Abstract
Background.
Oral contraceptive use has been previously associated with an increased risk of suicidal behavior in some, but not all, samples. The use of large, representative, longitudinally-assessed samples may clarify the nature of this potential association.
Methods.
We used Swedish national registries to identify women born between 1991 and 1995 (N = 216 702) and determine whether they retrieved prescriptions for oral contraceptives. We used Cox proportional hazards models to test the association between contraceptive use and first observed suicidal event (suicide attempt or death) from age 15 until the end of follow-up in 2014 (maximum age 22.4). We adjusted for covariates, including mental illness and parental history of suicide.
Results.
In a crude model, use of combination or progestin-only oral contraceptives was positively associated with suicidal behavior, with hazard ratios (HRs) of 1.73–2.78 after 1 month of use, and 1.25–1.82 after 1 year of use. Accounting for sociodemographic, parental, and psychiatric variables attenuated these associations, and risks declined with increasing duration of use: adjusted HRs ranged from 1.56 to 2.13 1 month beyond the initiation of use, and from 1.19 to 1.48 1 year after initiation of use. HRs were higher among women who ceased use during the observation period.
Conclusions.
Young women using oral contraceptives may be at increased risk of suicidal behavior, but risk declines with increased duration of use. Analysis of former users suggests that women susceptible to depression/anxiety are more likely to cease hormonal contraceptive use. Additional studies are necessary to determine whether the observed association is attributable to a causal mechanism.
Keywords: Cohort study, oral contraception, registry data, suicidal behavior
Introduction
The use of oral contraception (OC) among women is common, with at least 20% of reproductive-aged women in relationships reporting use in 31 countries in 2015 (United Nations, 2015). In the USA, 16.6% of women aged 15–19 and 19.5% of women aged 20–29 reported use in 2015–2017 (Daniels & Abma, 2018). OC is effective at preventing pregnancies and can be used to mitigate menstrual symptoms (Oinonen & Mazmanian, 2002), but is not without adverse side effects: sex hormones are known to impact mood and behavior (McEwen & Milner, 2017), and some prior research has identified a positive association between OC use and depressive symptoms (Skovlund, Morch, Kessing, & Lidegaard, 2016), though findings are inconsistent (Keyes et al., 2013).
OC may also impact the risk of suicidal behavior, which is itself a public health concern. Nearly 800 000 people die by suicide globally each year (World Health Organization. Reproductive Health and Research, 2010). Several countries, including the USA (Curtin, Warner, & Hedegaard, 2015), are experiencing increased rates of suicide; and there are manyfold more suicide attempts than deaths by suicide (Piscopo, Lipari, Cooney, & Glasheen, 2016; Substance Abuse and Mental Health Services Administration, 2018), and suicidal behavior is especially high among young women (Baca-Garcia, Perez-Rodriguez, Mann, & Oquendo, 2008). Relatively few studies have examined the association between OC use and suicidal behavior in population-based cohorts. Most prior reports are based on longitudinal studies of British women, ranging in size from ∼17 000 to 167 000 women, which all found non-significant increases in the risk of suicide completion among OC users (Beral et al., 1999; Colditz, 1994; Hannaford et al., 2010; Vessey, Villard-Mackintosh, McPherson, & Yeates, 1989). However, one study of a US cohort reported a significant positive association between OC and death by suicide (Charlton et al., 2014); another study, using a circumscribed sample of sexually active US women, found a negative association between OC use and past-year suicide attempts (Keyes et al., 2013).
More recently, a study by Skovlund, Morch, Kessing, Lange, and Lidegaard (2018) reported a positive association between contraceptive use and risk of suicidal behavior (attempts and completions) using Danish registry-based data and a sample size of nearly half a million women. Risk of a first suicide attempt was most pronounced in the first 2 months of contraceptive use and remained elevated for at least 1 year after the initiation of use; women aged 15–19 were at higher risk than those aged 20 or older. Importantly, a mediation analysis demonstrated that the observed association was attenuated, though not eliminated, with the inclusion of a mediation pathway through depression.
Some women with a psychiatric disorder (e.g. major depression) may use hormonal contraception to help control their mood-related menstrual symptoms (Pagano, Zapata, Berry-Bibee, Nanda, & Curtis, 2016), and in these cases, risk of suicidal behavior may be attributable to the underlying psychiatric issues rather than to contraceptive use per se. In addition, as noted above, OC use has been associated with depression or depressive symptoms in some samples (Skovlund et al., 2016) or subgroups of women (Duke, Sibbritt, & Young, 2007); others have reported no association (Duke et al., 2007; Toffol, Heikinheimo, Koponen, Luoto, & Partonen, 2011, 2012). A large study of Swedish women aged 12–30 reported an association between contraceptive use and psychotropic prescription drug use (which may be prescribed to treat conditions other than depressive or anxiety disorders), but only among adolescents (Zettermark, Perez Vicente, & Merlo, 2018). These overall inconsistencies may be due to differences across studies in the age range of the samples, participants’ motivations for using contraception, duration of use, or other factors (Robakis, Williams, Nutkiewicz, & Rasgon, 2019). Given the uncertainty surrounding this association, consideration of psychiatric history is critical when evaluating the association between hormonal contraceptives and suicidality.
Given the widespread use of OC, a clear understanding of their potential risks is of high public health relevance. In the current study, we assess whether OC use among young women aged 15–22 is associated with risk of suicidal behavior, using data drawn from Swedish national registries. We examine potential changes in risk as a function of the duration of use, and control for sociodemographic, familial, and psychiatric covariates.
