Abstract
Pleconaril is an orally active, broad-spectrum antipicornaviral agent which demonstrates excellent penetration into the central nervous system, liver, and nasal epithelium. In view of the potential pediatric use of pleconaril, we conducted a single-dose, open-label study to characterize the pharmacokinetics of this antiviral agent in pediatric patients. Following an 8- to 10-h period of fasting, 18 children ranging in age from 2 to 12 years (7.5 ± 3.1 years) received a single 5-mg/kg of body weight oral dose of pleconaril solution administered with a breakfast of age-appropriate composition. Repeated blood samples (n = 10) were obtained over 24 h postdose, and pleconaril was quantified from plasma by gas chromatography. Plasma drug concentration-time data for each subject were fitted to the curve by using a nonlinear, weighted (weight = 1/Ycalc) least-squares algorithm, and model-dependent pharmacokinetic parameters were determined from the polyexponential parameter estimates. Pleconaril was well tolerated by all subjects. A one-compartment open-model with first-order absorption best described the plasma pleconaril concentration-time profile in 13 of the subjects over a 24-h postdose period. Pleconaril pharmacokinetic parameters (means ± standard deviations) for these 13 patients were as follows. The maximum concentration of the drug in serum (Cmax) was 1,272.5 ± 622.1 ng/ml. The time to Cmax was 4.1 ± 1.5 h, and the lag time was 0.75 ± 0.56 h. The apparent absorption rate constant was 0.75 ± 0.48 1/h, and the elimination rate constant was 0.16 ± 0.07 1/h. The area under the concentration-time curve from 0 to 24 h was 8,131.15 ± 3,411.82 ng · h/ml. The apparent total plasma clearance was 0.81 ± 0.86 liters/h/kg, and the apparent steady-state volume of distribution was 4.68 ± 2.02 liters/kg. The mean elimination half-life of pleconaril was 5.7 h. The mean plasma pleconaril concentrations at both 12 h (250.4 ± 148.2 ng/ml) and 24 h (137.9 ± 92.2 ng/ml) after the single 5-mg/kg oral dose in children were higher than that from in vitro studies reported to inhibit >90% of nonpolio enterovirus serotypes (i.e., 70 ng/ml). Thus, our data support the evaluation of a 5-mg/kg twice-daily oral dose of pleconaril for therapeutic trials in pediatric patients with enteroviral infections.
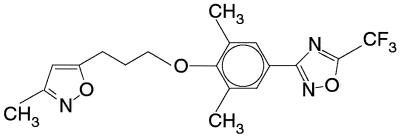
Pleconaril, 3-[3,5-dimethyl-4[[3-(3-methyl-5-isoxazolyl)propyl]oly]phenyl]-5-(trifluoromethyl)-1,2,4-oxadiazole (Fig. 1), is an orally active broad-spectrum antipicornaviral agent with potential therapeutic applications in the treatment of viral meningitis, upper respiratory disease (“summer flu”), and other enteroviral infections. Pleconaril, like similar [(oxazolylphenoxy)alkyl]isoxazole compounds, inhibits viral replication at the site of viral attachment and uncoating. These hydrophobic compounds insert themselves into a pocket beneath the canyon site on the icosahedral face of the virion, raising the floor of the canyon and thus altering the ability of the virus to attach to the cellular receptor. Additionally, these agents increase the stability of the viral capsid to receptor and pH-induced conformational changes which normally occur during the process of cellular entry. These events prevent the disassembly and release of viral ribonucleic acid (6).
FIG. 1.
Chemical structure of pleconaril.
Preclinical studies have demonstrated that the bioavailability of pleconaril in a solid-dose form is increased approximately sevenfold in the presence of food compared to under fasting conditions (11). In an attempt to minimize food effects on pleconaril bioavailability, an oral liquid formulation of the drug in a medium-chain-triglyceride-based vehicle was developed. A bioavailable oral liquid formulation of the drug is also required for its administration to young infants, children, and, potentially, geriatric patients. Given the prevalence of enteroviral infections in infants and young children and the anticipated pediatric application of pleconaril, we conducted an initial (i.e., phase II) single-dose pharmacokinetic study of the liquid formulation in children and young adolescents in order to study its disposition characteristics relative to age.
