Abstract
Objective:
To identify the effect of rapid maxillary expansion (RME) procedure on dynamic measurement of natural head position (NHP).
Materials and Methods:
The treatment group comprised 23 patients, 12 girls and 11 boys (mean age: 10.1 ± 1.1 years), and the control group comprised 15 subjects, 8 girls and 7 boys (mean age: 9.7 ± 1.4 years). The test subjects underwent RME treatment using full cap acrylic device, and the mean amount of expansion was 5.48 mm. An inclinometer and a portable data logger were used to collect the NHP data. Intragroup changes were evaluated by using nonparametric Wilcoxon test, and intergroup changes were analyzed with Mann-Whitney U-test. P values less than .05 were considered statistically significant.
Results:
The mean difference between initial and final NHP was 0.31°, and this difference was not statistically significant. Also, there were no statistically significant differences between the RME and control groups before and after treatment.
Conclusion:
Treatment with the RME procedure showed no statistically significant effects on dynamic measurement of NHP when compared with initial values or untreated control.
Keywords: Posture, Respiratory physiologic phenomena, Palatal expansion technique
INTRODUCTION
Rapid maxillary expansion (RME) has become an accepted procedure for the treatment of maxillary width deficiency or posterior crossbite. Many orthodontists routinely use RME and use it preferably in growing patients with a narrow maxilla.1 It has been noted that RME causes not only dentoalveolar changes, but also craniofacial structure changes.2
RME can also cause a total increase in the nasal cavity's total volume, since its lateral walls are displaced apart. Because the maxillary bones form half of the nasal cavity's anatomic structure, it has been hypothesized that midpalatal disjunction would affect the anatomy and the physiology of the nasal cavity.3 RME separates the external walls of the nasal cavity laterally and causes lowering of the palatal vault and straightening of the nasal septum.3 Several investigators have studied the effects of RME and reported a significant increase in nasal cavity width,3–5 and decreases in nasal resistance after expansion.5 Eventually, RME could result in improvement in the patient's ability to breathe through the nose.6
The influence of respiratory airway function on craniofacial development and head posture has been demonstrated by many authors.7,8 In addition to specific detrimental effects on the facial skeleton, impaired nasal breathing has been reported to cause changes in head posture.9 Moderate cranial extension is thought to decrease the resistance to airflow in the upper airway passages.10 Solow and Kreiborg11 claimed that posturally induced stretching of the soft tissue layer of the face might influence craniofacial morphological development. Thus, there would exist a control mechanism linking airway patency measured as nasal resistance to neuromuscular feedback, head posture, soft tissue stretching, and facial development.12 According to this theory, children with airway obstruction would be expected to show an increased craniocervical angulation.11
Head posture in children with nasal obstruction has been found to be altered after therapeutic measures for improving normal nasal breathing.13 Linder-Aronson14 determined that the average craniofacial morphology of adenoid children approaches that of the control group after adenoidectomy. A relationship between head posture and airway adequacy was demonstrated experimentally by the use of a nose clip by Vig et al.15 Several researchers observed significant changes in head posture and craniocervical angulation after therapy aimed at improving nasal respiratory function in longitudinal studies.16,17 Tecco et al.17 found that RME is capable of increasing nasopharyngeal airway adequacy, and this leads to a decrease in craniocervical angulation.
Head posture is a dynamic concept, and ideally its measurements should be performed in a dynamic and continuous manner.18 Various methods have been shown to obtain natural head position (NHP).19,20 Murphy et al.21 developed electronic equipment to measure head posture continuously over extended time periods. Usumez and Orhan22,23 introduced smaller and lighter device for recording NHP, and they reported it to be effective in the measurement and transfer of head posture.
It is clear from previous findings that there is a relationship between RME and the nasal airway and head posture and the nasal airway. The missing link, however, is the effect of RME on dynamic measurement of head posture. Therefore, this study aimed to identify the effect of RME on dynamic NHP in order to elucidate one of the possible mechanisms that enable RME to act on the nasal airway. For the purposes of this study, the null hypothesis assumed that the dynamic measurement of NHP is not significantly different between subjects who are treated with the RME procedure and the untreated control.