Materials and methods
Sample
We linked nationwide Swedish registers via the unique 10-digit identification number assigned at birth or immigration to all Swedish residents. The identification number was replaced by a serial number to ensure anonymity. The following sources were used to create our dataset: the Total Population Register, containing information about the year of birth and sex; the Multi-Generation Register, linking individuals born after 1932 to their parents; the medical birth register with information on all births from 1972 to 2014; the Longitudinal integrated database for health insurance and labor market studies, from 1990 to 2014 containing information on parental education; the Prescribed Drug Register, containing all prescriptions in Sweden picked up by patients from 2005 to 2014; the Hospital Discharge Register, containing hospitalizations for Swedish inhabitants from 1964 to 2014; the Outpatient Care Register, containing information from outpatient clinics from 2001 to 2014; and regional Primary Health Care Registers, for which availability varies by region due to different timing of digitalizing of the patient records (see online Supplemental Methods). We include all females in Sweden who turned 15 in August 2006 or later; this allowed us to obtain at least one full year of coverage of prescribed OC prior to age 15, resulting in a sample aged 15–22.
Outcome and predictor variables
The outcome of interest was the first instance of suicidal behavior (suicide attempt or suicide death). Cases were defined using the ICD-10 codes X60-X84 and Y10-Y34. The predictor of interest was oral contraceptive use. OC use was identified using the Anatomical Therapeutic Chemical (ATC) Classification System and divided into progestin-only pills and oral combination pills (see online Supplemental Methods for corresponding ATC codes), as progestin-only pills are frequently prescribed to women for whom combination pills are contraindicated (White et al., 2012; World Health Organization. Reproductive Health and Research, 2010) and these groups may differ with respect to risk. The duration was assumed to be in accordance with the number of pills picked up (typically 3 months). We further allowed a 28-day period after the prescription was obtained to account for a lag before the women began taking pills from that prescription.
Women with a suicidal event prior to age 15 were censored. Women were censored when they became pregnant, with the start of pregnancy defined as 9 months before childbirth, and thereafter. Women diagnosed with certain medical conditions were censored at the time of diagnosis. These were polycystic ovarian syndrome, endometriosis, venous thromboembolism, and cancer (except skin tumor); see online Supplemental Methods for ICD codes. Women who ceased using oral contraceptives during the observation period were excluded from the main analysis, but a sensitivity analysis was conducted to examine their risk.
Socioeconomic status was assessed using biological parent’s highest level of education during their lifetime, which was categorized into low (compulsory school only), middle (high school level) or high (university level). Parental history of suicide was a binary variable, where individuals with a parental history of suicide attempt/death (defined in accordance with the definition above) were coded 1 and others coded 0. Depression and anxiety disorders (DAD) were defined using ICD-10 codes F32, F33, F40 and F41; DAD was included as a time-varying covariate due to prior evidence that OC use can increase symptoms of DAD. We defined lifetime history of bipolar or non-affective psychosis (BPN) using ICD-10 codes F31, F20, F21, F22, F23, F24, F25, F26, F27, F28, and F29. Individuals could not be coded as having both DAD and BPN; women with both diagnoses were coded as having BPN only.
Statistical analyses
We used Cox proportional hazard models to study the association between OC use and suicidal behavior. We followed young women starting from age 15 until first registration for suicidal behavior, censoring (see above for conditions that led to censoring), or end of follow-up (31 December 2013), whichever came first. We used age as the underlying time scale, and contraceptive use was included as a time-dependent variable, with combination pills and progestin-only pills analyzed separately based on prior evidence of differential associations with mood disorders (Svendal et al., 2012) and suicidal behavior (Skovlund et al., 2018). To evaluate whether a possible effect of contraceptives varied during follow-up time, i.e. whether the proportionality assumption was fulfilled, we utilized three different approaches to model the effect of time: a linear model, a logarithmic model, and a quadratic model. We selected the best fitting model, and after running an initial crude model, we ran a model that adjusted for parental education. A subsequent model further adjusted for parental history of suicide attempt, which in the hypothetical case corresponds to where all confounders were adjusted for, providing an estimate of the total effect of contraceptive use on SA. To explore the effect of psychiatric disorders, we further included DAD and BPN. DAD was included as time-dependent variable while BPN was considered a lifetime characteristic.
We conducted a series of secondary/sensitivity analyses, many of which are reported in the online Supplemental Material, to facilitate interpretation of the primary model results. To address the problem with individual confounding - that is, that some women might be more inclined to both contraceptive use and suicide attempt - we used a frailty model to account for within-individual clustering of repeated observations. We further compared the risk of suicidal behavior in former users to current users, adjusting for the same covariates as above. We randomly matched each former user to a young woman, on the same class of contraceptive, born the same year, who starts to use OC at the same age (within 6 months), but who were still using OC when the former user stopped. We also tested whether OC use and suicidal behavior were associated outside the context of OC use leading to DAD by conducting an analysis in which women who received a DAD registration after OC use initiation were censored. Finally, we re-ran the primary model with the exclusion of women with a lifetime registration for BPN.
Results
Descriptive statistics
Data were available for N = 216 702 women, representing 899 997.8 person years of observation. Of these, 69 507 (32.07%) women had no record of hormonal contraceptive use, 97 515 (45.00%) used only combination pills during the observation period, 23 468 (10.83%) used only progestin-only pills, and 26 212 (12.10%) used both combination and progestin-only pills. Across the observation period, there were 1395 suicidal events (1359 non-fatal attempts and 36 deaths), corresponding to 15.50 suicidal events per 10 000 person years. The rate was 14.90 among those who never used hormonal contraception, 15.10 among those who used combination pills at the time of suicidal event, and 23.11 among women using progestin-only pills at the time of suicidal event. The mean age at suicidal event was 16.89 (S.D. = 1.35). Table 1 provides additional descriptive statistics on the sample.
Table 1.
