Abstract
Objective:
To compare the effectiveness of three different motivational techniques for maintaining good oral hygiene during fixed appliance orthodontic treatment.
Materials and Methods:
A total of 62 adolescents in the age range of 12–18 years, requiring fixed orthodontic treatment were evaluated for the efficacy of three different motivational techniques, ie, conventional plaque control measures (group I), chair side motivational tests with conventional plaque control measures (group II), and phase contrast microscopy with conventional plaque control measures (group III), in improving oral hygiene and gingival health over a period of 6 months.
Results:
A gradual decline in mean plaque scores in group III was found, ie, from 1.13 ± 0.42 at baseline to 0.64 ± 0.39 at 6 months (P < .05). An intragroup analysis of mean gingivitis scores in group III showed statistically significant decline in the mean gingival scores from 1.49 ± 0.45 to 1.08 ± 0.61 over a period of 6 months(P < .05).
Conclusions:
Phase contrast microscopy along with the conventional method of plaque disclosure and demonstration of the horizontal scrubbing method of brushing have a long-lasting effect on the patient. This reduces the need of frequent reinforcement sessions of plaque control programs when compared to chair side motivational tests and conventional plaque control measures.
Keywords: Phase contrast microscope, Motivational tests, Oral hygiene, Orthodontic treatment
INTRODUCTION
Maintaining good oral hygiene is a challenging task among patients undergoing fixed appliance orthodontic treatment.1,2 The brackets and other components present a favorable situation for rapid plaque accumulation and increased acid production leading to demineralization and incipient carious lesions.3,4 These incipient lesions appear as early as 2 to 3 weeks after plaque accumulation in buccolingual areas of the teeth.5 Studies have indicated that minimal periodontal disease, bone loss, and caries will occur in adolescents during the course of fixed appliance therapy, if adequate plaque control is maintained.6,7 In the present study, three different motivational techniques (conventional plaque control measures, chair side motivational tests, and phase contrast microscopy) were evaluated for their effectiveness in bringing about improvement in gingival health and oral hygiene of young orthodontic patients undergoing fixed orthodontic treatment.
MATERIALS AND METHODS
Seventy-eight patients requiring fixed orthodontic treatment were selected using the criteria mentioned below. This study was approved by the Institutional Ethical Committee, Postgraduate Institute of Medical Education and Research, Oral Health Sciences Centre, Chandigarh, India. After obtaining informed consent, 26 patients were allocated to each of three groups, using a systematic random sampling technique. Of 78 patients, only 62 (group I - 21, group II - 23 , group III - 18) were finally available for the first recording at the baseline since (1) some of the patients did not turn up for treatment and (2) treatment planning for some of the patients was changed later. Thus, 62 patients were taken as baseline reference in the study.
Inclusion criteria were as follows:
age between 12 and 18 years,
full complement of permanent dentition, and
absence of any active periodontal disease and dental caries.
Exclusion criteria were as follows:
medically compromised patients,
patients who are mentally or physically challenged, and
patients with cleft palate where oral hygiene regimen could be compromised.
Group I
Patients were motivated through conventional plaque control measures, ie, plaque was disclosed with 2% mercurochrome. The composition of plaque, its effects on oral health, and the importance of its removal were stressed, and a horizontal scrubbing technique of brushing was demonstrated to the patients.
