Abstract
Objective:
To evaluate the bond strength of a self-etch bonding system using static loading and cyclic fatigue with shear testing. This is a two-part evaluation; the first part will evaluate shear testing, the second part tensile testing.
Materials and Methods:
Bovine teeth (n = 82) were randomly distributed to either a self-etch (Transbond Plus) or total-etch (37% phosphoric-acid + Transbond XT) group. The static shear (SSBS) and cyclic shear (CSBS) bond strengths were measured 24 hours after the bonding of mesh-based brackets. The adhesive remnant index (ARI) and failure sites were evaluated.
Results:
The mean SSBS was 34.25 ± 9.21 and 24.64 ± 9.42 MPa for the total- and self-etch groups, respectively. CSBS was 24.07 ± 0.65 MPa and 18.92 ± 1.08 MPa for the total- and self-etch groups, respectively. Cyclic loading produced lower bond strengths compared to static testing for both adhesives; the difference was only statistically significant for the total-etch system. Comparison of the two materials showed a statistically significant difference between the two techniques. The total-etch had higher bond strengths than the self-etch bonding system. The samples showed a predominance of ARI scored of 2 and 1, and their bonding failure sites were cohesive within the composite.
Conclusion:
Cyclic loading, simulating occlusal forces, reduces the bond strength of both bonding systems. Even though the self-etch bonding system had lower shear bond strength than the total-etch system, both were still clinically acceptable.
Keywords: Bond strength, Self-etch, Total-etch, Shear testing, Cyclic fatigue
INTRODUCTION
Bonding of brackets, eliminating the need for bands, became a routine clinical procedure in the 1980s. Buonocore1 introduced the acid-etch technique in 1955, and in 1964 a direct-bonding technique was developed for bonding orthodontic brackets.2
Today, orthodontists commonly use the acid-etch technique when attaching brackets to the enamel surface. The most frequently used acid-etching agent for enamel surface preparation is phosphoric acid. Phosphoric acid etching requires rinsing and drying after application of the etching reagent. This technique is called the etch and rinse or total-etch technique. Even though it is still used widely, it has some disadvantages: it has been described as technique sensitive due to the need for proper moisture control,3 it has been reported that moisture in etched enamel may disturb resin penetration and thus reduce adhesion,4 it has been implicated in enamel decalcification in some cases,3 and some studies have reported mechanical damage to enamel during debonding after acid etching.5–7
Recently, there has been some interest in using self-etch bonding, a bonding system that could etch, prime, and bond in one step. It no longer requires an etch and rinse phase, which reduces both clinical application time and the risk of making errors during application and manipulation. Another important advantage of self-etch bonding is that the self-etching process and the enamel infiltration by the adhesive occur simultaneously. The self-etch bonding produces an etching pattern similar to phosphoric acid6,8–10 but causes no enamel fractures in the tooth surface after debonding procedures.11
Although self-etch bonding has handling characteristics that may make it superior to the conventional total-etch approach, studies have shown that the bracket bond strength of resin cements using phosphoric acid etching is greater than that of self-etch bonding. However, several studies have shown that the self-etch bonding provides acceptable bond strength.9,11 All these studies evaluated the orthodontic bond strength of self-etch bonding using static shear forces, but there have not been any studies using cyclic shear forces (cyclic fatigue).
In an in vivo situation, bonding systems are more likely to be challenged by repeated applications of stresses that are below the maximum stress that these systems could withstand. Therefore, fatigue test results would provide more accurate predictions of the in vivo performance of orthodontic bonding systems.12 The present study, therefore, will be undertaken to investigate the hypothesis that there is no statistically significant difference between the mean bond strength of the self-etch bonding and total-etch bonding systems used in bonding orthodontic brackets, when subjected to both static and cyclic fatigue loading using shear testing methods.
