Video
Endoscopic submucosal dissection using traction by a spring-and-loop with clip for a laterally spreading tumor in the inferior aspect of the cecum: a nonreferral center experience.
Abbreviation: ESD, endoscopic submucosal dissection
Endoscopic submucosal dissection (ESD) has been widely accepted as a minimally invasive treatment for early colorectal neoplasms.1 However, cecal ESD remains a challenging treatment owing to the anatomical features of the cecum, such as the thin wall, and confrontation of the endoscope vertically with the muscular layer.
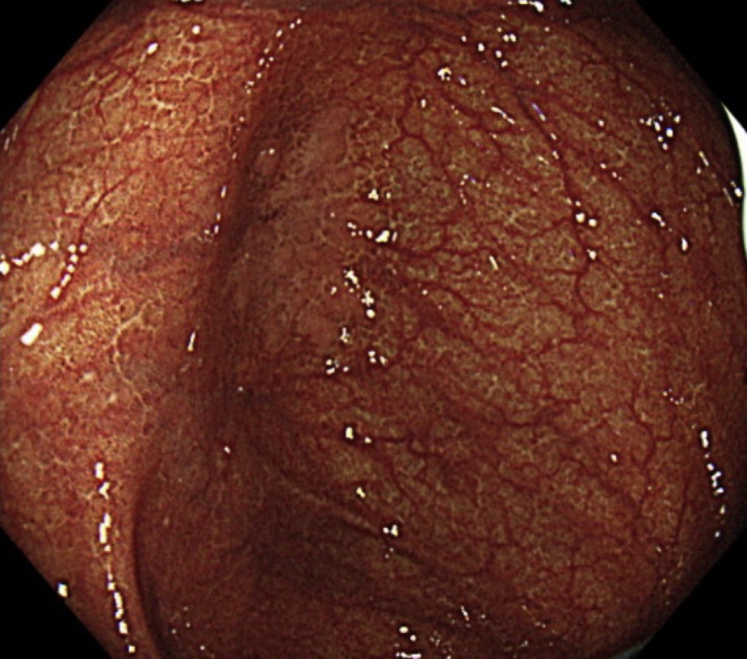
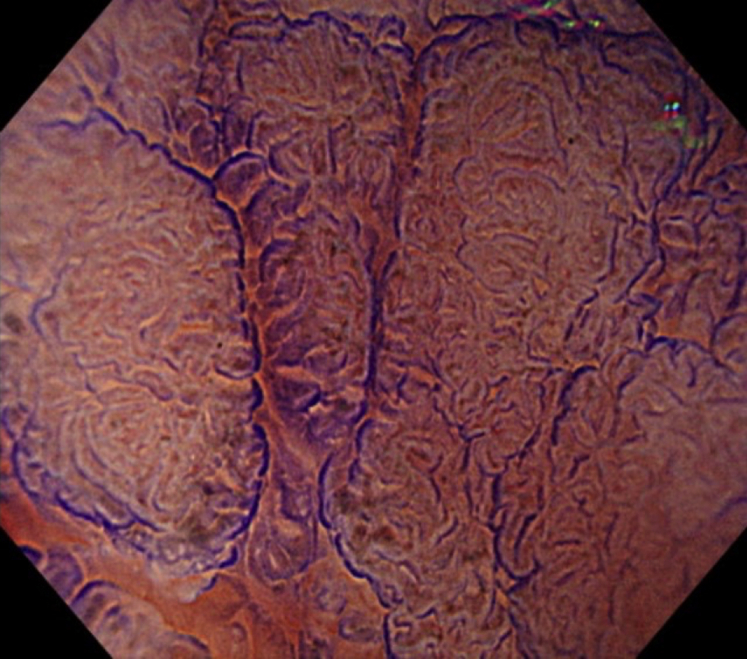
An 85-year-old woman had a flat, elevated lesion of approximately 25 mm in the inferior aspect of the cecum (Fig. 1). Magnifying chromoendoscopy displayed Kudo’s pit pattern types ⅢL and Ⅳ (Fig. 2).2 Although the type VI pit pattern was not displayed in the lesion on magnifying chromoendoscopy, the possibility of intramucosal cancer could not be ruled out from the tumor size, and en bloc resection was required. Generally, the limit of the tumor size for reasonable en bloc resection by endoscopic mucosal resection is reported to be 20 mm.3 Thus, we decided to resect the lesion by ESD (Video 1, available online at www.giejournal.org).