(This research was presented in part at the 99th annual meeting of the American Society for Clinical Pharmacology and Therapeutics, New Orleans, La., 30 March to 1 April 1998.)
MATERIALS AND METHODS
Subjects.
Eighteen children and young adolescents who were either inpatients or outpatients at the two participating institutions were enrolled. Subjects were eligible for enrollment if they met the following inclusion criteria: (i) age between 2 and 12 years; (ii) the presence of a culture-proven or clinically suspected viral infection; (iii) clinical and biochemical evidence of normal gastrointestinal, hepatic, and renal functions; (iv) the absence of concomitant systemic antiviral therapy; (v) body weight and height between the 5th and 95th percentile for age and gender; and (vi) the availability of parents and/or legal guardians for the purpose of informed consent. Additionally, female subjects who had attained menarche were required to have a negative serum pregnancy test prior to administration of the study drug. Subjects were excluded from participation if any of the following conditions were present: (i) a history or presence of a chronic disease state as indicated by the subject’s medical history, a physical examination, and/or laboratory tests; (ii) significant allergies (related to medication, food, etc.); (iii) abnormal gastrointestinal function as indicated by the subject’s medical history and a physical examination; (iv) an inability to tolerate an age-appropriate, normal oral diet; (v) consumption of an investigational drug administered as part of a clinical trial within 30 days of the administration of the study drug or a prescription drug known to interfere with the quantitation of pleconaril from plasma or to induce cytochrome P-450 metabolism; and (vi) the inability to tolerate required study procedures (e.g., maintaining vascular access sufficient to enable repeated blood sampling).
An investigation of medical history, a physical examination, and clinical laboratory tests (complete blood count, serum chemistry panel, liver function tests, and urinalysis) were performed for each subject prior to enrollment and within 48 h after completion of the study. All subjects were enrolled via informed parental consent and by patient assent when appropriate (i.e., for subjects >7 years of age). The study protocol was approved by the Investigational Review Board of the Children’s Mercy Hospital and the Human Research Advisory Committee of the University of Arkansas for Medical Sciences.
Study design.
The study design was an open-label, single-dose evaluation of pleconaril pharmacokinetics following the administration of the drug with an age-appropriate (in both amount and composition) breakfast. All subjects were admitted to the participating study facilities during the morning of the study, where they remained through the 24-h postdose sample collection period. Thirty minutes prior to pleconaril administration, each subject was given an age-appropriate breakfast consisting of at least 400 calories (e.g., cereal, milk, two slices of buttered toast with jelly, and 90 ml of apple or orange juice). Subsequently, subjects received a single 5-mg/kg of body weight oral dose of pleconaril solution (40 mg/ml) with 120 ml of milk. Complete swallowing and retention of the study medication was ensured by inspection of the oral cavity and close supervision by a Clinical Research Nurse.
Sample collection.
Blood samples (2 ml each) for determination of pleconaril concentrations were collected from an indwelling venous catheter into glass tubes containing EDTA. Samples were collected immediately prior to drug administration and at 1, 2, 3, 4, 5, 6, 8, 12, 16, and 24 h following the dose. Blood samples were maintained on ice for a period of ≤60 min before transport to the laboratory. Plasma was separated by centrifugation (2,500 rpm for 10 min at 4°C [Beckman GS-6R]) and stored in polypropylene tubes at −80°C until analysis, a period not exceeding 90 days from the time of collection.
Analytical procedures.
