Abstract
In just a few weeks, COVID-19 has become a global crisis and there is no longer any question of it being a major pandemic. The spread of the disease and the speed of transmission need to be squared with the forms and characteristics of economic globalization, disparities in development between the world’s different regions and the highly divergent degree of their interconnectedness. Combining a geographic approach based on mapping the global spread of the virus with the collection of data and socio-economic variables, we drew up an OLS model to identify the impact of certain socio-economic factors on the number of cases observed worldwide. Globalization and the geography of economic relations were the main drivers of the spatial structuring and speed of the international spread of the COVID-19.
Keywords: CoViD-19, Economic geography, World, Globalization, Spatial diffusion
Introduction
The increasing integration of the global economy has facilitated the interconnection between the world's territories. And globalization, characterized by the increase in human mobility and the exchange of goods throughout the world, can be considered a vector for the spread of epidemics and even pandemics (Berlinguer, 1999). The history of pandemics is a long one, and it is certainly not the first time that an infectious agent has spread across the globe. However, the most recent pandemics in historic terms appear to have been wiped from the collective memories. This helps to explain the widespread impression in the West that the current pandemic is exceptional, leading public and media reports to compare it with the “Spanish flu” of 1918–1919. Different factors account for the “forgotten” or otherwise overlooked pandemics: an available vaccination (Grippa A H1N1, 2009), initially linking the disease to what was believed to be a well-defined social group (SIDA, 1981), silent or almost silent media (Hong-Kong Flu in 1968–1970, Asian Flu 1956–1958), inadequate national resources to detect and record cases, the impression of a distant spatial threat (SARS-CoV, 2003) or an anthropological evolution that is often difficult to objectify (e.g., a shift in the relationship with death, lethal risks and mortality). It is nonetheless understandable that the danger represented by the SARS-COV-2 (WHO, 2020) has been seen as exceptional since, where almost a year was needed for the Spanish Flu to become a global pandemic, only three months was needed for Covid-19 to go global, and only two months for the main centers of globalization to be affected.
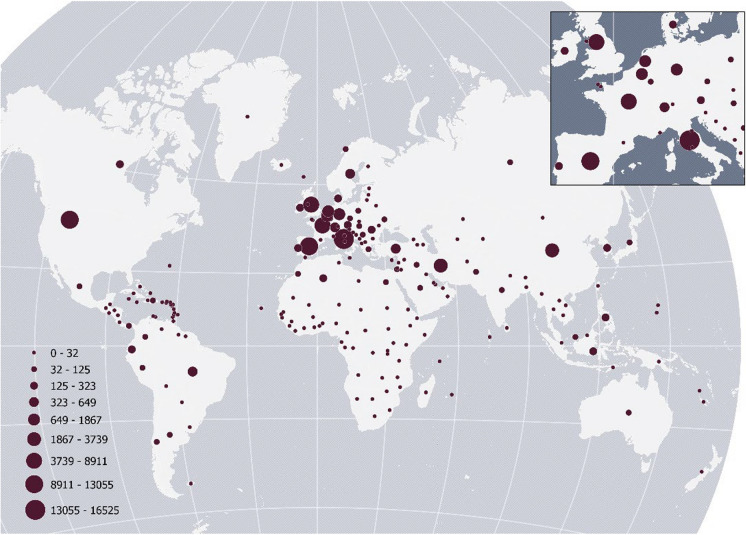
Indeed, as everyone feared from the moment the virus was first flagged in Wuhan (China) on 31 December 2019, the SARS-CoV-2 virus has now been transmitted worldwide (Al Hasan, 2020). While the global data available suffers from insurmountable problems (disparity in national institutions’ recording conditions, political agendas, unequal socio-economic effects in the identification and treatment of cases, etc.), it is nonetheless unquestionable that the virus has now escalated worldwide (Fig. 1). By 15 April 2020, 1,914,916 cases had been reported in over 180 countries or territories (194 member states of the WHO), with 123,010 deaths.
Fig. 1.
