater Boston Food Bank.
Figure 2.
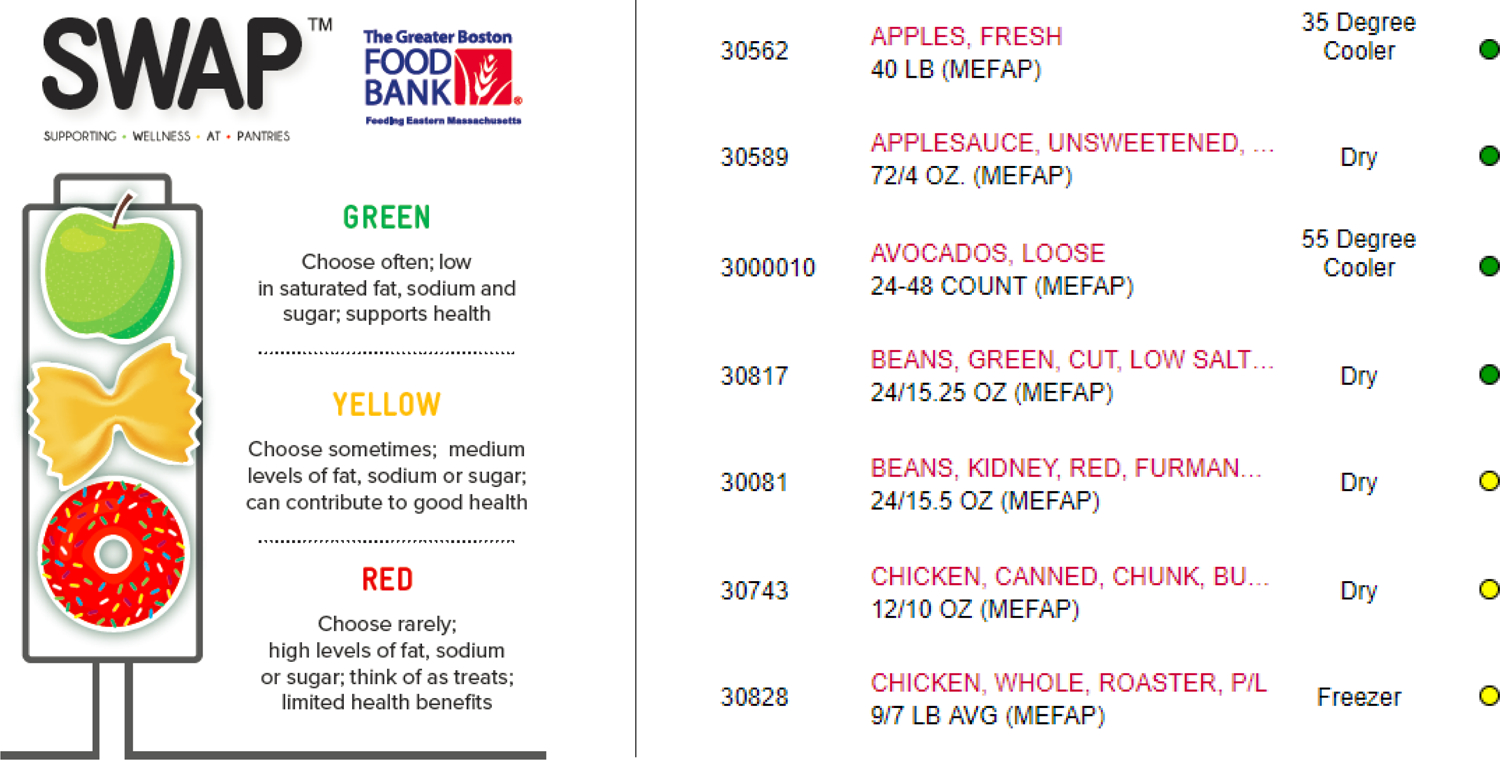
Example of Greater Boston Food Bank’s Online SWAP Ordering System for Food Pantries. Abbreviations: SWAP = Supporting Wellness at Pantries.
