Abstract
Objective:
To investigate the relationship between nasal obstruction and lip-closing force.
Materials and Methods:
Nasal airway resistance and lip-closing force measures were recorded for 54 Japanese females. The subjects were classified into normal and nasal obstruction groups according to nasal airway resistance values. Differences between the normal and nasal obstruction groups in lip-closing force were tested statistically. Correlation coefficients were calculated between the measures for the normal and nasal obstruction groups.
Results:
Lip-closing force for the nasal obstruction group was significantly less than for the normal group (P < .05). In the normal group, nasal airway resistance did not correlate with lip-closing force, while in the nasal obstruction group a significant negative correlation was found between nasal airway resistance and lip-closing force (P < .05).
Conclusions:
Nasal obstruction is associated with a decrease in lip-closing force. When the severity of nasal obstruction reaches a certain level, the lip-closing force is weakened.
Keywords: Nasal obstruction, Lip function, Airway
INTRODUCTION
Greater effort is required to breathe through the nose than through the mouth because of the tortuous nasal passage. If the nose is obstructed, nasal breathing switches to partial mouth breathing.1 Mouth breathers are expected to exhibit lip incompetence with weak lip-closing force. Therefore, it is interesting to examine lip-closing force in patients with nasal obstruction. Previously, nasal obstruction2–6 and lip function7–10 have been individually investigated in relation to craniofacial morphology.
With regard to the relationship between nasal obstruction and lip function, previous research11–13 has shown no relationship between nasal airway resistance and lip incompetence. Some patients exhibit parted lips at rest even though the nasal airway adequacy is normal.13 These reports have examined quantitative data relating to nasal airway resistance and the qualitative characteristics of lip function. No research has investigated the quantitative relationship between nasal airway resistance and lip-closing force.
The purposes of the present study were (1) to examine nasal airway resistance and lip-closing force in adults and (2) to investigate the relationship between nasal obstruction and lip-closing force.
MATERIALS AND METHODS
Fifty-four Japanese females (mean age: 24 years 7 months; range: 18 years 1 month–45 years 0 months) who were seeking orthodontic treatment because of malocclusion participated in this study. Subjects had good general and dental health, no skeletal discrepancy, and no history of facial surgery. They did not have nasal deformity, infection, allergies, or other nasal disease. Body heights ranged from 146 cm to 168 cm, and weights ranged from 41 kg to 71 kg. This study was approved by the Ethical Committee of the Kagoshima University Medical and Dental Hospital.
Nasal airway resistance was recorded for each subject using an anterior rhinomanometry device (RHINOREOGRAPH MPR-3100, Nihon-Kohden Co, Ltd, Tokyo, Japan) (Figure 1).14,15 Data were recorded for each bilateral breath. We calculated nasal airway resistance at peak flow using the equation R = delta P/V,16 where R indicates resistance, delta P indicates transnasal differential pressure, and V indicates nasal airflow. We used 100 Pa as a characteristic transnasal differential pressure for Japanese people.17,18
Figure 1.
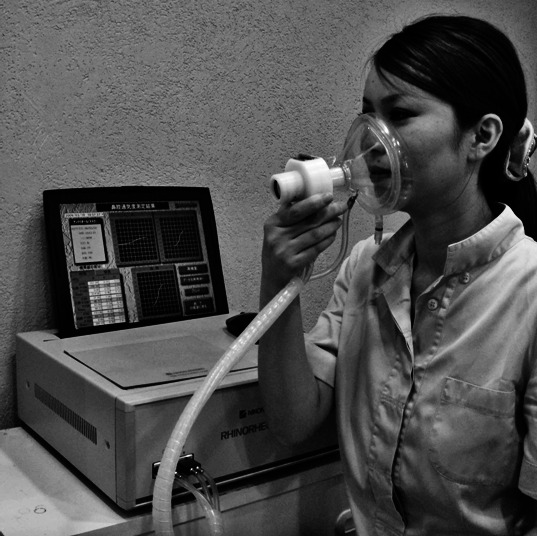
Anterior rhinomanometry device for measurement of nasal airway resistance (RHINOREOGRAPH MPR-3100, Nihon-Kohden Co, Ltd, Tokyo, Japan).
Maximum lip-closing force was recorded using a strain measuring device (LIP DE CUM LDC®-110R, Cosmo-Instruments Co, Ltd, Tokyo, Japan) (Figure 2).19,20 Subjects were in the seated position with the Frankfort plane parallel to the floor. Subjects inserted the lip pad into the oral vestibule with centric occlusion (Figure 3), preventing the lip pad from touching the frenum of the upper lip.19 Subjects had a 1-minute break before each measurement.
Figure 2.
