Abstract
Remote schooling due to COVID-19 created profound challenges for families. In this investigation, we examined parents’ depression and anxiety during remote schooling and their associations with parents’ reports of school support. We also evaluated indirect and interactive (i.e., moderation) associations. Participants were parents (N = 152, 92.8% mothers, 65.1% Black) from an urban area with high rates of COVID-19. Of the 152 parents, 27.6% reported elevated levels of depression and 34.2% reported elevated anxiety. Regression analyses showed that school support was negatively associated with parents’ depression (β = −.33, p < .01) and anxiety (β = −.21, p < .01). There was an indirect association between school support and parents’ mental health via household chaos and daily routines. Reported COVID-19 impact moderated the direct association between school support and parental depression and anxiety. There was a statistically significant association between school support and parents’ depression and anxiety when COVID-19 impact was low or moderate, but not when COVID-19 impact was high. These results may suggest that for parents who were not highly impacted by the pandemic, school support buffered the association between stress and parents’ mental health problems; parents most impacted by COVID-19 may need additional support.
Keywords: Parents’ mental health, school support, COVID-19
The COVID-19 pandemic, with significant rates of worldwide infection and death, along with concomitant mitigation efforts, have had an unprecedented global impact on families. The World Health Organization (WHO) declared COVID-19 a pandemic on March 1, 2020 as the virus spread across the globe. By mid-March, shelter-in-place orders were enacted in the United States (US), resulting in closure of school buildings, child care centers, work places, and community programs. Many adults were forced to shift to working from home, and others experienced job loss and economic burdens. Rates of unemployment in the US were the highest since the Great Depression (Falk et al., 2021).
During the COVID-19 pandemic, working parents were confronted with the additional burden of attempting to balance their professional lives, while also taking on the role of promoting their children’s remote schooling and well-being. This disruption of daily schedules created significant upheaval that impacted families, including parents’ mental health. In addition, the social and community supports that parents typically rely upon were upended by social distancing orders, undercutting the ability of families to seek and receive assistance. Lastly, the impact of COVID-19 itself has disproportionately affected Black Americans (CDC, 2020; Laurencin & McClinton, 2020) due to pre-existing structural racism (Yip, 2020), with COVID-19 occurring in tandem with the “second pandemic” of police- and civilian-perpetrated anti-Black violence (Dreyer, 2020). Within the context of the potentially differential impact of COVID-19, the purpose of the current study was to examine school support— which we defined as parents’ appraisal of schools’ provision of regular contact and opportunities for remote learning that made parents feel supported—as a modifiable factor that may relate to family life, including household chaos and routines, which may in turn be associated with parents’ mental health (Figure 1).
Figure 1.
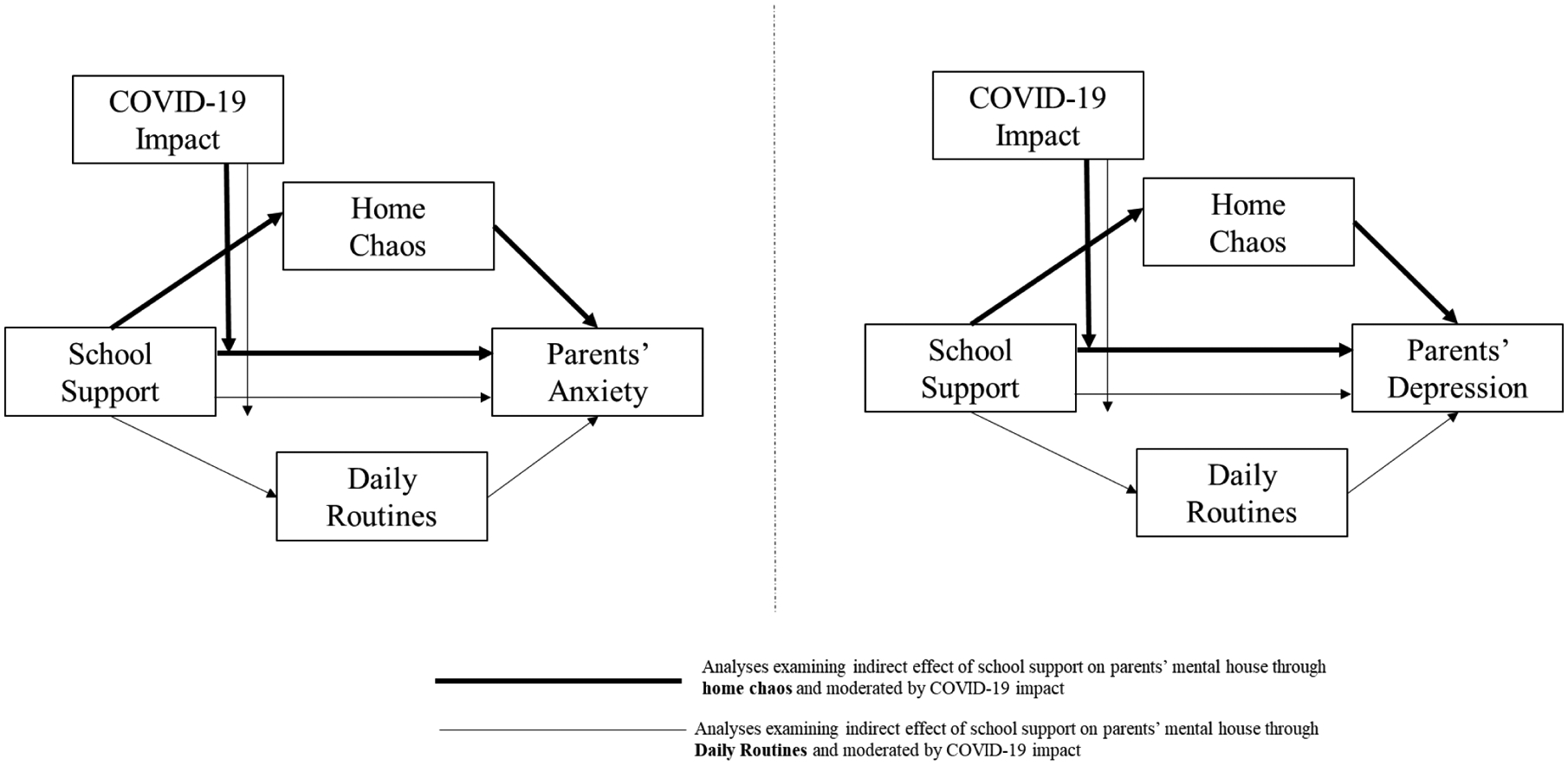
Hypothesized Relationships between School Support and Parents’ Mental Health and Indirect and Interactive (Moderation) Effects
Parental Mental Health during the COVID-19 Pandemic
Given that parents’ mental health is associated with parenting practices and child mental health (Goodman & Gotlib, 1999), understanding factors that influence parents’ mental health has implications for interventions across the COVID-19 pandemic, as well as future community disruptions (e.g., natural disasters). Individual, familial, and societal challenges associated with the COVID-19 pandemic have been linked to increased incidence of mental health problems for adults (Patrick et al., 2020; Racine et al., 2020). As such, the American Psychological Association (APA) stated that COVID-19 has resulted in a “national mental health crisis” (APA, 2020a). Using data collected during 2019 for baseline comparisons, the APA (2020b) found significant increases in adults’ stress generally. Moreover, US adults in 2020 were three times as likely to screen positive for depressive disorders, anxiety disorders, or both than in 2019 (Twenge & Joiner, 2020). Cameron and colleagues (2020) reported that, in a sample of predominately White parents, the prevalence of depression and anxiety increased substantially from 2019 to 2020 (9% to 28% and 7% to 34%, respectively). Parents reported additional stress compared to adults without children (APA, 2020b). For instance, over 70% of parents reported being worried about their children’s remote schooling, with disruptions to family routines and schedules being additional significant concerns (APA, 2020b). Given these elevated rates, it is important to identify factors that may have contributed to parents’ mental health early in the pandemic.