After the COVID-19 pandemic began significantly impacting the Revere community in March 2020, the number of recipients approximately tripled in just one month (Figure 3). The staff was able to package enough bags for a maximum of 80 patients (and their household members) per week. In the last six months of the study period, the MGH Revere Food Pantry distributed food to 384 people (i.e., patients and their household members) per month. By October 2020, there was a steady waitlist of approximately 10–20 patients at any given time, highlighting the rising needs of patients in the community due to the COVID-19 pandemic. Attrition rates allowed for 5–10 patients on the waitlist to be added to the roster of patients receiving food each week, so patients on the wait list generally received food within a few weeks of referral. Moreover, once receiving food, patients were able to continue to receive weekly food indefinitely. The staff observed a high level of retention month-over-month, although exact rates were not tracked during the study period.
Figure 3.
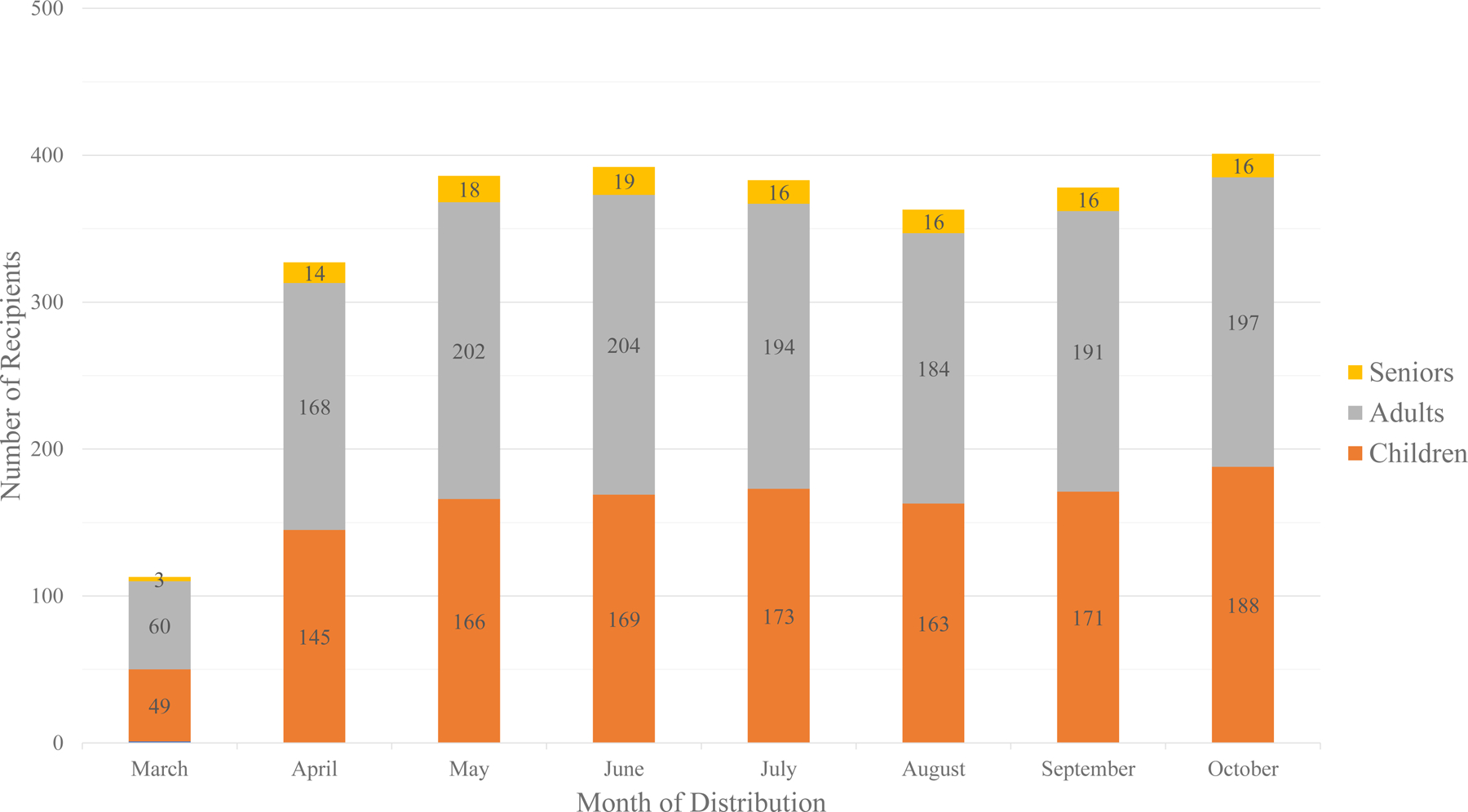
Recipients of Greater Boston Food Bank Food Distributed by the MGH Revere Food Pantry, March through October 2020.
