Abstract
Background and objectives:
Data on population-level outcomes after heart failure (HF) hospitalisation in Asia is sparse. This study aimed to estimate readmission and mortality after hospitalisation among HF patients and examine temporal variation by sex and ethnicity.
Methods:
Data for 105,399 patients who had incident HF hospitalisations from 2007 to 2016 were identified from a national discharge database and linked to death registration records. The outcomes assessed here were 30-day readmission, in-hospital, 30-day and one-year all-cause mortality.
Results:
Eighteen percent of patients (n = 16786) were readmitted within 30 days. Mortality rates were 5.3% (95% confidence interval (CI) 5.1–5.4%), 11.2% (11.0–11.4%) and 33.1% (32.9–33.4%) for in-hospital, 30-day and 1-year mortality after the index admission. Age, sex and ethnicity-adjusted 30-day readmissions increased by 2% per calendar year while in-hospital and 30-day mortality declined by 7% and 4% per year respectively. One-year mortality rates remained constant during the study period. Men were at higher risk of 30-day readmission (adjusted rate ratio (RR) 1.16, 1.13–1.20) and one-year mortality (RR 1.17, 1.15–1.19) than women. Ethnic differences in outcomes were evident. Readmission rates were equally high in Chinese and Indians relative to Malays whereas Others, which mainly comprised Indigenous groups, fared worst for in-hospital and 30-day mortality with RR 1.84 (1.64–2.07) and 1.3 (1.21–1.41) relative to Malays.
Conclusions:
Short-term survival was improving across sex and ethnic groups but prognosis at one year after incident HF hospitalisation remained poor. The steady increase in 30-day readmission rates deserves further investigation.
Keywords: outcomes, heart failure, trends, ethnicity
Introduction
Heart failure (HF) is both a debilitating and costly clinical syndrome, with an expenditure of 346 billion US$ globally [1]. Despite medical advancement in the management acute coronary syndromes, the five-year survival rates for HF is poorer than most cancers [2]. Nevertheless, cardiac remodelling and progression to HF can be modified by appropriate preventive strategies and timely effective treatments are available. Estimates on the average prognosis of HF at the population level are important for monitoring changes in healthcare delivery. On the individual patient level, knowing the absolute risks of mortality and readmission enables shared decision-making between health providers and patients when making plans for disease management [3].
As it is in high-income countries, HF is already demonstrated to be a major burden in middle-income countries and this is expected to pose an equal, if not greater financial and morbidity impact as some of these countries are still grappling with a concurrent infectious disease burden [4]. The amount of data published on the epidemiology of HF from these countries is highly disproportionate compared to developed nations. Relying on data extrapolations from high-income countries is inadequate given the differences in healthcare infrastructure, health spending and demographic composition. The Asian HF registry, which included 11 countries in the region, found that one-year mortality rate was 9.6% among registry patients [5]. However, it was also noted that patients enrolled in this registry were mainly treated in academic hospitals with echocardiography expertise and more resources, and hence not necessarily representative of overall hospitalised patients [5]. Recent data from Malaysia, a middle-income country in Southeast Asia, has shown a 39% rise in the absolute number of incident HF hospitalisations from 2007 to 2016 (Su Miin Ong, MSc, unpublished data, 2020). This highlights an urgent need to fill the existing gaps on temporal trends for clinical outcomes, specifically for Asia [4]. Accordingly, our objective was to estimate the short- and medium-term mortality and readmission outcomes after an incident hospitalisation for HF. We then described the temporal variation in these outcomes by sex and ethnicity in this ethnically diverse country.
Methods
Data sources
We used hospital discharge data from the Health Informatics Centre, Ministry of Health, Malaysia from January 1, 2007 to December 31, 2016. Briefly, the Hospital Discharge Register represents a module within a centralised database known as the Patient Management Information System (Sistem Maklumat Rawatan Pesakit). It has been in operation since 1999 with the compilation of aggregated data on inpatient admissions. Then, granular patient records for Ministry of Health (MOH) hospitals became available by gradual increase in hospital participation over the years. Based on data from the Health Informatics Centre, inpatient admissions to public (MOH) hospitals make up to about 83% of HF hospitalisations in the country between 2008 and 2016, with the rest being hospitalisations in private, university and Ministry of Defence hospitals.
We included only data for MOH hospitals to maintain uniformity as data from other hospital types were available for only a later portion of the study. Mortality outcomes were determined via linkage with the National Mortality Database from the National Registration Department and Department of Statistics by matching on the national identification number or passport number for foreign nationalities in combination with date of birth and sex [6]. Overall, death registration in Malaysia has a coverage of more than 90%; there is complete registration in West Malaysia but under-reporting remains in East Malaysia (comprising the states of Sabah and Sarawak) [6,7,8]. Deaths in hospitals were medically-certified by attending physicians or coroners. On the other hand, deaths in the community were certified by informants such as the policemen and medical assistants and these were considered non-medically certified [9,10]. For the reporting of all-cause mortality, we considered all deaths, regardless of whether they were certified by medical personnel whereas for the calculation of cause-specific deaths, only those which were medically-certified were analysed.
Study population
Patients aged 20 years and above, who were admitted to a MOH hospital for an incident HF hospitalisation were included. A discharge diagnosis of HF was defined by International Classification for Diseases version 10 (ICD-10) code I50 while a case was considered an incident hospitalisation if the patient had no admission for HF within the previous two years [11,12].
Study outcomes and definitions
The main outcomes of this study were trends on 30-day readmission, in-hospital and 30-day mortality rates and lastly, mortality at one-year. In addition, we compared the crude and adjusted differences in these trends by sex and ethnicity. Lastly, we tabulated ICD-10 coded causes of death and readmission.
Deaths from any cause up to one year from date of HF admission were reported for years 2007 to 2016 while readmission data were only available till 2015. A readmission was defined as an admission for any cause within 30 days after discharge from an index HF hospitalisation while in-hospital mortality was defined as death which occurred during the index hospital admission. Information on ICD-10 coded causes of death was available only for seven years, 2007 till 2013. To examine temporal changes in HF admission criteria, we estimated trend changes in the average number of admissions per patient within one year from the index admission.
Information on age at incident HF hospitalisation, sex and ethnicity were available within the Hospital Discharge Register. In 2016, the Malaysian population is comprised of three major ethnic groups, in which there were 68.6% Bumiputera (made up of mainly Malays and Indigenous groups), 23.4% Chinese, 7.0% Indians and 1.0% other ethnicities [13]. In the medical records, ethnicity was self-reported and categorised into four groups as follows: (i) Malay, (ii) Chinese, (iii) Indian and (iv) Others which include Peninsular Malaysia Indigenous groups, Sabah and Sarawak Indigenous groups such as Bajau, Kadazan, Murut, Melanau, Kedayan, Iban, Bidayuh as well as non-Malaysian nationalities [14]. Because we anticipate a majority of Others to come from East Malaysia (consisting of two states, Sabah and Sarawak), which is known to have lower hospital densities and healthcare staff per population, and more remote communities than West Malaysia, we sought to determine the relative percentages of ethnicities by these two geographical regions [15].