Group II
Patients in this group were motivated for the removal of dental plaque by using chair side motivational techniques. In this method an indicator dye, Bromocresol green, was demonstrated to change color from green to yellow on addition of a drop of 0.1N HCl acid in the depression of a color plate. This step was carried out to show the patient that the change in color of the dye is due to a drop in pH because of the addition of acid. A pooled plaque sample from the patient was then put into another depression of the color plate containing 1 drop of indicator dye which did not show any evident color change. This was followed by 10% glucose rinse for 1 minute by the individual. After 8–10 minutes, pooled plaque was taken from the patient's mouth and put into another depression of the color plate. A drop of Bromocresol green dye was added to the collected plaque. On addition of the dye, a color change occurred from green to yellow, and the pH dropped after a glucose rinse, depicting the acidic nature of dental plaque. In order to motivate the patients to regularly remove dental plaque, the effect of sweet foods on the production of weak acids in dental plaque by microorganisms was described to the patients. These weak acids initiate demineralization leading to cavity formation and other by-products of dental plaque bacteria that irritate gingival tissue to produce gingivitis. In addition, as in group I, conventional plaque control measures were also demonstrated to the patients.
Group III
Patients were motivated by showing live motile bacteria in their own plaque under a phase contrast microscope (Nikon, CFI 10 × 22, Yokohama, Japan). Plaque was collected from the interproximal areas or gingival crevice with the help of explorer or periodontal probe and immersed in two to three drops of physiologic saline on the glass slide. A cover slip was placed and pressure was applied to the cover slip to disperse the sample, excess water was carefully removed with tissue paper, and the edges of a cover slip were sealed with jelly to prevent dehydration. Patients were requested to observe active motile live bacteria through the microscope, under magnification power of 400×. A prerecorded video of the plaque bacteria was also shown to the patients. This was followed by plaque disclosure with 2% mercurochrome and demonstration of a horizontal scrubbing method of brushing as done in group I.
Recordings
Baseline observation (R-I) for oral hygiene was done by recording the Glass modified scoring system for debris,8 Loe and Silness Gingival Index,9 and Silness and Loe Plaque Index10 at the time of collection of orthodontic records and placement of separators or bands. After baseline recordings, the first motivational session (MS-I) was given, which varied according to group allocation. This was followed by an oral prophylaxis to bring down the plaque and gingivitis scores to zero. The horizontal scrubbing technique of tooth brushing was demonstrated and patients were instructed to brush three times a day with an orthodontic toothbrush. They were also instructed to brush after every major meal, with an average brushing time of 5 minutes, using a toothpaste containing 1000 ppm of fluoride.
The first follow-up visit (R-II) was after 1 month of orthodontic treatment during which oral hygiene parameters were recorded using the same indices as used in the baseline recording followed by a second motivational session (MS-II). A second follow-up (R-III) was done 3 months after beginning orthodontic treatment during which the parameters for oral hygiene were recorded again followed by a final motivational session. The final follow-up (R-IV) was after 6 months of orthodontic treatment during which the same recordings were done as previously.
Baseline oral debris, plaque, and gingival scores were compared with scores at 1 month, 3 months, and 6 months after placement of orthodontic brackets. Complete analysis of the data was done using analysis of variance (ANOVA), Kruskal-Wallis test, chi-square test, and Wilcoxon rank test.
RESULTS
Sixty-two patients were available for a baseline recording (group I - 21, group II - 23, and group III - 18). This was reduced to 51 (group I - 18, group II - 19, and group III - 14) at the end of the study period.
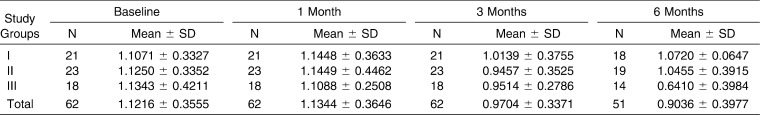
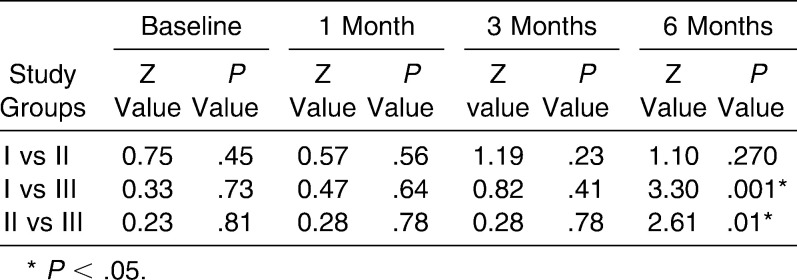
On intergroup comparison, a statistically significant difference was found in mean plaque scores of group III vs group I (P = .001) and group III vs group II (P = .01) between 3 months and 6 months (Tables 1 and 2). Intragroup comparison showed a statistically significant difference between mean plaque scores at 3 months vs 6 months (P = .012) in group I, baseline vs 3 months (P = .03) in group II, and baseline vs 1 month (P = .049) and baseline vs 3 months (P = .029) in group III. When the severity of the plaque score was analyzed, the maximum improvement was found in group III as compared to the other two groups.