Fresh produce was the largest category of distributed food from GBFB (47%; Figure 4). By the end of October 2020, a total of 96,247 pounds of food from GBFB was distributed to recipients. Food from other sources during this time totaled 21,495 pounds. In sum, the MGH Revere Food Pantry distributed 117,742 pounds of food during the study period.
Figure 4.
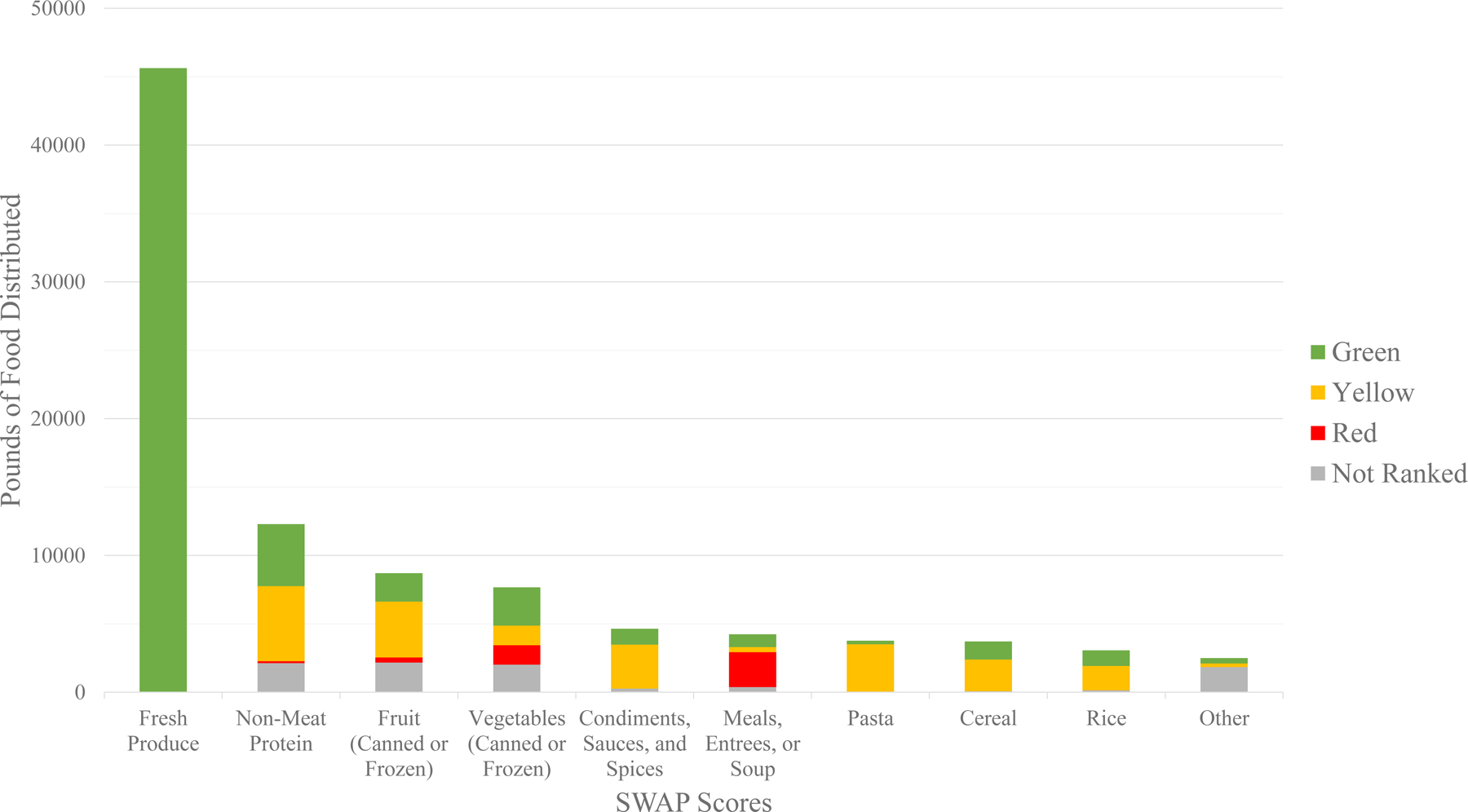
Pounds and SWAP Scores of Greater Boston Food Bank Food Distributed by the MGH Revere Food Pantry, March through October 2020. SWAP = Supporting Wellness at Pantries.
