A 73-year-old male, recently diagnosed with uncontrolled diabetes mellitus, presented with complaints of difficulty in opening the right eye and sudden painless loss of vision.
Clinical examination showed proptosis of the right eye with absent extraocular muscle movements, lid edema, chemosis, circumciliary congestion, fixed and dilated pupil, and no light perception. Fundus examination revealed retinal whitening and central retinal artery occlusion (CRAO). The left eye was unremarkable.
Emergency magnetic resonance imaging (MRI) of the brain, done to rule out any intracranial abnormality, revealed restricted diffusion in the intraocular and intraorbital segments of the right optic nerve [Fig. 1], diagnostic of acute anterior ischemic optic neuropathy (AION) and posterior ischemic optic neuropathy (PION), respectively. The rest of the right optic nerve appeared normal. In addition, axial proptosis of the right eye, bulky edematous right extra ocular muscles, extraconal fat stranding [Fig. 2], and a thin rim of periorbital fluid were suggestive of right orbital cellulitis. Right superior ophthalmic vein and cavernous sinus were normal. Left orbital structures and optic nerve were normal. Incidentally, extensive bilateral ethmoid and maxillary sinusitis [Fig. 2a] were also identified. Thus, a diagnosis of acute invasive fungal sinusitis with concomitant AION and PION was arrived at.
Figure 1.
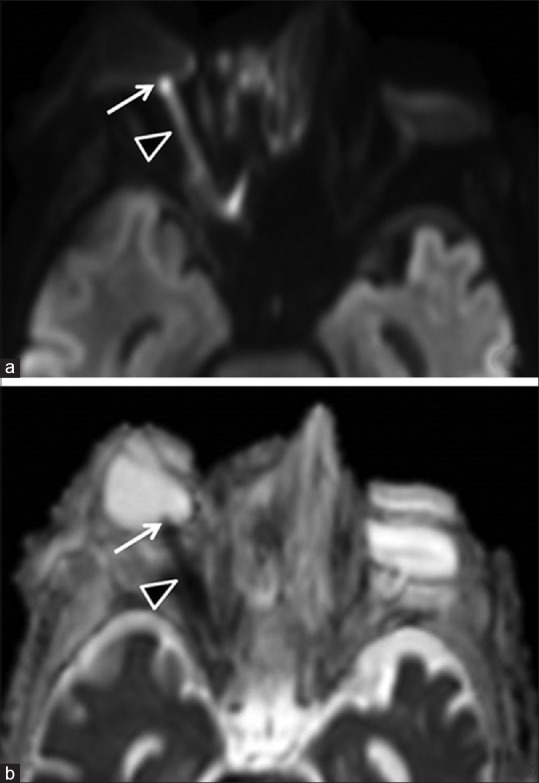
(a) Diffusion-weighted image (DWI) and (b) corresponding apparent diffusion coefficient (ADC) map show restricted diffusion in the intraocular (arrow) and intraorbital (arrowhead) segments of the right optic nerve, representing anterior ischemic optic neuropathy (AION) and posterior ischemic optic neuropathy (PION), respectively. Left optic nerve appears normal
Figure 2.

(a) Coronal STIR image depicting bulky STIR hyperintense right extraocular muscles (especially medial and superior rectii) and surrounding fat stranding (arrowheads) suggestive of orbital cellulitis, bilateral maxillary and ethmoidal sinusitis (arrows). (b) Arrow depicts axial proptosis of the right eye
Histopathology from functional endoscopic sinus surgery specimen confirmed rhino-orbital mucormycosis. The nasopharyngeal swab for SARS-CoV-2 obtained as part of the protocol was positive. No visual recovery was seen on subsequent follow-up.
Discussion
Only few cases of PION due to mucormycosis have been described in literature,[1,2] proposed to be due to angioinvasion of the small meningeal arteries.[2] Visualized as restricted diffusion of the intraorbital segment of the optic nerve,[3] PION is diagnosed on diffusion-weighted image (DWI) MRI even when clinical signs are absent, thereby being advantageous as otherwise PION is a diagnosis of exclusion. In our case, vision loss was attributed only to CRAO and there was no suspicion of PION. AION does not require imaging for diagnosis; however, it has been described in literature as diffusion restriction and postcontrast enhancement of the optic nerve head.[4] The former was seen in our case.
This case is unique as there is concomitant AION and PION, both being demonstrated on DWI imaging, thereby underscoring the significance of DWI. In addition, the patient had CRAO clinically.
We propose the angioinvasive property of the fungus as well as the inflammatory edematous compression as the probable causes; however, the cumulative effect of incidentally detected COVID-19 pneumonia should be considered as an added factor in causing immunosuppression, thereby enhancing the angioinvasive potential of mucor.
Ethical approval and consents
This report describes a rare diagnosis from routine diagnostic procedures. Hence, approval from the institutional review board was not obtained. Written informed consents for all the procedures were obtained before they were performed. For this type of study, consent for publication is not required as the data to be published is sufficiently anonymized.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mathur S, Karimi A, Mafee MF. Acute optic nerve infarction demonstrated by diffusion-weighted imaging in a case of rhinocerebral mucormycosis. AJNR Am J Neuroradiol. 2007;28:489–90. [PMC free article] [PubMed] [Google Scholar]
- 2.Ghabrial R, Ananda A, van Hal SJ, Thompson EO, Larsen SR, Heydon P, et al. Invasive fungal sinusitis presenting as acute posterior ischemic optic neuropathy. Neuroophthalmology. 2017;42:209–14. doi: 10.1080/01658107.2017.1392581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al-Shafai LS, Mikulis DJ, Diffusion MR. imaging in a case of acute ischemic optic neuropathy. AJNR Am J Neuroradiol. 2006;27:255–7. [PMC free article] [PubMed] [Google Scholar]
- 4.Adesina OO, Scott McNally J, Salzman KL, Katz BJ, Warner JE, McFadden M, et al. Diffusion-weighted imaging and post-contrast enhancement in differentiating optic neuritis and non-arteritic anterior optic neuropathy. Neuroophthalmology. 2017;42:90–8. doi: 10.1080/01658107.2017.1356856. [DOI] [PMC free article] [PubMed] [Google Scholar]