Associations of School Support, Household Chaos, and Routines with Parents’ Mental Health
When shelter-in-place orders were enacted in Spring 2020, schools were required to shift to remote instruction with online delivery. Given differential support, guidance, and resources (e.g., under-sourced schools in urban settings that serve predominately children of Color), schools varied in their modality and success in virtual teaching. In a survey conducted in Spring 2020 by PEW research (Horowitz, 2020), parents were asked about their satisfaction with the quality and amount of remote instruction. Under 50% reported being very satisfied with remote instruction, while 21% indicated their child received no or not much online instruction. Thus, the shift to remote learning may have negatively impacted family functioning, and relatedly, parents’ mental health.
Conversely, schools that offered organized, consistent, and structured remote educational opportunities for students during the early months of the pandemic may have positively affected parental mental health. Parents may have been less vulnerable to symptoms of depression and anxiety when they could easily reach out to their children’s teachers and when they perceived that school personnel were available to provide support during remote education. Such school support may function similarly to social support, including community-based systems, which is related to reduced levels of parental depression and anxiety symptoms (Reynolds & Crea, 2016). In line with the buffering hypothesis (Lakey & Cohen, 2000), which posits that social support can be protective against the impact of stress, school support may have mitigated some of the stress associated with childcare during shelter-in-place orders, thus improving parents’ mental health. However, in a sample of predominately White women with military spouses, Rosen and Moghadam (1990) noted that all sources of social support are not equally influential; to have a “buffering” impact, a source of support must match the specific stressor. They found that only support from other military wives, and not other forms of support, moderated the association between husbands’ length of deployment and distress. Gore and Aseltine (1995) used the term “matching theory” to describe this phenomenon. In support of the matching theory, Kim and Ross (2009) found that neighborhood-specific support, as compared to general social support, had the biggest buffering impact on the association between neighborhood stress and adults’ depression.
In the present investigation, we anticipated that support from schools during the early months of the pandemic may have served as an important buffer by helping parents create structure, such as providing a regular time children had to be awake in the morning and creating activities for children to do during the day. That is, school support may have reduced household chaos and facilitated the development of daily routines, which in turn may have promoted parents’ mental well-being. Household chaos, which includes noise, crowding, and disorganization (Evans & Wachs, 2010), is associated with child maladjustment (e.g., behavior problems, lower cognitive functioning; Deater-Deckard et al., 2009; Vernon-Feagans, Garrett-Peters, Willoughby, & Mills-Koonce, 2012) and poorer parental mental health (Marsh, Dobson, & Maddison, 2020). Conversely, family routines, including regular family mealtimes and sleep schedules, are observable, consistent family activities (Fiese et al., 2002) that are associated with low levels of household chaos (Evans & Wachs, 2010). Family routines are linked to parents’ positive mental health (Churchill & Stoneman, 2004) and healthy child outcomes, such as better sleep habits (Mindell et al., 2015).
Differential Impact of the COVID-19 Pandemic
While the pandemic can be viewed as a shared stressor across U.S. families, some families have been experiencing greater stress than others, due to job loss, food insecurity, and poor access to health care. In line with the buffering hypothesis (Lakey & Cohen, 2000), for families who experienced stressors associated primarily with remote schooling, school support may have been sufficient to buffer the impact of the pandemic. However, for families more impacted by COVID-19, school support may have been insufficient in helping them overcome the overwhelming and multi-faceted nature of COVID-19-related stressors, because school support may not be adequately “matched” (Gore & Aseltine, 1995) to meet these families’ needs. That is, this form of support may not be similarly protective for families facing additional COVID-19-related adversity: School support alone may not meet the social support needs of families most impacted by COVID-19.
Additionally, structural racism in the US is associated with health inequalities that increase the vulnerability for negative impacts of COVID-19 for Black Americans (Yip, 2020), including increased incidence, hospitalizations, and mortality (CDC, 2020). Beyond individual racial prejudice, structural racism is a “system of dominance, power, and privilege based on racial group designations…[that are perpetuated by]…maintaining structures, ideology, values, and behavior that have the intent or effect of leaving non-dominant-group members relatively excluded from power, esteem, status, and/or equal access to societal resources” (Harrell, 2000, p. 43). As such, the collateral damage of COVID-19, such as food insecurity and issues with childcare (Patrick et al., 2020), is also greater for Black and other people of Color (POCs). Unsurprisingly, compared to White parents, parents of Color reported increased worry regarding having basic needs met and healthcare access (APA, 2020b).
The Current Study
In the context of the COVID-19 pandemic in Spring, 2020, the purpose of the current study was to examine the associations between school support, household chaos, and family routines on Black, Other POC, and White parents’ mental health among families living in a large urban area in the U.S. We hypothesized that:
Higher school support would be associated with lower depression and anxiety symptoms in parents.
There would be an indirect association between lower school support and parents’ higher mental health symptoms via household chaos.
There would be an indirect association between higher levels of school support and parents’ lower mental health symptoms via family routines.
The reported severity of COVID-19 impact would moderate the association between school support and parents’ mental health such that school support would be less likely to serve as a buffer for parents’ mental health when COVID-19 impact was high.