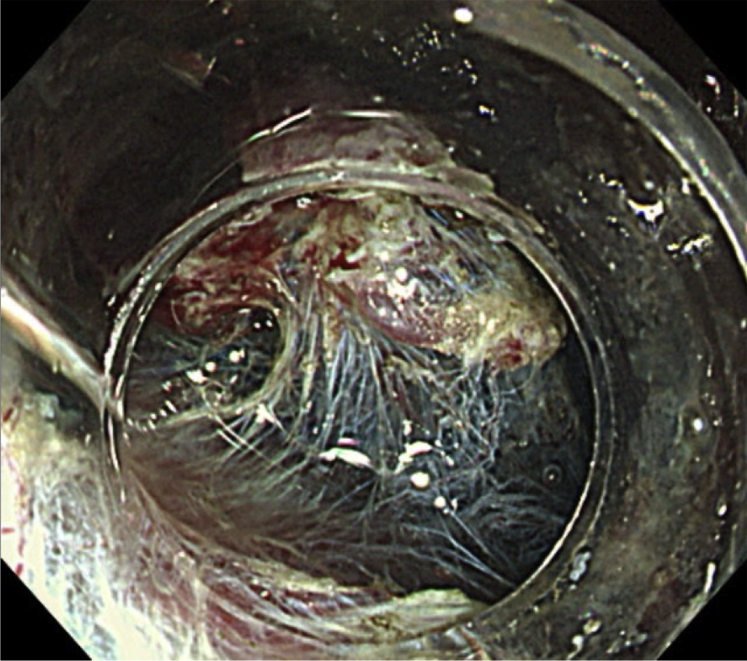
Figure 1.
A flat elevated lesion of approximately 25 mm was detected in the inferior aspect of the cecum.
Figure 2.
Magnifying chromoendoscopy displayed Kudo’s pit pattern types ⅢL and Ⅳ.
ESD was independently performed by a less-experienced endoscopist who had performed fewer than 100 colorectal ESD procedures at a nonreferral center. A small-caliber-tip transparent hood (DH-28GR; Fujifilm, Tokyo, Japan) was attached to the tip of a colonoscope (PCF-H290TI; Olympus, Tokyo, Japan). A mixture of glycerol, sodium hyaluronate, and indigo carmine was used for the submucosal injection. An electrosurgical generator (VIO 3; ERBE Elektromedizin GmbH, Tubingen, Germany) was set at endocut I (effect: 2, duration: 2, interval: 2) for mucosal incision and was set at swift coagulation effect 3 for submucosal dissection. A mucosal incision was performed mainly using DualKnife J (KD-655Q, Olympus) and submucosal dissection was performed mainly using an insulated-tip knife nano (KD-612Q, Olympus).