Number of deaths due to Covid-19 (7 Avril 2020)
Several previous studies have used mapping to analyze the spread of epidemics by highlighting “spatial patterns”. These include tuberculosis (Roth et al., 2016), cholera (Adesina, 1984; Ali et al., 2002), SARS-CoV (Lai et al., 2004; Meade, 2014; Shannon & Willoughby, 2004; Wang et al., 2008), MERS-CoV (Cotten et al., 2014), H1N1 influenza (Smallman-Raynor & Cliff, 2008; Souris et al., 2010), HIV (Wallace and Wallace, 1995; Wood et al., 2000) and dengue (Acharya et al., 2021; Atique et al., 2018; Zhu et al., 2019). In line with the approach of earlier studies, this paper attempts to analyze how the virus was transmitted across the globe and the underlying causes of its spread. We specifically interrogate how globalization has been a driver of the spatial diffusion of Covid-19.
In the rest of the paper, we present the methodology used. Then, we highlight our results before concluding and discussing the implications of our findings.
Method
Mapping epidemics and pandemics is a widely acknowledged method for understanding how they are transmitted and the factors that influence the spread (WHO, 2016). As Koch and Koch (2005) explain, using such techniques helps us to understand how to respond by being more prepared for health crises. In recent studies, it has been demonstrated that COVID-19 has primarly hit more developed regions (Bourdin et al., 2021; Paez et al., 2020). Therefore we have added in our model the GDP/capita which measures in a comparable way the levels of wealth of the States. In the same vein, in a context of globalisation where territories are interconnected (Michie, 2019), previous studies have shown that highly interconnected countries tend to be highly exposed in the event of an epidemic or pandemic (Hufnagel et al., 2004; Zou, 2016). Consequently, to understand the extent to which the spread of COVID-19 is due to economic globalization, we added a measure of trade intensity (intensity of commercial exchanges) for each country as an explanatory variable. Moreover, in medical geography (Meade, 2014; Dobis, 2020), health infrastructures have also been shown to play a role in the number of cases recorded in the epidemics observed. Therefore, we added two covariates relatives to health infrastructure: the density of beds and doctors.
At the global level, we only have access to data relative to the number of cases recorded, the number of deaths recorded and the number of recovered cases. We used the official data released by the WHO to inform our study, and we built a linear regression model (OLS) in order to complete our mapping analysis. Our model can be written as follow:
where represents the number of cases or the number of deaths;, are the parameters of the model (in italic in Table 1); and represents the error term.
Table 1.
Description of the variables
| Variable | Date of data | Source of data |
|---|---|---|
| Number of cases on 7/4/2020 | 7/4/2020 | World Health Organization |
| Number of deaths on 7/4/2020 | 7/4/2020 | World Health Organization |
| GDP/capita | 2018 | World Bank |
| Intensity of commercial exchanges (exports of goods and services in constant dollars) | The most recent value between 2016 and 2019 | World Bank |
| Number of doctors per 1000 inhabitants | The most recent value between 2016 and 2019 | World Bank |
| Number of beds per 1000 inhabitants | The most recent value between 2016 and 2019 | World Bank |
Results
Understanding the spread of COVID-19: Between geographical and functional proximities
Mapping deaths due to Covid-19 worldwide until 7 Avril 2020 showed that the SARS-CoV-2 virus is active across the globe and, potentially, in all societies and human groups, with the possible exception of the most isolated regions (notably Africa, Asia and Amazonia). The pandemic situation is thus indisputable, with some notable variations. In effect, Fig. 1 indicates that on 7 April 2020, the most severely affected regions in the world were the Extreme Orient, Europe and North America, with major infra-regional variations (especially between Western and Eastern Europe, and between the USA and Canada). Given what we now know about the exceptionally high degree of contagion, the average length of the incubation period (5/6 days and up to 14 days) and the very widespread potential of asymptomatic cases (Read et al., 2020; Ren et al., 2020; Wang et al., 2020), the global scale of diffusion makes it particularly challenging to eradicate the virus. This underscores the strategic importance of developing a vaccine in the fight against Covid-19 and the very high likelihood of resurgence (Table 2).
Table 2.