Pleconaril concentrations were determined by using a previously validated gas chromatographic technique with electron capture detection (7). A seven-point standard curve using the peak height ratio of active compound to internal standard (WIN 66407) was prepared daily and was used to calculate all plasma pleconaril concentrations. The limit of detection for the assay was established as the lower-limit standard (i.e., 49.39 ng/ml). The analytical method demonstrated linearity at plasma pleconaril concentrations ranging from 49.39 to 1,975.73 ng/ml (r2 > 0.99). Interday assay variability ranged from 2.3 to 10.2% and intraday assay variability ranged from 6.7 to 8.3% at concentrations of pleconaril in plasma spanning the range of linearity for the analytical methods (7). All assays were performed by an independent laboratory (Phoenix International Life Sciences, Inc., Montreal, Quebec, Canada). The mean concentrations in plasma from the analysis of duplicate samples were reported and used to accomplish the pharmacokinetic and statistical analyses.
Pharmacokinetic and statistical analyses.
Pharmacokinetic and statistical analyses were conducted using Kinetica version 1.1 (InnaPhase, Paris, France). Plasma drug concentration-time data were fitted to a curve by using a peeling algorithm to generate initial polyexponential parameter estimates. Final parameter estimates were determined from an iterative, nonlinear weighted least-squares regression algorithm with reciprocal (1/Ycalc) weighting. Final compartment model selection was accomplished through examination of the Akaike Information Criterion and the coefficients of variation for each polyexponential parameter estimate. Model-dependent pharmacokinetic parameters were then calculated from final polyexponential parameter estimates.
Individual maximum concentration of drug in serum (Cmax) and the time to Cmax (Tmax) were estimated by inspection of the observed plasma drug concentration-time data consequent to the relatively low number of points contained on the absorption phase and their inherent variability. The area under the concentration-time curve from 0 to 24 h postdose (AUC0–24) was determined by using the log-linear trapezoidal rule. Extrapolation of the AUC to infinity (AUC0–∞) was calculated by summation of AUC0–24 + Cp24/λz, where Cp24 is the plasma drug concentration at 24 h postdose predicted from the fitted apparent terminal elimination phase and λz is the apparent terminal elimination rate constant. The apparent total body clearance (CL/F) and apparent steady-state volume of distribution (VSS/F) were calculated from the AUC0–∞.
Pleconaril pharmacokinetic parameters for the study cohort were examined by using standard descriptive statistics (mean, standard deviation, and range). Examination of the data for possible age dependence in the pleconaril pharmacokinetic parameters (e.g., CL/F, VSS/F, AUC0–24, the apparent absorption rate constant [Ka], and λz) was undertaken using both linear and nonlinear least-squares regression techniques. Comparison of pleconaril pharmacokinetic parameters from the study population to those from a similar study conducted in healthy adults was performed using the Wilk-Shapiro test to assess homogeneity of variance, followed by a two-tailed, unpaired Student’s t test. The significance limit accepted for all statistical analyses was α = 0.05.
RESULTS
Eighteen subjects (12 male) ranging in age from 2 to 12 years (mean ± standard deviation, 7.5 ± 3.1 years) and in weight from 13.7 to 51.5 kg (29.9 ± 12.0 kg) completed this multicenter study and received the single 5-mg/kg oral dose of pleconaril solution, and 13 subjects had evaluable data. Demographic data from these 13 are provided in Table 1. Pleconaril was well tolerated in all subjects and no severe adverse events were reported by any of the participants during the study period. Additionally, no subject complained of poor palatability for the oral suspension formulation.
TABLE 1.
Demographics of study subjects
| Subject no. | Gendera | Age (yr) | Weight (kg) |
|---|---|---|---|
| 1 | M | 2 | 16.6 |
| 2 | M | 3 | 17.0 |
| 3 | M | 3 | 13.7 |
| 4 | M | 6 | 21.5 |
| 5 | M | 7 | 21.5 |
| 6 | M | 8 | 27.3 |
| 7 | F | 9 | 34.0 |
| 8 | M | 9 | 27.3 |
| 9 | M | 10 | 37.0 |
| 10 | M | 10 | 34.3 |
| 11 | M | 11 | 37.8 |
| 12 | F | 12 | 51.5 |
| 13 | F | 12 | 48.7 |
| Mean | 7.85 | 29.86 | |
| SD | 3.44 | 12.00 |
M, male; F, female.
