Purpose of review
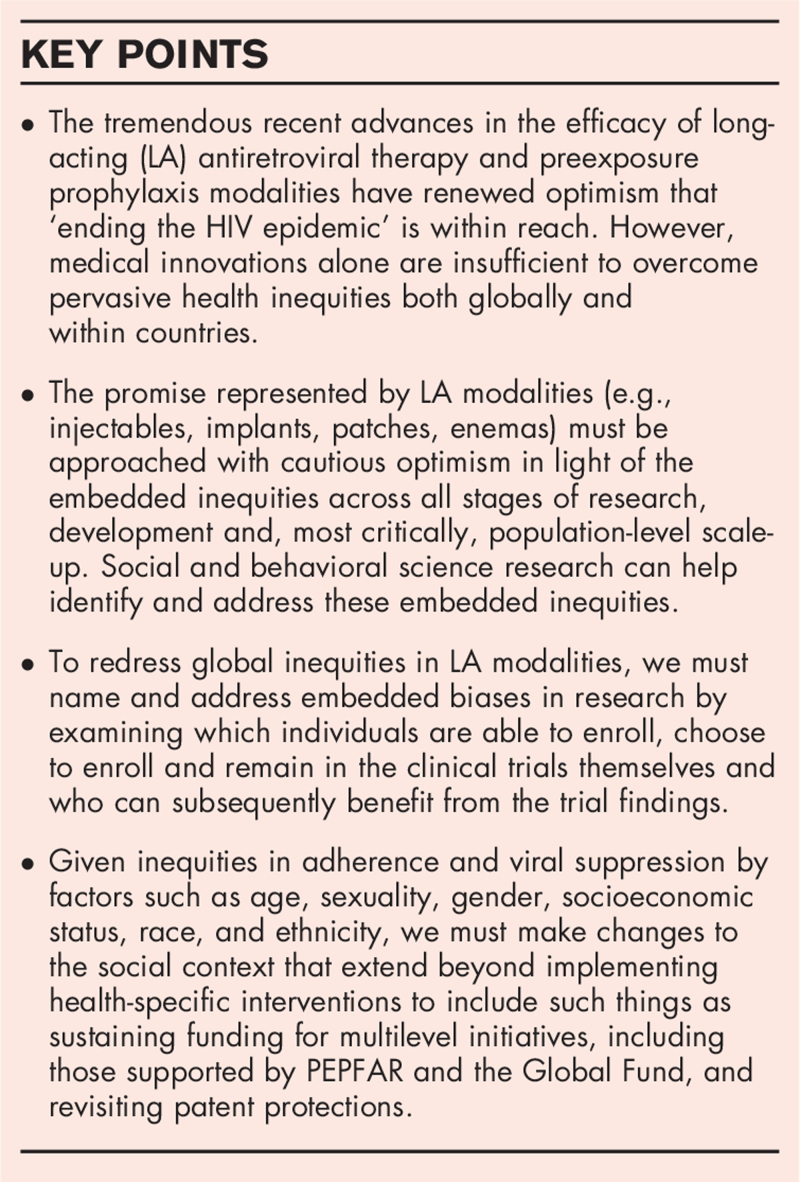
This paper provides a critical review of recent therapeutic advances in long-acting (LA) modalities for human immunodeficiency virus (HIV) treatment and prevention.
Recent findings
LA injectable antiretroviral therapy (ART) has been approved in the United States, Canada and Europe; the United States also has approved LA injectable preexposure prophylaxis (PrEP) and the World Health Organization has recommended the vaginal PrEP ring. Current LA PrEP modalities in clinical trials include injections, films, rings, and implants; LA ART modalities in trials include subcutaneous injections and long-term oral pills. Although LA modalities hold incredible promise, global availability is inhibited by long-standing multilevel perils including declining multilateral funding, patent protections and lack of political will. Once available, access and uptake are limited by factors such as insurance coverage, clinic access, labor markets, stigma, and structural racism and sexism. These must be addressed to facilitate equitable access for all.
Summary
There have been tremendous recent advances in the efficacy of LA ART and PrEP modalities, providing renewed hope that ‘ending the HIV epidemic’ is within reach. However, pervasive socio-structural inequities limit the promise of LA modalities, highlighting the need for cautious optimism in light of the embedded inequities in the trajectory of research, development, and population-level implementation.
Keywords: health equity, HIV prevention and care, long-acting antiretroviral therapy and preexposure prophylaxis, long-acting injectable, therapeutic innovation
INTRODUCTION
The advent of highly active antiretroviral therapy (ART) in 1996 transformed human immunodeficiency virus (HIV) infection into a manageable chronic condition for those in locales where it was available and accessible. Recent biomedical advances in long-acting (LA) modalities for ART and preexposure prophylaxis (PrEP) are once again expanding what is possible as we move toward ‘ending the HIV epidemic’ [1]. As of February 2022, LA injectable (LAI) ART with two month dosing [2] had been approved by the United States Food and Drug Administration (FDA) and Canadian and European regulators [3]. In 2021, the US FDA approved LAI PrEP and the World Health Organization (WHO) recommended the monthly vaginal ring for PrEP.
Box 1.
no caption available
Each new LA modality is an important tool in an ever-expanding toolkit and offers novel strategies to reduce barriers to daily pill taking [4,5]. Although LA modalities have the potential to change the course of the epidemic if provided as an option for all, they are not a panacea. The history of HIV and AIDS has underscored that framing biomedical treatment and prevention as sufficient for ‘ending the HIV epidemic’ flattens the deeply embedded social, cultural and political processes that drive the epidemic [6,7]. Historically, this has all too often resulted in incredible HIV technological advances that take a myopic individual-level approach and thus have limited population-level impacts; effective approaches to scaling up LA HIV modalities will require keen attention to socio-cultural dimensions [8].
LA modalities will not improve adherence without addressing long-standing multilevel perils that continue to constrain uptake of oral ART and PrEP, particularly among marginalized communities. For example, geopolitical determinants including fluctuations in funding for major HIV initiatives, such as the President's Emergency Plan for AIDS Relief (PEPFAR) and the Global Fund to Fight AIDS, Tuberculosis, and Malaria [9,10▪,11], patent protections [12–14] and lack of political will [15–17] can limit the in-country availability of approved HIV therapies. Clinical trials are sometimes the only avenue for communities in resource-limited settings to access emerging HIV treatment and prevention modalities, creating ethical questions about engagement in, vs. benefits from, research [18–21]. Even countries with approved LA modalities have striking inequities in access and uptake due to factors including: provider education, training and attitudes, insurance coverage and access, ability to attend clinic visits (e.g., transportation, labor market restrictions), medical mistrust and broader factors such as racism and sexual oppression [22,23▪,24,25].
This paper reviews the state of the science regarding LA ART and PrEP to underscore the tremendous recent advances. It also presents how embedded and deep-rooted inequities continue to exist in all phases of the research-to-implementation pipeline, and how these will limit who ultimately stands to benefit from LA modalities. We must attend to these perils, and approach LA HIV modalities with cautious optimism, in order to ensure availability, access and uptake for all.
THE STATE OF THE SCIENCE FOR LONG-ACTING ANTIRETROVIRAL THERAPY AND PREEXPOSURE PROPHYLAXIS MODALITIES
Long-acting injectable ART, administered every 2 months, has been approved by the US FDA, and Canadian and European regulators for virally suppressed people aged 18 years and over [2]. LAI PrEP, administered every 8 weeks, was approved by the US FDA in December 2021. The WHO recommended the vaginal PrEP ring in 2021 but the International Partnership for Microbicides (IPM) voluntarily withdrew its US FDA New Drug Application in December 2021 [26]. Additional LA ART and PrEP modalities are in all phases of clinical trials (Tables 1 and 2). In September 2021, there were 27 nonvaccine LA PrEP products in the pipeline [27]. LA ART modalities under study include injections and oral pills.
Table 1.