OLS model (7 April 2020)
| Model cases | Model deaths | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (1) | (2) | (3) | (4) | (5) | |
| Bed | − 0.182** | − 0125** | − 0.158 | − 0.112 | ||||||
| Doctor | 0.219*** | 0.195*** | 0.237** | 0.206** | ||||||
| Exchanges | 0.080** | 0.118** | 0.115** | 0.156** | ||||||
| GDP | 0.784*** | 0.768*** | 0.417*** | 0.485*** | ||||||
| R | 0.742 | 0.63 | 0.59 | 0.48 | 0.61 | 0.31 | 0.36 | 0.48 | 0.46 | 0.58 |
| Log likehood | − 72.258 | − 74.71 | − 77.16 | − 74.17 | − 76.62 | − 59.55 | − 59.34 | − 59.13 | − 58.84 | − 58.63 |
| AIC | 3284.7 | 3272.22 | 3259.74 | 3247.26 | 3234.78 | 2516.48 | 2391.46 | 2266.44 | 2394.49 | 2269.47 |
Overexposure to the epidemic of countries most deeply embedded in economic globalization
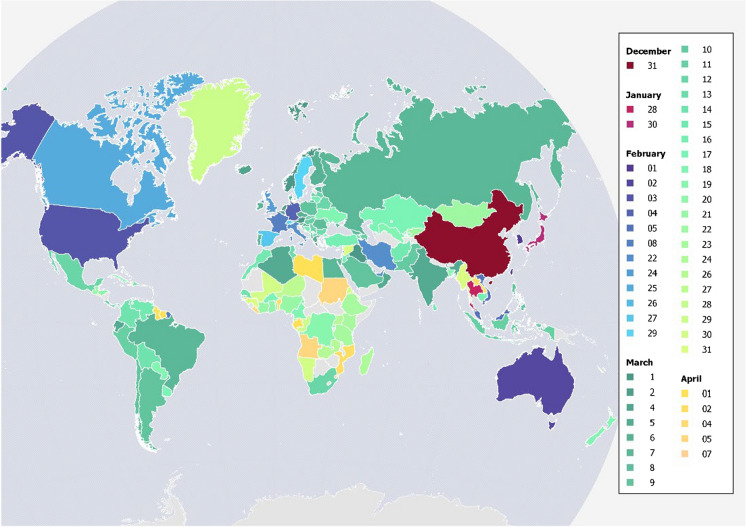
The pandemic spread across the globe in the space of 4 months. The main stages of the spatial spread of the virus closely follow the economic geography of today’s economic world. Thus, the spread of SARS-CoV-2 over space and time appears to provide considerable information about the main mechanisms at work (Fig. 2).
Fig. 2.
The global spread of Covid-19 from December 2019 (date when the threshold of ten cases was exceeded)
Three countries (Thailand, South Korea and Japan) reported their first cases quickly after the first case identified in Wuhan (16th of November 2019), at the end of January 2020. Taiwan followed suit on 1 February 2020. These are countries that, given their geographical proximity to the Chinese city where the epidemic first broke out, have frequent face-to-face interactions with Chinese interlocuters compared to more distant spatially countries where the cost of transport (both financial and temporal) to enact a physical encounter reduces the frequency of face-to-face interactions. Other countries in South-East Asia whose economies are linked to that of China and which have large Chinese diasporas were also affected (e.g., Vietnam, Malaysia).
When we analyse the Fig. 2, the case of Iran and the United Arab Emirates in the Middle East is more curious. However, one reason the United Arab Emirates has been affected could be to do with its positioning as an intercontinental air hub, with many commercial flights making a stopover between Europe and Asia. Iran, on the other hand, has enjoyed commercial and industrial relations with China linked to the oil sector for many years. March 2020 witnessed the spatial expansion of the epidemic to Latin America, South Asia, Eastern Europe (affected later than Western Europe) and Russia, as well as several regions in Africa. Regarding Russia, the relative lateness of the epidemic, while the country has borders with China, could be related to the geography of the country—so wide that the face-to-face interactions between Russians people from West to East is not so frequent (Sardadvar & Vakulenko, 2020), and the location of the Wuhan area, quite far from the China-Russia border.