MATERIALS AND METHODS
This study was approved by the Ethical Committee on Research of the Erciyes University. The study included 38 subjects with skeletal Class I malocclusions (mean age: 9.9 ± 1.3 years). The treatment group comprised 23 patients, 12 girls and 11 boys (mean age: 10.1 ± 1.1 years), and the control group comprised 15 subjects, 8 girls and 7 boys (mean age: 9.7 ± 1.4 years).
This study was organized as a parallel group design with one group receiving the experimental protocol and the other serving as the control. The power analysis was established by G*Power Ver. 3.0.10 (Franz Faul Universität, Kiel, Germany) software. Based on 1∶1 ratio between groups, a sample size of 15 patients in one group would give more than 75% power to detect significant differences with 0.30 effect size and at α = .05 significance level.
The samples consisted of patients with transverse maxillary deficiency. Patients who fulfilled the following inclusion criteria were selected:
white,
Class I molar relationship,
skeletal Class I relationship (ANB = 2° ± 2°),
normal vertical growth pattern (SN-MP = 32° ± 6°),
posterior crossbite,
confirmed date of birth,
no congenitally missing or extracted teeth, and
no deformity in the nasomaxillary complex.
Patients with craniofacial abnormality, psychosocial impairment, craniofacial anomaly, or skeletal open bite, nasal allergic conditions, or airway obstructions due to adenoids and previous orthodontic treatment were excluded from the study.
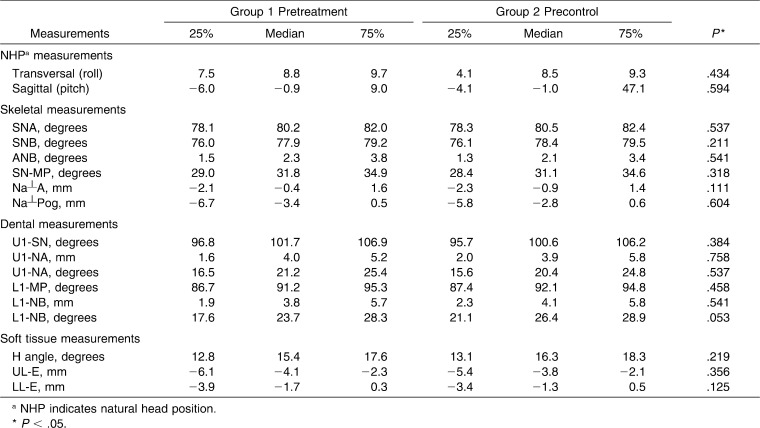
In the treatment group the median of the ANB angle was 2.3°, and the median of the SN-MP angle was 31.8° (Table 1).
Table 1.
Pretreatment/Control Values and Standard Deviations of Measurements and Statistical Comparisons
Patients were divided into two groups, randomly. Subjects in the first group were scheduled to begin treatment soon after the first visit (study group; 23 children). To constitute the control group, records were taken with parental permissions by obtaining informed consent from subjects/parents who did not accept treatment at that time. Most of these subjects accepted the treatment protocol by means of motivation. Nearly 7 months later, after the first visit, the second group began therapy (control group, 15 children). Subjects in the control group did not undergo any type of treatment (orthodontic or pharmacologic therapy) during the observation period.
A splint-type tooth and tissue-borne RME appliance was used.24 The midline expansion screw was activated twice a day for the first week and once a day until the desired change in the transverse dimension (the lingual cusps of the upper posterior teeth approximating the buccal cusps of the lower posterior teeth) was achieved. The appliance was left in place for 1 month after the active expansion period. Then, the appliance used in the active treatment was cleaned and used as a removable retention appliance. One operator based on clinician preference and the patients' individual malocclusions, decided expansion and retention regimens. The retention period lasted approximately 20 weeks in the treatment group.