LA ART and PrEP modalities that are approved or under review
| PHASE and PrEP vs. ART | Study name; modality; drug used; and pharmaceutical company | Start date and end date | Sample size | Study population and exclusion criteria | Global location | Treatment duration/ dosing | Main findings and/or comments |
| Phase III; ART | ATLAS [100▪▪]; two intramuscular injections (buttocks); cabotegravir and rilpivirine; ViiV Healthcare (sponsor) & Janssen Pharmaceuticals (collaborator) & GlaxoSmithKline (collaborator) | Start date: October 28, 2016; end date: May 29, 2018 | 618 | 18+ years old, all sexes. On uninterrupted current regimen for at least 6 months. Pregnant and/or breastfeeding participants excluded | United States, Argentina, Australia, Canada, France, Germany, Italy, South Korea, Mexico, Russia, South Africa, Spain, Sweden | Every 4 weeks | At 48 weeks, monthly injections of long-acting injectable cabotegravir and rilpivirine were noninferior to standard oral therapy. Adverse effects (injection site pain) were common (75%), but rarely resulted in study withdrawal [101]. Results were similar at 96 weeks [28] |
| Phase III; ART | ATLAS-2M [102]; two intramuscular injections (buttocks); cabotegravir and rilpivirine; ViiV Healthcare (sponsor) & Janssen Research and Development (collaborator) | Start date: October 27, 2017; end date: June 6, 2019 | 1049 | 18+ years old, all sexes. On uninterrupted current regimen for at least 6 months. Pregnant and/or breastfeeding participants excluded | United States, Argentina, Australia, Canada, France, Germany, Italy, South Korea, Mexico, Russia, South Africa, Spain, Sweden | Every 8 weeks | The efficacy and safety profiles of dosing long-acting injectable cabotegravir and rilpivirine every 8 weeks were similar to dosing every 4 weeks [29] |
| Phase III; ART | FLAIR [103]; two intramuscular injections (buttocks); cabotegravir and rilpivirine; ViiV Healthcare (sponsor) & Janssen Pharmaceuticals (collaborator) & GlaxoSmithKline (collaborator) | Start date: October 27, 2016; end date: August 30, 2018 | 631 | 18+ years old, all sexes. Treatment naïve (≤10 days of prior therapy with any ART following diagnosis). Pregnant and/or breastfeeding participants excluded | United States, Canada, France, Germany, Italy, Japan, Netherlands, Russia, South Africa, Spain, United Kingdom | Every 4 weeks | At 48 weeks, long-acting injectable cabotegravir and rilpivirine was noninferior to standard oral therapy. Injection-site reactions were common [104]. Results were similar at 96 weeks [105] |
| Phase IIb/III; PrEP | HPTN 083 [106▪▪]; one intramuscular injection (buttocks); cabotegravir; NIAID (sponsor) & ViiV Healthcare (collaborator) & Gilead Sciences (collaborator) | Start date: December 6, 2016; end date: March 16, 2020 | 4570 | 18+ years old, assigned male at birth (cisgender men and transgender women who have sex with men). Participants with surgically placed or injected buttock implants or fillers excluded | United States, Argentina, Brazil, Peru, South Africa, Thailand, Vietnam | Every 8 weeks | Long-acting injectable cabotegravir (CAB-LA) was superior to daily oral tenofovir-emtricitabine (TDF-FTC) in preventing HIV infection among MSM and transgender women [107] |
| Phase III; PrEP | HPTN 084 [108]; one intramuscular injection (buttocks); cabotegravir; NIAID (sponsor) | Start date: November 7, 2017; end date: November 5, 2020 | 3200 | 18–45 years old, assigned female at birth. Pregnant and/or breastfeeding women and women who exclusively have sex with women excluded | Botswana, Kenya, Malawi, South Africa, Swaziland, Uganda, Zimbabwe | Every 8 weeks | Long-acting injectable cabotegravir (CAB-LA) was safe and superior to daily oral tenofovir-emtricitabine (TDF-FTC) for HIV prevention among cisgender women in sub-Saharan Africa [109] |
| Phase III; PrEP | The Ring Study [110]; vaginal ring; dapivirine; IPM (sponsor) | Start date: March 2012; end date: December 2016 | 1950 | 18–45 years old, assigned female at birth. Self-reported sexually active. Pregnant and/or breastfeeding women excluded | South Africa, Uganda | Every month | The ring was reported safe, with no difference in safety concerns between the experimental and placebo groups. Any side effects were mild in nature [111] |
| Phase III; PrEP | ASPIRE [112]; vaginal ring; dapivirine; IPM (sponsor) & NIAID (collaborator) | Start date: June 2012; end date: June 2015 | 3540 | 18–45 years old, assigned female at birth. Pregnant and/or breastfeeding women excluded | Malawi, South Africa, Uganda, Zimbabwe | Every month | The ring was reported safe, with no difference in safety concerns or side effects between the experimental and placebo group [113] |
| Phase IIIb; PrEP | DREAM [114]; vaginal ring; dapivirine; IPM (sponsor) | Start date: July 13, 2016; end date: December 10, 2018 | 850 | 18–45 years old, assigned female at birth. Self-reported sexually active. Previously enrolled in The Ring Study. Pregnant and/or breastfeeding women excluded | South Africa, Uganda | Every month | Follow-up study to the Ring Study. Found to have similar safety profile [115] |
| Phase IIIb; PrEP | HOPE [116▪]; vaginal ring; dapivirine; IPM (sponsor) | Start date: August 2016; end date: October 10, 2018 | 1576 | 18–45 years old, assigned female at birth. Previously enrolled in the ASPIRE study. Pregnant and/or breastfeeding women excluded | South Africa | Every month | Follow-up study to ASPIRE. Found to have similar safety profile to ASPIRE. Moderate side effects related to dapivirine occurred in only two patients [117] |
ART, antiretroviral therapy; IPM, International Partnership for Microbicides, Inc.; NIAID, National Institute of Allergy and Infectious Diseases; PrEP, preexposure prophylaxis.
Table 2.
LA ART and PrEP products currently in the clinical trial phase
| PHASE and PrEP vs. ART | Study name; modality; drug used; and pharmaceutical company | Start date and end date | Sample size | Study population and exclusion criteria | Global location | Treatment duration/ dosing periods | Main findings and/or comments |
| Phase III; ART | LATITUDE [118▪]; two intramuscular injections (buttocks); cabotegravir and rilpivirine; NIAID (sponsor) & ViiV Healthcare (collaborator) | Start date: March 28, 2019; end date (estimated): October 1, 2025 | 350 (Est.) | 18+ years old, all sexes. HIV-1 plasma viral load >200 copies/ml within 60 days prior to study entry. Evidence of nonadherence. Pregnant and/or breastfeeding participants excluded | United States, Puerto Rico | Every 4 weeks | Study in progress, no results posted |
| Phase II/III; ART | CAPELLA [42]; one subcutaneous injection (abdomen); lenacapavir; Gilead Sciences (sponsor) | Start date: November 21, 2019; end date: October 5, 2020 | 72 | 12+ years old, all sexes. HIV-1 plasma viral load >400 copies/ml at screening. Have multidrug resistance | United States, Canada, Dominican Republic, France, Germany, Italy, Japan, South Africa, Spain, Taiwan, Thailand | Every 6 months | Lenacapavir administered subcutaneously every 6 months maintained high rates of virologic suppression (73%) through 26 weeks in patients with multidrug resistance on failing regimen [119] |
| Phase III; PrEP | IMPOWER-022 [41]; once-monthly oral pill; islatravir; Merck Sharp & Dohme Corp. (sponsor) | Start date: February 24, 2021; end date (estimated): July 5, 2024 | 4500 (Est.) | 16–45 years old, assigned female at birth (cisgender identifying only). Sexually active with male partner in 30 days prior to screening. High risk for HIV. Pregnant and/or breastfeeding women excluded | United States, South Africa | Every month | Study in progress, no results posted |
| Phase III; PrEP | IMPOWER-024 [120]; once-monthly oral pill; islatravir; Merck Sharp & Dohme Corp. (sponsor) | Start date: March 15, 2021; end date (estimated): September 27, 2024 | 1500 (Est.) | 16+ years old, assigned male at birth (cisgender men and transgender women). Is sexually active (anal intercourse) with a cisgender male or TGW at least once in the past month. High risk for HIV | United States, France, Japan, Peru, South Africa, Thailand | Every month | Study in progress, no results posted |
| Phase II; PrEP | HPTN 083-01 [121]; one intramuscular injection (buttocks); cabotegravir; NIAID (sponsor) | Start date: February 19, 2020; end date (estimated): May 31, 2023 | 50 (Est.) | Under 18 years old, assigned male at birth (cisgender men, transgender women, and gender nonconforming people who have sex with men). Participants with surgically placed or injected buttock implants or fillers excluded | United States | Two time points 4 weeks apart and every 8 weeks thereafter | Study in progress, no results posted |
| Phase II; PrEP | HPTN 084-01 [122]; one intramuscular injection (buttocks); cabotegravir; NIAID (sponsor) | Start date: November 4, 2020; end date (estimated): May 2024 | 50 (Est.) | Under 18 years old, assigned female at birth. Pregnant and/or breastfeeding women and women who exclusively have sex with women excluded | South African, Uganda, Zimbabwe | Two time points 4 weeks apart and every 8 weeks thereafter | Study in progress, no results posted |
| Phase II; PrEP | NCT04003103 [123]; once-monthly oral pill; islatravir; Merck Sharp & Dohme Corp. (sponsor) | Start date: September 19, 2019; End date (estimated): March 15, 2022 | 250 (Est.) | 18–65 years old, all sexes. Low risk of HIV infection. Pregnant and/or breastfeeding women excluded | United States, Israel, South Africa | Every month | Study in progress, no results posted |
| Phase II; PrEP | MK-8591-043 [124]; implant (upper arm); islatravir; Merck Sharp & Dohme Corp. (sponsor) | Start date (estimated): December 13, 2021; end date (estimated): March 7, 2024 | 175 (Est.) | 18–55 years old, all sexes. Low risk of HIV infection. Pregnant and/or breastfeeding women excluded | No location provided | Every year (52 weeks) | Study has not commenced, no results posted |
| Phase I; PrEP | NCT03422172 [85]; one intramuscular injection (buttocks); cabotegravir; ViiV Healthcare (sponsor) & PPD (collaborator) | Start date: April 10, 2018; end date: April 20, 2020 | 48 | 18–65 years old, assigned male at birth. At risk of HIV infection (a casual male or female partner in the last 2 years). | China | Two time points 4 weeks apart and every 8 weeks thereafter | Long-acting injectable cabotegravir (CAB-LA) was safe and well tolerated overall, with only one participant experiencing an adverse event |
| Phase I; PrEP | MTN-027 [125]; vaginal ring; vicriviroc and/or MK-2048; NIAID (sponsor) | Start date: May 2015; end date: March 2016 | 48 | 18–45 years old, assigned female at birth. Pregnant and/or breastfeeding women excluded | United States | Every 28 days | The rings were safe and well tolerated. Both VCV and MK-2048 were quantifiable in all matrices tested with peak compartmental drug concentrations similar for single and combination drug rings. Tissue-associated VCV and/or MK-2048 did not correlate with inhibition of HIV infection [126] |
| Phase I; PrEP | MTN-028 [127]; vaginal ring; vicriviroc and MK-2048; NIAID (sponsor) | Start date: June 2015; end date: March 2016 | 19 | 18–45 years old, assigned female at birth. Pregnant and/or breastfeeding women excluded | United States | Every 28 days | Both rings were found to be safe and well tolerated. Drug release and plasma drug exposure were higher for the original-dose than for the low-dose ring [128] |
| Phase I; PrEP | MTN-036/IPM 047 [129]; vaginal ring; dapivirine; IPM (sponsor) & NIH (collaborator) & NIAID (collaborator) | Start date: December 4, 2017; end date: January 23, 2019 | 49 | 18–45 years old, assigned female at birth. Pregnant and/or breastfeeding women excluded | United States | Every 13 weeks | The extended duration DPV rings (100 mg for 13 weeks) were well tolerated and achieved higher DPV concentrations when compared to the monthly (25 mg) DPV ring [130] |
| Phase I; PrEP | MTN-044/IPM 053/CCN019 [131]; vaginal ring; dapivirine and levonorgestrel; IPM (sponsor) & NICHD, NIAID, NIMH, NIH, (collaborators) | Start date: July 17, 2018; end date: October 7, 2019 | 25 | 18–45 years old, assigned female at birth. Pregnant and/or breastfeeding women excluded | United States | Every 90 days (taking out every 28 days for 2 days) | The ring delivered sustained levels of each drug when used continuously for 90 days at levels likely sufficient to protect against HIV and unwanted pregnancy [132] |