Utilizing a guiding framework of structural racism (Hicken et al., 2018), we also explored whether parents’ race was associated with COVID-19 impact, school support, and parents’ mental health. In addition, we examined possible associations between COVID-19 impact, school support, parents’ mental health, and other contextual factors, including parents’ diagnosis of COVID-19, children’s receipt of Medicaid, and parents’ education.
Method
Participants and Procedures
All procedures were approved by the Wayne State University Institutional Review Board. Parents (N = 195) of preschool-to-middle school aged children from three existing participant registries were invited to participate in the Families Coping and Resilience Examination (C.A.R.E.) during COVID-19 project. Families resided in a large metropolitan area in the Midwestern region of the U.S. that reported one of the highest rates of COVID-19 cases and deaths during Spring 2020 (Austin & Hershbein, 2020). The inclusion criterion for the current study was having a child who shifted from in-person to remote school during the COVID-19 pandemic, resulting in a sample of 152 parents (Table 1). Participating families that were not included in this investigation had a child that had not begun attending school (i.e., child that was not attending preschool) or did not complete outcome measures. Nearly all parental participants were female (141; 92.8%), more than half were Black (n = 99; 65.1%), 13 (8.55%) were other people of Color (e.g., Middle Eastern), 18 (11.8%) were White, and 5 (3.3%) selected “other” for race. Additionally, 105 (69.1%) reported that their children received Medicaid. Children were, on average, 7.80 years old (SD = 2.78). Parents reported having an average of 3.50 children (SD = 1.24; minimum = 1; maximum = 7) living in their homes.
Table 1.
Demographics for Participating Parents (N = 152)
| n (%) | |
|---|---|
| Race and Ethnicity | |
| Black | 99 (70.2%) |
| White | 18 (12.8%) |
| Asian or Asian Indian | 5 (3.5%) |
| Hispanic/Latino | 2 (1.4%) |
| Middle Eastern | 5 (3.3%) |
| Native American/Native Alaskan | 1 (.7%) |
| Other | 5 (3.3%6) |
| Choose not to answer/No response | 17 (11.1%) |
| Parent-reported Sex: | |
| Female: | 141 (92.8%) |
| Male: | 7 (4.6%) |
| Choose not to answer/No response | 4 (2.0%) |
| Parents’ Partnered Status | |
| Never married | 81 (53.3%) |
| Married or Living with Romantic Partner | 58 (38.2%) |
| Divorce | 5 (3.3%) |
| Widowed | 3 (2.0%) |
| Choose not to answer | 5 (3.3%) |
| Child(ren) receive Medicaid? | |
| Yes | 105 (69.1%) |
| No | 46 (30.3%) |
| Choose not to answer/No response | 1 (.7%) |
| COVID-19 Personal Diagnosis: | |
| Yes | 17 (11.2%) |
| No | 133 (87.5%) |
| Choose not to answer/No response | 2 (1.3%) |
| Parent highest level of education: | |
| Did not complete high school | 14 (9.2%) |
| High school graduate or GED | 37 (24.3%) |
| Some college | 29 (25.7%) |
| Associate’s degree | 23 (15.1%) |
| Bachelor’s degree | 12 (8.6%) |
| Master’s degree | 17 (11.2%) |
| Doctoral degree (e.g., Ph.D., M.D., J.D.) | 8 (5.3%) |
| Other | 1 (.7%) |
| Working from Home: | |
| Yes | 62 (40.8%) |
| No | 84 (55.3%) |
| Choose not to answer/No response | 6 (3.9%) |
Each parent received a text message asking them to participate and, if needed, received text reminders. Parents from one participant registry also received a phone call to tell them about the project. Participants completed the questionnaire through Qualtrics Survey Systems, with the exception of one participant who completed the survey over the phone. The survey took approximately 20 minutes to complete, and parents were compensated with a $10 gift card or Clincard (i.e., a debit-like card for research). Surveys were completed between the beginning of April and the second week of June 2020.
Measures
Parent and Family Characteristics
Demographics included race, ethnicity, biological sex, receipt of Medicaid as a proxy for income, parental diagnosis of COVID-19, parents’ highest level of education, and whether they were working from home during the pandemic.
Parental Depression and Anxiety.
The Patient-Reported Outcomes Measurement Information System (PROMIS) scales were used to measure parental depression and anxiety symptoms (Pilkonis et al., 2011). The anxiety and depression scales contain 8 items each. A depression sample item is: “I felt worthless.” An example anxiety item is: “I felt fearful.” Items are rated on a 5-point Likert scale ranging from 1 (never) to 5 (always). Items were summed and converted to t scores (population M = 50 + 10). Per PROMIS scoring guidelines (Cella et al., 2010), a score of 60 is considered moderate and a score of 70 is considered severe. Coefficient alpha internal consistency for depression and anxiety items were excellent (α = .95 and α = .95, respectively). Given the limitations of coefficient alpha for estimating internal reliability (Dunn, Baguley, & Brunsden, 2014), we also report omega (ω) reliability values for this measure and all subsequent measures, which were calculated using the PROCESS OMEGA macro (see Hayes & Coutts, 2020). Omega values were ω = .95 and ω = .95 for depression and anxiety, respectively.
School Support.
Parents’ perceived school support during COVID-19 remote schooling was measured with eight items created for this investigation. Parents answered five positively worded items, including “I feel supported by my child’s school,” “I am happy with how the school has responded to the COVID-19 crisis,” “My child has been provided with educational opportunities at home,” “It is easy to reach my child’s teacher at this time,” and “I receive regular contact from my child’s school.” Parents also completed three negatively valanced items, which were reverse scored, including, “I have not received enough guidance from my child’s school about at-home-education at this time,” “The school is asking me to do too much now,” and “I cannot handle all the tasks/activities the school is asking me to do.” Items were rated on a 4-point Likert scale ranging from 1 (definitely not true) to 4 (definitely true). Items were summed to create a school support score. Internal consistency was acceptable based on coefficient alpha (α = .76), with an identical value for omega (ω = .76).
Household Chaos.
Parents completed a modified version of the Confusion, Hubbub, and Order Scale (CHAOS; Matheny, Wachs, Ludwig, & Phillips, 1995). This 6-item version (Wang, Deater-Deckard & Bell, 2013) of the CHAOS included items related to noise levels, commotion, and disorganization with a 5-point Likert scale ranging from 1 (definitely disagree) to 5 (definitely agree; a sample item is: “You can’t hear yourself think in our home”). The CHAOS has been used in numerous studies, including research on parents’ mental health (Thomas & Spieker, 2016). Internal consistency was acceptable (α = .71), with a similar value for omega (ω = .74).
Routines.