Descriptive data for sample (total N = 216 702)
| Never users | Used only combination pills | Used only progestin-only pills | Used both progestin-only and combination pills | |
|---|---|---|---|---|
| Sample size | 69 507 (32.07%) | 97 515 (45.00%) | 23 468 (10.83%) | 26 212 (12.10%) |
| Mean (S.D.) age, start of taking pills | n/a | 17.16 (1.42) | 17.27 (1.49) | 16.51 (1.14) |
| Mean (S.D.) age, end of follow up | 19.73 (1.43) | 19.67 (1.45) | 19.52 (1.53) | 20.21 (1.33) |
| Parental education | ||||
| Low | 2934 (4.22%) | 2003 (2.05%) | 661 (2.82%) | 684 (2.61%) |
| Mid | 25 512 (36.70%) | 41 270 (42.32%) | 10 766 (45.88%) | 11 972 (45.67%) |
| High | 41 061 (59.07%) | 54 242 (55.62%) | 12 041 (51.31%) | 13 556 (51.72%) |
| Parental suicidal attempt | 1405 (2.01%) | 2145 (2.20%) | 734 (3.13%) | 748 (2.85%) |
| Lifetime depression or anxiety (DAD) | 11 029 (15.54%) | 17 822 (18.27%) | 5328 (22.40%) | 6321 (24.11%) |
| Lifetime bipolar disorder or non-affective psychosis (BPN) | 849 (1.20%) | 1026 (1.05%) | 385 (1.64%) | 391 (1.49%) |
s.d., standard deviation; DAD, depressive and anxiety disorders; BPN, bipolar disorder and non-affective psychosis.
Survival models
In an initial crude model, OC use was positively associated with suicidal behavior for both combination pills [HR = 1.40 (95% CI 1.22–1.60)] and progestin-only pills [HR = 2.18 (1.81–2.62)]. We next tested several models to determine which provided the best fit to the data without violations to the proportionality assumption of the Cox model. A model that included a quadratic time effect provided the best fit (AIC = 33 657.40; linear time model AIC = 33 659.66; log-transformed time model AIC = 33 661.02) and was selected for expansion.
Table 2 presents findings from the crude model and a series of adjusted models. For ease of interpretation, estimated hazard ratios (HRs) have been presented at specific time points. In the crude model, women who used hormonal contraceptives (combination or progestin-only pills) were at increased risk of suicidal events: 1 month after onset of OC use, for combination pills the HR was 1.73 (1.44–2.08) and for progestin-only pills, the HR was 2.78 (2.14–3.62). Risk of suicidal behavior declined substantially with increased duration of OC use but remained elevated 1 year beyond the initiation of use [combination pills HR = 1.25 (1.06–1.47); progestin-only pills HR = 1.82 (1.44–2.31)].
Table 2.
Hazard ratios and 95% confidence intervals from crude (unadjusted) and adjusted models with a quadratic effect of time.
| Model | ||||
|---|---|---|---|---|
| Crude | Adjusted 1 | Adjusted 2 | Adjusted 3 | |
| Predictor | AIC = 33 657.40 | AIC = 33 654.66 | AIC = 33 550.92 | AIC = 31 042.23 |
| Combination pills v. no contraception (time 1 month) | 1.73 (1.44–2.08) | 1.73 (1.44–2.08) | 1.71 (1.42–2.06) | 1.56 (1.30–1.88) |
| Combination pills v. no contraception (time 3 months) | 1.61 (1.38–1.88) | 1.61 (1.38–1.89) | 1.60 (1.37–1.87) | 1.47 (1.26–1.72) |
| Combination pills v. no contraception (time 6 months) | 1.47 (1.28–1.68) | 1.47 (1.28–1.68) | 1.45 (1.26–1.67) | 1.36 (1.18–1.56) |
| Combination pills v. no contraception (time 12 months) | 1.25 (1.06–1.47) | 1.25 (1.06–1.47) | 1.24 (1.05–1.46) | 1.19 (1.01–1.40) |
| Progestin-only pills v. no contraception (time 1 month) | 2.78 (2.14–3.62) | 2.77 (2.13–3.61) | 2.70 (2.08–3.51) | 2.13 (1.64–2.77) |
| Progestin-only pills v. no contraception (time 3 months) | 2.53 (2.03–3.15) | 2.52 (2.02–3.14) | 2.46 (1.97–3.07) | 1.96 (1.57–2.44) |
| Progestin-only pills v. no contraception (time 6 months) | 2.23 (1.84–1.70) | 2.22 (1.83–1.70) | 2.17 (1.79–2.63) | 1.75 (1.44–2.12) |
| Progestin-only pills v. no contraception (time 12 months) | 1.82 (1.44–2.31) | 1.82 (1.44–2.30) | 1.78 (1.41–2.25) | 1.48 (1.17–1.87) |
| Parental education, mid v. low | 0.74 (0.56–0.97) | 0.76 (0.58–1.00) | 0.79 (0.60–1.04) | |
| Parental education, high v. low | 0.69 (0.53–0.91) | 0.73 (0.56–0.96) | 0.75 (0.57–0.98) | |
| Parental suicidal attempt | 3.51 (2.87–4.29) | 2.21 (1.80–2.71) | ||
| DAD | 20.10 (17.73–22.79) | |||
| BPN (lifetime) | 31.27 (27.14–36.04) | |||
DAD, depressive and anxiety disorders; BPN, bipolar disorder and non-affective psychosis.
HRs for suicidal behavior at specific time points after the onset of oral contraceptive use are presented. See Fig. 1 for the overall trajectory of risk
Adjusting for parental education and parental history of suicidal event did not substantively impact suicidal behavior risks associated with contraception (Table 2, Adjusted Models 1 and 2, respectively). However, further accounting for a history of DAD (included as time-varying), and BPN (included as lifetime) attenuated the effect of both types of contraception (Adjusted Model 3 and Fig. 1). In this model, after 1 year of combination pill use, the lower confidence limit approached 1, while progestin-only pills remained more strongly associated with risk of suicidal behavior. As illustrated in Fig. 1, for both combination and progestin-only pills, the decline in risk begins to plateau between 1.5 and 2 years after initiation of OC use and remains above 1 for progestin-only pills. Given that internalizing disorders are associated with increased risk of suicidal behavior, and the possibility that OC use exacerbates internalizing symptoms, we further explored the relationship between OC use and suicidal behavior in the context of DAD. Complete results are presented in the online Supplemental Material. In brief, the OC-based risk of suicidal behavior among women using OC who had experienced DAD was less pronounced than among OC users without a prior DAD registration.
Fig. 1.
