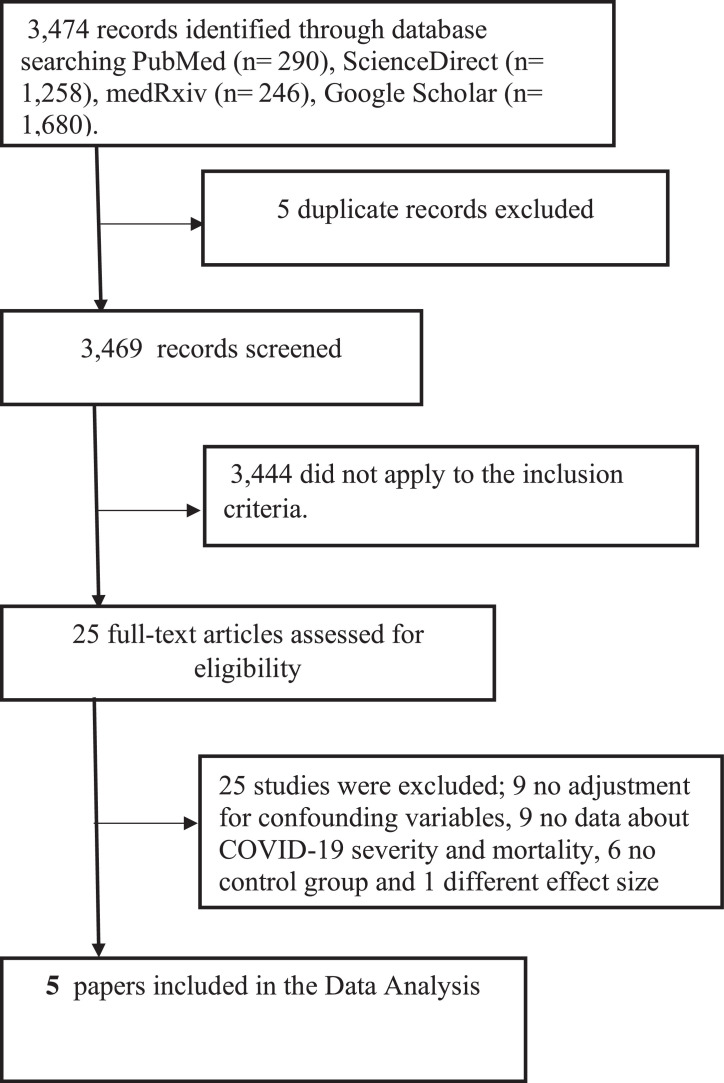
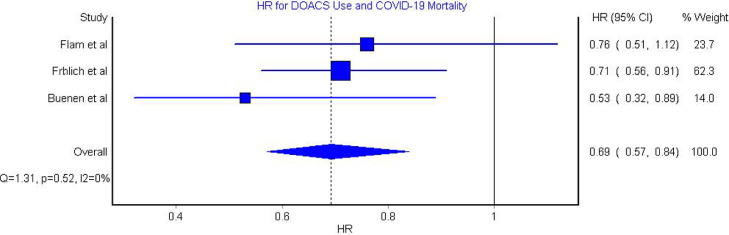
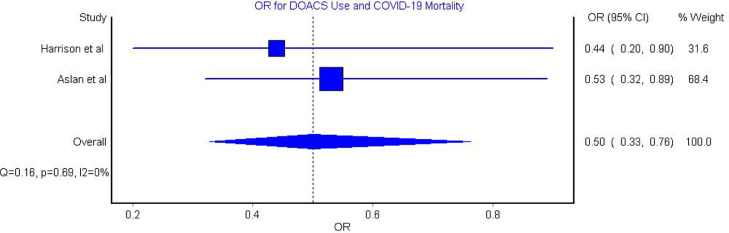
The COVID-19 pandemic has caused millions of cases and deaths, resulting in a public health emergency. It is well established that 1 of the complications of infections in critically ill patients is disseminated intravascular coagulation. This complication is driven by the activation of multiple systemic coagulation and inflammatory responses.1 From the beginning of the pandemic, early reports from Wuhan showed that patients with COVID-19 experienced abnormal coagulation, demonstrated by abnormal prothrombin time and partial thrombin time and elevated d-dimer.1 Furthermore, several studies showed that patients with COVID-19 with high d-dimer had worse outcomes and severe clinical courses.2 Presently, venous thromboembolism (VTE) prophylaxis is recommended for all patients with COVID-19 who are admitted to the hospital.1 Consequently, it was very important to establish whether oral preparation of VTE prophylaxis can prevent severe and fatal COVID-19 outcomes among patients with COVID-19. The following databases: PubMed, ScienceDirect, Google Scholar, and medRxiv were searched up to September 16 2021, using “COVID-19” and “oral anticoagulation” and their related medical subject headings terms. Studies were included if they were cohort or case control in design, included patients with COVID-19, compared between patients on direct oral anticoagulants (DOACs) before COVID-19 diagnosis and control group in terms of COVID-19 severity and mortality, and adjusted for confounding variables. The exposure of interest was the use of DOACs before COVID-19 infection regardless of the type of the used DOACs and the outcome of interest was COVID-19 severity and mortality. COVID-19 mortality was defined as death and COVID-19 severity was defined as mechanical ventilation and intensive care unit (ICU) admission. The quality of the included studies was assessed using the Newcastle-Ottawa scale for observational studies. The adjusted odds ratio (OR) and adjusted hazard ratio (HR) and its related 95% confidence interval (95% CI) were pooled using the random effects model using Meta XL, version 5.3 (EpiGear International, Queensland, Australia). Cochran Q heterogeneity test and I2 statistic were performed to estimate the heterogeneity. The search yielded 3,474 articles; after deduplication and applying the inclusion criteria, 5 articles3, 4, 5, 6 were included in the data extraction (Figure 1 ). The total number of patients with COVID-19 in the included articles was 148,027. Of them, 70.5% (104,429/148,031) were previous DOAC users and the rest were controls. The quality of all of the included studies was good (9/9). Furthermore, 0.4% (400/104,429) of patients taking DOAC developed severe or fatal COVID-19 infection. In comparison, 4.9% (2,126/43,602) of controls developed severe or fatal COVID-19 infection. The analysis of the HRs showed that DOAC use was significantly