MATERIALS AND METHODS
Extracted bovine lower incisors (n = 82) selected for this study were without caries, obvious defects, or attrition. The roots of the teeth were removed, and the teeth were stored in distilled water until bonding. Studies have concluded that the adhesive strength to enamel showed no statistical difference between bovine and human teeth, although the mean values were always slightly lower for bovine teeth.13,14
For the experiment, the teeth were embedded in auto-polymerized acrylic resin (Vitacryllic; Fricke Dental Manufacturing Co, Villa Park, IL) in a rubber mold (25 mm in diameter × 20 mm deep) such that the flat surface of the enamel was parallel to the base of the acrylic mold. The surfaces were polished with medium grit pumice for 5 seconds (Great Lakes Orthodontics Co, Ltd, Tonawanda, NY) and washed with water. The mounted teeth were then randomly divided into two groups.
Enamel Preparation
The enamel surface was prepared, and the brackets were bonded to the teeth according to the protocols described in the following sections.
Total-Etch Group
In the total-etch group, 41 teeth were etched with a 37% phosphoric acid gel for 20 seconds. The teeth were thoroughly washed with water for 15 seconds and gently dried for 2–5 seconds with an air source free of oil and moisture. A thin layer of the liquid unfilled resin of the Transbond XT (3M Unitek Orthodontic Products, Monrovia, Calif) was applied with a brush tip before bracket bonding and then dried for 2–5 seconds.
Self-Etch Group
The orthodontic one-step self-etch bonding solution Transbond Plus (TBP; 3M Unitek Orthodontic Products) was used in the bonding of orthodontic brackets for 41 samples. The TBP is predosed for single applications to avoid the problem of evaporization and possible contamination. For activation of the TBP, the first compartment was squeezed and then folded, followed by squeezing the second compartment into the third one. The resulting mix was applied directly onto the tooth surface. The area to be etched was rubbed with the solvent for 3 seconds and was gently air dried for 2–5seconds.
Bracket Bonding
Eighty-two stainless-steel upper right central incisor brackets (Victory series; 3M Unitek Orthodontic Products) with a base surface area of 12.6 mm2 were used for this study. Following the surface preparation, the brackets were bonded on the bovine incisors with Transbond XT light cured composite (3M Unitek Orthodontic Products), and any excess resin was removed with an explorer before the polymerization of the resin. The resin was cured for 10 seconds from the mesial and distal sides using a light-emitting diode light source (Ortholux LED; 3M Unitek Orthodontic Products). After completing the sample preparation, all samples were stored in distilled water at 37°C for 24 hours.
Testing Procedures
Bond strength of prepared samples was tested using a universal material testing system (Instron 1125; Canton, Mass). Measurements were performed at 24 hours after cure.
The Static Shear Testing
The prepared samples, 16 in each group, were mounted in a guillotine jig and evaluated at a crosshead speed of 2 mm/min according to testing procedures used by Drummond et al.15 This jig permits the force to be directed parallel to the enamel surface at the adhesive-enamel interface. The bond strengths (MPa) were determined by dividing the surface area of the bracket (mm2) into the fracture load (N).
The Cyclic Fatigue Testing
The cyclic fatigue testing was also performed at a crosshead speed of 2 mm/min using an up-and-down method according to the compressive fatigue method used by Draughn.16 The initial load was approximately 60% of the mean static testing results of each group, and the test was run for 1000 cycles or until bond failure. If any bracket survived the 1000 cycles, then the load was raised by a fixed amount of 20 Newton (N) for the next tested sample. On the other hand, if the bracket did not survive, ie, the bond failed at some point during the 1000 cycles, the load was lowered also by the same fixed amount of 20 N for the next sample. This procedure—raising the maximum load by 20 N following a test where the orthodontic bond has not failed and lowering the load by the same fixed amount following a bond failure—was continued for each following sample until all 25 samples in each group were evaluated.