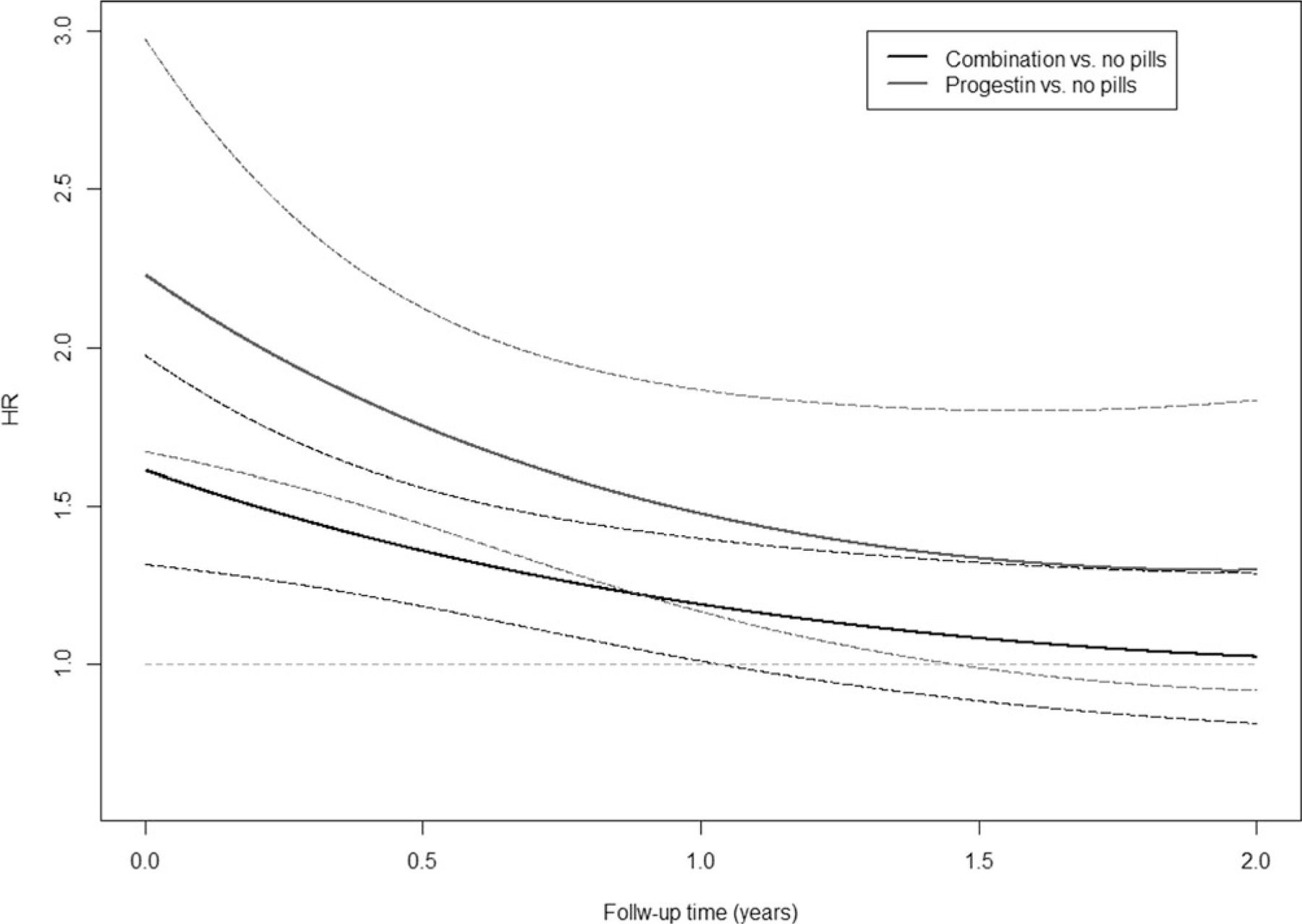
Hazard ratios (solid lines) and 95% confidence intervals (dashed lines) for the association between oral hormonal contraceptive use and suicidal behavior, as a function of follow-up time. Results correspond to Adjusted Model 3 in Table 2. The y-axis is on a linear scale.
Frailty model
We used a frailty model to address shifts in the risk of suicidal behavior before and after initiation of OC use. Results from the crude model closely paralleled the corresponding primary analysis: for combination pills, the HR was estimated at 1.40 (1.22–1.60) and for progestin-only pills HR = 2.31 (1.78–2.99). As in the primary analysis, risks associated with OC use were attenuated after inclusion of covariates but remained elevated [combination pills: HR = 1.31 (1.13–1.52); progestin-only pills: HR = 1.78 (1.45–2.20)].
Comparison to former users
Women may stop using OC due to adverse responses (e.g. symptoms of depression or other health concerns), which could be due to pre-existing liabilities. These women may be at increased risk for suicidal behavior. We therefore assessed risk among these users to determine whether, even after they ceased OC use, their risk of suicidal behavior was elevated relative to never users. Among women who went on to cease OC use, the prevalence of DAD registrations in the 3 months (the typical period for which a prescription is written) prior to cessation was 10.1% for combination pill users and 12.1% for progestin-only pill users. Among our matched controls who continued to use OC, the corresponding proportions were slightly lower, 9.28% and 10.75%, respectively. Time-specific HRs are presented in online Supplemental Table 4. HRs ranged from approximately 3 to 4 across the first year post-OC use and were highest immediately after cessation of use.
Sensitivity analyses
Censoring based on depression/anxiety diagnosis
Hormonal contraception may contribute to increases in depressive symptoms, which in turn could increase the risk of suicidal behavior (contraception → DAD → SB). To determine whether contraception persisted as a risk factor for suicidal behavior outside of this pathway, we conducted a sensitivity analysis wherein individuals who had a DAD registration after being prescribed hormonal contraception were censored at the time of their DAD registration (N = 10 162). Results are presented in online Supplemental Table 5. In these adjusted models, OC use was initially associated with suicidal behavior, but by 1 year after the onset of use, the HR did not differ significantly from 1 for users of combination pills [HR = 1.10 (0.92–1.33)]. Progestin-only pill use remained associated with an increased risk of suicidal behavior 1 year after initiation [HR = 1.57 (1.20–2.15)].