Ethical considerations
Ethics approval was obtained from the Medical Research and Ethics Committee, MOH (NMRR-19-1108-47994). A waiver of informed consent was granted as the analyses was done using observational data from routine clinical care. All data linkages between hospital discharge data and death records were conducted within the data environment of the Health Informatics Centre, MOH and only de-identified aggregated forms of the data were exported.
Statistical methods
We reported crude readmission and mortality rates stratified by age, sex and ethnicity. For trends analyses, we standardised the outcome measures to the 2016 Malaysian population. Multivariable Poisson models was used to quantify the independent effect of age, sex, ethnicity and admission year on the study outcomes. An interaction term between admission year and ethnicity was used to determine if trend changes differed between ethnicities. There was evidence of overdispersion in the data, so quasi-Poisson models were used. A linear model was used to demonstrate statistical significance in the change in number of admissions per patient with time. Only the ethnicity variable had missing data for 0.3% observations and since this was a negligible percentage, they were excluded from the regression analysis. To assess robustness to changes in the definition of incident HF hospitalisation, we compared the estimates from one-year and three-year lookback periods with the main analyses. Statistical significance was set at 0.05. We used the R statistical software version 3.6.1 for all analyses [16].
Results
Patient characteristics, mortality and readmission rates
Between 2007 and 2016, there were 105 399 incident admissions for HF. The patients had a mean age of 64.1 (standard deviation (SD) 13.3) (Table 1). Fifty-six percent were men and 61% were Malays. Almost all of the Malay (97.8%), Chinese (87.8%) and Indian (99.6%) patients lived in West Malaysia while more than three quarters of Others (78.6%) live in the states of Sabah and Sarawak in East Malaysia.
Table 1.
Patient characteristics and clinical outcomes for incident hospitalisations for heart failure.
|
| ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| YEAR | 2007–2008 | 2009–2010 | 2011–2012 | 2013–2014 | 2015–2016 | |||||||
|
|
|
|
|
|
||||||||
| n | % | n | % | n | % | n | % | n | % | |||
|
| ||||||||||||
| Age | ||||||||||||
|
| ||||||||||||
| Mean (SD) | 64.6 | 13.1 | 64.3 | 13.1 | 64.0 | 13.3 | 63.9 | 13.4 | 63.7 | 13.4 | ||
|
| ||||||||||||
| Age group | ||||||||||||
|
| ||||||||||||
| 20–<25 | 99 | 0.5 | 113 | 0.5 | 92 | 0.5 | 108 | 0.5 | 118 | 0.5 | ||
|
| ||||||||||||
| 25–<30 | 147 | 0.8 | 171 | 0.8 | 184 | 0.9 | 186 | 0.9 | 214 | 0.9 | ||
|
| ||||||||||||
| 30–<35 | 219 | 1.2 | 266 | 1.3 | 235 | 1.2 | 299 | 1.4 | 367 | 1.5 | ||
|
| ||||||||||||
| 35–<40 | 328 | 1.7 | 358 | 1.7 | 384 | 2.0 | 428 | 2.0 | 603 | 2.4 | ||
|
| ||||||||||||
| 40–<45 | 575 | 3.0 | 707 | 3.4 | 641 | 3.3 | 740 | 3.5 | 920 | 3.7 | ||
|
| ||||||||||||
| 45–<50 | 1123 | 5.9 | 1252 | 5.9 | 1211 | 6.2 | 1244 | 5.9 | 1530 | 6.2 | ||
|
| ||||||||||||
| 50–<55 | 1815 | 9.6 | 1948 | 9.2 | 1898 | 9.7 | 1956 | 9.3 | 2264 | 9.1 | ||
|
| ||||||||||||
| 55–<60 | 2228 | 11.8 | 2599 | 12.3 | 2516 | 12.9 | 2762 | 13.1 | 3177 | 12.8 | ||
|
| ||||||||||||
| 60–<65 | 2603 | 13.7 | 3036 | 14.4 | 2803 | 14.4 | 3190 | 15.2 | 3744 | 15.1 | ||
|
| ||||||||||||
| 65–<70 | 2733 | 14.4 | 2931 | 13.9 | 2666 | 13.7 | 2925 | 13.9 | 3657 | 14.7 | ||
|
| ||||||||||||
| 70–<75 | 2869 | 15.2 | 3184 | 15.1 | 2654 | 13.6 | 2615 | 12.4 | 3046 | 12.3 | ||
|
| ||||||||||||
| 75–<80 | 2106 | 11.1 | 2211 | 10.5 | 2144 | 11.0 | 2391 | 11.4 | 2612 | 10.5 | ||
|
| ||||||||||||
| 80–<85 | 1284 | 6.8 | 1420 | 6.7 | 1276 | 6.5 | 1332 | 6.3 | 1628 | 6.6 | ||
|
| ||||||||||||
| 85+ | 803 | 4.2 | 868 | 4.1 | 799 | 4.1 | 879 | 4.2 | 965 | 3.9 | ||
|
| ||||||||||||
| Sex | ||||||||||||
|
| ||||||||||||
| Male | 10459 | 55.2 | 11743 | 55.7 | 10808 | 55.4 | 11774 | 55.9 | 14082 | 56.7 | ||
|
| ||||||||||||
| Female | 8473 | 44.8 | 9321 | 44.3 | 8695 | 44.6 | 9281 | 44.1 | 10763 | 43.3 | ||
|
| ||||||||||||
| Geographical region | ||||||||||||
|
| ||||||||||||
| West Malaysia | 16615 | 87.8 | 18891 | 89.7 | 17459 | 89.5 | 18541 | 88.1 | 21989 | 88.5 | ||
|
| ||||||||||||
| East Malaysia | 2317 | 12.2 | 2173 | 10.3 | 2044 | 10.5 | 2514 | 11.9 | 2856 | 11.5 | ||
|
| ||||||||||||
| Ethnicity | ||||||||||||
|
| ||||||||||||
| Malay | 11233 | 59.3 | 12732 | 60.4 | 12102 | 62.1 | 12837 | 61.0 | 15242 | 61.3 | ||
|
| ||||||||||||
| Chinese | 3522 | 18.6 | 3968 | 18.8 | 3471 | 17.8 | 3764 | 17.9 | 4433 | 17.8 | ||
|
| ||||||||||||
| Indian | 2182 | 11.5 | 2355 | 11.2 | 2123 | 10.9 | 2284 | 10.8 | 2585 | 10.4 | ||
|
| ||||||||||||
| Others | 1922 | 10.2 | 1793 | 8.5 | 1798 | 9.2 | 2156 | 10.2 | 2585 | 10.4 | ||
|
| ||||||||||||
| Missing | 73 | 0.4 | 216 | 1.0 | 9 | 0.05 | 14 | 0.1 | 0 | 0 | ||
|
| ||||||||||||
| Length of Stay | ||||||||||||
|
| ||||||||||||
| Median (IQR) | 3 | 2–5 | 3 | 2–5 | 3 | 2–5 | 3 | 2–5 | 3 | 2–5 | ||
|
| ||||||||||||
| Mean (SD) | 4.7 | 12.2 | 4.5 | 14.4 | 4.3 | 7.0 | 4.2 | 7.0 | 4.1 | 5.0 | ||
|
| ||||||||||||
| Number of admissions per year | ||||||||||||
|
| ||||||||||||
| Median (IQR) | 1 | 0–2 | 1 | 0–2 | 1 | 0–2 | 1 | 0–2 | 1 | 0–2 | ||
|
| ||||||||||||
| Mean (SD) | 1.3 | 2.2 | 1.4 | 2.3 | 1.3 | 2.1 | 1.5 | 2.3 | 1.6 | 2.5 | ||
|
| ||||||||||||
| Mortality rate | ||||||||||||
|
| ||||||||||||
| In-hospital | 1309 | 6.9 | 1297 | 6.2 | 1177 | 6.0 | 859 | 4.1 | 918 | 3.7 | ||
|
| ||||||||||||
| 30-days | 2482 | 13.1 | 2526 | 12.0 | 2285 | 11.7 | 2076 | 9.9 | 2406 | 9.7 | ||
|
| ||||||||||||
| 1-year | 6531 | 34.5 | 6945 | 33.0 | 6299 | 32.3 | 6965 | 33.1 | 8163 | 32.9 | ||
|
| ||||||||||||
| Readmission rate | ||||||||||||
|
| ||||||||||||
| 30-days | 3144 | 16.6 | 3795 | 18.0 | 3387 | 17.4 | 4039 | 19.2 | 2421 | 19.6† | ||
|
| ||||||||||||
| Total | 18932 | 21064 | 19503 | 21055 | 24845 | |||||||
|
| ||||||||||||
† Data only available for 2015 and its denominator is 12373.
