Abstract
Food insecurity is associated with poor diet quality and increased diet-related disease risk. Food pantry clients (n=194) completed one 24-hour dietary recall and the Healthy Eating Index-2015 was used to evaluate diet quality. Differences in diet quality relative to participants’ last food pantry visit and self-reported ethnicity were evaluated using two-way ANOVA. Food pantry visits within 1–4 days compared to ≥5 days were associated with higher diet quality in non-Hispanics (p=0.01) but diet quality remained the same in Hispanics. Interventions to improve diet quality in food pantry users must consider potential ethnic differences when program planning.
Keywords: Diet quality, Healthy Eating Index, Food assistance, Food insecurity, Ethnicity
INTRODUCTION
Food insecurity, the lack of consistent access to sufficient amounts of safe and nutritious food, affected 11.1% of U.S. households in 2018.1 Food insecurity is associated with poor diet quality2,3 and a higher prevalence of diet-related disease4,5, and disproportionately burdens those living in poverty, rurally, and communities of color.1 Regional food banks serve as a safety net for food insecure households, collecting and redistributing donated, surplus, and subsidized food to a network of agency partner-operated food pantries and soup kitchens.6
Low diet quality (i.e., diets low in fruits and vegetables, nuts and seeds, and high in processed meats and trans fats) has been identified as the single greatest contributor to death from noncommunicable diseases.7,8 A systematic review evaluating the diet quality of food pantry users found overall diet quality fell far short of national recommendations, reflecting inadequate intake of fruits and vegetables, dairy products, and calcium.9 At the same time, studies conducted with food pantry clients have found positive associations between food pantry use and some aspects of diet quality.10,11 In an observational cohort study with dietary measurements taken before and after food pantry visits in the Midwest, Wright et al., found significant positive changes for total fruit servings (including 100% juice) and whole fruit, but no overall effects on diet quality.10 A cross-sectional study of Indiana food pantry clients found low overall diet quality, but significantly higher scores among those who visited a pantry more than once a month.11 These findings suggest a positive relationship between food pantry assistance and diet quality, emphasizing the importance of increased access to and support for food assistance programs to maintain the health of vulnerable populations. However, this and other related prior work in food pantries12,13 have primarily involved participants identifying as non-Hispanic White or Black, which is not representative of a growing majority of Americans, and may not reflect their experiences.
Nationally representative samples of children and adults participating in NHANES 2003–2004 suggest that diet quality differs substantially based on race/ethnicity, age, sex, income, and education level.14 In a 2003–2004 NHANES sample of adults, diet quality (assessed using the Healthy Eating Index 2005 (HEI-2005)) was significantly higher in Hispanics compared to non-Hispanic Blacks (HEI-2005 score of 59 versus 53 out of 100, p≤0.05) and to non-Hispanic Whites (HEI-2005 score of 59 versus 56 out of 100).14 Higher HEI-2005 score among Hispanics was attributed to greater reported intake of total fruit, dark green and orange vegetables and legumes, and lower intake of saturated fat and sodium compared to non-Hispanic Whites, and greater intake of milk, and lower intake of calories from solid fats, alcoholic beverages, and added sugars compared to non-Hispanic Blacks.14 Another analysis of NHANES data examined differences in level of food security and diet quality based on race and ethnicity in a sample of 4,393 low-income adults.15 Among non-Hispanic Whites, diet quality was higher in food secure compared to food insecure participants (HEI-2015 score of 53.1±1.5 versus 50.2±1.6, p=0.0002), yet there were no differences in diet quality based on level of food security in Hispanic adults.15 To our knowledge, only two studies have assessed the dietary intakes of food insecure Hispanic households who utilized food pantries16,17, and it is not clear whether racial/ethnic differences observed in nationally representative samples extend to this group, the fastest growing racial/ethnic minority in the United States who also experience almost two times the poverty rates of non-Hispanic Whites.18
To address this knowledge gap and generate actionable data to inform health-focused programs and policies at food banks and pantries, the University of Arizona and a regional food bank systematically evaluated diet quality, household health status, and measures of socioeconomic status in a sample of food bank clients. The regional food bank serves almost 200,000 individuals across 23,000 square miles; two-thirds of clients identify as Hispanic or Latino.19 In a recent client survey, 36% of respondents reported at least one family member with diabetes (Bedwell R, Renkert S, BARA Report on the Community Food Bank of Southern Arizona 2017 Client Survey, unpublished data, 2017), more than three times the national and state averages.20,21 In this same survey, 49% reported at least one family member with high blood pressure, and 41% indicated at least one family member with high cholesterol.
The objective of this study was to evaluate the relationship between the recent receipt of food pantry assistance and diet quality in this majority-Hispanic sample of food insecure adults living in the Southwest. Findings will guide food pantry programs and policies designed to improve diet quality and reduce the burden of diet-sensitive disease in ethnically diverse food insecure households.