This “up and down” method provides a good measure of the mean fatigue limit and allows calculation of the standard deviation of that mean. For accurate data analysis, a minimum of fifteen samples is required to perform the up and down test to evaluate the fatigue strength.16 In the present study, the number of each sample group was 25. According to the procedure addressed by Draughn,16 the data analysis was based on the event that occurred (bond failures, no bond failures) with the least frequency. These data were arranged in ascending manner, starting with the lowest strength and ending with the highest. The mean fatigue strength, x, and its standard deviation, s, are calculated by the standard formulae.
Adhesive Remnant Index Scoring
Adhesive Remnant Index (ARI) scores were recorded for each sample that was a failure. The ARI scoring scale is as follows: 0 = all composite resin remains on the bracket base, 1 = less than 50% composite remaining on the enamel, 2 = greater than 50% composite remains on the enamel, 3 = all composite remains on the enamel. The most desired situation is a high ARI, when all composite remains on the enamel surface; the likelihood of enamel fracture on debonding decreases when ARI scores are consistently high.
Statistical Analysis
The static shear bond strength (SSBS) data were analyzed using a t-test to determine the difference between the two different etching groups. SPSS for Windows (LEAD Technologies Inc, Chicago, Ill) was used for the analysis. The cyclic shear bond strength (CSBS) data were analyzed according to the design by Draughn.16 Student's t-test was used to determine significance between the cyclic subgroups and between static and cyclic groups. A Kruskal-Wallis test was used in conjunction with a Mann-Whitney test to compare the differences in the ARI scores.
RESULTS
Bond Strength Results
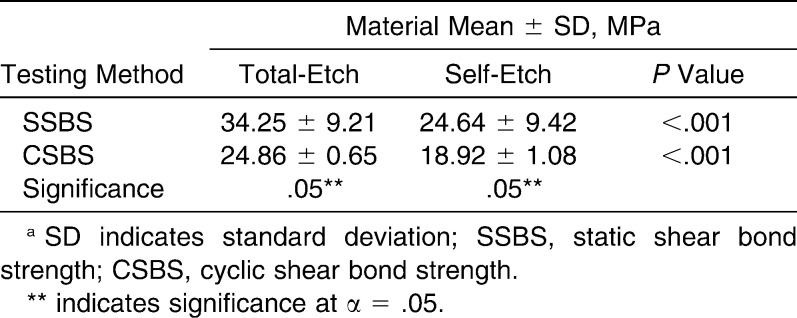
The SSBS and CSBS were measured. Mean bond strengths and standard deviations for all groups are shown in Table 1.
Table 1.
Mean Shear Bond Strengths and Standard Deviations for the Test and Control Groupsa
Cyclic Fatigue Resistance
A significant difference (P < .001) was found between the mean cyclic shear bond strength of the total- and self-etch bonding systems. Mean CSBS for the total-etch was 24.07 ± 0.65 MPa, whereas that of the self-etch was 18.92 ± 1.08 MPa. These values were approximately 70.6% and 76.8% of their mean SSBS, respectively. However, t-tests only revealed a significant difference between the CSBS and SSBS for the total-etch group (P < .05).
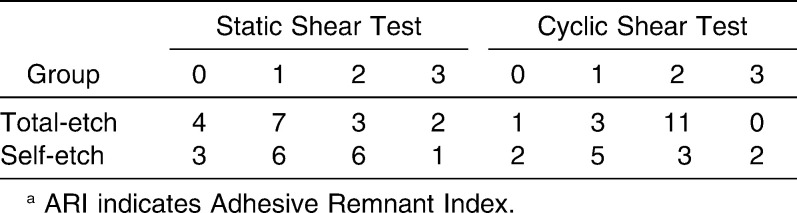
Adhesive Remnant Index
The raw ARI scores of shear tests for each group are reported in Table 2. The Mann- Whitney nonparametric test showed that there were no significant differences among the groups. From this data, all tested samples showed a predominance of ARI = 2 and ARI = 1.
Table 2.
Frequency Distribution of ARI Scores for the Test and Control Groupsa
DISCUSSION
The initial aim of this study was to compare the mean SSBS and mean CSBS of a self-etch bonding system to those of the total-etch one. The analyzed data and the results will be discussed in respect to three important aspects: cyclic fatigue resistance, clinical acceptability, and the ARI and enamel fracture potential.