| Phase I; PrEP | CAPRISA 018 [133]; implant (upper arm); tenofovir alafenamide; Center for the Aids Programme of Research in South Africa, Stichting Amsterdam institute for Global Health and Development, & Université Jean Monnet Saint-Etienne (sponsors) | Start date: January 1, 2017; end date (estimated): December 31, 2022 | 40 (Part A); 490 (Part B) (Est.) | Assigned female at birth. At-risk of HIV infection. Other inclusion and exclusion criteria not stated | South Africa | Optimal dosage and frequency to be determined during Part A lead-in | Study in progress, no results posted |
| Phase I; PrEP | MTN-026 [134]; rectal gel; dapivirine; NIAID (sponsor) | Start date: October 26, 2017; end date: September 20, 2018 | 28 | 18–45 years old, all sexes. History of receptive anal intercourse, per participant report. Pregnant and/or breastfeeding women excluded | United States, Thailand | Single dose, followed by 2-week washout period, followed by 7 consecutive days of dose administration | Participants reported favorable acceptability of the study DPV gel, with half preferring the gel over condoms and about 30% reporting equal preference. Side effects included leakage, diarrhea, and soiling [135] |
| Phase 1; PrEP | NCT03082690 [136]; rectal gel; IQP-0528; Johns Hopkins University (sponsor) & ImQuest Pharmaceuticals, Inc, & NIAID (collaborator) | Start date: November 1, 2017; end date: June 2, 2019 | 10 | 18+ years old, all sexes. History of receptive anal intercourse, per participant report | United Sates | Single dose | The gel was determined to be safe with one mild adverse event and no effect on rectal tissue histology. Benefits of the gel include local safety with no systematic absorption, delivery of local high IQP-0528 concentrations, and reductions in ex vivo HIV infectivity. The gel is limited by its rapid clearance and inability to penetrate vaginal tissue following rectal dosing [137] |
| Phase I; PrEP | MTN-033 [138]; rectal gel; dapivirine; NIAID (sponsor) | Start date: May 10, 2018; end date: December 3, 2018 | 16 | 18+ years old, assigned male at birth. History of receptive anal intercourse, per participant report | United States | Single dose, followed by 2- to 4-week washout period, followed by a second dose | DPV gel was reported safe and easy to use. However, a roughly 3-fold lower DPV exposure in plasma and lack of detectable DPV in tissue biopsies indicated formulation changes may be necessary to achieve protective tissue concentrations [139] |
| Phase I; PrEP | OB-002H-101 [140]; vaginal or rectal gel; OB-002H; Orion Biotechnology Polska Sp. z o.o. (sponsor) & SCOPE International AG (collaborator) | Start date: October 5, 2019; end date: August 31, 2020 | 60 | 18–45 years old, all sexes. Pregnant and/or breastfeeding women excluded. | Poland | Single dose vs. 5 consecutive days of dose administration | Overall, the product had a positive acceptability profile, and most of the participants would consider using the product against HIV infection and/or pregnancy. Only two Grade 2 adverse events occurred in the multiple dose arm of the study [141]. |
| Phase I; PrEP | DREAM-01 [142]; enema; tenofovir; John's Hopkin's University (sponsor) & University of California, Los Angeles (collaborator) & University of Pittsburgh (collaborator) | Start date: October 2016; end date: May 2019 | 21 | 18+ years old, assigned male at birth. History of receptive anal intercourse, per participant report | United States | Single dose | The product proved safe and acceptable with levels of TFV-DP reaching concentrations well above those linked to >90% efficacy. However, cumulative systemic tenofovir exposure was lower than seen with oral dosing. Only two adverse events were attributed to the study product [143] |
| Phase I; PrEP | PREVENT [144]; enema; Q-griffithsin; Rhonda Brand, University of Pittsburgh (sponsor) & NIAID (collaborator) & Intrucept Biomedicine LLC (collaborator) | Start date: July 10, 2019; end date: February 4, 2021 | 18 | 18–45 years old, all sexes. Pregnant and/or breastfeeding women excluded. Individuals undergoing gender reassignment excluded | United States | Single dose | Study permanently terminated due to the COVID-19 pandemic |
| Phase I; PrEP | DREAM-03 [145]; enema; tenofovir; John's Hopkin's University (sponsor) & NIAID (collaborator) & University of Pittsburgh (collaborator) | Start date: January 10, 2020; end date: April 27, 2021 | 9 | 18+ years old, all sexes. History of receptive anal intercourse, per participant report | United States | Three doses (sequence varies by experimental arm) | Study complete, but results not yet posted |
| Phase I; PrEP | ATN DREAM [146]; enema; tenofovir; University of Pittsburgh (sponsor) & University of North Carolina Chapel Hill (collaborator) & Emory University (collaborator) & Johns Hopkins University (collaborator) & NICHD (collaborator) | Start date: April 1, 2021; end date (estimated): July 1, 2022 | 16 (Est.) | 15–25 years old, assigned male at birth (cisgender MSM) | United States | Single dose | Study in progress, no results posted |
| Phase I; PrEP | DREAM-02 [147]; enema; tenofovir; John's Hopkin's University (sponsor) & NIAID (collaborator) & CONRAD (collaborator) | Start date: June 1, 2021; end date (estimated): December 31, 2021 | 16 (Est.) | 18+ years old, assigned male at birth. History of receptive anal intercourse, per participant report | United States | Single dose of study product (sequence and additional alternate product varies by experimental arm) | Study in progress, no results posted |
| Phase I; PrEP | IPM 042 [148]; vaginal insert (tablet); DS003; IPM (sponsor) | Start date: November 18, 2015; end date: August 26, 2016 | 36 | 18–45 years old, assigned female at birth. Pregnant and/or breastfeeding women excluded | No location provided | One tablet on Day 0 and one on Day 17 | DS003 tablets were safe and well tolerated [149], achieving local concentrations that are capable of protecting against HIV infection [150] |
| Phase I; PrEP | MTN-039 [151]; rectal insert; tenofovir alafenamide and elvitegravir; NIAID (sponsor) & CONRAD (collaborator) | Start date: December 11, 2019; end date: April 7, 2021 | 23 | 18+ years old, all sexes. History of receptive anal intercourse, per participant report. Pregnant and/or breastfeeding women excluded | United States | Single dose, followed by 7-day washout period, followed by two more doses | Study complete, but results not yet posted |
| Phase I; PrEP | NCT04319718 [152]; Vaginal film; MK-2048; Sharon Hillier, University of Pittsburgh (sponsor) & NIAID (collaborator) | Start date: August 19, 2020; end date (Estimated): December 21, 2021 | 48 (Est.) | 18–45 years old, assigned female at birth | United States | Single use | Study in progress, no results posted |
ART, antiretroviral therapy; IPM, International Partnership for Microbicides, Inc.; NIAID, National Institute of Allergy and Infectious Diseases; PrEP, preexposure prophylaxis.
Long-acting antiretroviral therapy modalities
LAI ART is a combination of cabotegravir and rilpivirine, branded as Vocabria and Rekambys in Europe and Cabenuva in the United States. In initial clinical trials LAI ART required two injections in the buttocks every 4 weeks and was noninferior to oral ART [28]. In subsequent trials, LAI ART administered every 8 weeks was noninferior to monthly injections [29]; this has been approved in Europe, Canada, and the United States [30,31]. LAI ART is only available to virologically suppressed individuals [32] and requires an oral lead-in [33]. Thus, LAI ART cannot substantially expand the number of virally suppressed individuals, though it may facilitate long-term viral suppression among those with episodic oral ART adherence. Also, because nonadherence is higher among minoritized populations (e.g., by race and ethnicity, sexuality, gender, and socioeconomic status) [34,35], this requirement may exacerbate existing inequities. To address these challenges, the LATITUDE study [36] is currently investigating LAI ART feasibility among nonsuppressed individuals, who must first achieve suppression using an oral lead-in.
Long-acting preexposure prophylaxis modalities
LAI PrEP was superior to oral PrEP in HIV Prevention Trials Network (HPTN) studies among cisgender men, transgender women, and cisgender women [37,38]. These trials are continuing as open-label extension studies and expanding to include acceptability assessments among those under 18 years of age [39,40]. LA PrEP is also in various stages of clinical trials including: monthly oral pills; vaginal and rectal gels; vaginal rings, films, and inserts; intramuscular and subcutaneous injections; implants; enemas; and micro-array patches [27]. As of June 2021, LA PrEP products in Phase III/IV clinical trials include a once-monthly vaginal ring, a once-monthly oral pill and a twice-yearly subcutaneous injection. Further, with goals of increased inclusivity, these studies include recruitment targets to increase participation among African-American and gender non-binary individuals [41,42]. The WHO has recommended the vaginal ring for PrEP [43] even though it reduced HIV infection risk by only 27–35% in Phase III studies, likely due to challenges with long-term adherence (this compares with 95% efficacy for LAI PrEP) [39,43].
EXISTING PERILS JEOPARDIZE THE PROMISE OF LONG-ACTING MODALITIES
One of the perils of LA modalities is that people who participated in the research that demonstrated their efficacy may not have equitable access to LA modalities once the modalities are approved and distributed. To some extent, this results from embedded biases in research that include where the trials are conducted, who is recruited for clinical trial enrollment, who is able to − and chooses to − enroll, and who benefits from post-research findings.
The need to ensure global availability
Though clinical trial eligibility criteria are necessary to determine a drug's efficacy, a lack of transparency regarding these criteria can directly affect participant trust [20,44,45] and willingness to engage with LA modalities once approved. For example, cisgender women were excluded from the initial DISCOVER trial (2016–2019) [46] that tested Descovy for PrEP among cisgender men and transgender women. Due to activism around their exclusion, a trial with cisgender women [47] began in 2021. Also, while the HPTN LAI PrEP trial [37] had an enrollment quota of 10% transgender women, it excluded individuals with buttock implants or fillers, a common practice among transgender women [48]. These exclusions are particularly salient since transgender women face increased HIV vulnerability [49].
Not all people choose to participate in clinical trials, and it is important to understand what motivates these choices for different people. Given the large number of LA modalities in development, sustained attention must also be given to informed refusal [50], namely individuals’ decisions to not consent for research participation, or the ways they may assert their own agency during trial participation. The two major oral PrEP trials among cisgender women, FEMPrEP [51], and VOICE [52], demonstrated the unique ways that cisgender women may choose to ‘opt out’ or engage in ‘informed refusal’ regarding PrEP use [53]. Studying informed refusal will make visible key silences and identify these individuals not as data omissions but rather as points of resistance and opportunities that offer insight into potential barriers to future access, uptake and sustained use [50,54,55,56▪▪]. Such insights are particularly important as new modalities are becoming more invasive (e.g., injection vs. pill) and may have different gender-based pharmacokinetics [57].
The vast majority of LA ART and PrEP clinical trials occur in South America, Asia, and sub-Saharan Africa due to high HIV incidence in these regions. While Global South participants often constitute the majority of clinical trial participants, the availability of the drug under study in these regions is often limited to clinical trial participation due to scant posttrial access. Yet, trial results are often used as the basis for the approval of HIV treatment and prevention modalities in the United States, Canada, and Europe (i.e., paralleling current LAI ART approval) vs. distribution in the Global South [20,58]. Also, despite differences in risk reductions (95% vs. approximately 30%), LAI PrEP was approved in the United States while the (less effective) ring is under review in sub-Saharan Africa, and has been approved in Zimbabwe [39,43,59]. Availability is also tempered by continued decreases in multilateral funding (e.g., PEPFAR) and patent protections that make medications prohibitively expensive. Though collaborations are forming to accelerate availability (e.g., by the International AIDS Vaccine Initiative, Scripps Research, and the US National Institutes of Health), affordable LA modalities will also require generic drug pricing and patent waivers [60,61].