METHODS
Setting, Participants, and Data Collection
This cross-sectional study was approved by the Institutional Review Board at the University of Arizona. Trained research assistants recruited 234 food bank clients from 3 food bank locations in Southern Arizona between June and December 2018 who provided written informed consent. The partner food bank serves clients directly at their main and satellite locations using a dedicated distribution (i.e., a food pantry). The three locations from which we recruited participants share the same distribution guidelines and food, obtained via two federal assistance programs: The Emergency Food Assistance Program (TEFAP), and the Commodity Supplemental Food Program (CSFP) for seniors aged 60 years and older. These two programs make up the majority of the food distributed by the food bank, and consist of primarily non-perishable items (e.g., dried and canned beans, canned vegetables, dried pasta, canned spaghetti sauce, dry ready-to-eat cereal, canned fruit in light syrup). A smaller proportion of food is obtained from local grocery store rescue and produce rescue from the port of entry in Nogales, Arizona, on the U.S.-Mexico border.22
Eligibility criteria included the ability to speak English or Spanish, ≥18 years old, having a U.S.-based telephone number, and visiting the food pantry from which they were recruited at least once in the preceding year to obtain food. A questionnaire was read aloud to each participant by the research assistant, prompting a verbal response to the following socioeconomic and health characteristics: age, gender, household size, race/ethnicity, number of household members with diabetes, high blood pressure, or high cholesterol, employment status, frequency of food pantry visits in the past year, and number and type of government benefits received. Participants could select more than one race/ethnicity. Participants who selected Hispanic ethnicity were considered Hispanic, while all others were grouped as non-Hispanic for analyses. Selection of the questionnaire characteristics was informed by prior research indicating relationships between these variables and diet quality.11,14,23 Participants completed one telephone-based 24-hour dietary recall administered by trained interviewers from the University of Arizona Behavioral Measurement and Interventions Shared Resource using the USDA multiple-pass methodology.24 A phone-based dietary recall was conducted to surmount time constraints and transportation challenges evident among low-income populations.25 During this interview, participants were also asked to provide the date on which they last received food at the food pantry location from which they were recruited. Study data were managed using REDCap.26 Participants received a $25 grocery store gift card for completing study activities.
Diet Quality
Diet data were summarized using the Nutrition Data System for Research (NDS-R) software, which provided intake estimates for 169 nutrients, nutrient ratios, and food servings.27,28 The HEI-2015 was used to determine the extent to which dietary intake of the study sample met the 2015–2020 Dietary Guidelines for Americans; this tool has been previously evaluated for content validity, construct validity, and reliability in diverse populations.14,29–31 The HEI-2015 consists of 13 individual nutrient components (total fruits, whole fruits, total vegetables, greens and beans, whole grains, dairy, total protein foods, seafood and plant proteins, fatty acids, refined grains, sodium, added sugars, and saturated fats) summed to create an index with a range from 0–100, with higher scores indicating higher diet quality.29 The National Cancer Institute’s Simple HEI scoring algorithm was used to generate scores for each component.32 Component scores were summed to calculate a total score for each individual, and a mean HEI score was generated for the entire sample. Sodium, added sugars, saturated fats, and refined grains have a negative impact on diet quality, and these components were scored so that higher numbers represented a lower (more desirable) intake.
Statistical Methods
Socioeconomic and health status differences were compared between those who indicated Hispanic ethnicity (n=130) and those who did not (n=64) using t-tests for continuous variables and Chi-square or Fisher’s exact tests for categorical variables. A t-test was first performed to compare differences in total diet quality by ethnicity (Hispanic versus non-Hispanic) and differences in total diet quality in participants who completed the dietary recall within one to four days of visiting the food pantry versus five or more days, as a typical emergency food package is designed to last four days. A two-way ANOVA was performed to determine differences in diet quality scores by the two dichotomous variables of ethnicity and number of days since last food pantry visit. An interaction term was included to determine whether the relationship between diet quality and the number of days between a participant’s last food pantry visit and interview date differed by ethnicity. The potential interaction between time since food was obtained and ethnicity was tested at the p<0.10 level rather than p<0.05 to adjust for the lower power to detect interactions versus main effects. If the interaction was found to be significant at p<0.10, t-tests were performed within each ethnicity to compare differences in diet quality by number of days since a participant’s last food pantry visit. Additional exploratory analyses using two-way ANOVA and t-tests were performed to identify potential interactions between, and differences within, each of the 13 individual components of diet quality in relation to number of days since food receipt, stratified by ethnicity. Assumptions of normality and constant variance were assessed using a histogram of error residuals and the Cook-Weisberg test for heteroskedasticity, respectively. Study retention was defined as the proportion of participants who completed all study activities, including informed consent, demographic data, and one 24-hour dietary recall interview conducted between one and four weeks after recruitment to the study. Alpha level was set to 0.05 for all analyses with the exception of testing a potential interaction. Statistical analyses were completed using Stata 16.0 (StataCorp., College Station, TX, 2019).
RESULTS
Of the 234 enrolled participants, 84.2% (n=197) completed the 24-hour dietary recall and provided socioeconomic and health data. Three participants had implausible values for the date between last food receipt and the dietary recall interview and were excluded, leaving 194 observations for analyses. Participant and household characteristics were summarized and stratified by ethnicity (Table 1). Participants’ ages ranged from 23 to 86 years, and they were majority female (77.8%, n=151) and Hispanic (67.0%, n=130). Forty-two percent (n=80) reported unemployment for all members of the household. Social services most frequently utilized were Medicaid (66.5%, n=121), Social Security (61.0%, n=111), Supplemental Nutrition Assistance Program (SNAP) (47.3%, n=86), and Medicare (46.2%, n=84). Forty percent of individuals (n=78) visited the food bank at least monthly (8.7 ± 5.7 visits in previous year, range: 1 to 24 times). Self-reported diet-sensitive conditions at the household level included high blood pressure 59.1% (n=114), high cholesterol 50.8% (n=98), and diabetes, 40.5% (n=77). Hispanic participants had a significantly larger household size (3.9 ± 2.1 versus 2.8 ± 2.0, p=0.0004) and greater use of Medicaid (73.0% versus 53.3%, p=0.01) compared to non-Hispanic participants. The number of participants without any household members employed was higher in non-Hispanic compared to Hispanic households (56.3% versus 34.9%, p=0.005). SNAP and Medicare use were also higher in non-Hispanic participants compared to Hispanic participants (58.3% versus 41.8%, p=0.04 and 61.7% versus 38.5%, p=0.004, respectively).