Cyclic Fatigue Resistance
The effects of simulated occlusal forces on the bond strength are the most relevant part of this study. The fatigue resistance of both the total-etch and self-etch bonding system was compared to that of the static counterpart. When comparing the means between the static and cyclic groups, the mean CSBS of the total-etch was 24.07 MPa and that of the self-etch was 18.92 MPa, which were approximately 70.6% and 76.8% of their mean SSBS, respectively. This clearly indicates that cyclic fatigue tests produce results that are much lower than their static counterpart. Drummond et al.17,18 reported even lower ratios when comparing cyclic to static loading. They reported ratios of 51% for their tests of primed composite resin adhesion and 60% for compressive strengths of porcelain bars. Therefore, it would seem to indicate that both the total-etch and self-etch systems have good fatigue resistance. Clinically this may be very important, since intraoral forces are of a repetitive nature, and materials that perform well under fatiguing conditions should do better in such an environment.
Clinical Acceptability
The bond strength needed for bracket bonding is relatively low compared to the bond strength needed for bonding dental restorations to enamel or dentin. It has been reported that shear bond strengths of 17–20 MPa are required for optimal enamel or dentin bonding and retention of dental restorations.19 On the other hand, shear bond strengths of 6–8 MPa are reported to be adequate to withstand the forces generated by orthodontic wires while also allowing for the removal of brackets without causing damage to the enamel at the end of the treatment during the debonding procedure.20 It has also been reported that the minimum bond strength needed by a stainless steel bracket to be clinically acceptable is 2.86 MPa.21,22
The two bonding systems were compared to each other to evaluate the differences in the static and cyclic shear bond strengths. The self-etching group had a trend toward having lower bond strengths. Katona and Long23 found that the bond strength with the self-etch system was significantly (P = .029) stronger than with the total-etch system. However, this study was performed using a different protocol, including storage and loading methods.
The mean SSBS of the self-etch (24.64 ± 9.21) was significantly lower than that of the total-etch bonding system (34.25 ± 9.42). This is somewhat controversial as Buyukyilmaz et al.24 reported that conditioning with TBP before bonding orthodontic brackets to the enamel surface resulted in a significantly (P ≤ .001) higher SSBS (mean 16.0 ± 4.5 MPa) than that found in the total-etch group (mean 13.1 ± 3.1 MPa). In 2003, Dorminey et al.25 found no difference between total-etch (11.3 ± 2.2 MPa) and the self-etch bonding (11.9 ± 3.2 MPa). Arnold et al.26 also showed no significant difference between a total-etch system and the TBP self-etching system. Although the mean shear bond strength of self-etch in this study is significantly lower than that of total-etch, it is still higher than what has been reported in all previously mentioned studies.
Therefore, the hypothesis stating that the self-etch system will show similar SSBS in vitro when compared to the traditional total-etch system is not valid in this study. Statistically, the self-etch had lower mean shear bond strength than that of the total-etch system. Nevertheless, both of these values were within a clinically acceptable range.
The ARI and Enamel Fracture Potential
In the literature, it has been stated that it is desirable to have resin remnants on the tooth surface after bracket debonding to prevent enamel crazing or fracturing.20 Adhesive removal after debonding from teeth surfaces can be a difficult and time-consuming process that may cause enamel damage. The optimal adhesive should exhibit bond strengths strong enough to withstand orthodontic forces and the masticatory forces but provide easy removal after treatment without causing enamel damage.
From the results, it is evident that all samples performed without enamel fracture, and there were no significant differences between the bond failure sites of the total-etch and those of the self-etch bonding system. The sites of bond failure were mainly within the composite. Also, if fatigue testing shows a mean decrease in bond strength, then one can infer that the actual debonding force needed to remove orthodontic brackets after treatment will be less than what static bond strength tests report, because static tests are done without simulating the oral environment conditions previous to debonding. The ARI score results indicate that enamel fracture was not a problem during both static and cyclic shear testing method.