Dynamic Measurement and Data Logging Procedure
An inclinometer device (linear-tilt sensor, SX-070DLIN; Advanced Orientation Systems, Linden, NJ) and a portable data logger (XR440, Pace Scientific Inc, Mooresville, NC) were used to collect the NHP data by one investigator as described previously (Figures 1 and 2).22 The mean dynamic head posture was calculated for each subject using the collected data. The NHP recordings were made at the initial stage of appliance placement and at the end of the RME therapy (mean treatment period: 7.32 ± 1.12 months). NHP records from the control sample were taken approximately 7–8 months after the first records, similar to the treatment group (mean observation period: 7.83 ± 1.47 months). All NHP recordings in the study group were taken from the patients without the RME appliance in situ.
Figure 1.
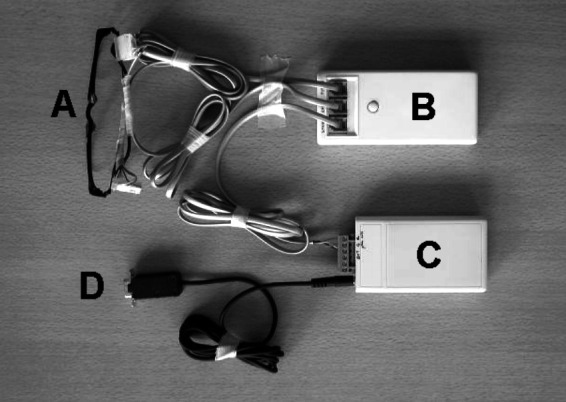
Instruments used in study. (A) Eyeglass frame with inclinometers. (B) Conversion module. (C) Data logger. (D) PC connection cable. A, B, and C were worn, and D was unplugged from logger during walking.
Figure 2.
Cranial portion of device. Note placement of inclinometers on opposite sides.
Statistical Analysis
All statistical analyses were performed using the Statistical Package for Social Sciences (SPSS), version 13.0 for Windows (SPSS Inc, Chicago, Ill). The normality test of Shapiro-Wilks and Levene's variance homogeneity were applied to the data. The data did not distribute normally, and there was no homogeneity of variance between the groups. Descriptive statistics were given as quartiles (25th, 50th [median], and 75th). Intragroup changes were evaluated by nonparametric Wilcoxon test, and intergroup changes were analyzed by Mann-Whitney U-test. When the P value was less than .05, the statistical test was determined as significant.
RESULTS
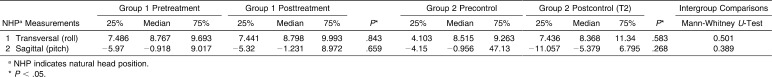
Descriptive pretreatment/control values of measurements and statistical comparisons are presented in Table 1. Pretreatment and posttreatment/control descriptive statistical values and comparisons are presented in Table 2.
Table 2.
Pretreatment and Posttreatment, Precontrol and Postcontrol Values and Standard Deviations of Measurements and Statistical Comparisons
Pretreatment and Precontrol Intergroup Comparisons
To determine whether the two subsamples of subjects were matched or not, a Mann-Whitney U-test was performed on the means of the pretreatment dental and skeletal measurements. It was found that the two subsamples were equally matched because the totality of the measurements was not significantly different.
Pretreatment and Posttreatment and Precontrol and Postcontrol Intragroup Comparisons
Wilcoxon signed rank test was used to determine whether the changes between the initial and final measurements were significant. Results showed no statistically significant differences.
Treatment and Control Changes Between Group Comparisons
A Mann-Whitney U-test was used to determine whether the changes between the groups were significantly different or not; we found that there were no statistically significant differences between the RME and the untreated control groups.
DISCUSSION
In the current study, an inclinometer system was used to analyze the possible relationships between RME and head position.22 The results showed that the changes in NHP following RME were statistically insignificant. Therefore, the null hypothesis could not be rejected in the present study.