Exclusion of bipolar/psychosis cases
Since BPN was the predictor most strongly associated with risk of suicidal behavior (Table 2), we conducted a sensitivity analysis in which individuals with a BPN registration were excluded (N = 2650; 1.22%). Time-specific HRs are presented in online Supplemental Table 6. The associations were comparable to those observed in Adjusted Model 3 (Table 2) and similarly declined with increasing duration of OC use.
Discussion
This study was designed to evaluate whether young women taking oral hormonal contraceptives are at increased risk of suicidal behavior relative to those who do not use oral contraceptives. In a cohort of Swedish women, we found that suicidal behavior is more common among those using oral contraceptives, and that risk declines nonlinearly with increased duration of use. Progestin-only pills were more strongly associated with risk than combination pills; for the latter, no significant association with suicidal behavior was observed beyond approximately 1.5 years of OC use. These findings suggest that young women using oral hormonal contraceptives, and their health care providers, should be vigilant to behavioral/mood changes or other indicators of risk of suicidal behavior, particularly within the first year of use.
Skovlund et al. (2018) reported on the association between hormonal contraceptive use and suicidal behavior in a Danish birth cohort. As in the current study, Skovlund et al. found that the risk of a suicidal event was increased after initiating contraceptive use. In their primary analysis (excluding mediation through psychiatric diagnosis), the effect of contraception on suicide attempt was estimated at HR = 1.97. That model is most comparable to our Adjusted Model 2, in which the corresponding estimate after 1 month of use was HR = 1.71 for combination pills. Likewise, risk in the Danish cohort declined with increasing duration of use, though to a less pronounced degree than observed in the current study.
A potentially important difference between these studies is the age of the samples: due to registry coverage, our sample was limited to those aged 15–22, while the Danish study was able to follow women through age 33. However, risks were most pronounced among the youngest members of the Danish cohort [aged 15–19; HR = 2.06 (1.92–2.21)], which is most closely matched to our sample. The two studies also used different time frames beyond which a prescription ended to classify women as former users (28 days in the current study v. 6 months in Skovlund’s report). Finally, we were unable to assess risks associated with injectable or implanted hormonal contraception due to insufficient sample size and data availability.
Beyond the Danish registry study, few reports on the association between hormonal contraceptive use and risk of suicidal behavior in population-based samples are available. Extant studies examined US or British cohorts and found only non-significant increases in risk (Beral et al., 1999; Colditz, 1994; Hannaford et al., 2010; Vessey et al., 1989), with one exception (Charlton et al., 2014). Given the prevalence of OC use - which was reported by 15–20% of US women aged 15–29 in 2015–2017 (Daniels & Abma, 2018) - understanding the potential risks is of high public health relevance. Importantly, sexual activity among young women is itself associated with suicidal ideation and attempt (Eaton et al., 2011). While we were unable to control for sexual activity in this nationwide sample, Keyes et al. (2013) found that sexually active US women using hormonal contraceptives (oral or otherwise) were less likely to attempt suicide, and reported fewer depressive symptoms, than sexually active women using non-hormonal, or no, contraceptives; it should be noted that restrictions on that sample (e.g. age, duration of OC use) preclude direct comparisons to the current study (Skovlund, 2018). Furthermore, the pre- and perinatal periods are associated with increased suicide risk (Mangla, Hoffman, Trumpff, O’Grady, & Monk, 2019), including among teenage mothers (Orri et al., 2019), though Mota et al. (2019) found that the period of pregnancy was protective in a Canadian cohort (pregnant women and mothers were censored in our analyses). The onset of sexual and reproductive behaviors is accompanied by a wide range of psychosocial factors (Caminis, Henrich, Ruchkin, Schwab-Stone, & Martin, 2007; Furman, Low, & Ho, 2009; Graber, 2013) that may act as confounders between OC use and suicidal behavior, reinforcing the need for studies that enable causal inference to further clarify the mechanism underlying the observed association.
A potential mechanism by which oral contraceptive use may increase the risk for suicidal behavior is via the impact of sex hormones on mood (Marrocco & McEwen, 2016; McEwen & Milner, 2017), which may in turn increase risk of suicidal behavior. While increases in depressive symptoms among women using combination pills have been observed in some studies (Gregory et al., 2018; Kulkarni, 2007; Skovlund et al., 2016), others have observed a negative association or reported null findings (Keyes et al., 2013; Toffol et al., 2011, 2012; Worly, Gur, & Schaffir, 2018; Zethraeus et al., 2017). We found that women with a history of DAD were more likely to be prescribed OC (see online Supplemental Material), which complicates the ability to interpret the contributions of OC v. an underlying liability to mood/anxiety problems. Because of the uncertainty surrounding the pathway from hormonal contraception to psychiatric symptoms to suicidal behavior, we pursued a sensitivity analysis within which women registered for DAD after the onset of contraceptive use were censored. This enabled us to address whether contraceptive use was associated with suicidal behavior among those with pre-existing DAD. The HRs between OC and suicidal behavior were modestly lower than in the primary analysis, but were significantly higher than 1, suggesting that OC use is associated with increased risk of suicidal behavior even when it does not lead to clinically significant internalizing problems.
A notable finding of the current study is that adjusting for parental history of suicidal behavior (N = 5061, 2.32%), which is strongly associated with risk in offspring (HR = 2.21–3.51), did not attenuate the impact of contraceptive use. This suggests that the observed association between contraceptive use and suicidal behavior is not simply due to an underlying familial liability, despite prior evidence that suicidal behavior is, in part, familial (Brent & Mann, 2005; Pedersen & Fiske, 2010). HRs from the frailty model, accounting for within-individual clustering, were consistent with the primary analysis, providing further support for the assertion that confounding factors do not entirely account for the observed association. Still, we are unable to attribute a causal impact of contraception in this observational study, as our sample size was insufficient for conducting co-relative analyses that would further supplement our efforts to assess the role of familial confounding factors.