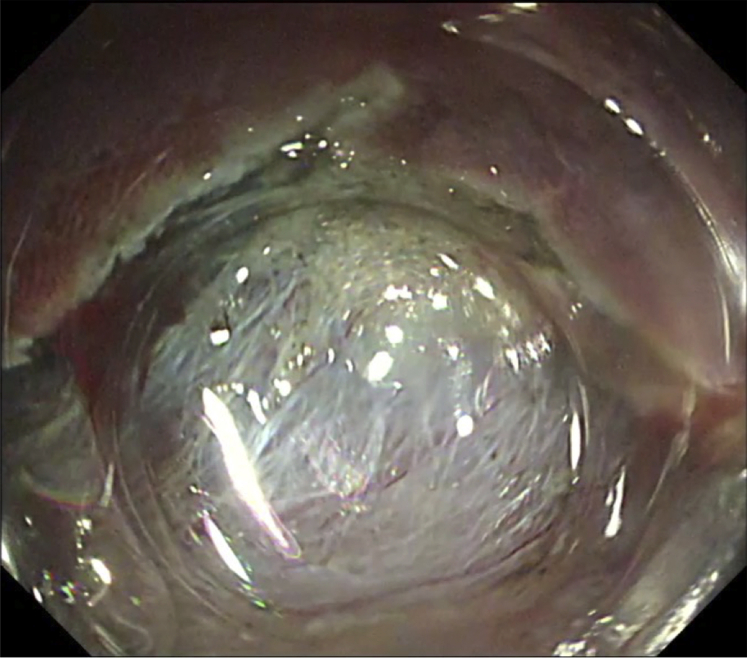
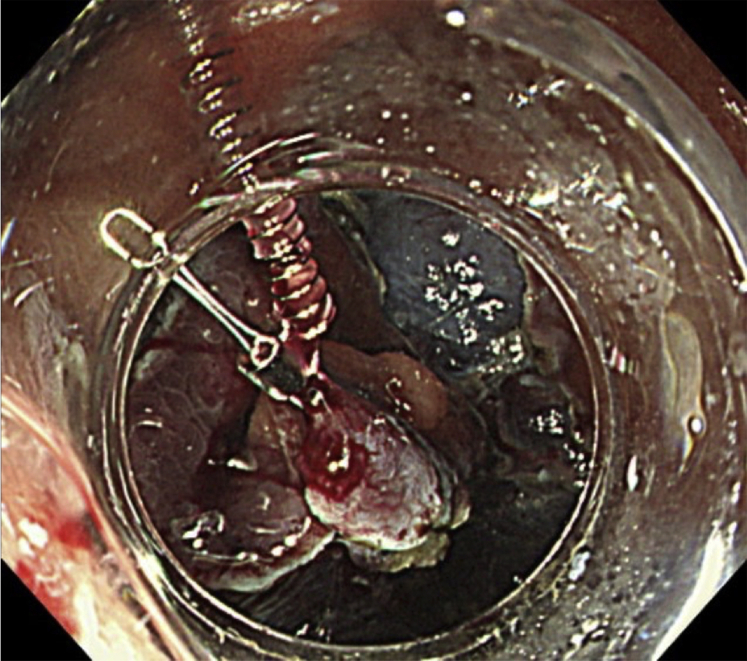
Mucosal incision and submucosal dissection were initially performed from the proximal side. The submucosal tissue on the proximal side was sufficiently exposed, and a circumferential incision was made around the lesion. However, sufficient space could not be secured for submucosal dissection, and confrontation of the endoscope vertically with the muscular layer occurred (Fig. 3). Therefore, we attached an endoclip with a ring-loaded spring (S-O clip, TC1H05; Zeon Medical, Tokyo, Japan) to the proximal edge of the nonneoplastic margin and towed the proximal edge to the opposite bowel wall on the anal side with another endoclip (Fig. 4).
Figure 3.
The endoscopic view confronted the muscular layer, and sufficient space to perform the submucosal dissection could not be secured.
Figure 4.
An S-O clip was attached to the proximal edge of the nonneoplastic margin.