Unresolved Questions
The MGH Revere Food Pantry team recognized several unanswered questions and limitations to the generalizability of our experience to others hoping to build academic medical center food pantries with a mission of serving plant-based foods. First, in the absence of health outcome assessments, it was not yet clear if the provision of plant-based foods improved the health of study participants. It is possible that participants did not receive enough healthy foods to offset the impact of unhealthy foods eaten from other sources, such as restaurants and bodegas. Moreover, improvements in health might require a longer timeframe or more robust clinical programming (e.g., a teaching kitchen with nutritionist-driven education or group medical visits) for salutary effects to take place. Future research is necessary to directly measure previously established positive outcomes, including changes in food insecurity [10,11], diet quality (e.g., fruit and vegetable intake [10] or Healthy Eating Index 2010 [11] scores), chronic disease outcomes (e.g., reductions in hemoglobin A1C [14] and blood pressure [15]), and healthcare utilization (e.g., skilled nursing facility and hospital admission rates [16,17]). It will be particularly important to focus on those conditions most impacted by the COVID-19 pandemic. Second, although the consistent attendance by many patients suggested a high degree of acceptability of plant-based foods, we did not formally assess patient preferences or the utilization of provided food at home. Qualitative studies replicating the acceptability of plant-based foods [38] in our diverse patient population will help improve our ability to meet patient needs in the future. Finally, although both food pantry staff [43] and patients with food insecurity [51] have previously demonstrated satisfaction using SWAP scores, more formal assessment of its benefits and limitations need to be clarified to facilitate workflow improvements at the MGH Revere Food Pantry.
We also recognized the importance of funding to support the mission of an academic medical center-based food pantry. The food pantry was temporarily supported by an operating budget resulting from a shift in resources due to changes in clinic activities in response to the COVID-19 pandemic. However, the food pantry team is currently planning to expand into a larger space, with a teaching kitchen, to support greater volume and resumption of clinical programming when it is safe to do so. This will be achieved, in part, through philanthropic support. The food pantry team is actively fundraising for this expansion. The food panty team also aspires to unite diverse stakeholders to further sustain the food pantry mission, which could include community members, insurance companies with risk-based contracts, and government agencies addressing social needs. The future growth of the pantry, as well as the genesis of others at MGH and beyond, will depend on sustainable funding to support oversight, expansion, and clinical programming.
Lessons for the Field
The MGH Revere Food Pantry team rapidly learned several lessons from the pilot as well as the increased needs and challenges brought on by the COVID-19 pandemic. Primarily, we found that a clinic-community food pantry partnership could provide patients with plant-based foods. Although we served many more patients than initially anticipated, our workflow was effectively and efficiently modified during the crisis. Second, we experienced the power of partnerships with local food banks that can provide food in addition to logistical knowledge and capabilities. Moreover, GBFB utilizes a SWAP system that helps food pantries like ours to easily make healthy decisions about food procurement choices. Third, with space and food agreements in place, we learned that food pantries require motivated and attentive staff to engage with patients and ensure efficient operations on a short (i.e., weekly) time cycle. Additionally, a focus on plant-based foods, such as shelf-stable canned beans or bags of whole grain rice, reduces the need for freezer and refrigerator costs and space. Some produce can be stored for brief periods of time without refrigeration, however more temperature-sensitive items, such as fresh berries and leafy greens, require adequate refrigeration. Finally, the team clarified the need for data capture, research and evaluation, fundraising, and further team building to support growth. Future efforts to replicate the MGH Revere Food Pantry model will similarly depend on the ability to create a small and successful initial workflow while also putting in place the evaluation and funding processes necessary for sustainability.