Table 1.
Demographic, Socioeconomic, and Health Characteristics of Study Participants Overall and Stratified by Ethnicity
| Overall (n=194) | Hispanic (n=130) | Non-Hispanic (n=64) | ||
|---|---|---|---|---|
|
| ||||
| Characteristics | Mean (SD) | Mean (SD) | Mean (SD) | p value |
| Participant Age, years | 56.6 (13.7) | 55.9 (14.0) | 58.0 (13.2) | 0.31 |
|
| ||||
| Household Size, number | 3.6 (2.1) | 3.9 (2.1) | 2.8 (2.0) | 0.0004 |
|
| ||||
| Frequency (%) | Frequency (%) | Frequency (%) | ||
|
| ||||
| Participant Gender | 0.95 | |||
| Female | 151 (77.8) | 101 (77.7) | 50 (78.1) | |
| Male | 43 (22.2) | 29 (22.3) | 14 (21.9) | |
|
| ||||
| Number of Household Members Employed | 0.005 | |||
| 0 | 80 (42.1) | 44 (34.9) | 36 (56.3) | |
| ≥1 | 110 (57.9) | 82 (65.1) | 28 (43.8) | |
|
| ||||
| Household Benefitsa | ||||
| AHCCCS/Medicaid | 121 (66.5) | 89 (73.0) | 32 (53.3) | 0.01 |
| Social Security | 111 (61.0) | 72 (59.0) | 39 (65.0) | 0.46 |
| SNAP/Food Stamps | 86 (47.3) | 51 (41.8) | 35 (58.3) | 0.04 |
| Medicare | 84 (46.2) | 47 (38.5) | 37 (61.7) | 0.004 |
| WIC | 11 (6.0) | 11 (9.0) | 0 (0.0) | 0.02 |
| Veterans Affairs | 9 (5.0) | 4 (3.3) | 5 (8.3) | 0.16 |
| Unemployment | 4 (2.2) | 3 (2.5) | 1 (1.7) | 0.60 |
| Other | 2 (1.1) | 2 (1.6) | 0 (0.0) | 1.0 |
|
| ||||
| Food Bank Visits in Past Year | 0.12 | |||
| 1 | 18 (9.3) | 13 (10.1) | 5 (7.8) | |
| 2–5 | 42 (21.8) | 22 (17.1) | 20 (31.3) | |
| 6–9 | 39 (20.2) | 30 (23.3) | 9 (14.1) | |
| 10–11 | 16 (8.3) | 13 (10.1) | 3 (4.7) | |
| ≥12 | 78 (40.4) | 51 (39.5) | 27 (42.2) | |
|
| ||||
| Household Health Conditionsb | ||||
| Diabetes | 0.18 | |||
| Yes | 77 (40.5) | 57 (44.9) | 20 (31.8) | |
| No | 111 (58.4) | 69 (54.3) | 42 (66.7) | |
| Unsure | 2 (1.1) | 1 (0.8) | 1 (1.6) | |
|
| ||||
| High Blood Pressure | 0.05 | |||
| Yes | 114 (59.1) | 83 (64.3) | 31 (48.4) | |
| No | 72 (37.3) | 43 (33.3) | 29 (45.3) | |
| Unsure | 7 (3.6) | 3 (2.3) | 4 (6.3) | |
|
| ||||
| High Cholesterol | 0.50 | |||
| Yes | 98 (50.8) | 68 (52.7) | 30 (46.9) | |
| No | 87 (45.1) | 57 (44.2) | 30 (46.9) | |
| Unsure | 8 (4.2) | 4 (3.1) | 4 (6.3) | |
SNAP- Supplemental Nutrition Assistance Program; AHCCCS- Arizona Health Care Cost Containment System; Missing data <5% except for household benefits (n=182); t-tests, Chi-square, or Fisher’s exact tests compared characteristics between Hispanic and Non-Hispanic ethnicity. Bolded text indicates statistical significance at p<0.05.
Households may select more than one benefit received, total n>182
Yes indicates ≥1 person in the household with a condition
The mean diet quality score across the sample was 52.6 ± 15.6. Seven of the thirteen components (total fruit, whole fruit, greens and beans, seafood and plant protein, dairy, fatty acids, and sodium) had a mean score of less than half of the maximum possible score. Total protein was the only component out of thirteen to near the maximum score. Sodium had the lowest score compared to its maximum, with a mean score of 3.1 ± 3.9 out of a maximum of 10.