The mean plasma pleconaril concentration-time data over the 24-h postdose period are illustrated in Fig. 2. The plasma drug concentration data reflected considerable intersubject variability for Cmax (1,272.5 ± 622.1 ng/ml) and the concentrations at both 12 h (250.4 ± 148.2 ng/ml) and 24 h (137.9 ± 92.2 ng/ml) postdose. In 13 of the subjects, the plasma drug concentration-time data were best characterized by using a one-compartment open model with first-order absorption. In five subjects, reliable pharmacokinetic parameter estimates could not be derived from application of the one-compartment open model. In one subject (male, 6 years of age), the plasma pleconaril concentrations increased throughout the sampling interval, reaching Cmax at 24 h. In three subjects, the Tmax occurred >8 h following drug administration. Accordingly, a sufficient number of plasma pleconaril concentration-time points were not present in the apparent terminal elimination phase to accurately estimate λz in these subjects. Finally, in one subject, measurable plasma pleconaril concentrations did not occur until more than 4 h postdose, thereby obviating the accurate estimation of all polyexponential parameters required by the one-compartment open model. The pharmacokinetic parameters for pleconaril in the 13 subjects with complete data sets are contained in Table 2.
FIG. 2.
Mean (plus standard deviation) plasma drug concentration-time profile in 13 pediatric patients administered a single 5-mg/kg dose of pleconaril oral solution.
TABLE 2.
Individual pediatric subject pharmacokinetic parameters
| Subject | Cmax (ng/ml) | Tmax (h) | AUC0–24 (ng · h/ml) | Ka (1/h) | λz (1/h) | CL/F (liters/h/kg) | VSS/F (liters/kg) |
|---|---|---|---|---|---|---|---|
| 1 | 1,820.0 | 4.0 | 12,541.5 | 0.48 | 0.17 | 0.38 | 2.39 |
| 2 | 1,610.0 | 4.0 | 8,196.5 | 0.54 | 0.15 | 0.55 | 4.18 |
| 3 | 1,405.0 | 4.0 | 9,288.5 | 0.35 | 0.17 | 0.50 | 3.08 |
| 4 | 2,533.0 | 2.0 | 11,626.0 | 1.03 | 0.04 | 0.31 | 4.30 |
| 5 | 814.0 | 4.0 | 6,888.5 | 0.42 | 0.12 | 0.62 | 5.93 |
| 6 | 729.0 | 4.0 | 6,242.0 | 0.49 | 0.12 | 0.71 | 6.14 |
| 7 | 228.0 | 3.0 | 1,312.5 | 0.46 | 0.34 | 3.45 | 9.18 |
| 8 | 901.0 | 4.0 | 8,243.5 | 0.87 | 0.11 | 0.51 | 5.073 |
| 9 | 1,631.0 | 3.0 | 9,953.5 | 1.68 | 0.16 | 0.46 | 3.33 |
| 10 | 1,682.0 | 8.0 | 13,213.0 | 0.27 | 0.17 | 0.35 | 1.87 |
| 11 | 1,276.0 | 4.0 | 7,404.5 | 1.52 | 0.13 | 0.60 | 5.32 |
| 12 | 513.0 | 3.0 | 3,113.0 | 1.26 | 0.24 | 1.61 | 6.82 |
| 13 | 1,401.0 | 6.0 | 7,682.0 | 0.37 | 0.16 | 0.53 | 3.29 |
| Mean | 1,272.5 | 4.1 | 8,131.2 | 0.75 | 0.16 | 0.81 | 4.68 |
| SD | 622.1 | 1.5 | 3,411.8 | 0.48 | 0.07 | 0.86 | 2.02 |
| Minimum | 228.0 | 2.0 | 1,312.5 | 0.27 | 0.04 | 0.31 | 1.87 |
| Maximum | 2,533.0 | 8.0 | 13,213.0 | 1.68 | 0.34 | 3.45 | 9.18 |
To examine potential age dependence in pleconaril pharmacokinetics, the parameter estimates obtained for our pediatric patients (Table 2) were compared to those generated from a study conducted with 12 healthy adult volunteers (7 females; 26.1 ± 5.3 years of age, 72.1 ± 14.2 kg) who were given a single oral dose (2.86 ± 0.53 mg/kg) of pleconaril oral suspension followed 30 min later by the ingestion of a standard English breakfast (e.g., two fried eggs, two sausage links, two slices of buttered toast, milk, orange