To measure daily routines, three items were created for this investigation. These items included: “We follow a regular bedtime routine in my home,” “We have meals at about the same time each day,” and “We follow a routine for getting schoolwork done each day.” Items were rated on a 5-point Likert scale ranging from 1 (definitely disagree) to 5 (definitely agree). Internal consistency of these items was good (α = .82), with an identical value for omega (ω = .82).
COVID-19 Impact.
COVID-19 impact was measured with four items from the Coronavirus Impact Scale created by Stoddard and Kaufman (2020). Parents rated the impact of COVID-19 on “family income/employment,” “food access,” “medical care access,” and “mental health treatment access” on a 4-point Likert scale ranging from 1 (no change) to 4 (severe). Items were averaged to compute a COVID-19 Impact score. Analyses looking at internal consistency showed α = .62 and ω = .63; these values are moderately low but acceptable. Notably, the COVID-19 Impact score may be best conceptualized as an index, rather than a scale; Streiner (2003) suggest indexes are comprised of theoretically unrelated items, making measures of internal consistency less appropriate.
Data Analytic Plan
We conducted preliminary analyses to examine if key variables (school support, parents’ anxiety and depression, household chaos, daily routines, and COVID-19 impact) were related to parents’ race (i.e., Black, Other POC, White, or Other), parental diagnosis of COVID-19, children’ receipt of Medicaid, working from home, and parents’ highest level of education. We also computed correlations among key variables. Next, we examined the frequency of elevated levels of depression and anxiety symptoms for parents. Then we examined the association between school support and parents’ anxiety and depression symptoms, respectively, using correlation analyses and hierarchical linear regression analyses, controlling for COVID-19 impact and demographics (hypothesis 1).
Next, we considered indirect associations (hypotheses 2 and 3) and whether COVID-19 impact moderated the association between school support and parents’ mental health (hypothesis 4). To simultaneously test both these hypotheses, we implemented the PROCESS macro using Model 5 (Hayes, 2018); this model allows for testing both the indirect association and the conditional associations at different levels (i.e., at the16th percentile, 50th percentile, and 84th percentile) of the proposed moderating variable. PROCESS creates bias-corrected 95% confidence intervals (CIs) of effects using bootstrapping, which is a resampling technique. Additionally, we used the steps outlined by Bodner (2017) to determine the effect size of the associations between school support and parents’ mental health at different levels of the moderator variable (i.e., COVID-19 impact). At the variable level, missing data was rare. As mentioned previously, to be included in this investigation all participants had to complete the PROMIS; thus there was no missing data for the outcome variables. For other key variables, there were missing scores for less than 2% of cases. Listwise deletion, which is the default setting in PROCESS and regression analyses, was used to handle missing data.
Results
Preliminary Analyses
We explored possible associations between parents’ race and other study variables. The only racial differences we found were that Black parents, compared to parents of all other races (White, Other POC, and Other), reported more COVID-19 Impact (M = 2.00, SD = .74 and M = 1.73, SD = .54, respectively; t [132] = −2.05, p = .04). COVID-19 diagnosis was related to parents’ depression symptoms (t [31.96] = −2.61, p = .01), but not other key variables. Parents who reported their child(ren) received Medicaid reported less school support (M = 3.11, SD = .58) than parents whose children did not receive Medicaid (M = 3.31, SD = .58; t [149] = −2.03, p = .045). Parents’ level of education and working from home during the pandemic were unrelated to any study variables. Therefore, race of parents, COVID-19 diagnosis, and receipt of Medicaid were included in the inferential analyses. Correlational analyses showed statistically significant associations among most key study variables in expected directions (Table 2). COVID-19 impact was unrelated to household chaos and family routines.
Table 2.
Descriptive Statistics and Correlations among Key Study Variables
| M (SD) | 1. | 2. | 3. | 4. | 5. | 6. | |
|---|---|---|---|---|---|---|---|
| 1. School Support | 3.16 (.57) | ----- | |||||
| 2. COVID-19 Impact | 1.92 (.67) | −.17* | ----- | ||||
| 3. Routines | 3.28 (.96) | .30** | −.14 | ----- | |||
| 4. Chaos | 2.88 (.69) | −.29** | .12 | −.74*** | ----- | ||
| 5. Parent Depression | 53.46 (10.18) | −.20* | .30*** | −.31*** | .40*** | ----- | |
| 6. Parent Anxiety | 55.21 (10.85) | −.31** | .26*** | −.40*** | .52*** | .83*** | ----- |
p < .05,
p < .01,
p < .001
Parents’ Mental Health and School Support
Of the 152 parent participants, more than a quarter (27.6%) reported elevated levels of depression, with 36 (23.7%) reporting moderate levels and 6 (3.9%) reporting severe levels. Additionally, approximately a third (34.2%) reported elevated anxiety, with 38 (25%) reporting moderate levels and 14 (9.2%) reporting severe levels. Correlation analyses showed that greater school support was associated with lower parental depression and anxiety (Table 2). Two regression analyses, controlling for key demographics and COVID-19 impact, showed that school support was significantly associated with parents’ depression and anxiety symptoms, respectively (Table 3).
Table 3.
Regression Analyses of the Association between School Support and Parent Depression and Anxiety while Accounting for Key Demographics and the Impact of COVID-19.
| Depression | Anxiety | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| B | β | t | R2Δ | B | β | t | p | R2Δ | |
| Step 1: | .03 | .04 | |||||||
| Black Parents | −2.51 | −.11 | 1.14 | −.23 | −.01 | −.10 | |||
| Parent COVID-19 Personal Diagnosis | 5.11 | .15 | 1.69 | 5.63 | .16 | 1.77 | |||
| Child(ren) receive Medicaid | −.73 | −.03 | −.34 | 2.93 | .12 | 1.29 | |||
| Step 2: | .07** | .09** | |||||||
| COVID-19 Impact | 4.06 | .27 | 3.12** | 4.77 | .30 | 3.51** | |||
| Step 3: | .10** | .04** | |||||||
| School Support | −6.08 | −.33 | −3.94** | −4.16 | −.21 | −2.50** | |||
p < .05,
p < .01
Indirect Associations and Moderation of the Direct Associations
Four analyses were run in which the mediator alternated between household chaos and routines and the dependent variable alternated between parental depression and anxiety (see Tables 4 and 5 for full results). For each analysis using PROCESS Model 5, there was a significant direct association between school support and parental mental health outcomes; however, in each analysis, there was also a significant indirect path from school support to parental mental health via household chaos or routines.
Table 4.