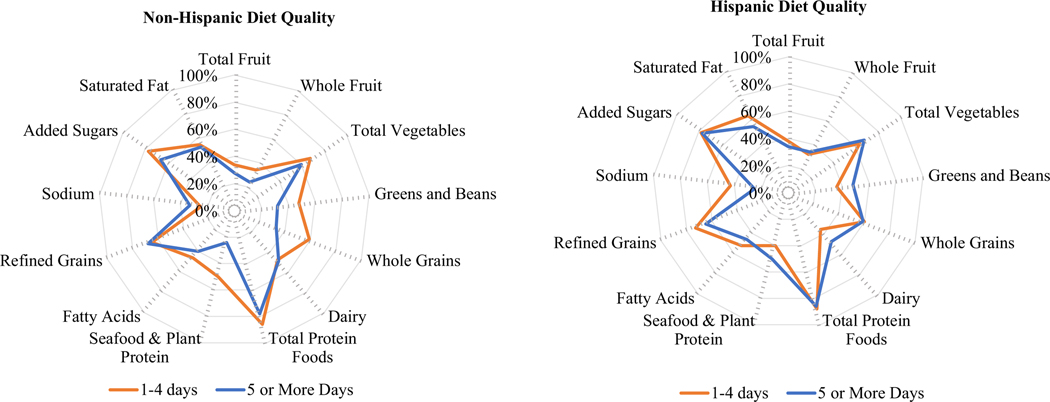
Total diet quality among Hispanic participants appeared higher compared to non-Hispanic participants (54.1 ± 15.3 versus 49.5 ± 15.8, p=0.052), and higher in participants who visited a food pantry within four days of their dietary recall interview compared to five or more days (56.0 ± 17.0 versus 51.2 ± 14.8, p=0.053). Using a two-way ANOVA, an interaction between the number of days since a food pantry visit and ethnicity was found to be significant at p=0.09, indicating that the association between the number of days since a food pantry visit and total diet quality differed by ethnicity. Within ethnic subgroup analyses stratified by number of days since a participant’s last visit to the food pantry, total diet quality of non-Hispanic participants was significantly higher when dietary recalls were obtained within 1 to 4 days of a food pantry visit compared with those who completed recalls 5 or more days after the last food pantry visit (57.1 ± 17.8 versus 46.5 ± 14.1, p=0.01, Table 2). This difference of higher diet quality scores within 1 to 4 days of a food pantry visit was also evident for the HEI components of total fruit, whole fruit, and added sugar. Hispanic participants who completed recalls within 1 to 4 days of a food pantry visit had higher HEI scores for sodium (indicating a favorable lower intake) compared to those completing recalls 5 or more days from a food pantry visit. An exploratory analysis of the 13 individual components of diet quality showed that the interaction between ethnicity and days since food receipt remained significant for total fruit (p=0.03), whole fruit (p=0.02), dairy (p=0.01), seafood and plant proteins (p=0.09), and added sugars (p=0.05). Figure 1 depicts diet quality component scores stratified by ethnicity and the number of days since a participant’s last food pantry visit.
Table 2.
Healthy Eating Index Scores, Overall, by Date of Most Recent Food Pantry Visit, and by Ethnicity
| Overall (n=194) | Hispanic (n=130) | Non-Hispanic (n=64) | ||||||
|---|---|---|---|---|---|---|---|---|
| Diet Quality Component (Minimum to maximum possible score) | 1–4 days since food receipt (n=37) | 5 or more days since food receipt (n=93) | p-value | 1–4 days since food receipt (n=18) | 5 or more days since food receipt (n=46) | p-value | p-value interaction | |
| Overall Diet Quality (0–100) | 52.6 (15.6) | 55.5 (16.9) | 53.5 (14.7) | 0.52 | 57.1 (17.8) | 46.5 (14.1) | 0.01 | 0.09 |
| Adequacy Components | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||
| Total Fruit (0–5)a | 1.8 (2.1) | 1.9 (2.2) | 1.7 (2.0) | 0.71 | 3.1 (2.2) | 1.4 (2.1) | 0.01 | 0.03 |
| Whole Fruit (0–5)b | 1.7 (2.3) | 1.6 (2.3) | 1.7 (2.2) | 0.80 | 2.9 (2.4) | 1.2 (2.1) | 0.01 | 0.02 |
| Total Vegetables (0–5)c | 3.3 (1.9) | 3.2 (1.8) | 3.4 (1.8) | 0.55 | 3.4 (1.9) | 3.0 (2.0) | 0.49 | 0.35 |
| Greens and Beans (0–5)c | 2.0 (2.4) | 1.8 (2.4) | 2.4 (2.4) | 0.20 | 1.9 (2.3) | 1.6 (2.3) | 0.63 | 0.25 |
| Whole Grains (0–10) | 5.2 (4.5) | 6.0 (4.3) | 5.9 (4.5) | 0.84 | 4.5 (4.5) | 3.3 (4.1) | 0.30 | 0.47 |
| Dairy (0–10)d | 4.8 (3.8) | 3.6 (3.2) | 4.8 (3.7) | 0.09 | 6.9 (3.8) | 4.9 (4.1) | 0.07 | 0.01 |
| Total Protein (0–5)c | 4.2 (1.5) | 4.4 (1.3) | 4.3 (1.3) | 0.76 | 4.3 (1.1) | 3.9 (1.9) | 0.43 | 0.55 |
| Seafood and Plant Protein (0–5)e | 2.1 (2.4) | 2.0 (2.4) | 2.5 (2.4) | 0.37 | 2.2 (2.5) | 1.2 (2.1) | 0.14 | 0.09 |
| Fatty Acids (0–10)f | 4.5 (3.7) | 5.2 (3.7) | 4.6 (3.6) | 0.43 | 3.9 (3.5) | 4.0 (4.1) | 0.96 | 0.63 |
| Moderation Components | ||||||||
| Refined Grains (0–10) | 6.7 (3.7) | 7.3 (3.7) | 6.5 (3.9) | 0.28 | 6.8 (3.9) | 6.8 (3.6) | 0.99 | 0.54 |
| Sodium (0–10) | 3.1 (3.9) | 4.3 (4.5) | 2.5 (3.6) | 0.02 | 3.2 (4.0) | 3.3 (4.1) | 0.92 | 0.16 |
| Added Sugars (0–10) | 7.5 (3.3) | 7.8 (3.2) | 7.7 (3.1) | 0.93 | 8.7 (2.0) | 6.6 (3.8) | 0.03 | 0.05 |
| Saturated Fat (0–10) | 5.6 (3.7) | 6.4 (3.7) | 5.5 (3.5) | 0.20 | 5.2 (3.2) | 5.3 (4.2) | 0.95 | 0.44 |
Two-way ANOVAs with an interaction term compared diet quality by ethnicity and days since last food receipt; t-tests were performed to determine differences within each ethnicity in overall and components of diet quality by days since last food receipt. Bolded text indicates statistical significance. Intakes between minimum and maximum standards are scored proportionately; all components are scored per 1,000kcal or percentage of energy, except for Fatty Acids; energy from alcohol is included in total energy intake
Includes 100% fruit juice
Includes all forms except juice
Includes legumes (beans and peas)
Includes all milk products, such as fluid milk, yogurt, and cheese, and fortified soy beverages
Includes seafood, nuts, seeds, soy products (other than beverages), and legumes (beans and peas)
Ratio of poly- and monounsaturated fatty acids to saturated fatty acids
Figure 1. Diet quality component scores stratified by ethnicity and number of days between dietary recall interview and last food pantry visit (within 1–4 days of dietary recall versus 5 or more days).