The need to ensure equitable access and uptake
Even once ART and PrEP are available, deep-seated inequities can still affect their access and uptake. For example, in the United States, AIDS-related mortality overall decreased once oral ART was developed, but declines were greater among white and economically-advantaged populations [62]. Similarly, with oral PrEP, 40% of white individuals in the United States with PrEP indications received a prescription in 2018, vs. 6% of African Americans and 11% of Latinx individuals [63,64]. Oral PrEP use was 3-times lower for women than men relative to new HIV diagnoses [63] and average length of use was 5.8 months for women vs. 8.4 months for men [65,66].
Potential pathways through which socioeconomic status, race and ethnicity, sexuality, and gender may affect ART and PrEP access and uptake in the United States include whether providers offer them [67▪]; healthcare and insurance access (e.g., Medicaid expansion) [68]; medical mistrust [69]; perceived risk [70]; clinical support and wrap-around services [71]; caregiving demands [71,72]; food insecurity [73]; drug use [74]; stigmatization [75,76]; and transportation and employment [24,25,77,78]. Patients’ social contexts are unlikely to change alongside the advent of new biomedical modalities; many barriers to access and uptake of oral formulations will still exist for long-acting modalities [72,77,78,79▪▪,80]. These systemic barriers may also be perpetuated by LAI ART eligibility criteria − namely viral suppression − as this differs by age [81], race and ethnicity [82▪], public insurance [83], and gender [84].
Variations in access and uptake may also differ by LA modality type. LAI ART and PrEP may increase adherence because they are clinic vs. patient administered. However, LAI modalities tether patients to clinics with little room for variation, increasing the cost of administration. In contrast, LA oral and subcutaneous formulations are self-administered and may increase patient autonomy, but also potentially lower adherence. Patients’ social contexts must be acknowledged to address known challenges to adherence, such as oral lead-in concerns, and issues related to long pharmacokinetic tails and the potential need to return to oral medications [4,85]. Patients have expressed concerns about switching from oral to LA ART as it requires a new drug regimen, may have different adverse effects, and it limits their control over daily dosing [77,86,87]. Patients have also noted potential stigma and workplace-based challenges associated with the frequency of LA ART-related clinic visits [72,79▪▪,88].
Access to LA ART will not be equally distributed in settings like the United States that lack universal healthcare. Cabenuva costs approximately $50 000 annually and there is no generic equivalent. Although the US-based AIDS Drug Assistance Program (ADAP) provided HIV medication to 284 973 low-income individuals in 2018 [89], ADAP access is state administered and not universal. As of October 2021, only 22 US states had updated their ADAP formulary after Cabenuva's approval: of these, 10 covered Cabenuva, and 12 did not. Thus, patients outside those 10 states that cover Cabenuva may be unable to access LAI ART, especially since the manufacturer's patient assistance program does not currently cover ADAP patients, nor those outside of the United States. Similar financial inequities will likely exist with LA PrEP. Although its cost remains unknown, it will likely be more expensive than oral PrEP, making it cost-prohibitive for many [90]. Unless structural supports (e.g., insurance, universal healthcare) are introduced, LA HIV modalities will exacerbate the cost-related inequities evidenced in oral ART and PrEP access.
Issues of availability, access, and uptake must also be contextualized within intersecting inequities − such as homelessness, incarceration, mental health and substance use [91–93]. LA modalities are also available to treat mental health and substance use conditions [94,95], and patients’ experiences with those modalities (e.g., Vivitrol for opioid use disorder) may affect their willingness to engage in LA ART and PrEP [79▪▪]. The additional clinical steps for delivering LA HIV modalities to vulnerable communities may also complicate the provision of a ‘one stop shop’ approach to service integration, including for unhoused or recently incarcerated individuals.
Future directions
As LA HIV treatment and prevention modalities continue to advance, research and practice must acknowledge and address the historical and social contexts that limit global availability and access. The integration of social and behavioral scientists into clinical trial design and subsequent implementation studies may be of particular use to identify multilevel approaches to increase inclusion and equity at all stages of the research-to-implementation pipeline [96]. In contexts where LA HIV modalities are available, further research should address access and uptake within healthcare settings, for example how providers may serve as gatekeepers who determine which patients are ‘ready’ to switch from oral to LA formulations (e.g., by developing patient-provider decision aids to choose between LAI vs. oral ART or whether to begin PrEP, and in which modality) [97]. Various healthcare delivery models (e.g., telehealth and mobile vans) should be explored to facilitate equitable and person-centered utilization of prevention and treatment methods, as these models have been successful for delivering naloxone, clean syringes and COVID-19 vaccines. Research also needs to address the multilevel drivers of health policy initiatives and patent protections, including incorporating intersectionality-enhanced frameworks, [98] to facilitate an equitable scale-up of LA treatment and prevention modalities for all.
CAUTIOUS OPTIMISM WITH ADDITIONAL TOOLS IN THE TOOLKIT
There have been tremendous advances in LA ART and PrEP modalities, with even more products in the pipeline. Yet the perils that constrain their availability, access and uptake demonstrate the need for cautious optimism as to whether ‘ending the HIV epidemic’ is within reach. Biomedical technologies, no matter how innovative, cannot reach their full promise without applying social and behavioral strategies to address context-specific factors. Such approaches will improve how these LA modalities are developed and tested, distributed, and who can access them (or opt-out if they so choose). This is particularly salient for scale-up in low-resource settings where context-specific challenges have historically impeded wide-scale rollout of HIV prevention and treatment technologies [99]. As the history of the HIV and AIDS response has demonstrated, focusing solely on the medication, clinic, and patient−provider interactions is insufficient: tackling the social and political dimensions that limit equitable access requires political struggle, social movements, and global accountability. Social and behavioral sciences should be leveraged as complementary tools to biomedical advances to better understand the lived experiences of marginalized community members; the failure to do so will increase medical paternalism and hinder patient−provider relationships. In order for LA HIV modalities to truly fulfill their promise of ‘ending the HIV epidemic’, equity in availability, access and uptake must be addressed on a global scale.
Acknowledgements
We would like to acknowledge and thank Dr Richard Parker and Dr Jesse Clark for their thorough and thoughtful comments during the development of this paper. We also want to acknowledge Rachel Maggi for her invaluable support in compiling the tables and supporting the development of the section on the state of the science.
Financial support and sponsorship
This work was supported in part by grants awarded from the U.S. National Institute of Health (National Institute on Drug Abuse: K01DA039804A and National Institute of Mental Health: R34MH124552) and the Canadian Institutes of Health Research (Canada Research Chair, Tier 2).
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1. Fast-Track − Ending the AIDS epidemic by 2030. Available at: https://www.unaids.org/en/resources/documents/2014/JC2686_WAD2014report [Accessed 1 December 2021] [Google Scholar]
- 2. ViiV Healthcare Announces US FDA Approval of Cabenuva (CABOTEGRAVIR, RILPIVIRINE) for Use Every Two Months, Expanding the LabelL of the First and only complete long-acting HIV Treatment, https://viivhealthcare.com/hiv-news-and-media/news/press-releases/2022/january/viiv-healthcare-announces-fda-approval-of-cabenuva-for-use-every-two-months/ [Accessed 14th February] [Google Scholar]
- 3. Injectable HIV therapy would have to cost less than $131 a year to be cost-effective in Africa. aidsmap.com. Available at: https://www.aidsmap.com/news/apr-2021/injectable-hiv-therapy-would-have-cost-less-131-year-be-cost-effective-africa [Accessed 22 November 2021] [Google Scholar]
- 4.Scarsi KK, Swindells S. The promise of improved adherence with long-acting antiretroviral therapy: what are the data? J Int Assoc Provid AIDS Care 2021; 20: 23259582211009012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Landovitz RJ, Kofron R, McCauley M. The promise and pitfalls of long acting injectable agents for HIV prevention. Curr Opin HIV AIDS 2016; 11:122–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kippax SC, Holt M, Friedman SR. Bridging the social and the biomedical: engaging the social and political sciences in HIV research. J Int AIDS Soc 2011; 14: (Suppl 2): S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kippax S, Stephenson N. Beyond the distinction between biomedical and social dimensions of HIV prevention through the lens of a social public health. Am J Public Health 2012; 102:789–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aggleton P, Parker R. Moving beyond biomedicalization in the HIV response: implications for community involvement and community leadership among men who have sex with men and transgender people. Am J Public Health 2015; 105:1552–1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benning L, Mantsios A, Kerrigan D, et al. Examining adherence barriers among women with HIV to tailor outreach for long-acting injectable antiretroviral therapy. BMC Womens Health 2020; 20:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10▪.Kanazawa JT, Saberi P, Sauceda JA, et al. The LAIs are coming! Implementation science considerations for long-acting injectable antiretroviral therapy in the United States: a scoping review. AIDS Res Hum Retroviruses 2021; 37:75–88. [DOI] [PMC free article] [PubMed] [Google Scholar]; This scoping review article used the PRISM model to review the ever-expanding literature on LAI ART implementation. The review revealed the need for more data and research on the acceptability of LAI ART among certain subgroups, cost effectiveness, patient satisfaction and outcomes, and additional ethical considerations.