Analyses of Indirect Associations between School Support and Parents’ Depression and Anxiety via Home Chaos and the Moderating Role of COVID-19 Impact
| Depression | Anxiety | |||||||
|---|---|---|---|---|---|---|---|---|
| Indirect effects | ||||||||
| Confidence Interval | Confidence Interval | |||||||
| Indirect Effect | SE | LL | UL | Indirect Effect | SE | LL | UL | |
| Home Chaos | −2.17 | .76 | −3.82 | −.83 | −1.76 | .73 | −3.43 | −.53 |
| Direct & interactive effects (moderation) | ||||||||
| Confidence Interval | Confidence Interval | |||||||
| Effect | SE | LL | UL | Effect | SE | LL | UL | |
| Black Parents | −2.89 | 1.78 | −6.41 | .64 | −.78 | 2.02 | −4.79 | 3.23 |
| Parent COVID-19 Diagnosis | 4.55 | 2.46 | −.32 | 9.42 | 6.05* | 2.80 | .51 | 11.58 |
| Child(ren) receive Medicaid | 1.44 | 1.73 | −1.99 | 4.87 | 4.78* | 1.97 | .88 | 8.68 |
| COVID-19 Impact | −14.78* | 6.05 | −26.76 | −2.79 | −13.41 | 6.88 | −27.04 | .21 |
| Home Chaos | 6.32*** | 1.04 | 4.26 | 8.37 | 5.13*** | 1.18 | 2.79 | 7.47 |
| School Support | −15.25*** | 4.12 | −23.40 | −7.09 | −13.63** | 4.68 | −22.90 | −4.36 |
| Interaction (School Support X COVID-19 Impact) | 5.53** | 1.93 | 1.71 | 9.37 | 5.42* | 2.19 | 1.08 | 9.76 |
PROCESS does not provide p-values for indirect effects
p < .05,
p < .01,
p < .001
Table 5.
Analyses of Indirect Associations between School Support and Parents’ Depression and Anxiety via Daily Routines and the Moderating Role of COVID-19 Impact
| Depression | Anxiety | |||||||
|---|---|---|---|---|---|---|---|---|
| Indirect effects1 | ||||||||
| Confidence Interval | Confidence Interval | |||||||
| Indirect Effect | SE | LL | UL | Indirect Effect | SE | LL | UL | |
| Daily Routines | −1.66 | .76 | −3.41 | −.47 | −1.54 | .72 | −3.23 | −.40 |
| Confidence Interval | Confidence Interval | |||||||
| Effect | SE | LL | UL | Effect | SE | LL | UL | |
| Black Parents | −3.86* | 1.90 | −7.63 | −.10 | −1.63 | 2.07 | −5.73 | 2.47 |
| Parent COVID-19 Diagnosis | 4.79 | 2.62 | −.41 | 9.98 | 6.28* | 2.86 | .62 | 11.94 |
| Child(ren) receive Medicaid | 2.03 | 1.84 | −1.63 | 5.68 | 5.29** | 2.01 | 1.31 | 9.28 |
| COVID-19 Impact | −16.04* | 6.45 | −28.81 | −3.27 | −14.26 | 7.03 | −28.17 | −.35 |
| Routines | −3.54*** | .84 | −5.21 | −1.87 | 3.29*** | .92 | −5.11 | −1.47 |
| School Support | −16.60*** | 4.49 | −25.28 | −7.92 | −13.29* | 4.78 | −23.85 | −4.93 |
| Interaction (School Support X COVID-19 Impact) | 5.95** | 2.05 | 1.89 | 10.02 | 5.69** | 2.24 | 1.26 | 10.12 |
PROCESS does not provide p-values for indirect effects
p < .05,
p < .01,
p < .001
Moreover, the results revealed significant moderated associations of the direct paths from school support to parental depression and anxiety via level of COVID-19 impact. Results of these significant interaction terms are presented in Tables 4 and 5. Simple slopes of the associations at low (at the 16th percentile), moderate (at the 50th percentile), and high (at the 84th percentile) are presented here. In the first analysis (see plot in Figure 2), with household chaos included as the mediating variable, school support was associated with parental depression when COVID-19 impact was low (Effect = −8.39, SE = 2.02, p = .00; LLCI = −12.39, ULCI = −4.39) or moderate (Effect = −5.57, SE = 1.45, p = .00; LLCI = −8.44, ULCI = −2.70), but not when COVID-19 impact was high (Effect = −.04, SE = 1.96, p = .99; LLCI = −3.91, ULCI = 3.84). This pattern of results was also present in the second analysis with depression as the outcome and routines as the mediator; school support was associated with parental depression when COVID-19 impact was low (Effect = −9.22, SE = 2.15, p = .00; LLCI = −13.48, ULCI = −4.95) or moderate (Effect = −6.18, SE = 1.55, p = .00; LLCI = −9.24, ULCI = −3.11), but not when COVID-19 impact was high (Effect = −.22 SE = 2.09, p = .92; LLCI = −4.36, ULCI = 3.92). In the third analysis, with anxiety as the outcome and home chaos as the mediator, school support was associated with parents’ anxiety when COVID-19 impact was low (Effect = −6.90, SE = 2.30, p = .003; LLCI = −11.45, ULCI = −2.36) or moderate (Effect = −4.14, SE= 1.64, p = .01; LLCI = −7.40, ULCI = −.87), but not when COVID-19 impact was high (Effect = 1.28, SE = .2.22, p = .56; LLCI = −3.12, ULCI = 5.69). This same pattern emerged with routines as the mediator; school support was associated with parents’ anxiety when COVID-19 impact was low (Effect = −7.34, SE = 2.34, p = .002; LLCI = −11.98, ULCI = −2.69) or moderate (Effect = −4.43, SE = 1.69, p = .01; LLCI = −7.77, ULCI = −1.10), but not when COVID-19 impact was high (Effect = 1.26, SE = 2.28, p = .58; LLCI = −3.26, ULCI = 5.77). The significant interactions were plotted; because they all followed the same pattern, one plotted interaction is presented as an example in Figure 2.
Figure 2.