A total of 16 786 (18.1%; 95% confidence interval (CI) 17.8–18.3%) patients had a readmission within 30 days of discharge. Mortality rates of hospitalised patients were 5.3% (95% CI 5.1–5.4%) during inpatient stay, 11.2% (95% CI 11.0–11.4%) within 30 days and 33.1% (95% CI 32.9–33.4%) within a year. The median length of hospital stay (LOS) was three days (interquartile range (IQR) 2–5). No association was found between LOS and in-hospital mortality. (Incidence rate ratio = 1.00, p-value = 0.529, adjusted for age, sex, ethnicity and time trend) Absolute risks for readmission and mortality by age, sex and ethnicity are displayed in Supplementary Table 1.
Thirty-day readmission rates were higher in men (19.4%) than women (16.4%). Although there were no apparent differences for inpatient mortality by sex (adjusted p = 0.340), mortality rates at 30 days and at one year were greater in men than women (11.4% vs 10.9% and 34.7% vs 31.2%, both adjusted p < 0.001) (Table 2). Age at index hospitalisation was a significant determinant of both short- and medium-term (one year) mortality. Patients who were on the extreme ends of the age spectrum, i.e., those aged 20–<25 years and 85 years and older had 2.4- and 1.8-fold increased risk of in-hospital death compared to those who were between 60 and 65 years. For patients who survived past 30 days, the risk of mortality within a year increased gradually from the 30–<35 years age band (adjusted risk ratio 0.85, 95% CI 0.77–0.94) to the oldest age band of 85 years and above (adjusted risk ratio 1.58, 95%CI 1.49–1.67) compared to the reference age category (60–<65 years).
Table 2.
Multivariable Poisson regression analysis for readmission and mortality rates during hospital stay, 30 days and 1 year.
|
| ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| READMISSION | MORTALITY | |||||||||||
|
|
|
|||||||||||
| 30-DAY | IN-HOSPITAL | 30-DAY | 1-YEAR | |||||||||
|
|
|
|
|
|||||||||
| RATE RATIO (95% CI) | p-VALUE | RATE RATIO (95% CI) | p-VALUE | RATE RATIO (95% CI) | p-VALUE | RATE RATIO (95% CI) | p-VALUE | |||||
|
| ||||||||||||
| Time | 1.02 | (1.01–1.03) | *** | 0.93 | (0.92–0.94) | *** | 0.96 | (0.96–0.97) | *** | 1.00 | (0.99–1.00) | |
|
| ||||||||||||
| Sex (ref = Women) | ||||||||||||
|
| ||||||||||||
| Men | 1.16 | (1.13–1.20) | *** | 1.02 | (0.97–1.08) | 1.11 | (1.07–1.15) | *** | 1.17 | (1.15–1.19) | *** | |
|
| ||||||||||||
| Ethnicity (ref = Malay) | ||||||||||||
|
| ||||||||||||
| Chinese | 1.12 | (1.08–1.16) | *** | 1.21 | (1.12–1.30) | ** | 1.08 | (1.03–1.13) | ** | 0.95 | (0.93–0.98) | *** |
|
| ||||||||||||
| Indian | 1.12 | (1.07–1.17) | ** | 0.82 | (0.74–0.91) | ** | 0.80 | (0.75–0.85) | *** | 0.87 | (0.84–0.90) | *** |
|
| ||||||||||||
| Others | 0.81 | (0.77–0.86) | *** | 1.91 | (1.77–2.07) | *** | 1.30 | (1.23–1.37) | *** | 0.96 | (0.93–0.99) | * |
|
| ||||||||||||
| Age (ref = 60–<65) | ||||||||||||
|
| ||||||||||||
| 20–<25 | 1.14 | (0.94–1.37) | 2.49 | (1.88–3.22) | *** | 1.73 | (1.40–2.11) | *** | 0.98 | (0.85–1.12) | ||
|
| ||||||||||||
| 25–<30 | 1.01 | (0.86–1.17) | 2.62 | (2.12–3.21) | *** | 1.75 | (1.48–2.04) | *** | 0.99 | (0.89–1.10) | ||
|
| ||||||||||||
| 30–<35 | 0.83 | (0.72–0.95) | ** | 2 | (1.64–2.43) | *** | 1.39 | (1.20–1.60) | *** | 0.86 | (0.78–0.94) | ** |
|
| ||||||||||||
| 35–<40 | 0.98 | (0.88–1.08) | 1.25 | (1.01–1.53) | * | 1.09 | (0.95–1.25) | 0.83 | (0.76–0.89) | *** | ||
|
| ||||||||||||
| 40–<45 | 0.95 | (0.87–1.03) | 1.15 | (0.96–1.36) | 0.98 | (0.88–1.10) | 0.83 | (0.78–0.88) | *** | |||
|
| ||||||||||||
| 45–<50 | 0.94 | (0.88–1.01) | 0.88 | (0.75–1.02) | 0.84 | (0.76–0.93) | ** | 0.82 | (0.78–0.86) | *** | ||
|
| ||||||||||||
| 50–<55 | 0.99 | (0.93–1.05) | 0.85 | (0.74–0.96) | * | 0.82 | (0.75–0.89) | *** | 0.87 | (0.83–0.91) | *** | |
|
| ||||||||||||
| 55–<60 | 0.98 | (0.93–1.03) | 0.93 | (0.83–1.05) | 0.90 | (0.83–0.97) | ** | 0.93 | (0.89–0.96) | *** | ||
|
| ||||||||||||
| 65–<70 | 0.97 | (0.92–1.02) | 1.07 | (0.96–1.20) | 1.08 | (1.01–1.16) | * | 1.05 | (1.02–1.09) | ** | ||
|
| ||||||||||||
| 70–<75 | 0.91 | (0.87–0.96) | ** | 1.14 | (1.02–1.27) | * | 1.23 | (1.15–1.31) | *** | 1.15 | (1.11–1.20) | *** |
|
| ||||||||||||
| 75–<80 | 0.86 | (0.81–0.91) | *** | 1.26 | (1.12–1.41) | *** | 1.34 | (1.25–1.44) | *** | 1.24 | (1.19–1.29) | *** |
|
| ||||||||||||
| 80–<85 | 0.84 | (0.79–0.90) | *** | 1.53 | (1.36–1.73) | *** | 1.59 | (1.47–1.71) | *** | 1.37 | (1.31–1.43) | *** |
|
| ||||||||||||
| 85+ | 0.75 | (0.69–0.81) | *** | 1.84 | (1.61–2.10) | *** | 1.94 | (1.79–2.11) | *** | 1.59 | (1.51–1.66) | *** |
|
| ||||||||||||
| Intercept | 0.16 | (0.15–0.17) | *** | 0.06 | (0.06–0.07) | *** | 0.11 | (0.10–0.12) | *** | 0.3 | (0.29–0.31) | *** |
|
| ||||||||||||
* p < 0.05, ** p < 0.01, *** p < 0.001.