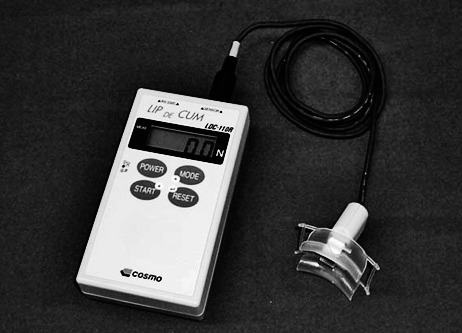
Full view of strain measuring device for maximum lip-closing force (LIP DE CUM LDC®-110R, Cosmo-Instruments, Co, Ltd, Tokyo, Japan).
Figure 3.

Example of measuring maximum lip-closing force.
Both measurements were performed three times for each subject. Because there were no significant differences among the three measurements, we defined the average value of the measurements as the subject's value. All measurements of nasal airway resistance and lip-closing force were conducted between 9 AM and 12 PM (noon) for the diagnosis and treatment planning.
Statistical Analysis
Spearman rank correlation coefficients were used to evaluate the effects of age, body height, and body weight on nasal airway resistance and lip-closing force. The subjects were classified into two groups according to Usui's21 classification of nasal obstruction. Subjects with less than 0.25 Pa/cm3/s in nasal airway resistance were classified into the normal group, and those with more than 0.25 Pa/cm3/s were classified into the nasal obstruction group. Differences in the values of lip-closing force between the normal and nasal obstruction groups were tested using the Student's t-test. Spearman rank correlation coefficients were calculated between the nasal airway resistance measures and lip-closing force in the normal and nasal obstruction groups. A P < .05 level of significance was chosen for all tests. Analyses were performed using statistical software (Microsoft Office Excel 2007, Microsoft Corporation, Tokyo, Japan).
RESULTS
No significant correlations were found between values for nasal airway resistance or lip-closing force and age, body height, or body weight. Therefore, we used the nasal airway resistance and lip-closing force data from all subjects for the analysis described below.
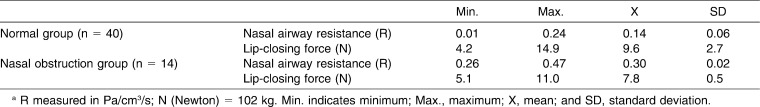
The measured values for nasal airway resistance and lip-closing force are shown in Table 1. Forty subjects had less than 0.25 Pa/cm3/s in nasal airway resistance and were classified into the normal group. Fourteen subjects had more than 0.25 Pa/cm3/s in nasal airway resistance and were classified into the nasal obstruction group.
Table 1.
The Measured Values for Nasal Airway Resistance and Lip-Closing Force in Two Groupsa
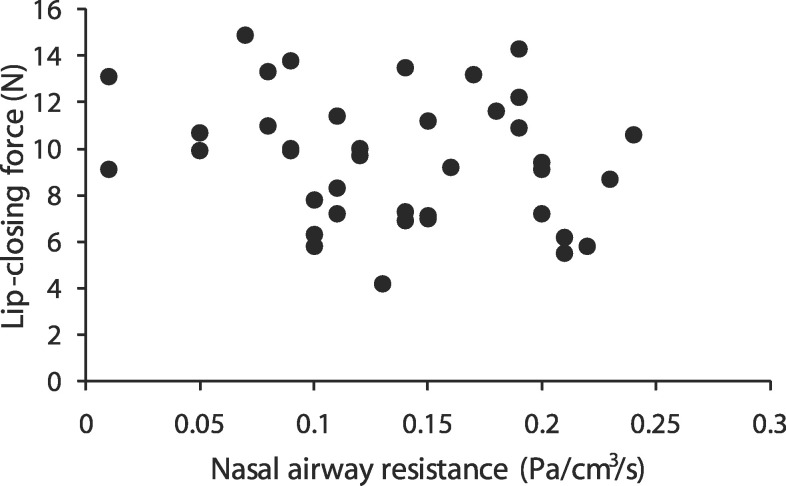
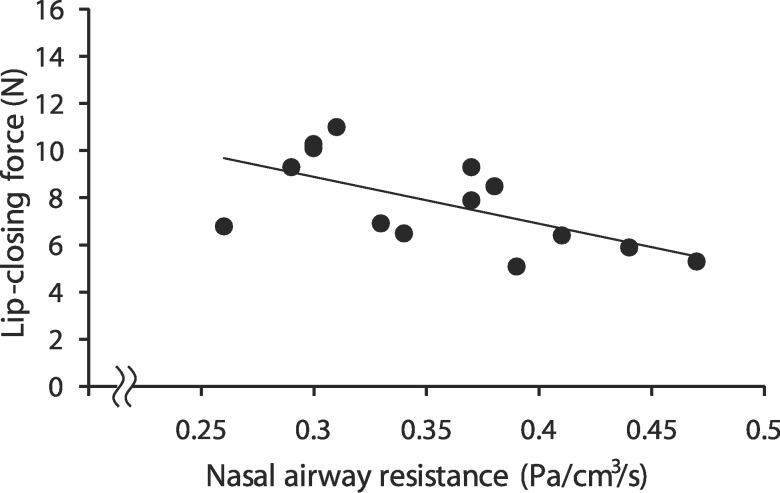
Lip-closing force was significantly lower for the nasal obstruction group than for the normal group (P < .05; Table 1). In the normal group, nasal airway resistance did not correlate with lip-closing force (Figure 4). In the nasal obstruction group, a significant negative correlation was found between nasal airway resistance and lip-closing force (γ = −0.616, P < .05; Figure 5).