juice, and coffee with cream) (2). This particular investigation utilized a formulation of pleconaril solution and an analytical approach identical to that of our study of pediatric patients. This comparison demonstrated that the mean AUC0–∞ (1.86 ± 0.81 μg · h/ml) and Cmax (0.26 ± 0.12 μg/ml) from our pediatric subjects corrected for a pleconaril dose of 1 mg/kg were significantly (P < 0.05) less than the corresponding parameters (3.2 ± 1.01 μg · h/ml and 0.41 ± 0.18 μg/ml, respectively) obtained from the adult study (4). In contrast, the CL/F (0.81 ± 0.86 liters/h/kg) and VSS/F (4.7 ± 2.0 liters/kg) for pleconaril in our pediatric subjects were significantly (P < 0.05) greater than the corresponding values (CL/F = 0.34 ± 0.12 liters/kg and VSS/F = 3.2 ± 2.0 liters/kg) reported for the subjects in the adult study (4).
Finally, the disposition of pleconaril in our study cohort of pediatric patients did not appear to vary as a function of age. This was reflected by the absence of significant correlations (i.e., r2 ≤ 0.25 for both linear and nonlinear regression analyses) between age and specific pharmacokinetic parameters (e.g., λz, Ka, CL/F, and VSS/F).
DISCUSSION
Nonpolio enteroviruses (NPEV) are estimated to cause 10 to 15 million illnesses each year (9). The majority of these illnesses are minor, presenting as upper respiratory tract infections with fever, malaise, and rash. However, serious infections, including aseptic meningitis, encephalitis, pericarditis, and myocarditis, do result with young children at greatest risk of infection and morbidity (8). Currently, no specific antiviral agents are available for the management of patients with enterovirus infections (3). Intravenous immune globulin has been used successfully in acute and chronic infections; however, the response is variable and may be a function of the timing of infusions and the neutralizing antibody titers within the preparation (1, 4). With new developments in PCR techniques resulting in increased rapidity and sensitivity of diagnosis, early institution of specific antiviral therapy against enterovirus may play an important role in managing acute, severe febrile illness as well as chronic infections (5).
Pleconaril is one such antiviral agent demonstrating potent activity against the picornaviridae. In vitro 50% tissue culture infectious dose assays have been conducted with pleconaril against 15 NPEV clinical isolates. The concentration of pleconaril required to inhibit >90% of the 215 clinical isolates of the NPEV serotypes tested was 70 ng/ml, with median 50% inhibitory concentrations (IC50s) for coxsackievirus group A serotypes of 6 ng/ml, coxsackievirus group B serotype IC50 of 7 to 62 ng/ml, and echovirus serotype IC50s of 2 to 50 ng/ml (11). Animal studies using radiolabeled [14C]pleconaril demonstrated concentrations in the liver, nasal epithelium, brain, and plasma of 6.1 to 17.5, 4.2, 2.8, and 0.7 mg/liter, respectively, 2 h following oral administration of pleconaril solution. These data suggest that following oral administration, pleconaril penetrates tissue where viral replication likely occurs at concentrations well above those observed in the plasma and considerably greater than the median IC50 for potentially important viral pathogens (11).