By ethnicity, 30-day readmission rates were highest in Indians (19.9%), followed by Chinese (19.5%), Malay (17.9%) and Others (14.5%). For short-term mortality, Others presented with the poorest outcomes: 9.4% for in-hospital mortality and 14.4% for 30-day mortality compared to 4.6% and 10.7% in Malays, the largest ethnic group in Malaysia. This translates to a 1.9-and 1.3-fold increase in risk for mortality relative to Malays when adjusted for age, sex and calendar year. Indian patients, on the other hand, had lower inpatient (3.8%), 30-day (8.4%) and one-year (28.6%) mortality rate than Malays. All ethnic differences in outcome measures remained when estimates were adjusted for age, sex and calendar year.
Trends for readmission and mortality
A 17.8% increase in overall readmissions from 16.6% in 2007–2008 to 19.6% in 2015 was observed and this trend remained significant at +2% per calendar year after adjusting for age, sex and ethnicity (p trend < 0.001). Figure 1(a) shows that age-standardised trends for 30-day readmission in men were proportionally higher than the rate for women. Although Others had the lowest readmission rates in 2007, its rise with time was the largest compared to the other ethnic groups (Figure 2 (a)). The mean number of hospitalisations per patient within a year has risen slightly from 1.3 in 2007 to 1.6 in 2015 and a modest increase of 0.04 per calendar year was still evident after accounting for age, sex and ethnicity (p trend < 0.001).
Figure 1.
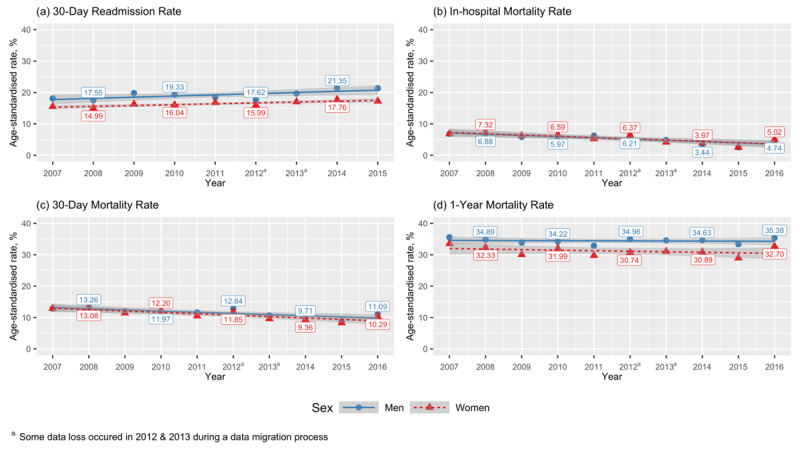
Trends for (a) 30-day readmission, (b) in-hospital, (c) 30-day and (d) one-year all-cause mortality rates by men and women.
Figure 2.
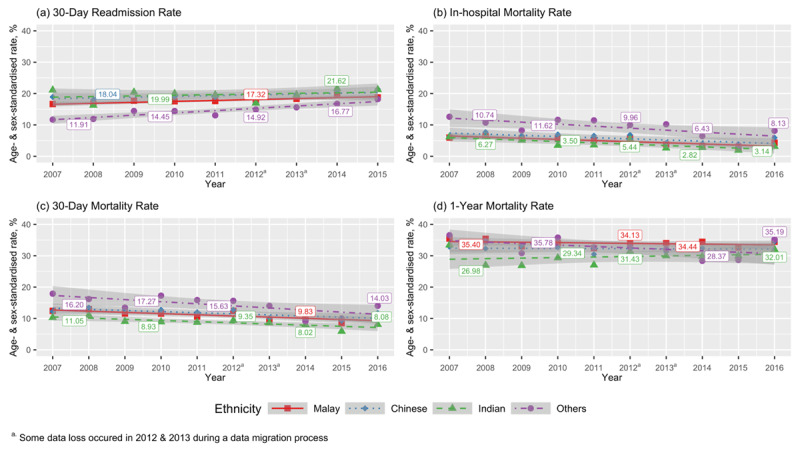
Trends for (a) 30-day readmission, (b) in-hospital, (c) 30-day and (d) one-year all-cause mortality rates by ethnicity.
Overall, in-hospital mortality rates nearly halved from 6.9% (95% CI 6.6–7.3) in 2007 to 3.7% (95% CI 3.5–3.9) in 2016 with similar trends for men and women (Figure 1(b)). This declining trend remained after adjustment for age, sex and ethnicity (average –7% per year; p trend < 0.001). Improvements in mortality were also evident within 30 days of hospitalisation, seen as a 26% decline from 13.1% (95% CI 12.6–13.6%) in 2007 to 9.7% (95% CI 9.3–10.1%) in 2016. Men had consistently higher 30-day mortality rates than women during the study period (Figure 1(c)). Upon full-model adjustment, the average improvement in 30-day mortality was 4% per calendar year (p trend < 0.001). By contrast, all-cause mortality in one year remained unchanged throughout the study period (p trend = 0.113) with men having almost uniformly higher rates than women (Figure 1(d)).