In conclusion, programs addressing health-related social needs within the healthcare system will be essential to effectively care for patient populations with low socioeconomic status. We envision plant-based food pantries improving food insecurity as well as health. Our experience at the MGH Revere Food Pantry can be used as a model for other organizations interested in the intersection of food insecurity and chronic disease.
References
- 1.World Health Organization. Chronic Disease Report. https://www.who.int/chp/chronic_disease_report/. Accessed November 13, 2020.
- 2.GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019. May 11;393(10184):1958–1972. doi: 10.1016/S0140-6736(19)30041-8. Epub 2019 Apr 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Friedman School of Nutrition Science and Policy at Tufts University. Food is Medicine: Key Facts. https://nutrition.tufts.edu/sites/default/files/documents/FIM%20Infographic-Web.pdf. Accessed November 16, 2020.
- 4.United States Department of Agriculture Economic Research Service. Definitions of Food Insecurity. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/definitions-of-food-security.aspx#:~:text=Food%20insecurity%E2%80%94the%20condition%20assessed,may%20result%20from%20food%20insecurity. Accessed November 13, 2020.
- 5.Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med. 2010. Jul 1;363(1):6–9. doi: 10.1056/NEJMp1000072. [DOI] [PubMed] [Google Scholar]
- 6.Nagata JM, Palar K, Gooding HC, Garber AK, Bibbins-Domingo K, Weiser SD. Food Insecurity and Chronic Disease in US Young Adults: Findings from the National Longitudinal Study of Adolescent to Adult Health. J Gen Intern Med. 2019. Dec;34(12):2756–2762. doi: 10.1007/s11606-019-05317-8. Epub 2019 Oct 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010. Feb;140(2):304–10. doi: 10.3945/jn.109.112573. Epub 2009 Dec 23. Erratum in: J Nutr. 2011 Mar;141(3):542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Feeding America. Understand Food Insecurity. https://hungerandhealth.feedingamerica.org/understand-food-insecurity/hunger-health-101/. Accessed November 13, 2020.
- 9.Berkowitz SA, Seligman HK, Meigs JB, Basu S. Food insecurity, healthcare utilization, and high cost: a longitudinal cohort study. Am J Manag Care. 2018. Sep;24(9):399–404. [PMC free article] [PubMed] [Google Scholar]
- 10.Seligman HK, Smith M, Rosenmoss S, Marshall MB, Waxman E. Comprehensive Diabetes Self-Management Support From Food Banks: A Randomized Controlled Trial. Am J Public Health. 2018. Sep;108(9):1227–1234. doi: 10.2105/AJPH.2018.304528. Epub 2018 Jul 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berkowitz SA, Delahanty LM, Terranova J, Steiner B, Ruazol MP, Singh R, Shahid NN, Wexler DJ. Medically Tailored Meal Delivery for Diabetes Patients with Food Insecurity: a Randomized Cross-over Trial. J Gen Intern Med. 2019. Mar;34(3):396–404. doi: 10.1007/s11606-018-4716-z. Epub 2018 Nov 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ivers LC, Chang Y, Gregory Jerome J, Freedberg KA. Food assistance is associated with improved body mass index, food security and attendance at clinic in an HIV program in central Haiti: a prospective observational cohort study. AIDS Res Ther. 2010. Aug 26;7:33. doi: 10.1186/1742-6405-7-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weinhardt LS, Galvao LW, Yan AF, Stevens P, Mwenyekonde TN, Ngui E, Emer L, Grande KM, Mkandawire-Valhmu L, Watkins SC. Mixed-Method Quasi-Experimental Study of Outcomes of a Large-Scale Multilevel Economic and Food Security Intervention on HIV Vulnerability in Rural Malawi. AIDS Behav. 2017. Mar;21(3):712–723. doi: 10.1007/s10461-016-1455-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ferrer RL, Neira LM, De Leon Garcia GL, Cuellar K, Rodriguez J. Primary Care and Food Bank Collaboration to Address Food Insecurity: A Pilot Randomized Trial. Nutr Metab Insights. 2019. Jul 29;12:1178638819866434. doi: 10.1177/1178638819866434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Emmert-Aronson B, Grill KB, Trivedi Z, Markle EA, Chen S. Group Medical Visits 2.0: The Open Source Wellness Behavioral Pharmacy Model. J Altern Complement Med. 2019. Oct;25(10):1026–1034. doi: 10.1089/acm.2019.0079. Epub 2019 Aug 28. [DOI] [PubMed] [Google Scholar]