Each component score is scaled as a percentage of the maximum score of that component, with moderation components reversed coded in the scoring process, meaning a lower percentage in moderation components reflects high intake of that component relative to recommendations. A perfect HEI score (100% in each component) would be represented by the outermost line of the radar plot.
DISCUSSION
To our knowledge, this is the first study to evaluate potential differences in diet quality in an ethnically diverse sample of food pantry clients in relation to their last food pantry visit, and identify dietary components associated with these differences. The overall diet quality in our sample was low relative to a large and nationally representative sample in which diet quality was assessed (HEI score of 52.6 in our sample versus 58.7 in NHANES sample).33 However, when food security was assessed using USDA categories in multiple consecutive samples of low-income NHANES participants (1999–2008, n=8,129), our sample fared better than adults classified as very low food secure (multiple indications of disrupted eating patterns and reduced food intake in the past 12 months), HEI score of 52.6 versus 45.5.2 Two cross-sectional studies conducted in the Midwest with majority non-Hispanic participants reported that diet quality is higher immediately following food pantry visits (n=455)10, and with a greater number of food pantry visits each month (n=270).11 This is similar to what we observed in our study, wherein non-Hispanic participants who completed the 24-hour dietary recall within one to four days of a food pantry visit had a significantly higher diet quality compared to those who completed the recall five or more days after a food pantry visit. Further, non-Hispanic total and whole fruit intake was significantly higher, and added sugar intake significantly lower, when interviews were conducted within one to four days of visiting a food pantry. This may reflect immediate use of the perishable items provided by the food pantry which support higher diet quality (e.g., whole fruit) while non-perishable and processed foods high in added sugars may be saved for use until food pantry assistance runs out. To our knowledge, prior research has not directly measured how long food pantry assistance lasts after receipt. However, studies have assessed the use of SNAP benefits throughout the month, finding that benefits are often used within the first two weeks of receipt34 and as the number of days since SNAP benefits increase, the use of benefits decline and use of food pantries increase.35 Changes in food acquisition throughout the month is an area that deserves further research, especially in relation to diet quality, as both the quantity and quality of food may impact management of chronic diseases that are highly prevalent among food insecure populations.36 Ultimately, these findings indicate a potentially greater influence of food pantry assistance on diet quality components among non-Hispanic individuals with food insecurity and support a need for increased frequency or quantity of food distribution to improve access to nutritious foods that are otherwise challenging to acquire.
The same findings were not seen in Hispanic participants; indeed, those who visited a food pantry within one to four days of their dietary recall interview had similar diet quality compared to those who had interviews conducted five or more days after visiting a food pantry. One possible explanation for this could be due to traditional Hispanic dietary patterns being very similar to some of the food assistance provided by the food pantry (e.g., dried and canned beans, fruits).37,38 These dietary patterns have been attributed to a lower overall mortality rate compared to non-Hispanic Whites39, despite a higher prevalence of metabolic risk factors such as obesity40 and socioeconomic disadvantage18 (i.e., the ‘Hispanic paradox’). Increasing acculturation among Hispanics may negatively impact diet quality.38 Given that 52.9% of Hispanic participants in our study preferred Spanish for their dietary recall interview language (using language preference as a proxy for acculturation41), baseline intake of fruits and vegetables may already be greater and represent more traditional Hispanic dietary patterns.42,43 This observation may explain the lack of changes in diet quality upon a recent food pantry visit, and future researchers should consider assessing diet quality relative to acculturation and among diverse ethnic subgroups that may identify broadly as Hispanic. Hispanic participants in our study also reported significantly greater number of household members employed and a greater household size compared to non-Hispanic participants. It is possible that this additional income might provide slightly greater food security for households of Hispanic participants, allowing for food dollars to ‘stretch’ further over the month. However, a greater household size may also reflect a larger number of individuals in need of food. We did not formally assess food insecurity in this study; however, almost half of our sample reported visiting a food bank or pantry once or more per month in the past year, indicating significant need among participants – this did not differ by ethnicity.