Figure 4.
Relationship between nasal airway resistance and lip closing-force in the normal group (n = 40).
Figure 5.
Relationship between nasal airway resistance and lip closing-force in the nasal obstruction group. (The straight line in the graph indicates regression equation. y = −0.019x + 0.504; γ = 0.616; n = 14; P < .05.)
DISCUSSION
There were no significant correlations between nasal airway resistance or lip-closing force values and age among subjects between 18 and 45 years of age in the present study. These results disagree with those described in a previous report,22 which found that age had significant effects on nasal respiratory function in subjects between the ages of 5 and 73 years. This disagreement could be explained by the difference in age distribution of the subjects in that study and those in the study reported here. The subjects in this study were between 18 and 45 years old, and all subjects were female. In the present study, no significant correlations were found between nasal airway resistance or lip-closing force and body height or body weight. These results indicate that nasal airway resistance and lip-closing force are not dependent on physical size in adult females aged between 18 and 45 years. The narrow range of body size of the subjects might cause no significant correlations between nasal airway resistance or lip-closing force and body size.
In the present study, lip-closing force was lower for the nasal obstruction group than for the normal group. In the normal group, nasal airway resistance did not correlate with lip-closing force. This indicates that lip-closing force is decreased when nasal airway resistance reaches a certain level. In the nasal obstruction group, a significant negative correlation was found between nasal airway resistance and lip-closing force. This indicates that in the nasal obstruction group, nasal obstruction was associated with a decrease in lip-closing force. These findings support previous reports1,13 that documented that increased nasal airway resistance is physiologically acceptable to some level and that nasal breathing is replaced by partial mouth breathing at a certain level of nasal airway resistance. The ratio of mouth breathing to nasal breathing is changeable. The change in the ratio may explain that there was a negative correlation between nasal airway resistance and lip-closing force in the nasal obstruction group. In addition, it is likely that mouth breathers routinely keep their lips apart and do not exercise the peri-oral muscles effectively. Therefore, mouth breathing may lead to weakened lip-closing force, although the relationship between mouth breathing and lip-closing force has not been investigated.
The results of the present study should contribute to improved insight into nasal airway pathology, adding to our understanding of the diagnosis and treatment of patients with nasal obstruction. We should be careful with patients with nasal obstruction because they may have weak lips.
CONCLUSIONS
Lip-closing force for the nasal obstruction group was significantly less than for the normal group.
Nasal airway resistance and lip-closing force showed no correlation in the normal group.
Nasal airway resistance and lip-closing force showed a negative correlation in the nasal obstruction group.
Acknowledgments
The authors wish to thank Nellie W. Kremenak for grammatical correction of the manuscript.