Despite poorer overall outcomes, Others showed the most pronounced improvements in short-term mortality over time compared to other groups (Figure 2(b) and (c)). The rates for 30-day mortality between Others and Malays narrowed from 6.2% in 2007 to 3.5% in absolute rate difference in 2016 but this difference was not significant after full model adjustment (p interaction = 0.091; Supplementary Table 2). With respect to 1-year mortality, only Others showed significant average decline by 1% per year (p interaction = 0.021) relative to Malays (Figure 2(d), Supplementary Table2).
Cause of readmission and death
Cardiovascular causes accounted for half of all 30-day readmissions (50.1%) (Figure 3) with HF specifically accounting for 27.8%. Analysis on all medically-certified deaths found 56% of patients died of cardiovascular causes within a year from index hospitalisation, with the leading cause being HF (21.1%) (Figure 4). Cardiovascular mortality rates have been decreasing by two percent per calendar year, with adjusted p trend = 0.001 (Supplementary table 3). Despite this decline, a corresponding increase in non-cardiovascular mortality with time resulted in the unchanged overall rates for one-year mortality and a look into the specific causes between two calendar year periods for 2007–2008 and 2012–2013 showed that the contribution of infections as a cause of non-cardiovascular deaths has been increasing (Supplementary Table 4).
Figure 3.
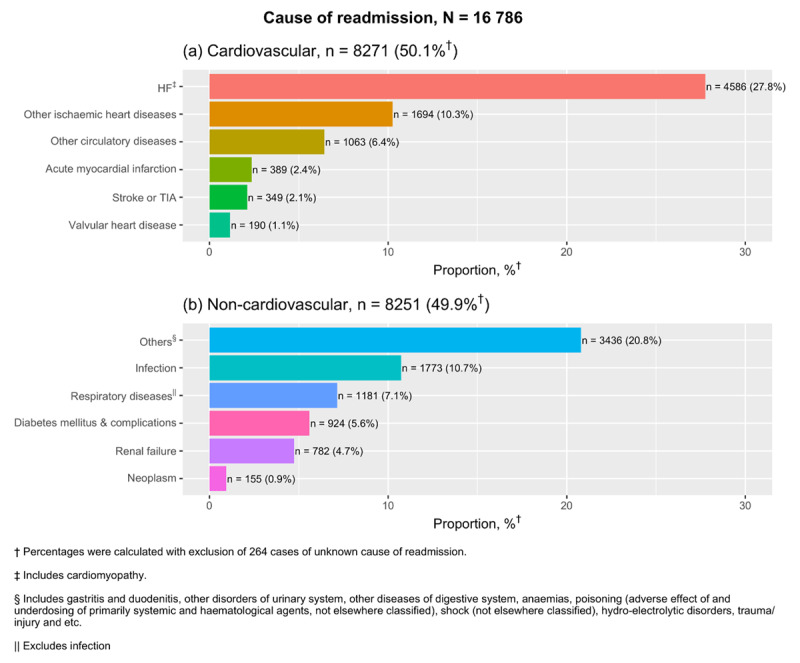
Causes of readmission in 30 days after index hospital admission from 2007–2015.
Figure 4.
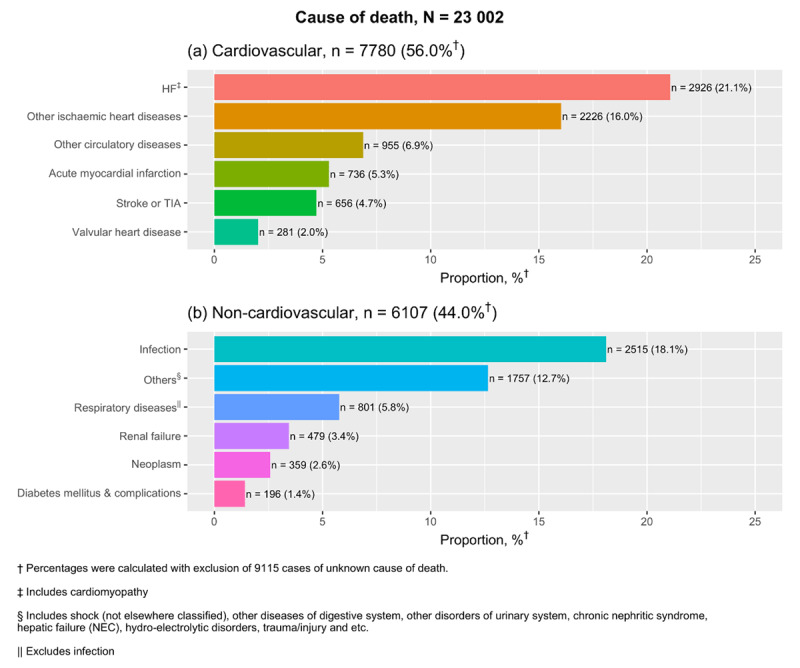
Causes of death for patients who died within one year after index admission from 2007–2013.
When the definition of incident HF hospitalisation was increased from a two-year to three -year lookback period, the percentage of reduction in false positives were between 1.7 to 3% annually. Nevertheless, the magnitude of outcome rates, trends and statistical significance of regression estimates were similar to the main results, for both the one-year and three-year definitions of incident hospitalisations (Supplementary Tables 5 and 6).
Discussion
We present here contemporary crude and age-standardised estimates for mortality and readmission rates among hospitalised HF patients in a middle-income Asian country. Using linked population data, this study has revealed improving trends in short-term mortality following an incident hospitalisation for HF in Malaysia. However, mortality at one year has remained constant while readmissions within thirty days rose steadily during the observation period. We have noted distinct differences in patient outcomes by sex and ethnicity. First, readmission rates were consistently higher in men compared to women and in Chinese and Indians compared to Malay patients. Second, overall short-term mortality outcomes were poorest in Others compared to all other ethnicities while men had slightly worse outcomes than women for 30-day mortality. Third, improvements in survival after HF hospitalisation varied by ethnic groups with Others showing the steepest decline in one-year mortality.
In-hospital mortality after incident HF hospitalisation in Malaysia was higher compared to the 4.1% reported from a HF registry in China [17]. Nevertheless, it is necessary to take into consideration that being enrolled in a registry is associated with better outcomes [18]. Next, we observed a seven percent decline for in-hospital mortality for both men and women. This is in contrast to a rise in Brazil, from 8.3% to 10.8% between 2008 and 2017 [19]. Similar to inpatient mortality, the rates of mortality within 30 days was also decreasing, albeit to a smaller extent. No direct comparisons were available for middle-income countries. However, the decline observed here were consistent to those observed in several high-income settings including Western Australia, the Netherlands, and Sweden [20,21,22,23]. Several explanations are possible. The observed decline in short-term mortality is partly a reflection of improving population health, as seen with life expectancy increases from 73.7 years in 2008 to 75 years in 2018 [24]. Other explanations include earlier identification of cases as a result of rising population health awareness, improved pre-hospital emergency services and an increase in the number of medical specialists in the past two decades [25,26]. MOH hospitals have experienced almost doubling of the number of emergency medicine specialists from 93 to 167 from 2010 to 2013 and a modest increase in the number of cardiologists from 47 to 53 within the same period [27]. There are no known changes in reimbursement practices or implementation of nationwide quality improvement programs during the study period, therefore we expect the coding of ICD-10 to remain consistent over this duration.