Future research is still needed in testing the self-etch bonding systems. Bond strengths obtained immediately (within 30 minutes) following the bonding procedure would probably be more representative of what is done clinically.
CONCLUSIONS
The results indicate that cyclic loading, simulating occlusal forces, have a significant impact on the bond strength of the self-etch bonding system. Cyclic fatigue tests produce results that are much lower than their static counterpart.
The self-etch bonding technique has lower shear bond strength values than those of the total-etch, but they are still clinically acceptable.
Acknowledgments
The research was completed at the College of Dentistry at the University of Illinois at Chicago. We would like to thank 3M Unitek for their generous donation of the materials used in this study.
REFERENCES
- 1.Buonocore M. G. A simple method of increasing the adhesion of acrylic filling materials to enamel surface. J Dent Res. 1955;34:849–853. doi: 10.1177/00220345550340060801. [DOI] [PubMed] [Google Scholar]
- 2.Newman G. V. Bonding plastic orthodontic attachments to tooth enamel. J New Jersey Dent Soc. 1964;35:346–358. [Google Scholar]
- 3.Gorelick L, Geiger A. M, Gwinnett A. J. Incidence of white spot formation after bonding and banding. Am J Orthod. 1982;81:93–98. doi: 10.1016/0002-9416(82)90032-x. [DOI] [PubMed] [Google Scholar]
- 4.Torii Y, Itou K, Hikasa R, Iwata S, Nishitani Y. Enamel tensile bond strength and morphology of resin-enamel interface created by acid etching system with or without moisture and self etching priming system. J Oral Rehab. 2002;29:528–533. doi: 10.1046/j.1365-2842.2002.00855.x. [DOI] [PubMed] [Google Scholar]
- 5.Brown C. R, Way D. C. Enamel loss during orthodontic bonding and subsequent loss during removal of filled and unfilled adhesives. Am J Orthod. 1978;74:663–671. doi: 10.1016/0002-9416(78)90005-2. [DOI] [PubMed] [Google Scholar]
- 6.Dierich P. Enamel alterations from bracket bonding and debonding: a study with scanning electron microscope. Am J Orthod Dentofacial Orthop. 1981;79:500–522. doi: 10.1016/s0002-9416(81)90462-0. [DOI] [PubMed] [Google Scholar]
- 7.Joseph V. P, Rossouw E. The shear bond strengths of stainless steel and ceramic brackets used with chemically and light-activated composite resins. Am J Orthod Dentofacial Orthop. 1990;97:121–152. doi: 10.1016/0889-5406(90)70084-P. [DOI] [PubMed] [Google Scholar]
- 8.Pashley D. H, Tay F. R. Aggressiveness of contemporary self-etching adhesives, part II: etching effects on unground enamel. Dent Mater. 2001;17:430–444. doi: 10.1016/s0109-5641(00)00104-4. [DOI] [PubMed] [Google Scholar]
- 9.Velo S, Carano A, Carano A. Self-etching vs. traditional bonding systems in orthodontics: an in vitro study. Orthod Craniofac Res. 2002;5:166–169. doi: 10.1034/j.1600-0544.2002.02193.x. [DOI] [PubMed] [Google Scholar]
- 10.Van Merbeek B, De Munck J, Yoshida Y, et al. Buonocore memorial lecture. Adhesion to enamel and dentine: current status and future challenges. Oper Dent. 2003;28:215–235. [PubMed] [Google Scholar]
- 11.Korbmacher H, Klocke A, Huck L, Kahl-Nieke B. Enamel conditioning for orthodontic bonding with a single-step bonding agent. J Orofac Orthop. 2002;63:463–471. doi: 10.1007/s00056-002-0130-5. [DOI] [PubMed] [Google Scholar]