It may be suspected that the wearing of the inclinometer apparatus itself has an effect on NHP. The head portion of the instrument used in this study was kept as light and small as possible to avoid affecting NHP. The cranial portion of the instrument used in this study weighed only 21.6 g. Furthermore, Murphy et al.21 demonstrated that the inclinometer apparatus does not have a significant effect on the wearer's head posture.
The inclinometers and cables were placed out of the subject's visual range. The inclinometers were placed on the arms of the eyeglasses without touching the temple, and the cables were directed from behind the neck without causing any discomfort. Operators could place the eyeglasses in the same position consistently on separate occasions, and it was demonstrated that a reasonably exact positioning of the inclinometer was repeatable.21 Therefore, these parameters were not tested in this study.
Usumez and Orhan23 measured NHP in 20 subjects 18 to 24 years of age. They showed that both sagittal and transversal NHP is reproducible after 2 years. The mutual vertical relationship of the bridge of the nose and the superior auricular fornix (where the spectacles that carry the inclinometers rest) is stable in nongrowing subjects over the short term. Despite this stability, differential growth or local soft tissue changes in these areas could change the seat of the spectacles for growing subjects. This might lead to overinterpretation or underinterpretation of the reproducibility of NHP. In this study, all patients were treated/observed over an approximate 7-month period (mean: 7.5 ± 1.28 months). However, many researchers confirmed that NHP is reproducible for the short term.25,26 Further investigation is useful to determine whether a later period after RME has an effect on NHP or not.
Tecco et al.17 included only girls in their study sample to avoid false conclusions about the effective changes in cervical curvature because the curvature of the cervical spine has been related to gender. Male subjects more often exhibit a straight curvature, and female subjects more often exhibit a partial reverse curvature.27 On the other hand, many researchers who investigated NHP found insignificant gender differences.23,28 Because of the limited sample size especially in the control group, and based on the above mentioned studies, gender differences were not evaluated in the present study.
The current study included 38 subjects with skeletal Class I malocclusions with a mean age of 9.9 ± 1.3 years. The patients who underwent RME treatment before a peak in skeletal growth showed significantly greater short-term increases in the width of nasal cavities and more pronounced craniofacial changes than patients treated during or slightly after the peak.29 On the other hand, Babacan et al.30 evaluated the effects of RME on subjects with different maturity levels. They evaluated RME in an adolescent group and surgically assisted RME (SARME) in an adult group and showed significant increases in nasal volume measured by acoustic rhinometry, but reported no differences between groups.31 Similarly, Basciftci et al.3 found no statistically significant differences in RME effects between two different age groups.
On clinical examination, some patients showed lip incompetence, dry lips at rest, dental crowding in the upper arch, adenoidal face, and reduced maxillary transverse dimension with bilateral crossbite. These factors were considered for the diagnosis of mouth breathing in agreement with Moyers' criteria.32 Ricketts10 hypothesized that head extension is often seen in mouth breathers and could be an important physiologic compensation for nasal airway inadequacy. Tecco et al.17 evaluated the effect of RME on nasopharyngeal airway adequacy, head posture, and facial morphology in children with nasal obstruction. Tecco et al.17 reported that their findings confirm this hypothesis, but it is very uncertain whether these changes in head posture are clinically relevant or not. In that study,17 head position changes were determined by lateral skull radiographs. In the current study, NHP was measured by the inclinometer method and did not confirm that hypothesis.