Table 1.
Comparison of Mean Plaque Scores Among the Groups
Table 2.
Intergroup Comparison of the Plaque Scores
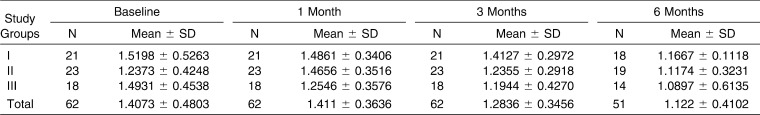
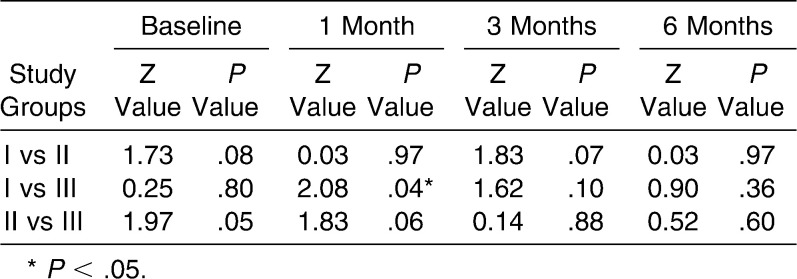
Similarly, intragroup analysis of gingival scores showed a significant difference between 3 months vs 6 months (P = .03) in group I, 1 month vs 6 months and 3 months vs 6 months in group II, and between baseline vs 1 month and baseline vs 3 months in group III. On intergroup comparison, a statistically significant difference in mean gingival scores was present only at 1 month (P = .04) (Tables 3 and 4). In group III, at baseline, 11% had mild, 83% had moderate, and 5.6% had severe gingivitis. After 1 month post bonding and the first motivational session, a definite shift in percentage of subjects was seen from moderate to mild category. The transition was from 28% to 61% in the mild category and from 72% to 39% in the moderate category, in a period of 6 months.
Table 3.
Comparison of Mean Gingival Scores Among the Groups
Table 4.
Intergroup Comparison of the Gingival Score
DISCUSSION
Adolescents exhibit a higher level of supragingival plaque and a higher incidence of gingivitis than adults.11–13 Thus, the sample age of 12–18 years was selected in this study. Another reason were maintaining oral hygiene among adolescents undergoing orthodontic treatment poses a greater problem.14 Erythrosine and 2% mercurochrome are usually the disclosing agents of choice because of their easy availability and ease of application, even at home.15 The red color of the dye is bright enough to motivate the subject for plaque removal. A horizontal scrubbing technique of brushing was taught after plaque disclosure, as vertical brushing has been found to be inadequate in cleaning gingival margins, which are of paramount importance in orthodontic patients.1,16,17 Bromocresol green indicator dye was used because of immediate color change from green to yellow. The change in plaque pH secondary to microbial activity of plaque bacteria provided a scientific rationale to motivate the patients regarding the harmful effects of plaque on the teeth and gums. Other chair side motivational tests, eg, Ora test using phosphoethanolamine dye in milk18 and the Snyder test19 have been used to depict the microbial activity in dental plaque. But, the time taken to record the color change in these tests is too long (ie, 24–96 hours), which is the major disadvantage as far as patient motivation for maintaining oral hygiene is concerned. Moreover, these tests are specific for caries activity rather than for plaque buildup.