- 16.Berkowitz SA, Terranova J, Randall L, Cranston K, Waters DB, Hsu J. Association Between Receipt of a Medically Tailored Meal Program and Health Care Use. JAMA Intern Med. 2019. Jun 1;179(6):786–793. doi: 10.1001/jamainternmed.2019.0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berkowitz SA, Terranova J, Hill C, Ajayi T, Linsky T, Tishler LW, DeWalt DA. Meal Delivery Programs Reduce The Use Of Costly Health Care In Dually Eligible Medicare And Medicaid Beneficiaries. Health Aff (Millwood). 2018. Apr;37(4):535–542. doi: 10.1377/hlthaff.2017.0999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gundersen C, Dewey A, Engelhard E, Strayer M, Lapinski L. Map the Meal Gap 2020: A Report on County and Congressional District Food Insecurity and County Food Cost in the United States in 2018. Feeding America; 2020. [Google Scholar]
- 19.Feeding America. The Impact of Coronavirus on Food Insecurity. https://www.feedingamerica.org/research/coronavirus-hunger-research. Accessed November 3, 2020.
- 20.The Greater Boston Food Bank. GBFB’s Response to COVID19. https://www.gbfb.org/2020/04/02/gbfbs-response-covid-19/. Accessed November 24, 2020.
- 21.Babbin M, Zack R, Granick J, & Betts K (2021). Food access initiatives: An integral piece of the Revere, Massachusetts, COVID-19 response. Journal of Agriculture, Food Systems, and Community Development, 10(2), 1–6. 10.5304/jafscd.2021.102.017 [DOI] [Google Scholar]
- 22.Tester JM, Rosas LG, Leung CW. Food Insecurity and Pediatric Obesity: a Double Whammy in the Era of COVID-19. Curr Obes Rep. 2020. Dec;9(4):442–450. doi: 10.1007/s13679-020-00413-x. Epub 2020 Oct 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ruiz-Roso MB, Knott-Torcal C, Matilla-Escalante DC, Garcimartín A, Sampedro-Nuñez MA, Dávalos A, Marazuela M. COVID-19 Lockdown and Changes of the Dietary Pattern and Physical Activity Habits in a Cohort of Patients with Type 2 Diabetes Mellitus. Nutrients. 2020. Aug 4;12(8):2327. doi: 10.3390/nu12082327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hemler EC, Hu FB. Plant-Based Diets for Personal, Population, and Planetary Health. Adv Nutr. 2019. Nov 1;10(Suppl_4):S275–S283. doi: 10.1093/advances/nmy117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Key TJ, Fraser GE, Thorogood M, Appleby PN, Beral V, Reeves G, Burr ML, Chang-Claude J, Frentzel-Beyme R, Kuzma JW, Mann J, McPherson K. Mortality in vegetarians and nonvegetarians: detailed findings from a collaborative analysis of 5 prospective studies. Am J Clin Nutr. 1999. Sep;70(3 Suppl):516S–524S. doi: 10.1093/ajcn/70.3.516s. [DOI] [PubMed] [Google Scholar]
- 26.Huang T, Yang B, Zheng J, Li G, Wahlqvist ML, Li D. Cardiovascular disease mortality and cancer incidence in vegetarians: a meta-analysis and systematic review. Ann Nutr Metab. 2012;60(4):233–40. doi: 10.1159/000337301. Epub 2012 Jun 1. [DOI] [PubMed] [Google Scholar]
- 27.Crowe FL, Appleby PN, Travis RC, Key TJ. Risk of hospitalization or death from ischemic heart disease among British vegetarians and nonvegetarians: results from the EPIC-Oxford cohort study. Am J Clin Nutr. 2013. Mar;97(3):597–603. doi: 10.3945/ajcn.112.044073. Epub 2013 Jan 30. [DOI] [PubMed] [Google Scholar]