- 12.Ruse N. D, Shew R, Feduik D. In vitro fatigue testing of a dental bonding system on enamel. J Biomed Mater Res. 1995;13:411–415. doi: 10.1002/jbm.820290316. [DOI] [PubMed] [Google Scholar]
- 13.Nakamichi I, Iwaku M, Fusayama T. Bovine teeth as possible substitutes in the adhesion test. J Dent Res. 1983;62:1076–1081. doi: 10.1177/00220345830620101501. [DOI] [PubMed] [Google Scholar]
- 14.Fowler C. S, Swartz M. L, Moore B. K, Rhodes B. F. Influence of selected variables on adhesion testing. Dent Mater. 1992;8:265–269. doi: 10.1016/0109-5641(92)90097-v. [DOI] [PubMed] [Google Scholar]
- 15.Drummond J. L, Racean D, Van Scoyoc J, Steinberg A. Effect of surface treatment on dentin bonding shear strength. Cells Mater. 1992;2:231–239. [Google Scholar]
- 16.Draughn R. A. Compressive fatigue limits of composite restorative materials. J Dent Res. 1979;58:1093–1096. doi: 10.1177/00220345790580031101. [DOI] [PubMed] [Google Scholar]
- 17.Drummond J. L, Van Scoyoc J. P, Racean D. C. Aging of ion exchanged porcelain. In: Fischman G, Clare A, Hench L, editors. Bioceramics Materials and Applications Ceramic Transactions Vol 48. Westerville, Ohio: The American Ceramic Society; 1995. pp. 191–200. [Google Scholar]
- 18.Drummond J. L, Sakaguchi R. L, Racean D. C, Wozny J, Steinberg A. D. Testing mode and surface treatment effects on dentin bonding. J Biomed Mater Res. 1996;32:533–541. doi: 10.1002/(SICI)1097-4636(199612)32:4<533::AID-JBM6>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 19.Davidson C. L, De Gee A. J, Feilzer A. The competition between the composite-dentin bond strength and polymerization contraction stress. J Dent Res. 1984;63:1396–1399. doi: 10.1177/00220345840630121101. [DOI] [PubMed] [Google Scholar]
- 20.Reynolds I. R. A review of direct orthodontic bonding. Br J Orthod. 1975;2:171–178. [Google Scholar]
- 21.Sharma-Sayal S. K, Rossouw P. E, Kulkarni G. V, Titley K. C. The influence of orthodontic bracket base design on shear bond strength. Am J Orthod Dentofacial Orthop. 2003;124:74–82. doi: 10.1016/s0889-5406(03)00311-1. [DOI] [PubMed] [Google Scholar]
- 22.Keizer S, Ten Cate J. M, Arends J. Direct bonding of orthodontic brackets. Am J Orthod. 1976;69:318–327. doi: 10.1016/0002-9416(76)90079-8. [DOI] [PubMed] [Google Scholar]
- 23.Katona T. R, Long R. W. Effect of loading mode on bond strength of orthodontic brackets bonded with 2 systems. Am J Orthod Dentofacial Orthop. 2006;129:60–64. doi: 10.1016/j.ajodo.2004.09.020. [DOI] [PubMed] [Google Scholar]
- 24.Buyukyilmaz T, Usumez S, Karaman A. I. Effects of self-etching primers on bond strength—are they reliable. Angle Orthod. 2003;73:64–70. doi: 10.1043/0003-3219(2003)073<0064:EOSEPO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.Dorminey J. C, Dunn W. J, Taloumis L. J. Shear bond strength of orthodontic brackets bonded with a modified 1-step etchant-and-primer technique. Am J Orthod Dentofacial Orthop. 2003;124:410–413. doi: 10.1016/s0889-5406(03)00404-9. [DOI] [PubMed] [Google Scholar]
- 26.Arnold R. W, Combe E. C, Warford J. H., Jr Bonding of stainless steel brackets to enamel with a new self-etching primer. Am J Orthod Dentofacial Orthop. 2002;122:274–276. doi: 10.1067/mod.2002.125712. [DOI] [PubMed] [Google Scholar]