Researchers suggested that RME would not be useful by itself in cases with turbine hypertrophy, nasal polyps, enormous adenoids, or septal deviations.2,3 A possible hypothesis about the role of RME in postural changes may be that the increased palatal diameter results in a consequent enlargement of pharyngeal airway space. This enlargement leads to improvement in respiratory function and the consequent flexion of the head upon the cervical column with an increase in the cervical lordosis angle and a decrease in craniocervical angulations.17 It is important to note that although, theoretically, changes in the nasal cavity can occur with changes in maxillary arch width, many factors exist that can influence nasal airway geometry and resultant patient perception of airflow.31
Several investigators reported significant increases in nasal cavity width3,5 and decreases in nasal resistance after expansion.3,33 However, Wertz34 reported that no airway justification existed for RME unless an obstruction was present in the anteroinferior aspect of the nose, which is the area mostly affected by maxillary expansion. Kurt et al.35 investigated changes in the nasopharyngeal airway following orthopedic and surgically assisted RME and found no statistically significant differences among the SARME, RME, and control groups. Hartgerink et al.36 stated that due to the high individual response variability, RME is not predictable by means of decreasing nasal resistance. Similarly, present findings showed that RME therapy has no statistically significant effects on NHP. Also, many studies have indicated that RME application has conflicting effects on the nasopharyngeal airway.
Hiyama et al.37 found that maxillary growth induced by protraction treatment has a significant positive effect on the superior upper airway dimension. Oktay and Ulukaya38 found that maxillary protraction increases distances and increments in the upper part of the airway space. Further investigation is needed to determine whether the maxillary orthopedic protraction has an effect on NHP or not.
The results of this study suggest that dynamic measurement of NHP recorded by an inclinometer apparatus, which is most probably dictated by the maintenance of the visual axis, is not significantly affected by RME. However, this does not necessarily mean that the craniocervical relation is not altered following RME, and this should be further investigated.
CONCLUSION
Treatment with the RME procedure showed no statistically significant effects on dynamic measurements of NHP when compared to initial values or untreated control.
Acknowledgments
Funding for this project was provided by King Saud University, Visiting Professor Project Unit (Grant No: KSU-VPP-112).
REFERENCES
- 1.Adkins M. D, Nanda R. S, Currier G. F. Arch perimeter changes on rapid palatal expansion. Am J Orthod Dentofacial Orthop. 1990;97:194–199. doi: 10.1016/S0889-5406(05)80051-4. [DOI] [PubMed] [Google Scholar]
- 2.Haas A. J. The treatment of maxillary deficiency by opening the midpalatal suture. Angle Orthod. 1965;35:200–217. doi: 10.1043/0003-3219(1965)035<0200:TTOMDB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Basciftci F. A, Mutlu N, Karaman A. I, Malkoc S, Kucukkolbasi H. Does the timing and method of rapid maxillary expansion have an effect on the changes in the nasal dimensions? Angle Orthod. 2002;72:118–123. doi: 10.1043/0003-3219(2002)072<0118:DTTAMO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Doruk C, Bicakci A. A, Basciftci F. A, Babacan H, Agar U. A comparison of the effects of rapid maxillary expansion and fan-type rapid maxillary expansion on dentofacial structures. Angle Orthod. 2004;74:184–194. doi: 10.1043/0003-3219(2004)074<0184:ACOTEO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Hershey H. G, Steward B. L, Warren D. W. Changes in nasal airway resistance associated with rapid maxillary expansion. Am J Orthod. 1976;69:274–284. doi: 10.1016/0002-9416(76)90076-2. [DOI] [PubMed] [Google Scholar]