- 28.Satija A, Bhupathiraju SN, Spiegelman D, Chiuve SE, Manson JE, Willett W, Rexrode KM, Rimm EB, Hu FB. Healthful and Unhealthful Plant-Based Diets and the Risk of Coronary Heart Disease in U.S. Adults. J Am Coll Cardiol. 2017. Jul 25;70(4):411–422. doi: 10.1016/j.jacc.2017.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, Merritt TA, Sparler S, Armstrong WT, Ports TA, Kirkeeide RL, Hogeboom C, Brand RJ. Intensive lifestyle changes for reversal of coronary heart disease. JAMA. 1998. Dec 16;280(23):2001–7. doi: 10.1001/jama.280.23.2001. Erratum in: JAMA 1999 Apr 21;281(15):1380. [DOI] [PubMed] [Google Scholar]
- 30.Li J, Lee DH, Hu J, Tabung FK, Li Y, Bhupathiraju SN, Rimm EB, Rexrode KM, Manson JE, Willett WC, Giovannucci EL, Hu FB. Dietary Inflammatory Potential and Risk of Cardiovascular Disease Among Men and Women in the U.S. J Am Coll Cardiol. 2020. Nov 10;76(19):2181–2193. doi: 10.1016/j.jacc.2020.09.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Joshi S, Ettinger L, Liebman SE. Plant-Based Diets and Hypertension. Am J Lifestyle Med. 2019. Sep 24;14(4):397–405. doi: 10.1177/1559827619875411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lopez PD, Cativo EH, Atlas SA, Rosendorff C. The Effect of Vegan Diets on Blood Pressure in Adults: A Meta-Analysis of Randomized Controlled Trials. Am J Med. 2019. Jul;132(7):875–883.e7. doi: 10.1016/j.amjmed.2019.01.044. Epub 2019 Mar 6. [DOI] [PubMed] [Google Scholar]
- 33.Qian F, Liu G, Hu FB, Bhupathiraju SN, Sun Q. Association Between Plant-Based Dietary Patterns and Risk of Type 2 Diabetes: A Systematic Review and Meta-analysis. JAMA Intern Med. 2019. Jul 22;179(10):1335–44. doi: 10.1001/jamainternmed.2019.2195. Epub ahead of print.; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barnard ND, Cohen J, Jenkins DJ, Turner-McGrievy G, Gloede L, Green A, Ferdowsian H. A low-fat vegan diet and a conventional diabetes diet in the treatment of type 2 diabetes: a randomized, controlled, 74-wk clinical trial. Am J Clin Nutr. 2009. May;89(5):1588S–1596S. doi: 10.3945/ajcn.2009.26736H. Epub 2009 Apr 1.; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Toumpanakis A, Turnbull T, Alba-Barba I. Effectiveness of plant-based diets in promoting well-being in the management of type 2 diabetes: a systematic review. BMJ Open Diabetes Res Care. 2018. Oct 30;6(1):e000534. doi: 10.1136/bmjdrc-2018-000534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.American Heart Association Nutrition Committee, Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, Franklin B, Kris-Etherton P, Harris WS, Howard B, Karanja N, Lefevre M, Rudel L, Sacks F, Van Horn L, Winston M, Wylie-Rosett J. Diet and lifestyle recommendations revision 2006: a scientific statement from the American Heart Association Nutrition Committee. Circulation. 2006. Jul 4;114(1):82–96. doi: 10.1161/CIRCULATIONAHA.106.176158. Epub 2006 Jun 19. Erratum in: Circulation. 2006 Dec 5;114(23):e629. Erratum in: Circulation. 2006 Jul 4;114(1):e27. [DOI] [PubMed] [Google Scholar]
- 37.Evert AB, Dennison M, Gardner CD, Garvey WT, Lau KHK, MacLeod J, Mitri J, Pereira RF, Rawlings K, Robinson S, Saslow L, Uelmen S, Urbanski PB, Yancy WS Jr. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. Diabetes Care. 2019. May;42(5):731–754. doi: 10.2337/dci19-0014. Epub 2019 Apr 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aiyer JN, Raber M, Bello RS, Brewster A, Caballero E, Chennisi C, Durand C, Galindez M, Oestman K, Saifuddin M, Tektiridis J, Young R, Sharma SV. A pilot food prescription program promotes produce intake and decreases food insecurity. Transl Behav Med. 2019. Oct 1;9(5):922–930. doi: 10.1093/tbm/ibz112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.North Suffolk Integrated Community Health Needs Assessment. 2019 North Suffolk Community Health Needs Assessment. https://www.northsuffolkassessment.org/2019-report-and-action-plans. Accessed November 24, 2020.