REFERENCES
- 1.Warren D. W, Mayo R, Zajac D. J, Rochet A. H. Dyspnea following experimentally induced increased nasal airway resistance. Cleft Palate Craniofac J. 1996;33:231–235. doi: 10.1597/1545-1569_1996_033_0231_dfeiin_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 2.Crupi P, Portelli M, Matarese G, et al. Correlations between cephalic posture and facial type in patients suffering from breathing obstructive syndrome. Eur J Paediatr Dent. 2007;8:77–82. [PubMed] [Google Scholar]
- 3.Jakobsone G, Urtane I, Terauds I. Soft tissue profile of children with impaired nasal breathing. Stomatologija. 2006;8:39–43. [PubMed] [Google Scholar]
- 4.Kluemper G. T, Vig P. S, Vig K. W. Nasorespiratory characteristics and craniofacial morphology. Eur J Orthod. 1995;17:491–495. doi: 10.1093/ejo/17.6.491. [DOI] [PubMed] [Google Scholar]
- 5.Weider D. J, Baker G. L, Salvatoriello F. W. Dental malocclusion and upper airway obstruction, an otolaryngologist's perspective. Int J Pediatr Otorhinolaryngol. 2003;67:323–331. doi: 10.1016/s0165-5876(02)00394-4. [DOI] [PubMed] [Google Scholar]
- 6.Zicari A. M, Albani F, Ntrekou P, et al. Oral breathing and dental malocclusions. Eur J Paediatr Dent. 2009;10:59–64. [PubMed] [Google Scholar]
- 7.Ambrosio A. R, Trevilatto P. C, Martins L. P, Santos-Pinto A. D, Shimizu R. H. Electromyographic evaluation of the upper lip according to the breathing mode: a longitudinal study. Braz Oral Res. 2009;23:415–423. doi: 10.1590/s1806-83242009000400011. [DOI] [PubMed] [Google Scholar]
- 8.Ambrosio A. R, Trevilatto P. C, Sakima T, Ignacio S. A, Shimizu R. H. Correlation between morphology and function of the upper lip: a longitudinal evaluation. Eur J Orthod. 2009;31:306–313. doi: 10.1093/ejo/cjn112. [DOI] [PubMed] [Google Scholar]
- 9.Jung M. H, Yang W. S, Nahm D. S. Effects of upper lip closing force on craniofacial structures. Am J Orthod Dentofacial Orthop. 2003;123:58–63. doi: 10.1067/mod.2003.54. [DOI] [PubMed] [Google Scholar]
- 10.Jung M. H, Yang W. S, Nahm D. S. Maximum closing force of mentolabial muscles and type of malocclusion. Angle Orthod. 2010;80:72–79. doi: 10.2319/020509-78.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vig P. S, Sarver D. M, Hall D. J, Warren D. W. Quantitative evaluation of nasal airflow in relation to facial morphology. Am J Orthod. 1981;79:263–272. doi: 10.1016/0002-9416(81)90074-9. [DOI] [PubMed] [Google Scholar]
- 12.Hartgerink D. V, Vig P. S. Lower anterior face height and lip incompetence do not predict nasal airway obstruction. Angle Orthod. 1989;59:17–23. doi: 10.1043/0003-3219(1989)059<0017:LAFHAL>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 13.Fricke B, Gebert H. J, Grabowski R, Hasund A, Serg H. G. Nasal airway, lip competence, and craniofacial morphology. Eur J Orthod. 1993;15:297–304. doi: 10.1093/ejo/15.4.297. [DOI] [PubMed] [Google Scholar]
- 14.Broms P, Ivarsson A, Jonson B. Rhinomanometry. I. Simple equipment. Acta Otolaryngol. 1982;93:455–460. doi: 10.3109/00016488209130904. [DOI] [PubMed] [Google Scholar]
- 15.Santiago-Diez de Bonilla J, McCaffrey T. V, Kern E. B. The nasal valve: a rhinomanometric evaluation of maximum nasal inspiratory flow and pressure curves. Ann Otol Rhinol Laryngol. 1986;95:229–232. doi: 10.1177/000348948609500304. [DOI] [PubMed] [Google Scholar]
- 16.Naito K, Iwata S, Ohoka E, Kondo Y, Takeuchi M. A comparison of current expressions of nasal patency. Eur Arch Otorhinolaryngol. 1993;250:249–252. doi: 10.1007/BF00171535. [DOI] [PubMed] [Google Scholar]
- 17.Naito K, Iwata S. Current advances in rhinomanometry. Eur Arch Otorhinolaryngol. 1997;254:309–312. doi: 10.1007/BF02630720. [DOI] [PubMed] [Google Scholar]
- 18.Ohki M, Hasegawa M. Studies of transnasal pressure and airflow values in a Japanese population. Rhinology. 1986;24:277–282. [PubMed] [Google Scholar]
- 19.Miura H, Kariyasu M, Sumi Y, Yamasaki K. Labial closure force, activities of daily living, and cognitive function in frail elderly persons. Nippon Ronen Igakkai Zasshi. 2008;45:520–525. doi: 10.3143/geriatrics.45.520. [DOI] [PubMed] [Google Scholar]
- 20.Sabashi K, Kondo S. Influence of frenulum labi superioris on lip closure in children. Shouni Shikagaku Zassi. 2004;42:661–667. [Google Scholar]
- 21.Usui N. Rhinomanometry. Nitijibi Senmoni Tusin. 1975;32:6–7. [Google Scholar]
- 22.Vig P. S, Zajac D. J. Age and gender effects on nasal respiratory function in normal subjects. Cleft Palate Craniofac J. 1993;30:279–284. doi: 10.1597/1545-1569_1993_030_0279_aageon_2.3.co_2. [DOI] [PubMed] [Google Scholar]