- 11. KFF. The U.S. & the Global Fund to Fight AIDS, Tuberculosis and Malaria. 2021. Available at: https://www.kff.org/global-health-policy/fact-sheet/the-u-s-the-global-fund-to-fight-aids-tuberculosis-and-malaria/ [Accessed 14 January 2022] [Google Scholar]
- 12.Novogrodsky N. Duty of treatment human rights and the HIV/AIDS pandemic. Yale Hum Rights Dev Law J 2009; 12:1–61. [Google Scholar]
- 13.Grover A, Citro B, Mankad M, et al. Pharmaceutical companies and global lack of access to medicines: strengthening accountability under the right to health. J Law Med Ethics 2012; 40:234–250. [DOI] [PubMed] [Google Scholar]
- 14.Boylan M. Medical pharmaceuticals and distributive justice. Camb Q Healthc Ethics 2008; 17:30–44. [DOI] [PubMed] [Google Scholar]
- 15.Piot P, Russell S, Larson H. Good politics, bad politics: the experience of AIDS. Am J Public Health 2007; 97:1934–1936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sidibé M, Piot P, Dybul M. AIDS is not over. Lancet 2012; 380:2058–2060. [DOI] [PubMed] [Google Scholar]
- 17.Berkman A, Garcia J, Muñoz-Laboy M, et al. A Critical analysis of the Brazilian response to HIV/AIDS: lessons learned for controlling and mitigating the epidemic in developing countries. Am J Public Health 2005; 95:1162–1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Braude HD. Colonialism, Biko and AIDS: reflections on the principle of beneficence in South African medical ethics. Soc Sci Med 2009; 68:2053–2060. [DOI] [PubMed] [Google Scholar]
- 19.Stadler J, Scorgie F, van der Straten A, et al. Adherence and the lie in a HIV prevention clinical trial. Med Anthropol 2016; 35:503–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sugarman J, Mayer KH. Ethics and preexposure prophylaxis for HIV infection. J Acquir Immune Defic Syndr 2013; 63:S135–S139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thabethe S, Slack C, Lindegger G, et al. Why don’t you go into suburbs? Why are you targeting us?: trust and mistrust in HIV vaccine trials in South Africa. J Empir Res Hum Res Ethics 2018; 13:525–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Flynn MB. Global capitalism as a societal determinant of health: a conceptual framework. Soc Sci Med 2021; 268:113530. [DOI] [PubMed] [Google Scholar]
- 23▪.Thoueille P, Choong E, Cavassini M, et al. Long-acting antiretrovirals: a new era for the management and prevention of HIV infection. J Antimicrob Chemother 2021; doi: 10. 1093/jac/dkab324. [Online ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]; This review problematizes the ‘one-size-fits-all’ approach to the administration of LAI ART and suggests that future research must consider the significant inter-individual variability in LAI ART pharmacokinetics. This review also offers therapeutic drug monitoring as a potential solution to improve the management of LAI ART in individual patients.
- 24.Philbin MM, Parker CM, Parker RG, et al. The promise of pre-exposure prophylaxis for black men who have sex with men: an ecological approach to attitudes, beliefs, and barriers. AIDS Patient Care STDS 2016; 30:282–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Philbin MM, Parker CM, Parker RG, et al. Gendered social institutions and preventive healthcare seeking for black men who have sex with men: the promise of biomedical HIV prevention. Arch Sex Behav 2018; 47:2091–2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. IPM Statement on US Food and Drug Administration Review of Dapivirine Vaginal Ring. Available at: https://www.ipmglobal.org/content/ipm-statement-us-food-and-drug-administration-review-dapivirine-vaginal-ring [Accessed 14 February 2022] [Google Scholar]
- 27. The Future of ARV-Based Prevention and More. AVAC. 2018. Available at: https://www.avac.org/infographic/future-arv-based-prevention [Accessed 5 November 2021] [Google Scholar]
- 28.Swindells S, Lutz T, van Zyl L, et al. Long-acting cabotegravir + rilpivirine for HIV-1 treatment: ATLAS week 96 results. AIDS 2022; 36:185–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Overton ET, Richmond G, Rizzardini G, et al. Long-acting cabotegravir and rilpivirine dosed every 2 months in adults with HIV-1 infection (ATLAS-2 M), 48-week results: a randomised, multicentre, open-label, phase 3b, noninferiority study. Lancet 2020; 396:1994–2005. [DOI] [PubMed] [Google Scholar]
- 30. ViiV Healthcare Announces US FDA Approval of Cabenuva (CABOTEGRAVIR, RILPIVIRINE) for Use Every Two Months, Expanding the LabelL of the First and only complete long-acting HIV Treatment, https://viivhealthcare.com/hiv-news-and-media/news/press-releases/2022/january/viiv-healthcare-announces-fda-approval-of-cabenuva-for-use-every-two-months/ [Accessed 14th February] [Google Scholar]
- 31. Long-acting injectable HIV treatment approved in the EU: includes two-monthly dosing | HTB | HIV i-Base. Available at: https://i-base.info/htb/39602 [Accessed 7 January 2022] [Google Scholar]
- 32. Clinical Trials | CABENUVA (cabotegravir; rilpivirine). Available at: https://cabenuvahcp.com/clinical-trials/ [Accessed 5 November 2021] [Google Scholar]
- 33. Research C for DE. FDA Approves Cabenuva and Vocabria for the Treatment of HIV-1 Infection. FDA. 2021. Available at: https://www.fda.gov/drugs/human-immunodeficiency-virus-hiv/fda-approves-cabenuva-and-vocabria-treatment-hiv-1-infection [Accessed 5 November 2021] [Google Scholar]
- 34. CDC. HIV and Women. Centers for Disease Control and Prevention. 2021. Available at: https://www.cdc.gov/hiv/group/gender/women/index.html [Accessed 20 July 2021] [Google Scholar]
- 35. CDC. HIV and Gay and Bisexual Men. Centers for Disease Control and Prevention. 2020. Available at: https://www.cdc.gov/hiv/group/msm/index.html [Accessed 18 August 2021] [Google Scholar]
- 36. A5359: The LATITUDE Study – ACTG Network. Available at: https://actgnetwork.org/studies/a5359-the-latitude-study/ [Accessed 5 November 2021] [Google Scholar]
- 37. The HIV Prevention Trials Network | Prevention Now. Available at: https://www.hptn.org/research/studies/hptn083 [Accessed 5 November 2021] [Google Scholar]
- 38. The HIV Prevention Trials Network | Prevention Now. Available at: https://www.hptn.org/research/studies/hptn084 [Accessed 5 November 2021] [Google Scholar]
- 39. HPTN 083-01. HPTN 083-01: Safety, Tolerability and Acceptability of Long-Acting Cabotegravir (CAB LA) for the Prevention of HIV among Adolescent Males – A sub-study of HPTN 083. DAIDS Document ID: 38654, Division of AIDS (DAIDS), United States (US) National Institute of Allergy and Infectious Diseases (NIAID), Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), US National Institutes of Health (NIH). 2021. Available at: https://www.hptn.org/sites/default/files/inline-files/HPTN%20083-01_Version%203.0_FINAL_2Jul2021.pdf. [Google Scholar]
- 40. The HIV Prevention Trials Network | Prevention Now. Available at: https://www.hptn.org/research/studies/084-01 [Accessed 5 November 2021] [Google Scholar]
- 41. Merck Sharp & Dohme Corp. A Phase 3, Randomized, Active-Controlled, Double-blind Clinical Study to Evaluate the Efficacy and Safety of Oral Islatravir Once-Monthly as Preexposure Prophylaxis in Cisgender Women at High Risk for HIV-1 Infection. Clinical Trial Registration NCT04644029, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT04644029 [Accessed 23 November 2021] [Google Scholar]
- 42. Gilead Sciences. A Phase 2/3 Study to Evaluate the Safety and Efficacy of Long Acting Capsid Inhibitor GS-6207 in Combination With an Optimized Background Regimen in Heavily Treatment Experienced People Living With HIV-1 Infection with Multidrug Resistance. Clinical Trial Registration NCT04150068, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT04150068 [Accessed 21 November 2021] [Google Scholar]
- 43. International Partnership for Microbicides. A Long-Acting Ring for Women's HIV Prevention. Available at: https://www.ipmglobal.org/sites/default/files/attachments/publication/ipm_ring_backgrounder_sept_2021_final.pdf [Accessed September 2021] [Google Scholar]
- 44.Perez-Brumer A, Naz-McLean S, Huerta L, et al. The wisdom of mistrust: qualitative insights from transgender women who participated in PrEP research in Lima, Peru. J Int AIDS Soc 2021; 24:e25769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bogart LM, Takada S, Cunningham WE. Medical mistrust, discrimination, and the domestic HIV epidemic. In: Ojikutu BO, Stone VE, editors. HIV in US communities of color. Cham: Springer International Publishing; 2021, 256 pages. Available at: https://link.springer.com/book/10.1007/978-3-030-48744-7#about. [Google Scholar]
- 46. Does DESCOVY for PrEP® Work?. Available at: https://www.descovy.com/clinical-trial-efficacy-results [Accessed 5 November 2021] [Google Scholar]
- 47. Gilead Announces New Arm of HIV Womens Prevention Study. Available at: https://www.gilead.com/news-and-press/company-statements/gilead-announces-new-arm-of-hiv-womens-prevention-study [Accessed 7 January 2022] [Google Scholar]
- 48.Rael CT, Martinez M, Giguere R, et al. Transgender women's concerns and preferences on potential future long-acting biomedical HIV prevention strategies: the case of injections and implanted medication delivery devices (IMDDs). AIDS Behav 2020; 24:1452–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. CDC Newsroom. CDC. 2016. Available at: https://www.cdc.gov/media/releases/2021/p0414-trans-HIV.html [Accessed 5 November 2021] [Google Scholar]
- 50.Benjamin R. Informed refusal: toward a justice-based bioethics. Sci Technol Hum Values 2016; 41:967–990. [Google Scholar]
- 51.Van Damme L, Corneli A, Ahmed K, et al. Preexposure prophylaxis for HIV infection among African women. N Engl J Med 2012; 367:411–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Marrazzo JM, Ramjee G, Richardson BA, et al. Tenofovir-based preexposure prophylaxis for HIV infection among African women. N Engl J Med 2015; 372:509–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.van der Straten A, Stadler J, Montgomery E, et al. Women's experiences with oral and vaginal preexposure prophylaxis: the VOICE-C qualitative study in Johannesburg, South Africa. PLoS One 2014; 9:e89118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.TallBear K. Native American DNA: Tribal Belonging and the False Promise o Genetic Science. 2013. Available at: https://www.upress.umn.edu/book-division/books/native-american-dna [Accessed 24 November 2021] [Google Scholar]
- 55.Molldrem S, Smith AKJ. Reassessing the ethics of molecular HIV surveillance in the era of cluster detection and response: toward HIV data justice. Am J Bioeth 2020; 20:10–23. [DOI] [PubMed] [Google Scholar]
- 56▪▪.Nuriddin A, Mooney G, White AIR. Reckoning with histories of medical racism and violence in the USA. Lancet 2020; 396:949–951. [DOI] [PMC free article] [PubMed] [Google Scholar]; This article describes the history of medical racism in the U.S. Although not explicitly mentioned, it can be inferred that the resulting medical mistrust that marginalized groups in the U.S., particularly African-Americans, experience towards the healthcare system has implications on the acceptability and uptake of new HIV biomedical technologies among these groups.