Besides, we can clearly see that the countries most directly linked to China economically are generally the richest and most developed nations, and these were the first to see a rapid rise in cases. In the table, we observe a positive and significant effect of the level of development on the number of cases. In addition, the extent of a country's participation in international trade as measured by trade intensity has a positive and significant effect on the number of cases. From this point of view, we can say that the very rapid planetary spread of the pandemic was driven by the reticular links of “functional proximity” woven by economic globalisation between territories that are often geographically very distant from one another but associated, and therefore articulated and interdependent. Countries that were heavily hit at the beginning of the crisis are countries where business and trade relations with China and between centers of economic globalization, of which they are part, lead to frequent mobilities of people engaged in Business activities: i.e., Western Europe, North America and Australia. For these countries, opportunities for interindividual exposure (mixing of people from different countries, transit, meetings, interconnection-supporting sites or simply co-presence) are far higher in globalized regions and cities than for populations in countries where economic globalization is less effective.
In our model, we also observe that there is a positive and significative effect of the level of healthcare system (proxied by the density of beds and doctors) on the number of cases. This result suggests that countries with the most cutting-edge healthcare systems present the highest number of infections. It may seem counterintuitive. But recent studies have shown that although the number of doctors and beds per capita was high, the scale of the epidemic meant that these high levels of health infrastructure were still insufficient. Furthermore, the overconfidence that developed countries had in their health systems had deleterious effects because they were ill-prepared for the coming wave (Rodríguez-Pose, & Burlina, 2021). They thought that the high level of health services would be sufficient to absorb the pandemic waves, but this was not the case (Gudi & Tiwari, 2020).
Thus, the spread of SARS-CoV-2 from the industrial city of Wuhan in China appears to be highly dependent on the spatial organization of economic globalization. What is generally considered as an (economic) advantage, in other words, being connected to the most intensive global economic flows, in this instance has become a component of direct and increased exposure to the risk of epidemic. In contrast, regions, economies and populations that are less exposed to economic globalization have been affected later and more slowly by the spatial spread of the Covid-19 epidemic. This illustrates the way economic globalization not only concerns the circulation of goods, but also an intense flow of people, the main factor in the transmission of the virus.
The speed of diffusion has led to the phenomenon that we began to observe at the end of March: the majority of regions affected include a large number of cases of infection requiring hospitalization and admission to intensive care units within a very short timeframe (a few weeks). Consequently, the hardest hit regions are all trying to obtain the same resources on the global marketplace more or less simultaneously: drugs and drug compounds, protective masks, protective medical gear, medical equipment (respirators, etc.), and so on. These directly concurrent demands, combined with their concentration due to the rapid onset of a large number of severe cases at the same time, inevitably leads to both economic and political tensions. The global production capacity for all this medical equipment cannot be increased with in such a pace to meet all the demands so quickly. The situation is made worse by the excessive concentration of production sites in China for much of the medical equipment needed, in addition to the fact that the country has had to compress a lot of this production which is based in the area where the epidemic first broke out, leading to many of its industrial activities slowing down or even stopping altogether (Ishida, 2020).
Increased risk and huge uncertainty for the least developed countries
These effects, linked to the speed of the spread of the epidemic, could be a major disadvantage for certain regions and countries that were less exposed in the initial stages of the global spread of SARS-CoV-2, but are also less well equipped and less able to ensure access to the medical equipment and drugs required. The present pandemic is thus likely to take a literally geo-economic turn of events as it leads to rivalry between national governments, themselves unequally able to deal with the issues affecting the health interests of their respective populations. The resulting economic and political tensions linked to access to medical resources between developed countries should be seen as a warning sign and a potentially aggravating factor with regard to the pandemic developing in Africa, Asia (Middle East, South Asia, Central Asia) and Latin America.
However, it is difficult to build a true picture as there is a lack of reliable epidemiological information on the different ways that populations respond to or will respond to the SARS-CoV-2 infection. Africa serves as a good illustration in this respect. While, on the one hand, the continent seems particularly lacking in equipment (hospitals, number of beds, amount of medical equipment available, etc.) and in political resources to deal with the risk of the spread of Covid-19, it is difficult to factor in other variables: relative youth of the population in face of a virus where the most severe cases appear to lead to death in patients over 65 years old (according to what has been observed in Europe); populations exposed to specific combinations of medical treatments and health-related environments; lessons learned from previous epidemics (Ebola, 2013–2016 in West Africa, for example), to name just a few.