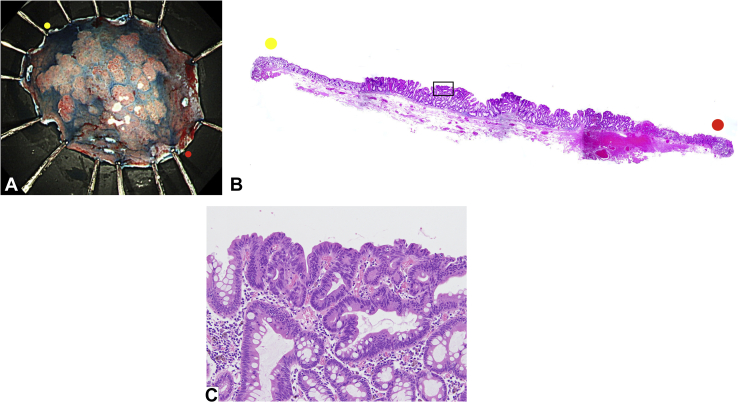
Use of the S-O clip improved the visibility of the submucosal layer even from a middle distance. Confrontation of the endoscope vertically with the muscular layer was avoided and enabled easy identification of the dissection line (Fig. 5). The lesion was successfully resected en bloc without any procedure-associated adverse events. The resected specimen showed a high-grade tubular adenoma measuring 23 × 15 mm, with a free margin (Fig. 6). Curative resection was achieved, and we are planning to perform surveillance total colonoscopy on the patient at 1 year after the ESD. Several reports have already been published regarding the usefulness of the S-O clip in colorectal ESD.4,5
Figure 5.
By using the S-O clip, the visibility of the submucosal layer was improved even from a middle distance, and confrontation of endoscope vertically with the muscular layer was avoided, enabling easy identification of the dissection line.
Figure 6.
The resected specimen and histopathological findings. A, The resected specimen. The tumor was well demarcated, flat, and elevated. B, A panoramic image of the line connecting the yellow and red points in (A) (H&E staining). C, A magnified image of the black box in (B). Histopathological findings indicated tubular adenoma with high-grade atypia (H&E, orig. mag. ×100).
In conclusion, we demonstrated that ESD coupled with S-O clip traction is an effective method, particularly for lesions in the inferior aspect of the cecum. Our present method enables safe endoscopic resection to be performed even by less-experienced endoscopists.
Disclosure
All authors disclosed no financial relationships.
Acknowledgments
We are indebted to Taku Sakamoto, associate professor of the Department of Gastroenterology, Graduate School of the Institute of Clinical Medicine, University of Tsukuba, for his advice on manuscript revision. We thank Miki Saito of Niizashiki Central General Hospital for her assistance with the endoscopic procedures. We are indebted to Helena Popiel, assistant professor of the Department of International Medical Communications of Tokyo Medical University, for her editorial review of this manuscript.
Supplementary data
Endoscopic submucosal dissection using traction by a spring-and-loop with clip for a laterally spreading tumor in the inferior aspect of the cecum: a nonreferral center experience.
References
- 1.Saito Y., Uraoka T., Yamaguchi Y., et al. A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video) Gastrointest Endosc. 2010;72:1217–1225. doi: 10.1016/j.gie.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Kudo S., Hirota S., Nakajima T., et al. Colorectal tumours and pit pattern. J Clin Pathol. 1994;47:880–885. doi: 10.1136/jcp.47.10.880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tanaka S., Oka S., Chayama K. Colorectal endoscopic submucosal dissection: present status and future perspective, including its differentiation from endoscopic mucosal resection. J Gastroenterol. 2008;43:641–651. doi: 10.1007/s00535-008-2223-4. [DOI] [PubMed] [Google Scholar]
- 4.Sakamoto N., Osada T., Shibuya T., et al. Endoscopic submucosal dissection of large colorectal tumors by using a novel spring-action S-O clip for traction (with video) Gastrointest Endosc. 2009;69:1370–1374. doi: 10.1016/j.gie.2008.12.245. [DOI] [PubMed] [Google Scholar]
- 5.Tamari H., Oka S., Ninomiya Y., et al. Use of a new traction device to expose the base of a pedunculated appendiceal polyp. VideoGIE. 2020;6:38–40. doi: 10.1016/j.vgie.2020.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic submucosal dissection using traction by a spring-and-loop with clip for a laterally spreading tumor in the inferior aspect of the cecum: a nonreferral center experience.
Endoscopic submucosal dissection using traction by a spring-and-loop with clip for a laterally spreading tumor in the inferior aspect of the cecum: a nonreferral center experience.