As is the case with other registry-based analyses, we lacked information on why some women stop OC use. A subset may experience mood disturbance while using hormonal contraceptives (Lundin et al., 2017; Skovlund et al., 2016), which could lead to discontinuation of use, though factors unrelated to side effects have also been associated with discontinuation (Malmborg, Persson, Brynhildsen, & Hammar, 2016; Simmons et al., 2019). Indeed, women who went on to cease OC use had higher rates of DAD in the preceding 3 months than matched women who continued OC use. Our sensitivity analysis indicated that former OC users were at increased risk of suicidal behavior, with stronger HRs than observed in the primary analysis. This suggests that exposure to hormones is not necessarily the causal factor, though it might exacerbate an underlying disposition in some women. Additional research is necessary to clarify biological or behavioral characteristics, or environmental factors, that contribute to increased risk of suicidal behavior among young women who are former OC users. A further complicating factor may be ‘healthy user bias’, wherein individuals who suffer adverse consequences (not limited to suicidality) cease OC use, resulting in a remaining ‘users’ sample that is non-representatively healthy; this phenomenon is suspected in a previous study of OC and venous thromboembolism (Lewis, 1999).
These results should be considered in light of several limitations. The use of registry data precludes detection of suicide attempts that do not result in a medical record; however, the available records meet a consistent standard and are unaffected by concerns surrounding self-report, e.g. recall bias. We were unable to include as a comparison group women using contraception who cannot be identified using the registries, e.g. copper IUDs, condoms, etc. Where such data are available, it will be important to test whether associations with suicidal behavior differ across non-hormonal and hormonal forms of women’s contraception. We also cannot distinguish between women who are v. are not sexually active, or who are v. are not in heterosexual relationships; not only might these women use OC for different reasons, but the risk of suicidal behavior might differ across groups. In this observational study, we are unable to attribute the associations between OC and suicidal behavior to a causal relationship; confounding factors that are unaccounted for in the study design may contribute to the associations.
Due to the limited time frame during which data from the prescription registry is available, only a relatively small birth cohort could be examined. Thus, a long-term follow-up of women who used OC beyond their mid-20’s was not possible. In addition, the corresponding small sample size precluded application of a co-relative model, which would provide further insights into causality.
While we pursued several options for clarifying the role that internalizing problems may play in the relationship between OC and suicidal behavior, our method of identifying DAD using only medical records likely results in the selection of severe cases. We elected not to use pharmacy records for antidepressants due to the use of these medications for conditions other than DAD. Given the attenuation of the OC-suicidal behavior association upon inclusion of DAD in the model (see Adjusted Models 2 and 3), we suspect that identification of lower severity DAD cases would have resulted in an even more pronounced decline in the OC risks.
In conclusion, in this Swedish national sample of young women, the use of oral hormonal contraceptives was associated with a moderately increased risk of suicidal behavior. These effects are modest when viewed in the context of suicidal events per person-year, particularly for combination pills. Furthermore, though not a focus of the current study, the associations between mental illness and suicidal behavior were far more pronounced than risks conveyed by OC use. Still, our findings merit reflection by clinicians. Discussions around the initiation or continuation of OC use should include consideration of the patient’s age, duration of use (if the use has already initiated), and history of mental illness, as these factors contribute to the nuanced nature of risk. Importantly, the risk of suicidal behavior associated with OC use dissipates over time, remaining significantly elevated for approximately 1 year among combination pill users. Clinical decisions regarding OC use among young women should also consider the mental health risks associated with sexual behavior more generally, including that of unintended pregnancy (Abbasi, Chuang, Dagher, Zhu, & Kjerulff, 2013; Herd, Higgins, Sicinski, & Merkurieva, 2016).
The current study neither provides evidence nor excludes the possibility that the relationship between contraception and suicidal behavior is causal in nature and as noted in response to the Skovlund report (Hughes & Majekodunmi, 2018), does not suggest that women using a combination or progestin-only contraceptive pills should stop; rather, health care providers and women seeking contraception should factor the potential risk of adverse mental health outcomes into their decision-making process. Further research is needed to develop a comprehensive model of how the interplay of sexual activity, hormonal or other contraceptive use, psychiatric conditions, and pregnancy/post-partum periods relate to risk of suicidal behavior.
Supplementary Material
Acknowledgements.
The current study was supported by NIH grants AA027522, AA023534, and DA030005; and by Swedish Research Council and ALF funding from Region Skåne, Sweden.
Footnotes
Supplementary material. The supplementary material for this article can be found at https://doi.org/10.1017/S0033291720003475
Conflicts of interest. None.