Phase contrast microscopy is based on the principle that higher refractive index structures bend light to a much greater angle than structures of low refractive index.20 This device was used to show the motile organisms from patient's own mouth to achieve a greater motivation for removal of dental plaque using visual techniques and making them aware of the disease process. It has been shown that dental plaque removal needs to be reinforced at regular intervals as it shows a relapse to baseline values, if not reinforced at timely intervals.
Boyd21 conducted a study to evaluate the effect of plaque control measures on gingivitis and found that a structured plaque control program only was effective in reducing dental plaque and gingivitis, provided there was periodic reinforcement at 4- to 7-week intervals; otherwise, the gingivitis scores tend to increase to preorthodontic treatment level, on cessation of reinforcement. Therefore, repeated motivational sessions were demonstrated to the patients in all the three groups.
The increase in mean plaque scores from baseline values to 1 month after fixed orthodontic treatment in group I and group II is mainly due to the placement of orthodontic components. However, the decrease in mean plaque scores observed in group III after 1 month may be attributed to an effective motivation through phase contrast microscopy. The prerecorded video shown to group III patients could also have influenced the decrease in plaque scores. There was a further decrease in plaque score in group III after 6 months showing a pronounced effect of phase contrast microscopy as a motivational tool even after 3 months of cessation of the motivational session. A similar study carried out by Shulman et al.22 using phase contrast microscopy as a motivational tool for oral hygiene found that reduction in visible plaque can be maintained at significant levels for up to 7 months.
This study shows that all the methods are equally effective in controlling gingival health when periodic reinforcement of oral hygiene is done. However, the clinical gingivitis scores based on the severity of the disease declined mainly in group III, where besides the conventional methods of plaque disclosure and brushing, the patients were motivated through phase contrast microscopy.
CONCLUSIONS
The implementation of various motivational techniques for effective plaque control in fixed orthodontic patients resulted in improvement in the gingival health over a period of 6 months after placement of fixed orthodontic appliances.
The plaque and gingivitis scores decreased during the study period, and the decrease in gingivitis scores was best evident where phase contrast microscopy was used as a motivational tool, in addition to conventional plaque control measures.
A phase contrast microscope may be an effective motivational tool for maintaining oral hygiene.
REFERENCES
- 1.Zachrisson B. U. Oral hygiene for orthodontic patients: current concepts and practical advice. Am J Orthod. 1974;66:487–497. doi: 10.1016/0002-9416(74)90110-9. [DOI] [PubMed] [Google Scholar]
- 2.Boyd R. L. Longitudinal evaluation of a system for self-monitoring plaque control effectiveness in orthodontic patients. J Clin Periodontol. 1983;10:380–388. doi: 10.1111/j.1600-051x.1983.tb01287.x. [DOI] [PubMed] [Google Scholar]
- 3.Balenseifen J. W, Madonia J. V. Study of dental plaque in orthodontic patients. J Dent Res. 1970;49:320–324. doi: 10.1177/00220345700490022101. [DOI] [PubMed] [Google Scholar]
- 4.Gwinnett J. A, Ceen R. F. Plaque distribution on bonded brackets: a scanning microscope study. Am J Orthod. 1979;75:667–677. doi: 10.1016/0002-9416(79)90098-8. [DOI] [PubMed] [Google Scholar]