Despite these reserves, temporality seems to be a fundamental and even decisive aspect of pandemics and their final impact healthwise. In effect, the rapid transmission of infection leading to numerous severe cases that require highly specific equipment in a very short space of time is bound to be an aggravating factor in view of the challenges involved in getting access to medical equipment. As we have seen, the rapidity of the spread is due to an epidemiological issue (the extreme contagiousness of the virus and the absence of an immune system barrier because of its novelty) combined to a specific geo-economic context (connectivity between major centers of economic globalization). Without these factors, the Covid-19 pandemic would not have had the same impact and would probably not have generated the same sense of urgency or such a major crisis. This is aggravated by the fact that the original outbreak just happened to be in one of the major production centers of goods that are now in global demand.
These considerations help us to understand that the kinetics of the spatial spread of SARS-CoV-2 across the globe need to be supplemented by other analytical frameworks to examine the issue on other scales. Thus, if we observe the process at European scale (excluding Russia), the different regional responses to the epidemic become much clearer. Not only do countries become affected at different times, as illustrated by the factors put forward above, but the national kinetics also appear to vary significantly. This suggests that within each country, the diffusion of SARS-CoV-2 does not occur at the same speed. This is all the more interesting in that Europe, compared to other regions of the world, is characterized by the existence of a regional integration institution, the European Union, and integrated, partner economies.
Finally, the temporal dimension of the pandemic has another consequence linked to the speed of its spread and so to multiple temporal coincidences between national crises: when the epidemic spreads to African countries, western and developed countries, including China, have been still in a crisis themselves and will not be able to help, support or provide additional resources which they can generally offer.
Conclusion
Covid-19, the first real pandemic of globalization?
The present Covid-19 pandemic could thus be considered as the first real pandemic of the age of globalization since it effectively combines certain underlying characteristics: global scale, extremely fast speed of transmission, cross effects of global interterritorial interdependencies, interdependence of nations in the management of their respective epidemics and growing complexity in the spatial organisation of economic globalization.
The speed of the spatial spread of SARS-CoV-2 appears to be largely due to the reciprocal economic integration of major economic globalization centers. The counterpart to this integration is the ever-growing rise in the circulation of goods and, above all, people for economic and tourism purposes over the last thirty years. The Covid-19 pandemic has now challenged this international spatial mobility of people. The interruption of the hypermobility inherent in globalization, and often even of mobility itself with confinements, has led to an unprecedented development of telework (Belzunegui-Eraso & Erro-Garcés, 2020), as if, under the constraint of Covid-19, the preference for proximity has overtaken that for mobility. The geography of mobility is reduced to its vital minimum. This is evidenced by the thousands of closed hotels (and restaurants) that have been closed with the lockdowns implemented in many countries around the world (Škare et al., 2021). And better still by the provision of thousands of unoccupied hotel rooms to caregivers whose homes are far from their hospitals or for people in precarious situations impacted by the crisis (Kirby, 2020).
In this respect, health risks and economic risks are dramatically interwoven, each having a major impact on the other in terms of public decision-making processes. The high economic cost of such measures may effectively give rise to neo-Darwinian approaches, in contrast to current thinking about public health and each individual’s right to health. And yet it is this right of each human being to healthcare which underpinned article 25 of the Universal Declaration of Human Rights.
Finally, the speed of the global spread of SARS-CoV-2 underpins and strengthens the need for a coordinated and far more integrated international response. However, this is not what we have observed to date, especially in the face of a “new” virus about which we lacked precise knowledge. It is therefore essential to drastically step up research in two directions:
First and foremost, medical and biological research in order to gain a better understanding of infectious agents liable to provoke such pandemics;
Second, Humanities and Social Science for a better understanding of social and organizational behaviors in the framework of a health crisis of this extent. Indeed, one thing the Covid-19 pandemic has shown is the extreme challenges of getting affected populations or those liable to be affected to adopt the new behaviors required in so little time and on such a scale.