Ethical standards. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
References
- Abbasi S, Chuang CH, Dagher R, Zhu J, & Kjerulff K (2013). Unintended pregnancy and postpartum depression among first-time mothers. Journal of Women’s Health (Larchmt), 22(5), 412–416. doi: 10.1089/jwh.2012.3926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baca-Garcia E, Perez-Rodriguez MM, Mann JJ, & Oquendo MA (2008). Suicidal behavior in young women. Psychiatric Clinics of North America, 31(2), 317–331. doi: 10.1016/j.psc.2008.01.002. [DOI] [PubMed] [Google Scholar]
- Beral V, Hermon C, Kay C, Hannaford P, Darby S, & Reeves G (1999). Mortality associated with oral contraceptive use: 25 year follow up of cohort of 46 000 women from Royal College of General Practitioners’ oral contraception study. The BMJ, 318(7176), 96–100. doi: 10.1136/bmj.318.7176.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, & Mann JJ (2005). Family genetic studies, suicide, and suicidal behavior. American Journal of Medical Genetics Part C Seminars in Medical Genetics, 133C(1), 13–24. doi: 10.1002/ajmg.c.30042. [DOI] [PubMed] [Google Scholar]
- Caminis A, Henrich C, Ruchkin V, Schwab-Stone M, & Martin A (2007). Psychosocial predictors of sexual initiation and high-risk sexual behaviors in early adolescence. Child and Adolescent Psychiatry and Mental Health, 1(1), 14. doi: 10.1186/1753-2000-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlton BM, Rich-Edwards JW, Colditz GA, Missmer SA, Rosner BA, Hankinson SE, … Michels KB (2014). Oral contraceptive use and mortality after 36 years of follow-up in the Nurses’ Health Study: Prospective cohort study. The BMJ, 349, g6356. doi: 10.1136/bmj.g6356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colditz GA (1994). Oral contraceptive use and mortality during 12 years of follow-up: The Nurses’ Health Study. Annals of Internal Medicine, 120(10), 821–826. doi: 10.7326/0003-4819-120-10-199405150-00002. [DOI] [PubMed] [Google Scholar]
- Curtin S, Warner M, & Hedegaard H (2015). Increase in suicide in the United States, 1999–2014 Hyattsville, MD: National Center for Health Statistics. Retrieved from https://www.cdc.gov/nchs/products/databriefs/db241.htm. [Google Scholar]
- Daniels K, & Abma JC (2018). Current contraceptive status among women aged 15–49: United States, 2015–2017. NCHS Data Brief, no. 327 Atlanta, GA: Centers for Disease Control and Prevention. [PubMed] [Google Scholar]
- Duke JM, Sibbritt DW, & Young AF (2007). Is there an association between the use of oral contraception and depressive symptoms in young Australian women? Contraception, 75(1), 27–31. doi: 10.1016/j.contraception.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Eaton DK, Foti K, Brener ND, Crosby AE, Flores G, & Kann L (2011). Associations between risk behaviors and suicidal ideation and suicide attempts: Do racial/ethnic variations in associations account for increased risk of suicidal behaviors among Hispanic/Latina 9thto 12th-grade female students? Archives of Suicide Research, 15(2), 113–126. doi: 10.1080/13811118.2011.565268. [DOI] [PubMed] [Google Scholar]
- Furman W, Low S, & Ho MJ (2009). Romantic experience and psychosocial adjustment in middle adolescence. Journal of Clinical Child and Adolescent Psychology, 38(1), 75–90. doi: 10.1080/15374410802575347. [DOI] [PubMed] [Google Scholar]
- Graber JA (2013). Pubertal timing and the development of psychopathology in adolescence and beyond. Hormones and Behavior, 64(2), 262–269. doi: 10.1016/j.yhbeh.2013.04.003. [DOI] [PubMed] [Google Scholar]
- Gregory ST, Hall K, Quast T, Gatto A, Bleck J, Storch EA, & DeBate R (2018). Hormonal contraception, depression, and academic performance among females attending college in the United States. Psychiatry Research, 270, 111–116. doi: 10.1016/j.psychres.2018.09.029. [DOI] [PubMed] [Google Scholar]
- Hannaford PC, Iversen L, Macfarlane TV, Elliott AM, Angus V, & Lee AJ (2010). Mortality among contraceptive pill users: Cohort evidence from Royal College of General Practitioners’ Oral Contraception Study. The BMJ, 340, c927. doi: 10.1136/bmj.c927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herd P, Higgins J, Sicinski K, & Merkurieva I (2016). The implications of unintended pregnancies for mental health in later life. American Journal of Public Health, 106(3), 421–429. doi: 10.2105/AJPH.2015.302973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes LD, & Majekodunmi O (2018). Hormonal contraception and suicide: A new dimension of risk. British Journal of General Practice, 68(676), 512–513. doi: 10.3399/bjgp18X699473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Cheslack-Postava K, Westhoff C, Heim CM, Haloossim M, Walsh K, & Koenen K (2013). Association of hormonal contraceptive use with reduced levels of depressive symptoms: A national study of sexually active women in the United States. American Journal of Epidemiology, 178(9), 1378–1388. doi: 10.1093/aje/kwt188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulkarni J (2007). Depression as a side effect of the contraceptive pill. Expert Opinion on Drug Safety, 6(4), 371–374. doi: 10.1517/14740338.6.4.371. [DOI] [PubMed] [Google Scholar]
- Lewis MA (1999). The transnational study on oral contraceptives and the health of young women. Methods, results, new analyses and the healthy user effect. Human Reproduction Update, 5(6), 707–720. doi: 10.1093/humupd/5.6.707. [DOI] [PubMed] [Google Scholar]
- Lundin C, Danielsson KG, Bixo M, Moby L, Bengtsdotter H, Jawad I, … Sundstrom Poromaa I (2017). Combined oral contraceptive use is associated with both improvement and worsening of mood in the different phases of the treatment cycle-A double-blind, placebo-controlled randomized trial. Psychoneuroendocrinology, 76, 135–143. doi: 10.1016/j.psyneuen.2016.11.033. [DOI] [PubMed] [Google Scholar]
- Malmborg A, Persson E, Brynhildsen J, & Hammar M (2016). Hormonal contraception and sexual desire: A questionnaire-based study of young Swedish women. European Journal of Contraception and Reproductive Health Care, 21(2), 158–167. doi: 10.3109/13625187.2015.1079609. [DOI] [PubMed] [Google Scholar]
- Mangla K, Hoffman MC, Trumpff C, O’Grady S, & Monk C (2019). Maternal self-harm deaths: An unrecognized and preventable outcome. American Journal of Obstetrics and Gynecology, 221(4), 295–303. doi: 10.1016/j.ajog.2019.02.056. [DOI] [PubMed] [Google Scholar]