Following a single 5-mg/kg dose of pleconaril oral solution in children, there was considerable variability in the plasma drug concentration-time profile for the drug (Fig. 2). Nonetheless, as previously reported in adult subjects (2), the pharmacokinetics of pleconaril were best described with a simple one-compartment model with first-order absorption. This is in contrast to the polyexponential postpeak decay previously observed following single-dose administration of a capsule formulation of the drug (11). The mean apparent elimination half-life of pleconaril (5.7 ± 4.4 h) following a single dose of the oral solution in children did not differ significantly from that previously reported for adults (6.7 ± 2.4 h) who received an identical formulation. It was, however, substantially lower than that previously observed for adults following a single oral dose of the drug administered as a capsule formulation (24.8 ± 12.3 h) (11). The apparent difference may represent formulation dependent changes in the absorption profile produced by rate-limiting differences in the release characteristics of the active drug from the respective formulations (i.e., oral solution versus capsule). Alternatively, discontinuation of postdose blood sampling past 24 h in both the previous (2) and present study may have obscured our ability to detect a prolonged terminal elimination phase for pleconaril in plasma representative of release of the drug from a deep tissue compartment (e.g., a γ-phase). However, given the fact that we sampled for approximately four times the apparent terminal elimination half-life, it is quite likely that we did obtain an accurate estimate of the elimination phase for the drug that is representative of its clearance from plasma.
When compared with data from adults (2), the dose normalized Cmax and AUC0–∞ were significantly lower in children (roughly 1.5- and 1.7-fold, respectively), a finding which could be a consequence of differences between the two studies associated with the administration of food near the time of pleconaril dosing. As well, the apparent CL/F and VSS/F for pleconaril in our pediatric patients were significantly higher than values observed in adults (2) (i.e., approximately 2.4- and 1.5-fold, respectively). These data suggest that a 5-mg/kg oral dose of pleconaril solution will be necessary in children to achieve plasma drug concentrations similar to those observed in adults following a standard 200-mg dose (i.e., approximately 3 mg/kg). Despite these apparent age-associated differences in pleconaril pharmacokinetics, we were not able to detect significant associations between subject age and the pharmacokinetic parameters for the drug in the pediatric patient. This was not surprising, given the relatively small sample size of our study cohort and the inherent variability in both the plasma concentration-time profile and pharmacokinetic parameters of the drug.
In the present study, the pharmacokinetic parameters for pleconaril could not be adequately characterized in five children where Tmax was significantly delayed, occurring between 8 and 24 h following drug administration. These findings could be ascribed to delayed gastric emptying in these patients, although we cannot explain them by alterations in diet (because the meals were standardized among all children) or by the presence of a pathophysiologic condition that might affect gastric emptying. Additionally, local minima were observed during the absorption phase of the plasma drug concentration-time profile in three of these subjects, suggesting a possible biphasic and/or non-first-order absorption process.
Despite our inability to completely characterize pleconaril pharmacokinetics in these five subjects, the Cmax and AUC0–∞ trended toward lower values but fell within the range of interpatient variability demonstrated for these parameters in the remaining 13 children (Table 2). These findings suggest that it is primarily the rate rather than the extent of pleconaril absorption that was altered in these subjects. Similarly, the plasma pleconaril concentration at 12 h in these five children was within the normal range of interpatient variability for the study. However, the plasma pleconaril concentration at 24 h postdose in these 5 subjects was markedly greater than that observed for the 13 completely evaluable subjects (Table 2), suggesting that adequate plasma drug concentrations were maintained throughout the dosing interval in these 5 subjects despite the alteration in absorption profile. Finally, there were no demographic differences between the five subjects for whom complete pharmacokinetic data were not available and the remaining subjects that would appear to adequately explain these findings.