associated with reduced risk of COVID-19 severity and mortality (HR 0.69, 95% CI 0.57 to 0.84; Figure 2 ) and the heterogeneity of this model was insignificant (I2 = 0%, p = 0.52). In the OR model, DOAC use was significantly associated with a reduced risk of COVID-19 severity and mortality (OR 0.50, 95% CI 0.33 to 0.76; Figure 3 ) and the heterogeneity of this model was insignificant (I2 = 0%, p = 0.69). Our analysis models revealed that patients who used DOACs before COVID-19 infection had a significant reduction by 50% and 31% in the risk of ICU admission, mechanical ventilation, and death because of COVID-19. This result was similar across all of the included studies except 1.3 It was well established that COVID-19 increases the risk for both arterial and venous thrombosis. Several studies showed that patients in the ICU with COVID-19 had higher incidence of VTE compared with matched patients in the ICU who were COVID-19-negative.7 Similarly, patients with acute respiratory distress syndrome because of COVID-19 experienced more VTE than their counterparts who had acute respiratory distress syndrome but were COVID-19 negative.8 Consequently, it was important to conduct studies that assess the benefits and risks of the use of anticoagulants. A large cohort study showed that patients with COVID-19 who received prophylactic anticoagulants had lower 30-day mortality with no increase in the risk for bleeding compared with patients who did not receive prophylactic anticoagulants.9 In contrast, the ACTIV (Accelerating COVID-19 Therapeutic Interventions) trial did not support using anticoagulants agents in treating nonhospitalized patients with COVID-19.10 Yet, the trial did not recruit patients with elevated risk for thromboembolic events or deaths and therefore was underpowered to assess the effect of anticoagulants on patients with COVID-19. This indicates that using anticoagulants among patients with COVID-19 should be considered according to the clinical picture. Accordingly, the relative impact of anticoagulants could be enhanced using the CHADS score which is a nonspecific tool but shown to be prognostic in patients with COVID-19.11 Because our meta-analysis included data from a large number of patients with COVID-19 who use DOACs, taken from 5 studies, and all of them were adjusted extensively for multiple potential confounding factors—the findings can be considered reliable. Our findings suggest a reduction in COVID-19 mortality and severity among patients with COVID-19 with previous use of DOACs. This supports the evidence that VTE is a very important prognostic factor among patients with COVID-19. Also, this substantiates the benefits of DOAC use in improving the outcomes of several diseases. However, much is left to be determined about which dose of DOAC is the most beneficial and when to start the therapy among patients with COVID-19. This necessitates the need for more data from well-designed prospective studies and clinical trials to support our results.