- Marrocco J, & McEwen BS (2016). Sex in the brain: Hormones and sex differences. Dialogues in Clinical Neuroscience, 18(4), 373–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS, & Milner TA (2017). Understanding the broad influence of sex hormones and sex differences in the brain. Journal of Neuroscience Research, 95(1–2), 24–39. doi: 10.1002/jnr.23809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mota NP, Chartier M, Ekuma O, Nie Y, Hensel JM, MacWilliam L, … Bolton JM (2019). Mental disorders and suicide attempts in the pregnancy and postpartum periods compared with non-pregnancy: A population-based study. Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie, 64(7), 482–491. doi: 10.1177/0706743719838784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oinonen KA, & Mazmanian D (2002). To what extent do oral contraceptives influence mood and affect? Journal of Affective Disorders, 70(3), 229–240. doi: 10.1016/s0165-0327(01)00356-1. [DOI] [PubMed] [Google Scholar]
- Orri M, Gunnell D, Richard-Devantoy S, Bolanis D, Boruff J, Turecki G, & Geoffroy M-C (2019). In-utero and perinatal influences on suicide risk: A systematic review and meta-analysis. The Lancet Psychiatry, 6(6), 477–492. doi: 10.1016/s2215-0366(19)30077-x. [DOI] [PubMed] [Google Scholar]
- Pagano HP, Zapata LB, Berry-Bibee EN, Nanda K, & Curtis KM (2016). Safety of hormonal contraception and intrauterine devices among women with depressive and bipolar disorders: A systematic review. Contraception, 94(6), 641–649. doi: 10.1016/j.contraception.2016.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen NL, & Fiske A (2010). Genetic influences on suicide and nonfatal suicidal behavior: Twin study findings. European Psychiatry, 25(5), 264–267. doi: 10.1016/j.eurpsy.2009.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piscopo K, Lipari RN, Cooney J, & Glasheen C (2016). Suicidal thoughts and behavior among adults: results from the 2015 national survey on drug use and health Rockville, MD: Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/sites/default/files/NSDUH-DR-FFR3-2015/NSDUH-DR-FFR3-2015.htm. [Google Scholar]
- Robakis T, Williams KE, Nutkiewicz L, & Rasgon NL (2019). Hormonal contraceptives and mood: Review of the literature and implications for future research. Current Psychiatry Reports, 21(7), 57. doi: 10.1007/s11920-019-1034-z. [DOI] [PubMed] [Google Scholar]
- Simmons RG, Sanders JN, Geist C, Gawron L, Myers K, & Turok DK (2019). Predictors of contraceptive switching and discontinuation within the first 6 months of use among Highly Effective Reversible Contraceptive Initiative Salt Lake study participants. American Journal of Obstetrics and Gynecology, 220(4), 376, e371–376 e312. doi: 10.1016/j.ajog.2018.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skovlund CW (2018). Clarifying methods and results in studies of the association between hormonal contraception and mental health issues: Response to Berlin et al. American Journal of Psychiatry, 175(7), 684–684. doi: 10.1176/appi.ajp.2018.18010057r. [DOI] [PubMed] [Google Scholar]
- Skovlund CW, Morch LS, Kessing LV, Lange T, & Lidegaard O (2018). Association of hormonal contraception with suicide attempts and suicides. American Journal of Psychiatry, 175(4), 336–342. doi: 10.1176/appi.ajp.2017.17060616. [DOI] [PubMed] [Google Scholar]
- Skovlund CW, Morch LS, Kessing LV, & Lidegaard O (2016). Association of hormonal contraception with depression. JAMA Psychiatry, 73(11), 1154–1162. doi: 10.1001/jamapsychiatry.2016.2387. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (2018). Key substance use and mental health indicators in the United States: Results from the 2017 national survey on drug use and health Rockville, MD: Substance Abuse and Mental Health Services Administration. Retrieved from http://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHFFR2017/NSDUHFFR2017.htm. [Google Scholar]
- Svendal G, Berk M, Pasco JA, Jacka FN, Lund A, & Williams LJ (2012). The use of hormonal contraceptive agents and mood disorders in women. Journal of Affective Disorders, 140(1), 92–96. doi: 10.1016/j.jad.2012.03.030. [DOI] [PubMed] [Google Scholar]
- Toffol E, Heikinheimo O, Koponen P, Luoto R, & Partonen T (2011). Hormonal contraception and mental health: Results of a population-based study. Human Reproduction, 26(11), 3085–3093. doi: 10.1093/humrep/der269. [DOI] [PubMed] [Google Scholar]
- Toffol E, Heikinheimo O, Koponen P, Luoto R, & Partonen T (2012). Further evidence for lack of negative associations between hormonal contraception and mental health. Contraception, 86(5), 470–480. doi: 10.1016/j.contraception.2012.02.014. [DOI] [PubMed] [Google Scholar]
- United Nations (2015). Trends in contraceptive Use worldwide 2015 (ST/ESA/SER.A/349) New York: United Nations Department of Economic and Social Affairs Population Division. [Google Scholar]
- Vessey MP, Villard-Mackintosh L, McPherson K, & Yeates D (1989). Mortality among oral contraceptive users: 20 year follow up of women in a cohort study. The BMJ, 299(6714), 1487–1491. doi: 10.1136/bmj.299.6714.1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White K, Potter JE, Hopkins K, Fernandez L, Amastae J, & Grossman D (2012). Contraindications to progestin-only oral contraceptive pills among reproductive-aged women. Contraception, 86(3), 199–203. doi: 10.1016/j.contraception.2012.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Reproductive Health and Research (2010). Medical eligibility criteria for contraceptive use (4th ed.). Geneva: Department of Reproductive Health and Research, World Health Organization. [Google Scholar]
- Worly BL, Gur TL, & Schaffir J (2018). The relationship between progestin hormonal contraception and depression: A systematic review. Contraception, 97(6), 478–489. doi: 10.1016/j.contraception.2018.01.010. [DOI] [PubMed] [Google Scholar]
- Zethraeus N, Dreber A, Ranehill E, Blomberg L, Labrie F, von Schoultz B, … Hirschberg AL (2017). A first-choice combined oral contraceptive influences general well-being in healthy women: A double-blind, randomized, placebo-controlled trial. Fertility and Sterility, 107(5), 1238–1245. doi: 10.1016/j.fertnstert.2017.02.120. [DOI] [PubMed] [Google Scholar]
- Zettermark S, Perez Vicente R, & Merlo J (2018). Hormonal contraception increases the risk of psychotropic drug use in adolescent girls but not in adults: A pharmacoepidemiological study on 800 000 Swedish women. PLoS One, 13(3), e0194773. doi: 10.1371/journal.pone.0194773. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