- 40.The Greater Boston Food Bank. Healthy Food in Eastern Massachusetts. https://www.gbfb.org/what-we-do/how-we-work/. Accessed May 31, 2021.
- 41.Zack RM, Weil R, Babbin M, Lynn CD, Velez DS, Travis L, Taitelbaum DJ, Fiechtner L. An Overburdened Charitable Food System: Making the Case for Increased Government Support During the COVID-19 Crisis. Am J Public Health. 2021. May;111(5):804–807. doi: 10.2105/AJPH.2021.306222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Feeding America. Our Work. https://www.feedingamerica.org/our-work/food-bank-network. Accessed May 31, 2021.
- 43.Martin KS, Wolff M, Callahan K, Schwartz MB. Supporting Wellness at Pantries: Development of a Nutrition Stoplight System for Food Banks and Food Pantries. J Acad Nutr Diet. 2019. Apr;119(4):553–559. doi: 10.1016/j.jand.2018.03.003. Epub 2018 May 1. [DOI] [PubMed] [Google Scholar]
- 44.Martin K, Xu R, Schwartz MB. Food pantries select healthier foods after nutrition information is available on their food bank’s ordering platform. Public Health Nutr. 2020. Nov 27:1–8. doi: 10.1017/S1368980020004814. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Berkowitz SA, Meigs JB, DeWalt D, Seligman HK, Barnard LS, Bright OJ, Schow M, Atlas SJ, Wexler DJ. Material need insecurities, control of diabetes mellitus, and use of health care resources: results of the Measuring Economic Insecurity in Diabetes study. JAMA Intern Med. 2015. Feb;175(2):257–65. doi: 10.1001/jamainternmed.2014.6888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Musicus AA, Vercammen KA, Fulay AP, Moran AJ, Burg T, Allen L, Maffeo D, Berger A, Rimm EB. Implementation of a Rooftop Farm Integrated With a Teaching Kitchen and Preventive Food Pantry in a Hospital Setting. Am J Public Health. 2019. Aug;109(8):1119–1121. doi: 10.2105/AJPH.2019.305116. Epub 2019 Jun 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hager ER, Quigg AM, Black MM, Coleman SM, Heeren T, Rose-Jacobs R, Cook JT, Ettinger de Cuba SA, Casey PH, Chilton M, Cutts DB, Meyers AF, Frank DA. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010. Jul;126(1):e26–32. doi: 10.1542/peds.2009-3146. [DOI] [PubMed] [Google Scholar]
- 48.Makelarski JA, Abramsohn E, Benjamin JH, Du S, Lindau ST. Diagnostic Accuracy of Two Food Insecurity Screeners Recommended for Use in Health Care Settings. Am J Public Health. 2017. Nov;107(11):1812–1817. doi: 10.2105/AJPH.2017.304033. Epub 2017 Sep 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.U.S. Department of Agriculture, Agricultural Research Service, Beltsville Human Nutrition Research Center, Food Surveys Research Group (Beltsville, MD) and U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics (Hyattsville, MD). What We Eat in America, NHANES 2011–2012. http://www.ars.usda.gov/News/docs.htm?docid=13793. Accessed June 29, 2021.
- 50.Massachusetts General Hospital. MGH Revere Food Pantry’s Golden Beet and Orange Salad Recipe. https://www.youtube.com/watch?v=QmOeaHdICGM. Accessed June 29, 2021.
- 51.Hampson J, MacNell L. Supporting wellness at pantries (SWAP) nutrition stoplight system aids rural food pantry clients living with chronic disease in selecting nutritious options. Chronic Illn. 2021. Jun 12:17423953211023976. doi: 10.1177/17423953211023976. Epub ahead of print. [DOI] [PubMed] [Google Scholar]