Although not the focus of our research question, the interaction between ethnicity and time since last food pantry visit may alternatively be interpreted by first observing differences by last food pantry visit and then stratifying by ethnicity. Among all participants who last visited the food pantry within four days, diet quality was the same in Hispanics and non-Hispanics, while among participants who visited the food pantry more than five days from their interview date, diet quality was higher among Hispanics. However, we framed our interpretation of the interaction based on the gap identified in prior research regarding limited evaluation of food pantry use among Hispanic individuals in relation to diet quality. Given our findings that a recent food pantry visit may disproportionately be associated with higher diet quality among non-Hispanics, but not in Hispanics, another important area for future research includes understanding how diet quality may be related to the higher rates of both food insecurity and diet-related disease among Hispanics compared to non-Hispanic Whites.1,20 In Tucson, AZ, the median income among Hispanics is dramatically less than that of non-Hispanic Whites ($42,035 versus $57,619, respectively).44 This income inequality is also important to consider and indicates a need for a more livable wage that could also directly impact food insecurity and inform intervention strategies to reduce these disparities.
Understanding which foods or nutrients are contributing to differences in diet quality among food pantry clients can inform strategic adjustments to food pantry assistance and related resources in order to significantly impact disease risk. Seligman et al., conducted a pilot study and later a randomized controlled trial with food pantry clients who had type 2 diabetes, testing the effects of twice monthly food packages, referrals to providers, and diabetes self-management education on changes in hemoglobin A1c.16,17 The pilot study reported significant improvements in hemoglobin A1c from baseline to 6 months16; however, there were no differences in hemoglobin A1c from baseline to 6 months between the RCT intervention and control groups.17 Notably, the RCT study had a low participation rate (only 19.7% meeting criteria for full engagement) despite a retention rate of 72%, emphasizing the importance of understanding and addressing barriers to participation and engagement for low-resource or food insecure persons with diabetes or related diet-sensitive conditions, and working in partnership with clients and food pantry staff to ensure modifications to food assistance and related resources are culturally appropriate and responsive to challenges faced by clients. Given the high self-reported household prevalence of type 2 diabetes in our sample, and the established relationship between poor diet quality and diet-related disease risk,45,46 the food bank has prioritized organizational resources and efforts to help address health-related disparities in their clients, including strategies to enhance the quality of food provided to clients. Examples include increasing the nutrient density of emergency food packages, as well as supplementing with additional resources and education (e.g., culturally responsive recipes, cooking tools) to help clients utilize all the food they are provided. High sodium intake was a major HEI score-driving component among our entire sample. In light of data indicating the high sodium content of many of the foods provided to clients, the food bank has already worked to reduce the sodium in foods provided through the emergency food package by eliminating canned tomato soup and switching canned vegetables to lower sodium varieties.
Our study had several strengths. One was our retention rate (84.2%), which we attribute to the direct involvement of food bank staff in study recruitment activities, and the strong community-academic partnership that produced this work, which privileged the voices of food bank clients. Many of our participants expressed great interest and engagement in a study focused on nutrition and health, which may also have contributed to the high participation rate. Another strength was the diversity of our sample, particularly that a majority of study participants identified as Hispanic, an underrepresented minority in research focused on food insecurity and health which to date, has been conducted primarily with non-Hispanic populations.10,12,13
Our study also had some limitations. Although, data were collected from a diverse group of food bank clients, the results may not be generalizable to other food banks and pantries around the nation. Additionally, study eligibility criteria specified a home address and working U.S.-based phone number, potentially narrowing the pool of respondents to those who were higher income or more food secure. While we did not ask participants questions regarding food acquisition in their dietary recall interviews, given prior research showing immediate use of other food assistance programs upon receipt35, it is a reasonable assumption that individuals who utilize emergency food assistance from food pantries would consume a large proportion of recently acquired food upon receipt. Finally, since 24-hour dietary recalls rely on self-report, data collected using this method may be influenced by social desirability bias leading to under- or overreporting of intake.47,48
CONCLUSION
Our study provided new information about differences in overall diet quality and dietary components based on the number of days since a food pantry visit and ethnicity (Hispanic and non-Hispanic) in participants recruited from a regional food bank in the Southwest. Food pantry visits within 1–4 days compared to ≥5 days were associated with higher diet quality among individuals identifying as non-Hispanic, but diet quality was the same among Hispanics. Diet quality scores of non-Hispanic participants reflected higher intake of total fruit and whole fruit, and lower intake of added sugar when dietary recalls were completed within four days of visiting a food pantry, but not if interviews were completed after five or more days. Future research is needed to understand the findings in diet quality among Hispanics, including consideration of ethnic groups and acculturation, both of which are associated with diet quality and dietary patterns. In order to make a significant impact on diet quality and reduce the burden of diet-related disease in food insecure households, this work must also continue to engage food bank personnel and clients in the co-development of relevant, culturally-appropriate, and efficacious programs and policies based on this and future research.