In keeping with earlier and recent studies from Western populations [28,29,30], we have also showed that men had higher risks of mortality and readmission than women after accounting for age, ethnicity and time trends. Poorer survival and higher readmission rates in men after HF hospitalisation may be explained by a predominant heart failure with reduced ejection fraction subtype among men and higher prevalence of macrovascular disease, myocardial ischemia and infarction, which underlie the aetiology of HF in this subgroup [31]. Unfortunately, the type of HF and aetiology were not available in the present data.
Amidst the overall improvements in short-term mortality, it is necessary to note that striking ethnic differences exists. Others had poorer outcomes than the rest of the population. This difference was apparent even in the presence of under-reporting of deaths in East Malaysia, from which the majority of Others reside. Hence, we expect the true estimates to be even higher than what was observed. The health status of this subgroup is known to be poorer compared to the general population and is characterised by lower socioeconomic status, shorter life expectancy, undernutrition, insulin resistance and lack of trust in modern medicine [32]. Moreover, accessibility to hospitals remains a challenge for some residents of the interior and remote parts of Sabah and Sarawak and it is also likely that this region has a higher prevalence of rheumatic heart disease which may contribute to poorer outcomes among those hospitalised for HF [33,34,35]. These findings highlight a need to improve access to healthcare and focus resources to narrow the disparities in short-term mortality particularly in Others. For short-term mortality trends, it is reassuring to observe that the largest disparity in mortality outcomes between Others and Malays have been narrowing. The remaining differences in mortality outcomes between ethnicity represents opportunities for health interventions.
About one in three patients hospitalised for HF in this study die within a year and this has remained fairly constant during the study period. Mortality at one year is almost 1.5-fold compared to the European Society of Cardiology Long Term Heart Failure registry, reflecting differences in income per capita, health systems and patient characteristics between Malaysia and the European and Mediterranean countries which participated in this registry [36]. Trend-wise, death due to cardiovascular disease has decreased and this could be the result of a higher use of disease-modifying therapy such as renin-aldosterone angiotensin system inhibitors and beta-blockers in recent years, as reported in several tertiary centres [37,38,39,40]. Numerous reports have shown that people of South Asian descent are predisposed to higher risk of ischaemic heart disease compared to the rest of the population [41]. Accordingly, our previous study had also found the highest incidence of HF hospitalisations amongst Indians in the Malaysian population. Interestingly though, when it comes to survival, be it short-term or at one-year, Indians had significantly better survival compared to other ethnic groups. This suggests a stronger influence of environmental and behavioural determinants over genetic influences in HF outcomes. Further investigation into use of HF medications and lifestyle factors by ethnic subgroups would hence be warranted.
Preventing decompensation is an important therapeutic goal after a diagnosis of HF. To our knowledge, there is no published data on 30-day readmission trends after HF hospitalisation among middle-income countries. The steady annual rise in 30-day readmissions that we have found were comparable to those reported in Spain, but in contrast to a two percent reduction among Veteran’s Affairs hospital admissions in the United States [42,43]. It is necessary though, to keep in mind that differences in healthcare financing and infrastructure exist between countries of middle- and high-income economies. Lowering admission threshold for HF is a potential reason for this observed rise in readmission rates in this study. Differential readmission rates by ethnicity were likely related to socioeconomic status and educational level. This is reflected as higher readmission rates among the Chinese and Indians who largely reside in urban locations, whereas greater access and logistical barriers to care exists among Others [44]. However, narrowing of the gap in readmission rates between Others and the population average suggests that physical access for Others to secondary care is improving over the last decade. The overall increasing trend in 30-day readmissions observed here deserve attention from researchers and policy makers alike because hospitalisations incur the greatest financial costs to HF health expenditures and about a quarter of these readmissions are preventable [45]. Standardised strategies to differentiate the severity of patients who present at the emergency department would be useful for risk stratifying them into those who require admission while the rest may be observed and treated on an outpatient basis. We know that half of these readmissions are due to non-cardiovascular causes; therefore, multi-faceted assessments which address all comorbidities can be incorporated into early care transition to outpatient clinics, nurse-led home visits and structured telephone monitoring, all of which have shown moderate effectiveness in reducing rehospitalisations [46,47].
In this study, we estimated the average prognosis after an index hospitalisation for HF using representative data from a large national database. These findings are generalisable to other middle-income countries with similar government-funded health systems and diverse ethnic composition. While most HF hospitalisation data for middle income countries in literature come from urban tertiary centres [4], we have presented here data across a range of hospitals within the public health sector in Malaysia. Unlike patient selection in disease registries, the inclusion of unselected cases of HF hospitalisations here allowed us to make reliable comparisons between sex and ethnic groups.
There were several limitations in this study. Complete data were available for only primary discharge diagnoses; therefore, the absolute number of HF hospitalisations was likely underestimated. Nevertheless, the trend data is unlikely to be affected by this underestimation as the selection criteria used was uniform across time points. We explored the use of secondary discharge diagnoses as proxy for underlying disease severity but found that data completeness was not consistent across time. Therefore, it is difficult to draw conclusions on the severity of patients who were hospitalised for HF. Information on HF subtypes (reduced, preserved and mid-range ejection fraction), medical history, treatments and device therapy were not available in the discharge database and thus, does not allow for correlation of these factors with HF outcomes. While this analysis encompassed an average of 83% of annual HF hospitalisations in Malaysia, it is necessary to point out that we have included only HF patients who were hospitalised in MoH hospitals. Thus, these results are not generalisable to patients treated in the community setting or private hospitals. The 30-day and one-year mortality estimates were slightly underestimated due to incomplete death registration in East Malaysia. Lastly, there were some data losses in 2012 and 2013 and imputations were not feasible in this situation because the exact number of missing records was not known.
To the best of our knowledge, this is one of the first studies to report national, age-standardised estimates for HF prognosis and trends for hospitalised HF patients in the South East Asian region. The declining trend and narrowing of ethnic differences for short-term mortality showed that these outcomes are amenable to targeted interventions. Moreover, the differential HF outcomes by sex and ethnicity seen here highlights the importance of incorporating these determinants into risk predictions models or when calculating likely accrual endpoints in the design of therapeutic studies.
Conclusion
Gradual improvements in short-term mortality were seen across sex and ethnicities although relative differences between ethnic subgroups remain apparent. The steady rise in 30-day readmission post-discharge and stagnating 1-year mortality rate raises concern, signalling a need for pro-active efforts from policymakers, physicians and research in making HF as a priority disease area.