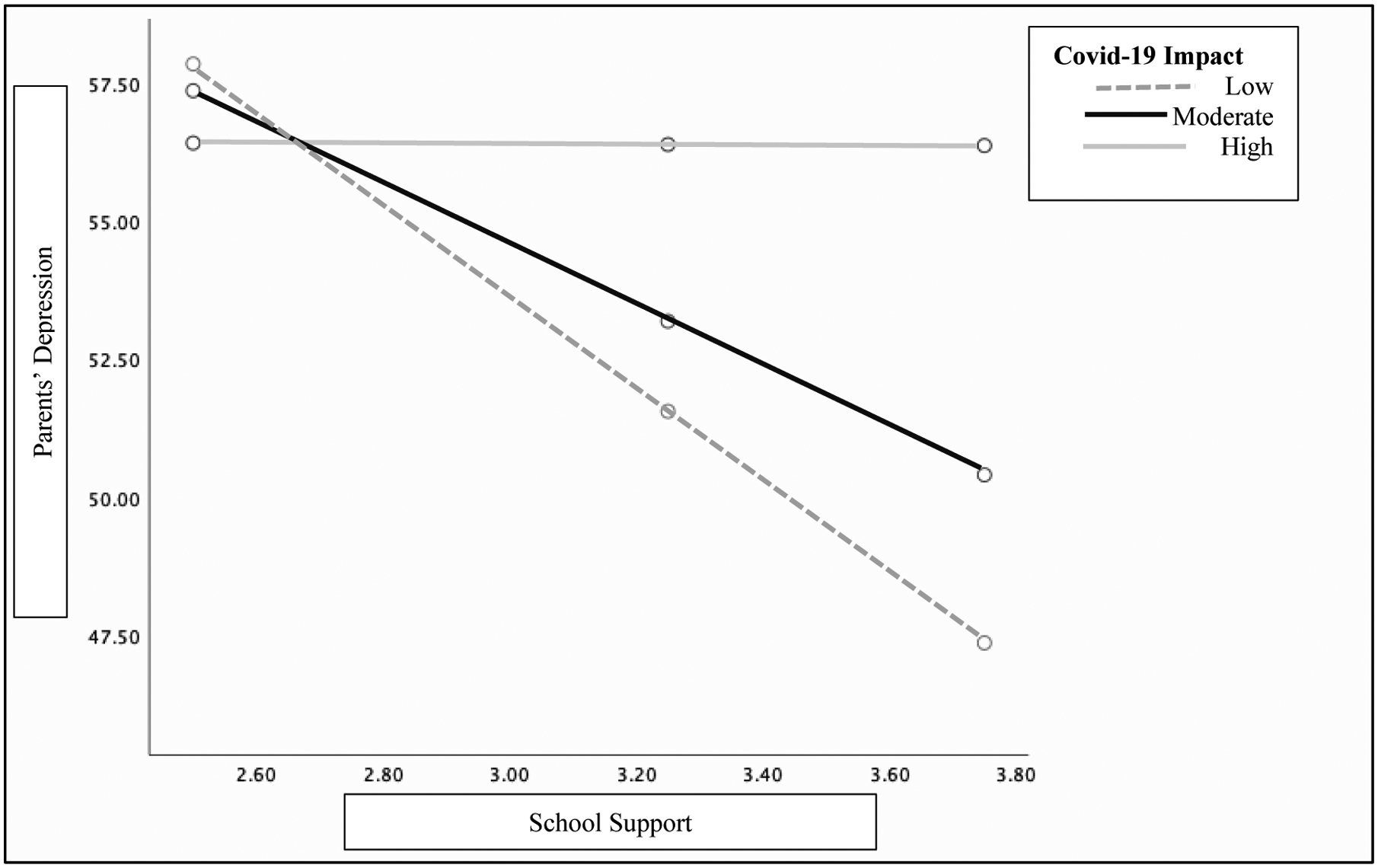
Example plot* of interactive effect at low (at 16th percentile), moderate (50th percentile), and high (at 84th percentile) levels of the COVID-19 Impact Moderator
* All interactions followed this same pattern; for brevity, only the above interaction is shown for illustrative purposes
To further understand the moderation results, we followed the procedures outlined by Bodner (2017) to calculate standardized effect sizes for the linear association between school support and parents’ mental health at low, moderate, and high levels of COVID-19 impact. For the first analyses, with depression as the dependent variable and including chaos, the analyses revealed semi-partial correlations of −.44, −.29, and −.002 for low, moderate, and high levels of COVID-19 impact. A similar pattern was found for the analysis with depression and including routines; the semi-partial correlations were −.48, −.32, and −.01 at low, moderate, and high levels of COVID-19 impact. For analysis with anxiety as the dependent variable including chaos, the semi-partial correlations were −.34, −.20, and .06 at low, moderate, and high levels of COVID-19 impact. Similarly, for the analysis with anxiety as the dependent variable including routines, the semi-partial correlations were −.35, −.22, and .06 at low, moderate, and high levels of COVID-19 impact. Thus, based on established standards for interpreting correlational effect sizes, including recommendations for semi-partial correlations (Bodner, 2017; Cohen, 1988), moderation analyses showed medium to large, small to medium, and close to zero effect sizes for the associations between school support and parents’ mental health when COVID-19 impact was low, moderate, and high, respectively.
Discussion
The purpose of the current study was to examine how parents’ mental health in the context of remote schooling may be associated with school support, household chaos, and routines early in the COVID-19 pandemic. Our findings are consistent with literature (e.g., Cameron et al., 2020) indicating that parents experienced high rates of depression and anxiety symptoms. In our investigation, parents reported elevated rates of depression (27.6%) and anxiety (34.2%) symptoms, which are slightly higher than findings from predominantly White national samples (Twenge & Joiner, 2020; 23.5% and 30.8%, respectively). It is possible that the rates in the current study are higher than national averages because participants were residing in a metropolitan area that was especially heavily impacted by COVID-19 during the early months of the pandemic (Austin & Hershbein, 2020).
Given the significant stress of managing children’s remote schooling and unstructured days while also trying to balance working from home or other home tasks, we predicted that, consistent with the buffering hypothesis (Lakey & Cohen, 2000), school support would be associated with parents’ positive mental health. Consistent with our first hypothesis, our results showed that higher levels of school support were associated with lower levels of depression and anxiety symptoms, even after controlling for COVID-19 impact and key demographic variables.
In line with our second and third hypotheses, the association between school support and parents’ mental health was partially accounted for by household chaos and daily routines. Higher levels of school support were associated with lower levels of household chaos, which in turn was related to fewer symptoms of depression and anxiety among parents. School support was also associated with greater endorsement of daily routines, with such routines being associated with fewer mental health symptoms among parents. Additional research is needed to track these processes over time to establish whether sustained school support continues to be associated with household chaos and routines, and positive mental health outcomes.
Our fourth aim was to evaluate whether level of COVID-19 impact (low, moderate, or high) would moderate the association between school support and parents’ mental health. Consistent with our hypothesis, school support was more likely to buffer the association between school support and mental health when COVID-19 impact was low or moderate. In contrast, school support was less likely to serve as a buffer for parents’ mental health when COVID-19 impact was high (i.e., when parents experienced pandemic-related food insecurity, job loss, and poor access to medical and mental health care). These findings fit with Cohen’s suggestion that the form of support must match the stressor in order for “buffering” to occur (Cohen & Wills, 1985). Parents experiencing the greatest stress due to COVID-19 may have needed support and resources beyond that provided from their children’s schools.