- 57.Landovitz RJ, Li S, Grinsztejn B, et al. Safety, tolerability, and pharmacokinetics of long-acting injectable cabotegravir in low-risk HIV-uninfected individuals: HPTN 077, a phase 2a randomized controlled trial. PLoS Med 2018; 15:e1002690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pyra MN, Haberer JE, Hasen N, et al. Global implementation of PrEP for HIV prevention: setting expectations for impact. J Int AIDS Soc; 2019; 22:e25370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Dapivirine Vaginal Ring for HIV Prevention No Longer Under Consideration by the FDA. Available at: https://www.medscape.com/viewarticle/967175#vp_1 [Accessed 14th February] [Google Scholar]
- 60.Chandiwana NC, Serenata CM, Owen A, et al. Impact of long-acting therapies on the global HIV epidemic. AIDS 2021; 35:S137–S143. [DOI] [PubMed] [Google Scholar]
- 61.Heath K, Levi J, Hill A. The Joint United Nations Programme on HIV/AIDS 95–95–95 targets: worldwide clinical and cost benefits of generic manufacture. AIDS 2021; 35:S197–S203. [DOI] [PubMed] [Google Scholar]
- 62.Rubin MS, Colen CG, Link BG. Examination of inequalities in HIV/AIDS mortality in the United States from a fundamental cause perspective. Am J Public Health 2010; 100:1053–1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Siegler AJ, Mouhanna F, Giler RM, et al. The prevalence of preexposure prophylaxis use and the preexposure prophylaxis-to-need ratio in the fourth quarter of 2017, United States. Ann Epidemiol 2018; 28:841–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Harris NS. Vital signs: status of human immunodeficiency virus testing, viral suppression, and HIV preexposure prophylaxis — United States, 2013–2018. MMWR Morb Mortal Wkly Rep 2019; 68:1117–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hicks S. Staying on PrEP is Significantly Different for PrEP Users With Commercial Insurance Versus Medicaid. TheBodyPRO.com. 2019. Available at: http://www.thebodypro.com/content/81655/staying-on-prep-commercial-insurance-vs-medicaid.html [Accessed 8 April 2019] [Google Scholar]
- 66.Huang Y-LA. Persistence with HIV preexposure prophylaxis in the United States, 2012–2016. 2019. Available at: http://www.croiwebcasts.org/console/player/41212?crd_fl=0&ssmsrq=1554747561744 [Accessed 8 April 2019] [Google Scholar]
- 67▪.Bradley E, Hoover K. Improving HIV preexposure prophylaxis implementation for women: summary of key findings from a discussion series with women's HIV prevention experts. Womens Health Issues 2019; 1:3–7. [DOI] [PubMed] [Google Scholar]; This article advances information on the challenges that women experience regarding PrEP uptake, including lack of knowledge about PrEP, lack of HIV-related health literacy and risk perception, difficulty assessing risk, provider bias, cost, contextual factors, and inadequate infrastructure and resources. This article helps inform potential barriers for future uptake of LA PrEP modalities as they move through the research and development pipeline.
- 68. The Kaiser Family Foundation. Status of State Action on the Medicaid Expansion Decision. The Henry J. Kaiser Family Foundation. 2019. Available at: https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/ [Accessed 8 April 2019] [Google Scholar]
- 69.Kalichman SC, Eaton L, Kalichman MO, et al. Race-based medical mistrust, medication beliefs and HIV treatment adherence: test of a mediation model in people living with HIV/AIDS. J Behav Med 2016; 39:1056–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Auerbach JD, Kinsky S, Brown G, et al. Knowledge, attitudes, and likelihood of pre-exposure prophylaxis (PrEP) use among US women at risk of acquiring HIV. AIDS Patient Care STDS 2014; 29:102–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mellins CA, Kang E, Leu CS, et al. Longitudinal study of mental health and psychosocial predictors of medical treatment adherence in mothers living with HIV disease. AIDS Patient Care STDS 2003; 17:407–416. [DOI] [PubMed] [Google Scholar]
- 72.Kerrigan D, Mantsios A, Gorgolas M, et al. Experiences with long acting injectable ART: a qualitative study among PLHIV participating in a Phase II study of cabotegravir + rilpivirine (LATTE-2) in the United States and Spain. PLoS One 2018; 13:e0190487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Spinelli MA, Frongillo EA, Sheira LA, et al. Food insecurity is associated with poor HIV outcomes among women in the United States. AIDS Behav 2017; 21:3473–3477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Carter A, Roth EA, Ding E, et al. Substance use, violence, and antiretroviral adherence: a latent class analysis of women living with HIV in Canada. AIDS Behav 2018; 22:971–985. [DOI] [PubMed] [Google Scholar]
- 75.Rice WS, Turan B, Fletcher FE, et al. A mixed methods study of anticipated and experienced stigma in healthcare settings among women living with HIV in the United States. AIDS Patient Care STDS 2019; 33:184–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kalichman SC, DiMarco M, Austin J, et al. Stress, social support, and HIV-status disclosure to family and friends among HIV-positive men and women. J Behav Med 2003; 26:315–332. [DOI] [PubMed] [Google Scholar]
- 77.Philbin MM, Parish C, Kinnard EN, et al. A multisite study of women living with HIV's perceived barriers to, and interest in, long-acting injectable antiretroviral therapy. J Acquir Immune Defic Syndr 2020; 84:263–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Philbin MM, Parish C, Kinnard EN, et al. Interest in long-acting injectable preexposure prophylaxis (LAI PrEP) among women in the women's interagency HIV study (WIHS): a qualitative study across six cities in the United States. AIDS Behav 2021; 25:667–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79▪▪.Philbin MM, Parish C, Bergen S, et al. A qualitative exploration of women's interest in long-acting injectable antiretroviral therapy across six cities in the women's interagency HIV study: intersections with current and past injectable medication and substance use. AIDS Patient Care STDS 2021; 35:23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]; This qualitative study conducted interviews with women living with HIV to assess interest for LAI ART. A particularly meaningful finding from this study came from women with a past history of substance use who had concerns about LAI ART triggering a recurrence. While other substance users did not have concerns, this insight has implications for LAI ART uptake among individuals in this at-risk group.
- 80.Philbin MM, Bergen S, Parish C, et al. Long-acting injectable ART and PrEP among women in six cities across the United States: a qualitative analysis of who would benefit the most. AIDS Behav 2021; Oct 14. doi: 10.1007/s10461-021-03483-7. [Online ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Centers for Disease Control and Prevention. HIV Among Youth | Age | HIV by Group | HIV/AIDS | CDC. 2019. Available at: https://www.cdc.gov/hiv/group/age/youth/index.html [Accessed 30 August 2019] [Google Scholar]
- 82▪.Crepaz N, Dong X, Hess KL, et al. Racial and ethnic disparities in sustained viral suppression and transmission risk potential among persons aged 13–29 years living with diagnosed HIV infection, United States, 2016. J Acquir Immune Defic Syndr 2020; 83:334–339. [DOI] [PMC free article] [PubMed] [Google Scholar]; This article assessed rates of sustained viral suppression among racial/ethnic groups aged 18–39 in the U.S. The researchers found that sustained viral suppression in this age group was suboptimal and transmission risk was high. In addition, it was found that racial/ethnic groups were disproportionately affected, with Black individuals having the lowest prevalence of sustained viral suppression. These results have implications for LAI ART uptake, as viral suppression is currently required to be eligible for LAI ART.
- 83.Geter A, Sutton MY, Armon C, et al. Disparities in viral suppression and medication adherence among women in the USA, 2011–2016. AIDS Behav 2019; 23:3015–3023. [DOI] [PubMed] [Google Scholar]
- 84.Beer L, Mattson CL, Bradley H, et al. Understanding cross-sectional racial, ethnic, and gender disparities in antiretroviral use and viral suppression among HIV patients in the United States. Medicine (Baltimore) 2016; 95:e3171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. ViiV Healthcare. An Open Label, Phase 1 Study to Evaluate the PK, Safety, Tolerability and Acceptability of Long Acting Injections of the HIV Integrase Inhibitor, Cabotegravir (CAB; GSK1265744) in HIV Uninfected Chinese Men. Clinical Trial Registration NCT03422172, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT03422172 [Accessed 22 November 2021] [Google Scholar]
- 86.Dubé K, Eskaf S, Evans D, et al. The dose response: perceptions of people living with HIV in the United States on alternatives to oral daily antiretroviral therapy. AIDS Res Hum Retroviruses 2020; 36:324–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kerrigan D, Sanchez Karver T, Muraleetharan O, et al. A dream come true: perspectives on long-acting injectable antiretroviral therapy among female sex workers living with HIV from the Dominican Republic and Tanzania. PLoS One 2020; 15:e0234666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mantsios A, Murray M, Karver TS, et al. Efficacy and freedom: patient experiences with the transition from daily oral to long-acting injectable antiretroviral therapy to treat HIV in the context of Phase 3 trials. AIDS Behav 2020; 24:3473–3481. [DOI] [PubMed] [Google Scholar]
- 89. Total ADAP Clients Enrolled and Served. KFF. 2021. Available at: https://www.kff.org/hivaids/state-indicator/total-adap-clients-served/ [Accessed 17 November 2021] [Google Scholar]
- 90. Neilan A. Cost-effectiveness of long-acting PrEP among MSM/TGW in the US. 2021. [Google Scholar]
- 91. Psychosocial Mediators of Antiretroviral Nonadherence in HIV-Positive Adults with Substance Use and Mental Health Problems. PsycNET. Available at: https://psycnet.apa.org/doiLanding?doi=10.1037%2F0278-6133.23.4.363 [Accessed 22 November 2021] [Google Scholar]
- 92.Haas AD, Technau K-G, Pahad S, et al. Mental health, substance use and viral suppression in adolescents receiving ART at a paediatric HIV clinic in South Africa. J Int AIDS Soc 2020; 23:e25644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Philbin MM, Tanner AE, DuVal A, et al. Factors affecting linkage to care and engagement in care for newly diagnosed HIV-positive adolescents within fifteen adolescent medicine clinics in the United States. AIDS Behav 2014; 18:1501–1510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Flexner C, Thomas DL, Swindells S. Creating demand for long-acting formulations for the treatment and prevention of HIV, tuberculosis, and viral hepatitis. Curr Opin HIV AIDS 2019; 14:13–20. [DOI] [PubMed] [Google Scholar]
- 95.Morgan JR, Schackman BR, Leff JA, et al. Injectable naltrexone, oral naltrexone, and buprenorphine utilization and discontinuation among individuals treated for opioid use disorder in a United States commercially insured population. J Subst Abuse Treat 2018; 85:90–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Morton T, Chege W, Swann E, et al. Advancing long-acting and extended delivery HIV prevention and treatment regimens through behavioural science: NIH workshop directions. AIDS 2021; 35:1313–1317. [DOI] [PubMed] [Google Scholar]
- 97. Online decision aid addresses health disparities among MSM | Health Communication Core. Available at: https://healthcommcore.org/news/online-decision-aid-addresses-health-disparities-among-msm [Accessed 5 November 2021] [Google Scholar]
- 98. Intersectionality-Enhanced Consolidated Framework for Implementation Research. Available at: https://knowledgetranslation.net/wp-content/uploads/2020/02/Intersectionality_Enhanced_CFIR_Table_final.pdf. [Google Scholar]
- 99.Landovitz RJ, Grinsztejn B. Long-acting injectable preexposure prophylaxis for HIV prevention in South Africa: is there a will and a way? J Infect Dis 2016; 213:1519–1520. [DOI] [PubMed] [Google Scholar]
- 100▪▪. ViiV Healthcare. A Phase III, Randomized, Multicenter, Parallel-group, Noninferiority, Open-label Study Evaluating the Efficacy, Safety, and Tolerability of Switching to Long-acting Cabotegravir Plus Long-acting Rilpivirine From Current INI- NNRTI-, or PI-based Antiretroviral Regimen in HIV-1-infected Adults Who Are Virologically Suppressed. Clinical Trial Registration NCT02951052, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT02951052 [Accessed 19 July 2021] [Google Scholar]; The ATLAS clinical trial found that the combination of cabotegravir and rilpivirine administered as an intramuscular injection every 4 weeks was noninferior to oral ART. This trial, in addition to the FLAIR clinical trial (which was conducted among treatment naïve individuals) lead to the approval of the use of LAI ART for people 18 years of age and older by regulatory bodies in the U.S., Canada, and Europe. ATLAS-2M is a subsequent clinical trial that found that LAI ART administered every 8 weeks is noninferior to injections every 4 weeks.