In conclusion, the mean values of CL/F and VSS/F for pleconaril following oral administration of a solution formulation to children with suspected viral infection were greater than the corresponding values for these parameters previously reported from a single-dose study of this same formulation administered to fed adults (2). These “changes” apparently gave rise to a lower Cmax and AUC0–∞ for the drug in pediatric patients when the dose was normalized based upon body weight (i.e., to 1 mg/kg). Nonetheless, plasma pleconaril concentrations at 12 h after a single 5-mg/kg dose of oral solution under fed conditions to children remained approximately 3.5-fold greater than that required to inhibit 90% of NPEV in cell culture. Thus, it would appear that pleconaril oral suspension administered at 5 mg/kg twice daily would be appropriate for children 2 to 12 years of age in future trials of drug efficacy and safety.
ACKNOWLEDGMENTS
We gratefully acknowledge the professional assistance provided by Kathy Johnson and Nancy Lowery. The editorial assistance provided by Ralph E. Kauffman is also appreciated.
This research was supported in part by a grant from ViroPharma, Inc. (Malvern, Pa.), and grants 1 U10 HD31313-05 (to G.L.K.) and 1 U10 HD31324-05 (to T.G.W.) from the National Institute of Child Health and Human Development, Bethesda, Md.
REFERENCES
- 1.Abdel-Rahman S M, Kearns G L. Single dose pharmacokinetics of pleconaril (VP63843) oral suspension and the effect of prandial state. Antimicrob Agents Chemother. 1998;42:2706–2709. doi: 10.1128/aac.42.10.2706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abzug M J, Keyserling H L, Lee M L, Levin M J, Rotbart H A. Neonatal enterovirus infection: virology, serology, and effects of intravenous immune globulin. Clin Infect Dis. 1995;20:1201–1206. doi: 10.1093/clinids/20.5.1201. [DOI] [PubMed] [Google Scholar]
- 3.Berlin L E, Rorabaugh M L, Heldrich F, Roberts K, Doran T, Modlin J F. Aseptic meningitis in infants <2 years of age: diagnosis and etiology. J Infect Dis. 1993;168:888–892. doi: 10.1093/infdis/168.4.888. [DOI] [PubMed] [Google Scholar]
- 4.Dagan R. Nonpolio enterovirus and the febrile young infant: epidemiologic, clinical and diagnostic aspects. Pediatr Infect Dis J. 1996;15:67–71. doi: 10.1097/00006454-199601000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Keyserling H L. Other viral agents of perinatal importance: varicella, parvovirus, respiratory syncytial virus, and enterovirus. Clin Perinatol. 1997;24:193–211. [PubMed] [Google Scholar]
- 6.McKinlay M A, Pevear D C, Rossmann M G. Treatment of the picornavirus common cold by inhibitors of viral uncoating and attachment. Annu Rev Microbiol. 1992;46:635–645. doi: 10.1146/annurev.mi.46.100192.003223. [DOI] [PubMed] [Google Scholar]
- 7.Phoenix International Life Sciences. Validation of a high resolution gas chromatographic method for the determination of VP 63843 in human plasma by electron capture detection. Phoenix Project no. 952145/EJN. Montreal, Quebec, Canada: Phoenix International Life Sciences; 1996. [Google Scholar]
- 8.Rotbart H A. Enteroviral infections of the central nervous system. Clin Infect Dis. 1995;20:971–981. doi: 10.1093/clinids/20.4.971. [DOI] [PubMed] [Google Scholar]
- 9.Strikas R A, Anderson L J, Parker R A. Temporal and geographic patterns of isolates of nonpolio enterovirus in the United States, 1970–1983. J Infect Dis. 1986;153:346–351. doi: 10.1093/infdis/153.2.346. [DOI] [PubMed] [Google Scholar]
- 10.Thoren A, Widell A. PCR for the diagnosis of enteroviral meningitis. Scand J Infect Dis. 1994;26:249–254. doi: 10.3109/00365549409011792. [DOI] [PubMed] [Google Scholar]
- 11.ViroPharma Incorporated. VP63843 Clinical Investigators Brochure. ViroPharma Incorporated, Malvern, Pa.