Importantly, increased impact of COVID-19 was not randomly distributed across racial groups in our sample. In line with Yip (2020), our findings support that structural racism (e.g., Hicken et al., 2018) further affects Black parents, who had significantly higher rates of COVID-19 impact than Other POC and White parents in our sample. The general geographic location of our sample, including increased prevalence of COVID-19 in the urban area, was consistent across families. Therefore, this difference in impact cannot be easily explained through variation in class or neighborhoods. As such, the current investigation bolsters other research that shows the disproportionate impact of the pandemic on Black Americans (e.g., CDC, 2020).
Implications
Although the results of this study are correlational and cannot be interpreted causally, they may have important implications for policy regarding the protective role schools may play during national and global emergencies. Schools may play a significant role, even when offered remotely, in helping parents structure their days and protect their mental health. Therefore, it is critical that schools have adequate structural and financial resources to support families during the pandemic and beyond. Given that school support did not serve as a buffer for many Black parents in our sample, who, on average, reported higher impact of COVID-19 than parents of other races, greater societal support is needed beyond what schools can provide. Thus, policy implications for parents must include addressing the larger societal contexts and systems that harm Black people due to structural racism (Gómez, 2015), including in U.S. governmental practices, policing, voting, education, housing, healthcare, and employment (Cook & Gómez, 2020). Taken together, the policy implications of this study suggest the need for a focus on health equity for parents and social justice in response to the pandemic.
Limitations and Final Considerations
This study has several limitations. First, the sample was relatively small and from only one metropolitan area in the US, limiting generalizability. Given the low numbers of Other POCs, we were unable to look between and within POC ethnic groups to assess for differences in all measures. Additionally, this investigation did not include a measure of structural and cultural racism; future research should assess these constructs at both micro and macro levels, including interpersonal discrimination and neighborhood segregation, respectively (Hicken et al., 2018). Moreover, analyses within this investigation were based on parental self-report data collected at one time point, which prevents conclusions about direction of effects. Specifically, parents’ mental health may influence their ratings of school support; likewise, living in homes that already had more structure and less chaos may increase the likelihood that parents perceive schools as more supportive. A significant strength of this investigation, however, is that it documents school-family associations during a unique point in history, in a predominantly racially marginalized sample, and through a critical race lens (Bell, 1995). As such, the current investigation has implications for understanding the associations among schools, communities, institutions, and structural racism and their links to parental and child well-being during global emergencies.
Impact and Implications Statement.
Early in the COVID-19 pandemic, parents reported high rates of depression and anxiety. Parents who reported more support from schools during remote schooling reported less depression and anxiety; however, this association was not significant for parents most impacted by the pandemic. Results highlight the important role schools can play in supporting families and the need for additional support beyond school systems for families most impacted by COVID-19.
Acknowledgements:
Support for Dr. McGoron’s time was from a K01 award from the National Institute of Mental Health (K01MH110600). Funding for participant incentives was provided by the Merrill-Palmer Skillman Institute for Child and Family Development. We thank the members of our research team for their valuable contributions to this project, including Steven J. Ondersma, John Hannigan, Elizabeth Towner, Joi Webb, Toni Lewis, Ava Palopoli, Kowsar Hijazi, and Lexi Hamlin. Finally, we especially thank parents that took time to participate in research during a global emergency.
References
- American Psychological Association (2020a). Stress in America 2020: A National Mental Health Crisis. [Google Scholar]
- American Psychological Association (2020b). Stress in America 2020: Stress in the Time of COVID-19. Volume 1. [Google Scholar]
- Austin JC & Hershbein B (2020, June, 4). Why Covid-19 hit Michigan so hard. The Avenue. [Google Scholar]
- Bell DA (1995). Who’s Afraid of Critical Race Theory? University of Illinois Law Review 4, 893–910. [Google Scholar]
- Bodner TE (2017). Standardized effect sizes for moderated conditional fixed effects with continuous moderator variables. Frontiers in Psychology, 8(562). doi: 10.3389/fpsyg.2017.00562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron EE, Joyce KM, Delaquis CP, Reynolds K, Protudjer JLP, & Roos LE (2020). Maternal psychological distress & mental health service use during the COVID-19 pandemic. Journal of Affective Disorders, 276, 765–774. https://doi-org.proxy.lib.wayne.edu/10.1016/j.jad.2020.07.081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Group PC, 2010. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of Clinical Epidemiology. 63 (11), 1179–1194. 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC; 2020). Cases, data, and surveillance. Coronavirus disease 2019 (COVID-19). Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/cases-update/index.html [Google Scholar]
- Centers for Disease Control (April, 2020). COVIDView: A weekly surveillance summary of U.S. COVID-19 activity. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html#mortality
- Churchill SL & Stoneman Z (2004). Correlates of family routines in Head Start families. Early Childhood Research & Practice, 6. [Google Scholar]
- Cohen J (1988). Statistical Power Analysis for the Behavioral Sciences (2nd ed.). Hillsdale, NJ: Lawrence Erlbaum Associates, Publishers. [Google Scholar]
- Cohen S, & Wills TA (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98, 310–357. [PubMed] [Google Scholar]
- Cook J, & Gómez JM (2020, July 3). Encouraging bravery and fortitude in dismantling the insidious stronghold of racism. The Hill. https://thehill.com/opinion/civil-rights/505685-encouraging-bravery-and-fortitude-in-dismantling-the-insidious [Google Scholar]
- Deater-Deckard K, Mullineaux PY, Beekman C, Petrill SA, Schatschneider C, & Thompson LA (2009). Conduct problems, IQ, and household chaos: A longitudinal multi-informant study. Journal of Child Psychology and Psychiatry, 50, 1301–1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dreyer BP, Trent M, Anderson AT, Askew GL, Boyd R, Coker TR, … & Montoya-Williams D (2020). The death of George Floyd: Bending the arc of history towards justice for generations of children. Pediatrics, Article e2020009639. doi.org/ 10.1542/peds.2020-009639 [DOI] [PubMed] [Google Scholar]