Acknowledgements
Special thanks to the UA research assistants and staff, Martina Sepulveda, Jayati Sharma, Guadalupe Anaid Serrano, Angela Yung; the CFB staff, Jessica Sheava, Chris Mazzarella, Linda Hampton, Debby Acuna, Lilia Dawson, Brandi Smith; and, AmeriCorps VISTA Carol Tessein for their assistance.
Financial Support
Research reported in this publication was supported by the Community Food Bank of Southern Arizona; the National Cancer Institute of the National Institutes of Health (D.J.R., award number P30 CA023074); the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (E.S., D.J.R. and M.H., award number R34DK118486); the Department of Health and Human Services Health Resources Services Administration (D.T., Advanced Nurse Education – Sexual Nurse Assault Examiner Program grant number T96HP32508 and Western Region Public Health Training Center, grant number UB6HP31687). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Financial Conflicts of Interest Disclosure
D.T. is the Editor-in-Chief for Nutrition Reviews. All other authors have no financial conflicts of interest to report.
Data availability statement
Due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available.
REFERENCES
- 1.Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2018. U.S. Department of Agriculture, Economic Research Service. 2019:1–47. [Google Scholar]
- 2.Leung CW, Epel ES, Ritchie LD, Crawford PB, Laraia BA. Food insecurity is inversely associated with diet quality of lower-income adults. J Acad Nutr Diet. 2014;114:1943–1953. [DOI] [PubMed] [Google Scholar]
- 3.Hanson KL, Connor LM. Food insecurity and dietary quality in US adults and children: a systematic review. Am J Clin Nutr. 2014;100(2):684–692 [DOI] [PubMed] [Google Scholar]
- 4.Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J Gen Intern Med. 2007;22:1018–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140(2):304–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.America Feeding. What is a food bank? https://www.feedingamerica.org/our-work/food-bank-network. Accessed September 30th, 2020.
- 7.Mokdad AH, Ballestros K, Echko M, et al. The state of US health, 1990–2016: Burden of diseases, injuries, and risk factors among US states. JAMA. 2018;319(14):1444–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murray CJ, Atkinson C, Bhalla K, et al. The state of US health, 1990–2010: Burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simmet A, Depa J, Tinnemann P, Stroebele-Benschop N. The dietary quality of food pantry users: a systematic review of existing literature. J Acad Nutr Diet. 2017;117:563–576 [DOI] [PubMed] [Google Scholar]
- 10.Wright BN, Bailey RL, Craig BA, et al. Daily dietary intake patterns improve after visiting a food pantry among food-insecure rural Midwestern adults. Nutrients. 2018;10:583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu Y, Zhang Y, Remley DT, Eicher-Miller HA. Frequency of food pantry use is associated with diet quality among Indiana food pantry clients. J Acad Nutr Diet. 2019;119(10):1703–1712. [DOI] [PubMed] [Google Scholar]
- 12.Duffy P, Zizza C, Jacoby J, Tayie FA. Diet quality is low among female food pantry clients in Eastern Alabama. J Nutr Educ Behav. 2009;41:414–419. [DOI] [PubMed] [Google Scholar]
- 13.Robaina KA, Martin KS. Food insecurity, poor diet quality, and obesity among food pantry participants in Hartford, CT. J Nutr Educ Behav. 2013;45(2):159–164. [DOI] [PubMed] [Google Scholar]
- 14.Hiza HA, Casavale KO, Guenther PM, Davis CA. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. J Acad Nutr Diet. 2013;113:297–306. [DOI] [PubMed] [Google Scholar]
- 15.Leung CW, Tester JM. The Association between Food Insecurity and Diet Quality Varies by Race/Ethnicity: An Analysis of National Health and Nutrition Examination Survey 2011–2014 Results. J Acad Nutr Diet. 2019;119(10):1676–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Seligman HK, Lyles C, Marshall MB, et al. A pilot food bank intervention featuring diabetes-appropriate food improved glycemic control among clients in three states. Health Affairs (Project Hope). 2015;34:1956–1963. [DOI] [PubMed] [Google Scholar]
- 17.Seligman HK, Smith M, Rosenmoss S, Marshall MB, Waxman E. Comprehensive diabetes self-management support from food banks: A randomized controlled trial. Am J Public Health. 2018;108:1227–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Semega J, Kollar M, Creamer J, Mohanty A. Income and poverty in the United States: 2018. Current Population Reports. 2019:P60–266. [Google Scholar]
- 19.Community Food Bank of Southern Arizona. Our Service Area. https://www.communityfoodbank.org/Realities-of-Hunger/Facts-and-Figures/Our-Service-Area. Accessed September 30th, 2020.
- 20.Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017: Estimates of Diabetes and Its Burden in the United States. Atlanta, GA: Centers for Disease Control and Prevention. 2017:1–20. [Google Scholar]
- 21.Centers for Disease Control and Prevention. Prevelance of Self-reported Diagnosed Diabetes in Adults, Aged 18 Years or Older, Arizona. U.S. Department of Health & Human Services. 2013. [Google Scholar]
- 22.Community Food Bank of Southern Arizona. Our Work: Programs. https://www.communityfoodbank.org/Our-Work/Programs. Accessed September 17th, 2020.