Additional File
The additional file for this article can be found as follows:
Rounds Evaluation Rubric in French and English.
Acknowledgements
We thank the Director-General of Health for his support in the publication of these findings. We are grateful to the Health Informatics Centre, National Registration Department and Department of Statistics Malaysia for providing the data used in this study.
Funding Statement
The study was funded by a research grant from the Ministry of Health Malaysia (NMRR-19-1108-47994). YMFL is supported by the University Medical Center Utrecht Global Health Support Program and the BigData@Heart project (under Innovative Medicines Initiative 2 Joint Undertaking grant agreement number 116074) and FWA is supported by the UCL Hospital NIHR Biomedical Research Centre.
Abbreviations
| HF | Heart failure |
| ICD | International Classification for Diseases |
| MOH | Ministry of Health |
Funding Information
The study was funded by a research grant from the Ministry of Health Malaysia (NMRR-19-1108-47994). YMFL is supported by the University Medical Center Utrecht Global Health Support Program and the BigData@Heart project (under Innovative Medicines Initiative 2 Joint Undertaking grant agreement number 116074) and FWA is supported by the UCL Hospital NIHR Biomedical Research Centre.
Competing Interests
The authors have no competing interests to declare.
Author Contributions
YMFL, SMO, WYH, IV, HBL and SS conceptualized the study. SMO conducted the data analysis and YMFL wrote the first draft. All authors contributed to results interpretation. SMO, WYH, SK, HBL, JR, FWA, DEG, IV and SS critically reviewed drafts of the manuscript. All authors read and approved the final manuscript.
References
- 1.Lippi G, Sanchis-Gomar F. Global epidemiology and future trends of heart failure. AME Medical Journal. 2020; 5. DOI: 10.21037/amj.2020.03.03 [DOI] [Google Scholar]
- 2.Braunwald E. The war against heart failure: the Lancet lecture. The Lancet. 2015; 385: 812–824. DOI: 10.1016/S0140-6736(14)61889-4 [DOI] [PubMed] [Google Scholar]
- 3.Hemingway H, Croft P, Perel P, et al. Prognosis research strategy (PROGRESS) 1: A framework for researching clinical outcomes. BMJ. 2013; 346. DOI: 10.1136/bmj.e5595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Callender T, Woodward M, Roth G, et al. Heart failure care in low- and middle-income countries: A systematic review and meta-analysis. PLoS Med. 2014; 11: e1001699. DOI: 10.1371/journal.pmed.1001699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MacDonald MR, Tay WT, Teng T-HK, et al. Regional Variation of Mortality in Heart Failure With Reduced and Preserved Ejection Fraction Across Asia: Outcomes in the ASIAN-HF Registry. Journal of the American Heart Association. 2020; 9: e012199. DOI: 10.1161/JAHA.119.012199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shamsuddin K, Lieberman E. Linking death reports from the Malaysian Family Life Survey-2 with birth and death certificates. Med J Malaysia. 1998; 53: 343–353. [PubMed] [Google Scholar]
- 7.United Nations. Levels and trends of mortality since 1950. New York: United Nations; 1982. [Google Scholar]
- 8.Rao C, Omar MA, Ganapathy SS, Tamin NSI. Strengthening Mortality Statistics for Health Programs in Malaysia: Lessons from the Field. Dr Sulaiman Al Habib Medical Journal. 2019; 1: 52–54. DOI: 10.2991/dsahmj.k.191214.003 [DOI] [Google Scholar]
- 9.Omar A, Ganapathy SS, Anuar MFM, et al. Cause-specific mortality estimates for Malaysia in 2013: Results from a national sample verification study using medical record review and verbal autopsy. BMC Public Health. 2019; 19: 110. DOI: 10.1186/s12889-018-6384-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adnan TH, Bujang MA, Supramaniam P, et al. Trend Analysis of Medically Certified Death in Malaysia, 1995–2010. Health Informatics Journal. 2012; 6. [Google Scholar]
- 11.Camplain R, Kucharska-Newton A, Cuthbertson CC, Wright JD, Alonso A, Heiss G. Misclassification of incident hospitalized and outpatient heart failure in administrative claims data: the Atherosclerosis Risk in Communities (ARIC) study. Pharmacoepidemiol Drug Saf. 2017; 26: 421–428. DOI: 10.1002/pds.4162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Griffiths RI, O’Malley CD, Herbert RJ, Danese MD. Misclassification of incident conditions using claims data: Impact of varying the period used to exclude pre-existing disease. BMC Med Res Methodol. 2013; 13: 32. DOI: 10.1186/1471-2288-13-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Department of Statistics Malaysia. Current Population Estimates, Malaysia, 2014–2016. Putrajaya, Malaysia: Department of Statistics Malaysia; 2016. [Google Scholar]
- 14.Ministry of Health Malaysia. National Health Data Dictionary, Health Informatics Standards. 2nd Edition. Kuala Lumpur: Ministry of Health Malaysia; 2007. [Google Scholar]
- 15.Ministry of Health Malaysia, Harvard University TH Chan School of Public Health. Malaysia Health Systems Research: Contextual analysis of the Malaysian health system. Vol. 1. Putrajaya: Ministry of Health Malaysia; 2016. [Google Scholar]
- 16.R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical. Computing; 2019. [Google Scholar]
- 17.Zhang Y, Zhang J, Butler J, et al. Contemporary Epidemiology, Management, and Outcomes of Patients Hospitalized for Heart Failure in China: Results From the China Heart Failure (China-HF) Registry. J Card Fail. 2017; 23: 868–875. DOI: 10.1016/j.cardfail.2017.09.014 [DOI] [PubMed] [Google Scholar]
- 18.Lund LH, Carrero J-J, Farahmand B, et al. Association between enrolment in a heart failure quality registry and subsequent mortality-a nationwide cohort study. Eur J Heart Fail. 2017; 19: 1107–1116. DOI: 10.1002/ejhf.762 [DOI] [PubMed] [Google Scholar]
- 19.Fernandes ADF, Fernandes GC, Mazza MR, et al. A 10-year trend analysis of heart failure in the less developed brazil. Arquivos brasileiros de cardiologia. 2020; 114: 222–231. DOI: 10.36660/abc.20180321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Teng T-H K, Finn J, Hobbs M, Hung J. Heart failure: Incidence, case fatality, and hospitalization rates in Western Australia between 1990 and 2005. Circ Heart Fail. 2010; 3: 236–243. DOI: 10.1161/CIRCHEARTFAILURE.109.879239 [DOI] [PubMed] [Google Scholar]