- Dunn TJ, Baguley T, & Brunsden V (2014). From alpha to omega: A practical solution to the pervasive problem of internal consistency estimation. British Journal of Psychology, 105(3), 399–412. https://doi-org.proxy.lib.wayne.edu/10.1111/bjop.12046 [DOI] [PubMed] [Google Scholar]
- Evans GW, & Wachs TD (2010). Chaos and its influence on children’s development: An ecological perspective. Washington, DC: American Psychological Association. [Google Scholar]
- Falk G, Carter JA, Nicchitta I, Nyhof EC, & Romero PD (2021, January). Unemployment Rates during the COVID-19 Pandemic: In Brief. (CRS Report, R46554). https://fas.org/sgp/crs/misc/R46554.pdf
- Fiese BH, Tomcho TJ, Douglas M, Josephs K, Poltrock S, & Baker T (2002). A review of 50 years of research on naturally occurring family routines and rituals: Cause for celebration? Journal of Family Psychology, 16, 381–390. [DOI] [PubMed] [Google Scholar]
- Goodman SH, & Gotlib IH (1999). Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review, 106(3), 458–490. 10.1037/0033-295X.106.3.458. [DOI] [PubMed] [Google Scholar]
- Gómez JM (2015). Microaggressions and the enduring mental health disparity: Black Americans at risk for institutional betrayal. Journal of Black Psychology, 41, 121–143. 10.1177/0095798413514608 [DOI] [Google Scholar]
- Gore S, & Aseltine RH (1995). Protective processes in adolescence: Matching stressors with social resources. American Journal of Community Psychology, 23(3), 301–327. https://doi-org.proxy.lib.wayne.edu/10.1007/BF02506947 [DOI] [PubMed] [Google Scholar]
- Harrell SP (2000). A multidimensional conceptualization of racism-related stress: Implications for the well-being of people of color. American Journal of Orthopsychiatry, 70, 42–57. [DOI] [PubMed] [Google Scholar]
- Hayes AF (2018). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York: Guilford Press. [Google Scholar]
- Hayes AF, & Coutts JJ (2020). Use omega rather than Cronbach’s alpha for estimating reliability. But … Communication Methods and Measures, 14, 1–24. 10.1080/19312458.2020.1718629 [DOI] [Google Scholar]
- Hicken MT, Kravitz-Wirtz N, Durkee M, & Jackson JS (2018). Racial inequalities in health: Framing future research. Social Science & Medicine (1982), 199, 11–18. 10.1016/j.socscimed.2017.12.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz JM (2020, April 15). Lower-income parents most concerned about their children falling behind amid COVID-19 school closures. Pew Research Center. https://www.pewresearch.org/facttank/2020/04/15/lower-income-parents-most-concerned-abouttheir-children-falling-behind-amid-covid-19-school-closures/ [Google Scholar]
- Kim J, & Ross CE (2009). Neighborhood-specific and general social support: Which buffers the effect of neighborhood disorder on depression? Journal of Community Psychology, 37(6), 725–736. https://doi-org.proxy.lib.wayne.edu/10.1002/jcop.20327 [Google Scholar]
- Lakey B, & Cohen S (2000). Social support theory and measurement. In Cohen S, Underwood LG & Gottlieb BH (Eds.), Social support measurement and intervention: A guide for health and social scientists (pp. 29–52). Oxford University Press. 10.1093/med:psych/9780195126709.003.0002 [DOI] [Google Scholar]
- Laurencin CT, & McClinton A (2020). The COVID-19 pandemic: A call to action to identify and address racial and ethnic disparities. Journal of racial and ethnic health disparities, 1–5. Advanced Online Publication. https://dx.doi.org/10.1007%2Fs40615-020-00756-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh S, Dobson R, & Maddison R (2020). The relationship between household chaos and child, parent, and family outcomes: A systematic scoping review. BMC Public Health, 20, 1–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheny AP, Wachs TD, Ludwig JL, & Phillips K (1995). Bringing order out of chaos: Psychometric characteristics of the confusion, hubbub, and order scale. Journal of Applied Developmental Psychology, 16, 429–444. [Google Scholar]
- Mindell JA, Li AM, Sadeh A, Kwon R, & Goh DYT (2015). Bedtime routines for young children: A dose-dependent association with sleep outcomes. Sleep, 38, 717–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick SW, Henkhaus LE, Zickafoose JS, Lovell K, Halvorson A, Loch S, Letterie M, & Davis MW (2020). Well-being of parents and children during the COVID-19 pandemic: A national survey. Pediatrics, 146(4), e2020–16824. [DOI] [PubMed] [Google Scholar]
- Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D, & the PROMIS Cooperative Group. (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): Depression, anxiety, and anger. Assessment, 18, 263–283. 10.1177/1073191111411667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine N, Birken C, & Madigan S (2020). Supporting the mental health of parents and children during and after coronavirus. Journal of Developmental and Behavioral Pediatrics, e-pub ahead of print. [DOI] [PubMed] [Google Scholar]
- Reynolds AD & Crea TM (2016). Household stress and adolescent behaviors in urban families: the mediation roles of parent mental health and social supports. Child & Family Social Work, 21, 569–580. [Google Scholar]
- Rosen LN, & Moghadam LZ (1990). Matching the support to the stressor: Implications for the buffering hypothesis. Military Psychology, 2(4), 193–204. https://doi-org.proxy.lib.wayne.edu/10.1207/s15327876mp0204_1 [Google Scholar]
- Stoddard+ J, & Kaufman J (2020). Coronavirus Impact Scale. Retrieved from https://www.phenxtoolkit.org/toolkit_content/PDF/CIS_Stoddard.pdf
- Streiner DL (2003). Being inconsistent about consistency: When coefficient alpha does and doesn’t matter. Journal of Personality Assessment, 80(3), 217–222. [DOI] [PubMed] [Google Scholar]
- Thomas KA, & Spieker S (2016). Sleep, depression, and fatigue in late postpartum. MCN: The American Journal of Maternal/Child Nursing, 41, 104–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge JM & Joiner TE (2020). Mental distress among US adults during the Covid-19 pandemic. Journal of Clinical Psychology, 76, 2170–2182. doi: 10.1002/jclp.23064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vernon-Feagans L, Garrett-Peters P, Willoughby M, & Mills-Koonce R (2012). Chaos, poverty, and parenting: Predictors of early language development. Early Childhood Research Quarterly, 27, 339–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z, Deater-Deckard K, & Bell MA (2013). Household chaos moderates the link between maternal attribution bias and parenting. Parenting: Science and Practice, 13(4), 233–252. https://doi-org.proxy.lib.wayne.edu/10.1080/15295192.2013.832569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yip T (2020). Addressing inequities in education during the COVID-19 pandemic: How education policy and schools can support historically and currently marginalized children and youth. Society for Research in Child Development. https://www.srcd.org/sites/default/files/resources/FINAL_AddressingInequalitiesVolume-092020.pdf