- 101.Swindells S, Andrade-Villanueva J-F, Richmond GJ, et al. Long-acting cabotegravir and rilpivirine for maintenance of HIV-1 suppression. N Engl J Med 2020; 382:1112–1123. [DOI] [PubMed] [Google Scholar]
- 102. ViiV Healthcare. A Phase IIIb, Randomized, Multicenter, Parallel-group, Noninferiority, Open-label Study Evaluating the Efficacy, Safety, and Tolerability of Long-acting Cabotegravir Plus Long-acting Rilpivirine Administered Every 8 Weeks or Every 4 Weeks in HIV-1-infected Adults Who Are Virologically Suppressed. Clinical Trial Registration NCT03299049, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT03299049 [Accessed 18 November 2021] [Google Scholar]
- 103. ViiV Healthcare. A Phase III, Randomized, Multicenter, Parallel-group, Open-Label Study Evaluating the Efficacy, Safety, and Tolerability of Long-Acting Intramuscular Cabotegravir and Rilpivirine for Maintenance of Virologic Suppression Following Switch From an Integrase Inhibitor Single Tablet Regimen in HIV-1 Infected Antiretroviral Therapy Naive Adult Participants. Clinical Trial Registration NCT02938520, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT02938520 [Accessed 19 July 2021] [Google Scholar]
- 104.Orkin C, Arasteh K, Górgolas Hernández-Mora M, et al. Long-acting cabotegravir and rilpivirine after oral induction for HIV-1 infection. N Engl J Med 2020; 382:1124–1135. [DOI] [PubMed] [Google Scholar]
- 105.Orkin C, Oka S, Philibert P, et al. Long-acting cabotegravir plus rilpivirine for treatment in adults with HIV-1 infection: 96-week results of the randomised, open-label, phase 3 FLAIR study. Lancet HIV 2021; 8:e185–e196. [DOI] [PubMed] [Google Scholar]
- 106▪▪. National Institute of Allergy and Infectious Diseases (NIAID). A Phase 2b/3 Double Blind Safety and Efficacy Study of Injectable Cabotegravir Compared to Daily Oral Tenofovir Disoproxil Fumarate/Emtricitabine (TDF/FTC), For Pre-Exposure Prophylaxis in HIV-Uninfected Cisgender Men and Transgender Women Who Have Sex With Men. Clinical Trial Registration NCT02720094, clinicaltrials.gov. 2020. Available at: https://clinicaltrials.gov/ct2/show/NCT02720094 [Accessed 16 November 2021] [Google Scholar]; The HPTN 083 clinical trial found that cabotegravir administered as an intramuscular injection every 8 weeks was superior to oral PrEP regimens among cisgender men and transgender women. A similar clinical trial, HPTN 084, conducted among cisgender women also found that LAI PrEP was superior to oral PrEP, with even greater effectiveness than the 083 trial. Currently two additional clinical trials, HPTN 083-01 (cisgender men and transgender women) and HPTN 084-01 (cisgender women), are recruiting participants to assess the effectiveness of LAI PrEP in individual under the age of 18.
- 107.Landovitz RJ, Donnell D, Clement ME, et al. Cabotegravir for HIV prevention in cisgender men and transgender women. N Engl J Med 2021; 385:595–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. National Institute of Allergy and Infectious Diseases (NIAID). A Phase 3 Double Blind Safety and Efficacy Study of Long-Acting Injectable Cabotegravir Compared to Daily Oral TDF/FTC for Pre-Exposure Prophylaxis in HIV-Uninfected Women. Clinical Trial Registration NCT03164564, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT03164564 [Accessed 16 November 2021] [Google Scholar]
- 109. HPTN 084 Study Demonstrates Superiority of Injectable Cabotegravir to Oral FTC/TDF for the Prevention of HIV in Cisgender Women in Sub-Saharan Africa | The HIV Prevention Trials Network. Available at: https://www.hptn.org/news-and-events/announcements/hptn-084-study-demonstrates-superiority-of-injectable-cabotegravir-to [Accessed 24 November 2021] [Google Scholar]
- 110. International Partnership for Microbicides, Inc. A Multi-Centre, Randomised, Double-Blind, Placebo-Controlled Safety and Efficacy Trial of a Dapivirine Vaginal Matrix Ring in Healthy HIV-Negative Women. Clinical Trial Registration NCT01539226, clinicaltrials.gov. 2021. https://clinicaltrials.gov/ct2/show/NCT01539226 [Accessed 21 November 2021] [Google Scholar]
- 111.Nel A, van Niekerk N, Kapiga S, et al. Safety and efficacy of a dapivirine vaginal ring for HIV prevention in women. N Engl J Med 2016; 375:2133–2143. [DOI] [PubMed] [Google Scholar]
- 112. International Partnership for Microbicides, Inc. A Multi-Center, Randomized, Double-Blind, Placebo-Controlled Phase 3 Safety and Effectiveness Trial of a Vaginal Matrix Ring Containing Dapivirine for the Prevention of HIV-1 Infection in Women. Clinical Trial Registration NCT01617096, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT01617096 [Accessed 21 November 2021] [Google Scholar]
- 113.Baeten JM, Palanee-Phillips T, Brown ER, et al. Use of a vaginal ring containing dapivirine for HIV-1 prevention in women. N Engl J Med 2016; 375:2121–2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. International Partnership for Microbicides, Inc. A Follow-On, Open-Label Trial To Assess Continued Safety Of And Adherence To The Dapivirine (25 Mg) Vaginal Ring-004 In Healthy, HIV-Negative Women. Clinical Trial Registration NCT02862171, clinicaltrials.gov, 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT02862171 [Accessed 21 November 2021] [Google Scholar]
- 115.Nel A, Niekerk N van, Baelen BV, et al. Safety, adherence, and HIV-1 seroconversion among women using the dapivirine vaginal ring (DREAM): an open-label, extension study. Lancet HIV 2021; 8:e77–e86. [DOI] [PubMed] [Google Scholar]
- 116▪. International Partnership for Microbicides, Inc. A Phase 3B Open-Label Follow-on Trial to Assess the Continued Safety of and Adherence to a Vaginal Ring Containing Dapivirine in Women. Clinical Trial Registration NCT02858037, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT02858037 [Accessed 21 November 2021] [Google Scholar]; The Ring Study was the first clinical trial to assess the effectiveness of monthly dapivirine vaginal rings as long-acting PrEP among cisgender women in Sub-Saharan Africa. This trial and subsequent trials have found that the rings were safe and effective and have been recommended by the WHO in their HIV guidelines.
- 117.Baeten JM, Palanee-Phillips T, Mgodi NM, et al. Safety, uptake, and use of a dapivirine vaginal ring for HIV-1 prevention in African women (HOPE): an open-label, extension study. Lancet HIV 2021; 8:e87–e95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118▪. National Institute of Allergy and Infectious Diseases (NIAID). A Phase III Study to Evaluate Long-Acting Antiretroviral Therapy in Non-Adherent HIV-Infected Individuals. Clinical Trial Registration NCT03635788, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT03635788 [Accessed 16 November 2021] [Google Scholar]; The LATITUDE study (anticipated completion October 2023) will investigate whether LAI ART is feasible among nonadherent individuals. Although this study also requires an oral lead prior to LAI ART initiation, the inclusion of nonadherent individuals in this trial has the potential to eventually expand the current patient eligibility for LAI ART (e.g. only virally suppressed individuals).