- 6.Oliveira De Felippe N. L, Da Silveira A. C, Viana G, Kusnoto B, Smith B, Evans C. A. Relationship between rapid maxillary expansion and nasal cavity size and airway resistance: short- and long-term effects. Am J Orthod Dentofacial Orthop. 2008;134:370–382. doi: 10.1016/j.ajodo.2006.10.034. [DOI] [PubMed] [Google Scholar]
- 7.Solow B, Tallgren A. Head posture and craniofacial morphology. Am J Phys Anthropol. 1976;44:417–436. doi: 10.1002/ajpa.1330440306. [DOI] [PubMed] [Google Scholar]
- 8.Solow B, Tallgren A. Dentoalveolar morphology in relation to cranio-cervical posture. Angle Orthod. 1977;47:157–164. doi: 10.1043/0003-3219(1977)047<0157:DMIRTC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Huggare J. A, Laine-Alava M. T. Nasorespiratory function and head posture. Am J Orthod Dentofacial Orthop. 1997;112:507–511. doi: 10.1016/s0889-5406(97)70078-7. [DOI] [PubMed] [Google Scholar]
- 10.Ricketts R. M. Respiratory obstruction syndrome. Am J Orthod. 1968;54:495–507. doi: 10.1016/0002-9416(68)90218-2. [DOI] [PubMed] [Google Scholar]
- 11.Solow B, Kreiborg S. Soft-tissue stretching: a possible control factor in craniofacial morphogenesis. Scand J Dent Res. 1977;85:505–507. doi: 10.1111/j.1600-0722.1977.tb00587.x. [DOI] [PubMed] [Google Scholar]
- 12.Weber Z. J, Preston C. B, Wright P. G. Resistance to nasal airflow related to changes in head posture. Am J Orthod. 1981;80:536–545. doi: 10.1016/0002-9416(81)90248-7. [DOI] [PubMed] [Google Scholar]
- 13.Wenzel A, Henriksen J, Melsen B. Nasal respiratory resistance and head posture: effect of intranasal corticosteroid (Budesonide) in children with asthma and perennial rhinitis. Am J Orthod. 1983;84:422–426. doi: 10.1016/0002-9416(93)90005-r. [DOI] [PubMed] [Google Scholar]
- 14.Linder-Aronson S. Effects of adenoidectomy on dentition and nasopharynx. Trans Eur Orthod Soc. 1972:177–186. [PubMed] [Google Scholar]
- 15.Vig P. S, Showfety K. J, Phillips C. Experimental manipulation of head posture. Am J Orthod. 1980;77:258–268. doi: 10.1016/0002-9416(80)90081-0. [DOI] [PubMed] [Google Scholar]
- 16.Solow B, Siersbæk-Nielsen S, Greve E. Airway adequacy, head posture and craniofacial morphology. Am J Orthod. 1984;86:214–223. doi: 10.1016/0002-9416(84)90373-7. [DOI] [PubMed] [Google Scholar]
- 17.Tecco S, Festa F, Tete S, Longhi V, D'Attilio M. Changes in head posture after rapid maxillary expansion in mouth-breathing girls: a controlled study. Angle Orthod. 2005;75:171–176. doi: 10.1043/0003-3219(2005)075<0167:CIHPAR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Preston C. B, Evans W. G, Todres J. I. The relationship between ortho head posture and head posture measured during walking. Am J Orthod Dentofacial Orthop. 1997;111:283–287. doi: 10.1016/s0889-5406(97)70186-0. [DOI] [PubMed] [Google Scholar]
- 19.Showfety K. J, Vig P. S, Matteson S. A simple method for taking natural head position cephalograms. Am J Orthod. 1983;83:495–500. [PubMed] [Google Scholar]
- 20.Marcotte M. R. Head posture and dentofacial proportions. Angle Orthod. 1981;51:208–213. doi: 10.1043/0003-3219(1981)051<0208:HPADP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Murphy K. E, Preston C. B, Evans W. G. The development of instrumentation for the dynamic measurement of changing head posture. Am J Orthod Dentofacial Orthop. 1991;99:520–526. doi: 10.1016/S0889-5406(05)81628-2. [DOI] [PubMed] [Google Scholar]