For a pandemic like Covid-19, it seems that medical solutions need to closely tie in with organizational, behavioral and, no doubt, cultural solutions.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations
Conflict of interest
We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
Ethical approval
We confirm that the manuscript has been read and approved by all named authors. We confirm that the order of authors listed in the manuscript has been approved by all named authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Acharya, K. P., Subramanya, S. H., & Neupane, D. (2021). Emerging pandemics: Lesson for one-health approach. Veterinary Medicine and Science, 7(1), 273. [DOI] [PMC free article] [PubMed]
- Adesina HO. Identification of the cholera diffusion process in Ibadan, 1971. Social Science & Medicine. 1984;18(5):429–440. doi: 10.1016/0277-9536(84)90059-5. [DOI] [PubMed] [Google Scholar]
- Al Hasan SM, Saulam J, Kanda K, Hirao T. The Novel Coronavirus Disease (COVID-19COVID-19) Outbreak Trends in Mainland China: A Joinpoint Regression Analysis of the Outbreak Data from January 10 to February 11, 2020. Bulletin of WHO; 2020. [Google Scholar]
- Ali M, Emch M, Donnay JP, Yunus M, Sack RB. The spatial epidemiology of cholera in an endemic area of Bangladesh. Social Science & Medicine. 2002;55(6):1015–1024. doi: 10.1016/S0277-9536(01)00230-1. [DOI] [PubMed] [Google Scholar]
- Atique, S., Chan, T. C., Chen, C. C., Hsu, C. Y., Iqtidar, S., Louis, V. R., ⋯, & Chuang, T. W. (2018). Investigating spatio-temporal distribution and diffusion patterns of the dengue outbreak in Swat, Pakistan. Journal of Infection and Public Health,11(4), 550–557. [DOI] [PubMed]
- Belzunegui-Eraso A, Erro-Garcés A. Teleworking in the context of the Covid-19 crisis. Sustainability. 2020;12(9):3662. doi: 10.3390/su12093662. [DOI] [Google Scholar]
- Berlinguer G. Globalization and global health. International Journal of Health Services. 1999;29(3):579–595. doi: 10.2190/1P5R-QV3M-2YHH-JN3F. [DOI] [PubMed] [Google Scholar]
- Bourdin S, Jeanne L, Nadou F, Noiret G. Does lockdown work? A spatial analysis of the spread and concentration of Covid-19Covid-19 in Italy. Regional Studies. 2021 doi: 10.1080/00343404.2021.1887471. [DOI] [Google Scholar]
- Cotten, M., Watson, S. J., Zumla, A. I., Makhdoom, H. Q., Palser, A. L., Ong, S. H., ⋯, Albarrak, A. (2014). Spread, circulation, and evolution of the Middle East respiratory syndrome coronavirus. MBio,5(1), e01062–13. [DOI] [PMC free article] [PubMed]
- Gudi SK, Tiwari KK. Preparedness and lessons learned from the novel coronavirus disease. The International Journal of Occupational and Environmental Medicine. 2020;11(2):108. doi: 10.34172/ijoem.2020.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishida S. Perspectives on supply chain management in a pandemic and the post-COVID-19 era. IEEE Engineering Management Review. 2020;48(3):146–152. doi: 10.1109/EMR.2020.3016350. [DOI] [Google Scholar]
- Hufnagel L, Brockmann D, Geisel T. Forecast and control of epidemics in a globalized world. Proceedings of the National Academy of Sciences. 2004;101(42):15124–15129. doi: 10.1073/pnas.0308344101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby T. Efforts escalate to protect homeless people from COVID-19 in UK. The Lancet Respiratory Medicine. 2020;8(5):447–449. doi: 10.1016/S2213-2600(20)30160-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koch T, Koch T. Cartographies of Disease: Maps, Mapping, and Medicine. Esri Press; 2005. p. 840. [Google Scholar]
- Lai PC, Wong CM, Hedley AJ, Lo SV, Leung PY, Kong J, Leung GM. Understanding the spatial clustering of severe acute respiratory syndrome (SARS) in Hong Kong. Environmental Health Perspectives. 2004;112(15):1550–1556. doi: 10.1289/ehp.7117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meade MS. Medical geography. In: Cockerham WC, editor. The Wiley Blackwell Encyclopedia of Health, Illness, Behavior, and Society. Wiley; 2014. pp. 1375–1381. [Google Scholar]