- 23.Zhang FF, Liu J, Rehm CD, Wilde P, Mande JR, Mozaffarian D. Trends and disparities in diet quality among US adults by Supplemental Nutrition Assistance Program participation status. JAMA Network Open. 2018;1:e180237-e180237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moshfegh AJ, Rhodes DG, Baer DJ, et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr. 2008;88:324–332. [DOI] [PubMed] [Google Scholar]
- 25.George S, Duran N, Norris K. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am J Public Health. 2014;104(2):e16–e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nutrition Coordinating Center UoM. Guide to Creating Variables, Needed to Calculate Scores for Each Component of the Healthy Eating Index-2015 (HEI-2015). 2017; http://www.ncc.umn.edu/healthy-eating-index-hei/. Accessed September 30th, 2020.
- 28.NDS-R Versions 2017 & 2018. [computer program]. Minneapolis, MN: Nutrition Coordinating Center. [Google Scholar]
- 29.Krebs-Smith SM, Pannucci TE, Subar AF, et al. Update of the Healthy Eating Index: HEI-2015. J Acad Nutr Diet. 2018;118:1591–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reedy J, Lerman JL, Krebs-Smith SM, et al. Evaluation of the healthy eating index-2015. J Acad Nutr Diet. 2018;118(9):1622–1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schap T, Kuczynski K, Hiza H. Healthy Eating Index-Beyond the Score. J Acad Nutr Diet. 2017;117(4):519–521. [DOI] [PubMed] [Google Scholar]
- 32.National Cancer Institute. Healthy Eating Index: Overview of the Methods & Calculations. https://epi.grants.cancer.gov/hei/hei-methods-and-calculations.html. Accessed September 30th, 2020.
- 33.National Center for Health Statistics. Healthy Eating Index-2015 Scores. What We Eat in America/National Health and Nutrition Examination Survey, 2015–2016. https://www.fns.usda.gov/hei-scores-americans. Accessed September 30th, 2020.
- 34.Smith TA, Berning JP, Yang X, Colson G, Dorfman JH. The effects of benefit timing and income fungibility on food purchasing decisions among Supplemental Nutrition Assistance Program households. Am J Agric Econ. 2016;98(2):564–580. [Google Scholar]
- 35.Fan L, Gundersen C, Baylis K, Saksena M. The use of charitable food assistance among low-income households in the United States [published online ahead of print, Sep 18 2020]. J Acad Nutr Diet. doi: 10.1016/j.jand.2020.07.026 [DOI] [PubMed] [Google Scholar]
- 36.Gucciardi E, Vahabi M, Norris N, Del Monte JP, Farnum C. The intersection between food insecurity and diabetes: A review. Curr Nutr Rep. 2014;3(4):324–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Winham DM, Tisue ME, Palmer SM, Cichy KA, Shelley MC. Dry bean preferences and attitudes among Midwest Hispanic and non-Hispanic white women. Nutrients. 2019;11(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Batis C, Hernandez-Barrera L, Barquera S, Rivera JA, Popkin BM. Food acculturation drives dietary differences among Mexicans, Mexican Americans, and non-Hispanic whites. J Nutr. 2011;141(10):1898–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McDonald JA, Paulozzi LJ. Parsing the paradox: Hispanic mortality in the US by detailed cause of death. J Immigr and Minor Health. 2019;21(2):237–245. [DOI] [PubMed] [Google Scholar]
- 40.Kurian AK, Cardarelli KM. Racial and ethnic differences in cardiovascular disease risk factors: a systematic review. Ethn Dis. 2007;17(1):143. [PubMed] [Google Scholar]
- 41.Kirkman-Liff B, Mondragón D. Language of interview: relevance for research of southwest Hispanics. Am J Public Health. 1991;81(11):1399–1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Reininger B, Lee M, Jennings R, Evans A, Vidoni M. Healthy eating patterns associated with acculturation, sex and BMI among Mexican Americans. Public Health Nutr. 2017;20(7):1267–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Di Noia J, Monica D, Cullen KW, Pérez-Escamilla R, Gray HL, Sikorskii A. Differences in fruit and vegetable intake by race/ethnicity and by Hispanic origin and nativity among women in the Special Supplemental Nutrition Program for Women, Infants, and Children, 2015. Prev Chronic Dis. 2016;13:E115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Making Action Possible for Southern Arizona. Economy, Median Houshold Income 2018. https://mapazdashboard.arizona.edu/economy/median-household-income. Accessed September 28, 2020.
- 45.Ley SH, Pan A, Li Y, et al. Changes in overall diet quality and subsequent type 2 diabetes risk: Three U.S. prospective cohorts. Diabetes Care. 2016;39(11):2011–2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sotos-Prieto M, Bhupathiraju SN, Mattei J, et al. Changes in diet quality scores and risk of cardiovascular disease among US men and women. Circulation. 2015;132(23):2212–2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Taren DL, Tobar M, Hill A, et al. The association of energy intake bias with psychological scores of women. Eur J Clin Nutr. 1999;53:570–578. [DOI] [PubMed] [Google Scholar]
- 48.Thompson FE, Subar AF. Dietary assessment methodology. In: Nutrition in the Prevention and Treatment of Disease. Elsevier; 2017:5–48. [Google Scholar]