- 22.Usumez S, Orhan M. Inclinometer method for recording and transferring natural head position in cephalometrics. Am J Orthod Dentofacial Orthop. 2001;120:664–670. doi: 10.1067/mod.2001.117201. [DOI] [PubMed] [Google Scholar]
- 23.Usumez S, Orhan M. Reproducibility of natural head position measured with an inclinometer. Am J Orthod Dentofacial Orthop. 2003;123:451–454. doi: 10.1067/mod.2003.71. [DOI] [PubMed] [Google Scholar]
- 24.Basciftci F. A, Karaman A. I. Effects of a modified acrylic bonded rapid maxillary expansion appliance and vertical chin cap on dentofacial structures. Angle Orthod. 2002;72:61–71. doi: 10.1043/0003-3219(2002)072<0061:EOAMAB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.Sandham A. Repeatability of head posture recordings from lateral cephalometric radiographs. Br J Orthod. 1988;15:157–162. doi: 10.1179/bjo.15.3.157. [DOI] [PubMed] [Google Scholar]
- 26.Lundström A, Forsberg C. M, Westergren H, Lundström F. A comparison between estimated and registered natural head posture. Eur J Orthod. 1991;13:59–64. doi: 10.1093/ejo/13.1.59. [DOI] [PubMed] [Google Scholar]
- 27.Hellsing E, Reigo T, McWilliam J, Spangfort E. Cervical and lumbar lordosis and thoracic kyphosis in 8, 11 and 15-year-old children. Eur J Orthod. 1987;9:129–138. doi: 10.1093/ejo/9.2.129. [DOI] [PubMed] [Google Scholar]
- 28.Peng L, Cooke M. S. Fifteen-year reproducibility of natural head posture: a longitudinal study. Am J Orthod Dentofacial Orthop. 1999;116:82–85. doi: 10.1016/s0889-5406(99)70306-9. [DOI] [PubMed] [Google Scholar]
- 29.Baccetti T, Franchi L, Cameron C. G, McNamara J. A., Jr Treatment timing for rapid maxillary expansion. Angle Orthod. 2001;71:343–350. doi: 10.1043/0003-3219(2001)071<0343:TTFRME>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 30.Babacan H, Sokucu O, Doruk C, Ay S. Rapid maxillary expansion and surgically assisted rapid maxillary expansion effects on nasal volume. Angle Orthod. 2006;76:66–71. doi: 10.1043/0003-3219(2006)076[0066:RMEASA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 31.Gordon J. M, Rosenblatt M, Witmans M, Carey J. P, Heo G, Major P. W, Flores-Mir C. Rapid palatal expansion effects on nasal airway dimensions as measured by acoustic rhinometry. A systematic review. Angle Orthod. 2009;79:1000–1007. doi: 10.2319/082108-441.1. [DOI] [PubMed] [Google Scholar]
- 32.Moyers R. E. Handbook of Orthodontics 3rd ed. Chicago, Ill: Year Book Medical Publishers; 1973. p. 442. [Google Scholar]
- 33.Linder-Aronson S, Aschan G. Nasal resistance to breathing and palatal height before and after expansion of the median palatal suture. Odontol Revy. 1963;14:254–270. [Google Scholar]
- 34.Wertz R. A. Changes in nasal airflow incident to rapid maxillary expansion. Angle Orthod. 1968;38:1–11. doi: 10.1043/0003-3219(1968)038<0001:CINAIT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 35.Kurt G, Altuğ-Ataç A. T, Atac M. S, Karasu H. A. Changes in nasopharyngeal airway following orthopedic and surgically assisted rapid maxillary expansion. J Craniofac Surg. 2010;21:312–317. doi: 10.1097/SCS.0b013e3181cf5f73. [DOI] [PubMed] [Google Scholar]
- 36.Hartgerink D. V, Vig P. S, Abbott D. W. The effect of rapid maxillary expansion on nasal airway resistance. Am J Orthod Dentofacial Orthop. 1987;92:381–389. doi: 10.1016/0889-5406(87)90258-7. [DOI] [PubMed] [Google Scholar]
- 37.Hiyama S, Suda N, Suzuki M. I, Tsuiki S, Ogawa M, Suzuki S, Kuroda T. Effects of maxillary protraction on craniofacial structures and upper airway dimension. Angle Orthod. 2002;72:43–47. doi: 10.1043/0003-3219(2002)072<0043:EOMPOC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 38.Oktay H, Ulukaya E. Maxillary protraction appliance effect on the size of the upper airway passage. Angle Orthod. 2008;78:209–214. doi: 10.2319/122806-535.1. [DOI] [PubMed] [Google Scholar]