- Michie J, editor. The Handbook of Globalisation. Edward Elgar Publishing; 2019. [Google Scholar]
- Paez A, Lopez FA, Menezes T, Cavalcanti R, Pitta MGDR. A spatio-temporal analysis of the environmental correlates of COVID-19 incidence in Spain. Geographical Analysis. 2020 doi: 10.1111/gean.12241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read, J. M., Bridgen, J. R., Cummings, D. A., Ho, A., & Jewell, C. P. (2020). Novel coronavirus 2019-nCoV: early estimation of epidemiological parameters and epidemic predictions. medRxiv. [DOI] [PMC free article] [PubMed]
- Ren, L. L., Wang, Y. M., Wu, Z. Q., Xiang, Z. C., Guo, L., Xu, T., ⋯ & Fan, G. H. (2020). Identification of a novel coronavirus causing severe pneumonia in human: a descriptive study. Chinese Medical Journal,133, 1015–1024 [DOI] [PMC free article] [PubMed]
- Rodríguez-Pose A, Burlina C. Institutions and the uneven geography of the first wave of the COVID-19 pandemic. Journal of Regional Science. 2021;61:728–752. doi: 10.1111/jors.12541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sardadvar S, Vakulenko E. Estimating and interpreting internal migration flows in Russia by accounting for network effects. Socio-Economic Planning Sciences. 2020;69:100685. doi: 10.1016/j.seps.2019.01.007. [DOI] [Google Scholar]
- Shannon GW, Willoughby J. Severe acute respiratory syndrome (SARS) in Asia: A medical geographic perspective. Eurasian Geography and Economics. 2004;45(5):359–381. doi: 10.2747/1538-7216.45.5.359. [DOI] [Google Scholar]
- Škare M, Soriano DR, Porada-Rochoń M. Impact of COVID-19 on the travel and tourism industry. Technological Forecasting and Social Change. 2021;163:120469. doi: 10.1016/j.techfore.2020.120469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smallman-Raynor M, Cliff AD. The geographical spread of avian influenza A (H5N1): Panzootic transmission (December 2003–May 2006), pandemic potential, and implications. Annals of the Association of American Geographers. 2008;98(3):553–582. doi: 10.1080/00045600802098958. [DOI] [Google Scholar]
- Souris M, Gonzalez JP, Shanmugasundaram J, Corvest V, Kittayapong P. Retrospective space-time analysis of H5N1 Avian Influenza emergence in Thailand. International Journal of Health Geographics. 2010;9(1):3. doi: 10.1186/1476-072X-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace, R., & Wallace, D. (1995). US apartheid and the spread of AIDS to the suburbs: A multi-city analysis of the political economy of spatial epidemic threshold. Social Science & Medicine, 41(3), 333–345. [DOI] [PubMed]
- Wang, D., Hu, B., Hu, C., Zhu, F., Liu, X., Zhang, J., ... & Zhao, Y. (2020). Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. Jama. [DOI] [PMC free article] [PubMed]
- Wang JF, Christakos G, Han WG, Meng B. Data-driven exploration of ‘spatial pattern-time process-driving forces’ associations of SARS epidemic in Beijing, China. Journal of Public Health. 2008;30(3):234–244. doi: 10.1093/pubmed/fdn023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood E, Chan K, Montaner JS, Schechter MT, Tyndall M, O’Shaughnessy MV, Hogg RS. The end of the line: Has rapid transit contributed to the spatial diffusion of HIV in one of Canada’s largest metropolitan areas? Social Science & Medicine. 2000;51(5):741–748. doi: 10.1016/S0277-9536(99)00479-7. [DOI] [PubMed] [Google Scholar]
- World Health Organization . Mapping the Risk and Distribution of Epidemics in the WHO African Region Technical report. WHO; 2016. [Google Scholar]
- World Health Organization . Naming the Coronavirus Disease (COVID-19COVID-19) and the Virus That Causes It, Technical Guidance. WHO; 2020. [Google Scholar]
- Zhu G, Xiao J, Liu T, Zhang B, Hao Y, Ma W. Spatiotemporal analysis of the dengue outbreak in Guangdong Province, China. BMC Infectious Diseases. 2019;19(1):493. doi: 10.1186/s12879-019-4015-2. [DOI] [PMC free article] [PubMed] [Google Scholar]