- 119. Gilead's Investigational Lenacapavir Demonstrates Sustained Long-Acting Efficacy Through Week 26 in Data Presented at CROI. Available at: https://www.gilead.com/news-and-press/press-room/press-releases/2021/3/gileads-investigational-lenacapavir-demonstrates-sustained-long-acting-efficacy-through-week-26-in-data-presented-at-croi [Accessed 24 November 2021] [Google Scholar]
- 120. Merck Sharp & Dohme Corp. A Phase 3, Randomized, Active-Controlled, Double-Blind Clinical Study to Evaluate the Efficacy and Safety of Oral Islatravir Once-Monthly as Preexposure Prophylaxis in Cisgender Men and Transgender Women Who Have Sex with Men, and are at High Risk for HIV-1 Infection. Clinical Trial Registration NCT04652700. clinicaltrials.gov. Available at: https://clinicaltrials.gov/ct2/show/NCT04652700 [Accessed 30 November 2021] [Google Scholar]
- 121. National Institute of Allergy and Infectious Diseases (NIAID). Safety, Tolerability and Acceptability of Long-Acting Cabotegravir (CAB LA) for the Prevention of HIV Among Adolescent Males − A Sub-study of HPTN 083. Clinical Trial Registration NCT04692077, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT04692077 [Accessed 16 November 2021] [Google Scholar]
- 122. National Institute of Allergy and Infectious Diseases (NIAID). Safety, Tolerability and Acceptability of Long-Acting Cabotegravir (CAB LA) for the Prevention of HIV Among Adolescent Females − A Sub-study of HPTN 084. Clinical Trial Registration NCT04824131, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT04824131 Accessed 16 November 2021] [Google Scholar]
- 123. Merck Sharp & Dohme Corp. A Phase 2a, Double-Blind, Placebo-Controlled Study to Evaluate the Safety, Tolerability, and Pharmacokinetics of Oral MK-8591 Once-Monthly in Participants at Low- Risk for HIV-1 Infection. Clinical Trial Registration NCT04003103, clinicaltrials.gov. 2020. Available at: https://clinicaltrials.gov/ct2/show/NCT04003103 [Accessed 23 November 2021] [Google Scholar]
- 124. Merck Sharp & Dohme Corp. A Phase 2a, Double-Blind, Placebo-Controlled Study to Evaluate the Safety, Tolerability, and Pharmacokinetics of a Radiopaque Matrix MK-8591 Implant in Participants at Low-Risk for HIV-1 Infection. Clinical Trial Registration NCT05115838, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT05115838 [Accessed 21 November 2021] [Google Scholar]
- 125. National Institute of Allergy and Infectious Diseases (NIAID). Phase 1 Safety and Pharmacokinetics Study of MK-2048/Vicriviroc (MK-4176)/MK-2048A Intravaginal Rings. Clinical Trial Registration NCT02356302, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT02356302 [Accessed 22 November 2021] [Google Scholar]
- 126.Hoesley CJ, Chen BA, Anderson PL, et al. Phase 1 safety and pharmacokinetics study of MK-2048/Vicriviroc (MK-4176)/MK-2048A intravaginal rings. Clin Infect Dis 2019; 68:1136–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. National Institute of Allergy and Infectious Diseases (NIAID). Phase 1 Pharmacokinetic Trial of Two Intravaginal Rings (IVRs) Containing Different Dose Strengths of Vicriviroc (MK-4176) and MK-2048. Clinical Trial Registration NCT02419456, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT02419456 [Accessed 22 November 2021] [Google Scholar]
- 128.Liu AY, Zhang J, Anderson PL, et al. Phase 1 pharmacokinetic trial of 2 intravaginal rings containing different dose strengths of vicriviroc (MK-4176) and MK-2048. Clin Infect Dis 2019; 68:1129–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. International Partnership for Microbicides, Inc. A Phase 1, Randomized Pharmacokinetics and Safety Study of Extended Duration Dapivirine Vaginal Rings. Clinical Trial Registration NCT03234400, clinicaltrials.gov. 2019. Available at: https://clinicaltrials.gov/ct2/show/NCT03234400 [Accessed 21 November 2021] [Google Scholar]
- 130.Liu AY, Dominguez Islas C, Gundacker H, et al. Phase 1 pharmacokinetics and safety study of extended duration dapivirine vaginal rings in the United States. J Int AIDS Soc 2021; 24:e25747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131. International Partnership for Microbicides, Inc. A Randomized, Phase 1, Open-Label Study in Healthy HIV-Negative Women to Evaluate the Pharmacokinetics, Safety and Bleeding Patterns Associated With 90-Day Use of Matrix Vaginal Rings Containing 200 mg Dapivirine and 320 mg Levonorgestrel. Clinical Trial Registration NCT03467347, clinicaltrials.gov. 2019. https://clinicaltrials.gov/ct2/show/NCT03467347 [Accessed 21 November 2021] [Google Scholar]
- 132. Second early phase study of 90-day vaginal ring containing dapivirine and contraceptive shows promise as dual-purpose product for preventing both HIV and pregnancy | Microbicide Trials Network. Available at: https://mtnstopshiv.org/news/second-early-phase-study-90-day-vaginal-ring-containing-dapivirine-and-contraceptive-shows [accessed 24 November 2021] [Google Scholar]
- 133. CAPRISA 018: A randomised controlled trial to assess the safety, acceptability and pharmacokinetics of a sustained-release tenofovir alafenamide sub-dermal implant for HIV prevention in women — ERA-LEARN. Available at: https://www.era-learn.eu/network-information/networks/edctp-ii/research-innovation-action-strategic-actions-supporting-large-scale-clinical-trials/caprisa-018-a-randomised-controlled-trial-to-assess-the-safety-acceptability-and-pharmacokinetics-of-a-sustained-release-tenofovir-alafenamide-sub-dermal-implant-for-hiv-prevention-in-women [Accessed 22 November 2021] [Google Scholar]
- 134. National Institute of Allergy and Infectious Diseases (NIAID). A Randomized, Double Blind, Placebo-Controlled, Phase 1 Safety and Pharmacokinetic Study of Dapivirine Gel (0.05%) Administered Rectally to HIV-1 Seronegative Adults. Clinical Trial Registration NCT03239483, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT03239483 [Accessed 22 November 2021] [Google Scholar]
- 135.Bauermeister JA, Tingler RC, Dominguez C, et al. Acceptability of a dapivirine/placebo gel administered rectally to HIV-1 seronegative adults (MTN-026). AIDS Behav 2021; Oct 17. doi: 10.1007/s10461-021-03490-8. [Online ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Johns Hopkins University. Phase 1 Study of the Safety, Toxicity, Pharmacokinetics, Pharmacodynamics and Luminal Distribution of Single-dose DuoGel Through Rectal Administration. Clinical Trial Registration NCT03082690, clinicaltrials.gov. 2019. Available at: https://clinicaltrials.gov/ct2/show/NCT03082690 [Accessed 22 November 2021] [Google Scholar]
- 137.Al-Khouja A, Shieh E, Fuchs EJ, et al. Examining the safety, pharmacokinetics, and pharmacodynamics of a rectally administered IQP-0528 gel for HIV pre-exposure prophylaxis: a first-in-human study. AIDS Res Hum Retroviruses 2021; 37:444–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. National Institute of Allergy and Infectious Diseases (NIAID). An Open Label Randomized Phase 1 Pharmacokinetic Study of Dapivirine Gel Administered Rectally to HIV-1 Seronegative Adults. Clinical Trial Registration NCT03393468, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT03393468 [Accessed 22 November 2021] [Google Scholar]
- 139.Ho K, Islas CD, Szydlo D, et al. Comparing applicator vs. ‘as lubricant’ delivery of rectal dapivirine gel (MTN-033). J Int AIDS Soc 2021; 24:40–41. [Google Scholar]
- 140. Orion Biotechnology Polska Sp. z o.o. A Monocentric Phase I Safety, Acceptability, and Pharmacokinetic Trial of OB-002H Gel Administered Vaginally and Rectally in Open-Label and Randomised, Double- Blind, Placebo-Controlled Cohorts of HIV-1 Seronegative Adults. Clinical Trial Registration NCT04791007, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT04791007 [Accessed 21 November 2021] [Google Scholar]
- 141.McGowan IM, Tzakis N, Kosak B, et al. Evaluation of the safety, acceptability, and pharmacokinetic profile of a gel formulation of OB-002 in healthy volunteers. AIDS Res Hum Retroviruses 2021; 37:453–460. [DOI] [PubMed] [Google Scholar]
- 142. Johns Hopkins University. DREAM-01: Optimization of a Tenofovir Enema for HIV Prevention. Clinical Trial Registration NCT02750540, clinicaltrials.gov. 2019. Available at: https://clinicaltrials.gov/ct2/show/NCT02750540 [Accessed 21 November 2021] [Google Scholar]
- 143. Tenofovir Rectal Douche Provides Protective Drug Levels in MSM Colon Tissue − on-demand, behaviorally-congruent. Available at: https://www.natap.org/2018/HIVR4P/HIVR4P_26.htm [Accessed 24 November 2021] [Google Scholar]
- 144. Brand R. A Randomized, Double-Blind Phase 1 Safety and Pharmacokinetic Study of Q-Griffithsin Enema Administered Rectally to HIV-1 Seronegative Adults. Clinical Trial Registration NCT04032717, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT04032717 [Accessed 21 November 2021] [Google Scholar]
- 145. Johns Hopkins University. A Phase I, Open-label Multiple Dose Safety, Pharmacokinetic, Pharmacodynamic, and Acceptability Study of Tenofovir Rectal Douche. Clinical Trial Registration NCT04016233, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT04016233 [Accessed 22 November 2021] [Google Scholar]
- 146. University of Pennsylvania. Safety, PK/PD, Acceptability, and Desirability of a Novel HIV Prevention Douche Among Adolescent Men (DREAM). Clinical Trial Registration NCT04686279, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT04686279 [Accessed 22 November 2021] [Google Scholar]
- 147. Johns Hopkins University. A Phase 1 Open Label Study Evaluating the Distribution of a Tenofovir Douche in Combination With Tap Water Douching and Simulated Receptive Anal Intercourse (DREAM-02). Clinical Trial Registration NCT04195776, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT04195776 [Accessed 22 November 2021] [Google Scholar]
- 148. International Partnership for Microbicides, Inc. A Double-blind, Randomised, Placebo-controlled, Dose Escalation Trial to Evaluate the Safety and to Assess Local and Systemic Pharmacokinetics of DS003 Vaginal Tablets Administered to Healthy HIV-negative Women. Clinical Trial Registration NCT02877979, clinicaltrials.gov. 2017. Available at: https://clinicaltrials.gov/ct2/show/NCT02877979 [Accessed 21 November 2021] [Google Scholar]
- 149.Friend C, Steytler J, van Niekerk N, et al. P05.08 − Pharmacodynamic Activity of DS003, a Novel gp120 Blocker, When Administered to Women as a Vaginal Tablet. Presented at: HIV Research For Prevention (HIVR4P); 2018 October 21−25; Madrid, Spain. Available at: https://www.professionalabstracts.com/hivr4p2018/iPlanner/#/presentation/1300 [Accessed 24 November 2021] [Google Scholar]
- 150.Nuttall J, Ariën K, Michiels J, et al. P21.02 − Pharmacodynamic Activity of DS003, a Novel gp120 Blocker, When Administered to Women as a Vaginal Tablet. Presented at: HIV Research For Prevention (HIVR4P); 2018 Oct 21−25; Madrid, Spain. Available at: https://www.professionalabstracts.com/hivr4p2018/iPlanner/#/presentation/1452 [Accessed 24 November 2021] [Google Scholar]
- 151. National Institute of Allergy and Infectious Diseases (NIAID). A Phase 1 Open Label Safety and Pharmacokinetic Study of Rectal Administration of a Tenofovir Alafenamide/Elvitegravir Insert at Two Dose Levels. Clinical Trial Registration NCT04047420, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT04047420 [Accessed 22 November 2021] [Google Scholar]
- 152.Bunge K. A Randomized, Double Blinded Study of the Safety and Pharmacokinetics of Two Vaginal Film Formulations Containing the Integrase Inhibitor MK-2048. Clinical Trial Registration NCT04319718, clinicaltrials.gov. 2021. Available at: https://clinicaltrials.gov/ct2/show/NCT04319718 [Accessed 22 November 2021] [Google Scholar]