- 5.Lundström F, Krasse B. Caries incidence in orthodontic patients with high levels of Streptococcus mutans. Eur J Orthod. 1987;9:117–121. doi: 10.1093/ejo/9.2.117. [DOI] [PubMed] [Google Scholar]
- 6.Lundström F, Hamp S. E. Effect of oral hygiene education on children with and without subsequent orthodontic treatment. Scand J Dent Res. 1980;88:53–59. doi: 10.1111/j.1600-0722.1980.tb00720.x. [DOI] [PubMed] [Google Scholar]
- 7.Huber S. J, Vernino A. R, Nanda R. S. Professional prophylaxis and its effect on the periodontium of full-banded orthodontic patients. Am J Orthod Dentofacial Orthop. 1987;91:321–327. doi: 10.1016/0889-5406(87)90174-0. [DOI] [PubMed] [Google Scholar]
- 8.Glass R. L. A clinical study of hand and electric toothbrushing. J Periodontol. 1965;36:322–327. doi: 10.1902/jop.1965.36.4.322. [DOI] [PubMed] [Google Scholar]
- 9.Loe H, Silness J. Periodontal disease in pregnancy: prevalence and severity. Acta Odontol Scand. 1963;21:532–551. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 10.Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964;22:121–135. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 11.Boyd R. L, Leggott P. J, Quinn R. S, Chambers D. W. Periodontal implications of orthodontic treatment in adults with reduced or normal periodontal tissues versus those of adolescents. Am J Orthod Dentofacial Orthop. 1989;96:191–199. doi: 10.1016/0889-5406(89)90455-1. [DOI] [PubMed] [Google Scholar]
- 12.Boyd R. L, Baumrind S. Periodontal consideration in the use of bonds or bands on molars in adolescents and adults. Angle Orthod. 1992;62:117–126. doi: 10.1043/0003-3219(1992)062<0117:PCITUO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 13.Hamp S. E, Lundström F, Nyman S. Periodontal conditions in adolescents subjected to multiband orthodontic treatment with controlled oral hygiene. Eur J Orthod. 1982;4:77–86. doi: 10.1093/ejo/4.2.77. [DOI] [PubMed] [Google Scholar]
- 14.Anderson G. B, Bowden J, Morrison E. C, Caffesse R. G. Clinical effects of chlorhexidine mouthwashes on patients undergoing orthodontic treatment. Am J Orthod Dentofacial Orthop. 1997;111:606–612. doi: 10.1016/s0889-5406(97)70312-3. [DOI] [PubMed] [Google Scholar]
- 15.Arnim S. S. Use of disclosing agents for measuring tooth cleanliness. J Periodontol. 1963;34:227–245. [Google Scholar]
- 16.Zachrisson B. U, Zachrisson S. Caries incidence and oral hygiene during orthodontic treatment. Scand J Dent Res. 1971;79:394–401. doi: 10.1111/j.1600-0722.1971.tb02028.x. [DOI] [PubMed] [Google Scholar]
- 17.Zachrisson S, Zachrisson B. U. Gingival condition associated with orthodontic treatment. Angle Orthod. 1972;42:26–34. doi: 10.1043/0003-3219(1972)042<0026:GCAWOT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Tal H, Rosenberg M. Estimation of dental plaque levels and gingival inflammation using a simple oral rinse technique. J Periodontol. 1990;61:339–342. doi: 10.1902/jop.1990.61.6.339. [DOI] [PubMed] [Google Scholar]
- 19.Snyder M. L, Arbor A. A simple colorimetric method for diagnosis of caries activity. J Am Dent Assoc. 1941;28:44–49. [Google Scholar]
- 20.Periodontal Risk Assessment Microscopes Available at: https://www.oratec.net/product.asp Accessed Dec. 6, 2008.
- 21.Boyd R. L. Longitudinal evaluation of a system for self-monitoring plaque control effectiveness in orthodontic patients. J Clin Periodontol. 1983;10:380–388. doi: 10.1111/j.1600-051x.1983.tb01287.x. [DOI] [PubMed] [Google Scholar]
- 22.Shulman J. Clinical evaluation of the phase contrast microscope as a motivational aid in oral hygiene. J Am Dent Assoc. 1976;92:759–765. doi: 10.14219/jada.archive.1976.0424. [DOI] [PubMed] [Google Scholar]