- 21.Mosterd A, Reitsma JB, Grobbee DE. Angiotensin converting enzyme inhibition and hospitalisation rates for heart failure in the Netherlands, 1980 to 1999: the end of an epidemic? Heart. 2002; 87: 75. DOI: 10.1136/heart.87.1.75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schaufelberger M, Swedberg K, Köster M, Rosén M, Rosengren A. Decreasing one-year mortality and hospitalization rates for heart failure in Sweden; Data from the Swedish Hospital Discharge Registry 1988 to 2000. Eur Heart J. 2004; 25: 300–307. DOI: 10.1016/j.ehj.2003.12.012 [DOI] [PubMed] [Google Scholar]
- 23.Jackson SL, Tong X, King RJ, Loustalot F, Hong Y, Ritchey MD. National Burden of Heart Failure Events in the United States, 2006 to 2014. Circ Heart Fail. 2018; 11: e004873. DOI: 10.1161/CIRCHEARTFAILURE.117.004873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Department of Statistics Malaysia. Press release: Abridged life tables, Malaysia 2016–2018. 2018. [Google Scholar]
- 25.Hisamuddin NARN, Hamzah MS, Holliman CJ. Prehospital emergency medical services in Malaysia. J Emerg Med. 2007; 32: 415–421. DOI: 10.1016/j.jemermed.2006.08.021 [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization. Regional Office for Western Pacific. Malaysia health system review. Vol. 3. Manila: WHO Regional Office for the Western Pacific; 2012. [Google Scholar]
- 27.Clinical Research Centre. National Healthcare Establishment and Workforce Statistics (Hospital) 2012–2013. Kuala Lumpur: Clinical Research Centre, Ministry of Health Malaysia; 2015. [Google Scholar]
- 28.Ho KK, Anderson KM, Kannel WB, Grossman W, Levy D. Survival after the onset of congestive heart failure in Framingham Heart Study subjects. Circulation. 1993; 88: 107–115. DOI: 10.1161/01.CIR.88.1.107 [DOI] [PubMed] [Google Scholar]
- 29.Vaartjes I, Hoes A, Reitsma J, et al. Age- and gender-specific risk of death after first hospitalization for heart failure. BMC Public Health. 2010; 10: 637. DOI: 10.1186/1471-2458-10-637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Taylor CJ, Ordóñez-Mena JM, Jones NR, et al. National trends in heart failure mortality in men and women, United Kingdom, 2000–2017. Eur J Heart Fail. 2021; 23: 3–12. DOI: 10.1002/ejhf.1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lam CSP, Arnott C, Beale AL, et al. Sex differences in heart failure. European Heart Journal. 2019; 40: 3859–3868c. DOI: 10.1093/eurheartj/ehz835 [DOI] [PubMed] [Google Scholar]
- 32.Tuan Abdul Aziz TA, Teh LK, Md Idris MH, et al. Increased risks of cardiovascular diseases and insulin resistance among the Orang Asli in Peninsular Malaysia. BMC Public Health. 2016; 16. DOI: 10.1186/s12889-016-2848-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chew KS, Chan HC. Prehospital care in Malaysia: issues and challenges. International Paramedic Practice. 2011; 1: 47–51. DOI: 10.12968/ippr.2011.1.2.47 [DOI] [Google Scholar]
- 34.Hussin N. Socio demographic profiles of rheumatic heart disease (RHD) patients in Sabah. International Journal of Public Health Research. 2016; 6: 736–740. [Google Scholar]
- 35.Hussin N. Insights from a rheumatic heart disease registry in a tertiary centre in Sabah. International Journal of Public Health Research. 2017; 7: 757–764. [Google Scholar]
- 36.Crespo-Leiro MG, Anker SD, Maggioni AP, et al. European Society of Cardiology Heart Failure Long-Term Registry (ESC-HF-LT): 1-year follow-up outcomes and differences across regions. Eur J Heart Fail. 2016; 18: 613–625. DOI: 10.1002/ejhf.566 [DOI] [PubMed] [Google Scholar]
- 37.Chin SP, Sapari S, How SH, Sim KH. Managing congestive heart failure in a general hospital in Malaysia. Are we keeping pace with evidence? Med J Malaysia. 2006; 61: 278–283. [PubMed] [Google Scholar]
- 38.Chong A-Y, Rajaratnam R, Hussein NR, Lip GYH. Heart failure in a multiethnic population in Kuala Lumpur, Malaysia. Eur J Heart Fail. 2003; 5: 569–574. DOI: 10.1016/S1388-9842(03)00013-8 [DOI] [PubMed] [Google Scholar]
- 39.Reyes EB, Ha J-W, Firdaus I, et al. Heart failure across Asia: Same healthcare burden but differences in organization of care. International Journal of Cardiology. 2016; 223: 163–167. DOI: 10.1016/j.ijcard.2016.07.256 [DOI] [PubMed] [Google Scholar]
- 40.Zainal Abidin HA, Isa MR, Mohd Arshad MK, et al. Guideline Adherence to Prescription in Heart Failure Population in North Kuala Lumpur Region. International Journal of Cardiology. 2017; 249: S38. DOI: 10.1016/j.ijcard.2017.09.135 [DOI] [Google Scholar]
- 41.Chaturvedi N. Ethnic differences in cardiovascular disease. Heart. 2003; 89: 681–686. DOI: 10.1136/heart.89.6.681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fernandez-Gasso L, Hernando-Arizaleta L, Palomar-Rodríguez JA, Abellán-Pérez MV, Pascual-Figal DA. Trends, causes and timing of 30-day readmissions after hospitalization for heart failure: 11-year population-based analysis with linked data. Int J Cardiol. 2017; 248: 246–251. DOI: 10.1016/j.ijcard.2017.07.094 [DOI] [PubMed] [Google Scholar]
- 43.Parizo JT, Kohsaka S, Sandhu AT, Patel J, Heidenreich PA. Trends in Readmission and Mortality Rates Following Heart Failure Hospitalization in the Veterans Affairs Health Care System From 2007 to 2017. JAMA Cardiol. 2020; 5: 1042–1047. DOI: 10.1001/jamacardio.2020.2028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mariapun J, Ng C-W, Hairi NN. The Gradual Shift of Overweight, Obesity, and Abdominal Obesity Towards the Poor in a Multi-ethnic Developing Country: Findings From the Malaysian National Health and Morbidity Surveys. J Epidemiol. 2018; 28: 279–286. DOI: 10.2188/jea.JE20170001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ziaeian B, Fonarow GC. The Prevention of Hospital Readmissions in Heart Failure. Progress in Cardiovascular Diseases. 2016; 58: 379–385. DOI: 10.1016/j.pcad.2015.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Feltner C, Jones CD, Cené CW, et al. Transitional care interventions to prevent readmissions for persons with heart failure: A systematic review and meta-analysis. Ann Intern Med. 2014; 160: 774–784. DOI: 10.7326/M14-0083 [DOI] [PubMed] [Google Scholar]
- 47.Chan WX, Lin W, Wong RCC. Transitional Care to Reduce Heart Failure Readmission Rates in South East Asia. Card Fail Rev. 2016; 2: 85–89. DOI: 10.15420/cfr.2016:9:2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Rounds Evaluation Rubric in French and English.