Figure 1.
Flow chart
Figure 2.
Hazard Ratio for the Association between DOACS use and COVID-19 Severity and Mortality.
Figure 3.
Odds Ratio for the Association between DOACS use and COVID-19 Severity and Mortality.
Funding
None.
Disclosures
The authors have no conflicts of interest to declare.
References
- 1.Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020;135:2033–2040. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study [published correction appears in Lancet 2020;395:1038] [published correction appears in Lancet 2020;395:1038] Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flam B, Wintzell V, Ludvigsson JF, Mårtensson J, Pasternak B. Direct oral anticoagulant use and risk of severe COVID-19. J Intern Med. 2021;289:411–419. doi: 10.1111/joim.13205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harrison RF, Forte K, Buscher MG, Jr, Chess A, Patel A, Moylan T, Mize CH, Werdmann M, Ferrigno R. The association of preinfection daily oral anticoagulation use and all-cause in hospital mortality from novel coronavirus 2019 at 21 days: a retrospective cohort study. Crit Care Explor. 2021;3:e0324. doi: 10.1097/CCE.0000000000000324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buenen AG, Sinkeldam M, Maas ML, Verdonschot M, Wever PC. Prior use of anticoagulation is associated with a better survival in COVID-19. J Thromb Thrombolysis. 2021;52:1207–1211. doi: 10.1007/s11239-021-02486-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aslan B, Akyüz A, Işık F, Çap M, İnci Ü, Kaya İ, Karahan MZ, Aktan A, Bilge Ö, Özbek M, Altıntaş B, Boyraz B. The effect of chronic DOAC treatment on clinical outcomes of hospitalized patients with COVID-19. Int J Clin Pract. 2021;75:e14467. doi: 10.1111/ijcp.14467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Helms J, Tacquard C, Severac F, Leonard-Lorant I, Ohana M, Delabranche X, Merdji H, Clere-Jehl R, Schenck M, Fagot Gandet F, Fafi-Kremer S, Castelain V, Schneider F, Grunebaum L, Anglés-Cano E, Sattler L, Mertes PM, Meziani F, CRICS TRIGGERSEP Group (Clinical Research in Intensive Care and Sepsis Trial Group for Global Evaluation and Research in Sepsis) High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46:1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rentsch CT, Beckman JA, Tomlinson L, Gellad WF, Alcorn C, Kidwai-Khan F, Skanderson M, Brittain E, King JT, Jr, Ho YL, Eden S, Kundu S, Lann MF, Greevy RA, Jr, Ho PM, Heidenreich PA, Jacobson DA, Douglas IJ, Tate JP, Evans SJW, Atkins D, Justice AC, Freiberg MS. Early initiation of prophylactic anticoagulation for prevention of coronavirus disease 2019 mortality in patients admitted to hospital in the United States: cohort study. BMJ. 2021;372:n311. doi: 10.1136/bmj.n311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Connors JM, Brooks MM, Sciurba FC, Krishnan JA, Bledsoe JR, Kindzelski A, Baucom AL, Kirwan BA, Eng H, Martin D, Zaharris E, Everett B, Castro L, Shapiro NL, Lin JY, Hou PC, Pepine CJ, Handberg E, Haight DO, Wilson JW, Majercik S, Fu Z, Zhong Y, Venugopal V, Beach S, Wisniewski S, Ridker PM, ACTIV-4B Investigators Effect of antithrombotic therapy on clinical outcomes in outpatients with clinically stable symptomatic COVID-19: the ACTIV-4B randomized clinical trial. JAMA. 2021;326:1703–1712. doi: 10.1001/jama.2021.17272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ruocco G, McCullough PA, Tecson KM, Mancone M, De Ferrari GM, D'Ascenzo F, De Rosa FG, Paggi A, Forleo G, Secco GG, Pistis G, Monticone S, Vicenzi M, Rota I, Blasi F, Pugliese F, Fedele F, Palazzuoli A. Mortality risk assessment using CHA(2)DS(2)-VASc scores in patients hospitalized with coronavirus disease 2019 infection. Am J Cardiol. 2020;137:111–117. doi: 10.1016/j.amjcard.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]